Abstract
Background
Ischemic heart disease (IHD) is the leading cause of death worldwide. High fasting plasma glucose (FPG) is an increasing risk factor for IHD. We aimed to explore the long-term trends of high FPG-attributed IHD mortality during 1990–2019.
Methods
Data were obtained from the Global Burden of Disease Study 2019 database. Deaths, disability-adjusted life-years (DALYs), the age-standardized mortality rate (ASMR) and age-standardized DALY rate (ASDR) of IHD attributable to high FPG were estimated by sex, socio-demographic index (SDI), regions and age. Estimated annual percentage changes (EAPCs) were calculated to assess the trends of ASMR and ASDR of IHD attributable to high FPG.
Results
IHD attributable to high FPG deaths increased from 1.04 million (0.62–1.63) in 1990 to 2.35 million (1.4–3.7) in 2019, and the corresponding DALYs rose from 19.82 million (12.68–29.4) to 43.3 million (27.8–64.2). In 2019, ASMR and ASDR of IHD burden attributable to high FPG were 30.45 (17.09–49.03) and 534.8 (340.7–792.2), respectively. The highest ASMR and ASDR of IHD attributable to high FPG occurred in low-middle SDI quintiles, with 39.28 (22.40–62.76) and 742.3 (461.5–1117.5), respectively, followed by low SDI quintiles and middle SDI quintiles. Males had higher ASMR and ASDR compared to females across the past 30 years. In addition, ASRs of DALYs and deaths were highest in those over 95 years old.
Conclusion
High FPG-attributed IHD mortality and DALYs have increased dramatically and globally, particularly in low, low-middle SDI quintiles and among the elderly. High FPG remains a great concern on the global burden of IHD and effective prevention and interventions are urgently needed to curb the ranking IHD burden, especially in lower SDI regions.
Keywords: Ischemic heart disease, High fasting plasma glucose, Mortality, Disability-adjusted life years
1. Introduction
Ischemic heart disease (IHD) is a major global public concern, ranking the first cause of mortality and morbidity worldwide, including acute myocardial infarction (AMI), chronic IHD (angina; asymptomatic IHD following MI) and ischemic heart failure [1,2]. In 2019, IHD was accountable for over 182 million disability-adjusted life years (DALYs) and 9.14 million deaths [3]. And coronary heart disease causes catastrophic health expenditure among countries and regions. For instance, in the United States, heart diseases are schemed to increase by 41% from $126.2 billion in 2010 to $177.5 billion in 2040 [4]. Therefore, monitoring the burden of IHD is critically important globally.
High fasting plasma glucose (FPG) has been becoming an urgent public health issue [5,6]. As reported, high FPG has ranked one of the top 5 risk factors for deaths and DALYs worldwide and high FPG exposure has increased substantially among the other risks such as hypertension. High FPG is a crucial risk factor for cardiovascular disease. In 2019 the overall deaths and DALYs attributable to high FPG were above 6.50 million and 172.07 million respectively [5]. Among all deaths, the ranking causes attributable to high FPG were diabetes mellitus (DM) and ischemic heart disease [5].
Although a growing number of studies have delivered the harm of higher glucose levels among overall disease burden. To the best of our knowledge, little literature has focused on the direct intersection between hyperglycemia and IHD, and the tendency of IHD burden attributable to high FPG. Considering the high burden of IHD and the increasing high FPG prevalence, we constructed this analysis to exhibit the high FPG-attributable burden of IHD across 204 countries and territories from 1990 to 2019 based on Global Burden of Disease (GBD) Study database 2019. Evaluation of IHD attributable to high FPG is critical and essential for policymakers and researchers to create effective strategies to reduce the prevalence of IHD attributable to high FPG.
2. Methods
2.1. Overview of the GBD study
The GBD 2019 project provides levels and trends of communicable diseases, non-communicable diseases and injuries globally. a range of data sources, such as hospital data, censuses, clinical trials, demographic surveillance, disease registries, financial records and vital registration, were utilized to estimate incidence, prevalence, mortality, years of life lived with disability (YLDs), years of life lost (YLLs) and DALYs for 369 causes of death and disability, and 87 risk factors in 204 countries and territories, 7 super-regions and 21 regions from 1990 to 2019 [7,8].
2.2. Study data
Annual deaths, DALYs, corresponding age-standardized rates (ASRs) and their 95% uncertainty intervals (UIs) across 4 world regions, 5 sociodemographic indexes of IHD attributed to high FPG between 1990 and 2019 for 204 countries and territories worldwide were obtained from GBD 2019 through the global health data exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool). We selected populations aged >30 years and by 5-year intervals (30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, 85–89, 90–94, 95+ years old) because IHD are uncommon in younger groups [9]. We obtained the age-standardized mortality rate (ASMR) and age-standardized disability-adjusted life rate (ASDR) per 100 000 population of IHD accountable to high fasting plasma glucose from the GBD 1990–2019 project. Data of cases and age-standardized rates were reported as values with 95% confidence interval (CIs) or UIs. The SDI is a geometric average of 0–1 by combining the total fertility rate of women under 25, the education level of people aged 15 and above, and the lag of per capita income distribution. The lower SDI value indicates a lower social development level and vice versa. In GBD 2019, countries and regions were divided into five SDI quintiles according to SDI value: high (>0.81), high-middle (0.70–0.81), middle (0.61–0.69), low-middle (0.46–0.60), and low (<0.46) [10]. Disability-adjusted life years are the sum of the number of years of life lost and the number of years of life lost due to disability. One DALY represents the loss of 1 year in full health. The YLLs refer to the number of deaths and the life lost due to early death, and the YLDs refer to any healthy life years lost resulting from disability. Deaths were defined as the number of deaths occurring in a population during a specific period.
We utilized ASMR and ASDR to quantify the global burden accountable to high FPG. The methods for estimating the IHD burden have been detailed by GBD 2019 Diseases and Injuries Collaborators [7]. Briefly, IHD is defined based on the World Health Organization clinical criteria and the international statistical classification of diseases, and high FPG is defined as any level above the theoretical minimum-risk exposure levels (TMREL), which is 4.8–5.4 mmol/L (88–99 mg/dl) according to the 2019 GBD study [5]. The relative risk (RR) of IHD in population exposed to high glucose levels was first estimated based on published systematic reviews and meta-regression. A Bayesian meta-regression model (DisMod-MR 2.1) and a spatiotemporal Gaussian process regression model were applied based on the large population-based survey to analyze the exposure level of risk and its TMREL. The attributable proportions of age-standardized rates of deaths and DALYs by age, sex, and year were evaluated by population-attributable fractions (PAFs), which is the estimated fraction of all cases that would not occur if there was no high FPG exposure [7,9].
2.3. Statistical analysis
The ASMR and ASDR were calculated from GBD 2019 based on the world standard population to minimize the influence of the population age structure differences. The ASR per 100 000 population is calculated as follows:
In the formula, ai stands for the age-specific rate in the i age group; wi stands for the number of people in the corresponding i age group among the standard population; A stands for the number of age groups and 100 000 means per 100 000 population.
