Abstract
Introduction and importance
Spontaneous iliac artery dissection (IAD) is a rare condition that is usually associated with connective tissue diseases. Complications include ischemia due to malperfusion and bleeding due to rupture. Treatments vary depending on the expertise and presenting symptoms; they include conservative, endovascular, and surgical options.
Presentation of case
Here, we present the case of a 45-year-old man who presented with right lower quadrant pain and hypertension as well as normal laboratory results. A contrast-enhanced computed tomography (CT) scan of the abdomen revealed an isolated dissection of the right external iliac artery. The patient had intact distal pulses and no other abnormal findings. He was admitted to the intensive care unit to control his high blood pressure with antihypertensive medications. The patient recovered well and was discharged home in stable condition with antiplatelet and antihypertensive therapy. The follow-up with the patient continued for one year.
Discussion
Given the rarity of this disease, the treatment protocols and outcomes are still a matter of ongoing debate. Complicated cases with rupture should be treated on an emergency basis using open and endovascular repairs. In asymptomatic and symptomatic patients without rupture, medical treatment and possibly endovascular treatments are considered.
Conclusion
Conservative management of uncomplicated asymptomatic IAD should be considered as first-line therapy.
Keywords: Dissection, Iliac artery, Conservative treatment, Endovascular intervention, Case report
Highlights
-
•
Peripheral artery dissection arises most frequently in conjunction with aortic dissection.
-
•
Spontaneous peripheral arterial dissection that occurs without aortic dissection has rarely been reported.
-
•
Treatment protocols and outcomes are not clear, given the rarity of the disease.
-
•
Conservative management of uncomplicated asymptomatic IAD should be considered as first-line therapy.
-
•
Complicated cases with rupture should be treated on an emergency basis using open and endovascular repairs.
1. Introduction
Although peripheral artery dissection arises most frequently in conjunction with aortic dissection, spontaneous peripheral arterial dissection that occurs without aortic dissection has rarely been reported [1]. Spontaneous isolated iliac artery dissection (IAD) is a rare vascular-pathological condition that causes arterial dissection in the common iliac artery [2]. Only a few cases have been reported in the literature. Although this rare vascular-pathological condition may occasionally be asymptomatic, arterial dissection can have catastrophic consequences, and it might be fatal [2].
Despite the precise underlying causes of IAD remain elusive, previous studies suggested a variety of etiologies, including hypertension, pregnancy, traumatic injuries, iliac artery catheterization, atherosclerosis, fibromuscular dysplasia, and connective tissue disorders like Marfan syndrome, Ehlers-Danlos syndrome, Erdheim-Gsell, and cystic medial degeneration [2,3].
Clinically, IAD can imitate arterial limb ischemia and present with symptoms such as sudden-acute onset pain, pulselessness, paleness, paresthesia, and poikilothermia, according to reported cases in the literature [3]. Nevertheless, IAD can remain asymptomatic and undiagnosed for years, and go undiagnosed for years, only to be incidentally discovered during diagnostic testing for other concurrent conditions. [2,3]
Here, we report a case of asymptomatic isolated right external IAD found incidentally during a work-up for abdominal pain and managed conservatively. This case report has been described in line with the SCARE criteria [4].
2. Presentation of case
A 45-year-old man is known to have type 2 diabetes mellitus and colonic diverticular disease. He presented to the emergency department of Dr. Sulaiman Al Habib Hospital, Riyadh, Saudi Arabia with a complaint of chronic right lower quadrant pain for the past three months. The pain was intermittent, did not increase with meals, and was not radiating. The patient denied any history of weight loss, fatigue, anorexia, jaundice, and diarrhea or vomiting. Additionally, the patient denied any vigorous exercise and has no history of smoking or alcohol intake. He had a long history of constipation for 10 years on intermittent laxative medications. The past personal history or family history was unremarkable. Upon general physical examination, the patient was well-nourished, in moderate pain, and had no pallor or jaundice. His blood pressure was 210/110 mmHg, and he was not taking antihypertensive drugs. Abdominal examination revealed minimal tenderness in the right lower quadrant area with no palpable masses. The lower limb examination was unremarkable, with palpable pulses and no sensory or motor neurological deficit. Laboratory value were all within the normal range (Table 1).
