Abstract
Purpose
Lung cancer screening (LCS) by low-dose computed tomography (LDCT) demonstrated a 20–40% reduction in lung cancer mortality. National stakeholders and international scientific societies are increasingly endorsing LCS programs, but translating their benefits into practice is rather challenging. The “Model for Optimized Implementation of Early Lung Cancer Detection: Prospective Evaluation Of Preventive Lung HEalth” (PEOPLHE) is an Italian multicentric LCS program aiming at testing LCS feasibility and implementation within the national healthcare system. PEOPLHE is intended to assess (i) strategies to optimize LCS workflow, (ii) radiological quality assurance, and (iii) the need for dedicated resources, including smoking cessation facilities.
Methods
PEOPLHE aims to recruit 1.500 high-risk individuals across three tertiary general hospitals in three different Italian regions that provide comprehensive services to large populations to explore geographic, demographic, and socioeconomic diversities. Screening by LDCT will target current or former (quitting < 10 years) smokers (> 15 cigarettes/day for > 25 years, or > 10 cigarettes/day for > 30 years) aged 50–75 years. Lung nodules will be volumetric measured and classified by a modified PEOPLHE Lung-RADS 1.1 system. Current smokers will be offered smoking cessation support.
Conclusion
The PEOPLHE program will provide information on strategies for screening enrollment and smoking cessation interventions; administrative, organizational, and radiological needs for performing a state-of-the-art LCS; collateral and incidental findings (both pulmonary and extrapulmonary), contributing to the LCS implementation within national healthcare systems.
Keywords: Lung cancer, Lung cancer screening, Low-dose computed tomography, Lung-RADS, Primary and secondary prevention
Introduction
Lung cancer (LC) is the leading cause of oncologic morbidity and mortality worldwide; accounting for 2.2 million new diagnoses and 1.8 million deaths in 2020 (18% of all cancer deaths) [1]. In Italy, the current prognosis of LC is as poor as 15.9% survival at 5 years after diagnosis [2]. The high mortality rate of LC is related to diagnosis in the advanced stage with limited curative options; hence, control of LC mortality is expected from secondary prevention by early diagnosis with LC screening (LCS), as well as primary prevention by smoking cessation.
Several trials demonstrated 20–40% reduction of LC mortality by low-dose computed tomography (LDCT) screening, which is increasingly endorsed by national stakeholders and international scientific societies [3, 4]. However, the translation of LCS benefits from trial to the general population is challenging, as shown by the US experience where LCS is being reimbursed through Medicare since 2015 [5]. The European Commission is shaping plans to tackle the recognized hurdles of LCS [6]:
Engagement of high-risk individuals, usually nested in the most fragile socioeconomic strata [5, 7].
Maintaining high participation rates during the various time points, which is tackled by the “satisfaction effect” after a first negative screen with consequent drop in the adherence to LCS [8].
Continuous quality assurance for optimization of resources and reduction of risks (related to work up and radiation exposure)
In 2021, the “Model for Optimized Implementation of Early Lung Cancer Detection: Prospective Evaluation Of Preventive Lung HEalth” (PEOPLHE) —an Italian multicentric LCS program—was launched to test the feasibility and implementation of LCS within the national healthcare system. PEOPLHE addresses specific LCS issues (e.g., enrollment strategies, adherence to LCS rounds, and adherence to smoking cessation programs), testing the feasibility of LCS by sampling three geographically heterogeneous environments through the Italian territory. PEOPLHE is intended to describe:
The impact of LCS by assessing strategies to optimize LCS workflow, radiological quality assurance and the need for dedicated resources, including smoking cessation facilities.
Quantifying the impact of LCS on life expectancy of high-risk subjects by evaluating standard outcomes, including the proportion of early-stage LC, the number of limited resection surgeries, and surgical approaches performed for benign diseases.
Material and methods
Study design
PEOPLHE is a three-year multicentric project supported by the Italian Ministry of Health (MOH) (RF-2019-12371462).
PEOPLHE aims at recruiting 1.500 high-risk individuals across 3 tertiary general hospitals (500 screenees for each center) that are community-based and provide comprehensive services to large populations of three Italian regions, including thoracic oncology multidisciplinary team. The multicentric design aims at exploring geographic, demographic, and socioeconomic diversities that might hamper the implementation of Italian LCS practice.
Selection criteria were derived from the NELSON trial [9], as follows: (i) 50–75 years of age; (ii) smoking habit of > 15 cigarettes/day for > 25 years or > 10 cigarettes/day for > 30 years; (iii) current or former smoker quitting < 10 years; (iiii) no history of cancer in the previous five years.