We used estimated annual percentage changes (EAPCs) to evaluate the trends of ASMR and ASDR attributable to high FPG. EAPC is a measure of the ASR over a period. EAPC and its 95% CI were calculated by fitting a linear regression line to the natural algorithm of the ASR to quantity the tendency of ASR. The EAPC is calculated as follows:
x represents calendar year, represents error term correspondingly. If EAPC and its 95% CI lower limits are both more than 0, ASR exhibits an upward trend. If EAPC and its 95% CI upper limits are both less than 0, ASR indicated a downward trend. Moreover, no significant change was considered if the EAPC and its corresponding 95% CI included 0 [11].
The PAF for high FPG is calculated as follows:
is the relative risk as a function of exposure level, (x) for high FPG, cause (o), age group (a), and sex (s). is the distribution of exposure for high FPG according to age group (a), sex (s), location (g), and year(t). Location (g) with the lower level of observed exposure as 1 and the highest as u [7,8].
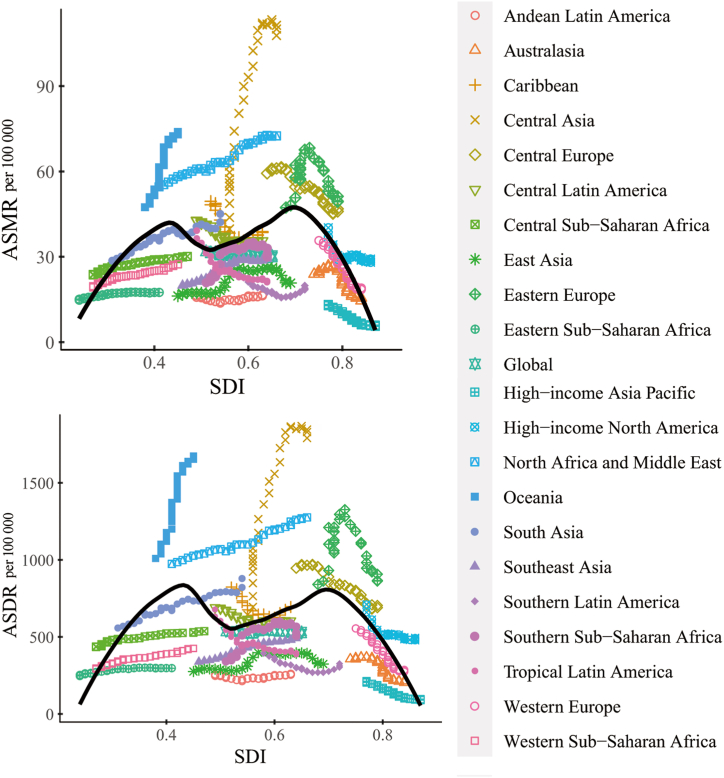
The non-parametric method of locally weighted scatterplot smoothing (LOESS) regression has been widely used in previous GBD surveys to investigate the correlation between two variables by fitting a smooth curve [12,13]. In present study, we employed LOESS regression to estimate the association between SDI levels and age-standardized rates for IHD attributable to high FPG for 21 GBD regions using GBD 2019 estimates from 1990 to 2019. The two-sided p-value less than 0.05 (p < 0.05) was considered to be significant throughout this study's statistical analysis. All statistics were conducted by the R software (Version 4.1.2, R core team, Vienna, Austria). We used ggplot2, ggrepel, reshape, dplyr, ggmap, mmaps, rgdal R packages to analyze and visualize our data in this study.
3. Results
3.1. Global burden of IHD attributable to high FPG and trends from 1990 to 2019
Globally, the overall deaths and DALYs of IHD attributable to high FPG increased from 1.04 million (0.62–1.63) in 1990 to 2.35 million (1.36–3.70) in 2019, and 19.82 million (12.68–29.36) in 1990 to 43.25 million (27.82–64.16) in 2019, respectively. The global age-standardized mortality and DALY rates of IHD attributable to high FPG changed from 32 (17.89–52.25) per 100 000 in 1990 to 30.45 (17.09–49.03) per 100 000 in 2019, and 534.8 (331.6–804.8) per 100 000 in 1990 to 534.8 (340.7–792.2) per 100 000 in 2019, respectively. Despite the increasing population, the trends of ASMR and ASDR were relatively steady with the corresponding EAPC of −0.13 (−0.58–0.31) and −0.03 (−0.6–0.54) from 1990 to 2019. However, PAF of age-standardized death and DALYs rates increased from 18.77% to 25.82%, and from 17.01% to 23.84%, respectively from 1990 to 2019 (Supplementary Table 3). More males than females suffered from IHD attributable to high FPG in 2019. There were 1.30 million deaths (0.78–2.0) and 26.39 million (16.80–39.05) DALYs for males, whereas 1.05 million (0.56–1.76) deaths and 16.86 million (10.07–25.94) DALYs for females. The ASMR and ASDR of IHD attributable to high FPG for males were 38.53 (22.30–60.1) and 703.4 (451–1043.4), and the corresponding ASRs for females were 23.9 (12.68–40) and 384.8 (230.1–590.3) (Table 1, Table 2, Supplementary Fig. 1). The global rates of deaths and DALYs were increasing along with aging and toped at the oldest age group (95+) in 2019. In terms of the absolute number of deaths and DALYs, patients aged 80–84 had the highest number of death cases of 395.42 thousand (146.78–785.56) (Fig. 1A), and patients aged 65–69 had the highest number of DALYs of 6.09 million (2.63–10.51) (Fig. 1B–Supplementary Tables 1 and 2, Supplementary Fig. 2).
Table 1.
Death cases and ASMR of IHD attributable to high FPG between 1990 and 2019.