Table 1.
Laboratory values.
| Examination | Value |
|---|---|
| Blood count | |
| Hemoglobin | 12.8 g/dL |
| Leucocyte count | 8.10 × 109/L |
| Hematocrit | 34.5 % |
| Platelet count | 323 × 109/L |
| Liver function test | |
| Albumin | 39 g/L |
| Total bilirubin | 13 μmol/L |
| Direct bilirubin | 5.3 μmol/L |
| AST | 13 IU/L |
| ALT | 9 IU/L |
| Alkaline phosphatase | 90 IU/L |
| GGT | 17 IU/L |
| Coagulation profile | |
| PT | 12.2 s |
| PTT | 26 s |
| INR | 1.09 |
| Renal function tests | |
| Creatinine | 89.1 mmol/L |
| Urea | 7 mmol/L |
Abbreviations: AST, Aspartate Aminotransferase; ALT, Alanine Aminotransferase; GGT, Gamma-Glutamyl Transferase; PT, Prothrombin Time; PTT, Partial Thromboplastin Time; INR, International Normalized Ratio.
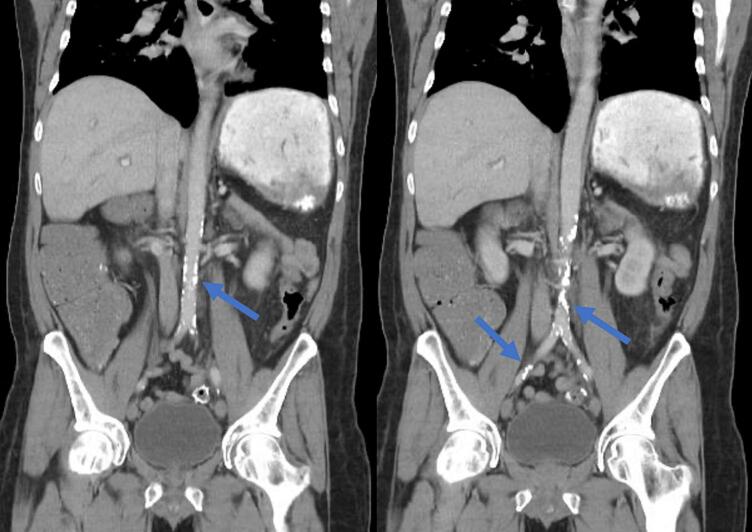
Despite the absence of alarming symptoms such as weight loss, fatigue, anorexia, or jaundice, the chronicity and persistence of the right quadrant pain in addition to the patient's diverticular disease warranted further investigation to rule out underlying pathology. Therefore, a contrast-enhanced computed tomography (CT) scan of the abdomen was ordered to thoroughly evaluate the underlying cause of the chronic pain, assess for possible complications related to known comorbidities, and exclude other differential diagnoses. The imaging showed an incidental finding of a right external iliac artery dissection. The proximal entry tear was in the mid-external iliac artery and extended for 1.8 cm. The distal exit tear was present, and there was no flow limitation, dilatation, or aneurysmal changes (Fig. 1). The abdominal aorta and common iliac arteries were mildly calcified without dissection (Fig. 2). The past personal history did not reveal conditions such as connective tissue disorders, vascular diseases, hypertension, intermittent claudication, arrhythmia, cardiac disease, trauma, intervention, or drug therapy. The past surgical and family histories were unremarkable. The patient's collagen connective tissue work-up was unremarkable. The ankle-brachial index was found to be 1.1 on the right and 1.2 on the left. Since the patient is asymptomatic and the pain was related to his chronic colonic diverticular disease. Additionally, there was no clinical history or signs of claudication or limb ischemia.
Fig. 1.

