Abstract
Introduction and importance
Intussusception, a condition primarily seen in pediatric populations, involves the telescoping of one segment of the bowel into an adjacent section. In adults, intussusception is rare and presents unique diagnostic and management challenges. This case report highlights a 73-year-old female with ileocecal colonic intussusception complicated by an underlying adenocarcinoma, emphasizing the need for early diagnosis and a multidisciplinary approach.
Case presentation
A 73-year-old female with a history of hypertension and type 2 diabetes presented with right-sided abdominal pain, nausea, and vomiting. Physical examination revealed tenderness in the right upper quadrant, and no palpable mass or rectal bleeding. Lab results, including tumour markers, were normal. Multi-detector computed tomography (MDCT) identified ileocecal colonic intussusception with the “target sign” and low colonic wall enhancement. An emergency laparoscopic right colectomy was performed due to compromised blood supply. Postoperatively, an anastomotic leak was managed with antibiotics, bowel rest, and wound care. Pathological examination revealed cecal adenocarcinoma with one positive lymph node, staged as T3N1aM0, necessitating adjuvant chemotherapy.
Clinical discussion
Adult intussusception, a rare condition, often has an identifiable organic cause, with clinical symptoms ranging from acute to chronic or asymptomatic. Diagnostic imaging, such as MDCT, plays a crucial role in diagnosis and evaluation. Surgical management varies based on the nature and location of the lead point. In this case, the chronic symptoms, lymph node as the lead point, and low colonic wall enhancement warranted an urgent laparoscopic right colectomy with complete mesocolic excision.
Conclusion
This case underscores the complexity of adult ileocecal colonic intussusception, especially when associated with adenocarcinoma. Timely diagnosis, multidisciplinary collaboration, and meticulous surgical intervention are essential. Effective management of postoperative complications, like the anastomotic leak, is crucial.
Keywords: Ileocecal colonic intussusception, Adenocarcinoma, Surgery, Laparoscopy, Case report
Highlights
-
•
The case is particularly notable due to the presence of an underlying well-differentiated adenocarcinoma in the cecal region, adding complexity to the clinical presentation.
-
•
The surgical decision-making process is explored, detailing the choice of an emergency laparoscopic right colectomy with complete mesocolic excision based on factors such as the patient's age, chronic symptoms, and the nature of the lead point (cecal adenocarcinoma).
-
•
The case underscores the complexity of adult ileocecal colonic intussusception, emphasizing the need for timely diagnosis, multidisciplinary collaboration, and comprehensive surgical intervention, with implications for the importance of adherence to clinical guidelines for standardized reporting.
1. Introduction
Intussusception is a relatively uncommon gastrointestinal condition, often associated with pediatric populations, which involves the telescoping of one segment of the bowel into an adjacent section. However, in the adult population, intussusception is a rare and typically alarming clinical entity, warranting immediate attention and management [1]. Traditionally, intussusception predominantly affects pediatric patients aged 0 to 6 years, with 90 % of cases attributed to primary idiopathic causes. It can occur in adults. Unlike pediatric cases, over 90 % of adult intussusception cases have identifiable underlying reasons [2]. We aim to shed light on the intricate diagnostic challenges, surgical decision-making, and postoperative management encountered in this unique case conforming to the SCARE guidelines 2023 [3].
2. Case presentation
A 73-year-old female patient presented to the emergency department with right-sided abdominal pain, accompanied by nausea and vomiting. The patient has a medical history significant for hypertension and type 2 diabetes. She reported experiencing intermittent abdominal pain for three weeks before admission with no any bowel abnormality in the past prior to this episode. There was no palpable mass or rectal bleeding upon examination. Physical evaluation revealed tenderness in the right upper quadrant of the abdomen. Tumour markers, the ACE, were negative. A multi-detector computed tomography (MDCT) scan identified an ileocecal colonic intussusception displaying the characteristic “target sign” and a decreased enhancement of the colonic wall (Fig. 1). Additionally, a necrotic lymph node was observed in the ileocecal region. Due to the compromised blood supply to the colonic wall, an emergency laparoscopic approach was chosen. Intraoperative findings confirmed an irreducible ileocecal colonic intussusception with an ischemia of the intussuscepted bowel portion (Fig. 2). A right colectomy with complete mesocolic excision and side-to-side isoperistaltic extracorporeal ileo-transverse colon anastomosis was performed through a 10 cm midline incision (Fig. 3). After specimen resection, palpable induration was noted in the cecal region. The postoperative course was complicated by an anastomotic leak at the midline incision site, which was managed with antibiotics, bowel rest, total parenteral nutrition, and daily wound care. The fistula resolved after 20 days' post-surgery. Pathological examination revealed a well-differentiated adenocarcinoma of the cecum with one positive lymph node out of the 36 collected, leading to a tumour staging of T3N1aM0. Subsequently, adjuvant chemotherapy was recommended for the patient, following the XELOX protocol (Oxaliplatin and capecitabine) for four cycles. After one year of follow up, there was no recurrence.