| Death counts (Thousands, 95% UI) |
ASMR per 100 000 people (95% UI) |
EAPC (95% CI) |
|||
|---|---|---|---|---|---|
| 1990 | 2019 | 1990 | 2019 | ||
| Global | 1042.56 (618.72–1634.70) | 2353.42 (1361.23–3701.92) | 32.00 (17.89–52.25) | 30.45 (17.09–49.03) | −0.13 (−0.58 to 0.31) |
| Sex | |||||
| Male | 550.75 (339.81–822.09) | 1302.84 (777.74–2002.10) | 39.50 (22.70–62.92) | 38.53 (22.30–60.10) | −0.02 (−0.10 to 0.05) |
| Female | 491.81 (268.46–826.25) | 1050.58 (556.49–1758.03) | 26.28 (13.87–45.22) | 23.90 (12.68–40.00) | −0.26 (−0.34 to −0.18) |
| SDI region | |||||
| High SDI | 369.98 (203.68–596.86) | 434.30 (228.00–730.00) | 35.06 (19.48–56.41) | 19.95 (10.93–32.56) | −2.01 (−2.65 to −1.36) |
| High-middle SDI | 322.42 (192.33–496.40) | 595.58 (331.33–954.08) | 36.31 (20.51–58.53) | 30.27 (16.66–48.89) | −0.69 (−1.15 to −0.24) |
| Middle SDI | 197.57 (119.63–306.87) | 724.10 (413.95–1138.70) | 26.53 (14.67–44.30) | 34.80 (18.71–56.26) | 1.13 (0.78–1.48) |
| Low-middle SDI | 112.28 (70.90–174.32) | 461.13 (275.98–721.64) | 24.75 (14.20–41.10) | 39.28 (22.40–62.76) | 1.54 (1.12–1.95) |
| Low SDI | 39.56 (24.43–63.44) | 136.76 (81.26–222.67) | 22.74 (12.95–39.38) | 33.35 (18.57–55.52) | 1.24 (0.83–1.64) |
| GBD region | |||||
| Andean Latin America | 2.78 (1.50–4.52) | 8.75 (4.55–15.15) | 16.38 (8.62–27.47) | 16.59 (8.57–29.03) | 0.15 (−0.15 to 0.44) |
| Australasia | 5.30 (2.95–8.97) | 8.27 (3.96–15.14) | 23.90 (12.84–41.60) | 14.53 (7.08–25.85) | −2.29 (−2.92 to −1.65) |
| Caribbean | 11.64 (6.73–18.78) | 20.06 (11.07–31.79) | 49.51 (27.73–82.72) | 38.58 (21.28–61.34) | −1.03 (−1.39 to −0.68) |
| Central Asia | 14.93 (8.74–23.70) | 58.95 (32.38–96.01) | 36.96 (21.17–59.46) | 107.79 (54.47–184.25) | 3.99 (3.62–4.35) |
| Central Europe | 76.51 (44.04–122.07) | 105.57 (53.79–180.33) | 59.36 (32.82–96.35) | 46.85 (24.13–79.33) | −1.13 (−1.54 to −0.72) |
| Central Latin America | 28.63 (16.01–45.69) | 79.47 (44.28–129.70) | 42.81 (22.77–71.46) | 35.57 (19.48–58.45) | −0.73 (−1.09 to −0.37) |
| Central Sub-Saharan Africa | 3.78 (2.30–6.08) | 11.49 (6.60–19.34) | 23.61 (13.53–40.97) | 30.13 (16.09–52.25) | 0.91 (0.43 to −1.40) |
| East Asia | 98.39 (60.41–154.34) | 351.87 (199.79–571.78) | 16.23 (8.98–26.04) | 20.77 (11.34–34.59) | 1.57 (1.03–2.11) |
| Eastern Europe | 116.23 (72.28–174.32) | 171.37 (99.41–261.19) | 47.31 (28.64–71.21) | 49.36 (28.87–75.65) | −0.35 (−1.05 to −0.36) |
| Eastern Sub-Saharan Africa | 7.53 (4.24–12.26) | 20.68 (11.68–35.24) | 14.81 (7.61–27.27) | 17.44 (9.33–31.12) | 0.66 (−0.06 to 1.37) |
| High-income Asia Pacific | 23.28 (13.63–37.04) | 34.48 (17.02–62.61) | 13.28 (7.50–21.42) | 6.00 (3.16–10.33) | −3.23 (−4.10 to −2.35) |
| High-income North America | 148.01 (87.76–228.08) | 203.00 (112.83–327.21) | 40.21 (24.36–61.37) | 29.20 (16.6–46.25) | −0.60 (−1.32 to 0.14) |
| North Africa and Middle East | 72.91 (46.02–112.45) | 255.31 (148.83–396.26) | 54.60 (32.17–90.17) | 72.52 (39.80–117.18) | 1.05 (0.94–1.16) |
| Oceania | 1.14 (0.68–1.79) | 4.57 (2.79–6.90) | 47.43 (27.00–76.08) | 73.89 (43.02–115.15) | 1.73 (1.08–2.38) |
| South Asia | 123.76 (78.50–191.99) | 546.34 (328.42–838.30) | 28.64 (16.75–46.91) | 45.06 (26.10–69.79) | 1.37 (0.90–1.84) |
| Southeast Asia | 37.70 (22.22–60.78) | 144.73 (82.10–232.15) | 19.90 (10.78–34.29) | 29.94 (16.05–49.24) | 1.50 (1.17–1.83) |
| Southern Latin America | 9.94 (5.80–15.54) | 17.10 (8.95–29.09) | 23.92 (13.49–38.72) | 19.86 (10.47–33.68) | −0.88 (−1.43 to −0.33) |
| Southern Sub-Saharan Africa | 4.58 (2.54–7.68) | 13.62 (7.75–21.95) | 20.87 (10.68–36.47) | 29.86 (16.03–49.09) | 1.32 (0.96–1.68) |
| Tropical Latin America | 28.37 (16.37–44.79) | 48.42 (27.11–78.36) | 39.15 (20.92–64.16) | 21.04 (11.67–34.55) | −1.86 (−2.34 to −1.37) |
| Western Europe | 215.36 (110.80–370.70) | 213.19 (98.99–389.98) | 35.75 (18.49–61.07) | 19.05 (9.57–33.46) | −2.59 (−3.18–1.99) |
| Western Sub-Saharan Africa | 11.78 (6.54–21.3) | 11.78 (6.54–21.3) | 19.24 (10.08–37.08) | 19.24 (10.08–37.08) | 1.11 (0.92–1.31) |
Abbreviations: IHD, ischemic heart disease; FPG, fasting plasma glucose; ASMR, age-standardized mortality rate; UI, uncertainty interval; CI, confidence interval; EAPC, estimated annual percentage change; GBD, Global Burden of Disease; SDI, sociodemographic index.
Table 2.
DALYs and ASDR of IHD attributable to high FPG between 1990 and 2019.