A contrast-enhanced computed tomography (CT) scan of the abdomen showed an incidental finding of a right external iliac artery dissection (blue arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 2.
Coronal view of CT scan of the abdomen revealed a mildly calcified abdominal aorta and common iliac arteries without dissection (blue arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Based on history, and clinical findings, conservative treatment was chosen. The patient was admitted to the intensive care unit for observation and blood pressure control. A left radial arterial line and a right internal jugular central venous catheter were inserted for continuous monitoring. Vital signs and peripheral pulses were checked hourly, and meticulous measurement of input and output was maintained. The patient was kept fasting with intravenous hydration. Intravenous labetalol 1 mg/mL solution with an infusion rate of 20 mg/h was started. The rate was increased to 40 mg/h, and the blood pressure was stabilized. The following day, the blood pressure treatment transitioned to oral beta blockers, and he started a progressive oral diet. After controlling his blood pressure, he was discharged home in good condition with antiplatelet therapy (acetylsalicylic acid, 81 mg orally daily) and antihypertensive therapy (atenolol, 100 mg orally daily). The patient was followed up in the outpatient department. He remained stable throughout a one-year follow-up period, and the CT examination revealed no changes (Fig. 3).
Fig. 3.
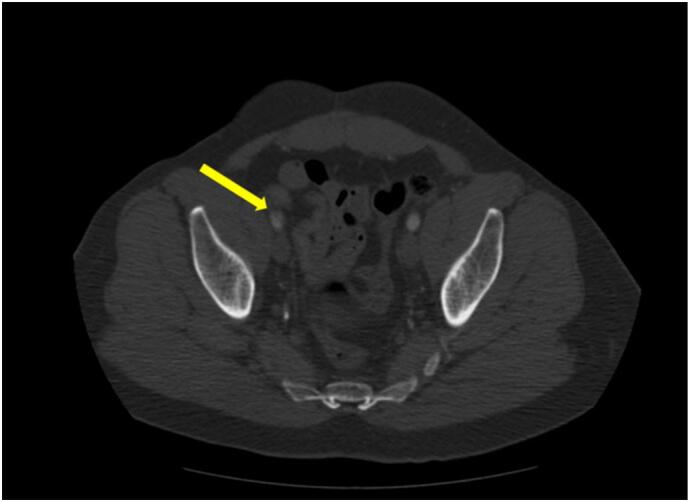
One-year follow-up CT scan showing the right external iliac artery dissection (yellow arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3. Discussion
Peripheral artery dissection arises most frequently in conjunction with aortic dissection; however, spontaneous peripheral arterial dissection that occurs without aortic dissection has rarely been reported [1]. The pathophysiology of these lesions is complex, and dissection may occur as a result of uncontrolled hypertension. Notably, the risk of aortic dissection is significant at systolic blood pressure of more than 132 mmHg and diastolic blood pressure of more than 75 mmHg [5]. High blood pressure can initiate the intimal injury that eventually results in the dissection.
In the presented case, the patient had diabetes mellitus, a recognized risk factor for cardiovascular diseases and peripheral arterial disease. The exact mechanism linking diabetes to arterial dissection is uncertain, but the vascular changes in diabetes, such as endothelial dysfunction and oxidative stress, may compromise arterial wall integrity, rendering it more vulnerable to dissection [6]. Therefore, it is important for clinicians to recognize this disease as a potential predisposing factor for arterial dissection.
The optimal approach to treating isolated IAD remains a subject of debate. The urgency of intervention is dictated by the patient's clinical presentation; those presenting with acute limb ischemia or rupture require immediate endovascular or open repair [7]. Conversely, conservative management is typically reserved for asymptomatic individuals. However, due to the rarity of the condition, there are currently no established management guidelines for asymptomatic IAD patients. According to a study by Liang et al. [2], asymptomatic patients can safely undergo conservative treatment without experiencing complications. Nevertheless, there is still a lack of consensus on follow-up recommendations for non-surgical patients. These patients are at increased risk of arterial aneurysm development due to the nature of the disease. Therefore, administering β blockers and conducting annual clinical evaluations, along with screening using ultrasonography or CT scan to monitor for potential arterial aneurysm formation is recommended. We have chosen this approach with close clinical, instrumental, and laboratory monitoring. Clinical attention has been focused on hemodynamic stability given the asymptomatic nature of the patient's disease.
