Abstract
Introduction:
Accidental ingestion of caustic agents poses a significant concern in pediatric emergency departments globally. It is a growing public health concern in low-to-middle income countries, which often lack comprehensive data reporting. This study examines high doses of corticosteroid treatment outcomes of caustic ingestion injuries in Syrian pediatric patients, addressing clinical features, and associated variables.
Methods and materials:
A retrospective observational study was conducted at University Pediatric Hospital from January 2016 to January 2019. Medical records were reviewed for patients aged <10 years with esophagoscopy-confirmed grade IIa, IIb, or III burns. Data collected included sociodemographics, esophagoscopy results, treatment details, and outcomes.
Results:
Among 114 pediatric patients, 76 (67%) were males and 38 (33%) were females. Age groups included <1 year (11%), 1–3 years (39%), 3–5 years (29%), 5–7 years (11%), and >7 years (11%). Alkaline burns accounted for 54% of injuries, acidic for 32%, and other substances for 13%. Complications included bleeding (19%) and psychomotor disability (7%). The most common burn site was the entire esophagus (62%), with 81% having grade II burns. Healing was achieved in 71% of patients with high doses of corticosteroids treatment, and 29% required dilation, with final 92% healing rate.
Conclusion:
The use of corticosteroids for esophageal strictures remains inconclusive, demanding further robust research with larger sample sizes and control groups. While our study revealed that high doses of corticosteroids treatment followed by esophageal dilation had a 92% success rate. However, our study demonstrates promising results, methodological limitations and absence of a control group underscore the need for more definitive evidence. Both alkali and acidic ingestion contribute to stricture development.
Keywords: Caustic ingestion, pediatric patients, esophageal strictures, corticosteroid treatment, treatment outcomes, Chi-square test
Introduction
Caustic ingestion remains a global scourge, particularly affecting young children aged one to three, often resulting in severe acute injuries and long-term complications, including esophageal perforation, strictures, and even death.1–11 Apart from perforation, the most serious complication is the formation of strictures with a frequency of 5%, increasing to 47% in severe cases.12–14 Various therapeutic approaches have been employed, including esophageal stents, corticosteroid medication, early dilatation prior to stricture development, or a combination of these techniques, to prevent stricture formation. 15 However, the effectiveness of corticosteroids in preventing corrosive-induced strictures remains a subject of debate.16–18 Animal trials have shown that steroids significantly reduce the incidence of strictures.14,15 Caustic ingestion poses a significant public health concern, especially in low-to-middle income countries like Syria, where the incidence is increasing and the data is scarce.6,19,20 Given these circumstances, it is crucial to evaluate treatment protocols for individuals who have ingested corrosive substances and their associated factors, with a specific focus on Syria, a country facing an 11-year-long conflict that exacerbates healthcare challenges. Following an extensive review of the available literature, no studies were found that specifically examined the outcomes of caustic ingestion high doses of corticosteroids treatment in Syrian patients. However, the data hold immense importance for the advancement of health promotion and healthcare services in Syria. Therefore, the objective of this study was to comprehensively analyze the clinical features, treatment outcomes, and relevant variables associated with caustic ingestion injuries in children receiving treatment at the University Pediatric Hospital.
Methods and materials
Study design, settings, and variables
Our study focuses on a retrospective observational study conducted at University Pediatric Hospital, including patients who were admitted to the emergency department with caustic ingestion between January 2016 and January 2019. The University Pediatric Hospital is the largest pediatric hospital in Syria and the only government hospital in Damascus. Prior to data collection, Stemosis data collection group underwent training sessions covering caustic ingestion in pediatric patients and the specific information to be gathered for the study. In March 2022, data were extracted from the medical records stored in paper-based archives and subsequently entered Excel spreadsheet. Due to paper-based medical records in our study, parents were contacted via telephone to validate the data and provide any additional missing details, including sociodemographic characteristics.
Our research methodology involved collecting pertinent data from the patients’ medical records including sociodemographic characteristics, esophagoscopy results, feeding state, complications, caustic substance type, physicians’ examination, and treatment course. Rigid esophagoscopy results was performed under general anesthesia in all patients included in the study within 24–48 h of injury. The mouth, larynx, and esophagus were assessed and the esophagus injury was classified according to Zargar classification as follows 21 :
Grade I: Superficial injury: This grade represents the mildest form of caustic injury. It is characterized by superficial mucosal erythema or edema without ulceration or necrosis.
Grade IIa: Deep injury without stricture: This grade indicates a deeper injury involving the submucosal layer but without the development of strictures. It may present with ulceration, necrosis, or blisters.
