Abstract
Background
Women with chronic coronary disease are generally older than men and have more comorbidities but less atherosclerosis. We explored sex differences in revascularization, guideline‐directed medical therapy, and outcomes among patients with chronic coronary disease with ischemia on stress testing, with and without invasive management.
Methods and Results
The ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) trial randomized patients with moderate or severe ischemia to invasive management with angiography, revascularization, and guideline‐directed medical therapy, or initial conservative management with guideline‐directed medical therapy alone. We evaluated the primary outcome (cardiovascular death, myocardial infarction, or hospitalization for unstable angina, heart failure, or resuscitated cardiac arrest) and other end points, by sex, in 1168 (22.6%) women and 4011 (77.4%) men. Invasive group catheterization rates were similar, with less revascularization among women (73.4% of invasive‐assigned women revascularized versus 81.2% of invasive‐assigned men; P<0.001). Women had less coronary artery disease: multivessel in 60.0% of invasive‐assigned women and 74.8% of invasive‐assigned men, and no ≥50% stenosis in 12.3% versus 4.5% (P<0.001). In the conservative group, 4‐year catheterization rates were 26.3% of women versus 25.6% of men (P=0.72). Guideline‐directed medical therapy use was lower among women with fewer risk factor goals attained. There were no sex differences in the primary outcome (adjusted hazard ratio [HR] for women versus men, 0.93 [95% CI, 0.77–1.13]; P=0.47) or the major secondary outcome of cardiovascular death/myocardial infarction (adjusted HR, 0.93 [95% CI, 0.76–1.14]; P=0.49), with no significant sex‐by‐treatment‐group interactions.
Conclusions
Women had less extensive coronary artery disease and, therefore, lower revascularization rates in the invasive group. Despite lower risk factor goal attainment, women with chronic coronary disease experienced similar risk‐adjusted outcomes to men in the ISCHEMIA trial.
Registration
URL: http://wwwclinicaltrials.gov. Unique identifier: NCT01471522.
Keywords: coronary artery disease, ischemic heart disease, sex differences, women's health
Subject Categories: Ischemia, Clinical Studies
Nonstandard Abbreviations and Acronyms
- CCD
chronic coronary disease
- GDMT
guideline‐directed medical therapy
Clinical Perspective.
What Is New?
Cardiac catheterization rates were similar by sex in both the routine invasive management strategy group and the conservative management strategy group, but women had lower likelihood of obstructive coronary artery disease at angiography, and therefore underwent revascularization less often than men in both groups, despite a requirement for moderate or severe ischemia on stress testing.
Use of guideline‐directed medical therapy was lower among women than men in the trial, with fewer treatment goals achieved, despite protocolized trial guidance on medical therapy.
Rates of the primary and secondary clinical outcomes were not different by sex.
What Are the Clinical Implications?
The similar clinical outcomes for men and women randomized in the ISCHEMIA (International Study of Comparative Health Effectiveness with Medical Invasive Approaches) trial represent the net effects of sex differences that reflect opposing risks: women were older than men and had higher rates of hypertension and diabetes with poorer risk factor control throughout follow‐up, but had less extensive anatomic coronary artery disease and ischemia on imaging.
Additional efforts are needed to achieve equity in risk factor control for women and men with chronic coronary disease.
In patients with chronic coronary disease (CCD), the prevalence of obstructive coronary artery disease (CAD) is lower in women than in men, whereas, conversely, there is a higher prevalence of ischemia with no obstructive coronary arteries in women. 1 , 2 Women, in general, often present at older ages and with more clinical comorbidities than men. 3 , 4 However, unlike patients presenting with acute coronary syndromes, women with CCD have not been shown to be at higher risk of adverse cardiovascular outcomes compared with men in previously published clinical trials and registries. 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12
Unique among studies of patients with CCD, the ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) trial randomized participants before cardiac catheterization to an initial invasive or conservative management strategy. Site‐assessed moderate or severe ischemia at baseline was a prerequisite for trial inclusion, resulting in a high prevalence of severe multivessel CAD. 13 Enrolled participants with adequate renal function had prerandomization coronary computed tomography angiography (CCTA) to confirm the presence of at least 50% stenosis in a coronary artery and to exclude patients with significant left main CAD. Consequently, this process excluded more women than men because of the higher prevalence of ischemia with no obstructive coronary arteries, and even among those randomized, women had less severe and extensive anatomic CAD than men. 14 Prior studies have demonstrated that, compared with men, women with CCD have lower rates of revascularization, particularly surgical revascularization, and may have poorer outcomes after revascularization. 15 , 16 , 17 , 18 However, the extent to which lower rates of revascularization among women may relate to sex differences in severity of ischemia remains unknown. Lower use of guideline‐directed medical therapy (GDMT) among women may also affect outcomes. 19 , 20 GDMT recommendations are identical for patients with CCD of both sexes, yet gaps in care remain. The extent to which protocolized guidance within a clinical trial structure may narrow these gaps requires further investigation.
Women had more severe angina at randomization in the ISCHEMIA trial, independent of other clinical variables. 14 This greater angina burden is consistent with observational studies and has the potential to influence the likelihood of symptom‐driven cardiac catheterization and revascularization during follow‐up. 21 , 22 Women with acute coronary syndrome exhibit lower troponin values than men, and sex‐specific high‐sensitivity troponin assays improve the diagnosis of myocardial infarction (MI); thus, sex has the potential to influence reporting and adjudication of acute coronary syndrome events occurring during clinical trial follow‐up. 23 , 24 Thus, the aim of this analysis was to compare outcomes and medical therapy use between women and men with CCD randomized in the ISCHEMIA trial to help inform the future management of women with CCD.
METHODS
Deidentified ISCHEMIA trial data will be shared with researchers through the National Heart, Lung, and Blood Institute BioLINCC repository (https://biolincc.nhlbi.nih.gov/). The ISCHEMIA trial design has been published. 25 In brief, patients with site‐assessed moderate or severe ischemia based on stress testing were randomized to an initial invasive management strategy or an initial conservative management strategy. CCTA was performed before randomization to ensure that randomized participants had significant epicardial coronary stenosis but not left main disease but was not required if the estimated glomerular filtration rate was <60 mL/min per 1.73 m2 or the coronary anatomy was known to meet entry criteria based on recent imaging. Major exclusion criteria were acute coronary syndrome within 2 months before randomization, left ventricular ejection fraction <35%, unacceptable angina severity despite maximal medical therapy, estimated glomerular filtration rate <30 mL/min per 1.73 m2, heart failure hospitalization within the past 6 months, and New York Heart Association class III to IV heart failure. The study was approved by the NYU School of Medicine Institutional Review Board and by the review board of each participating site. All patients provided informed consent to participate in the ISCHEMIA trial.
All participants were to receive GDMT, and sites were provided algorithms to guide pharmacologic treatment to targets of low‐density lipoprotein cholesterol (LDL‐C) <70 mg/dL and systolic blood pressure (SBP) <140 mm Hg. The SBP goal was later lowered to <130 mm Hg, but we used the original goal in this analysis. Participants with diabetes were to be treated to a goal hemoglobin A1c of <8%, but this was not considered a primary goal, and a treatment algorithm was not provided. Lifestyle interventions were applied in a protocolized manner toward goals of lower saturated fat in the diet, increased activity level, normal body mass index, and nonsmoking. Medication‐taking behavior was assessed by self‐report at the time of randomization, using a modified 4‐item Morisky‐Green‐Levine Adherence Scale, allowing participants to be classified as adherent or nonadherent.
Participants randomized to the invasive strategy were to undergo cardiac catheterization with revascularization of all ischemic territories based on stress test results, diagnostic angiography, or measurement of fractional flow reserve. An algorithm was used to guide complete revascularization, and a Heart Team approach was used by sites to determine suitability of patients with complex anatomy for percutaneous coronary intervention or coronary artery bypass grafting as the method of revascularization.
An angiographic core laboratory reviewed coronary angiograms from patients enrolled in the invasive group to determine the severity of stenosis, extent of disease, and completeness of revascularization. Extent and severity of CAD were quantified using the Duke Jeopardy Score and the Synergy between Percutaneous Coronary Intervention with TAXus and Cardiac Surgery score, as well as the number of vessels with ≥50% or ≥70% stenosis. 26 , 27
The primary end point was a composite of cardiovascular death, nonfatal MI, or hospitalization for unstable angina, heart failure, or resuscitated cardiac arrest. The major secondary clinical outcome was the composite of cardiovascular death or nonfatal MI. Additional secondary outcomes were each component of the primary outcome, all‐cause mortality, and stroke. Clinical outcomes were reported by sites or identified in the electronic data capture system and were adjudicated by an independent clinical events committee blinded to treatment strategy allocation. Health status outcomes represented a major secondary outcome and will be reported in relation to sex separately. The use of, and reasons for, cardiac catheterization and revascularization were collected in both treatment strategy groups during follow‐up. MI was defined according to trial criteria and was categorized according to type. 25 , 28 Procedural MI was defined as type 4a or 5. To increase ascertainment of MI and unstable angina, sites were required to report all emergency department visits and hospitalizations and to report whether cardiac markers were collected, the values, and the discharge diagnoses associated with these visits. All end point events were adjudicated by an independent clinical events classification committee whose members were blinded to the study treatment assignment.
Statistical Analysis
Outcomes were assessed according to biological sex, which was known for all randomized participants and assessed by self‐report. We did not collect sex. For simplicity of language in this report, we refer to females as women and males as men. Baseline characteristics are presented separately for women and men within each treatment group. Categorical variables are presented as counts (percentages), and differences between women and men were assessed using the χ 2 test or Fisher exact test, as appropriate. Continuous variables are presented as the number of nonmissing values and median (quartile 1–quartile 3), and differences between women and men were compared using the Wilcoxon rank‐sum test or Student t‐test, as appropriate. Imputation was not performed for descriptive tables; missing data are excluded from all denominators. The α level was set at 0.05.
To distinguish the timing of clinical events, cumulative event rates and 95% CIs are estimated as a function of follow‐up time in women and men with use of the Kaplan‐Meier method 29 for events that are not subject to competing risks (eg, all‐cause mortality) and by a nonparametric cumulative incidence function estimator 30 for events that are subject to competing risks (eg, cardiovascular death or MI, where death from noncardiovascular causes is treated as a competing event). The cumulative incidence function estimators for competing risks data are identical to the Kaplan‐Meier estimate when applied to end points that are not subject to competing risks. The associated P values from the Gray test 31 or log‐rank test are also presented. To characterize the association of sex on clinical outcomes, the number of confirmed first events and hazard ratios (HRs; comparing women versus men), 95% CIs, and P values from unadjusted and adjusted Cox regression models are reported. As was specified in the ISCHEMIA main trial final analysis, adjustment covariates include age at randomization, estimated glomerular filtration rate, ejection fraction, diabetes, and randomized treatment strategy group. 32 Each “adjusted” model also assessed sex‐by‐age, sex‐by‐treatment, sex‐by‐degree of ischemia, and sex‐by‐diabetes interactions. To maximize the amount of information each covariate provides to the covariate‐adjusted analysis, multiple imputation, using the same approach as was used in the main trial, was used to impute missing covariate data (Data S1). 28 To account for nonlinear relationships, continuous variables were modeled as restricted cubic splines with knots at the 10th, 50th, and 90th percentiles of each variable's empirical distribution. Unadjusted cumulative incidence function estimates (accounting for the competing risk of death) of catheterization or revascularization were summarized over several time points by sex. Estimates were computed separately for participants randomized to the 2 treatment strategy groups. Descriptive statistics on the use of catheterization and revascularization in both treatment groups were summarized and compared by sex using the same previously stated methods.
The distribution of total emergency department admissions was tabulated among women and men and compared using a t‐test or Wilcoxon rank‐sum test, as appropriate. For medical therapy analysis, the proportion of participants meeting each goal at the end of the study was summarized, with end of study defined as the latest visit (at least 12 months after randomization) at which the goal was evaluable. If the latest visit where the goal is evaluable was <12 months after randomization, then the individual goal was considered to be missing. Note that the SBP goal of <140 mm Hg was used here, although by the end of the trial, sites were asked to use an SBP treatment goal of <130 mm Hg.
RESULTS
Patient Population
A total of 1168 (22.6%) women and 4011 (77.4%) men were randomized. As previously reported, hypertension and diabetes were more common among women, and women were slightly older than men. 14 Women were less likely to smoke and to have history of MI or prior coronary revascularization. Women were more likely to have been enrolled after stress imaging rather than exercise tolerance testing than men, and women had less severe ischemia on imaging than men. Fewer women underwent CCTA than men (67.4% versus 70.0%; P=0.02). 14 Randomized women also had less extensive and severe anatomic CAD on study CCTA than randomized men, and women had overall lower degrees of ischemia, and slightly higher left ventricular ejection fraction. 14 Baseline characteristics were well balanced between treatment strategy arms within each sex (Table S1).
Protocol‐Assigned Invasive Procedures by Sex
Although there was no difference in the proportion of women and men randomized to the invasive strategy who underwent cardiac catheterization or in the timing of catheterization after randomization, women were less likely to undergo revascularization (73.4% of invasive‐assigned women received revascularization versus 81.2% of invasive‐assigned men; P<0.001) (Table 1; Figure 1A). Women had less severe CAD at invasive angiography than men, with more nonobstructive disease (12.3% versus 4.5% with no stenosis ≥50%; P<0.001) and less 3‐vessel CAD (29.8% versus 42.7%; P<0.001) (Table 2). Within the subgroup of invasive‐assigned patients who underwent CCTA, women still had higher likelihood of nonobstructive CAD on invasive angiography (10.2% versus 3.9%; P<0.001). Consistent with this, the most common reason that revascularization was not performed was the absence of obstructive CAD, which was the reason in 71.7% of women not revascularized versus 53.3% of men. The likelihood of revascularization did not differ by sex in analysis stratified by the number of diseased vessels at coronary angiography (Table 2). In the invasive strategy group, the first revascularization was more likely to be percutaneous coronary intervention in women compared with men (79.1% versus 72.8%; P=0.008). Within the subset of patients with 3‐ or 2‐vessel CAD, including severe proximal left anterior descending artery stenosis on CCTA (Duke score 6), there was no difference in the rate of revascularization (percutaneous coronary intervention or coronary artery bypass grafting; 80.5% in women versus 81.9% in men; P=0.825). In the same Duke score 6 subgroup, among those who did undergo revascularization, there was no difference in the rate of coronary artery bypass grafting by sex (10 of 33 women [30.3%] versus 103 of 249 men [41.4%]; P=0.223; Table S2).
Table 1.
Use of Catheterization and Revascularization in Participants Randomized to the Invasive Strategy Group by Sex
| Characteristic | Women (N=606) | Men (N=1982) | P value |
|---|---|---|---|
| Participants with at least 1 catheterization during follow‐up | 570/606 (94.1) | 1859/1982 (93.8) | 0.81 |
| Time from randomization to first catheterization, d | 18 (9–31) | 20 (10–31) | 0.28 |
| Fractional flow reserve testing used | 119/568 (21.0) | 400/1854 (21.6) | 0.75 |
| Participants with at least 1 revascularization during follow‐up | 445/606 (73.4) | 1609/1982 (81.2) | <0.001 |
| Time from randomization to first revascularization, d | 24 (11–45) | 27 (14–52) | 0.02 |
| First revascularization was PCI | 352/445 (79.1) | 1172/1609 (72.8) | 0.008 |
| Time from randomization to first PCI, d | 22 (9–41) | 22 (12–41) | 0.24 |
| Drug‐eluting stent placed | 319/352 (90.6) | 1069/1171 (91.3) | 0.70 |
| First revascularization was CABG | 93/445 (20.9) | 437/1609 (27.2) | 0.008 |
| Time from randomization to first CABG, d | 37 (22–76) | 45 (25–89) | 0.50 |
| IMA graft placed during CABG | 84/93 (90.3) | 402/436 (92.2) | 0.55 |
| Participants with at least 1 catheterization or revascularization during follow‐up | 582/606 (96.0) | 1893/1982 (95.5) | 0.58 |
| Catheterization or revascularization performed within 90 d of randomization | 561/606 (92.6) | 1822/1982 (91.9) | 0.61 |
| With 1‐vessel CAD | 86/96 (89.6%) | 242/264 (91.7%) | 5.54 |
| With 2‐vessel CAD | 88/93 (94.6%) | 316/341 (92.7%) | 0.51 |
| With 3 ‐vessel CAD | 96/102 (94.1%) | 546/592 (92.2%) | 0.50 |
| Site‐reported reason for no catheterization performed by 6‐wk visit | 0.49 | ||
| Patient preference | 27/45 (60.0) | 91/160 (56.9) | |
| Physician preference | 2/45 (4.4) | 5/160 (3.1) | |
| Intercurrent illness | 4/45 (8.9) | 10/160 (6.3) | |
| Participant died | 1/45 (2.2) | 0/160 (0.0) | |
| Other | 6/45 (13.3) | 29/160 (18.1) | |
| Missing or unknown | 5/45 (11.1) | 22/160 (13.8) | |
| Intended management strategy after first diagnostic catheterization in participants with a catheterization | 137 | 284 | |
| Medical therapy only | 127/137 (92.7) | 244/284 (85.9) | 0.02 |
| Reason for medical therapy | 0.002 | ||
| No obstructive CAD | 91/127 (71.7) | 130/244 (53.3) | |
| Anatomy not suitable for any mode of revascularization | 23/127 (18.1) | 88/244 (36.1) | |
| Patient preference | 8/127 (6.3) | 20/244 (8.2) | |
| Other | 5/127 (3.9) | 6/244 (2.5) | |
| PCI/CABG/hybrid | 9/137 (6.6) | 40/284 (14.1) | |
| Undecided | 0/137 (0.0) | 0/284 (0.0) | |
| Unknown | 1/137 (0.7) | 0/284 (0.0) | |
| Missing | 0/137 (0.0) | 0/284 (0.0) |
Data are given as number/total (percentage) or median (quartile 1–quartile 3). CABG indicates coronary artery bypass grafting; CAD, coronary artery disease; IMA, internal mammary artery; and PCI, percutaneous coronary intervention.
