Abstract
Introduction and importance
Cystic echinococcosis (CE) is a chronic illness caused by the tapeworm Echinococcus granulosus. It is classified as a neglected disease and is a priority according to the World Health Organization. CE is prevalent in populations engaged in specific livestock practices and is associated with poor living conditions.
Case presentation
41-year-old female Maasai patient who presented with symptoms of cough, dyspnea, fever, and weight loss. Physical examination and CT scans confirmed the presence of cystic masses in the lungs and liver. The patient underwent a thoracotomy procedure to address complications from a hepato-pleural fistula.
Clinical discussion
Echinococcus is a tropical disease that affects over a million people worldwide annually. It primarily affects communities engaged in animal husbandry and causes the development of hydatid cysts. Diagnosis can be challenging due to prolonged asymptomatic periods. In rare cases, cysts can rupture into the pleura and bronchial tree, causing respiratory symptoms. Surgical treatment involves the systematic evacuation of cysts and visceral cyst excision, with concurrent laparotomy and thoracotomy being the optimum approach.
Conclusion
Hydatid cysts remain a significant health problem, particularly when large pleural cysts occur with subphrenic liver cysts. Surgical intervention, specifically a single-stage thoracotomy, is the preferred first-line treatment. This approach allows for both cysts to be addressed in a single procedure, providing effective and efficient treatment to patients.
Keywords: Pulmonary hydatidosis, Hepatopleural fistula, Thoracotomy, Diagnosis and management, Poor setting resources, Case report
Highlights
-
•
Cystic echinococcosis (CE) is a neglected disease caused by Echinococcus granulosus, affecting populations engaged in livestock practices and associated with poor living conditions.
-
•
A 41-year-old Maasai female patient presented with respiratory symptoms and was diagnosed with CE based on physical examination and CT scans revealing cystic masses in the lungs and liver.
-
•
The patient underwent a thoracotomy procedure to address complications arising from a hepato-pleural fistula, a rare but serious complication of CE.
-
•
Echinococcus is a tropical disease affecting millions globally, with diagnosis often challenging due to prolonged asymptomatic periods. In this case, the patient's symptoms and diagnostic imaging allowed for prompt identification.
-
•
Surgical treatment, specifically a single-stage thoracotomy, proved to be an effective approach for simultaneous removal of cystic masses in both the lung and liver, providing efficient and comprehensive treatment for the patient's condition.
1. Introduction
Cystic echinococcosis (CE) is a chronic illness caused by the larval form of the tapeworm Echinococcus granulosus that is transmitted through contact with infected animal [1]. This disease is classified as neglected and designated as a priority by the World Health Organization for tropical illnesses [2]. CE is prevalent in populations that engage in semi-nomadic and extensive livestock keeping practices in various areas of the world, such as Asia, Africa, South America, Australia, and Europe [3]. The disease is commonly associated with poor living conditions. Transmission of hydatid disease is influenced by several factors related to the host and the environment. Activities such as dog farming and breeding, home slaughtering, and releasing stray dogs into slaughterhouse areas can lead to the spread of the disease, and one get infected by means of contact with infected dogs or consuming contaminated vegetables [4]. Infected individuals may harbor the disease for prolonged periods without experiencing symptoms until the cysts grow to a stage where they produce clinical signs, which can result in severe and even fatal complications [5].Complications associated with CE include the compression of adjacent organs and structures, cyst rupture into hollow structures (e.g., bronchi, biliary ducts) or body cavities (e.g., peritoneal or pleural cavity), subsequent spread, allergic reactions, and bacterial infections. Managing human CE is a complex challenge, where active cysts require extended treatment with anti-parasitic drugs or invasive procedures like surgery [6]. Moreover, patients require prolonged follow-up to detect any recurrence or reactivation. One of the complications associated with CE is hepato-pleural fistula, which is primarily treated through surgery. Typically, both thoracic and abdominal approaches are necessary, leading to increased morbidity and mortality.