Grade IIb: Deep injury with stricture: In this grade, there is a deep injury with the development of strictures.
Grade III: Perforation or complete destruction: This grade represents the most severe form of caustic injury. It involves full-thickness necrosis of the esophageal wall, leading to perforation or complete destruction.
In the present study patients with endoscopic findings “normal or grade I” with no dysphagia are indicated as Healed group and the patients with other classification in endoscopic findings are indicated as Non-Healed group. Moreover, using the endoscopic findings the site of the injured esophagus was determined as upper, middle, lower, and whole esophagus. The feeding state previous to the injury was considered as liquid state (breast-feeding, formula-feeding, or both), solid state, and diversified nutrition. Complications after the caustic ingestion found in our study are bleeding and psychomotor development disability (disability in cognitive process or physical activity). The type of caustic substances are acidic, alkaline, and other substances.
The treatment protocol, which is adopted from previous study, where physicians gave patients Methylprednisolone intravenously at high doses (1 g/1.73 m2/day) as a prolonged therapy along with antibiotics and PPIs,22,23 involved the administration of ceftriaxone (100 mg/kg/day) and omeprazole (2 mg/kg/day) intravenously. In addition to the administration of anti-reflux therapy to prevent any secondary damage caused by gastroesophageal reflux, which significantly increases the risk of stricture formation (Figure 1). 24
Figure 1.
Treatment protocol using high-dose steroids for pediatric caustic ingestions.
Oral feeding was stopped, and total parenteral nutrition was started. Methylprednisolone was given intravenously at high doses (1 g/1.73 m2/day), lasting 6 h per day for 10 days. On the 10th day, esophageal endoscopy was performed. If the endoscopy showed a normal esophagus or a minor injury (grade I), the intravenous infusion was halted, and oral prednisolone was initiated for a duration of 2 weeks, gradually reducing the dosage. In cases where the endoscopy revealed moderate (grade II) or severe (grade III) injuries, the intravenous methylprednisolone infusion was continued for an additional 5 days (days 10–15 post-injury). On the 15th day, another endoscopy was performed. If the results indicated a normal esophagus or grade I injury, the intravenous infusion was stopped, and oral prednisolone was initiated for 2 weeks, gradually reducing the dosage. If the injuries persisted on the 15th day, the intravenous infusion was continued until the 20th day when another endoscopy was conducted. If the results were normal or showed grade I injury, the intravenous infusion was stopped, and oral prednisolone was administered. However, if the injuries persisted on the 20th day, the intravenous infusion was discontinued, and oral prednisolone was administered, gradually reducing the dosage. A gastro-esophageal barium swallow was performed after 3 weeks to initiate dilatation.
Study sample size and participants
The research in question employs a retrospective study design that is based on the comprehensive analysis of all pediatric patients admitted to the University Pediatric Hospital in Syria due to caustic ingestion during the specified study period. Since this study incorporates the entire population that meets the defined criteria, formal sample size calculation is not applicable and is unnecessary. But if we use Cochran’s sample size formula with the assumption of 95.5% confidence level (Z = 2), e is the margin of error which is 10%, p is the (estimated) proportion of the population which has the attribute in question, and it equals 50% (or 0.5), and q is 1−p.
Therefore, with a confidence of 95.5 and an error ranging from 5% to 10%, a sample size should not be less than 100 individuals. And we collected 114 participants. 25
The eligibility criteria for patient enrollment in this study comprised the following conditions:
Patients’ age below 10 years.
Arrived to the hospital within 48 h of injury and had esophagoscopy within 24–48 h of injury.
Had grade IIa, IIb, or III esophageal burns due to ingestion of caustic substances according to Zargar classification. Initially, a total 119 patients were included in the study.
However, we excluded three patients due to the inability to establish communication with their parents via phone calls or due to incomplete medical records. Additionally, two patients known to swallowed household bleach (sodium hypochlorite) were excluded from the study since this substance known to cause only superficial injury of the mucosa and no reported results causing strictures in pediatric patients. 26
Consequently, the final analysis included 114 patients. Our research adhered to the ethical standards outlined in the Declaration of Helsinki and was carried out on human subjects. Approval for the study was obtained from the Ethical Committee at Damascus University’s Faculty of Medicine (ID: 14152). Written Informed consent was obtained from all the legally authorized representatives of the subjects prior to study.
Statistical analysis
The data analysis was conducted using IBM SPSS version 25 for data analysis. Categorical variables describing demographic characteristics were presented using frequency and percentage. Although continuous variables describing the characteristics were presented using mean and standard deviation. To compare categorical variables, The chi-square test was employed. Statistical significance was based on a value of p-value less than 0.01.