| DALYs (Thousands, 95% UI) |
ASDR per 100 000 people (95% UI) |
EAPC (95% CI) |
|||
|---|---|---|---|---|---|
| 1990 | 2019 | 1990 | 2019 | 1990–2019 | |
| Global | 19820.67 (12680.03–29360.12) | 43253.27 (27821.41–64164.59) | 534.8 (331.6–804.8) | 534.8 (340.7–792.2) | −0.03 (−0.60 to 0.54) |
| Sex | |||||
| Male | 11708.66 (7667.85–17574.09) | 26388.89 (16794.53–39051.55) | 692.3 (437.2–1023.6) | 703.4 (451.0–1043.4) | 0.04 (−0.02 to 0.10) |
| Female | 8112.01 (4887.07–12451.07) | 16864.38 (10065.16–25938.25) | 400.5 (236.9–619) | 384.8 (230.1–590.3) | −0.13 (−0.20 to −0.06) |
| SDI region | |||||
| High SDI | 6062.98 (3739.26–9260.95) | 6460.62 (3872.16–9861.01) | 573.2 (355.9–862.9) | 334.8 (213.0–492.7) | −1.97 (−2.80 to −1.13) |
| High-middle SDI | 6093.08 (3924.76–8939.09) | 9947.46 (6354.42–14816.68) | 605.5 (376.6–893.6) | 493 (312.1–736.1) | −0.89 (−1.52 to −0.26) |
| Middle SDI | 4151.22 (2738.65–6247.83) | 13984.14 (8788.14–21059.25) | 449.6 (283.2–681.8) | 592.7 (370.8–905.3) | 1.09 (0.66–1.53) |
| Low-middle SDI | 2595.40 (1689.50–3863.40) | 9846.85 (6088.26–14774.82) | 460.7 (293.4–704.8) | 742.3 (461.5–1117.5) | 1.58 (1.06–2.10) |
| Low SDI | 904.37 (580.37–1349.60) | 2984.21 (1882.19–4563.03) | 416.4 (258.7–664.8) | 615.7 (373.6–957.9) | 1.24 (0.79–1.70) |
| GBD region | |||||
| Andean Latin America | 48.36 (28.90–72.78) | 141.24 (79.16–219.55) | 256.1 (150.3–390.8) | 260.5 (145.1–412.0) | 0.12 (−0.27 to 0.51) |
| Australasia | 82.69 (50.03–131.07) | 108.14 (56.38–180.83) | 356.4 (214.3–560.3) | 203.3 (109.8–334.2) | −2.59 (−3.37 to −1.79) |
| Caribbean | 207.55 (132.76–307.38) | 359.57 (222.34–543.10) | 823.7 (523.2–1238.1) | 693.8 (427.7–1048.2) | −0.75 (−1.15 to −0.35) |
| Central Asia | 284.71 (180.73–428.07) | 1158.15 (681.71–1817.75) | 643.6 (398.4–978.8) | 1790.7 (1001–2862.2) | 3.74 (3.25–4.22) |
| Central Europe | 1332.04 (830.89–2025.67) | 1556.99 (883.90–2424.73) | 946.3 (591.3–1431.6) | 703.8 (412.1–1082.8) | −1.38 (−2.01 to −0.75) |
| Central Latin America | 524.26 (330.04–794.96) | 1399.72 (872.24–2102.81) | 690.7 (417.3–1059.2) | 604.7 (372.7–909.2) | −0.59 (−1.10 to −0.08) |
| Central Sub-Saharan Africa | 88.95 (56.34–138.05) | 250.15 (150.24–407.24) | 434.5 (268.2–694.4) | 537.2 (310.7–903.6) | 0.79 (0.18–1.41) |
| East Asia | 2142.27 (1325.76–3328.17) | 6201.95 (3888.24–9606.33) | 275.3 (170.7–424.5) | 323.8 (199.0–502.0) | 1.12 (0.57–1.67) |
| Eastern Europe | 2248.47 (1507.09–3212.54) | 2950.45 (1884.76–4321.48) | 840.8 (554.0–1198.0) | 862.7 (563.5–1254.1) | −0.48 (−1.42 to 0.48) |
| Eastern Sub-Saharan Africa | 156.65 (92.43–242.46) | 415.51 (249.09–677.82) | 246.2 (138.9–398.9) | 296.4 (173.7–500.8) | 0.70 (−0.08 to 1.49) |
| High-income Asia Pacific | 408.89 (260.44–617.77) | 463.05 (259.54–768.90) | 212.6 (134.5–322.4) | 96.5 (58.3–153.5) | −3.28 (−4.38 to −2.18) |
| High-income North America | 2525.39 (1612.33–3709.97) | 3149.48 (1974.55–4590.47) | 711.3 (467.7–1036.4) | 493.8 (320.1–708.0) | −0.82 (−1.70 to −0.07) |
| North Africa and Middle East | 1545.52 (1007.02–2322.73) | 5149.50 (3151.39–7762.32) | 974 (626.7–1481.7) | 1276.1 (768.5–1950.3) | 0.95 (0.73–1.16) |
| Oceania | 30.57 (18.28–46.94) | 128.68 (74.90–197.17) | 1009.4 (609.4–1562.0) | 1674.4 (1026.4–2514.3) | 1.95 (1.14–2.77) |
| South Asia | 3043.80 (1967.16–4492.37) | 12123.75 (7474.62–17919.53) | 558.1 (355.2–846.2) | 879.3 (543.0–1301.8) | 1.41 (0.83–1.99) |
| Southeast Asia | 774.92 (497.93–1187.48) | 2773.01 (1717.24–4223.93) | 338.0 (204.6–529.7) | 501.2 (304.8–769.7) | 1.37 (0.95–1.79) |
| Southern Latin America | 175.93 (110.80–262.53) | 275.68 (156.70–434.26) | 393.4 (242.9–587.3) | 325.9 (188.0–510.5) | −0.94 (−1.70 to −0.19) |
| Southern Sub-Saharan Africa | 86.04 (55.04–131.20) | 263.00 (159.94–410.61) | 341.2 (206.5–535.0) | 507.8 (300.3–797.8) | 1.55 (1.08–2.02) |
| Tropical Latin America | 573.75 (353.11–874.39) | 925.12 (557.71–1425.97) | 678.6 (409.2–1055.4) | 387.1 (232.7–602.0) | −1.63 (−2.23 to −1.04) |
| Western Europe | 3327.88 (1921.73–5403.29) | 2809.28 (1552.81–4715.77) | 554.7 (327.4–889.0) | 285.4 (165.9–454.4) | −2.83 (−3.64 to −2.01) |
| Western Sub-Saharan Africa | 212.02 (129.30–343.47) | 650.83 (383.02–1070.35) | 291.4 (168.6–515.9) | 425.4 (237.8–708.1) | 1.26 (1.04–1.48) |
Abbreviations: IHD, ischemic heart disease; FPG, fasting plasma glucose; DALYs, disability-adjusted life years; ASDR, age-standardized DALY rate; UI, uncertainty interval; CI, confidence interval; EAPC, estimated annual percentage change; GBD, Global Burden of Disease; SDI, sociodemographic index.
Fig. 1.
Global age-specific rates of IHD attributable to high FPG per 100 000 population in 2019, by sex. (A) Deaths. (B) DALYs. IHD, ischemic heart disease; FPG, fasting plasma glucose; DALYs, disability-adjusted life years.
3.2. Geographical burden variations in IHD due to high FPG
In 2019, across 21 GBD regions, South Asia had the highest burden of IHD attributable to high FPG, with a number of death cases of 546.34 thousand (328.42–838.30) and number of DALYs cases of 12.12 million (7.47–17.92). In terms of ASRs, Central Asia exhibited the heaviest ASMR and ASDR of IHD attributable to high FPG of 107.79 (54.47–184.25) and 1790.7 (1001–2862.2) per 100 000 population, respectively. While High-income Asia Pacific presented the lowest age-standardized death and DALYs rates of 6 (3.16–10.33) and 96.5 (58.3–153.5) per 100 000, respectively (Fig. 2A and B). From 1990 to 2019, Central Asia witnessed the highest increase of both ASMR and ASDR, with an EAPC of 3.99 (3.62–4.35), and 3.74 (3.25–4.22), respectively, while High-income Asia Pacific showed the most significant drop of ASMR and ASDR of IHD attributable to high FPG, with an EAPC of −3.23 (−4.1 to −2.35) and −3.28 (−4.38 to −2.18) respectively (Table 1, Table 2, Fig. 2C and D, Supplementary Fig. 3).
