Abstract
Introduction and importance
Primary laryngeal tuberculosis (PLTB) is a rare condition. The symptoms and findings are not specific in most of the cases. Patients are diagnosed essentially based on histopathological examination and mycobacterial culture.
Case report
We report the case of a 42-year-old woman who presented to our hospital with dysphonia and dysphagia. Direct laryngoscopy revealed a lesion of the supraglottis. CT scan found a diffuse thickening of the entire surface of the larynx. A biopsy confirmed the diagnosis of tuberculosis.
Clinical discussion
Primary laryngeal tuberculosis is a rare clinical entity despite its close anatomical and physiological proximity to the lungs.
Conclusion
Clinician should keep in mind the existence of primary laryngeal tuberculosis to avoid delayed diagnosis and treatment, which can lead to high morbidity and mortality.
Keywords: Tuberculosis, Primary, Larynx, Anti tubercular drugs, Case report
Highlights
-
•
Primary laryngeal tuberculosis is a rare condition.
-
•
Incidence in rise
-
•
Non specific clinical presentation making it a diagnostic Dilemma
-
•
Need for early diagnosis and treatment
1. Introduction
Tuberculosis of the larynx is a rare disease accounting for less than 1 % of all cases of extrapulmonary tuberculosis (EPTB) [1]. Nevertheless, there is a resurgence of its incidence and its clinical pattern and spread mechanism have also changed [2]. Clinical manifestations are showing a changing trend towards predominant laryngeal symptoms with absence of constitutional symptoms. It is difficult to differentiate laryngeal tuberculosis from other inflammations and neoplasms based solely on physical examination. Laryngoscopy and biopsy are mandatory to establish a definitive diagnosis [3]. Treatment is mainly medical based on anti-tuberculosis drugs [4].
In this study, we report in this case primary laryngeal tuberculosis in a patient and we discuss the diagnostic difficulties and therapeutic management of this pathology. The work has been reported in line with the SCARE criteria 2023 [5].
2. Case report
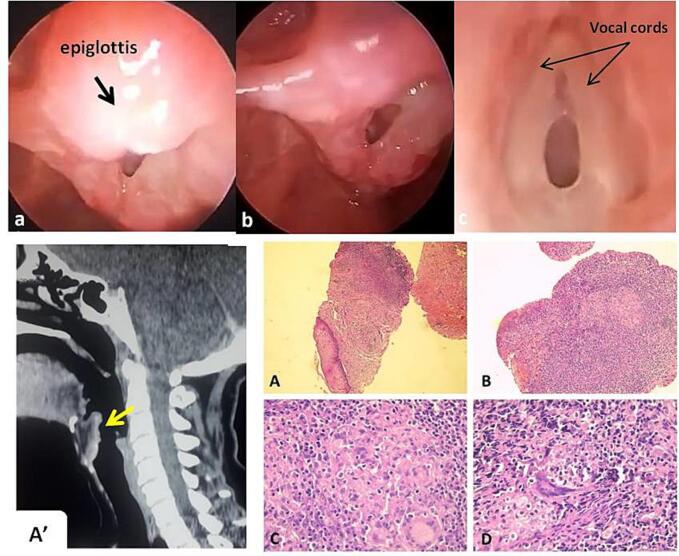
A 42-year-old female presented with worsening hoarseness accompanied by voice fatigue and dysphagia for one year. She had also irritative dry cough, but no other symptoms like fever, chest pain, alteration of the general state. She had no history of close contact with patients who had pulmonary TB. On examination, the patient was afebrile, with no cervical lymphadenopathy. Indirect laryngoscopy revealed significant diffuse edema and erythema, especially of the epiglottis, mimicking as acute epiglottitis. Vocal cords were moving with no signs of infiltration. After a standard evaluation, our patient underwent direct laryngoscopy (Fig. 1a,b,c) under general anesthesia and biopsy was taken from epiglottis. Her computed tomography (CT) scan is showed in Fig. 1A′. Furthermore, the patient had negative findings on radiological examinations of the chest and negative sputum cultures. So, there was no evidence of pulmonary primary tubercular dommage. The results of routine laboratory tests were unremarkable. Tuberculin skin test was positive and she was negative for the human immunodeficiency virus (HIV). The histopathological examination showed a chronic granulomatous inflammation without caseous necrosis and sections were negative for malignancy (Fig. 1A,B,C,D). Taking into account the endemicity in our country, the absence of other arguments in favor of granulomatosis, the diagnosis of laryngeal tuberculosis was retained. Since there was no evidence of the disease in any other organ or system, the diagnosis of PLTB was considered likely in our patient. Therefore, a standard six month treatment with a combination of isoniazid, rifampicin, pyrazinamide, and ethambutol was started for two months followed by isoniazid and rifampicin for additional four months. Our patient was under regular monthly follow up, and there was an improvement of laryngeal inflammatory lesions with no clinical or laboratory evidence of recurrence even after 1 year of treatment.
