Abstract
Introduction
Solitary ovarian plasmacytoma is a rare form of extramedullary plasmacytic tumor that develops outside the bone marrow.
Presentation of case
We report the case of a 52-year-old female patient who consulted for pelvic pain and abdominal distension. Clinical examination revealed an abdominopelvic mass and a pelvic MRI confirmed a right ovarian mass. The diagnosis of ovarian plasmacytoma was made after exploratory laparotomy.
Discussion
Extramedullary plasmacytoma (EMP) is rare and most often found in the upper aerodigestive tract, ovarian localization is exceptional. Histological and immunohistochemical features of EMP highlights similarities with multiple myeloma. EMP treatment options are discussed, including radiotherapy, surgery, and chemotherapy. The prognosis of EMP depends on several factors, including tumor size and timing of treatment.
Conclusion
Solitary ovarian plasmacytoma is a rare but important entity to consider in the diagnosis of abdominopelvic masses. Appropriate treatment, such as surgery combined with radiotherapy, can be effective, although regular monitoring is necessary due to the risk of relapse and transformation into multiple myeloma.
Keywords: Ovarian plasmacytoma, Surgery, Radiotherapy, Case report
Highlights
-
•
Solitary ovarian plasmacytoma is a rare form of extramedullary plasma cell tumor.
-
•
Appropriate treatment, such as surgery combined with radiotherapy, can be effective.
-
•
Prognosis depends on several factors, including tumor size and timing of treatment.
1. Introduction
Plasmacytoma is a discrete, solitary mass of neoplastic plasma cells. It results from clonal proliferation of plasma cells that are cytologically and immuno-phenotypically identical to myeloma. Extramedullary plasmacytoma (EMP) is a rare entity arising in tissues other than bone, accounting for around 1 % of all plasma cell neoplasms. Over 90 % of extramedullary plasmacytomas occur in the head and neck, particularly in the upper airways; ovarian localization is very rare [1]. This case report has been reported per the SCARE 2020 criteria [2].
2. Presentation of case
The patient was 52 years old, of low socioeconomic status, with no particular pathological history, post-menopausal for two years, mother of 4 living children. She presented with eight months of pelvic pain with abdominal distension, with no associated urinary or digestive signs, all evolving in a context of altered general condition.
Clinical examination revealed a hard, fixed abdominal-pelvic mass reaching to the umbilicus and interfering with abdominal palpation. The cervix was normal and there was no abnormal uterine bleeding.
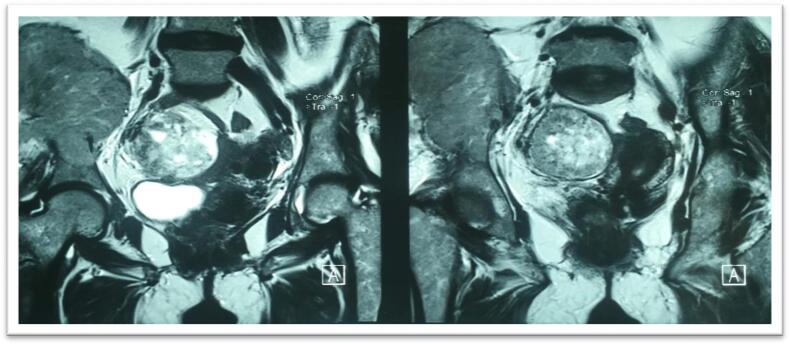
A pelvic MRI revealed a mass of probable ovarian origin, hyposignal T1, multi-lobulated, calcified in places, and slightly necrotic, heterogeneously enhanced after injection of gadolinium, measuring 100x86x50 mm (Fig. 1).
Fig. 1.
A mass of probable ovarian origin, hypo signal T1, multi-lobulated, calcified in places, and slightly necrotic, heterogeneously enhanced after injection of gadolinium, measuring 100 × 86 × 50 mm.
The patient's laboratory workup was normal, with carcinoembryonic antigen (CEA) at 1.8 ng/mL, Alpha Foeto-Proteine at 2.2 ng/mL, and serum cancer antigen (CA-125) at 25.6 U/mL.
The patient underwent exploratory laparotomy, which revealed a suspicious-looking polylobed right ovarian mass measuring 10 cm long, with moderate ascites. Total hysterectomy with bilateral salpingo-oophorectomy was performed, together with omentectomy, peritoneal biopsies, and ascites fluid collection (Fig. 2).
Fig. 2.
Operative items: Total hysterectomy without adnexal preservation, omentectomy, peritoneal biopsies, and ascites fluid sampling.