Results
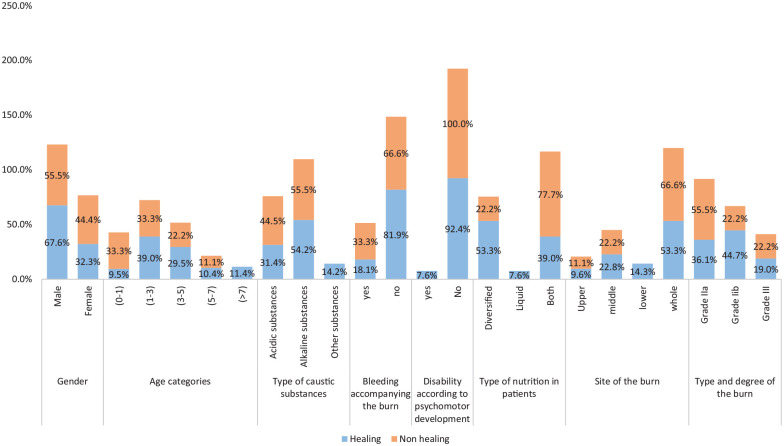
We reviewed the medical records of 114 pediatric patients admitted University Pediatric Hospital’s emergency department between January 2016 and January 2019. The study included 76 males (67%) and 38 females (33%) across different age groups. The patients were categorized as follows: 13 (11%) were under 1 year old, 44 (39%) were between 1 and 3 years old, 33 (29%) were between 3 and 5 years old, 12 (11%) were between 5 and 7 years old, and 12 (11%) were above 7 years old (Table 1). The average age of the patients was 3.9 ± 2.7 years. Most esophageal caustic ingestion burns (54%) were caused by alkaline substances, whereas 37 (32%) and 15 (13%) patients had burns caused by acidic and other substances, respectively. Only 22 (19%) patients experienced accompanying bleeding, and 8 (7%) had psychomotor disability. Before the incident, approximately half of the patients (51%) had a diverse type of nutrition, including liquid nutrition such as breast-feeding or formula-feeding (8%) and a combination of diversified and liquid nutrition (42%) (Figure 2).
Table 1.
Comparison of variables between healed and non-healed groups.
| Patients groups | Total n = 114 (%) a | p-Value* | ||
|---|---|---|---|---|
| Characteristics | Healing n = 105 (%) a (%) b | Non healing n = 9 (%) a (%) b | ||
| Gender | ||||
| Male | 71 (62%) (67.6%) | 5 (4%) (55.5%) | 76 (67%) | 0.01 < 0.46 |
| Female | 34 (30%) (32.3%) | 4 (4%) (44.4%) | 38 (33%) | |
| Total | 105 (92%) (100%) | 9 (8%) (100%) | 114 (100%) | |
| Age categories | ||||
| 0–1 | 10 (9%) (9.5%) | 3 (3%) (33.3%) | 13 (11%) | 0.01 < 0.25 |
| 1–3 | 41 (36%) (39%) | 3 (3%) (33.3%) | 44 (39%) | |
| 3–5 | 31 (27%) (29.5%) | 2 (2%) (22.2%) | 33 (29%) | |
| 5–7 | 11 (10%) (10.4%) | 1 (1%) (11.1%) | 12 (11%) | |
| +7 | 12 (11%) (11.4%) | 0 (0%) (0%) | 12 (11%) | |
| Total | 105 (92%) (100%) | 9 (8%) (100%) | 114 (100%) | |
| Type of caustic substances | ||||
| Acidic substances | 33 (29%) (31.4%) | 4 (4%) (44.5%) | 37 (32%) | 0.01 < 0.42 |
| Alkaline substances | 57 (50%) (54.2%) | 5 (4%) (55.5%) | 62 (54%) | |
| Other substances | 15 (13%) (14.2%) | 0 (0%) (0%) | 15 (13%) | |
| Total | 105 (92%) (100%) | 9 (8%) (100%) | 114 (100%) | |
| Bleeding accompanying the burn | ||||
| Yes | 19 (17%) (18.1%) | 3 (3%) (33.3%) | 22 (19%) | 0.01 < 0.27 |
| No | 86 (75%) (81.9%) | 6 (5%) (66.6%) | 92 (81%) | |
| Total | 105 (92%) (100%) | 9 (8%) (100%) | 114 (100%) | |
| Disability according to psychomotor development | ||||
| Yes | 8 (7%) (7.6%) | 0 (0%) (0%) | 8 (7%) | 0.01 < 0.39 |
| No | 97 (85%) (92.4%) | 9 (8%) (100%) | 106 (93%) | |
| Total | 105 (92%) (100%) | 9 (8%) (100%) | 114 (100%) | |
| Type of nutrition in patients | ||||
| Diversified | 56 (49%) (53.3%) | 2 (2%) (22.2%) | 58 (51%) | 0.01 < 0.07 |
| Liquid | 8 (7%) (7.6%) | 0 (0%) (0%) | 8 (7%) | |
| Both | 41 (36%) (39%) | 7 (6%) (77.7%) | 48 (42%) | |
| Total | 105 (92%) (100%) | 9 (8%) (100%) | 114 (100%) | |
| Site of the burn | ||||
| Upper | 10 (9%) (9.6%) | 1 (1%) (11.1%) | 11 (10%) | 0.01 < 0.66 |
| Middle | 24 (21%) (22.8%) | 2 (2%) (22.2%) | 26 (23%) | |
| Lower | 15 (13%) (14.3%) | 0 (0%) (0%) | 15 (13%) | |
| Whole | 56 (49%) (53.3%) | 6 (5%) (66.6%) | 62 (54%) | |
| Total | 105 (92%) (100%) | 9 (8%) (100%) | 114 (100%) | |
| Type and degree of the burn | ||||
| Grade IIa | 38 (33%) (36.1%) | 5 (4%) (55.5%) | 43 (38%) | 0.01 < 0.34 |
| Grade IIb | 47 (41%) (44.7%) | 2 (2%) (22.2%) | 49 (43%) | |
| Grade III | 20 (18%) (19%) | 2 (2%) (22.2%) | 22 (19%) | |
| Total | 105 (92%) (100%) | 9 (8%) (100%) | 114 (100%) | |
Percentage of total rounding to the nearest one.
Percentage of patients groups rounding to the nearest 10th.
Pearson Chi-square.
Figure 2.
Illustrating the characteristics of sample patients within the healed and non-healed groups.
Regarding the burn sites, more than half of the patients (62%) had burns throughout the entire esophagus, which was the most common location. Other burn sites were distributed as follows: 26 (23%) in the middle, 15 (13%) in the lower, and 11 (10%) in the upper regions. Most patients (81%) had second-degree burns, with 43 classifieds as grade IIa and 49 as grade IIb, whereas 22 (19%) patients had grade III burns. Our study did not document any early complications such as mediastinitis, pneumonia, or perforation (Figure 2).