Study sites
Parma (Emilia Romagna; coordinating center), hereafter called Unit 1: Parma is a medium-sized city (about 200.000 inhabitants) in Northern Italy; its greater area comprises more than 450.000 citizens.
Pavia (Lombardy), Unit 2: Pavia is a small/medium-sized city (about 70.000 inhabitants) in Northern Italy; its greater area comprises more than 500.000 citizens.
Catania (Sicily), Unit 3: Catania is a medium-sized city (about 300.000 inhabitants), in Southern Italy; its greater area comprises than 1.100.000 citizens.
Screenees enrollment
PEOPLHE enrollment focuses on a) systematic recruitment of eligible subjects, b) involvement of general practitioners (GP), c) efficiency of referral to LCS hub, and d) capacity needs.
Noteworthy, PEOPLHE was designed before the pandemic of severe acute respiratory distress syndrome coronavirus 2 (SARS-CoV-2), when the peripheral network of GPs was hypothesized to leverage LCS toward the population. However, this structure needed to be converted to cope with the increased workload following the pandemic. Furthermore, tailored approaches are needed to guarantee safe management of patients, screenees and healthcare personnel [10].
The informative campaign rolled out at different levels:
Media level: local and institutional newspapers, social media pages, local television networks on health-dedicated shows. Dedicated informative events were hosted during national anti-tobacco days.
Hospital level: flyers and roll-ups of the PEOPLHE trial reporting study objectives, inclusion criteria, and contacts (email, phone, and QR code toward the subscription website) were placed in the radiology and pneumology departments of the three Units.
Healthcare providers level: dedicated conferences involving local GPs, pulmonologists, and any healthcare provider.
Administrative and organizational needs
PEOPLHE will assess and quantify the need for dedicated healthcare providers across the full range from recruitment to LC treatment, focusing on radiology department needs, including data managers and administrative staff, radiographers, smoking cessation providers, radiologists, and multidisciplinary teams.
Smoking cessation
Questionnaires on nicotine addiction will be filled at baseline, at 12 and 24 months, thus recording information on potential variation in the smoking habit over time. The source of information will be the Fagerstrom Test for nicotine dependence. This relatively fast test allows the stratification of four categories of smokers (ranging from low dependence to high dependence).
The PEOPLHE researchers will suggest participation to anti-smoking centres during baseline and recall rounds, providing information on access routes and contacts.
Radiological quality assurance
The workload of LDCT and multidisciplinary management needs to be defined to estimate the required capacity to deliver a new healthcare service such as LCS.
Radiological requirements.
The radiological capacity includes performing CT scanners for low-dose imaging and radiologists experienced in thoracic imaging. The PEOPLHE employs highly performing CT scanners and is coordinated by medical staff with long-standing experience in LCS [11–14].
CT scanning protocols
CT examinations will be performed according to state-of-the-art technical requirements. Radiation exposure will be maintained as low as reasonably achievable, providing qualitative standards to detect and characterize pulmonary nodules using CT scanners equipped with advanced CT image acquisition systems and radiation dose reduction systems at all Units (e.g., automatic current modulation systems, high sensitivity detectors, iterative reconstruction algorithms); meanwhile, the scanner at Unit 1 will also be equipped with X-ray beam filtration for maximized reduction of radiation exposure (e.g., tin filter). Table 1 details the scanning protocols of each unit.
Table 1.