Fig. 2.
Age-standardized rates of IHD attributable to high FPG per 100 000 population in 2019, by country. (A) ASMR. (B) DALYs. (C) EAPC of ASMR. (D) EAPC of ASDR. IHD, ischemic heart disease; FPG, fasting plasma glucose; EAPC, estimated annual percentage changes; ASMR, age-standardized mortality rates; ASDR, age-standardized disability-adjusted life years.
3.3. Global burden of IHD attributable to high FPG by SDI
Across all SDI quintiles, countries with low-middle SDI had the peak ASMR of 39.28 (22.40–62.76) per 100 000 in 2019, followed by countries with middle SDI and low SDI levels, while countries with high SDI quintile exhibited the lowest ASMR of 19.95 (10.93–32.56) per 100 000 population (Fig. 3A). In terms of age-standardized rates of DALYs for IHD attributable to high FPG, countries with low-middle SDI quintile had the highest ASDR of 742.3 (461.5–1117.5) per 100 000 population, followed by countries with low and middle SDI levels, while countries with high SDI quintile showed the lowest ASDR of 334.8 (213.0–492.7) per 100 000 population (Fig. 3B). From 1990 to 2019, ASMR and ASDR have increased in low, low-middle and middle SDI quintiles, with the most highly increase both observed in countries with low-middle SDI, with EAPC of 1.54 (1.12–1.95) for ASMR and 1.58 (1.06–2.1) for ASDR, respectively. However, the most significantly decline of ASMR and ASDR both occurred in countries with high SDI, with EAPC of −2.01 (−2.65 to −1.36) for ASMR and −1.97 (−2.8 to −1.13) for ASDR, respectively. In 1990, countries with high-middle SDI had highest ASMR and ASDR of IHD attributed to high FPG, with 36.31 (20.51–58.53) and 605.5 (376.6–893.6) per 100 000, respectively. In 2019, the top deaths and DALYs of IHD attributable to high FPG occurred in middle SDI quintiles and low-middle SDI quintiles, with 724.1 thousand (413.95–1138.70) deaths and 9.85 million (6.09–14.77) DALYs, respectively. (Table 1, Table 2, Supplementary Table 3, Fig. 4A and B).
Fig. 3.
Changes of age-standardized rates of IHD attributable to high FPG per 100 000 population, by SDI,1990–2019. (A) Deaths. (B) DALYs. IHD, ischemic heart disease; FPG, fasting plasma glucose; SDI, socio-demographic index; DALYs, disability-adjusted life years.
Fig. 4.
Trend in age-standardized rates of IHD attributable to high FPG for 21 GBD regions by SDI, 1990–2019. (A) Deaths. (B) DALYs. IHD, ischemic heart disease; FPG, fasting plasma glucose; SDI, socio-demographic index; DALYs, disability-adjusted life years.
4. Discussion
To the best of our knowledge, this is the first study that systematically evaluated the global burden of IHD attributed to high FPG among 204 countries and territories from 1990 to 2019. In this study, we revealed that the absolute number of deaths and DALYs have dramatically increased from 1990 to 2019. Although the ASRs of high FPG-induced IHD changed slightly in the global level, there existed significant variations in different SDI quintiles, especially in countries with lower SDI. Moreover, males had higher ASMRs and ASDRs of IHD attributable to high FPG compared to females from 1990 to 2019.
The prevalence of hyperglycemia was increased greatly worldwide, with PAF reached over 25% in 2019. High FPG has broad and far-reaching adverse effects on individuals with IHD [3,6,14,15]. Previous studies have demonstrated that patients with hyperglycemia have higher mortality rates after AMI compared to patients with normal glucose levels, and there existed a J-shaped association between IHD and high FPG [[16], [17], [18]]. Hyperglycemia disturbs a diversity of physical function through various mechanisms such as oxidative stress response, accumulated glycation end products and fatty acids, resulting in vascular inflammation, vasoconstriction and cardiac remodeling [18]. Besides, high FPG, accompanied with other metabolic risk factors, such as high low-density lipoprotein cholesterol, high systolic blood pressure and high BMI, could cause severe high IHD mortality and morbidity together [15,19]. Therefore, population with high FPG can benefit a lot from lowering glucose to a suggestive level [20]. Individuals with high glucose levels should pay attention to the increased risk of IHD, and take interventions to curb the progression of IHD in time.
Globally, we found the rates of mortality and DALYs of IHD attributable to high FPG were higher in males than in females, which was consistent with previous large-scale global research [[21], [22], [23], [24]]. It is reported that women presented with fewer ST-segment elevation myocardial infarction and better cardiac function when facing diabetic heart disease compared to males [[25], [26], [27]]. And they are less likely to develop obesity, insulin resistance and high FPG [28]. Estrogen play a preliminary role in glucose metabolism, insulin synthesis and arterial balance, resulting in these sex differences [[29], [30], [31]].
The sex differences between mortality and morbidity rates of IHD can also be explained by behavior risk factors, such as smoking, stress, obesity and lack of physical activity, which are more prevalent in males than females, resulting in poor glucose regulation and hyperglycemia [24,32]. Furthermore, females and males differed greatly in disease prevention and therapy choices. For instance, primary prevention strategies (e.g., healthy foods, physical activeness, health awareness) were more presented in women [21], and women may respond positively to some therapies such as angiotensin-converting enzyme inhibitors (ACEI), by contrast, men are more likely to receive secondary prevention treatments such as revascularisation procedures [27,33]. Therefore, Better management of hyperglycemia through lifestyle interventions, raising awareness of risk factors, and medicine usage are critical to lower rates of DALYs and deaths in high FPG induced IHD.
Our study found that the rate of deaths and DALYs of patients with IHD attributable to high FPG increased along with age, peaking in the oldest age group. Notably, aging is the strongest risk factor for cardiovascular disease as senescence is associated with a decline in a diversity of physiological processes such as immunity, DNA repairing and endocrine regulation [2,34]. It has been reported that FPG levels were progressively 0.7–1.1 mg/dl higher per decade causing high hazards of IHD attributable to high FPG in the old [35,36]. Aged individuals are more likely to suffer from comorbidities like dementia, depression and polypharmacy, and old patients have significantly longer sedentary time compared with the young [36,37]. Undoubtedly, those health risks increased the high FPG induced IHD risk [38,39]. Furthermore, most clinical trials excluded the elderly aged >75 years, which may influence recommendations for DM and IHD therapy in the old [37]. Considering the growing population and high burden of IHD attributable to high FPG in the elderly, it is urgent to involve those patients in clinical trials and provide the most appropriate therapies [40,41].