Figure 1. Unadjusted cumulative incidence plot of revascularization by sex, excluding revascularization for a suspected primary end point event.
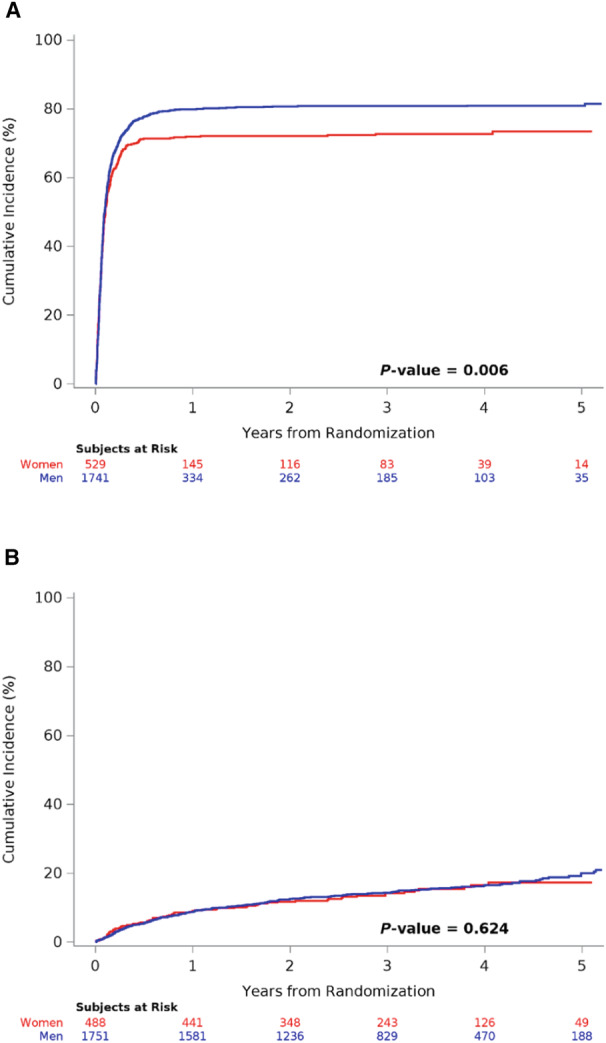
A, Invasive strategy. B, Conservative strategy. Note that revascularization prompted by a suspected end point event is not included.
Table 2.
Invasive Angiographic Findings in Participants Randomized to the Invasive Strategy Group by Sex
| Characteristic | Women (N=578) | Men (N=1895) | P value |
|---|---|---|---|
| Any obstructive disease ≥50% stenosis | |||
| Overall | 504/573 (88.0) | 1795/1877 (95.6) | <0.001 |
| After CCTA performed | 362/403 (89.8) | 1425/1483 (96.1) | <0.001 |
| No. of native vessels with ≥50% stenosis | <0.001 | ||
| 0 Vessels | 69/560 (12.3) | 82/1811 (4.5) | |
| Revascularization done | 5/69 (7.2) | 3/82 (3.7) | 0.47 |
| 1 Vessel | 155/560 (27.7) | 374/1811 (20.7) | |
| Revascularization done | 124/155 (80.0) | 314/374 (84.0) | 0.27 |
| 2 Vessels | 169/560 (30.2) | 582/1811 (32.1) | |
| Revascularization done | 154/169 (91.1) | 532/582 (91.4) | 0.91 |
| 3 Vessels | 167/560 (29.8) | 773/1811 (42.7) | |
| Revascularization done | 149/167 (89.2) | 694/773 (89.8) | 0.83 |
| Specific native vessels with ≥50% stenosis | |||
| Left main | 16/578 (2.8) | 79/1895 (4.2) | 0.13 |
| LAD | 396/568 (69.7) | 1463/1862 (78.6) | <0.001 |
| Proximal LAD | 168/578 (29.1) | 727/1895 (38.4) | <0.001 |
| Left circumflex | 294/574 (51.2) | 1218/1866 (65.3) | <0.001 |
| Right coronary artery | 309/569 (54.3) | 1227/1841 (66.6) | <0.001 |
| Any obstructive disease ≥70% stenosis | 410/573 (71.6) | 1603/1877 (85.4) | <0.001 |
| No. of native vessels with ≥70% stenosis | <0.001 | ||
| 0 | 158/560 (28.2) | 258/1811 (14.2) | |
| 1 | 199/560 (35.5) | 672/1811 (37.1) | |
| 2 | 143/560 (25.5) | 555/1811 (30.6) | |
| 3 | 60/560 (10.7) | 326/1811 (18.0) | |
| Specific native vessels with ≥70% stenosis | |||
| Left main | 7/578 (1.2) | 30/1895 (1.6) | 0.52 |
| LAD | 260/568 (45.8) | 1013/1862 (54.4) | <0.001 |
| Proximal LAD | 94/578 (16.3) | 460/1895 (24.3) | <0.001 |
| Left circumflex | 184/574 (32.1) | 870/1866 (46.6) | <0.001 |
| Right coronary artery | 222/569 (39.0) | 911/1841 (49.5) | <0.001 |
| SYNTAX score | <0.001 | ||
| No. | 577 | 1890 | |
| Median (Q1–Q3) | 11 (5–21) | 16 (8–25) | |
| Duke Jeopardy score | <0.001 | ||
| No. | 577 | 1890 | |
| Median (Q1–Q3) | 3 (2–5) | 4 (2–5) | |
Data are given as number/total (percentage) unless otherwise indicated. CCTA indicates coronary computed tomography angiography; LAD, left anterior descending artery; Q1, quartile 1; and Q3, quartile 3; SYNTAX, Synergy between Percutaneous Coronary Intervention with TAXus and Cardiac Surgery.
Cardiac Catheterization and Revascularization in the Conservative Strategy Group by Sex
The percentage of women and men randomized to the conservative strategy with at least 1 catheterization during follow‐up, whether or not it was in relation to a primary end point event, was similar (26.3% versus 25.6%, respectively; P=0.717) (Table 3). There was no difference by sex in the performance of revascularization within the conservative treatment strategy group overall (19.2% versus 21.5%, respectively; P=0.242) and excluding revascularization for a suspected primary end point event (Figure 1B). When performed, time to first cardiac catheterization was similar by sex (median [quartile 1–quartile 3] days: 283 [78–653] versus 337 [113–683], respectively; P=0.316), and the rate of revascularization was lower among women (72.3% [107/148] versus 82.3% [427/519] of men who underwent cardiac catheterization; P=0.007). In both sexes, the reasons for revascularization in the conservative strategy group were mostly either a suspected or a confirmed end point event or refractory angina. Cumulative incidence plots of catheterization and revascularization in the conservative treatment group during follow‐up are presented in Figures S1 and S2.
Table 3.
Use of Catheterization and Revascularization in Participants Randomized to the Conservative Strategy Group by Sex
| Characteristic | Women (N=562) | Men (N=2029) | P value |
|---|---|---|---|
| Participants with at least 1 catheterization during follow‐up | 148/562 (26.3) | 519/2029 (25.6) | 0.72 |
| Time from randomization to first catheterization, d | 283 (78–653) | 337 (113–683) | 0.32 |
| Participants with at least 1 revascularization | 108/562 (19.2) | 436/2029 (21.5) | 0.24 |
| Participants with at least 1 revascularization other than for a suspected primary end point event | 70/488 (14.3) | 269/1751 (15.4) | 0.58 |
| Time from randomization to first revascularization, d | 282 (72–613) | 317 (108–684) | 0.23 |
| First revascularization was PCI | 78/108 (72.2) | 291/436 (66.7) | 0.28 |
| Time from randomization to first PCI, d | 282 (68–645) | 288 (93–656) | 0.44 |
| Drug‐eluting stent placed | 66/78 (84.6) | 252/287 (87.8) | 0.46 |
| First revascularization was CABG | 30/108 (27.8) | 145/436 (33.3) | 0.28 |
| Time from randomization to first CABG, d | 288 (112–596) | 347 (137–715) | 0.37 |
| IMA graft placed during CABG | 0/30 (0.0) | 0/145 (0.0) | N/A |
| Indication for first revascularization | 0.46 | ||
| Suspected event | 32/108 (29.6) | 119/436 (27.3) | |
| CEC confirmed event | 29/108 (26.9) | 133/436 (30.5) | |
| Failure of GDMT/refractory angina | 13/108 (12.0) | 34/436 (7.8) | |
| Nonadherence/other | 34/108 (31.5) | 150/436 (34.4) | |
| Participants with at least 1 catheterization or revascularization during follow‐up | 149/562 (26.5) | 528/2029 (26.0) | 0.82 |
| Time from randomization to first catheterization or revascularization, d | 270 (75–645) | 327 (106–670) | 0.34 |
| Catheterization or revascularization performed within 90 d of randomization | 40/562 (7.1) | 119/2029 (5.9) | 0.27 |
| Intended management strategy after first diagnostic catheterization in participants with a catheterization, n | 41 | 92 | |
| Medical therapy only | 36/41 (87.8) | 62/92 (67.4) | 0.01 |
| Reason for medical therapy | 0.07 | ||
| No obstructive CAD | 29/36 (80.6) | 36/62 (58.1) | |
| Anatomy not suitable for any mode of revascularization | 4/36 (11.1) | 16/62 (25.8) | |
| Patient preference | 3/36 (8.3) | 5/62 (8.1) | |
| Other | 0/36 (0.0) | 5/62 (8.1) | |
| PCI/CABG/hybrid | 1/41 (2.4) | 21/92 (22.8) | |
| Undecided | 3/41 (7.3) | 7/92 (7.6) | |
| Unknown | 1/41 (2.4) | 2/92 (2.2) | |
| Missing | 0/41 (0.0) | 0/92 (0.0) |
Data are given as number/total (percentage) or median (25th–75th percentile). CABG indicates coronary artery bypass grafting; CAD, coronary artery disease; CEC, clinical events adjudication committee; GDMT, guideline‐directed medical therapy; IMA, internal mammary artery; and PCI, percutaneous coronary intervention.
GDMT by Sex
Women were less likely to meet goals for blood pressure, LDL‐C, and aspirin use by the end of the study, but were less likely to smoke (Figure 2; Table 4). The SBP goal of <140 mm Hg was met at the end of the study by 73.6% of women and 77.9% of men (P=0.003). The LDL‐C goal of <70 mg/dL was met at the end of the study by 50.2% of women and 61.3% of men (P<0.001). Women were less likely to be on a high‐intensity statin (60.7% versus 64.3%; P=0.025), and less likely to be on aspirin or an aspirin alternative (other antiplatelet agent) than men (95.6% versus 97.2%; P=0.009) but were similarly likely to be taking a β‐blocker (88.0% versus 83.5%; P=0.124). Women met fewer medical therapy goals at study end. Women scored lower on the Morisky‐Green‐Levine scale assessing adherence to medications (79.1% classified as adherent versus 82.2%; P=0.018). Hemoglobin A1c was less likely to be <8% at the end of the trial among women than men, although this was not a specified medical therapy goal (79.5% of women versus 85.3% of men; P<0.001). Women were similarly likely than men to be taking an antianginal medication (including β‐blockers, calcium channel blockers, and other antianginals) at the end of the study (91.1% versus 90.2%; P=0.367), but the number of antianginal medications was higher at the end of the study for women compared with men (Table 4). All of these sex differences were also present at the time of randomization, but the trend toward more antianginal medications among women was not statistically significant at randomization. Results were similar in the subset of patients who underwent CCTA (Table S3), except for similar rates of smoking and medication adherence between women and men in this subset. In the subset who underwent cardiac catheterization with the finding of obstructive CAD, women remained less likely to receive a statin than men, but were similarly likely to receive aspirin and high‐intensity statin therapy. Still, women were less likely to reach the trial goal of LDL‐C <70 mg/dL or to attain a high level of medical therapy optimization, and fewer risk factor goals were met among women. However, scores on the Morisky‐Green‐Levine medication adherence scale indicated similar frequency of adherence for women and men (Table S4).
Figure 2. Sex differences in management and outcomes of patients with chronic coronary disease in the ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) trial.
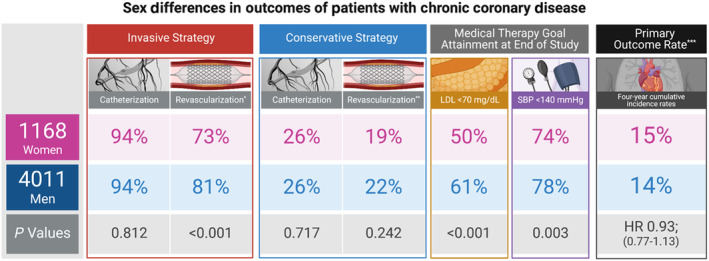
*No sex differences in revascularization rates when stratified by number of vessels diseased on coronary angiography, invasive group. **Revascularization in 72.3% of those undergoing catheterization in conservative group among women, 82.3% among men (P=0.007). ***The primary composite outcome included cardiovascular death, myocardial infarction, hospitalization for heart failure, unstable angina, or resuscitated cardiac arrest. The use of invasive procedures, medical therapy goal attainment, and the primary outcome event rate were compared by participant sex in the ISCHEMIA trial. The use of cardiac catheterization was similar for women and men in both the routine invasive strategy group and the conservative strategy group. The rate was far lower in the conservative strategy group in which catheterization was reserved for failure of medical therapy. The rate of revascularization was far lower for women in the invasive group. However, there was no sex difference in revascularization after stratifying for the lower number of vessels diseased on coronary angiography in women (see Table 2 for details). In the conservative strategy group, overall revascularization rates were similar, but among those who had catheterization, revascularization was lower among women (**). Women were less likely to reach the low‐density lipoprotein (LDL) and systolic blood pressure (SBP) treatment goals. The primary outcome event rate was similar for women and men. HR indicates hazard ratio. Created with BioRender.com.
Table 4.
Medical Therapy for Randomized Participants at Baseline and End of Study by Sex
| Medical therapy characteristics | Baseline | End of Study* | ||||
|---|---|---|---|---|---|---|
| Women (N=1168) | Men (N=4011) | P value | Women (N=1168) | Men (N=4011) | P value | |
| On guideline‐directed medical therapy | ||||||
| Not smoking | 1057/1167 (90.6) | 3477/4007 (86.8) | <0.001 | 1007/1091 (92.3) | 3355/3738 (89.8) | 0.01 |
| Systolic blood pressure<140 mm Hg | 725/1164 (62.3) | 2635/3986 (66.1) | 0.016 | 819/1113 (73.6) | 2999/3849 (77.9) | 0.003 |
| LDL‐C<70 mg/dL | 287/1116 (25.7) | 1334/3824 (34.9) | <0.001 | 553/1102 (50.2) | 2316/3781 (61.3) | <0.001 |
| On aspirin or aspirin alternative | 1085/1146 (94.7) | 3787/3922 (96.6) | 0.004 | 1033/1080 (95.6) | 3630/3734 (97.2) | 0.009 |
| On high‐intensity statin therapy | 377/1106 (34.1) | 1534/3834 (40.0) | <0.001 | 681/1122 (60.7) | 2492/3873 (64.3) | 0.03 |
| On ACE inhibitor/ARB† | 742/1022 (72.6) | 2376/3266 (72.7) | 0.927 | 729/981 (74.3) | 2351/3152 (74.6) | 0.86 |
| On β‐blocker† | 170/189 (89.9) | 738/834 (88.5) | 0.567 | 162/184 (88.0) | 677/811 (83.5) | 0.12 |
| No. of goals met‡ | <0.001 | <0.001 | ||||
| 0 | 2/1111 (0.2) | 6/3801 (0.2) | 1/1072 (0.1) | 3/3658 (0.1) | ||
| 1 | 38/1111 (3.4) | 157/3801 (4.1) | 24/1072 (2.2) | 69/3658 (1.9) | ||
| 2 | 376/1111 (33.8) | 1091/3801 (28.7) | 194/1072 (18.1) | 482/3658 (13.2) | ||
| 3 | 536/1111 (48.2) | 1738/3801 (45.7) | 488/1072 (45.5) | 1513/3658 (41.4) | ||
| 4 | 159/1111 (14.3) | 809/3801 (21.3) | 365/1072 (34.0) | 1591/3658 (43.5) | ||
| High level of medical therapy optimization§ | 159/1111 (14.3) | 809/3801 (21.3) | <0.001 | 365/1072 (34.0) | 1591/3658 (43.5) | <0.001 |
| On aspirin or aspirin alternative/other antiplatelet among all participants | 1106/1167 (94.8) | 3872/4007 (96.6) | 0.003 | 1076/1123 (95.8) | 3768/3872 (97.3) | 0.010 |
| LDL‐C<70 mg/dL and on a statin | 281/1116 (25.2) | 1318/3822 (34.5) | <0.001 | 543/1098 (49.5) | 2286/3777 (60.5) | <0.001 |
| On ACE inhibitor/ARB among all participants | 788/1168 (67.5) | 2628/4005 (65.6) | 0.241 | 791/1123 (70.4) | 2678/3873 (69.1) | 0.41 |
| On statin | 1087/1168 (93.1) | 3817/4006 (95.3) | 0.003 | 1049/1123 (93.4) | 3706/3874 (95.7) | 0.002 |
| On antianginal medications|| | 1060/1168 (90.8) | 3641/4005 (90.9) | 0.869 | 1023/1123 (91.1) | 3495/3875 (90.2) | 0.37 |
| No. of antianginal medications|| | 0.479 | 0.002 | ||||
| 1 | 454/1060 (42.8) | 1674/3641 (46.0) | 469/1023 (45.8) | 1797/3495 (51.4) | ||
| 2 | 430/1060 (40.6) | 1404/3641 (38.6) | 397/1023 (38.8) | 1243/3495 (35.6) | ||
| 3 | 148/1060 (14.0) | 471/3641 (12.9) | 128/1023 (12.5) | 356/3495 (10.2) | ||
| 4 | 24/1060 (2.3) | 76/3641 (2.1) | 21/1023 (2.1) | 89/3495 (2.5) | ||
| ≥5 | 4/1060 (0.4) | 16/3641 (0.4) | 8/1023 (0.8) | 10/3495 (0.3) | ||
| HbA1c<8% | 578/762 (75.9) | 2245/2677 (83.9) | <0.001 | 667/839 (79.5) | 2516/2950 (85.3) | <0.001 |
| Adherent to medications based on Morisky‐Green‐Levine assessment | 808/1127 (71.7) | 2864/3840 (74.6) | 0.052 | 874/1105 (79.1) | 3117/3791 (82.2) | 0.02 |
Data are given as number/total (percentage). ACE indicates angiotensin‐converting enzyme; ARB, angiotensin receptor blocker; HbA1c, hemoglobin A1C; and LDL‐C, low‐density lipoprotein cholesterol.