Technical information on the CT acquisition protocols of each unit
| Unit 1 (Parma) | Unit 2 (Pavia) | Unit 3 (Catania) | |
|---|---|---|---|
| CT scanner | SIEMENS go.TOP | SIEMENS SOMATOM DEFINITION | GENERAL ELECTRIC Optima 660 |
| Tube voltage | Sn100 | 100 | 120 |
| Tube current | CARE kV Quality ref. mAs@120 kV = 6 | CARE Kv 4D—3 mAs | Noise index 30 (10–40) |
| Pitch | 0.8 | 1 | 0.984 |
| Rotation time | 0.33 | 0.5 s | 0.5 s |
| Reconstruction 1 | |||
| Kernel | Br48 | B50f medium sharp | Bone plus |
| Slice thickness | 1 mm | 1 mm | 0.625 mm |
| Slice increment | 0.7 mm | 0.7 mm | 0.625–1.250 |
| IR | SAFIRE 3 | – | – |
| Window | Lung | Lung | Lung |
| Reconstruction 2 | |||
| Kernel | Sa36 | B31f medium smooth + | Detail |
| Slice thickness | 3 mm | 3 mm | 2.5 mm |
| Slice increment | 1.5 mm | 1.5 mm | 1.25 mm |
| IR | SAFIRE 3 | – | – |
| Window | Mediastinum | Mediastinum | Mediastinum |
| Reconstruction 3 | |||
| Kernel | Sa36 | B31f medium smooth + | Detail |
| Slice thickness | 1 mm | 1 mm | 1.25 mm |
| Slice increment | 0.7 mm | 0.7 mm | 0.6–1.25 mm |
| IR | SAFIRE 3 | – | – |
| Window | Lung | Lung | Bone |
| CAD software | MM Oncology (SIEMENS Healthineers) | Nodule Detection (Philips Intellispace Portal) | Lung VCAR (General Electric Healthcare) |
| Volumetry measured on | Reconstruction 3 | Reconstruction 3 | Reconstruction 3 |
SAFIRE Sinogram affirmed iterative reconstruction
Scheduling LCS
Trial activities will be held during dedicated LCS time slots: days and daytimes will be tested, and screenees’ preferences recorded.
Unit 1: different LCS slots will be tested to fulfil participants' preferences (e.g., Monday/Friday afternoon, or Saturday morning).
Unit 2: dedicated LCS slot will include different LCS slots will be tested to fulfil participants' preferences (e.g., Monday/Friday afternoon).
Unit 3: dedicated LCS slot will include Friday and Saturday afternoons.
Tailored appointments will be proposed for those screenees for whom participation during the abovementioned LCS slot will not be possible.
The hypothesis behind the organization of dedicated LCS time slots is that it could optimize LCS resources through and homogeneous workflow.
LDCT reading, reporting and management of nodules
A single radiologist with CAD as second reader will read LDCT scans. Pulmonary nodules will be measured with volumetric approach. LDCT outcome will be based on Lung Imaging Reporting and Data System (Lung-RADS) version 1.1 [15], with biennial round for subjects with negative LDCT, as they were demonstrated to be safe in Italian and Dutch trials and granting a 30% reduction in radiological workload [11, 16–18].
Based on previous LCS data, the screening algorithm will be set on the following LDCT intervals, according to the dominant lesion:
24-month interval: Lung-RADS 1 or solid nodule Lung-RADS 2
12-month interval: sub-solid nodule included in the dimensional thresholds of Lung-RADS 2
6-month interval: solid nodules Lung-RADS 3
3-month interval: Lung-RADS 4A
Work up: Lung-RADS 4B and 4X.
The proposed algorithm will mostly parallel Lung-RADS 1.1 scheme, except for point a) [15].
For CT findings requiring action, management will be based on multidisciplinary management per daily clinical practice.
Management of collateral and incidental findings
LDCT findings other than pulmonary nodules are classified as:
- “collateral findings”, which include smoking-related abnormalities such as calcifications of coronary arteries, pulmonary emphysema, respiratory bronchiolitis, and interstitial pulmonary abnormality/disease;
Coronary artery calcification
Coronary artery calcium (CAC) will be visually scored by a four-point severity scale (0: no CAC; 1: mild CAC—only isolated flecks within a segment; 2: moderate CAC—intermediate CAC between mild and heavy; 3: heavy CAC—continuous CAC within a segment) in each coronary artery (left main, left anterior descending, left circumflex, right coronary artery).
Emphysema
Emphysema will be assessed using a semi-quantitative visual scoring method based on a 5-category extent (absent, <5%, 5-25%, 25-50%, > 50%) and will include morphological description (e.g., centrilobular, paraseptal, advanced).
Interstitial lung abnormality/disease
Detection of nondependent abnormalities affecting more than 5% of any lung zone identified in subjects without known or suspected interstitial lung diseases (ILD) will be classified as interstitial lung abnormalities (ILA) [19]. Both ILA and ILD will be classified according to current guidelines, including evaluation of distribution (subpleural or non-subpleural), presence of fibrosis (fibrotic or non-fibrotic), and extent (5%-point scale). Frequency, morphology and extent will be recorded, as well as the number of screenees referred to multidisciplinary evaluation.
- “incidental findings”, which encompass non-smoking-related abnormalities [20].