This case is reported in line with the SCARE criteria [7].
2. Case presentation
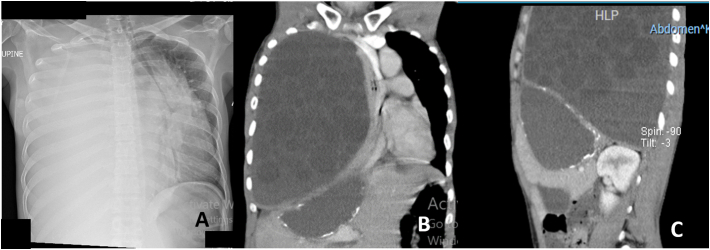
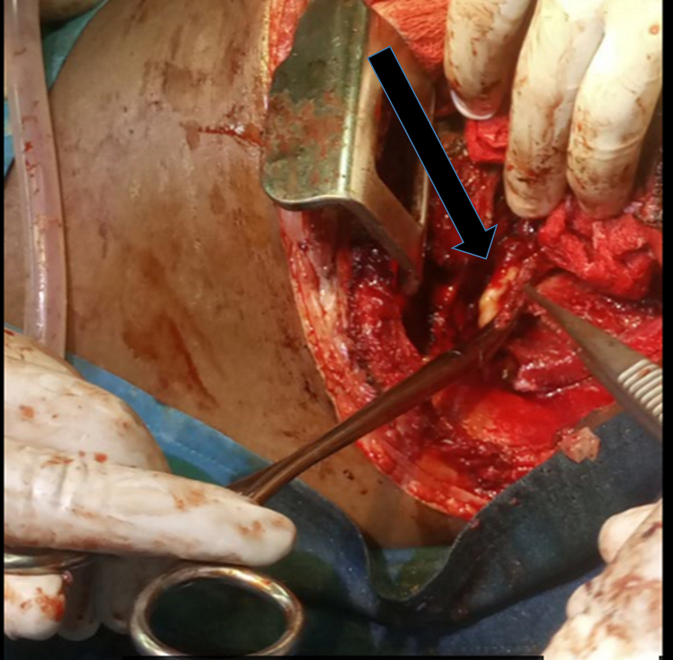
A 41-year-old female, a Maasai patient was referred to our Centre with a complaint of productive cough for 1 year of yellow watery sputum, accompanied by dyspnea on lying flat, intermittent history of fever and significant loss of weight. The patient was able to breathe effectively and comfortably but had severe cough if tried to lie down. On examination she was mildly pale, no jaundice, not dyspnea, underweight with no lower limb edema. She did not have peripheral lymphadenopathy. It was noted that the respiratory rate was 30breaths per minutes, pulse was 80 beats per minute, the pressure was 110/70 mmHg, the axillary temperature was 37.5 °C, and the oxygen saturation was 98 % in room air. Pulmonary examination found diminished breath sounds on the right side. The abdomen was found soft with no organomegaly and normal bowel sounds heard on auscultation. Her laboratory investigations revealed normal white cell counts with its differentials, haemoglobin of 14 g/dl and normal renal and liver functions. A CT-scan of the chest-abdomen revealed the presence of a right-side pleural effusion with multiple daughter cysts within a large cyst are seen in the left pleura causing complete collapse of right lung and complete left sided mediastinal shift. CT-scan also revealed a round well-defined cystic masses in the liver parenchyma just at the bed of the diaphragm on the right side but no obvious clear communication with the pleural collection (Fig. 1).The patient underwent a right posterolateral thoracotomy at sixth intercostal space, revealing turbid pleural fluids and multiple daughter cysts (Fig. 2) and, the lung that was firmly attached to the chest wall and the diaphragm, with extensive adhesions from the cyst wall and parietal pleura restricting movements. Adhesions between the lung, chest wall, and diaphragm were addressed, and communication between a hepatic cyst and the thorax was identified (Fig. 3). Complete lung decortication was performed, along with marsupialization of the hepatic cyst. Thorough lavage with 70 % ethanol was done, two drainages were placed, one on the pleura, and another on the marsupialized hepatic cyst. And the chest was closed in layers. The patient was monitored in the intensive care unit for 4 days. On the second postoperative day, the general condition was stable, with no respiratory difficulties, and the vital signs were stable and the drains were patent draining serous fluid (Fig. 4). She was discharged on day 12 on oral Albendazole. Her 4-week visit at the clinic was uneventful with no clinical features of recurrence and chest symptoms.