Among the 114 patients, 81 (71%) achieved healing after corticosteroid treatment, whereas 33 (29%) patients with strictures required dilation. Following dilation, only 9 (7.89%) patients had persistent strictures requiring further management, which was beyond the scope of our study. The treatment plan yielded a remarkable healing rate of approximately 92%. A flow diagram illustrating the patient treatment plan is presented in Figure 3.
Figure 3.

Illustrating the treatment protocol reaching the healed and non-healed groups.
According to Table 1 and Figure 2, the patient’s gender did not have a statistically significant impact between the two groups as both male and female patients exhibited similar outcomes. Likewise, the different age groups did not show variations as well. Other variables, including the type of caustic substance, presence of bleeding with the burn, psychomotor disability, and type of nutrition, did not statistically differ between the two groups. Furthermore, patients with different burn sites and varying burn grades exhibited similar results.
Discussion
Caustic ingestion in pediatric patients is a significant medical and social problem,10,11,27 with potential severe consequences, including stenosis, dysphagia, pain, and malnutrition. 18
Clinicians have commonly used steroids as a treatment to prevent the formation of stenosis and strictures. However, the effectiveness of this treatment remains uncertain due to limited studies and inadequate statistical power.26,28
A previous study recommended the use of corticosteroids for second- and third-degree cases. 18 Therefore, our retrospective study aimed to evaluate the use of steroids in pediatric patients with caustic ingestion and second and third-degree injuries. In 1950, Spain et al. first assessed the effect of steroids on the inflammatory response in mice, and subsequent studies have investigated their impact on esophageal stricture formation. 29 Povilavičius et al. conducted a study where all patients underwent endoscopic dilation alone, with satisfactory outcomes achieved after an average of 15 dilation procedures. 24
In a study by Usta et al., 16 which focused on grade IIb esophageal burns only, the stricture development rate was significantly lower in the patients treated with high doses of methylprednisolone (1 g/1.73 m2 per day for 3 days), with ceftriaxone and ranitidine than in those who did not receive this treatment modality, with 3.53 times greater stricture formation in the control group compared to the study group. The positive effect of methylprednisolone was also noted in a study by Boukthir et al. 23 and in a study from Tunisia. 30 In addition, for the study by Usta et al. 16 The novel methodology employed in this study indicates that patients with grade 2B injuries, who exhibit both an elevated risk of stricture formation and a negligible risk of perforation, may derive the greatest therapeutic benefit and suffer the least potential harm from the wound-softening effects of glucocorticoid treatment. 6 However, Anderson et al. 26 concluded that stricture formation is related only to the severity of the corrosive injury. In their study, 21 of 31 patients who received steroids and 18 of 29 controls did not have strictures (p > 0.05). It is worth noting that the control group had 13 patients with first-degree burns compared to only 6 in the steroid group and 5 patients with second-degree burns in the control group compared to 15 in the steroid group. 26 Another point is that recent pediatric guidelines have added Usta’s protocol for the management of grade IIb injuries to their recommendations.6,31
In our study, the use of corticosteroids resulted in 71% satisfactory results, and when followed by a single endoscopic dilation procedure, a total of 92% satisfaction was achieved. This suggests that using corticosteroids followed by dilation, when necessary, can yield satisfactory outcomes with fewer invasive procedures required.