Both collateral and incidental findings will be detailed in the LCS report and managed according to the Quality Assurance Standards prepared for the Targeted Lung Health Checks Programme from the National Health Service (NHS) England. Interventions prompted by detecting these findings on LDCT for LCS will be recorded. The discrepancy between the number of assigned Lung-RADS category “S” and the number of additional investigations will help in defining the cost-efficacy of LCS.
Data collection and management
Investigators will collect and manage data locally at each site; subsequently, all data will be securely transferred to Unit 1 for quality controls and analysis.
Scientific output
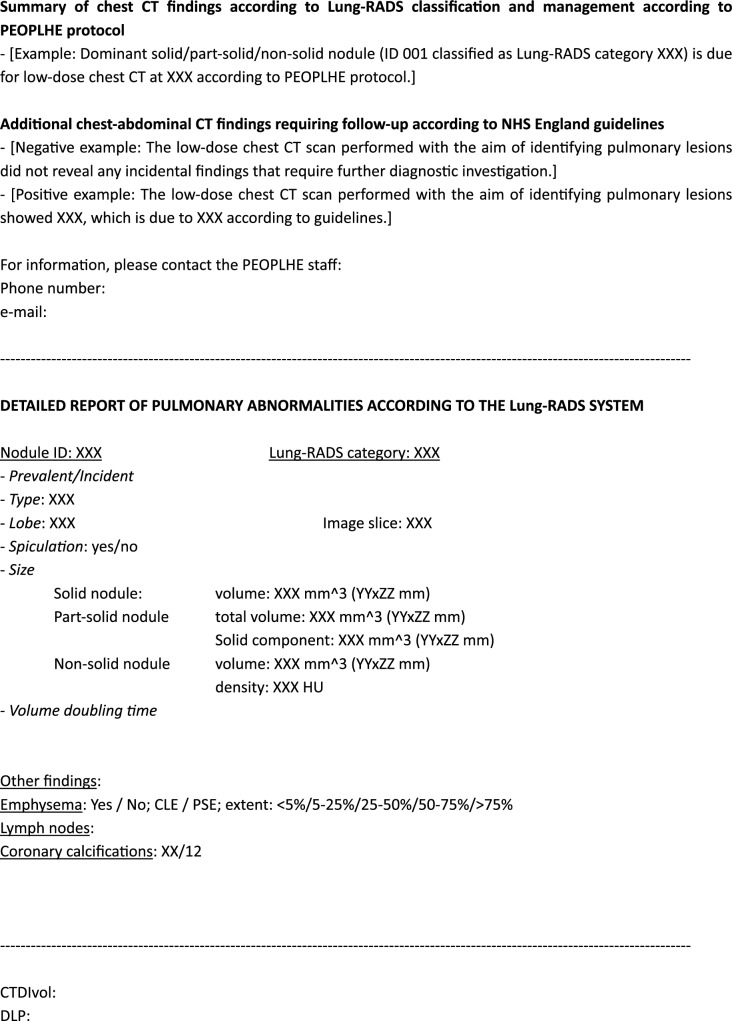
The first scientific manuscript for the PEOPLHE project will describe the baseline round results, including the strategies used to prompt the enrollment of screenees. Subsequent papers will detail the impact of collateral and incidental findings, and how many diagnostic procedures were requested for findings other than lung cancer (Fig. 1).
Fig. 1.
Template of the structured report used within the PEOPLHE project. The first section summarizes the findings: including this information as the first paragraph was intended to increase readability and comprehension for both GPs and screenees; contact details are reported to allow easy interaction with the researchers. Subsequently, we designed a second paragraph including detailed results of LDCT reading (focused on both pulmonary nodules and other findings). The last section of the structured report includes data on radiation exposure and the study protocol.
Ethics
The Institutional Review Boards of each Unit approved the study protocol. Before each baseline LDCT, written information on benefits and harms of LCS will be provided and informed consent will be obtained from all screenees. The study was conducted carefully following the indication from Dlgs 101/20 on radiological screening. Participants will be informed about the goals of LCS, along with its potential positive and negative consequences and limitations.
Discussion
The convincing evidence of LC mortality reduction in large randomized controlled trials ought to European endorsement of LCS implementation. Italy does not currently have a LCS program, but its implementation is being discussed and will be supported by analysis of other ongoing LCS programs [20]. PEOPLHE will address several important issues relevant to the implementation of LCS. It will aim at apportioning the workload and capacity needed for implementation of LCS, including lung cancer screening outcomes and the clinical management of incidental findings. PEOPLHE will also assess the effect, if any, of invitation to LCS has on smoking rates, which was heterogeneous in previous studies and it is known to be subject to bias related to selecting people willing to engage in a research study for health improvement [21–23]. The information from three tertiary Italian hospitals located in different geographical areas is expected to cover a range of geographical and organizational variables.