Fig. 1.

A coronal CT-scan view of the ileo-colonic intussusception (red arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 2.

Laparoscopic intraoperative view of the ileo-colonic intussusception (red arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 3.
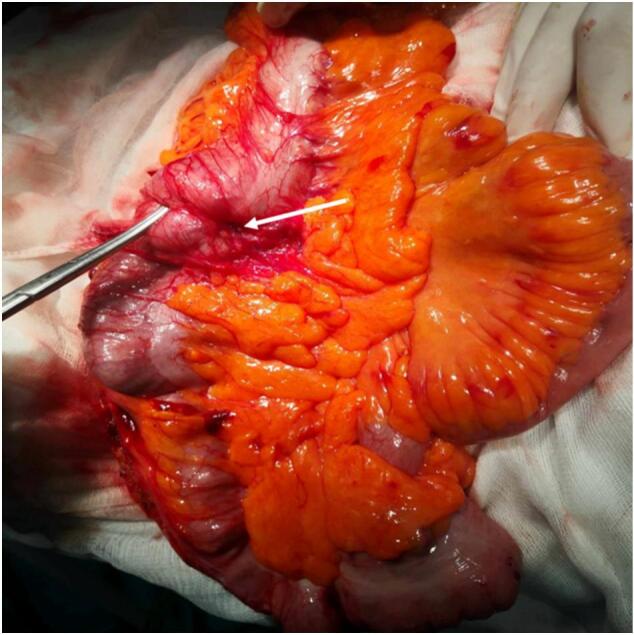
Intraoperative view showing the operative specimen and the ileo-colonic intussusception (white arrow).
3. Discussion
Intussusception occurs when one part of the intestinal tract folds into an adjacent section, potentially leading to bowel obstruction, ischemia, and perforation. Historically, intussusception was first described by Barbette of Amsterdam in 1674, with Sir Johnathan Hutchinson performing the initial surgical intervention in 1871 [4]. Clinical manifestations of intussusception vary widely, ranging from acute symptoms, often characterized by intermittent abdominal pain, “red currant jelly” stool, and a palpable abdominal mass, to chronic and even asymptomatic cases [5]. Traditionally, intussusception predominantly affects pediatric patients aged 0 to 6 years, with 90 % of cases attributed to primary idiopathic causes. Nevertheless, intussusception can also occur in adults, albeit less frequently. Unlike pediatric cases, over 90 % of adult intussusception cases have identifiable underlying reasons, referred to as “lead points,” which may be discovered before or during surgery [2,6]. Lead points can have diverse etiologies, classified into three groups: malignant, benign, and idiopathic. Additionally, postoperative adhesions and the presence of an intestinal tube have been reported as potential causes of intussusception [7]. Depending on the location of the lead point, adult intussusception can be categorized into four types: small intestine, ileocecal, ileocolic, and colocolic. In our case a malignant colon lesion was the etiology in an elderly patient which make the clinical presentation original with a particular ileo-caecal location. Identifying the nature of the lead point, particularly its malignancy, is crucial in adult cases. Kil Hwan Kim et al. explored preoperative factors for malignant lead points, finding that chronic symptomatology and the location within the colon are indicative of malignancy. Clinical diagnosis can be challenging due to the varied and nonspecific physical signs [8]. Therefore, diagnostic imaging plays a crucial role, with abdominal ultrasonography and multi-detector computed tomography (MD-CT) being pivotal. Abdominal ultrasonography may reveal characteristic findings such as the “target sign” or “doughnut sign” in cross-sectional images and the “pseudo kidney sign” in longitudinal sections. MD-CT is the preferred method for detecting and assessing adult bowel intussusception, offering an accuracy rate of 58–100 % [9]. It enables visualization of the intussusception site, the affected digestive segment, the presence of lead points, and potential complications such as intestinal wall ischemia and perforation—frequent reasons for emergent surgery [10]. In contrast to pediatric cases, where treatment often involves air contrast enema, adult intussusception cases almost invariably require surgical intervention. The choice of surgical approach depends on the lead point's location and nature. In our presented case, several factors prompted an urgent laparoscopic right colectomy with complete mesocolic excision [11,12]: the patient's age, the chronicity of her symptoms, the identification of a lymph node as the lead point, and the observed decreased blood flow in the intestinal wall. Generally, in case of an acute abdomen a laparotomy is chosen. However, in our case due to the absence a bowel dilation the laparoscopic approach was considered feasible.