In this study, we found that high FPG-attributed IHD burden varied significantly across countries with different SDI levels. Countries with high SDI and high-middle SDI exhibited decreasing trends from 1990 to 2019, and countries with high SDI had the lowest ASRs of mortality and DALYs of IHD attributable to high FPG in 2019. High-income Asia Pacific not only had the lowest ASRs of mortality and DALYs in 2019, but also showed the most rapid declines in ASRs across the 30-year period, consistent with previous studies [42,43]. Undoubtedly, the drop in this trend has been achieved through a diversity of strategies [42]. Residents in high-income Asia-Pacific with hyperglycemia benefit a lot from good health-care management. For example, lifestyle modifications rank priority in the primary prevention of prediabetes, such as the promotion of healthy foods (e.g., fruits, vegetables), harnessing unhealthy foods (e.g., saturated fats, refined carbohydrates), and encouraging physical activity in daily life [44,45]. As for population who have high FPG levels or have multiple risk factors in developing diabetes, medicine like metformin is considered and prescribed [46]. Whereas poor diets and high BMI are more prevalent in individuals lived in lower SDI quintiles [[47], [48], [49]]. Also, Also, population in developed countries is more health-conscious, about 52.3% patients with DM have satisfying glucose control in the United States, whereas only 23% patients have advised glucose levels in low and middle income countries [10]. Good medical devices, adequate medicine, and sound surveillance systems vary greatly across different SDI quintiles [50,51]. For instance, the medicines are more commonly available and affordable in high SDI quintiles whereas least attainable in lower SDI countries such as Kyrgyzstan (Central Asia), India and Pakistan [46]. In high-income countries, metformin and insulin were available in 100% and 93.8% of pharmacies, compared to 64.7% and 10.3% of pharmacies in low-income countries. It is estimated that 26.9% of households cannot afford metformin and 63% of households cannot afford insulin [52]. These regions with lower SDI levels should improve health infrastructure and improved health awareness of residents [6]. In general, the burden of hyperglycemia has arisen globally and threatens public health severely, urgent strategies is needed to address the high mortality and DALYs rates of IHD attributable to high FPG, especially in low and middle SDI locations, where hyperglycemia and metabolic factors are increasing rapidly [15,53].
5. Limitation
Our study has several limitations. Firstly, the documentation of IHD burden attributable to high FPG depends largely on admissions to hospitals, which would be less complete for patients with financial problems particularly in less developed regions. For example, residents who live poor are unlikely to go to hospitals until they suffer heavy IHD or diabetes, and the health-care workers in those countries are kind of scarcity, thus the high FPG associated IHD burden might be underestimated and less representative. Secondly, there is no universal standard for determining the main causes of death from IHD. Even in the same region, such criteria depend on the resources of doctors and hospitals. These factors could significantly influence the mortality rates. Furthermore, IHD is often associated with a variety of complications, making it difficult to determine the underlying cause of death, especially in the elderly. The data conducted in the present study may not accurately represent the mortality of IHD attributed to high FPG. Thirdly, our study is limited to individuals aged over 30 years old, and those patients who are younger than 30 years have been excluded from the study due to the low incidence of IHD attributable to high FPG. Finally, our study is based on GBD 2019, and data collected from different regions and countries may vary significantly in quality and accuracy, as well as missing data. Even adjusting the data with several statistical methods as much as possible, the estimates will inevitably lead to some bias.
6. Conclusions
There existed great inequities and variations in the burden of IHD attributable to high FPG among global regions. Although we have made great achievements in IHD attributable to high FPG prevention and treatment, the burden is still substantial. More strategies such as greater healthcare financing and reduced risks exposure are needed to curb the ranking IHD mortality and morbidity, particularly in lower SDI quintiles.
Ethics statement
All data sources used in GBD 2019 is publicly available at the Global Health Data Exchange website (http://ghdx.healthdata.org/gbd-results-tool); therefore, this study does not require ethical approval and informed consent.
Funding
This work was supported by grants from the National Natural Science Foundation of China (No. 81670051, 81970050 grant to Prof. Manxiang Li), the Integration of Basic and Clinical Science Project of School of Basic Medical Sciences, Xi'an Jiaotong University (Grant No. YXJLRH2022034).
Data availability statement
The data sets that were analyzed in our study can be obtained from an open data source, using the Global Health Data Exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool) in the Global Burden of Disease database. Data are available on reasonable request from the corresponding author.
CRediT authorship contribution statement
Nirui Shen: Writing – original draft, Methodology, Conceptualization. Jin Liu: Writing – review & editing. Yan Wang: Formal analysis. Yuanjie Qiu: Methodology. Danyang Li: Methodology, Formal analysis. Qingting Wang: Data curation. Limin Chai: Data curation. Yuqian Chen: Data curation. Huizhong Hu: Validation. Manxiang Li: Writing – review & editing, Supervision, Funding acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank all individuals who have contributed to the Global Burden of Disease 2019 Study and its collaborators who prepared these publicly available data. Also, we would like to thank the National Natural Science Foundation of China sincerely.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e27065.
Abbreviations
- IHD
ischemic heart disease
- FPG
fasting plasma glucose
- GBD
global burden of disease
- DALYs
disability-adjusted life-years
- ASMR
age-standardized mortality rate
- ASDR
age-standardized ASDR rate
- SDI
socio-demographic index
- EAPC
estimated annual percentage changes
- AMI
acute myocardial infarction
- YLDs
year of life lived with disability
- YLLs
year of life lost
- ASR
age-standardized rate
- UIs
uncertainty intervals
- CIs
confidence intervals
- DM
diabetes mellitus
- ACE
converting enzyme
- CRT
cardiac resynchronization
- BMI
body mass index
- ICD
international classification of disease
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Safiri S., Karamzad N., Singh K., Carson-Chahhoud K., Adams C., Nejadghaderi S.A., et al. Kolahi A.A. Burden of ischemic heart disease and its attributable risk factors in 204 countries and territories, 1990–2019. Eur. J. Prev. Cardiol. 2022;29(2):420–431. doi: 10.1093/eurjpc/zwab213. [DOI] [PubMed] [Google Scholar]