Howell et al. 18 reported that patients with first-degree burns showed complete healing without strictures and had a favorable prognosis. Consequently, the use of corticosteroids is not recommended for these patients. However, patients with second and third-degree burns are at risk of developing esophageal strictures. Howell et al. 18 found that the use of steroids in these patients demonstrated statistical significance compared to patients who did not receive steroid treatment. Furthermore, a previous review highlighted that the available evidence does not support the use of corticosteroids due to methodological weaknesses and small sample sizes in the primary studies. 17
Therefore, further studies with a control group and a significant sample size are needed to obtain more definitive results.
The extent and circumference of the injury play a significant role in the development of esophageal strictures. 24 Acidic substances primarily cause coagulative necrosis at the superficial layer, whereas alkaline substances result in deeper injuries, reaching the muscles with liquefaction necrosis. Hence, alkali ingestion, particularly lye, is associated with more severe esophageal lesions. 24 Both acidic and alkaline substances have been linked to the development of strictures, as demonstrated in our study. 31
In our study, the ratio of males to females was similar to a previous study by Usta et al., 16 where 54.2% were boys and 45.8% were girls. This aligns with another study that indicated a male-to-female ratio of 2:1. 32
The predominance of male patients was also observed in a systematic review by Rafeey et al., 33 emphasizing the need for increased attention and care by parents toward young boys to prevent such ingestion incidents. Most patients in our study were between 1 and 3 years old, and 79% of patients were under 5 years old, which is older than in other studies where 85% of patients were under 3 years old. 34 This pattern may be attributed to children’s curiosity and eagerness to explore new things. 35 Although our study did not find statistically significant differences in gender, age category, feeding state, and other variables, this may be due to the small sample size. This further emphasizes the need for more studies to assess various variables that impact the treatment of pediatric patients with caustic ingestion.
The most common symptoms observed in patients who experienced caustic ingestion were related to the digestive system, respiratory system, and ear, nose, and throat region. 33 However, the relationship between the severity of the injury and the presence of symptoms remains uncertain. 20
In the analysis conducted by Casasnovas et al., 32 no significant predictive relationship was found between esophageal burns and the presence of symptoms or signs.
In our study, no early complications such as mediastinitis, pneumonia, or perforation were documented. However, in terms of bleeding, which are more commonly associated with stomach involvement, we found that 22 children had burns in the esophagus accompanied by active bleeding, accounting for 19% of the cases. This is in contrast to the study conducted by Usta et al., 16 where no evidence of early complications, including mediastinitis, pneumonia, upper gastrointestinal bleeding, or perforation, was reported. It is worth noting that bleeding following corrosive ingestion typically resolves on its own and is self-limiting. 20 Moreover, when examining the condition at discharge, there were no significant differences between those who experienced bleeding and those who did not. This could be attributed to the low occurrence of non-healing cases compared to cases that had already healed.
Our study was constrained by several limitations, primarily related to its retrospective design and small sample size. In our study, although we achieved a 92% success rate when using steroids followed by esophageal dilation, if necessary, we did not include a control group. This study primarily focused on early treatment outcome of the patients, and no late follow-up were done due to the war and resulting circumstances such as difficulty in transportation in Syria, our study included only patients who treated with steroids with no control group to further assess the benefit of this treatment.