For each individual guideline‐directed medical therapy (GDMT) goal, the last visit is defined as the latest visit (at least 12 months after randomization) where the goal is evaluable. If the latest visit where the goal is evaluable is <12 months after randomization, then the individual GDMT goal is missing.
Participants who are not indicated for ACE inhibitor/ARBs or β‐blockers are counted as having missing data for the individual goals.
The following GDMT goals contribute to the number of goals met: not smoking, systolic blood pressure<140 mm Hg, LDL‐C<70 mg/dL and on any statin, and on aspirin or other antiplatelet or anticoagulant. Number of goals met is missing if any of the individual goals are missing.
High Level of medical therapy optimization is defined as a participant meeting all of the following goals: not smoking, systolic blood pressure<140 mm Hg, LDL‐C<70 mg/dL and on any statin, and on aspirin or other antiplatelet or anticoagulant. High level of medical therapy optimization is missing if any of the individual goals are missing.
Includes β blocker, calcium channel blocker, long‐acting nitrate, ranolazine, trimetazidine, ivabradine, nicorandil, and other antianginal medications marked as “unknown.”
Trial Primary and Secondary Outcomes by Sex
There were no significant differences in the main treatment effect by sex in the primary composite outcome (adjusted HR for women versus men, 0.93 [95% CI, 0.77–1.13]; P=0.465) or the major secondary outcome of cardiovascular death or MI (adjusted HR, 0.93 [95% CI, 0.76–1.14]; P=0.494) (Figure 3; Table 5). There was also no difference by sex in MI overall (adjusted HR, 0.82 [95% CI, 0.64–1.04]; P=0.101), but the rate of periprocedural MI was lower among women (adjusted HR, 0.40 [95% CI, 0.21–0.76]; P=0.005), consistent with lower rates of revascularization among women. When considering only women and men in the invasive strategy group who underwent revascularization, there was no difference in the 4‐year rate of procedural MI, 1.8% (95% CI, 0.4%–5.8%) among women versus 2.8% among men (95% CI, 1.6%–4.5%) (P=0.514). The effect of CAD severity (≥50%) on MI risk did appear to vary significantly by sex (P=0.018; Table S5). There were no significant interactions between participant sex and age, magnitude/extent of ischemia, or diabetes on clinical outcomes. Bleeding rates reported by sites through discharge were not different by sex (3.5% in women and 4.2% in men; P=0.317).
Figure 3. Unadjusted cumulative incidence plot of trial primary and major secondary outcomes and all‐cause mortality by sex.
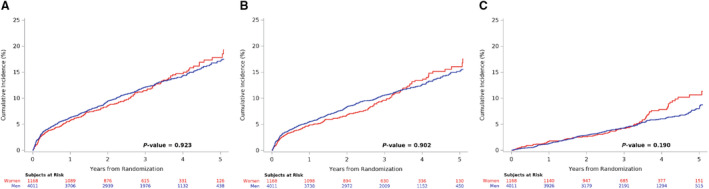
A, Cardiovascular death, myocardial infarction (MI), hospitalization for unstable angina or heart failure, or resuscitated cardiac arrest. B, Cardiovascular death or MI. C, All‐cause death.
Table 5.
Cumulative Incidence Rates and Estimated HRs of Sex for Clinical Outcomes
| Event | Women (N=1168) | Men (N=4011) | Unadjusted HR, women vs men (95% CI) | Adjusted* HR, women vs men (95% CI) | P value |
|---|---|---|---|---|---|
| Cardiovascular death, MI, hospitalization for unstable angina or heart failure, or resuscitated cardiac arrest | |||||
| No. of events | 151 | 519 | 0.99 (0.82–1.18) | 0.93 (0.77–1.13) | 0.47 |
| Cumulative incidence rate at 4 y (95% CI), % | 14.8 (12.4–17.2) | 14.3 (13.1–15.6) | |||
| Cardiovascular death or MI | |||||
| No. of events | 133 | 457 | 0.98 (0.81–1.19) | 0.93 (0.76–1.14) | 0.49 |
| Cumulative incidence rate at 4 y (95% CI), % | 13.4 (11.2–15.9) | 12.6 (11.5–13.8) | |||
| All‐cause death | |||||
| No. of events | 75 | 214 | 1.19 (0.92–1.55) | 1.10 (0.84–1.45) | 0.48 |
| Cumulative incidence rate at 4 y (95% CI), % | 7.9 (6.1–10.1) | 6.1 (5.2–7.0) | |||
| Cardiovascular death | |||||
| No. of events | 59 | 144 | 1.40 (1.03–1.89) | 1.30 (0.94–1.78) | 0.11 |
| Cumulative incidence rate at 4 y (95% CI), % | 6.7 (5.0–8.7) | 3.9 (3.3–4.7) | |||
| MI | |||||
| No. of events | 90 | 353 | 0.86 (0.68–1.09) | 0.82 (0.64–1.04) | 0.10 |
| Cumulative incidence rate at 4 y (95% CI), % | 8.5 (6.7–10.5) | 9.9 (8.8–11.0) | |||
| Nonprocedural MI (type 1, 2, 4b, 4c) | |||||
| No. of events | 74 | 252 | 1.00 (0.77–1.30) | 0.95 (0.73–1.24) | 0.70 |
| Cumulative incidence rate at 4 y (95% CI), % | 7.2 (5.6–9.1) | 7.3 (6.4–8.3) | |||
| Procedural MI (type 4a, 5) | |||||
| No. of events | 11 | 83 | 0.45 (0.24–0.85) | 0.40 (0.21–0.76) | 0.005 |
| Cumulative incidence rate at 4 y (95% CI), % | 1.0 (0.5–1.7) | 2.2 (1.7–2.7) | |||
| Stroke | |||||
| No. of events | 22 | 61 | 1.23 (0.76–2.01) | 1.04 (0.63–1.74) | 0.87 |
| Cumulative incidence rate at 4 y (95% CI), % | 2.1 (1.3–3.3) | 1.7 (1.3–2.2) | |||
| Hospitalization for heart failure | |||||
| No. of events | 24 | 52 | 1.58 (0.97–2.56) | 1.54 (0.93–2.58) | 0.10 |
| Cumulative incidence rate at 4 y (95% CI), % | 1.9 (1.1–2.9) | 1.5 (1.1–1.9) | |||
| Cardiovascular death, MI, hospitalization for unstable angina or heart failure, resuscitated cardiac arrest, or stroke | |||||
| No. of events | 163 | 559 | 0.99 (0.83–1.18) | 0.93 (0.77–1.11) | 0.41 |
| Cumulative incidence rate at 4 y (95% CI), % | 16.1 (13.7–18.7) | 15.4 (14.1–16.7) | |||
HR indicates hazard ratio; and MI, myocardial infarction.
Adjusted for randomized treatment arm, age at randomization, estimated glomerular filtration rate, ejection fraction, and diabetes. Continuous variables are modeled as restricted cubic splines with knots at the 10th, 50th, and 90th percentile of each variable's empirical distribution.
There was no significant interaction between sex and treatment strategy for the primary outcome, the major secondary outcome, mortality (both cardiac and all cause), or MI. The P value for interaction between sex and treatment on stroke was 0.044, with relatively greater hazard for these outcomes in the invasive group among women than men and lower hazard for women compared with men in the conservative strategy group (Table S6).
Chest Pain Admissions During Follow‐Up
Women experienced more emergency department admissions for noncardiac chest pain than men (38/1168 [3.3%] versus 74/4011 [1.8%]; P=0.004), but a similar number of hospitalizations for noncardiac chest pain (22/1168 [1.9%] versus 54/4011 [1.3%]; P=0.179).
DISCUSSION
In the ISCHEMIA trial, women and men experienced similar rates of the primary and secondary outcomes. Women assigned to the invasive treatment strategy were less likely than men to undergo revascularization because of the lower rate of obstructive CAD at cardiac catheterization and lesser extent of CAD when present. In the conservative treatment strategy group, women and men were equally likely to have cardiac catheterization for a suspected clinical event or failed GDMT, despite higher angina burden and less severe ischemia on stress testing among women at trial entry. 14 Once cardiac catheterization was performed, revascularization was again less likely among women than men. Standardized algorithms were provided to enrolling sites to guide optimization of GDMT and of complete ischemic revascularization, without regard to sex. 25 Yet, women attained fewer GDMT goals by the end of the study.
The similar clinical outcomes for men and women represent the net effects of sex differences that reflect opposing risks. Women randomized in the ISCHEMIA trial were older than men and had higher rates of hypertension and diabetes with poorer risk factor control throughout follow‐up, but had less extensive anatomic CAD and ischemia on imaging. We found the effect of CAD severity of MI varied significantly by sex.
The design of the ISCHEMIA trial is different from the prior clinical outcomes utilizing revascularization and aggressive drug evaluation and the bypass angioplasty revascularization investigation 2 diabetes trials in that randomization of ISCHEMIA trial subjects occurred before diagnostic angiography and there was a higher predefined threshold of ischemia at baseline to qualify for study entry. CCTA was performed before randomization in most patients to confirm the presence of obstructive CAD and to exclude significant left main disease. A similar proportion of women and men had protocol‐assigned catheterization in the invasive assigned group. This equal access to cardiac catheterization and revascularization is notable, given that previous studies have demonstrated that women are less likely to undergo further evaluation after a positive functional test result, even within the randomized prospective multicenter imaging study for evaluation of chest pain trial. 33 , 34 Still, among invasive therapy–assigned patients, fewer women underwent revascularization, largely because of the absence of obstructive CAD at cardiac catheterization. This was the case even though the trial used prerandomization CCTA to confirm obstructive CAD in most participants. This finding is consistent with numerous studies reporting less extensive CAD among women, and with the CCTA findings among randomized participants in this trial, previously reported. 14 When we stratified the invasive group by the number of vessels with at least 50% stenosis, revascularization rates were similar for women and men.
The rates of cardiac catheterization and revascularization by sex within the conservative treatment strategy group were similar, although angina frequency was higher among randomized women compared with randomized men. 14 Whether or not this resulted in worse health status outcomes among women assigned to conservative management will be addressed in ongoing analyses. It is noteworthy, however, that more women experienced chest pain emergency department visits than men, without a difference in adjudicated MI or unstable angina. This pattern is consistent with prior analyses of the relationship between angina severity and the outcomes of cardiovascular hospitalization, MI, and death (namely, more frequent angina in patients with CCD is associated with more angina hospitalizations and heart failure events, but not with increased risk of MI after adjustment for clinical variables). 35 , 36 Greater angina frequency has also been historically associated with increased rates of revascularization. However, this was not observed in the ISCHEMIA trial, likely because of the study protocol, in which conservative‐assigned participants were recommended to undergo revascularization only for symptoms refractory to medical therapy or a suspected end point event. Furthermore, the ISCHEMIA trial excluded patients with an unacceptable level of angina at the time of enrollment.
Despite the rigorous design of the trial and the emphasis on lifestyle intervention and intensive, goal‐directed pharmacologic secondary prevention in both arms for all participants, use of GDMT in women was unexpectedly and disappointingly lower than in men throughout study follow‐up. Women were less likely to attain blood pressure control, LDL‐C targets, and the hemoglobin A1c target. These differences were similar in magnitude when comparing baseline medical therapy with medical therapy at the end of the study, despite improvement over the course of the study in the cohort in general. For example, the difference in the proportion of patients meeting the LDL‐C goal was 9 percentage points lower among women at baseline (25.7% versus 34.9%) and 11 percentage points lower among women at the end of the study (50.2% versus 61.3%). The reasons for this are unclear. Self‐reported adherence was modestly lower among women. When we assessed these differences in the subset of patients with obstructive CAD on CCTA, results were largely similar, likely related to the blinded nature of study CCTA in this trial. Interestingly, analysis of the subset of patients within the invasive strategy group who had at least single‐vessel CAD, and in the subset with CCTA performed, showed that self‐reported adherence to medications was similar between women and men. It has previously been reported that awareness by patients of coronary computed tomography results has the potential to increase adherence. 37 Within the subset of patients in the invasive strategy group with obstructive CAD, high‐intensity statin therapy and blood pressure goal attainment were similar by sex. Still, even with the knowledge by both patients and physicians of anatomic details of significant CAD, the LDL‐C treatment goal was less likely to be met among women, and women attained fewer medical therapy goals. Although we do not have access to detailed information about dose titration in response to blood pressure and laboratory values in the ISCHEMIA trial, analysis of the relationship between risk factor goal attainment and outcomes in the trial is ongoing. Nevertheless, the imperative to achieve equitable use of GDMT implementation among women with CCD is both an important challenge and an opportunity for improved clinical outcomes.
We have previously reported that ISCHEMIA trial participants with 3‐vessel CAD were at particularly high risk of cardiovascular events, and that the rate of cardiovascular death or MI tended to be lower among invasive strategy–assigned patients than conservative strategy–assigned patients in the most severe CAD subgroup. 38 Interestingly, there was evidence of interaction between sex and CAD severity on the end point of MI, such that women with 3‐vessel CAD had higher risk of MI than men, and at lesser extent of CAD, women were at lower risk of MI than men. This raises a question of whether undertreatment of women could have been particularly impactful in those with more extensive CAD. There was also interaction between sex and treatment on stroke, with women at higher risk of stroke in the invasive strategy group, and no difference by treatment group in stroke among men. The interaction test results should be interpreted with caution, especially as adjustment for multiple testing was not performed.
This analysis has several limitations. The ISCHEMIA trial cohort was only 23% female, because of obstructive CAD and moderate or severe ischemia eligibility criteria, which women more often failed to meet. 14 Specific drugs and doses of GDMT were not available. As a randomized trial, we are able to address the effectiveness of alternative management strategies, but the real‐world effectiveness will require different types of studies. Heath status outcomes will be reported separately.
CONCLUSIONS
Despite a higher angina burden and less obstructive CAD, women and men with CCD and site‐assessed moderate or severe ischemia in the ISCHEMIA trial experienced similar adjusted rates of the primary and secondary outcomes during 3.2‐year median follow‐up. Cardiac catheterization was used at similar rates by sex, but revascularization was less frequent among women, because of the higher prevalence of ischemia with no obstructive coronary arteries and lesser extent of CAD at angiography. Disappointingly, medical therapy goal attainment was lower among women than men, which represents an important challenge and opportunity for improvement.
Sources of Funding
This work was supported by National Institutes of Health grants U01HL105907, U01HL105462, U01HL105561, and U01HL105565. This project was supported in part by Clinical Translational Science Award No. 11UL1TR001445 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences, the National Heart, Lung, and Blood Institute, the National Institutes of Health, or the US Department of Health and Human Services.