- 2.Moran A.E., Tzong K.Y., Forouzanfar M.H., Rothy G.A., Mensah G.A., Ezzati M., et al. Naghavi M. Variations in ischemic heart disease burden by age, country, and income: the global burden of diseases, injuries, and risk factors 2010 study. Global Heart. 2014;9(1):91–99. doi: 10.1016/j.gheart.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fu X., Wang J., Jiang S., Wu J., Mu Z., Tang Y., et al. Zhao Y. Mortality trend analysis of ischemic heart disease in China between 2010 and 2019: a joinpoint analysis. BMC Publ. Health. 2023;23(1):644. doi: 10.1186/s12889-023-15549-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Odden M.C., Coxson P.G., Moran A., Lightwood J.M., Goldman L., Bibbins-Domingo K. The impact of the aging population on coronary heart disease in the United States. Am. J. Med. 2011;124(9):827–833.e5. doi: 10.1016/j.amjmed.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liang R., Feng X., Shi D., Yang M., Yu L., Liu W., et al. Chen W. The global burden of disease attributable to high fasting plasma glucose in 204 countries and territories, 1990-2019: an updated analysis for the Global Burden of Disease Study 2019. Diabetes Metabol. Res. Rev. 2022;38(8) doi: 10.1002/dmrr.3572. [DOI] [PubMed] [Google Scholar]
- 6.Chew N.W.S., Ng C.H., Tan D.J.H., Kong G., Lin C., Chin Y.H., et al. Muthiah M.D. The global burden of metabolic disease: data from 2000 to 2019. Cell Metabol. 2023;35(3):414–428 e3. doi: 10.1016/j.cmet.2023.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Collaborators G.R.F. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collaborators G.D.a.I. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Danaei G., Lawes C.M., Vander Hoorn S., Murray C.J., Ezzati M. Global and regional mortality from ischaemic heart disease and stroke attributable to higher-than-optimum blood glucose concentration: comparative risk assessment. Lancet. 2006;368:1651–1659. doi: 10.1016/S0140-6736(06)69700-6. [DOI] [PubMed] [Google Scholar]
- 10.Liu Y., Wang W., Huang X., Zhang X., Lin L., Qin J.J., et al. Cheng B. Global disease burden of stroke attributable to high fasting plasma glucose in 204 countries and territories from 1990 to 2019: an analysis of the Global Burden of Disease Study. J. Diabetes. 2022;14(8):495–513. doi: 10.1111/1753-0407.13299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu J., Yuan M., Chen Y., Wang Y., Wang Q., Zhang Q., et al. Li M. Global burden of asthma associated with high body mass index from 1990 to 2019. Ann. Allergy Asthma Immunol. 2022;129(6):720–730.e8. doi: 10.1016/j.anai.2022.08.013. [DOI] [PubMed] [Google Scholar]
- 12.Collaborators G.C.o.D. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Collaborators G.M. Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1684–1735. doi: 10.1016/S0140-6736(18)31891-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Collaborators G.R.F. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1345–1422. doi: 10.1016/S0140-6736(17)32366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu S., Xu W., Guan C., Lv M., Jiang S., Jinhua Z. Global burden of cardiovascular disease attributable to metabolic risk factors, 1990–2019: an analysis of observational data from a 2019 Global Burden of Disease study. BMJ Open. 2023;13(5) doi: 10.1136/bmjopen-2022-069397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee J.H., Han K., Huh J.H. The sweet spot: fasting glucose, cardiovascular disease, and mortality in older adults with diabetes: a nationwide population-based study. Cardiovasc. Diabetol. 2020;19(1):44. doi: 10.1186/s12933-020-01021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Selvin Elizabeth, Lazo Mariana, Chen Yuan, Shen Lu, Rubin Jonathan, McEvoy John W., et al. Coresh J. Diabetes, pre-diabetes and incidence of subclinical myocardial damage. Circulation. 2014;130(16):1374–1382. doi: 10.1161/CIRCULATIONAHA.114.010815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ding X.S., Wu S.S., Chen H., Zhao X.Q., Li H.W. High admission glucose levels predict worse short-term clinical outcome in non-diabetic patients with acute myocardial infraction: a retrospective observational study. BMC Cardiovasc. Disord. 2019;19(1):163. doi: 10.1186/s12872-019-1140-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kang S.Y., Kim Y.S. Relationships between fasting glucose levels, lifestyle factors, and metabolic parameters in Korean adults without diagnosis of diabetes mellitus. J. Diabetes. 2022;14(1):52–63. doi: 10.1111/1753-0407.13238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharif K., Ghadir S., Jakubowicz D., Amital H., Bragazzi N.L., Watad A., et al. Bar-Dayan Y. Improved outcome of patients with diabetes mellitus with good glycemic control in the cardiac intensive care unit: a retrospective study. Cardiovasc. Diabetol. 2019;18(1):4. doi: 10.1186/s12933-019-0810-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xie X.X., Zhou W.M., Lin F., Li X.Q., Zhong W.L., Lin S.G., et al. Lin X. Ischemic heart disease deaths, disability-adjusted life years and risk factors in Fujian, China during 1990–2013: data from the Global Burden ofDisease Study 2013. Int. J. Cardiol. 2016;214:265–269. doi: 10.1016/j.ijcard.2016.03.236. [DOI] [PubMed] [Google Scholar]
- 22.Dai H., Much A.A., Maor E., Asher E., Younis A., Xu Y., et al. Bragazzi N.L. Global, regional, and national burden of ischaemic heart disease and its attributable risk factors, 1990-2017: results from the Global Burden of Disease Study 2017. Eur. Heart J. Qual. Care Clin. Outcomes. 2022;8(1):50–60. doi: 10.1093/ehjqcco/qcaa076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmadizar F., Wang K., Aribas E., Fani L., Heshmatollah A., Ikram M.K., Kavousi M. Impaired fasting glucose, type 2 diabetes mellitus, and lifetime risk of cardiovascular disease among women and men: the Rotterdam Study. BMJ Open Diabetes Res. Care. 2021;9(1) doi: 10.1136/bmjdrc-2021-002406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perrino C., Ferdinandy P., Botker H.E., Brundel B., Collins P., Davidson S.M., et al. Ytrehus K. Improving translational research in sex-specific effects of comorbidities and risk factors in ischaemic heart disease and cardioprotection: position paper and recommendations of the ESC Working Group on Cellular Biology of the Heart. Cardiovasc. Res. 2021;117(2):367–385. doi: 10.1093/cvr/cvaa155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Athithan L., Chowdhary A., Swarbrick D., Gulsin G.S., Singh A., Jex N., et al. McCann G.P. Male sex adversely affects the phenotypic expression of diabetic heart disease. Ther. Adv. Endocrinol. Metabol. 2020;11:1–11. doi: 10.1177/2042018820927179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thrainsdottir I.S., Aspelund T., Gudnason V., Malmberg K., Sigurdsson G., Thorgeirsson G., et al. Ryden L. Increasing glucose levels and BMI predict future heart failure experience from the Reykjavik Study. Eur. J. Heart Failure. 2007;9(10):1051–1057. doi: 10.1016/j.ejheart.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 27.Dunlay S.M., Roger V.L. Gender differences in the pathophysiology, clinical presentation, and outcomes of ischemic heart failure. Curr. Heart Fail. Rep. 2012;9(4):267–276. doi: 10.1007/s11897-012-0107-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vaccarino V., Badimon L., Corti R., de Wit C., Dorobantu M., Manfrini O., et al. Bugiardini R. Presentation, management, and outcomes of ischaemic heart disease in women. Nat. Rev. Cardiol. 2013;10(9):508–518. doi: 10.1038/nrcardio.2013.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu W., Tang Q., Jin J., Zhu T., Dai Y., Shi Y. Sex differences in cardiovascular risk factors for myocardial infarction. Herz. 2021;46(Suppl 1):115–122. doi: 10.1007/s00059-020-04911-5. [DOI] [PubMed] [Google Scholar]