Conclusion
Caustic substance ingestions persist as a substantial public health burden globally, with considerable associated morbidity and mortality. The use of corticosteroids for esophageal strictures remains inconclusive, demanding further robust research. The research addressed a critical gap in the existing literature by specifically examining the outcomes of caustic ingestion in the context of an 11-year-long conflict in Syria, underscoring the importance of effective treatment strategies.
The employed treatment protocol, including high doses of corticosteroids, intravenous ceftriaxone, omeprazole, and esophageal dilation, if necessary, demonstrated a commendable success rate of 92% in preventing esophageal strictures.
Although the study primarily focused on immediate treatment outcomes, the findings lay the groundwork for future research endeavors, especially concerning the long-term impact of high doses of corticosteroid treatment. The extent and type of injury were also found to play a significant role in the development of esophageal strictures. Finally, this study highlights the pressing need for more comprehensive research to conclusively determine the efficacy of high-dose corticosteroid treatment, particularly in the unique healthcare context of low-income or stricken countries.
Limitations
The study faced several challenges and limitations:
First, it is important to acknowledge the unique context in which this research was conducted. Syria’s ongoing conflict and related challenges, including difficulty in transportation and data collection, presented significant obstacles to conducting comprehensive long-term follow-up studies.
Second, the retrospective study design employed in this research comes with inherent limitations that must be acknowledged. the study focuses on a specific hospital’s patient population during a defined period, potentially differing from cases treated elsewhere or those not admitted. Incomplete or missing data from medical records and the exclusion of certain patients due to unavailable information introduce further limitations.
Third, the study focuses on a specific hospital’s patient population during a defined period, potentially differing from cases treated elsewhere or those not admitted. The exclusion of certain patients due to unavailable information introduce further limitations.
In our study, although we achieved a 92% success rate when using steroids followed by esophageal dilation, if necessary, we did not include a control group. Furthermore, a previous review highlighted that the available evidence does not support the use of corticosteroids due to methodological weaknesses and small sample sizes in the primary studies. 28 However, despite these limitations, retrospective studies serve as valuable tools for hypothesis generation and initial exploration of associations, particularly when prospective research is unfeasible or unethical. Acknowledging these constraints is crucial for interpreting the findings appropriately and provides a basis for designing future research to offer more robust evidence on the subject.
However, acknowledging these constraints is crucial for interpreting the findings appropriately and provides a basis for designing future research to offer more robust evidence on the subject.
Acknowledgments
The authors would like to thank the data collection team for their efforts in participating in this study. They thank Mr. Mohmmad Emad Hamadiya and Ms. Aya Kabbani for their efforts in visually displaying the figures for this research, and Ms. Hiba Faraj for her contribution and efforts to help analyze the data several times. They also wish to show their appreciation to Stemosis for Scientific Research, a Syrian Scientific Research official entity managed by Dr. Nafiza Martini for the scientific environment they provide and their considerable contribution in publishing this article and would like to thank the anonymous reviewers for their constructive comments.
Footnotes
Authors’ note: Stemosis: Stemosis for Scientific Research, a Syrian Non-Governmental Organization (NGO), licensed by “the Ministry of Higher Education and Scientific Research by Resolution No. 5/011006/54 on the date 16/4/2021” and “the Ministry of Social Affairs and Labor by Resolution No. 2395 on the date 2/10/2021,” we aim to enhance scientific research in Syria among youth researchers in many specializations and raise the classification of Syrian universities through scientific publishing in highly rated international peer-reviewed journals. Stemosis for Scientific Research group of collaborators: Mustafa Albokai (mustafa.albokai@gmail.com); Majd Hanna (mzu.hn-407@hotmail.com); Douaa Albelal (douaa.albelal98@gmail.com); Osama Al Horani (osama.alhorany@gmail.com); Riffa Alassri (Rfaaassri@gmail.com); Raghad Alhelou (Raghadallholo2000@gmail.com); Nour Kara Tahhan (nour.kara.tahan@gmail.com); Ahmad Al-Farouh (ahmadfarouh213@gmail.com). They belong to Faculty of Medicine, Damascus University, Damascus, SYR and Stemosis for Scientific Research, Damascus, SYR.
Author contributions: Martini Nafiza and Almasri Imad-Addin are first authors equally. Martini Nafiza: Conceptualization, methodology, writing original draft, editing and reviewing. Almasri Imad-Addin: Methodology, performing the statistical analysis, editing, and reviewing. Almouallem Mhd Moamen, Khaled Raghad, Hamdar Hussein, and Nahle Ali Alakbar: Writing—original draft preparation, editing, and contributing to reviewing the literature. Mahmoud Jaber: Conceptualization, methodology, conceiving and supervising the study. All authors read and approved the final manuscript.