Disclosures
Harmony R. Reynolds reports grants from National Heart, Lung, and Blood Institute, during the conduct of the study, she receives support from Abbott Vascular (donation of optical coherence tomography catheters for an unrelated research study) and Biotelemetry Inc (donation of telemetry monitors for an unrelated research study). Derek D. Cyr reports grants from National Heart, Lung, and Blood Institute during the conduct of the study. Noel Bairey Merz reports grants from National Heart, Lung, and Blood Institute, Louis B. Mayer Foundation, National Institutes of Health (NIH)‐Clinical Translational Science Institute, congressionally directed medical research programs ‐ Department of Defense, NIH‐Caladrius, California Institute for Precision Medicine, and Sanofi‐Vascular; personal fees from Medscape, Sanofi‐Vascular, NIH Center for Scientific Review and NIH Office of Research on Women's Health, iRhythm, and Caladrius; personal fees from Abbott Diagnostics. Bernard R. Chaitman reports grants from National Heart, Lung, and Blood Institute during the conduct of the study, personal fees from Merck, NovoNordisk, Sanofi, Lilly, Johnson and Johnson, Daiichi Sankyo, Tricida, Relypsa, Imbria, and Xylocor outside the submitted work. William E. Boden reports grants from National Heart, Lung, and Blood Institute, during the conduct of the study; grants from Abbvie, Amarin, and Amgen, personal fees from Amgen, Cleveland Clinic Clinical Coordinating Center, and Janssen, outside the submitted work. Sripal Bangalore reports grants from the National Heart, Lung, and Blood Institute during the conduct of the study, grants and personal fees from Abbott Vascular, personal fees from Biotronik, Pfizer, Amgen, and Reata outside of the submitted work. Gregg W. Stone reports grants and personal fees from the National Heart, Lung, and Blood Institute during the conduct of the study; personal fees from Terumo, Amaranth, and Shockwave; personal fees and other from Valfix; personal fees from TherOx, Reva, Vascular Dynamics, Robocath, HeartFlow, Gore, Ablative Solutions, Matrizyme, Miracor, Neovasc, V‐wave, Abiomed, Claret, and Sirtex; personal fees and other from Ancora and Qool Therapeutics; other from Cagent, Applied Therapeutics, Biostar family of funds, and MedFocus family of funds; personal fees and other from SpectraWave; personal fees from MAIA Pharmaceuticals; personal fees and other from Orchestra Biomed; other from Aria; personal fees from Vectorious; and other from Cardiac Success, outside the submitted work. John Spertus reports grants from National Heart, Lung and Blood Institute, during the conduct of the study; personal fees from Bayer, Novartis, AstraZeneca, Amgen, Janssen, and United Healthcare, grants from American College of Cardiology, personal fees from Blue Cross Blue Shield of Kansas City, outside the submitted work. In addition, Dr Spertus has a patent copyright to Seattle Angina Questionnaire with royalties paid and equity in Health Outcomes Sciences. Jonathan Newman reports receiving funding from the National Heart, Lung, and Blood Institute. Jeffrey S. Berger reports grants from National Heart, Lung, and Blood Institute during the conduct of the study. Ahmed Elghamaz reports grants from the National Heart, Lung, and Blood Institute during the conduct of the study. Renato D. Lopes reports grants from the National Heart, Lung, and Blood Institute during the conduct of the study; other from Bayer and Boehringer Ingelheim; grants and other from Bristol Myers Squibb; other from Daiichi Sankyo; grants and other from GlaxoSmithKline and Medtronic; other from Merck; grants and other from Pfizer; other from Portola; and grants and other from Sanofi, outside the submitted work. James K. Min reports grants from National Heart, Lung, and Blood Institute, during the conduct of the study; other from CLEERLY INC, grants and other from GE HEALTHCARE, other from ARINETA, outside the submitted work. Daniel S. Berman receives software royalties from Cedars‐Sinai Medical Center outside the submitted work. Raymond Y. Kwong reports grants from National Heart, Lung, and Blood Institute during the conduct of the study. Robert A. Harrington reports grants from the National Heart, Lung, and Blood Institute, Duke/Patient‐Centered Outcomes Research Institute (Aspirin Dosing: A patient‐centric Trial Assessing the Benefits and Long‐term Effectiveness), Jannsen (Factor Xla inhibitor), CSL (HDL), Baim Institute, National Heart, Lung, and Blood Institute (REPRIEVE), and UColorado; personal fees from National Heart, Lung, and Blood Institute (COVID/CONNECTS), Atropos Health, Bitterroot Bio, BMS, Bridge Bio, Element Science, Foresight, and WebMD; Board of Directors at American Heart Association and Cytokinetics. Sean M. O'Brien reports grants from the National Heart, Lung, and Blood Institute during the conduct of the study. David J. Maron reports grants from the National Heart, Lung, and Blood Institute during the conduct of the study. Judith S. Hochman is the principal investigator for the ISCHEMIA trial for which, in addition to support by the National Heart, Lung, and Blood Institute grant, devices and medications were provided by Abbott Vascular; Medtronic Inc; Abbott Laboratories (formerly St. Jude Medical, Inc); Royal Philips NV (formerly Volcano Corporation); Arbor Pharmaceuticals, LLC; AstraZeneca Pharmaceuticals, LP; Merck Sharp & Dohme Corp; Omron Healthcare, Inc, Sunovion Pharmaceuticals, Inc, Espero BioPharma; and Amgen, Inc; and financial donations from Arbor Pharmaceuticals LLC and AstraZeneca Pharmaceuticals LP. She is principal investigator for ISCHEMIA‐EXTEND. The remaining authors have no disclosures to report.
Supporting information
Acknowledgments
We are particularly indebted to the coordinators at the ISCHEMIA trial sites who collected study data and to the patients who agreed to provide their quality of life data for the trial.
Appendix A.
| Country (No. Randomizations) | Investigator(s) | Study Coordinator(s) | City and State | Institution (No. Randomizations) |
|---|---|---|---|---|
| (If Applicable) | ||||
| United States (853)* | ||||
| Country Leader | ||||
| David J. Maron, MD | ||||
| Regional Leader for VA Sites | ||||
| William E. Boden, MD | ||||
| Kreton Mavromatis, MD | John Doan, MD | Decatur, GA | Atlanta VA Medical Center (139) | |
| Jason Linefsky, MD | Raven Lee, CCRP | |||
| Risha Patel | ||||
| Todd Miller, MD | So Yang Cho | Rochester, MN | Mayo Clinic (50) | |
| Susan Milbrandt | ||||
| Dawn Shelstad | ||||
| Subhash Banerjee, MD | Preeti Kamath, BDS, MHA, CCRP | Dallas, TX | V.A. North Texas Health Care System (35) | |
| Ishita Tejani, BDS, MS, MSPH | ||||
| Harmony R. Reynolds, MD | Stanley E. Cobos, BA | New York, NY | NYU Langone Medical Center‐Bellevue Hospital (26) | |
| Jonathan D. Newman, MD, MPH | Kirsten J. Quiles, MS | |||
| Sripal Bangalore, MD | Raven R. Dwyer, MPH | |||
| Robert M. Donnino, MD | Dalisa Espinosa, MBS | |||
| Lawrence M. Phillips, MD | ||||
| Muhamed Saric, MD, PhD | ||||
| Khaled Abdul‐Nour, MD | Allison Schley, BS | Detroit, MI | Henry Ford Health System (21) | |
| Heather Golden | ||||
| Peter H. Stone, MD | Hermine Osseni, MS | Boston, MA | Brigham and Women's Hospital, Harvard Medical School (21) | |
| Charlene Wiyarand | ||||
| Peter Douglass, BA | ||||
| Hayley Pomeroy, BA | ||||
| Alexandra Craft, BA | ||||
| Bethany Harvey, BA | ||||
| James J. Jang, MD | Olivia Anaya | San Jose, CA | Kaiser Permanente San Jose (18) | |
| Gennie Yee, MD | Phoebe Goold, RN | |||
| Steven Weitz, MD | Steven Giovannone | Schenectady, NY | Cardiology Associates of Schenectady P.C. (17) | |
| Lori Pritchard, RN | ||||
| Suzanne Arnold, MD | Rosann Gans, RN | Kansas City, MO | Saint Luke's Hospital (17) | |
| James Henry O'Keefe, Jr, MD (PI from 2012 to 2016) | Paul Kennedy, RN | |||
| Michael D. Shapiro, DO | Shobana Ganesan, PhD | Portland, OR | Oregon Health and Science University (17) | |
| David Schlichting, LPN | ||||
| Aynun Naher | ||||
| Mohammad El‐Hajjar, MD | Albany, NY | Albany Medical Center Hospital (16) | ||
| Mandeep S. Sidhu, MD, MBA | ||||
| Steven A. Fein, MD | Wendy L. Stewart, MS | |||
| Mikhail T. Torosoff, MD, PhD | Kristin M. Salmi, BS | |||
| Radmila Lyubarova, MD | ||||
| Sulagna Mookherjee, MD | ||||
| Krzysztof Drzymalski, MD | ||||
| Edward O. McFalls, MD, PhD | Minneapolis, MN | Minneapolis VAMC (15) | ||
| Santiago A. Garcia, MD | ||||
| Stefan C. Bertog, MD | Debra K. Johnson, RN | |||
| Rizwan A. Siddiqui, MD | Rebekah R. Herrmann, RN | |||
| Areef Ishani, MD | ||||
| Ronnell A. Hansen, MD | ||||
| Michel Georges Khouri, MD | Kristine Arges | Durham, NC | Duke University Medical Center (15) | |
| Melissa LeFevre | ||||
| Jennifer Tomfohr | ||||
| Jonathan L. Goldberg, MS, MD | Kimberly Ann Byrne | Cleveland, OH | Louis Stokes Cleveland Veterans Affairs Medical Center (14) | |
| Taissa Zappernick | ||||
| Richard Goldweit, MD | Sallie Canada | Englewood, NJ | Englewood Hospital and Medical Center (13) | |
| Meghana Kakade | ||||
| Patricia Mieses | ||||
| Stanley E. Cobos, BA | Brooklyn, NY | NYU‐HHC Woodhull Hospital (12) | ||
| Raven R. Dwyer, MPH | ||||
| Ronny A. Cohen, MD | Dalisa Espinosa, MBS | |||
| Brooks Mirrer, MD | Kirsten J. Quiles, MS | |||
| Victor Navarro, MD | Magdalena Rantinella, BS | |||
| Jessica Rodriguez, BS | ||||
| Olivia Mancilla, BS | ||||
| David E. Winchester, MD, MS | Susan Stinson, RN | Gainesville, FL | Malcom Randall VAMC (11) | |
| Marvin Kronenberg, MD | Terry Weyand | Nashville, TN | Vanderbilt University Medical Center (11) | |
| Philip Rogal, MD | Sherron C. Crook | |||
| Christopher McFarren, MD | ||||
| John F. Heitner, MD | Jean Ho | Brooklyn, NY | New York‐Presbyterian/Brooklyn Methodist Hospital (10) | |
| Saadat Khan | ||||
| Mahmoud Mohamed | ||||
| Ira M. Dauber, MD | Mary R. Soltau, RN | Littleton, CO | South Denver Cardiology Associates, P.C. (10) | |
| Delsa K. Rose, RN | ||||
| Rebecca J. Wimmer, RN | ||||
| Kathy E. Siegel, RN | ||||
| Susan Derbyshire | ||||
| Charles Cannan, MD | Michelle Dixon | Portland, OR | Providence Heart and Vascular Institute (10) | |
| Gerald Leonard | ||||
| Sriram Sudarshan, MD | Ciarra Heard, LVN | Wichita Falls, TX | Wichita Falls Heart Clinic (9) | |
| Viviana Gabriel, LVN | ||||
| Sukie Desire | ||||
| Puja K. Mehta, MD | Atlanta, GA | Emory University (9) | ||
| Michael McDaniel, MD | Fauzia Rashid, PhD | |||
| Stamatios Lerakis, MD | Senait Asier | |||
| Arshed Quyyumi, MD | Keyur Patel | |||
| Nanette K. Wenger, MD | ||||
| Chester M. Hedgepeth, MD, PhD | Jennifer Gillis, APRN | Warwick, RI | Kent Hospital (9) | |
| Heather Hurlburt, MD | Megan Manocchia, RN | |||
| Alan Rosen, MD | Susan Moore, RN | |||
| Elizabeth Congdon | ||||
| Zakir Sahul, MD | Gail Brandt | Ypsilanti, MI | Michigan Heart, PC (9) | |
| Nora Marchelletta | ||||
| Kristina Wippler | ||||
| David Booth, MD | Yvonne Taul, RN | Lexington, KY | University of Kentucky (8) | |
| Steve Leung, MD | Jennifer Isaacs, MS | |||
| Ahmed Abdel‐Latif, MD, PhD | Viktoria Bulkley, RN | |||
| Hassan Reda, MD | Caroline Rodgers | |||
| Khaled Ziada, MD | ||||
| Sampoornima Setty, MD | Kimberly E. Halverson, RHIT | La Crosse, WI | Gundersen Lutheran Medical Center (8) | |
| Christine Roraff, RN | ||||
| Jonean Thorsen, RN | ||||
| Rajat S. Barua, MD, PhD | Amarachi Ojajuni | Kansas City, MO | Kansas City VA Medical Center (8) | |
| Oni Olurinde | ||||
| Kamalakar Surineni | ||||
| Fadi Hage, MD | Badhma Valaiyapathi, MD | Birmingham, AL | UAB Vascular Biology and Hypertension Program (8) | |
| Christiano Caldeira, MD | ||||
| James E. Davies, MD | ||||
| Massoud Leesar, MD | ||||
| Jaekyeong Heo, MD | ||||
| Amy Iskandrian, MD | ||||
| Firas Al Solaiman, MD | ||||
| Satinder Singh, MD | ||||
| Khaled Dajani, MD | Carol M. Kartje, BSN | Maywood, IL | Loyola University Medical Center (8) | |
| Mohammad El‐Hajjar, MD | Albany, NY | Samuel Stratton VA Medical Center of Albany NY (7) | ||
| Paul Der Mesropian, MD | ||||
| Joseph Sacco, MD | Michele Rawlins, NP | |||
| Brian McCandless, MD | Jennifer Thomson, MA | |||
| Marisa Orgera, MD | ||||
| Mandeep S. Sidhu, MD, MBA (2012–2016) | ||||
| Mary Colleen Rogge, RN | Cincinnati, OH | Cincinnati VA Medical Center (7) | ||
| Imran Arif, MD | Julie Bunke, BA | |||
| Hanan Kerr, MD | Kendra Unterbrink, PA | |||
| Jacqueline Fannon, RN | ||||
| Cynthia Burman, NP | ||||
| Jorge F. Trejo (Gutierrez), MD | Marcia F. Dubin, CCRP | Jacksonville, FL | Mayo Clinic Florida (7) | |
| Gerald Fletcher, MD | ||||
| Gary E. Lane, MD | ||||
| Lynn M. Neeson, DNP | ||||
| Pragnesh P. Parikh, MD | ||||
| Peter M. Pollak, MD | ||||
| Brian P. Shapiro, MD | ||||
| Kevin Landolfo, MD | ||||
| Anthony Gemignani, MD | Sarah Beaudry, RN | White River Junction, VT | VAMC‐White River Junction (7) | |
| Daniel O'Rourke, MD | ||||
| Judith L. Meadows, MD | Stephanie A. Tirado, RN | West Haven, CT | VA Connecticut Healthcare System (7) | |
| Janet Halliday | ||||
| Pamela Julian | ||||
| Jason T. Call, MD | Stephanie, M. Lane, RN, BSN, CCRN | Winchester, VA | Winchester Cardiology and Vascular Medicine, PC (7) | |
| Jennifer L. Stanford, RN, MSN | ||||
| Joseph Hannan, MD | Worcester, MA | Saint Vincent Hospital at Worcester Medical Center (7) | ||