Administrative and organizational needs.
A major LCS challenge is represented by the lack of systematic and coordinated support, especially for a site first approaching LCS activities, which would be the potential situation of almost all Italian hospitals [24]. By reporting the experience of three academic hospitals, we aim to identify the needed up-front infrastructural and manpower investments.
Enrollment and engagement strategies.
Identified barriers hampering LCS participation include travel issues or psychological factors (anxiety and stigma), which negatively impact a person’s motivation to attend [25, 26]. Uptake and adherence disparities were potentially related to structural barriers preventing receipt of equitable care, lower socioeconomic status and difficulties in obtaining reimbursements [27–29].
Participation of high-risk populations can be enriched through tailored communication strategies with several invitation approaches, or by offering a mobile setting [30, 31]. The PEOPLHE trial will test the role of telephone triage to present the trial, foster participation of screenees, and organize LCS appointments. A similar approach was previously proposed by the Yorkshire Lung Screening Trial (YLST) in the United Kingdom [7]. Centralization of LDCT in a tertiary hospital is the way to specialized thoracic radiologists and state-of-the-art technology (high-performance scanner, CAD tools, and volumetric nodule measurement). Moreover, the use of mobile CT scanners is associated with higher costs and it seems that scanner location is not the main determinant of LCS uptake [32].
Notably, a minor trust in LCS has been recently reported to challenge LCS implementation in the US, while knowledge of LCS guidelines is a strong and independent predictor for a higher likelihood of suggesting LCS by several healthcare providers [29, 33]. To increase the awareness of the advantages related to LCS, the PEOPLHE staff organized several meetings, both online and in-person, with GPs and other healthcare providers, seeking support from local health associations for recruiting screenees, as well as social media campaigns [34]. A similar role for these health associations has been endorsed by Swiss experts [35].
Previous literature reported generally large rates of drop-out from LCS [36]. We will assess the need for human and financial resources to ensure screenees engagement. Focused analyses of drop-off from LCS based on LDCT outcome categories will be performed, as previous experiences reported higher rates of “no-shows” in subjects with baseline Lung-RADS 3 to 4 as compared with Lung-RADS 1 to 2 [37]. Although potentially affected by the relatively limited time-span of our study, we will explore whether the possibility of low adherence after the baseline round can be counteracted by an NSLT-like active approach, including the administration of annual questionnaires on smoking habit and periodic telephone calls and e-mails.
Smoking cessation.
Smoking cessation is the most effective strategy for reducing LC mortality and morbidity. A legitimate concern arose about the possibility that current smokers might consider LCS as a surrogate for an excuse to continue smoking, due to reassurance from a “negative” LDCT. On the other hand, LCS can positively affect smoking cessation among smokers who undergo screening and anti-tobacco counselling [38, 39].
Combined psychological and pharmacologic support have been reported to increase quit rates, with favorable cost-effectiveness ratio when antismoking therapy of natural origin is introduced or when smoking cessation services are proposed immediately after a Target Lung Health Check [14, 40]. However, rates of decline have slowed, and certain categories, namely “hardcore smokers” including smokers less willing to quit, heavy smokers, and who exhibit high-level nicotine dependence, show resistance to tobacco control measures [41–43].
PEOPLHE—by integrating a strict anti-tobacco activity—will record the number of subjects quitting smoking, and the characteristics of both quitters and “hardcore smokers”, expanding the available literature on the topic with potential perspectives on strategies to improve quitting.
LDCT acquisition, reading and reporting.
Current recommendations suggest annual LCS throughout a long-time span (up to 25 years) [3] LDCT-based LCS might be associated with the potential risk of radiation-induced LC [44]. Balancing the positive impact of LCS on LC mortality with the risks of radiation exposure is one major focus of LCS literature. Recent improvements in CT hardware and software fostered a great interest in reducing the radiation burden beyond the current state-of-the-art in thoracic imaging (LDCT) toward imaging at a calculated radiation dose of below 1 milliSievert, termed ultra-low-dose CT (ULDCT) [45, 46].
The cost-effectiveness of LCS might vary substantially as it is implemented in real-world settings depending on screenees’ selection, false-positive rate, and rates of invasive procedures. Two independent radiologists have usually performed LCS reading, causing an increased cost for LC [47]. Therefore, the implementation of CAD tools within the workflow can reduce costs and reduce variability in detection rates, with the advantage of reducing the risk of false-negative LDCTs, especially for small pulmonary nodules and nodules in peri-hilar regions [20, 48, 49].