Anatomopathological examination of the surgical specimens showed a diffuse tumor proliferation in the right ovary and epiploic region, with an appearance of plasmacytic differentiation. Immunohistochemistry showed diffuse CD138 expression, confirming the plasma cell nature of the tumor. Anti-Kappa and anti-lambda tests were inconclusive, and CKAE1/AE3 was negative.
Postoperative blood and urine immuno-protein tests showed no monoclonal gammopathy; bone marrow investigations (myelogram and osteomedullary biopsy) revealed no plasma cell infiltration; the same applied to immunophenotyping and cytogenetic studies of bone marrow cells. A PET scan did not reveal any bone localization. The diagnosis was therefore extraosseous ovarian plasmacytoma.
Localized pelvic radiotherapy was indicated with rigorous clinical and biological monitoring with a current follow-up of 1 year.
3. Discussion
Extramedullary plasmacytoma (EMP) is a very rare primary plasmacytic tumor of the soft tissues, occurring most frequently (90 %) in the upper aerodigestive tract. It accounts for <5 % of all plasma cell tumors, remains generally localized, and responds better to treatment [3].
EMP refers to plasma cell tumors that originate outside the hematopoietic tissues of the bone marrow. With the continuing advent of new drugs, the survival time of myeloma patients has increased considerably, but the incidence of extramedullary lesions is rising [3]. Using sensitive imaging technologies such as PET-CT and MRI, the rate of EMP diagnosis has improved considerably [4].
The age of presentation is quite variable, ranging from 30 to 84 years, with a mean age of 46. A single case involving a 12-year-old child has been described [5].
EMP shares a common cell type, morphology, and pathology with MM, but lacks the systemic properties of its more severe counterpart. Diagnosis of a solitary EMP requires the exclusion of multiple myeloma. This distinction is important, as over 60 % of patients treated for solitary plasmacytoma are cured with local therapies alone, whereas 5-year survival for MM patients is around 35 % [3]. Diagnostic criteria for solitary EMP include a histologically confirmed solitary plasma cell lesion, <5 % plasma cells found on bone marrow biopsy from a distant site, absence of end-organ lesions as found in MM, and a whole-body skeletal survey to exclude intramedullary disease [1,5]. In solitary EMP, all laboratory values should be normal, except gammapathies that may be monoclonal. These include immunoglobulin beta2, blood count, electrolytes, serum-free light chains, and serum protein electrophoresis [1].
EMP is considered devoid of characteristic clinical manifestations and usually manifests as pelvic pain caused by compression of adjacent tissues. The tumor is usually diagnosed at a large size [4]. The largest reported size was a 35 cm long axis, while the minimum reported size was a 4 cm long axis, somewhat reminiscent of the first case reported by Voegt in 1938, who described the tumor as the size of a fist [6]. The large size at presentation is more likely due to the insidious progression of this tumor [3].
EMP in the ovary is rare and lacks specific clinical and radiological features. The diagnostic criteria for EMP are as follows [4]:
-
-
histologically confirmed solitary plasma cell lesion;
-
-
Bone marrow biopsy showing <5 % of plasma cells;
-
-
Absence of systemic forms, such as MM;
-
-
Skeletal survey excluding intramedullary disease;
Except for possible monoclonal gammapathies, all laboratory tests were normal, including the beta-2 microglobulin test, complete blood count, electrolytes, serum-free light chains, and serum protein electrophoresis [7].
Ovarian EMP can be diagnosed when the clinical history is consistent and the following imaging features are present: a well-circumscribed solitary soft tissue mass in the unilateral or bilateral ovaries. CT showing homogeneous masses of medium density with significant and homogeneous enhancement after contrast injection. MRI showed homogeneous lesions with slightly hypointense signals on T1, isointense signals on T2, restricted diffusion, and low ADC value <1.2 × 10−3mm2/s [4].
EMP is composed of neoplastic monoclonal plasma cells, but there are obvious differences. Susnerwala and Shanks classified EMP into three grades according to the degree of cellular differentiation: grade I (low grade), grade II (intermediate grade), and grade III (high grade) [8]. Immunohistochemistry generally shows positive expressions of CD79a, CD38, CD138, and Lambda/Kappa, with a Ki-67 proliferation index of around 40 % and negative expressions of CD3, CD5 and CD20 [7,9].