| Robert Bojar, MD | Patricia Arsenault, RN | |||
| Deepti Kumar, MD | Pamela Sigel, RN | |||
| John Mukai, MD | ||||
| Edward T. Martin, MS, MD | Miriam Brooks | Tulsa, OK | Oklahoma Heart Institute (7) | |
| Gabriel Vorobiof, MD | Ladda Douangvila | Los Angeles, CA | Ronald Reagan UCLA Medical Center (7) | |
| Rubine Gevorgyan | ||||
| Alec Moorman, MD | Fatima Ranjbaran, RN | Seattle, WA | University of Washington Medical Center (7) | |
| Bryn Smith, BS | ||||
| Carly Ohmart | ||||
| Scott Kinlay, MBBS, PhD | West Roxbury, MA | VA Boston Healthcare System (6) | ||
| Robert J. Hamburger, MD | ||||
| Thomas P. Rocco, MD | Samantha Ly, MA | |||
| Deepak L. Bhatt, MD, MPH | Margot C. Quinn, BA | |||
| Kevin Croce, MD, PhD | Sara Temiyasathit, PhD | |||
| Jacquelyn A Quin, MD | Jacquelyn Do, MPH | |||
| Jati Anumpa, MD | Desiree Tobin, MPH | |||
| Marco Zenati, MD, MSc | ||||
| David P Faxon, MD | ||||
| Glenn Rayos, MD | Jennifer Langdon | Daytona Beach, FL | Daytona Heart Group (6) | |
| Marcia Werner Bayer | ||||
| Ashraf Seedhom, MD | Amanda O'Malley | Albany, NY | Capital Cardiology Associates (6) | |
| Lance Sullenberger, MD | Erin Orvis | |||
| Gregory Kumkumian, MD | Mandy Murphy, RN | Bethesda, MD | NIH Heart Center at Suburban Hospital (6) | |
| Ann Greenberg, RN | ||||
| Margaret Iraola, RN | ||||
| Steven P. Sedlis, MD | Leandro C.Maranan, CCRC | New York, NY | VA New York Harbor Health Care System (6) | |
| Robert M. Donnino, MD | ||||
| Jeffrey Lorin, MD | ||||
| Jacqueline E. Tamis‐Holland, MD | Ammy Malinay, RN | Ridgewood, NJ | Mount Sinai Saint Luke's Hospital (6) | |
| Robert Kornberg, MD | ||||
| Robert Leber, MD | ||||
| Souheil Saba, MD | Candice P. Edillo, RN | Southfield, MI | Providence‐Providence Park Hospital (6) | |
| Michael W. Lee, MD | ||||
| Delano R. Small, MD | ||||
| Wassim Nona, MD | ||||
| Patrick B. Alexander, MD | ||||
| Iram Rehman, MD | ||||
| Umesh Badami, MD | Ann Ostrander, RN | Saginaw, MI | Covenant Medical Center, Inc (5) | |
| Stephanie Wasmiller, RN | ||||
| Kevin Marzo, MD | Wendy Drewes, RN | Mineola, NY | NYU Winthrop (5) | |
| Dipti Patel, RN | ||||
| Inga H. Robbins, MD | Pomona, NJ | AtlantiCare Regional Medical Center (5) | ||
| Howard A. Levite, MD | Jackie M White, RN, BSN CCRC | |||
| Sanjay Shetty, MD | Alison Hallam | |||
| Mayuri Patel, MD | ||||
| Glenn S. Hamroff, MD | Benjamin J Spooner, RPA‐C | Cortlandt Manor, NY | NYP Medical Medical Group Hudson Valley Cardiology (5) | |
| Linda M Hollenweger, LPN,CCRC | ||||
| Raymond W. Little, MD | Holly Little | Houston, TX | Houston Heart and Vascular Associates (5) | |
| Brandi D. Zimbelman, FNP‐C | Tiffany Little | |||
| Charles Y. Lui, MD | Nona A Eskelson, RN | Salt Lake City, UT | Salt Lake City VA Medical Center (4) | |
| Brigham R. Smith, MD | ||||
| Daniel P. Vezina, MD, MSC | ||||
| Lillian L. Khor, MBBCh, MSc | ||||
| Josephine D. Abraham, MD, MPH | ||||
| David A. Bull, MD | ||||
| Stephen H. McKellar, MD, MSc | ||||
| David Booth, MD | Yvonne Taul, RN | Lexington, KY | Lexington VA Medical Center (4) | |
| John Kotter, MD | Caroline Rodgers, RN | |||
| Ahmed Abdel‐Latif, MD, PhD | Jennifer Isaacs, MS | |||
| Viktoria Bulkley | ||||
| Bob Hu, MD | Renee Kaneshiro | Palo Alto, CA | Palo Alto Medical Foundation Research Institute (4) | |
| Arthur J. Labovitz, MD | Tampa, FL | University of South Florida (4) | ||
| Michael Berlowitz, MD | Bonnie J. Kirby, RN, MSN | |||
| Philip Rogal, MD | Nhi N. Tran, MS | |||
| Christopher McFarren, MD | Catherine Jahrsdorfer, RN, BSN | |||
| Fadi Matar, MD | ||||
| Christiano Caldeira, MD | ||||
| David J. Maron, MD | Stanford, CA | Stanford University School of Medicine (4) | ||
| Fatima Rodriguez, MD, MPH | Reem Yunis, PhD | |||
| Ingela Schnittger, MD | Jhina Patro | |||
| William F. Fearon, MD | ||||
| Prakash Deedwania, MD | Antonia Vega | Fresno, CA | UCSF‐Fresno Community Regional Medical Center (4) | |
| Kiran Reddy, MD | ||||
| Joseph Sweeny, MD | Hugo Bloise‐Adames | New York, NY | Icahn School of Medicine at Mount Sinai (4) | |
| Santa Jimenez | ||||
| Nicole Saint Vrestil | ||||
| Reyna Bhandari | ||||
| Christopher Spizzieri, MD | Danielle Schade | Camp Hill, PA | Holy Spirit Hospital Cardiovascular Institute (4) | |
| Roxanne Yost | ||||
| Claudia P Hochberg, MD | Paula Beardsley | Boston, MA | Boston Medical Center (4) | |
| Denise Fine | ||||
| William D. Salerno, MD | Jana Tancredi, RN, MA/MSN, CCRN | Saddle Brook, NJ | Hackensack University Medical Center (4) | |
| Patricia Arakelian | ||||
| Susan Mathus | ||||
| Deborah O'Neill | ||||
| Ray Wyman, MD | Joy Burkhardt, CCRP | Torrance, CA | Torrance Memorial Medical Center (4) | |
| Suellen Hosino, RN, BSN, CCRP | ||||
| Oksana A. Lubyanaya, BA | Santa Ana, CA | Coastal Heart Medical Group (4) | ||
| Jose D. Salas, BS | ||||
| Amer Zarka, MD | Maria Aguirre | |||
| Anil V. Shah, MD | Manu Dhawan | |||
| Diana Parra | ||||
| Tri Tran | ||||
| Thomas Haldis, DO | Catherine Weick, BSRT(R)(VI) | Fargo, ND | Sanford Health (4) | |
| Katie Fowler‐Lehman, BSN | ||||
| Natalie Spitzer, BSN | ||||
| Casey Riedberger | ||||
| Catherine Weick | ||||
| Jeffrey A. Kohn, MD | Stanley E. Cobos, BA | New York, NY | NYU New York Medical Associates (4) | |
| Raven R. Dwyer, MPH | ||||
| Dalisa Espinosa, MBS | ||||
| Kirsten J. Quiles, MS | ||||
| Saket Girotra, MD | Carrie Drum, RN | Iowa City, IA | University of Iowa Hospitals and Clinics (4) | |
| Kimberly Miller‐Cox, RN | ||||
| Amy Ollinger, RN | ||||
| Omar Almousalli, MD | Elizabeth Capasso‐Gulve | Fairview Heights, IL | Advanced Heart Care Group (4) | |
| Alaine Melanie Loehr | ||||
| Marlowe Mosley | ||||
| Mayil S. Krishnam, MD | Shirin Heydari, MS | Orange, CA | University of California Irvine Medical Center (3) | |
| Jeffrey C. Milliken, MD | Andrea M. Lundeen, MA | |||
| Pranav M. Patel, MD | Edgar Karanjah, MD | |||
| Arnold H. Seto, MD | Wanda C. Marfori, MD | |||
| Kevin T. Harley, MD | Eduardo Hernandez‐Rangel, MD | |||
| Michael A. Gibson, MD | Pam Singh | |||
| Byron J. Allen, MD | ||||
| Rita Coram, MD | Anne Marie Webb, BSN | Louisville, KY | University of Louisville (3) | |
| Ellie Fridell, BS | ||||
| Heidi Wilson, BS | ||||
| Sabu Thomas, MD, MSc | Angela Kim, BS | Rochester, NY | University of Rochester (3) | |
| Ronald G Schwartz, MD, MS | Patrick Wilmot, BS | |||
| Wei Chen, MD, MS | ||||
| Mahfouz El Shahawy, MD | Ramona Stevens | Sarasota, FL | Cardiovascular Center of Sarasota (3) | |
| James Stafford, MD | Loriane Black | Baltimore, MD | University of Maryland Medical Center (3) | |
| William B. Abernethy, MD | Amber B. Hull, RN | Asheville, NC | Asheville Cardiology Associates (3) | |
| Olivia J. Lim, RN | ||||
| Helen C. Tucker | ||||
| Natasha C. Putnam, RN | ||||
| Linda L. Hall | ||||
| Tia Cauthren | ||||
| Trish Tucker | ||||
| Andrew Zurick, MD | Hollie Horton | Nashville, TN | Saint Thomas Hospital (3) | |
| Jan Orga | ||||
| Thomas M. Meyer, MD | Joyce R. White, MSN NP‐C | Lynchburg, VA | Stroobants Cardiovascular Center (3) | |
| Ronald G. Morford, MD | Cynthia Baumann, RN | |||
| Bruce Rutkin, MD | Vidya Seeratan | Manhasset, NY | Northwell Health‐Manhasset (3) | |
| Sabahat Bokhari, MD | Magnolia Jimenez | New York, NY | Columbia University Medical Center (3) | |
| Seth I. Sokol, MD | Cidney Schultz, RN | Bronx, NY | Jacobi Medical Center (3) | |
| Jay Meisner, MD | Jeanne Russo, RN | |||
| Ihab Hamzeh, MD | Houston, TX | Baylor College of Medicine (3) | ||
| Arunima Misra, MD | Zohra Huda, RN, BSN, CCRP | |||
| Matthew Wall Jr., MD | Araceli Boan | |||
| Veronica Lenges De Rosen, MD | ||||
| Mahboob Alam, MD | ||||
| Michael C. Turner, MD | Christine R Hinton | Lake Charles, LA | Cardiovascular Specialists of Southwest Louisiana (3) | |
| Thomas J. Mulhearn, MD | ||||
| Arnold P. Good, MD | Beth A. Archer, BSN, RN | Columbus, OH | Ohio Health Grant Medical Center (3) | |
| Julia S. Dionne, BA | ||||
| Cheryl A. Allardyce, BSN, RN | ||||
| Lindsey N. Sikora, BSN, RN | ||||
| Jennifer H. Czerniak, RN | ||||
| Jennifer A. Mull, MSN, RN | ||||
| Elizabeth Ferguson | ||||
| Frances Laube | ||||
| Nicolas W. Shammas, MD, MS | Gail A Shammas, BSN, RN | Davenport, IA | Midwest Cardiovascular Research Foundation (3) | |
| Lori Christensen | ||||
| Holly Park | ||||
| Robert Chilton, MD | Joan Hecht | San Antonio, TX | Audie Murphy V.A. (2) | |
| Patricia K. Nguyen, MD | Davis Vo, BS | Palo Alto, CA | VA Palo Alto Healthcare System (2) | |
| James Hirsch | ||||
| Matthew Jezior, MD | Jody Bindeman | Bethesda, MD | Walter Reed National Military Medical Center (2) | |
| Sara Salkind | ||||
| Dalisa Espinosa, MBS | Providence, RI | Miriam Hospital (2) | ||
| Lori‐Ann Desimone, BSN | ||||
| Paul C. Gordon, MD | Lina Felix‐Stern | |||
| Thomas Crain, MD | Jassira Gomes | |||
| Catherine Gordon, BSN | ||||
| Robert Stenberg, MD | Aimee Mann | Johnstown, PA | Conemaugh Valley Memorial Hospital (2) | |
| Theresa McCreary | ||||
| Ronald P. Pedalino, MD | Stanley E. Cobos, BA | Brooklyn, NY | NYU‐HHC Kings County Hospital Center (2) | |
| Raven R. Dwyer, MPH | ||||
| Dalisa Espinosa, MBS | ||||
| Kirsten J. Quiles, MS | ||||
| Joseph Wiesel, MD | Stanley E. Cobos, BA | Flushing, NY | New York University ‐ Langone Cardiovascular Associates (2) | |
| Raven R. Dwyer, MPH | ||||
| Dalisa Espinosa, MBS | ||||
| Kirsten J. Quiles, MS | ||||
| George J. Juang, MD | Candace Gopaul, BS | Brooklyn, NY | Coney Island Hospital (2) | |
| Karen Hultberg | ||||
| Tauqir Huk | ||||
| Afshan Hussain | ||||
| Mohammed Al‐Amoodi, MD | Yesenia Zambrano, BS | Yuma, AZ | Yuma Regional Medical Center (2) | |
| Sarah Medina Rodriguez | ||||
| Trudie Milner | ||||
| David Wohns, MD | Abbey Mulder, RN | Grand Rapids, MI | Spectrum Health (2) | |
| Stacie Van Oosterhout, MEd | ||||
| Ellis W. Lader, MD | Martha Meyer, RN, MSN | Kingston, NY | Mid Valley Cardiology (1) | |
| Michael Mumma, MD | Nancy L. Clapp, RN, BA, CCRC | Sarasota, FL | Sarasota Memorial Hospital (1) | |
| Heather Barrentine | ||||
| Lekshmi Dharmarajan, MD | Jenne M. Jose, PA | Bronx, NY | NYU‐HHC Lincoln Medical and Mental Health Center (1) | |
| Stanley E. Cobos, BA | ||||
| Raven R. Dwyer, MPH | ||||
| Dalisa Espinosa, MBS | ||||
| Kirsten J. Quiles, MS | ||||
| Jenne Manchery | ||||
| Joseph F.X. McGarvey Jr, MD | Vera McKinney, RN | Doylestown, PA | Doylestown Health Cardiology (1) | |
| Linda Schwarz, RN | ||||
| Thomas R. Downes, MD (till Dec. 2016) | Scott M. Kaczkowski | Loveland, CO | Medical Center of the Rockies (1) | |
| Gary J. Luckasen, MD (from Dec. 2016) | Adam J. Jaskowiak | |||
| Joel Klitch | ||||
| Benjamin Cheong, MD | Debra Dees | Houston, TX | Baylor St. Luke's Medical Center (1) | |
| Srinivasa Potluri, MD | Precilia Vasquez | Plano, TX | Baylor Research Institute at Legacy Heart Center (1)† | |
| Ronald A. Mastouri, MD | Indianapolis, IN | Indiana University/Krannert Institute of Cardiology (1) | ||
| Jeffery A. Breall, MD, PhD | Elise L. Hannemann, RN,CCRC | |||
| George E. Revtyak, MD | Judy Mae Foltz, RN,CCRC | |||
| Jonathan W. Bazeley, MD | ||||
| Dayuan Li, MD | Emily DeRosa | St. Paul, MN | HealthEast Saint Joseph's Hospital (1) | |
| Beth Jorgenson | ||||
| Joyce Riestenberg‐Smith | ||||
| Kenneth Giedd, MD | New York, NY | Beth Israel Medical Center (1) | ||
| Wayne Old, MD | Rebecca Bariciano | Chesapeake, VA | Cardiovascular Associates, Ltd (1) | |
| Francis Burt, MD | Bethlehem, PA | Saint Luke's Hospital and Health Network (1) | ||
| Kozhaya Sokhon, MD | Jessica Waldron | Sugar land, TX | Medicus Alliance Clinical Research Org, Inc (1) | |
| Michelle Mayon | ||||
| Deepika Gopal, MD | Plano, TX | The Heart Hospital Baylor (1) | ||
| Uma S. Valeti, MD | Gretchen Ann Peichel, RN | Minneapolis, MN | University of Minnesota (1) | |
| Jon Kobashigawa, MD | Brandy Starks | Beverly Hills, CA | Cedars Sinai Medical Center (1) | |
| Lucilla Garcia | ||||
| Maria Thottam | ||||
| India (941) | ||||
| Country Leader | ||||
| Balram Bhargava, DM | ||||
| Anjali Anand, MSc | Calicut | Government Medical College (208) | ||
| Sajeev Chakanalil Govindan, MD, DNB, DM, PhD | Janitha Raj, B.Tech | |||
| Rajesh Gopalan Nair, MD, DNB, DM | Reshma Ravindran, MSc | |||
| Rajalekshmi VS, MSc, MScCRRA | ||||
| Cholenahally Nanjappa Manjunath, MD, DM | Nandita Nataraj, BE(Biotech) PGDICRCDM | Bengaluru | Sri Jayadeva Institute of Cardiovascular Sciences and Research (149) | |
| Nagaraja Moorthy, MD, DM | Soundarya Nayak, BE(Biotech) PGDICRCDM | |||
| Satvic Cholenahally Manjunath, MD,DM | Mahevamma Mylarappa, GNM (General Nursing) | |||
| Suryaprakash Narayanappa, MBBS | ||||
| Neeraj Pandit, MD, DM | Sheromani Bajaj | New Delhi | Dr Ram Manohar Lohia Hospital (101) | |
| Ranjit Kumar Nath, MD, DM | Vandana Yadav, Msc,PGDACR | |||
| Girish Mishra, Msc, PGDACR | ||||
| S.K. Dwivedi, DM | Roma Tewari, PG | Lucknow | King George's Medical University, Department of Cardiology (100) | |
| V.S. Narain, DM | Meenakshi Mishra, PG | |||
| Sharad Chandra, DM | Shivali Patel | |||
| Suman Singh, PG | ||||
| Gurpreet S. Wander, DM | Ludhiana | Hero DMC Heart Institute, Dayanand Medical College and Hospital (83) | ||
| Rohit Tandon, MD | ||||
| Sarju Ralhan, M.Ch (CTVS) | Baljeet Kaur, MSc (Biotechnology) | |||
| Naved Aslam, DM | Sonika Gupta, MBA, B. Pharmacy | |||