Availability of data and materials: The datasets generated and/or analyzed during the current study are not publicly available, but they are available from the corresponding author upon reasonable request.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from Ethical Committee at Damascus University’s Faculty of Medicine (ID: 14152) and complied with the principles of the Helsinki Declaration.
Trial registration: Not applicable.
ORCID iDs: Almasri Imad-Addin  https://orcid.org/0000-0002-4741-3721
https://orcid.org/0000-0002-4741-3721
Hamdar Hussein  https://orcid.org/0009-0002-5986-4383
https://orcid.org/0009-0002-5986-4383
References
- 1. Nuutinen M, Uhari M, Karvali T, et al. Consequences of caustic ingestions in children. Acta Paediatr 1994; 83(11): 1200–1205. [DOI] [PubMed] [Google Scholar]
- 2. Byrne WJ. Foreign bodies, bezoars, and caustic ingestion. Gastrointest Endosc Clin N Am 1994; 4(1): 99–119. [PubMed] [Google Scholar]
- 3. Wasserman RL, Ginsburg CM. Caustic substance injuries. J Pediatr 1985; 107(2): 169–174. [DOI] [PubMed] [Google Scholar]
- 4. Gaudreault P, Parent M, McGuigan MA, et al. Predictability of esophageal injury from signs and symptoms: a study of caustic ingestion in 378 children. Pediatrics 1983; 71(5): 767–770. [PubMed] [Google Scholar]
- 5. Moazam F, Talbert JL, Miller D, et al. Caustic ingestion and its sequelae in children. South Med J 1987; 80(2): 187–190. [DOI] [PubMed] [Google Scholar]
- 6. Hoffman RS, Burns MM, Gosselin S. Ingestion of caustic substances. N Engl J Med 2020; 382(18): 1739–1748. [DOI] [PubMed] [Google Scholar]
- 7. Pierre R, Neri S, Contreras M, et al. Guía de práctica clínica Ibero-Latinoamericana sobre la esofagitis cáustica en Pediatría: aspectos terapéuticos (2a. Parte). Rev Chil Pediatría 2020; 91(2): 289–299. [DOI] [PubMed] [Google Scholar]
- 8. Pierre R, Neri S, Contreras M, et al. Guía de práctica clínica Ibero-Latinoamericana sobre la esofagitis cáustica en Pediatría: fisiopatología y diagnóstico clínico-endoscópico (1a Parte). Rev Chil Pediatría 2020; 91(1): 149–157. [DOI] [PubMed] [Google Scholar]
- 9. Almanza-Miranda E, Blanco-Rodríguez G, Penchyna-Grub J, et al. Importance of early endoscopic and clinical evaluation of children with caustics ingestion. Bol Med Hosp Infant Mex 2021; 78(6): 544–548. [DOI] [PubMed] [Google Scholar]
- 10. Kurowski JA, Kay M. Caustic ingestions and foreign bodies ingestions in pediatric patients. Pediatr Clin North Am 2017; 64(3): 507–524. [DOI] [PubMed] [Google Scholar]
- 11. Oliva S, Romano C, De Angelis P, et al. Foreign body and caustic ingestions in children: a clinical practice guideline. Dig Liver Dis 2020; 52(11): 1266–1281. [DOI] [PubMed] [Google Scholar]
- 12. Pelclová D, Navrátil T. Do corticosteroids prevent oesophageal stricture after corrosive ingestion? Toxicol Rev 2005; 24(2): 125–129. [DOI] [PubMed] [Google Scholar]
- 13. Lamireau T, Llanas B, Deprez C, et al. [Severity of ingestion of caustic substance in children]. Arch Pediatr 1997; 4(6): 529–534. [DOI] [PubMed] [Google Scholar]
- 14. Kobayashi S, Tomokuni A, Gotoh K, et al. A retrospective analysis of the clinical effects of neoadjuvant combination therapy with full-dose gemcitabine and radiation therapy in patients with biliary tract cancer. Eur J Surg Oncol 2017; 43(4): 763–771. [DOI] [PubMed] [Google Scholar]
- 15. Cadranel S, Scaillon M, Goyens P, et al. Treatment of esophageal caustic injuries: experience with high-dose dexamethasone. Pediatr Surg Int 1993; 8(2): 97–102. [Google Scholar]
- 16. Usta M, Erkan T, Cokugras FC, et al. High doses of methylprednisolone in the management of caustic esophageal burns. Pediatrics 2014; 133(6): E1518–E1524. [DOI] [PubMed] [Google Scholar]
- 17. Katibe R, Abdelgadir I, McGrogan P, et al. Corticosteroids for preventing caustic esophageal strictures: systematic review and meta-analysis. J Pediatr Gastroenterol Nutr 2018; 66(6): 898–902. [DOI] [PubMed] [Google Scholar]