Fig. 1.
Preoperative imaging (A) plain chest x-ray pre-operative showing a pleural effusion with a deviated trachea, (B) chest and abdomen CT scan showing multiple daughter cysts on coronal view, (C) chest and abdominal CT scan on sagittal view showing multiple daughter cysts.
Fig. 2.
Intra operative image of multiple daughter cysts after thoracotomy (black arrow).
Fig. 3.
Intra operative image showing the fistula between the liver and the pleural cavity (black arrow).
Fig. 4.
Post-operative image of control plain chest x-ray.
3. Discussion
Echinococcus is a tropical disease that is often overlooked, but is recognized as a major public health issue by the World Health Organization. It affects over a million people worldwide annually and is primarily associated with communities engaged in animal husbandry [2]. This disease results in the development of hydatid cysts, which are commonly found in the lungs and liver, but may also affect other organs [4]. While symptom manifestation is dependent on the size and location of the cyst, many infected individuals remain asymptomatic for long periods of time, making early diagnosis a challenge [8]. Studies have shown that childhood infections can lead to extended asymptomatic periods with incidental diagnosis via chest radiographs in adult patients [9].The prominent symptom of hydatid cysts with a pneumo-biliary fistula is bilioptysis especially if bronchial tree is involved, but patients may also experience general respiratory symptoms for an extended period of time like our patient [6]. One of the major complications of the hydatid cyst of the liver is its rupture into the pleura and bronchial tree. This happens either due to the pressure from the expanding hydatid cyst leading to erosion into the diaphragm or from the destructive effect of a superimposed infection [10].
The principles of surgical treatment for managing thoracic and abdominal hydatid cysts involve the systematic evacuation of cysts along with visceral cyst excision to prevent contamination, and effective management of the resulting residual cavity [11]. The surgical approach employed for this purpose may vary based on the surgeon's preference and the clinical presentation of the patient Despite the optimum approach for addressing concurrent hydatid cysts in the liver and lung being through concurrent laparotomy and thoracotomy and most recently employment of laparoscopic surgeries through thoracoscopy, the option of using a thoracotomy approach was deemed feasible in our case because of lack of experties and equipment's for laparascopic surgery . This is primarily due to the fact that when a hydatid cyst in the liver erodes from the dome of the liver through the diaphragm, and subsequently reaches the lung through the pleura, it forms a fibrotic tract that has no communication with the surrounding structures. This unique condition allows surgeons to reach the cyst without permitting full communication with adjacent structures [11,12]. Although this approach poses a significant morbidity risk and entails the potential for mortality especially that are associated with spillage of the fluids into peritoneal cavity ad injury of the liver parenchyma, it is nevertheless viable and allows for a single surgical procedure to address both cysts without significant complications.
4. Conclusion
Hydatid cysts remain a significant health problem in our region, particularly when large pleural cysts occur in conjunction with sub phrenic liver cysts. Surgical intervention is the preferred first- line treatment, with a single stage thoracotomy proving to be more practical than other methods. This approach is especially beneficial for individuals who have both cysts, as it allows for both issues to be addressed in a single procedure while avoiding the need for an additional operation. By utilizing this method, healthcare professionals can provide patients with the most effective and efficient treatment possible.
Ethical consideration
The research was conducted in accordance with the principles set out in the Declaration of Helsinki (as revised in 2013). Ethical clearance was granted by the Institutional Review Board of KCMUCO. The informed consent was obtained from the patient to publish this case report and accompanying images.