| Abhishek Goyal, DM | ||||
| Balram Bhargava, DM | Chandini Suvarna, BDS | New Delhi | All India Institute of Medical Sciences (67) | |
| G.Karthikeyan, DM | ||||
| S.Ramakrishnan, DM | ||||
| Sandeep Seth, DM | ||||
| Rakesh Yadav, DM | ||||
| Sandeep Singh, DM | ||||
| Ambuj Roy, DM | ||||
| Neeraj Parakh, DM | ||||
| Sunil Kumar Verma, DM | ||||
| Rajiv Narang, DM | ||||
| Sundeep Mishra, DM | ||||
| Nitish Naik, DM | ||||
| Gautam Sharma, DM | ||||
| Shiv Kumar Choudhary, M.Ch | ||||
| Chetan Patel, DNB | ||||
| Gurpreet Gulati, MD | ||||
| Sanjeev Sharma, MD | ||||
| V. K. Bahl, DM | ||||
| Anoop Mathew, MD | Binoy Mannekkattukudy Kurian | Kolenchery | MOSC Medical College Hospital (39) | |
| Eapen Punnoose, MD | ||||
| Milind Avdhoot Gadkari, MD | Sheetal Rupesh Karwa, BHMS | Pune | KEM Hospital Pune (35) | |
| Siddharth Gadage, MD DNB | Suvarna Kolhe, MSc | |||
| Tapan Umesh Pillay, BHMS MSc | ||||
| Santhosh Satheesh, MBBS, MD, DM | R. J. Vindhya, B.Sc. (Bio‐Technology), MSc(Bio‐Informatics) | Pondicherry | Jawaharlal Institute of Postgraduate Medical Education and Research (31) | |
| Peeyush Jain, MD | New Delhi | Fortis Escort Heart Institute | ||
| Ashok Seth, MD | −31 | |||
| Zile Singh Meharwal, MD | ||||
| Atul Mathur, MD | Atul Verma, MD | |||
| Upendra Kaul, MD | Mona Bhatia, MD | |||
| Ankush Sachdeva, MD | ||||
| Thounaojam Indira Devi, RN | ||||
| Nungshi Jungla, RN | ||||
| Johann Christopher, MD, DNB | K. Manjula Rani, MSc. | Hyderabad | Gurunanak CARE Hospital (27) | |
| Rajeev Menon, MD, DNB | M. Sowjanya Reddy, BSc | |||
| Nirmal Kumar, MD, DNB | K. Preethi, BSc | |||
| Abraham Oomman, MD, DM, DNB | Rinu R sidh, MSc(Clinical Research) | Chennai | Apollo Research and Innovation (23) | |
| Robert Mao, MD, DM | T. Ramakrishnan, B.Tech(Biotechnology) | |||
| Hilda Solomon, PhD | Rajesh Francis, MSc(Clinical Research) | |||
| Sudhir Naik, MD, DM | Vamshi Priya P., MSc | Hyderabad | Apollo Research and Innovations (13) | |
| Sajeeda Parveen Khan, MBBS, (Dip.Card) | ||||
| Johann Christopher, MD | Kotiboinna Preethi | Hyderabad | CARE Nampally (11) | |
| Nirmal Kumar, MD | ||||
| Purvez Grant, MD | Shweta Hande, BHMS, PGDCR | Pune | Ruby Hall Clinic, Grant Medical Foundation (10) | |
| Poonam Sonawane, B.ScMicrobiology, ACCR | ||||
| Ranjan Kachru, MD | Abhishek Dubey | New Delhi | Fortis Healthcare Fl.t Lt. Rajan Dhall Hospital (4) | |
| Kavita Rawat | ||||
| Ajit Kumar VK, MD, DM | Trivandrum | Sree Chitra Tirunal Institute for Medical Sciences and Technology (3) | ||
| Sanjay Ganapathi, MD, DM | ||||
| Jayakumar K, MS, M.Ch | Vineeth CP | |||
| Harikrishnan Sivadasanpillai, MD, DM | Manas Chacko, RN | |||
| Bijulal Sasidharan, MD, DM | Suresh Babu | |||
| Kapilamoorthy TR, MD | ||||
| Johann Christopher, MD | Sowjanya Reddy | Hyderabad | CARE Hospital (3) | |
| Praneeth Polamuri, MD | Manjula Rani | |||
| Upendra Kaul, MD | Priyadarshani Arambam | New Delhi | Batra Hospital and Medical Research Centre (3) | |
| Bebek Singh | ||||
| United Kingdom (539) | ||||
| Country Leaders | ||||
| Roxy Senior, MBBS, MD, DM | ||||
| Keith AA Fox, MBChB (past) | ||||
| Country Coordinators | ||||
| Grace M. Young, MSc, BSc (Hons) | ||||
| Kathryn Carruthers (past) | ||||
| Roxy Senior, MBBS, MD, DM | Harrow | Northwick Park Hospital Harrow/Royal Brompton Hospital London (202) | ||
| Ahmed Elghamaz, MB BCh | ||||
| Sothinathan Gurunathan, MBChB | ||||
| Nikolaos Karogiannis, MBBS | Grace M. Young, MSc, BSc (Hons) | |||
| Benoy N Shah, MD, MBBS, BSc (Hons) | Christopher Kinsey | |||
| Richard HJ Trimlett, MBBS, CCST | Raisa Kavalakkat, MSc, BSc, RN | |||
| Michael B Rubens, LRCP, MRCS, MBBS, DMRD | Jo Evans, RN | |||
| Edward D Nicol, MD, BMedSci, MBBS, DTM&H | Ikraam Hassan, RN | |||
| Tarun K Mittal, MD | ||||
| Reinette Hampson, BSc (Hons), BA (Hons) | ||||
| Reto Andreas Gamma, MBBS | Sarah Williams, RN | Chelmsford | Broomfield Hospital (39) | |
| Kim Holland, RN | ||||
| Karen Swan, RN | ||||
| Mark A de Belder, MD | Bev Atkinson, RN | Middlesbrough | The James Cook University Hospital, Middlesbrough (37) | |
| Jeet Thambyrajah, MD | ||||
| Thuraia Nageh, BSc(Hons) MBBS MD MRCP | Swapna Kunhunny, MRes Clin Res, BSc (N), RN | Westcliffe on Sea | Southend University Hospital (34) | |
| John R Davies, MBBS, PhD | ||||
| Steven J. Lindsay, MD | Craig Atkinson, RN | Bradford | Bradford Royal Infirmary (20) | |
| John Kurian, MD | Carita Krannila, RN | |||
| Haqeel Jamil, MD | Manitha Vinod, RN | |||
| Osama Raheem, MD | ||||
| Angela Hoye, MD | Lisa Chaytor | Cottingham | The University of Hull/Castle Hill Hospital (19) | |
| Leanne Cox | ||||
| Julie Morrow | ||||
| Kay Rowe | ||||
| Patrick Donnelly, MD | Stephanie Kelly, RN | Belfast | South Eastern Health and Social Care (17) | |
| Bernardas Valecka, MD | Susan Regan, RN | |||
| Dawn Turnbull | ||||
| Anoop Chauhan, MD | Catherine Fleming | Blackpool | Blackpool Teaching Hospitals (16) | |
| Arijit Ghosh | ||||
| Karen Gratrix | ||||
| Stephen Preston | ||||
| Craig Barr, MD | Anne Cartwright | Dudley | Russells Hall Hospital (15) | |
| Khaled Alfakih, MBBS, MD | Abigail Knighton, BSc., PG Dip. | London | King's College NHS Foundation Hospital (14) | |
| Jonathan Byrne, PhD | Katherine Martin, RGN, Dip. N, MSc | |||
| Ian Webb, PhD, MA | ||||
| Peter Henriksen, PhD, MB ChB, BSc(Hons) | Laura Flint, RGN | Edinburgh | Royal Infirmary of Edinburgh (13) | |
| James Harrison, BSc(Hons), PG dip | ||||
| Peter OKane, MD | Nicki Lakeman | Bourneouth | Royal Bournemouth Hospital (13) | |
| Anja Ljubez | ||||
| Ramesh de Silva, MB ChB, MD | Bedford | Bedford Hospital NHS Trust (11) | ||
| Dwayne S. G. Conway, MD | Judith Wright | Wakefield | Pinderfields Hospital (11) | |
| Donna Exley | ||||
| Alexander A Sirker, MB BChir, PhD | London | |||
| Mervyn Andiapen, RN | University College London Hospitals NHS Foundation Trust | |||
| Amy J. Richards, BSc | BartsHealth NHS Trust | |||
| BartsHealth NHS Trust (11) | ||||
| Stephen P. Hoole, MD | Lisa Wong, MSc | Cambridge | Papworth Hospital (10) | |
| Fraser N. Witherow, MD | Melanie J. Munro, RGN | Dorchester | Dorset County Hospital (8) | |
| Nicola Johnston, MB, Bch BAO, MRCP, MD | Belfast | Belfast Trust (7) | ||
| Mark Harbinson, MB, Bch BAO, MRCP, MD | Michelle McEvoy, RN | |||
| Simon Walsh, MB, Bch BAO, MD | Caroline Brown, RN | |||
| Hanna Douglas, MB, Bch BAO, MRCP, MD | ||||
| Matthew Luckie, MD | Thabitha Charles | Manchester | Central Manchester University Hospital (7) | |
| Laurel Kolakaluri | ||||
| Hannah Phillips | ||||
| Jolanta Sobolewska, MD | Louise Morby, RN | Oldham | The Pennine Acute Hospitals NHS Trust (6) | |
| Karen Hallett, RN | ||||
| Carolyn Corbett, RN | ||||
| Lynne Winstanley | ||||
| Paramjit Jeetley, MD | Angelique Smit, RN | London | Royal Free London NHS Foundation Trust (6) | |
| Niket Patel, MD | ||||
| Tushar Kotecha, MBChB, Mpharm | ||||
| Christopher Travill, MBBS, MD | Susan Gent, SRN RGN | Luton | Luton and Dunstable University Hospital NHS FT (5) | |
| Iqbal Karimullah, MBBS | Nafisa Hussain, BSc | |||
| Mahmud Al‐Bustami, MBBS | ||||
| Denise Braganza, MD | Fiona Haines | Peterborough | Peterborough City Hospital (5) | |
| Joanne Taaffe | ||||
| Robert Henderson, MD | Jane Burton | Nottingham | Nottingham University Hospitals (4) | |
| Kate Pointon, MBBS | Maria Colton | |||
| Surendra Naik, PhD | Rachel King | |||
| Thomas Mathew, MBBS, MD, DM | ||||
| Ammani Brown, MSc BA RN | Clydebank | University of Glasgow (4) | ||
| Andrew Docherty, RN | ||||
| Colin Berry, BSc MB ChB, PhD | Lisa McCloy, RN | |||
| Damien Collison, MB ChB | Kate Robb, RN | |||
| Giles Roditi, MB ChB | Craig Paterson, PhD | |||
| Wenda Crawford, RN | ||||
| Joanne Kelly, RN | ||||
| Lorraine McGregor, RN | ||||
| Andrew J Moriarty, BSc MB PhD | Anne Mackin, RN, BSc | Craigavon | Cardiovascular Research Unit, Craigavon Area Hospital (2) | |
| Jason D. Glover, MBBS | Janet P Knight, RN | Basingstoke | Hampshire Hospitals NHS Foundation Trust (2) | |
| Jiwan Pradhan, MBBS | ||||
| Ghada Mikhail, MD | Tuhina Bose | London | Imperial College Healthcare NHS Trust (1) | |
| Darrel P. Francis, MD, MA | ||||
| Canada (447)* | ||||
| Country Leaders | ||||
| Vladimir Dzavik, MD | ||||
| Shaun Goodman, MD, MSc | ||||
| Gilbert Gosselin, MD | ||||
| Gilbert Gosselin, MD | Anna Proietti, RN | Montreal, QC | Montreal Heart Institute (90) | |
| Myriam Brousseau, RN | ||||
| Magalie Corfias, RN | ||||
| Patricia Blaise | ||||
| Luc Harvey | ||||
| Ariel Diaz, MD | Trois‐Rivieres, QC | Centre Hospitalier de Regional Trois‐Rivieres (71) | ||
| Philippe Rheault, MD | ||||
| Miguel Barrero, MD | ||||
| Carl‐Éric Gagné, MD | Patricia Alarie | |||
| Yanek Pépin‐Dubois, MD | Linda Arcand | |||
| Ricardo Costa, MD | Isabelle Roy | |||
| Ying Tung Sia, MD | Estelle Montpetit | |||
| Catherine Lemay, MD | ||||
| Alejandro Gisbert, MD | ||||
| Pierre Gervais, MD | ||||
| Alain Rheault, MD | ||||
| Katia Drouin, RN | Terrebonne, QC | CISSSL‐Hopital Pierre‐Le Gardeur (42) | ||
| Denis Carl Phaneuf, MD | Christine Bergeron, RN | |||
| Gilbert Gosselin, MD | Christine Shelley | |||
| Christine Masson | ||||
| Pallav Garg, MBBS, MSc | Sandy Carr, RN | London, ON | London Health Sciences Centre (35) | |
| Catherine Bone, RN | ||||
| Benjamin J.W. Chow, MD | Ermina Moga | Ottawa, ON | University of Ottawa Heart Institute (29) | |
| Renee C. Hessian, MD | Janetta Kourzenkova | |||
| Rob S. Beanlands, MD | Olga Walter | |||
| Richard F. Davies, MD | ||||
| Kevin R. Bainey, MD, MSc | Norma Hogg, RN | Edmonton, AB | University of Alberta (28) | |
| Suzanne Welsh, RN | ||||
| Asim N. Cheema, MD, PhD | Toronto, ON | St. Michael's Hospital (27) | ||
| Akshay Bagai, MD, MHS | ||||
| Ron Wald, MDCM, MPH | ||||
| Shaun Goodman, MD, MSc | Khrystyna Kushniriuk, HBSc, MD | |||
| John Joseph Graham, MRCP, MB ChB, BSc | Mohammed Hussain | |||
| Mark Peterson, MD, FRCSC, PhD | Olugbenga Bello | |||
| Chi‐Ming Chow, MD, CM, MSc | ||||
| Beth Abramson, MD, MSc | ||||
| Asim Nazir Cheema, MD | Ishba Syed, MBBS | Mississauga, ON | Dixie Medical Group (24) | |
| Mohammad Tariq Vakani, MD | Mohammed Hussain, BSc(H) | |||
| Khrystyna Kushniriuk, MBBS | ||||
| James Cha, MD | Judy Otis, CRC | Oshawa, ON | Dr James Cha (21) | |
| Rebecca Otis, CRC | ||||
| Andrew G Howarth, MD, PhD | Michelle M Seib, RN | Calgary, AB | University of Calgary (15) | |
| Sandra M Rivest, RN | ||||
| Rosa Sandonato, BSCN | ||||
| Graham Wong, MD | Jackie Chow | Vancouver, BC | Vancouver General Hospital (15) | |
| Andrew Starovoytov | ||||
| Naomi Uchida | ||||
| Ngaire Meadows | ||||
| Amar Uxa, MD | Nadia Asif | Toronto, ON | University Health Network (14) | |
| Suzana Tavares | ||||
| Paul Galiwango, MD | Bev Bozek, RN, CCRC | Scarborough, ON | Scarborough Cardiology Research (9) | |
| Saleem Kassam, MD | Maria Shier | |||
| Ashok Mukherjee, MD | Lori‐Ann Larmand | |||
| A. Joseph Ricci, MD | Amir Janmohamed | |||
| Brenda Hart | ||||
| Andy Lam, MD | Jane Marucci | East Grimsby, ON | West Lincoln Memorial Hospital (8) | |
| Sharon Tai | ||||
| Shamir Mehta, MD | Sonya Brons, RN | Hamilton, ON | Hamilton General Hospital (7) | |
| Chris Beck, RN | ||||
| Glenda Wong, RN | ||||
| Krystal Etherington | ||||
| Thippeekaa Arumairajah | ||||
| Jacob Udell, MD | Maria Aprile | Toronto, ON | Women's College Hospital (7) | |
| Sara Karlsson | ||||
| Susan Webber | ||||
| Philippe Généreux, MD | Chantale Mercure | Montréal, QC | Centre Intégré Universitaire de Santé et de Services Sociaux du Montréal (2) | |
| Adnan Hameed, MD | Nancy Aedy | St. Catharines, ON | Saint Catharines General Hospital (2) | |
| Ledjalem Daba, MD | Fran Farquharson | Vaughan, ON | Northwest GTA Cardiovascular and Heart Rhythm Program (1) | |
| Anam Siddiqui | ||||
| Brazil (399) | ||||
| Country Leaders | ||||
| Antonio Carlos Carvalho, MD, PhD | ||||
| Renato D. Lopes, MD, PhD | ||||
| Whady Hueb, MD | Myrthes Emy Takiuti, RN | São Paulo | Heart Institute (InCor) University of São Paulo (127) | |
| Paulo Cury Rezende, MD | ||||
| Expedito Eustáquio Ribeiro Silva, MD | ||||
| Alexandre Ciappina Hueb, MD | ||||
| Paola Emanuela Poggio Smanio, MD, PhD | Leonardo Pizzol Caetano, PhD | São Paulo | Instituto Dante Pazzanese de Cardiologia (98) | |
| Alexandre Schaan de Quadros, MD | Porto Alegre | Instituto de Cardiologia de Porto Alegre (41) | ||
| Renato Abdala Karam Kalil, MD | Aline Peixoto Deiro | |||
| José Luiz da Costa Vieira, MD | Alice Manica Muller | |||
| Gabriel Grossmann, MD | Maria Antonieta Pereira de Moraes | |||
| Pedro Píccaro de Oliveira, MD | Bruna Maria Ascoli | |||
| Leonardo Bridi, MD | Sílvia Zottis Poletti | |||
| Simone Savaris, MD | ||||
| João V Vitola, MD, PhD | Curitiba | Quanta Diagnostico and Terapia (33) | ||
| Rodrigo J Cerci, MD, Msc | Sandra S. Zier, BSc | |||
| Fabio R Farias, MD, Msc | Vilmar Veiga, Jr, BSc | |||
| Miguel M Fernandes, MD, PhD | ||||
| José Antonio Marin‐Neto, MD, PhD | Ribeirao Preto | Hospital das Clinicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (31) | ||
| André Schmidt, MD, PhD | ||||
| Moysés de Oliveira Lima Filho, MD, PhD | Diego Franca da Cunha | |||
| Ricardo Mendes Oliveira, MD | ||||
| João Reynaldo Abbud Chierice, MD | ||||