LDCT reports produced in the PEOPLHE trial will be standardized, containing all information bolstered by the European Society of Thoracic Imaging (ESTI) [50]. The PEOPLHE LDCT report has been developed to minimize misunderstandings between screenees and healthcare providers. The outcome and suggested management are clearly stated in the first paragraph, followed by more detailed information; during dedicated phone calls from healthcare providers (trained radiology residents, data managers, experienced radiologists), indeterminate and positive findings and further actions (including the timing of follow-ups or additional investigations) will be discussed.
The PEOPLHE program will provide relevant information on administrative and organizational needs for implementation of lung cancer screening within national healthcare system.
Acknowledgements
The Corresponding Author accepts to undertake all the responsibility for authorship during the submission and review stages of our manuscript.
Author contributions
NS, MS, GM and EI contributed to the study conception and design. The first draft of the manuscript was written by Gianluca Milanese and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Open access funding provided by Università degli Studi di Parma within the CRUI-CARE Agreement. The PEOPLHE trial is supported by grants from the Italian Ministry of Health (RF 2019-12371462). The sponsors had no role in conducting and interpreting the study.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of each Institution.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nicola Sverzellati, Email: nicola.sverzellati@unipr.it.
the PEOPLHE consortium:
Lorenzo Aliotta, Sebastiano Barbarino, Santo Borzì, Virginia Casotto, Marco Catalano, Domenico Maria Cavalieri, Mariangela Clemenza, Martina Contino, Luca Crimi, Bruno Curia, Pasquale Favia, Vita Ida Gallone, Giulia Guicciardi, Giuliana La Rosa, Ludovica Leo, Rebecca Mura, Antonella Priore, Lidia Ruongo, Carlotta Scavone, and Carlotta Zilioli
References
- 1.Sung H, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Allemani C, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kauczor HU, et al. ESR/ERS statement paper on lung cancer screening. Eur Radiol. 2020;30(6):3277–3294. doi: 10.1007/s00330-020-06727-7. [DOI] [PubMed] [Google Scholar]
- 4.Baldwin D et al. (2023) Developing a Pan-European technical standard for a comprehensive high-quality lung cancer CT screening program: an ERS technical standard. Eur Respir J [DOI] [PubMed]
- 5.Silvestri GA, et al. Characteristics of persons screened for lung cancer in the united states : a cohort study. Ann Intern Med. 2022;175(11):1501–1505. doi: 10.7326/M22-1325. [DOI] [PubMed] [Google Scholar]
- 6.Ward B, et al. Important steps towards a big change for lung health: a joint approach by the European Respiratory Society, the European Society of Radiology and their partners to facilitate implementation of the European Union's new recommendations on lung cancer screening. ERJ Open Res. 2023 doi: 10.1183/23120541.00026-2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crosbie PAJ et al. (2022) Participation in community-based lung cancer screening: the Yorkshire Lung Screening Trial. Eur Respir J. 60(5) [DOI] [PMC free article] [PubMed]
- 8.Silvestri GA, et al. Outcomes from more than 1 million people screened for lung cancer with low-dose CT imaging. Chest. 2023;164:18. doi: 10.1016/j.chest.2023.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Koning HJ, et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med. 2020;382(6):503–513. doi: 10.1056/NEJMoa1911793. [DOI] [PubMed] [Google Scholar]
- 10.Milanese G, et al. Feasibility and safety of lung cancer screening and prevention program during the COVID-19 pandemic. Chest. 2021;160(1):e5–e7. doi: 10.1016/j.chest.2021.02.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pastorino U, et al. Baseline computed tomography screening and blood microRNA predict lung cancer risk and define adequate intervals in the BioMILD trial. Ann Oncol. 2022;33(4):395–405. doi: 10.1016/j.annonc.2022.01.008. [DOI] [PubMed] [Google Scholar]