- 30.Tramunt B., Smati S., Grandgeorge N., Lenfant F., Arnal J.F., Montagner A., Gourdy P. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia. 2020;63(3):453–461. doi: 10.1007/s00125-019-05040-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.A M. Sex differences for fasting levels of glucose and insulin: expanding our understanding. Nat. Rev. Endocrinol. 2021;17(3):131. doi: 10.1038/s41574-021-00472-7. [DOI] [PubMed] [Google Scholar]
- 32.Mansur A.P., Favarato D., Strunz C.M.C., Avakian S.D., Pereira-Barretto A.C., Bocchi E.A., Cesar L.A.M. Sex differences in cardiovascular disease mortality in Brazil between 1996 and 2019. Int. J. Environ. Res. Publ. Health. 2022;19(19) doi: 10.3390/ijerph191912827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fogg A.J., Welsh J., Banks E., Abhayaratna W., Korda R.J. Variation in cardiovascular disease care: an Australian cohort study on sex differences in receipt of coronary procedures. BMJ Open. 2019;9(7) doi: 10.1136/bmjopen-2018-026507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen L., Yin X., Zhao Y., Chen H., Tan T., Yao P., Tang Y. Biological ageing and the risks of all-cause and cause-specific mortality among people with diabetes: a prospective cohort study. J. Epidemiol. Community Health. 2022;76(9):771–778. doi: 10.1136/jech-2022-219142. [DOI] [PubMed] [Google Scholar]
- 35.Chia C.W., Egan J.M., Ferrucci L. Age-related changes in glucose metabolism, hyperglycemia, and cardiovascular risk. Circ. Res. 2018;123(7):886–904. doi: 10.1161/CIRCRESAHA.118.312806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jha R.P., Shri N., Patel P., Dhamnetiya D., Bhattacharyya K., Singh M. Trends in the diabetes incidence and mortality in India from 1990 to 2019: a joinpoint and age-period-cohort analysis. J. Diabetes Metab. Disord. 2021;20(2):1725–1740. doi: 10.1007/s40200-021-00834-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Forbes A., Murrells T., Sinclair A.J. Examining factors associated with excess mortality in older people (age ≥ 70 years) with diabetes - a 10-year cohort study of older people with and without diabetes. Diabet. Med. 2017;34(3):387–395. doi: 10.1111/dme.13132. [DOI] [PubMed] [Google Scholar]
- 38.Fritschi C., Park H., Richardson A., Park C., Collins E.G., Mermelstein R., et al. Quinn L. Association between daily time spent in sedentary behavior and duration of hyperglycemia in type 2 diabetes. Biol. Res. Nurs. 2016;18(2):160–166. doi: 10.1177/1099800415600065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ballin M., Nordstrom P., Niklasson J., Nordstrom A. Associations of objectively measured physical activity and sedentary time with the risk of stroke, myocardial infarction or all-cause mortality in 70-year-old men and women: a prospective cohort study. Sports Med. 2021;51(2):339–349. doi: 10.1007/s40279-020-01356-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Forbes A. Reducing the burden of mortality in older people with diabetes: a review of current research. Front. Endocrinol. 2020;11:133. doi: 10.3389/fendo.2020.00133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bourgeois F.T., Orenstein L., Ballakur S., Mandl K.D., Ioannidis J.P.A. Exclusion of elderly people from randomized clinical trials of drugs for ischemic heart disease. J. Am. Geriatr. Soc. 2017;65(11):2354–2361. doi: 10.1111/jgs.14833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang F., Mubarik S., Zhang Y., Shi W., Yu C. Risk assessment of dietary factors in global pattern of ischemic heart disease mortality and disability-adjusted life years over 30 years. Front. Nutr. 2023;10 doi: 10.3389/fnut.2023.1151445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nowbar A.N., Gitto M., Howard J.P., Francis D.P., Al-Lamee R. Mortality from ischemic heart disease. Circ. Cardiovasc. Qual. Outcomes. 2019;12(6) doi: 10.1161/CIRCOUTCOMES.118.005375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gupta R., Yusuf S. Challenges in management and prevention of ischemic heart disease in low socioeconomic status people in LLMICs. BMC Med. 2019;17(1):209. doi: 10.1186/s12916-019-1454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Touloumi G., Karakosta A., Kalpourtzi N., Gavana M., Vantarakis A., Kantzanou M., et al. group E.s High prevalence of cardiovascular risk factors in adults living in Greece: the EMENO National Health Examination Survey. BMC Publ. Health. 2020;20(1):1665. doi: 10.1186/s12889-020-09757-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mirasol R., Thai A.C., Salahuddin A.A., Tan K., Deerochanawong C., Mohamed M., et al. Uddin F. A consensus of key opinion leaders on the management of pre-diabetes in the Asia-Pacific region. J. ASEAN Fed. Endocr. Soc. 2017;32(1):6–12. doi: 10.15605/jafes.032.01.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mullachery P.H., Vela E., Cleries M., Comin-Colet J., Nasir K., Diez Roux A.V., Cainzos-Achirica M., Mauri J., Bilal U. Inequalities by income in the prevalence of cardiovascular disease and its risk factors in the adult population of catalonia. J. Am. Heart Assoc. 2022;11(17) doi: 10.1161/JAHA.122.026587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nawsherwan, Mubarik S., Bin W., Le Z., Sang M., Lin Y., et al. Wang Y. Epidemiological Trends in cardiovascular disease mortality Attributable to modifiable risk Factors and its Association with sociodemographic Transitions across BRICS-plus countries. Nutrients. 2023;15(17):3757. doi: 10.3390/nu15173757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Amini M., Zayeri F., Salehi M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-toincidence ratio: results from global burden of disease study 2017. BMC Publ. Health. 2021;21(1):401. doi: 10.1186/s12889-021-10429-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Polupanov A.G., Khalmatov A., Altymysheva A., Lunegova O.S., Mirrakhimov A.E., Sabirov I.S., et al. Mirrakhimov E. The prevalence of major cardiovascular risk factors in a rural population of the Chui region of Kyrgyzstan: the results of an epidemiological study. Anatol. J. Cardiol. 2020;24(3):183–191. doi: 10.14744/AnatolJCardiol.2020.59133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Supiyev A., Kossumov A., Kassenova A., Nurgozhin T., Zhumadilov Z., Peasey A., Bobak M. Diabetes prevalence, awareness and treatment and their correlates in older persons in urban and rural population in the Astana region, Kazakhstan. Diabetes Res. Clin. Pract. 2016;112:6–12. doi: 10.1016/j.diabres.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 52.Chow C.K., Ramasundarahettige C., Hu W., AlHabib K.F., Avezum A., Jr., Cheng X., et al. Investigators P., Availability and affordability of essential medicines for diabetes across high-income, middle-income, and low-income countries: a prospective epidemiological study. Lancet Diabetes Endocrinol. 2018;6(10):798–808. doi: 10.1016/S2213-8587(18)30233-X. [DOI] [PubMed] [Google Scholar]
- 53.Ali M.K., Pearson-Stuttard J., Selvin E., Gregg E.W. Interpreting global trends in type 2 diabetes complications and mortality. Diabetologia. 2022;65(1):3–13. doi: 10.1007/s00125-021-05585-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data sets that were analyzed in our study can be obtained from an open data source, using the Global Health Data Exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool) in the Global Burden of Disease database. Data are available on reasonable request from the corresponding author.