Consent
Written informed consent was obtained from the patients to publish this case report and accompanying images. On request, a copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethical approval
Ethical approval for this study (pg 46/2023) was provided by the Ethical Committee Kilimanjaro Christian Medical University College research and ethical committee.
Funding
No funding for this research.
Author contribution
Elizabeth Ubald Wampembe: manuscript writing, patient clerkship and surgery.
Lele Mutombo Fabrice: literature search and manuscript review.
Jay Lodhia: manuscript review.
Joseph Elisante: assistant surgeon for surgery and case review.
Salum Kondo Chilonga: Critical review and final approval of the manuscript.
Anna Dohho - literature search and manuscript review.
Guarantor
Elizabeth Ubald Wampembe.
Research registration number
N.A. This is not a First in Man case report.
Conflict of interest statement
No conflict of interest.
References
- 1.Kern P., Menezes da Silva A., Akhan O., Müllhaupt B., Vizcaychipi K.A., Budke C., et al. 2017. The Echinococcoses. In; pp. 259–369. [DOI] [PubMed] [Google Scholar]
- 2.Black C. WHO_EB147 22MAY2020_761.jpg [Internet] 2020. http://apps.who.int/bookorders Available from:
- 3.Deplazes P., Rinaldi L., Alvarez Rojas C.A., Torgerson P.R., Harandi M.F., Romig T., et al. 2017. Global Distribution of Alveolar and Cystic Echinococcosis; pp. 315–493. [DOI] [PubMed] [Google Scholar]
- 4.Otero-Abad B., Torgerson P.R. A systematic review of the epidemiology of echinococcosis in domestic and wild animals. PLoS Negl. Trop. Dis. Jun 6 2013;7(6) doi: 10.1371/journal.pntd.0002249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brunetti E., Kern P., Vuitton D.A. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. Apr 2010;114(1):1–16. doi: 10.1016/j.actatropica.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Akbulut S. Parietal complication of the hydatid disease. Medicine (Baltimore) May 2018;97(21) doi: 10.1097/MD.0000000000010671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int J Surg [Internet]. May 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ernest E., Nonga H.E., Kassuku A.A., Kazwala R.R. Hydatidosis of slaughtered animals in Ngorongoro district of Arusha region, Tanzania. Trop. Anim. Health Prod. Oct 23 2009;41(7):1179–1185. doi: 10.1007/s11250-008-9298-z. [DOI] [PubMed] [Google Scholar]
- 9.Topçu S., Kurul I.C., Taştepe I., Bozkurt D., Gülhan E., Çetin G. Surgical treatment of pulmonary hydatid cysts in children. J. Thorac. Cardiovasc. Surg. Dec 2000;120(6):1097–1101. doi: 10.1067/mtc.2000.110181. [DOI] [PubMed] [Google Scholar]
- 10.Mazziotti S., Gaeta M., Blandino A., Barone M., Salamone I. Hepatobronchial fistula due to transphrenic migration of hepatic echinococcosis: MR demonstration. Abdom. Imaging. Sep 2000;25(5):497–499. doi: 10.1007/s002610000080. [DOI] [PubMed] [Google Scholar]
- 11.Loinaz C., Hernández T., Mitjavila M., Martín J., Ochando F., Madariaga M.L., et al. Biliobronchial fistula after liver surgery for Giant hydatid cyst. HPB Surg. Sep 2011;22(2011):1–4. doi: 10.1155/2011/347654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dokumcu Z., Arslan S., Divarci E., Erdener A., Ozcan C. Thoracoscopic treatment of pulmonary hydatid cysts may have a high morbidity risk in children: retrospective analysis. Eurasian J Med [Internet]. Oct 25 2017;49(3):172–177. doi: 10.5152/eurasianjmed.2017.17080. https://www.eajm.org//en/thoracoscopic-treatment-of-pulmonary-hydatid-cysts-may-have-a-high-morbidity-risk-in-children-retrospective-analysis-132979 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]