Fig. 1.
a,b. Direct laryngoscopy showing diffuse congestion and irregular lesions on the supra-glottic region (epiglottis and false vocal cords), arytenoids, interarytenoid region and aryepiglottic folds. c. Vocal cords were moving with no signs of infiltration.
Fig. 1A′. Laryngeal CT scan revealed a diffuse thickening and homogeneous contrast enhancement of the entire surface of the larynx with intact cartilaginous framework; B. Sagittal image showed irregular thickening of the epiglottic from where the biopsy was taken (arrow).
3. Discussion
Laryngeal tuberculosis is the most common granulomatous disease of the larynx and usually occurs as a complication of pulmonary tuberculosis [6,7]. Primary laryngeal tuberculosis is a rare clinical entity despite its close anatomical and physiological proximity to the lungs. With the advent of antitubercular drugs, the incidence has come down to less than 1 % of the extra-pulmonary locations of the disease [8].
The etiology of this pathology can be explained by many theories. It is the result of direct invasion of the larynx by inhaled mycobacteria, rather than ascending infection from the lower airways [6,8]. Larynx can also be infected via hematogenous or lymphatic spread [2,9].
This disease usually occurs in adult aged between 40 and 50 years. It is found more frequently in males than in females [2,4,9]. Currently, with the advent of anti-tubercular drugs, the clinical pattern of laryngeal tuberculosis has changed [10]. The presenting symptoms are typically hoarseness (80 %–100 %), odynophagia, and dysphagia (55 %–100 %). While dry cough (11 %–45 %) and dyspnea are uncommon symptoms [1,9].
Systemic signs (fever, asthenia, loss of weight and loss of appetite) are often minor in primary forms of laryngeal tuberculosis and alteration of the general state is essentially observed in advanced forms [1].
According to literature, tuberculosis of larynx is often seen in person who are chronic alcoholic and smokers, hence shares the same risk factors as that of laryngeal carcinoma [1,4]. In recent years, with the advent of antituberculosis chemotherapy, the incidence of TB has come down significantly, but there has been an increase in the incidence of (EPTB) including primary otorhinolaryngeal TB due to HIV infection [6]. Other predisposing factors that have been found to occur in these patients include the absence of Bacillus Calmette-Guerin vaccination, malnutrition, promiscuity and low immunity [4,9,11].
The diagnosis is essentially based on direct laryngoscopy with biopsy in order to specify the site and appearance of the tuberculous lesions and to exclude underlying pathologies [1,12]. The location of the lesion is extremely variable. Recent publications show that the commonest laryngeal sites affected by tuberculosis are the ligamentous vocal cords (50 %–70 %) and the least affected is the epiglottis. In cases of tuberculous epiglottitis, the epiglottis is infiltrated and swollen masking the rest of the larynx and causing severe odynophagia [1,7]. For our patient the lesion was supra-glottal. According to literature, the lesion is bilateral in 75 % of the cases [11]. Moreover, the morphological description has also changed. It has been reported that nonspecific or polypoid lesions are seen relatively more frequently than ulcerative or granulomatous lesions [3,7,10]. The danger of misdiagnosing laryngeal tuberculosis as a laryngeal cancer is evident. Deeper and repeated biopsies must be performed when histological examination is inconclusive. However, clinicians should also remember that these two diseases may co-exist. Several cases of concomitant carcinoma and tuberculosis have been reported in the literature [3,4].
Therefore, laryngeal biopsies remain the key to ascertain the diagnosis. Specimens are sent for histopathological examination and mycobacterial culture [1]. Anatomopathologic examination reveals the classical tuberculous follicle composed of a central zone of caseation surrounded by epithelioid cells and lymphocytes along with Langhans giant cells [1,3,8]. However, microscopy demonstrates chronic granulomatous inflammation with caseous necrosis, which is pathognomonic of tuberculosis, in only 34 % of cases [2]. In our case and in some cases of histological presentation showing absence of caseations, the TB of larynx is confirmed by response of patients to antitubercular therapy (ATT) [13].
The radiological findings of laryngeal tuberculosis are varied and non-specific, they depend on the stage and lesion extension. Computed tomography (CT) remains the reference imaging examination and typically demonstrates diffuse, bilateral lesions with no destruction of the laryngeal architecture. Calcifications are not common and the para-laryngeal fat spaces are usually spared. Certain features can differentiate this pathology from laryngeal carcinoma. The major differentiating feature from laryngeal malignancy is the intact laryngeal cartilaginous framework [2]. Moreover, CT scan allows precise assessment of any complications especially glottic or subglottic stenosis [1,11].
The chest radiograph must be done systematically in laryngeal tuberculosis to rule out pulmonary pathology [13]. However, CT scan of the thorax is not a routine investigation if the chest X-ray shows normal findings [9].
After confirming the positive diagnosis of laryngeal TB, treatment must be initiated as rapidly as possible [1]. The treatment of this disease is similar to pulmonary tuberculosis [13]. As per the World Health Organization guidelines, the laryngeal tuberculosis or EPTB should be treated with four drug regimens for 2 months followed by two drugs for the next 4 months. The drug combination used includes isoniazid, rifampicin, ethambutol, and pyrazinamide [13]. Initiation of ATT must be preceded by a detailed pretreatment assessment and must comprise close surveillance of treatment-related complications [1].