- 12.Pastorino U, et al. Prolonged lung cancer screening reduced 10-year mortality in the MILD trial: new confirmation of lung cancer screening efficacy. Ann Oncol. 2019;30(7):1162–1169. doi: 10.1093/annonc/mdz117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Veronesi G, et al. Lung cancer screening with low-dose computed tomography: a non-invasive diagnostic protocol for baseline lung nodules. Lung Cancer. 2008;61(3):340–349. doi: 10.1016/j.lungcan.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 14.Pastorino U, et al. Cytisine therapy improved smoking cessation in the randomized screening and multiple intervention on lung epidemics lung cancer screening trial. J Thorac Oncol. 2022;17:1276. doi: 10.1016/j.jtho.2022.07.007. [DOI] [PubMed] [Google Scholar]
- 15.https://www.acr.org/-/media/ACR/Files/RADS/Lung-RADS/LungRADSAssessmentCategoriesv1-1.pdf?la=en
- 16.Sverzellati N, et al. Low-dose computed tomography for lung cancer screening: comparison of performance between annual and biennial screen. Eur Radiol. 2016;26(11):3821–3829. doi: 10.1007/s00330-016-4228-3. [DOI] [PubMed] [Google Scholar]
- 17.Pastorino U, et al. Ten-year results of the Multicentric Italian Lung Detection trial demonstrate the safety and efficacy of biennial lung cancer screening. Eur J Cancer. 2019;118:142–148. doi: 10.1016/j.ejca.2019.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yousaf-Khan U, et al. Final screening round of the NELSON lung cancer screening trial: the effect of a 2.5-year screening interval. Thorax. 2017;72(1):48–56. doi: 10.1136/thoraxjnl-2016-208655. [DOI] [PubMed] [Google Scholar]
- 19.Tomassetti S et al. (2022) Incidental discovery of interstitial lung disease: diagnostic approach, surveillance and perspectives. Eur Respir Rev. 31(164) [DOI] [PMC free article] [PubMed]
- 20.Silva M, et al. Low-dose CT for lung cancer screening: position paper from the Italian college of thoracic radiology. Radiol Med. 2022;127(5):543–559. doi: 10.1007/s11547-022-01471-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van der Aalst CM, et al. Lung cancer screening and smoking abstinence: 2 year follow-up data from the Dutch-Belgian randomised controlled lung cancer screening trial. Thorax. 2010;65(7):600–605. doi: 10.1136/thx.2009.133751. [DOI] [PubMed] [Google Scholar]
- 22.Brain K, et al. Impact of low-dose CT screening on smoking cessation among high-risk participants in the UK Lung Cancer Screening Trial. Thorax. 2017;72(10):912–918. doi: 10.1136/thoraxjnl-2016-209690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ashraf H, et al. Smoking habits in the randomised Danish Lung Cancer Screening Trial with low-dose CT: final results after a 5-year screening programme. Thorax. 2014;69(6):574–579. doi: 10.1136/thoraxjnl-2013-203849. [DOI] [PubMed] [Google Scholar]
- 24.Buehler KE, et al. Imaging administrators: the overlooked barrier to lung cancer screening implementation. Chest. 2022;161(2):583–585. doi: 10.1016/j.chest.2021.07.005. [DOI] [PubMed] [Google Scholar]
- 25.Ali N, et al. Barriers to uptake among high-risk individuals declining participation in lung cancer screening: a mixed methods analysis of the UK Lung Cancer Screening (UKLS) trial. BMJ Open. 2015;5(7):e008254. doi: 10.1136/bmjopen-2015-008254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quaife SL, et al. Psychological targets for lung cancer screening uptake: a prospective longitudinal cohort study. J Thorac Oncol. 2021;16(12):2016–2028. doi: 10.1016/j.jtho.2021.07.025. [DOI] [PubMed] [Google Scholar]
- 27.Nunez ER, et al. Factors associated with declining lung cancer screening after discussion with a physician in a cohort of US veterans. JAMA Netw Open. 2022;5(8):e2227126. doi: 10.1001/jamanetworkopen.2022.27126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tailor TD, et al. Utilization of lung cancer screening in the medicare fee-for-service population. Chest. 2020;158(5):2200–2210. doi: 10.1016/j.chest.2020.05.592. [DOI] [PubMed] [Google Scholar]
- 29.Melzer AC, et al. "We just never have enough time": clinician views of lung cancer screening processes and implementation. Ann Am Thorac Soc. 2020;17:1264. doi: 10.1513/AnnalsATS.202003-262OC. [DOI] [PubMed] [Google Scholar]
- 30.Crosbie PA, et al. Implementing lung cancer screening: baseline results from a community-based 'Lung Health Check' pilot in deprived areas of Manchester. Thorax. 2019;74(4):405–409. doi: 10.1136/thoraxjnl-2017-211377. [DOI] [PubMed] [Google Scholar]