| Carísi A. Polanczyk, MD | Guilherme G Rucatti, PsyD | Porto Alegre | Hospital de Clínicas de Porto Alegre | |
| Mariana V. Furtado, MD | Fernanda Igansi, BSc | Hospital de Clínicas de Porto Alegre (12) | ||
| Luis F. Smidt, MD | Mauren P Haeffner, BSc | |||
| Antonio Carlos Carvalho, MD | Viviane Almeida | Sao Paulo | Unifesp‐Hospital São Paulo (9) | |
| Gustavo Pucci, MD | Gabriela Sanchez de Souza | |||
| Flavio Lyra, MD | ||||
| Alvaro Rabelo Alves Junior, MD | Mayana Almeida | Salvador | Fundacao Bahiana de Cardilogia (9) | |
| Viviane dos Santos | ||||
| Marianna D. A. Dracoulakis, MD, PhD | Natalia S Oliveira, RN | Salvador | Hospital da Bahia (8) | |
| Rodolfo G. S. D Lima, MD | ||||
| Estevao Figueiredo, MD | Bruna Edilena Paulino Azevedo | Belo Horizonte | Hospital Lifecenter (8) | |
| Paulo Ricardo Caramori, MD | Marco Bizzaro Santos | Porto Alegre | Hospital Sao Lucas da Pontificia Universidade Catolica do Rio Grande do Sol (7) | |
| Amanda Germann | ||||
| Vitor Gomes | ||||
| Rosa Homem | ||||
| Ellen Magedanz | ||||
| Rogerio Tumelero, MD | Rosane Laimer | Fundo | Hospital Sao Vicente de Paulo (5) | |
| Alexandre Tognon | ||||
| Frederico Dall'Orto, MD | Pocos de Caldas | Hospital Maternidade e Pronto Socorro Santa Lucia (4) | ||
| Claudio T. Mesquita, MD | Roberta P Santos, RN | Botafogo | Hospital Pró‐Cardíaco (3) | |
| Alexandre S. Colafranseschi, MD | ||||
| Amarino C. Oliveira Jr., MD | ||||
| Luiz A. Carvalho, MD | ||||
| Isabella C. Palazzo, MD | ||||
| Andre S. Sousa, MD | ||||
| Expedito Eustáquio Ribeiro da Silva, MD, PhD | São Paulo | Hospital TotalCor (2) | ||
| Pedro Gabriel Melo de Barros e Silva, MD, PhD | Mariana Yumi Okada, RN | |||
| Luciana de Pádua Silva Baptista, MD, PhD | Ana Paula Batista, RN | |||
| Marcelo Jamus Rodrigues, MD | Aline Nogueira Rabaça, BS | |||
| Marcos Valério Coimbra de Resende, MD, PhD | ||||
| Jose Francisco Saraiva, MD | Larissa Miranda Trama | Sao Paulo | Hospital Celso Pierro (1) | |
| Talita Silva | ||||
| Camila Thais de Souza Ormundo | ||||
| Carla Vicente | ||||
| Costantino Costantini, MD, PhD | Caroline Pinheiro | Curitiba | Hospital Cardiologico Costantini (1) | |
| Daniele Komar | ||||
| Poland (333) | ||||
| Country Leaders | ||||
| Witold Ruzyllo, MD | ||||
| Hanna Szwed, MD, PhD | ||||
| Country Coordinator | ||||
| Radoslaw Pracon, MD, PhD | ||||
| Marcin Demkow, MD, PhD | Warsaw | Coronary and Structural Heart Diseases Department, Institute of Cardiology (127) | ||
| Radoslaw Pracon, MD, PhD | ||||
| Cezary Kepka, MD PhD | ||||
| Anna Teresinska, MD PhD | Olga Walesiak | |||
| Karolina Kryczka, MD PhD | Katarzyna Malinowska | |||
| Jan Henzel, MD PhD | ||||
| Mateusz Solecki, MD PhD | ||||
| Edyta Kaczmarska, MD PhD | ||||
| Tomasz Mazurek, MD, PhD | Jakub Maksym, MD | Warszawa | Medical University of Warsaw (48) | |
| Karolina Wojtera, MD | ||||
| Anna Fojt, MD | ||||
| Ewa Szczerba, MD | ||||
| Jaroslaw Drozdz, PhD | Lodz | Cardiology Clinic, Medical University in Lodz (43) | ||
| Bartosz Czarniak, MD | ||||
| Malgorzata Frach (formerly Stasiak), MD | ||||
| Konrad Szymczyk, MD | ||||
| Iwona Niedzwiecka, MD | ||||
| Sebastian Sobczak, MD | ||||
| Tomasz Ciurus, MD | ||||
| Piotr Jakubowski, MD | ||||
| Magdalena Misztal‐Teodorczyk, MD | ||||
| Dawid Teodorczyk, MD | Marta Swiderek, MA | |||
| Aleksandra Fratczak, MD | Ewelina Wojtala, MA | |||
| Marcin Szkopiak, MD | ||||
| Patrycja Lebioda, MD | ||||
| Michal Wlodarczyk, MD | ||||
| Anna Plachcinska, MD | ||||
| Jacek Kusmierek, MD | ||||
| Magdalena Miller, MD | ||||
| Halina Marciniak, MD | ||||
| Karolina Wojtczak‐Soska, MD | ||||
| Katarzyna Łuczak, MD | ||||
| Tomasz Tarchalski, MD | ||||
| Anna Cichocka‐Radwan, MD | ||||
| Hanna Szwed, MD, PhD | Jaroslaw Karwowski, MD | Warsaw | National Institute of Cardiology, Warsaw (35) | |
| Grazyna Anna Szulczyk, MD | ||||
| Adam Witkowski, MD, PhD | Warsaw | Department of Interventional Cardiology and Angiology, Institute of Cardiology (20) | ||
| Krzysztof Kukuła, MD, PhD | ||||
| Małgorzta Celińska‐Spodar, MD | ||||
| Joanna Zalewska, MD | ||||
| Grzegorz Gajos, MD, PhD | Krakow | Department of Coronary Disease, John Paul II Hospital, Jagiellonian University Medical College (16) | ||
| Krzysztof Bury, MD, PhD | ||||
| Piotr Pruszczyk, MD, PhD | Andrzej Łabyk, MD | Warszawa | Department of Internal Medicine and Cardiology, Infant Jesus Teaching Hospital, Medical University of Warsaw (15) | |
| Marek Roik, MD, PhD | Agnieszka Szramowska, MD | |||
| Olga Zdończyk, MD | ||||
| Krystyna Łoboz‐Grudzień, MD, PhD | Joanna Jaroch, MD, PhD | Wrocław | T.Marciniak Hospital (11) | |
| Leszek Sokalski, MD, PhD | ||||
| Barbara Brzezińska, MD, PhD | ||||
| Maciej Lesiak, Professor, MD | Poznan | Szpital Kliniczny Przemienienia Pańskiego (10) | ||
| Magdalena Łanocha, MD | ||||
| Krzysztof W. Reczuch, MD | Adam Kolodziej, MD | Wroclaw | Military Hospital/Medical University (4) | |
| Zbigniew Kalarus, MD | Zabrze | Medical University of Silesia, School of Medicine with the Division of Dentistry, Department of Cardiology, Congenital Heart Diseases and Electrotherapy, Silesian Center for Heart Diseases (3) | ||
| Andrzej Swiatkowski, MD | ||||
| Mariola Szulik, MD | ||||
| Wlodzimierz J. Musial, MD | Marta Marcinkiewicz‐Siemion, MD | Bialystok | University Hospital in Bialystok (1) | |
| Russia (303) | ||||
| Country Coordinator | ||||
| Olga Bockeria, MD, PhD | ||||
| Leo Bockeria, MD, PhD | Olga Bockeria, MD, PhD | Moscow | National Medical Research Center for Cardiovascuar Surgery (113) | |
| Karen Petrosyan, MD, PhD | Zalina Kudzoeva, MD | |||
| Tatiana Trifonova, MD | Nodira Aripova, MD | |||
| Alexander M. Chernyavskiy, MD, PhD | Ivan A. Naryshkin, MD | Novosibirsk | E.Meshalkin National Medical Research Center of the Ministry of Health of the Russian Federation (101) | |
| Evgeniy I. Kretov, MD | Alena Kuleshova, MD | |||
| Igor O. Grazhdankin, MD | Dastan Malaev, MD | |||
| Leonid L. Bershtein, MD, PhD | Saint Petersburg | North‐Western State Medical University (50) | ||
| Sergey A. Sayganov, MD, PhD | Irina Subbotina | |||
| Anastasia M. Kuzmina‐Krutetskaya, MD | Victoria Gumerova | |||
| Elizaveta V. Zbyshevskaya, MD, PhD | ||||
| Nana O. Katamadze, MD, PhD | ||||
| Elena A. Demchenko, MD, PhD | Olga B. Nikolaeva, MD | Saint Petersburg | Federal Almazov North‐West Medical Research Centre (39) | |
| Pavel S. Kozlov, MD | ||||
| Vikentiy Y. Kozulin, MD | ||||
| Ekaterina I. Lubinskaya, MD | ||||
| Spain (286)* | ||||
| Country Leader | ||||
| Jose Luis Lopez‐Sendon, MD, PhD | ||||
| Country Coordinator | ||||
| Almudena Castro, MD | ||||
| Jose Lopez‐Sendon, MD, PhD | Virginia Fernández‐Figares, Pharm | Madrid | Hospital La Paz. IdiPaz (118) | |
| Almudena Castro, MD | ||||
| Elena Refoyo Salicio, MD | ||||
| Gabriela Guzman, MD | ||||
| Gabriel Galeote, MD | ||||
| Silvia Valbuena, MD | ||||
| Jesús Peteiro, MD, PhD | A Coruna | Complexo Hospitalario Universitario A Coruña Sergas, Department of Cardiology. INIBIC A Coruña. CIBER‐CV. Universidad de A Coruña, Spain (112) | ||
| María Dolores Martínez‐Ruíz, MD | ||||
| Ruth Pérez‐Fernández, MD | Moisés Blanco‐Calvo, PhD | |||
| José J Cuenca‐Castillo, MD | Encarnación Alonso‐Álvarez, BSc | |||
| Xacobe Flores‐Ríos, MD | Paula García‐González, BSc | |||
| Óscar Prada‐Delgado, MD | ||||
| Gonzalo Barge‐Caballero, MD | ||||
| Jose Ramon Gonzalez Juanatey, MD, PhD | Jose Seijas Amigo, Pharm | Santiago de Compostela | Hospital Clinico Universitario de Santiago (17) | |
| Miguel Souto Bayarri, MD, PhD | ||||
| Virginia Pubull Nuñez, MD | ||||
| Raymundo Ocaranza Sanchez, MD, PhD | ||||
| Belen Cid Alvarez, MD | ||||
| Carlos Peña Gil, MD, PhD | ||||
| Amparo Martinez Monzonis, MD | ||||
| Alessandro Sionis, MD | Ana Fernández Martínez, RN | Barcelona | Hospital de la Santa Creu i Sant Pau (11) | |
| Montserrat Vila Perales, MD | ||||
| Josep Maria Padró, MD | ||||
| Antonio Serra Peñaranda, MD | ||||
| Joan García Picart, MD | ||||
| Antonino Ginel Iglesias, MD | ||||
| Xavier Garcia‐Moll Marimon, MD | ||||
| Guillem Pons Lladó, MD | ||||
| Francesc Carreras Costa, MD | ||||
| Vicente Miro, MD | Begoña Igual, MD | Valencia | Hospital Universitario y Politecnico La Fe (10) | |
| Jose L Diez, MD | ||||
| Pilar Calvillo, MD | ||||
| F. Marin Ortuño, MD, PhD | Murcia | HUVA, Hospital Clínico Universitario Virgen De La Arrixaca (8) | ||
| M. Valdés Chávarri, MD, PhD | M. Quintana Giner, MD | |||
| A. Tello Montolliu, MD, PhD | A.I. Romero Aniorte, MD | |||
| E. Pinar Bermudez, MD, PhD | JM. Rivera Caravaca, MD | |||
| G. De La Morena, MD, PhD | ||||
| Montserrat Gracida Blancas, MD | Olga Cañavate | Barcelona | Hospital De Bellvitge (4) | |
| Sonia Guerrero | ||||
| Silvia Riera | ||||
| Jose Enrique Castillo Luena, MD | Jose Enrique Castillo Luena | Zaragoza | Hospital Universitario Miguel Servet (4) | |
| Maria Lasala | ||||
| Francisco Fernandez‐Aviles, MD | Maria Lorenzo | Madrid | Hospital General Universitario Gregorio Maranon (2) | |
| Olga Sobrino | ||||
| Alexandra Vazquez | ||||
| China (246) | ||||
| Country Leader | ||||
| Lixin Jiang, MD, PhD | ||||
| Jiyan Chen, MD | Haojian Dong | Guangzhou | Guangdong General Hospital (102) | |
| Peiyu He | ||||
| Chunli Xia | ||||
| Junqing Yang | ||||
| Qi Zhong | ||||
| Yongjian Wu, MD, PhD | Yanmeng Tian, MD | Beijing | Chinese Academy of Medical Sciences, Fuwai Hospital (17) | |
| Dongze Li | Urumqi | First Affiliated Hospital of Xinjiang Medical University (15) | ||
| Yitong Ma, MD | Xiaomei Li | |||
| Yining Yang, MD | Xiang Ma | |||
| Zixiang Yu | ||||
| Qian Zhao | ||||
| Zheng Ji, MD | Chunguang Li | Tangshan | Tangshan Gongren Hospital (15) | |
| Lei Zhang | ||||
| Yu Zhao | ||||
| Bolin Zhu | ||||
| Xinchun Yang, MD | Mulei Chen | Beijing | Beijing Chao‐yang Hospital, Capital Medical University (12) | |
| Hongjie Chi | ||||
| Yang Wang | ||||
| Jing Zhang | ||||
| Wenhua Lin, MD | Rui Jing | Tianjing | TEDA International Cardiovascular Hospital (12) | |
| Jingjing Liu | ||||
| Hesong Zeng, MD | Qiang Zhou, MD | Wuhan | Tongji Medical College (11) | |
| Chang Xu, MD | ||||
| Zhuxi Li, MD | ||||
| Junhua Li, MD | ||||
| Luyang Xiong, MD | ||||
| Xin Fu, MD | Dan Gao | Zhengzhou | The First Affiliated Hospital of Zhengzhou University (11) | |
| Dengke Jiang | ||||
| Ran Leng | ||||
| Xutong Wang | ||||
| Qianqian Yuan | ||||
| Lili Zhang | ||||
| Bin Yang, MD | Ziliang Bai | Taiyuan | Shanxi Cardiovascular Hospital (10) | |
| Jianhua Li | ||||
| Jie Qi | ||||
| Fei Wang | ||||
| Haitao Wang | ||||
| Bin Yang | ||||
| Zhou Yue | ||||
| Zhulin Zhang | ||||
| Songtao Wang, MD | Yumei Dong | Qingdao | Qingdao Fuwai Hospital (8) | |
| Jiajia Mao | ||||
| Bin Zhang | ||||
| Gong Cheng, MD | Xiuhong Li | Xian | Shanxi Provincial People's Hospital (6) | |
| Xiaowei Yao | ||||
| Nier Zhong | ||||
| Ning Zhou | ||||
| Yulan Zhao, MD | Yaping Huang, MS | Zhengzhou | The Second Affiliated Hospital of Zhengzhou University (6) | |
| Panpan Zhou, MS | ||||
| Xuehua Fang, MD | Wei Su | Beijing | Liangxiang Hospital, Beijing Fangshan District (6) | |
| Qiutang Zeng, MD | Yu Kunwu | Wuhan | Wuhan Union Hospital, Tongji Medical College, Huazhong Science and Tech University (3) | |
| Yudong Peng | ||||
| Xin Su | ||||
| Xi Su, MD | Chen Wang | Wuhan | Wuhan Asia Heart Hospital (3) | |
| Yunhai Zhao | ||||
| Qingxian Li, MD | Yaming Geng | Jining | Affiliated Hospital of Jining Medical University (3) | |
| Yanfu Wang | ||||
| Shao‐ping Nie, MD, PhD | Jing‐yao Fan, MD | Beijing | Beijing Anzhen Hospital (2) | |
| Si‐ting Feng, MD,PhD | ||||
| Xiao Wang, MD,PhD | ||||
| Yan Yan, MD,PhD | ||||
| Hui‐min Zhang, MD,PhD | ||||
| Qin Yu, MD | Lingping Chi | Dalian | Affiliated Zhongshan Hospital of Dalian University (2) | |
| Fang Liu | ||||
| Jian'an Wang, MD | Han Chen | Hangzhou | The Second Affiliated Hospital Zhejiang University School of Medicine (1) | |
| Jun Jiang | ||||
| Huajun Li | ||||
| Jian'an Wang | ||||
| Yechen Han, MM | Beijing | Peking Union Medical College Hospital (1) | ||
| Lihong Xu, RN | ||||
| Shuyang Zhang, MD, PhD | Zhenyu Liu | |||
| Zhenyu Liu, MD | Gang Chen | |||
| Rongrong Hu | ||||
| Italy (139)* | ||||
| Country Leader | ||||
| Aldo P. Maggioni, MD | ||||
| Gian Piero Perna, MD | Francesca Pietrucci, PhD | Ancona | Cardiology and CCU‐Ospedali Riuniti Ancona (54) | |
| Marco Marini, MD | ||||
| Gabriele Gabrielli, MD | ||||
| Stefano Provasoli, MD | Anna Di Donato | Varese | Ospedale di Circolo e Fondazione Macchi (23) | |
| Edoardo Verna, MD | ||||
| Lorenzo Monti, MD | Rozzano | Humanitas Research Hospital, Rozzano (MI) (17) | ||
| Barbara Nardi, MD | ||||
| Antonio Di Chiara, MD | Francesca Pezzetta, MD | Tolmezzo | Azienda Servizi Sanitaria n.3 Alto Friuli‐Collinare‐Medio Friuli (9) | |
| Andrea Mortara, MD | Valentina Casali, MD | Monza | Policlinico di Monza, Monza MB (8) | |
| Marcello Galvani, MD | Chiara Attanasio | Forli | Ospedale “G.B. Morgagni–L. Pierantoni” Forli (AUSL della Romagna) (8) | |
| Filippo Ottani, MD | ||||
| Marco Sicuro, MD | Gianpiero Leone, MD | Aosta | Ospedale Regionale Umberto Parini (5) | |
| Francesco Pisano, MD | ||||
| Cristina Bare, BSc | ||||
| Paolo Calabro, MD | Fabio Fimiani | Napoli | AORN Dei Colli “V. Monaldi” UOC Cardiologia Università della Campania “L.Vanvitelli” (4) | |