Open surgery is currently the most common treatment for these conditions, especially in the presence of rupture. Considering that most investigators use percutaneous transluminal angioplasty with endovascular stents [[8], [9], [10]], there are some cases of IAD treated with balloon angioplasty alone [11]. Endovascular intervention can be considered if there are symptoms (mostly pain) without signs of rupture [[8], [9], [10]].
The endovascular intervention for IAD aims to keep the distal and hypogastric arteries perfused while excluding and achieving thrombosis in the false lumen by sealing the proximal entry tear. Kwak et al. [12] discussed the benefits of endovascular treatment for IAD. The authors described two cases of iliac axis dissections that were successfully treated with the implantation of self-expanding stents, and post-intervention follow-up showed good results [12]. Additionally, Yoshida et al. [13] reported a total endovascular treatment of common IAD using two covered stents to maintain pelvic circulation. The authors placed two covered stents in the common and external iliac arteries. The hypogastric artery's origin was not covered, and the results of the post-intervention follow-up showed good results.
During endovascular intervention for IAD, at least one hypogastric artery needs to be preserved to avoid ischemic complications [14]. Maintaining the patency of the hypogastric artery in young patients, especially those with idiopathic IAD, is preferable as the contralateral iliac artery may become affected by other vascular conditions (stenosis, aneurysms) with the aging process. Whereas it is not recommended to use endovascular devices in IAD caused by collagen disease [15].
In our case, conservative management was chosen based on the patient's clinical presentation, imaging findings, and stable hemodynamics achieved through prompt pharmacological therapy. Despite potential risks, the patient remained asymptomatic during follow-up with no adverse outcomes on imaging. Favorable responses to conservative measures, such as blood pressure control, support the decision to avoid invasive intervention. This case highlights the importance of individualized treatment approaches in managing rare vascular-pathological conditions like isolated IAD, where conservative management may offer a safe and effective alternative to invasive procedures, particularly in asymptomatic patients without evidence of disease progression.
4. Conclusion
Spontaneous isolated dissection of the iliac artery is a rare vascular-pathological condition. The treatment options should be individualized based on the patient clinical presentation. We advocate that medical therapy alone should be the first line of treatment for uncomplicated asymptomatic dissection. Nevertheless, careful monitoring can help detect forms that tend towards morphological changes, increasing the risk of rupture.
Patient perspective and informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Ethical approval was obtained from the Research Center of the Dr. Sulaiman Al Habib Hospital, Riyadh, Saudi Arabia. Reference number (RC23.12.01) Dated 18/12/2023.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
MYD: Substantial contributions to the design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published.
TA: Substantial contributions to the design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published.
HA: Substantial contributions to the design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published.
SA: Substantial contributions to the design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published.
Guarantor
Mohammed Aldossary.
Research registration number
Not required.
Conflict of interest statement
All authors declare that there is no conflict of interest.
Acknowledgment
Not available.
Data availability
The data for this study will be available from the corresponding author upon reasonable request.