4. Conclusions
In conclusion, this case underscores the complexity of adult ileocecal colonic intussusception, especially when associated with an underlying adenocarcinoma. Treat undiagnosed intussusception in elderly as a malignancy and follow the oncosurgical principles of resection is challenging. We should keep in mind the colon adenocarcinoma as a differential diagnosis in case of intessuction in adults. Postoperative complications, including an anastomotic leak, were effectively managed. In case of controlled fistula, without systemic signs, may be managed conservatively. The successful outcome reinforces the importance of early intervention and comprehensive care in such rare clinical scenarios.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Patient consent
Written informed consent was obtained from the patient to publish this case report and accompanying images. On request, a copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethical approval
Ethical approval is exempt/waived at our institution.
Funding
None.
Author contribution
All the authors participated in the manuscript and validated the final version of the manuscript.
Guarantor
Mohamed Ali Chaouch, MD
Research registration number
Not applicable.
Conflict of interest statement
No conflict of interest to disclose.
Acknowledgements
There were no acknowledgements to mention.
References
- 1.Lindor R.A., Bellolio M.F., Sadosty A.T., Earnest F., IV, Cabrera D. Adult intussusception: presentation, management, and outcomes of 148 patients. J. Emerg. Med. 2012;43(1):1–6. doi: 10.1016/j.jemermed.2011.05.098. [DOI] [PubMed] [Google Scholar]
- 2.Cochran A.A., Higgins G.L., III, Strout T.D. Intussusception in traditional pediatric, nontraditional pediatric, and adult patients. Am. J. Emerg. Med. 2011;29(5):523–527. doi: 10.1016/j.ajem.2009.11.023. [DOI] [PubMed] [Google Scholar]
- 3.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. International Journal of Surgery (London, England). 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yalamarthi S., Smith R.C. Adult intussusception: case reports and review of literature. Postgrad. Med. J. 2005;81(953):174–177. doi: 10.1136/pgmj.2004.022749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marinis A., Yiallourou A., Samanides L., Dafnios N., Anastasopoulos G., Vassiliou I., et al. Intussusception of the bowel in adults: a review. World J Gastroenterol: WJG. 2009;15(4):407. doi: 10.3748/wjg.15.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jabra S.B., Chaouch M.A., Moussa A., Jallali M., Toumi O., Noomen F. Incomplete common mesentery with Ladd’s band and Meckel’s diverticulum: a rare cause of small bowel obstruction. Int. J. Surg. Case Rep. 2023;108159 doi: 10.1016/j.ijscr.2023.108159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta R.K., Agrawal C.S., Yadav R., Bajracharya A., Sah P.L. Intussusception in adults: institutional review. Int. J. Surg. 2011;9(1):91–95. doi: 10.1016/j.ijsu.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Kim K.H., Namgung H., Park D.G. Adult intussusceptions: preoperative predictive factors for malignant lead point. Annals of Surgical Treatment and Research. 2014;86(5):244–248. doi: 10.4174/astr.2014.86.5.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Valentini Viola, Loretta Buquicchio Grazia, Galluzzo Michele, Ianniello Stefania, Di Grezia Graziella, Ambrosio Rosa, Trinci Margherita, Miele Vittorio. Intussusception in Adults: The Role of MDCT in the Identification of the Site and Cause of Obstruction. Gastroenterology Research and Practice. 2016;2016 doi: 10.1155/2016/5623718. Article ID 5623718, 10 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lief K., Janakan G., Clark C., Coffey D. Diagnostic challenge of the non-specific presentation of adult intussusception. BMJ Case Reports CP. 2019;12(11) doi: 10.1136/bcr-2019-229931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaouch M.A., Dougaz M.W., Bouasker I., Jerraya H., Ghariani W., Khalfallah M., et al. Laparoscopic versus open complete mesocolon excision in right colon cancer: a systematic review and meta-analysis. World J. Surg. 2019;43(12):3179–3190. doi: 10.1007/s00268-019-05134-4. [DOI] [PubMed] [Google Scholar]
- 12.Oweira H., Reissfelder C., Elhadedy H., Rahbari N., Mehrabi A., Fattal W., et al. Robotic colectomy with CME versus laparoscopic colon resection with or without CME for colon cancer: a systematic review and meta-analysis. annals. févr. 2023;105(2):113–125. doi: 10.1308/rcsann.2022.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]