- 31.Revel MP, et al. Lung cancer screening in french women using low-dose CT and artificial intelligence for detection: the CASCADE study protocol. BMJ Open. 2022;12(12):e067263. doi: 10.1136/bmjopen-2022-067263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bartlett EC, et al. Baseline results of the west london lung cancer screening pilot study—impact of mobile scanners and dual risk model utilisation. Lung Cancer. 2020;148:12–19. doi: 10.1016/j.lungcan.2020.07.027. [DOI] [PubMed] [Google Scholar]
- 33.Lewis JA, et al. Low provider knowledge is associated with less evidence-based lung cancer screening. J Natl Compr Canc Netw. 2019;17(4):339–346. doi: 10.6004/jnccn.2018.7101. [DOI] [PubMed] [Google Scholar]
- 34.Strong A, Renaud M. Using social media as a platform for increasing knowledge of lung cancer screening in high-risk patients. J Adv Pract Oncol. 2020;11(5):453–459. doi: 10.6004/jadpro.2020.11.5.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jungblut L, et al. The Swiss Approach: feasibility of a national low-dose CT lung cancer screening program. Swiss Med Wkly. 2022;152:15–16. doi: 10.4414/SMW.2022.w30154. [DOI] [PubMed] [Google Scholar]
- 36.Tanner NT, et al. Screening adherence in the veterans administration lung cancer screening demonstration project. Chest. 2020;158(4):1742–1752. doi: 10.1016/j.chest.2020.04.063. [DOI] [PubMed] [Google Scholar]
- 37.Lin Y, et al. Patient adherence to lung CT screening reporting & data system-recommended screening intervals in the United States: a systematic review and meta-analysis. J Thorac Oncol. 2022;17(1):38–55. doi: 10.1016/j.jtho.2021.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wender R, et al. American Cancer Society lung cancer screening guidelines. CA Cancer J Clin. 2013;63(2):107–117. doi: 10.3322/caac.21172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tammemagi MC, et al. Impact of lung cancer screening results on smoking cessation. J Natl Cancer Inst. 2014;106(6):dju084. doi: 10.1093/jnci/dju084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buttery SC, et al. Immediate smoking cessation support versus usual care in smokers attending a targeted lung health check: the QuLIT trial. BMJ Open Respir Res. 2022;9(1):e001030. doi: 10.1136/bmjresp-2021-001030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Centers for Disease, C> and Prevention Quitting smoking among adults–United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60(44):1513–1519. [PubMed] [Google Scholar]
- 42.Darville A, Hahn EJ. Hardcore smokers: what do we know? Addict Behav. 2014;39(12):1706–1712. doi: 10.1016/j.addbeh.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 43.Popova L, et al. Who are the smokers who never plan to quit and what do they think about the risks of using tobacco products? Addict Behav. 2018;87:62–68. doi: 10.1016/j.addbeh.2018.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rampinelli C, et al. Exposure to low dose computed tomography for lung cancer screening and risk of cancer: secondary analysis of trial data and risk-benefit analysis. BMJ. 2017;356:j347. doi: 10.1136/bmj.j347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vliegenthart R, et al. Innovations in thoracic imaging: CT, radiomics AI x-ray velocimetry. Respirology. 2022;27(10):818–833. doi: 10.1111/resp.14344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Milanese G, et al. Ultra-low dose computed tomography protocols using spectral shaping for lung cancer screening: comparison with low-dose for volumetric LungRADS classification. Eur J Radiol. 2023;161:110760. doi: 10.1016/j.ejrad.2023.110760. [DOI] [PubMed] [Google Scholar]
- 47.Bartlett EC, et al. false-negative results in lung cancer screening-evidence and controversies. J Thorac Oncol. 2021;16(6):912–921. doi: 10.1016/j.jtho.2021.01.1607. [DOI] [PubMed] [Google Scholar]
- 48.Miki S, et al. Prospective study of spatial distribution of missed lung nodules by readers in CT lung screening using computer-assisted detection. Acad Radiol. 2021;28(5):647–654. doi: 10.1016/j.acra.2020.03.015. [DOI] [PubMed] [Google Scholar]
- 49.Park S, et al. Application of computer-aided diagnosis for Lung-RADS categorization in CT screening for lung cancer: effect on inter-reader agreement. Eur Radiol. 2022;32(2):1054–1064. doi: 10.1007/s00330-021-08202-3. [DOI] [PubMed] [Google Scholar]
- 50.(ESTI), E.S.o.T.I., Structured report basic template