There is no unified treatment regimen for EMP. However, a treatment regimen that takes into account the specific site, size, differentiation, and invasiveness of the lesion is necessary. Radiotherapy is the first choice for head and neck lesions. For patients undergoing radiotherapy alone, a moderate radiation dose (40–60 Gy) can achieve a local control rate of 80–100 % (overall local control rate 88 %), with no obvious dose-dependent effect [2,10]. In addition, for lesions of the gastrointestinal tract and testicles, surgical resection has effects roughly equivalent to those of radiotherapy, and for patients with high malignancy and relapse after treatment, adjuvant chemotherapy may be considered [1]. Treatment with the targeted drug bortezomib has been reported to have a good effect on EMP. Therefore, second-line drugs combined with the new drug bortezomib can be used as first-line treatment in patients with MM and EMP [10].
EMP prognosis depends on many factors, including the patient's general condition, tumor size, degree of differentiation and invasion, and whether treatment is standardized and timely. The 5-year survival rate for patients with EMP is around 50–70 %, and the median survival time after treatment is around 6–8 years. Some patients followed for EMP progress to MM after some time [1,3].
4. Conclusion
Solitary ovarian plasmacytoma is a very rare entity among extramedullary plasmacytomas. It is essential to take them into account in the differential diagnosis in front of abdominopelvic masses to help patients receive appropriate treatment, although a thorough work-up is necessary to establish an accurate diagnosis of this entity. Our case appears to have been successfully treated by surgery combined with radiotherapy, with no signs of recurrence after a 1-year follow-up. The risk of local and distant relapse and transformation into MM justifies regular surveillance.
Ethical approval
I declare on my honor that my establishment has exempted the ethical approval.
Funding
None.
Author contribution
El Abbassi Imane: Corresponding author writing the paper
Elhodaigui Najlae: Writing the paper
Boufettal Houssine: Study concept
Mahdaoui Sakher: Study concept
Samouh Naima: Correction of the paper
Guarantor
Dr. El Abbassi Imane
Research registration number
researchregistry2464
Patient's consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflict of interest statement
The authors declare having no conflicts of interest in this article.
References
- 1.Gouiaa N., Ellouze S., Bellaaj H., Louati D., Abid H., Mnif H.…Boudawara T. Plasmocytome ovarien bilatéral: une observation. Imagerie de la Femme. 2011;21(3):111–114. [Google Scholar]
- 2.Agha R.A., Franchi T., Sohrab C., Mathew G., Kirwan A., Thomas A., et al. The SCARE 2020 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84(1):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 3.Haloui A., Karich N., Akouh N., Seghrouchni N., Najioui Y., Aissaoui A.…Bennani A. Ovarian plasmacytoma: a case report. Pan Afr. Med. J. 2023;44 doi: 10.11604/pamj.2023.44.108.37603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jiang Q., Sun C., Li J., Fu J. Clinical and radiological presentations of ovarian plasmacytoma. Am. J. Transl. Res. 2023;15(2):1452. [PMC free article] [PubMed] [Google Scholar]
- 5.Andze G., Pagbe J.J., Edzoa T., Tchokoteu P., Mbakop A., Yomi J. Le plasmocytome solitaire extraosseux ovarien: à propos d’un cas exceptionnel chez une enfant de 12 ans. J. Chir. 1993;130(3):137–140. [PubMed] [Google Scholar]
- 6.Voegt H. Extramedullary plasmocytoma. Virchows Arch. Pathol. Anat. 1938;320:497–508. [Google Scholar]
- 7.El Maataoui A., Taoufiq A., Fares S., Sokori K. Étude transversale descriptive sur les profils cliniques et paracliniques des gammapathies monoclonales au niveau d’une région agricole du Souss-Massa au Maroc. Pan Afr. Med. J. 2022;41(1) doi: 10.11604/pamj.2022.41.69.32470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Susnerwala S.S., Shanks J.H., Banerjee S.S., Scarffe J.H., Farrington W.T., Slevin N.J. Plasmocytome extramédullaire de la région de la tête et du cou: corrélation clinicopathologique dans 25 cas. Br. J. Cancer. 1997;75(6):921–927. doi: 10.1038/bjc.1997.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ayed K., Hamza F., Belayouni R., Maaloul M., Guermazi F. Plasmocytome ovarien bilatéral découvert par TEP-TDM au 18FDG dans le cadre du bilan d’extension d’un myélome multiple: à propos d’un cas. Méd. Nucl. 2023;47(2):85–86. [Google Scholar]
- 10.Salah H.B., Hdiji S., Makni S., Ghorbel A.M., Boudawara T., Elloumi M., Daoud J. Plasmocytomes extraosseux. Cancer/Radiothérapie. 2012;16(4):282–287. doi: 10.1016/j.canrad.2012.03.008. [DOI] [PubMed] [Google Scholar]