References
- 1.Guthrie W., Maclean H. Dissecting aneurysms of arteries other than the aorta. J. Pathol. 1972;108:219–235. doi: 10.1002/path.1711080308. [DOI] [PubMed] [Google Scholar]
- 2.Liang Z., Guo W., Du C., Xie Y. Effectiveness of the conservative therapy for spontaneous isolated iliac artery dissection: preliminary results. Vascular. 2017;25(6):649–656. doi: 10.1177/1708538117710845. [DOI] [PubMed] [Google Scholar]
- 3.Novotny R., Chlupac J., Beran J., Janousek L., Fronek J. Spontaneous isolated common iliac artery dissection treated with self-expandable stent in a 38-year-old patient: a case report. EJVES Short Rep. 2018;42:4–6. doi: 10.1016/j.ejvssr.2018.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hibino M., Otaki Y., Kobeissi E., Pan H., Hibino H., Taddese H., et al. Blood pressure, hypertension, and the risk of aortic dissection incidence and mortality: results from the J-SCH study, the UK biobank study, and a Meta-analysis of cohort studies. Circulation. 2022;145(9):633–644. doi: 10.1161/CIRCULATIONAHA.121.056546. [DOI] [PubMed] [Google Scholar]
- 6.Fadini G.P., Albiero M., Bonora B.M., Avogaro A. Angiogenic abnormalities in diabetes mellitus: mechanistic and clinical aspects. J. Clin. Endocrinol. Metab. 2019;104(11):5431–5444. doi: 10.1210/jc.2019-00980. [DOI] [PubMed] [Google Scholar]
- 7.Dueppers P., Jankowiak S., Schelzig H., Wagenhäuser M.U., Oberhuber A. Spontaneous rupture of an isolated iliac artery dissection in a young man because of cystic medial degeneration Erdheim-Gsell. Ann. Vasc. Surg. 2015;29(596):e11–e13. doi: 10.1016/j.avsg.2014.10.041. [DOI] [PubMed] [Google Scholar]
- 8.Cook P.S., Erdoes L.S., Selzer P.M., Rivera F.J., Palmaz J.C. Dissection of the external iliac artery in highly trained athletes. J. Vasc. Surg. 1995;22(2):173–177. doi: 10.1016/s0741-5214(95)70113-3. [DOI] [PubMed] [Google Scholar]
- 9.Thevenet A., Latil J.L., Albat B. Fibromuscular disease of the external iliac artery. Ann. Vasc. Surg. 1992;6(3):199–204. doi: 10.1007/BF02000263. [DOI] [PubMed] [Google Scholar]
- 10.Engin C., Calkavur T., Apaydin A.Z., Durmaz I. Bilateral spontaneous and isolated dissection of the external iliac arteries: report of a case. EJVES Extra. 2005;9(2):19–21. doi: 10.1016/j.ejvsextra.2005.01.005. [DOI] [Google Scholar]
- 11.Murphy T.P., Dorfman G.S., Segall M., Carney W.I., Jr. Iatrogenic arterial dissection: treatment by percutaneous transluminal angioplasty. Cardiovasc. Intervent. Radiol. 1991;14(5):302–306. doi: 10.1007/BF02578455. [DOI] [PubMed] [Google Scholar]
- 12.Kwak H.S., Han Y.M., Chung G.H., Yu H.C., Jeong Y.J. Isolated spontaneous dissection of the common iliac artery: percutaneous stent placement in two patients. Cardiovasc. Intervent. Radiol. 2006;29(5):883–885. doi: 10.1007/s00270-005-0087-z. [DOI] [PubMed] [Google Scholar]
- 13.Yoshida Rde A., Kolvenbach R., Vieira P.R., Moura R., Jaldin R.G., Yoshida W.B. Endovascular treatment of spontaneous isolated common and external iliac artery dissections with preservation of pelvic blood flow. Ann. Vasc. Surg. 2015;29(1) doi: 10.1016/j.avsg.2014.08.013. (126.e9-14) [DOI] [PubMed] [Google Scholar]
- 14.Lin P.H., Chen A.Y., Vij A. Hypogastric artery preservation during endovascular aortic aneurysm repair: is it important? Semin. Vasc. Surg. 2009;22(3):193–200. doi: 10.1053/j.semvascsurg.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 15.Akin I., Kische S., Rehders T.C., Chatterjee T., Schneider H., Körber T., Nienaber C.A., Ince H. Current role of endovascular therapy in Marfan patients with previous aortic surgery. Vasc. Health Risk Manag. 2008;4(1):59–66. doi: 10.2147/vhrm.2008.04.01.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data for this study will be available from the corresponding author upon reasonable request.