Laryngeal tuberculosis responds well to anti-tuberculosis chemotherapy within 18 weeks. Most cases in the literature had favorable outcomes and the overall mortality was low [3,9,12].
Thus, early diagnosis and timely administration of anti tubercular drugs provide good prognosis, completely curing the disease without any complications [10]. PLTB may progress into disseminated TB that carries a poor prognosis [4,9,12]. Moreover, it could cause arytenoid immobility, or glottic or subglottic stenosis, particularly in the presence of cricoid scarring [1,10].
Finally, treatment is primarily medical and is based on anti-tuberculosis chemotherapy. The duration of treatment typically ranged from 6 to 12 months [12]. Surgery is no longer part of the current treatment options, except for patients with laryngeal stenosis [1,11]. In the present case, our patient responded well to medical treatment by showing improvement in symptoms and endoscopic signs after several weeks.
4. Conclusion
There are very few cases of PLTB in literature and it must be considered as a differential diagnosis in patient with laryngeal lesions. Positive mycobacterial cultures along with a typical histopathological appearance remain the cornerstone of diagnosis. Consequently, otolaryngologists should keep in mind the existence of this disease to avoid delayed diagnosis and treatment. Timely administration of anti tubercular drugs and long-term follow-up provide good prognosis, completely curing the disease without any complications.
Funding
None sources of funding.
Ethical approval
Not applicable: no figure or data that compromise the identity of patients.
Author contribution
Bouatay Rachida: study conception, writing the paper
Bouaziz Nawres: writing the manuscript
Abdallah Hela: data analysis
Ben Hammouda Seifeddine: interpretation of the histological part
Koubaa Jamel: revising the manuscript
Guarantor
Rachida Bouatay
Consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflict of interest statement
The authors declare no conflicts of interest.
References
- 1.El Ayoubi F., Chariba I., El Ayoubi A., Chariba S., Essakalli L. Primary tuberculosis of the larynx. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2014;131:361–364. doi: 10.1016/j.anorl.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Ponni S., Venkatesan S.K., Saxena S.K., Suryanarayanan G. Primary laryngeal tuberculosis-changing trends and masquerading presentations: a retrospective study. Int J Otorhinolaryngol Head Neck Surg. 2019;5:634. [Google Scholar]
- 3.Agarwal R., Gupta L., Singh M., et al. Primary laryngeal tuberculosis: a series of 15 cases. Head Neck Pathol. 2019;13:339–343. doi: 10.1007/s12105-018-0970-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ling L., Zhou S.H., Wang S.Q. Changing trends in the clinical features of laryngeal tuberculosis: a report of 19 cases. Int. J. Infect. Dis. 2010;14:e230–e235. doi: 10.1016/j.ijid.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 5.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saldanha M., Sima N.H., Bhat V.S., Kamath S.D., Aroor R. Present scenario of laryngeal tuberculosis. Int J Otorhinolaryngol Head Neck Surg. 2018;4:242–246. [Google Scholar]
- 7.Kiakojuri K., Roushan M. Laryngeal tuberculosis without pulmonary involvement. Caspian J Internal Med. 2012;3(1):397–399. [PMC free article] [PubMed] [Google Scholar]
- 8.Pandiyan H., Sivanand N., Kumar S.S. Isolated laryngeal tuberculosis: a diagnostic dilemma. Indian J Otolaryngol Head Neck Surg. 2020;74:2308–2310. doi: 10.1007/s12070-020-02139-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guan L.S., Jun T.K., Azman M., Baki M.M. Primary laryngeal tuberculosis manifesting as irregular vocal fold lesion. Turk Arch Otorhinolaryngol. 2021;60(1):47–52. doi: 10.4274/tao.2021.2021-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim J.Y., Kim K.M., Choi E.C., Kim Y.H., Kim H.S., Choi H.S. Current clinical propensity of laryngeal tuberculosis: review of 60 cases. Eur. Arch. Otorhinolaryngol. 2006;263(9):838–842. doi: 10.1007/s00405-006-0063-5. [DOI] [PubMed] [Google Scholar]
- 11.El Kettani N.E., El Hassani M., Chakir N., Jiddane M. Primary laryngeal tuberculosis mimicking laryngeal carcinoma: CT scan features. Indian J Radiol Imaging. 2010;20(1):11–12. doi: 10.4103/0971-3026.59745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Benwill J.L., Sarria J.C. Laryngeal tuberculosis in the United States of America: a forgotten disease. Scand. J. Infect. Dis. 2014;46:241–249. doi: 10.3109/00365548.2013.877157. [DOI] [PubMed] [Google Scholar]
- 13.Swain S.K., Behera I.C., Sahu M.C. Primary laryngeal tuberculosis: our experiences at a tertiary care teaching hospital in eastern India. J. Voice. 2019;33(812):e9–14. doi: 10.1016/j.jvoice.2018.04.010. [DOI] [PubMed] [Google Scholar]