- 18. Howell JM, Dalsey WC, Hartsell FW, et al. Steroids for the treatment of corrosive esophageal injury: a statistical analysis of past studies. Am J Emerg Med 1992; 10(5): 421–425. [DOI] [PubMed] [Google Scholar]
- 19. Alser O, Hamouri S, Novotny NM. Esophageal caustic injuries in pediatrics: a sobering global health issue. Asian Cardiovasc Thorac Ann 2019; 27(6): 431–435. [DOI] [PubMed] [Google Scholar]
- 20. Contini S, Scarpignato C. Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol 2013; 19(25): 3918–3930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zargar SA, Kochhar R, Mehta S, et al. The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest Endosc 1991; 37(2): 165–169. [DOI] [PubMed] [Google Scholar]
- 22. Boukthir S, Fetni I, Mazigh Mrad S, et al. Corticothérapie à forte dose dans le traitement des oesophagites caustiques sévères chez l’enfant. Arch Pédiatr 2004; 11: 13–17. [DOI] [PubMed] [Google Scholar]
- 23. Boukthir S, Fetni I, Mrad SM, et al. [High doses of steroids in the management of caustic esophageal burns in children]. Arch Pediatr 2004; 11(1): 13–17. [DOI] [PubMed] [Google Scholar]
- 24. Povilavičius J, Samalavičius NE, Verkauskas G, et al. Conservative treatment of caustic oesophageal injuries in children: 15 years of experience in a tertiary care paediatric centre. Prz Gastroenterol 2019; 14(4): 286–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Darjazini Nahas L, Hmadieh M, Audeh M, et al. Cleft lip and palate risk factors among otorhinolaryngology: head and neck surgery patients in two hospitals. Medicine (Baltimore) 2023; 102(42): e34419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Anderson KD, Rouse TM, Randolph JG. A controlled trial of corticosteroids in children with corrosive injury of the esophagus. N Engl J Med 1990; 323(10): 637–640. [DOI] [PubMed] [Google Scholar]
- 27. Mamede RCM, De Mello Filho FV. Treatment of caustic ingestion: an analysis of 239 cases. Dis Esophagus 2002; 15(3): 210–213. [DOI] [PubMed] [Google Scholar]
- 28. Hawkins DB, Demeter MJ, Barnett TE. Caustic ingestion: controversies in management. A review of 214 cases. Laryngoscope 1980; 90(1): 98–109. [DOI] [PubMed] [Google Scholar]
- 29. Spain, David M., Norman Molomut, and Alvin Haber. The effect of cortisone on the formation of granulation tissue in mice. Am J Pathol 1950; 26(4): 710. [Google Scholar]
- 30. Mazigh Mrad S, Boukthir S, Sfaihi L, et al. [Therapeutic management and clinical course of severe caustic oesophageal burns in children treated with methyl-prednisolone. Experience at a digestive endoscopic unit]. Tunis Med 2004; 82(10): 951–957. [PubMed] [Google Scholar]
- 31. Thomson M, Tringali A, Dumonceau JM, et al. Paediatric gastrointestinal endoscopy: European Society for Paediatric Gastroenterology Hepatology and Nutrition and European Society of Gastrointestinal Endoscopy Guidelines. J Pediatr Gastroenterol Nutr 2017; 64(1): 133–153. [DOI] [PubMed] [Google Scholar]
- 32. Bautista Casasnovas A, Estevez Martinez E, Varela Cives R, et al. A retrospective analysis of ingestion of caustic substances by children. Ten-year statistics in Galicia. Eur J Pediatr 1997; 156(5): 410–414. [DOI] [PubMed] [Google Scholar]
- 33. Rafeey M, Ghojazadeh M, Sheikhi S, et al. Caustic ingestion in children: a systematic review and meta-analysis. J Caring Sci 2016; 5(3): 251–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Friedman EM. Caustic ingestions and foreign bodies in the aerodigestive tract of children. Pediatr Clin North Am 1989; 36(6): 1403–1410. [DOI] [PubMed] [Google Scholar]
- 35. Peden M, Oyegbite K, Ozanne-Smith J, et al. World report on child injury prevention. Geneva: World Health Organization, http://www.ncbi.nlm.nih.gov/books/NBK310641/ (2008, accessed 15 November 2023). [PubMed] [Google Scholar]