| Tiziana Formisano, MD | ||||
| Giuseppe Tarantini, MD | Alberto Barioli, MD | Padua | University of Padua‐Cardiology Clinic (3) | |
| Umberto Cucchini, MD | Federica Ramani | |||
| Anto Luigi Andres, MD | ||||
| Emanuela Racca, MD | Fabrizio Rolfo, MD | Cuneo | Azienda Ospedaliera S. Croce e Carle (3) | |
| Cecilia Goletto | ||||
| Carlo Briguori, MD | Francesca De Micco | Naples | Clinica Mediterranea (2) | |
| Roberto Amati, MD | Stefano Di Marco, MD | Pescia | UO Cardiologia Ospedale SS Cosma e Damiano (2) | |
| William Vergoni, MD | Martina Tricoli | |||
| Aldo Russo, MD | Massimo Villella, MD | San Giovanni Rotondo | IRCCS “Casa Sollievo della Sofferenza” (1) | |
| Raffaele Fanelli, MD | ||||
| Singapore (61)* | ||||
| Country Leader | ||||
| Harvey Douglas White, MD | ||||
| Country Coordinator | ||||
| Caroline Alsweiler | ||||
| Kian‐Keong Poh, MD | Singapore | National University Heart Center Singapore (33) | ||
| Ping Chai, MD | ||||
| Titus Lau, MD | ||||
| Joshua P. Loh, MD | ||||
| Edgar L. Tay, MD | ||||
| Kristine Teoh, MD | Sik‐Yin V Tan, BSc | |||
| Lynette L. Teo, MD | Winnie C Sia, BSc | |||
| Ching‐Ching Ong, MD | Audrey W Leong, BSc | |||
| Raymond C. Wong, MD | ||||
| Poay‐Huan Loh, MD | ||||
| Theodoros Kofidis, MD | ||||
| Wan Xian Chan, MD | ||||
| Koo Hui Chan, MD | ||||
| David Foo, MBBS | Li Hai Yan, RN | Singapore | Tan Tock Seng Hospital (22) | |
| Jason Loh Kwok Kong, MD | ||||
| Ching Min Er, MD | ||||
| Fahim Haider Jafary, MD | ||||
| Terrance Chua, MD | Nasrul Ismail | Singapore | National Heart Centre Singapore (6) | |
| Min Tun Kyaw | ||||
| Deborah Yip | ||||
| Germany (54) | ||||
| Country Leader | ||||
| Rolf Doerr, MD | ||||
| Rolf Doerr, MD | Dresden | Praxisklinik Herz und Gefaesse (29) | ||
| Juergen Stumpf, MD | Dorit Grahl | |||
| Klaus Matschke, MD, PhD | Franziska Guenther | |||
| Gregor Simonis, MD, PhD | Kerstin Bonin | |||
| Clemens T. Kadalie, MD | ||||
| Udo Sechtem, MD | Ina Wenzelburger | Stuttgart | Robert‐Bosch‐Krankenhaus (22) | |
| Peter Ong, MD | Susanne Gruensfelder, RN | |||
| P. Christian Schulze, MD, PhD | Jena | University Hospital Jena (2) | ||
| Bjoern Goebel, MD | ||||
| Karsten Lenk, MD | ||||
| Georg Nickenig, MD | Jan‐Malte Sinning, MD | Bonn | Universitatsklinikum Bonn (1) | |
| Marcel Weber, MD | ||||
| Nikos Werner, MD | ||||
| Austria (50) | ||||
| Country Leaders | ||||
| Irene Marthe Lang, MD | ||||
| Kurt Huber, MD | ||||
| Herwig Schuchlenz, MD | Gudrun Steinmaurer | Graz | LKH Graz West Austria (35) | |
| Stefan Weikl, MD | ||||
| Irene Marthe Lang, MD | Max‐Paul Winter, MD | Vienna | Medical University of Vienna, Department of Cardiology (8) | |
| Tijana, Andric, MD | Vienna | Wilhelminen Hospital Vienna (7) | ||
| Kurt Huber, MD | Maximilian, Tscharre, MD | |||
| Gabriele, Jakl‐Kotauschek, MD | Claudia, Wegmayr, MSc | |||
| Bernhard, Jäger, MD | ||||
| Florian, Egger, MD | ||||
| Hungary (49) | ||||
| Country Leader | ||||
| Matyas Keltai, MD, PhD, DSc | ||||
| Andras Vertes, MD | Judit Sebo, MD | Budapest | Eszszk‐ Szent Istvan Hospital (20) | |
| Zoltan Davidovits, MD | ||||
| Laszlone Matics | ||||
| Albert Varga, MD, PhD | Gergely Ágoston, MD | Szeged | University of Szeged (12) | |
| Geza Fontos, MD | Gabor Dekany, MD | Budapest | George Gottsegen National Institute of Cardiology (9) | |
| Bela Merkely, MD, PhD, DSc | Andrea Bartykowszki, MD | Budapest | Heart and Vascular Center, Semmelweis University (8) | |
| Pal Maurovich‐Horvat, MD, PhD, MPH | ||||
| Gabor Kerecsen, MD | Agnes Jakal | Budapest | Military Hospital, Budapest (1) | |
| Serbia (47) | ||||
| Sasa Hinic, MD, BSc | Jelena Djokic, MD | Belgrade | University Hospital Center Bezanijska Kosa (13) | |
| Marija Zdravkovic, MD, PhD | ||||
| Vladan Mudrenovic, MD | ||||
| Bogdan Crnokrak, MD | ||||
| Branko D. Beleslin, MD, PhD | Belgrade | Faculty of Medicine, University of Belgrade; Cardiology Clinic, Clinical Center of Serbia (10) | ||
| Nikola N. Boskovic, MD | Ana D. Djordjevic‐Dikic, MD, PhD | |||
| Marija T. Petrovic, MD | Vojislav L. Giga, MD, PhD | |||
| Milan R. Dobric, MD | Jelena J. Stepanovic, MD, PhD | |||
| Zeljko Z. Markovic, MD, PhD | ||||
| Ana S. Mladenovic, MD, PhD | ||||
| Nada Cemerlic‐Adjic, MD | Lazar Velicki, MD | Sremska Kamenica | Institute of Cardiovascular Diseases Vojvodina, Sremska Kamenica, Serbia and Faculty of Medicine, University of Novi Sad (9) | |
| Ljiljana Pupic | ||||
| Goran Davidović, MD, PhD | Stefan M. Simović, MD | Kragujevac | Clinical Center Kragujevac (7) | |
| Rada Vučić, MD | ||||
| Milica Nikola Dekleva, MD PhD | Miroslav Stevo Martinovic, MD | Belgrade | University Clinical Hospital Zvezdara (6) | |
| Gordana Stevanovic | ||||
| Goran Stankovic, MD | Milan Dobric | Belgrade | Clinical Center of Serbia (1) | |
| Svetlana Apostolovic, MD | Sonja Salinger Martinovic | Nis | Clinic for Cardiovascular Diseases, Clinical Center Nis (1) | |
| Dragana Stanojevic | ||||
| Mexico (46) | ||||
| Jorge Escobedo, MD | Ramon de Jesús‐Pérez, RN | Benito Juarez | Instituto Mexicano del Seguro Social (35) | |
| Rubén Baleón‐Espinosa, MD | ||||
| Arturo S Campos‐Santaolalla, MD | ||||
| Elihú Durán‐Cortés, MD | ||||
| José M Flores‐Palacios, MD | ||||
| Andrés García‐Rincón, MD | ||||
| Moisés Jiménez‐Santos, MD | ||||
| Joaquín V Peñafiel, MD | ||||
| José A Ortega‐Ramírez, MD | ||||
| Aquiles Valdespino‐Estrada, MD | ||||
| Erick Alexánderson Rosas, MD | María Fernanda Canales Brassetti, MD | Mexico City | Instituto Nacional de Cardiología “Ignacio Chávez” (11) | |
| Diego Adrián Vences Anaya, MD | ||||
| María Pérez García | ||||
| Isabel Estela Carvajal Juarez, MD | ||||
| Magdalena Madero Rovalo, MC | ||||
| Erick Donato Morales Rodríguez, MD | ||||
| Australia (45) | ||||
| Country Leaders | ||||
| Joseph B. Selvanayagam, MBBS (Hons), DPhil | ||||
| Jamie Rankin, MBBS (past) | ||||
| Country Coordinator | ||||
| Deirdre Murphy | ||||
| Joseph B. Selvanayagam, MBBS (Hons), DPhil | Sau Lee, PhD | Adelaide | Flinders Medical Centre (30) | |
| Majo X. Joseph, MBBS | Prince Thomas, RN | |||
| Suku T. Thambar, MBBS | Melissa D Chaplin, RN | New Lambton Heights | John Hunter Hospital (8) | |
| Stephanie C Boer, B Biotechnology (Honors) | ||||
| John F. Beltrame, MD | Jeanette K. Stansborough, RN | Woodville South | The Queen Elizabeth Hospital (5) | |
| Marilyn Black, RN | ||||
| Graham S. Hillis, PhD | Michelle M. Bonner, B. Nursing | Perth | Royal Perth Hospital (2) | |
| Kim F. Ireland, RN | ||||
| Clare Venn‐Edmonds, RN | ||||
| France (42) | ||||
| Country Leader | ||||
| Philippe‐Gabriel Steg, MD | ||||
| Country Coordinators | ||||
| Helene Abergel | ||||
| Jean‐Michel Juliard | ||||
| Corine Thobois, RN | Chartres | C.H. Louis Pasteur (21) | ||
| Christophe Thuaire, MD | Emilie Tachot, RN | |||
| Téodora Dutoiu, MD | Christophe Laure, RN | |||
| Christel Vassaliere, RN | ||||
| Philippe Gabriel Steg, MD | Helene Abergel, MSc | Paris | Bichat Hospital (9) | |
| Jean‐Michel Juliard, MD | Axelle Fuentes, MSc | |||
| Michel S. Slama, MD | Ludivine Eliahou, MD | Clamart Cedex | Antoine‐Beclere Hospital (5) | |
| Rami El Mahmoud, MD | Olivier Dubourg, MD | Boulogne | Ambroise Pare Hospital (2) | |
| Pierre Michaud, MD | ||||
| Eric Nicollet, MD | Sarah Hadjih | Corbeil‐Essonnes Cedex | Centre Hospitalier Sud Francilien (2) | |
| Pascal Goube, MD | Patricia Brito | |||
| Gilles Barone‐Rochette, MD | Gilles Barone‐Rochette | Grenoble | Grenoble University Hospital (2) | |
| Alain Furber, MD | Charles Cornet, MD, PhD | Angers Cedex 9 | Centre Hospitalier Universitaire d'Angers (1) | |
| Loïc Bière, MD | Jeremy Rautureau, MD, PhD | |||
| Lithuania (39) | ||||
| Agne Juceviciene, MD | Vilnius | Vilnius University Hospital Santariskes Clinic (39) | ||
| Irma Kalibataite‐Rutkauskiene, MD | ||||
| Laura Keinaite | ||||
| Aleksandras Laucevicius, MD | Monika Laukyte | |||
| Jelena Celutkiene, MD | Gelmina Mikolaitiene | |||
| Akvile Smigelskaite, MD | ||||
| Ilona Tamasauskiene, MD | ||||
| Agne Urboniene, MD | ||||
| Netherlands (37)* | ||||
| Elvin Kedhi MD, PhD | Zwolle | Isala Klinieken (25) | ||
| Jorik Timmer, MD | Ilse Bouwhuis | |||
| Rik Hermanides, MD | Lia Nijmeijer | |||
| Eliza Kaplan, MD | ||||
| Robert K. Riezebos, MD, PhD | Amsterdam | Cardio Research Hartcentrum OLVG (11) | ||
| Pouneh Samadi, MD | Jeannette, J. M. Schoep, RN | |||
| Elise van Dongen, MD | Elisabeth, M. Janzen, RN | |||
| Sander R. Niehe, MD | ||||
| Harry Suryapranata, MD | Sandra Ahoud | Nijmegen | Radboudumc (1) | |
| Stijn van Vugt, MD, PhD | ||||
| Portugal (33) | ||||
| Ruben Ramos, MD | Lisbon | Hospital de Santa Marta (25) | ||
| Duarte Cacela, MD | ||||
| Ana Santana, MD | ||||
| Antonio Fiarresga, MD | ||||
| Lidia Sousa, MD | ||||
| Hugo Marques, MD | ||||
| Lino Patricio, MD | Mafalda Selas | |||
| Luis Bernanrdes, MD | Filipa Silva | |||
| Pedro Rio, MD | Cláudia Freixo | |||
| Ramiro Carvalho, MD | ||||
| Rui Ferreira, MD | ||||
| Tiago Silva, MD | ||||
| Ines Rodrigues, MD | ||||
| Pedro Modas, MD | ||||
| Guilherme Portugal, MD | ||||
| Jose Fragata, MD | ||||
| Fausto J. Pinto, PhD | Inês Zimbarra Cabrita, PhD | Lisbon | Santa Maria University Hospital, Cardiology Department, CHLN (6) | |
| Miguel Nobre Menezes, MD | Andreia Rocha, MSc | |||
| Guilhermina Cantinho Lopes, MD | Francisca Patuleia Figueiras, PhD | |||
| Ana Gomes Almeida, PhD | Andreia Coelho, BSc | |||
| Pedro Canas Silva, MD | Marta Capinha | |||
| Angelo Nobre, MD | Maria Inês Caetano | |||
| Ana Rita Francisco, MD | Susana Silva | |||
| Nuno Ferreira, MD | Vila Nova de Gaia | Centro Hospitalar de Vila Nova de Gaia/Espinho, EPE (2) | ||
| Ricardo L. Lopes, MD | ||||
| Argentina (29) | ||||
| Country Leader | ||||
| Rafael Diaz, MD (past) | ||||
| Luis Guzman, MD | Veronica Tinnirello | Cordoba | Instituto Medico DAMIC (11) | |
| Julio César Figal, MD | Matías Nicolás Mungo | Ciudad Autonoma de Buenos Aires | Fundación Favaloro (10) | |
| Oscar Méndiz, MD | ||||
| Claudia Cortés, MD | ||||
| Roberto René Favaloro, MD | ||||
| Carlos Alvarez, MD | Marina Garcia | Bahia Blanca | Hospital Italiano Regional del Sur Bahia Blanca (3) | |
| Javier Courtis, MD | Valeria Godoy | Cordoba | Clinica Romagosa and Clinica De La Familia (2) | |
| Gabriela Zeballos, MD | ||||
| Lilia Schiavi, MD | Maria Victoria Actis | Cordoba | Clinica Del Prado (2) | |
| Mariano Rubio, MD | Graciela Scaro, MD | Cordoba | Clínica Privada Vélez Sarsfield (1) | |
| New Zealand (28)* | ||||
| Country Leader | ||||
| Harvey Douglas White, MD | ||||
| Country Coordinator | ||||
| Caroline Alsweiler | ||||
| Gerard Patrick Devlin, MD | Liz Low, RN | Hamilton | Waikato Hospital (22) | |
| Raewyn Fisher, MD | Jayne Scales, RN | |||
| Kirsty Abercrombie, RN | ||||
| Ralph Alan Huston Stewart, MCChB, MD | Leah Howell, RN | Auckland | Auckland City Hospital (6) | |
| Harvey Douglas White, MD | Cathrine Patten, RN | |||
| Jocelyne Benatar, MD | ||||
| Macedonia (28)* | ||||
| Sasko Kedev, MD, PhD | Skopje | University Clinic of Cardiology (28) | ||
| Irena Peovska Mitevska, MD, PhD | ||||
| Elizabeta Srbinovska Kostovska, MD, PhD | ||||
| Hristo Pejkov, MD, PhD | ||||
| Sweden (23)* | ||||
| Country Leader | ||||
| Claes Held, MD, PhD | ||||
| Claes Held, MD, PhD | Uppsala | Uppsala University (18) | ||
| Kai Eggers, MD, PhD | ||||
| Gunnar Frostfelt, MD, PhD | Christina Björklund, RN | |||
| Nina Johnston, MD, PhD | Maria Andreasson, RN | |||
| Maciej Olsowka, MD | Marie Essermark, RN | |||
| Axel Åkerblom, MD, PhD | ||||
| Inga Soveri, MD, PhD | ||||
| Johannes Aspberg, MD | Liselotte Persson | Stockholm | Karolinska Institutet at Danderyd Hospital (5) | |
| Israel (15) | ||||
| Country Leaders | ||||
| Rafael Beyar, MD, MD, DSc, MPH | ||||
| Tali Sharir, MD | ||||
| Country Coordinator | ||||
| Eugenia Nikolsky, MD | ||||
| Tali Sharir, MD | Or Harel, MA | Tel‐Aviv | Assuta Medical Centers (9) | |
| Dan Elian, MD | ||||
| Arthur Kerner, MD | Margalit Bentzvi | Haifa | Rambam Medical Center (6) | |
| Samia Massalha, MD | Ludmila Helmer | |||
| Japan (14) | ||||
| Country Leader | ||||
| Shun Kohsaka, MD | ||||
| Keiichi Fukuda, MD, PhD | Ikuko Ueda, PhD | Shinjuku‐ku | Keio University (7) | |
| Shun Kohsaka, MD | Jun Fujita, MD | |||
| Satoshi Yasuda, MD, PhD | Akemi Furukawa, RN | Suita‐shi | National Cerebral and Cardiovascular Center | |
| Kanae Hirase, RN | National Cerebral and Cardiovascular Center (4) | |||
| Toshiyuki Nagai, MD, PhD | ||||
| Fumiyuki Otsuka, MD, PhD | ||||
| Shigeyuki Nishimura, MD | Shintaro Nakano | Hidaka | Saitama Medical University (3) | |
| Belgium (7)* | ||||
| Country Leader | ||||
| Frans Van de Werf, MD, PhD | ||||
| Country Coordinator | ||||
| Kaatje Goetschalckx, MD | ||||
| Kaatje Goetschalckx, MD | Valerie Robesyn | Leuven | University Hospital Leuven (7) | |
| Frans Van de Werf, PhD, MD | ||||
| Kathleen Claes, PhD, MD | ||||
| Taiwan (7)* | ||||
| Country Leader | ||||
| Harvey Douglas White, MD | ||||
| Country Coordinator | ||||
| Caroline Alsweiler | ||||
| Chung‐Lieh Hung, MD | Yi‐Hsuan Yang | Taipei City | Mackay Memorial Hospital (7) | |
| Chun‐Ho Yun, MD | ||||
| Charles Jia‐Yin Hou, MD | ||||
| Jen‐Yuan Kuo, MD | ||||
| Hung‐I Yeh, MD, PhD | ||||
| Ta‐Chuan Hung, MD | ||||
| Jiun‐Yi Li, MD, PhD | ||||
| Chen‐Yen Chien, MD, PhD | ||||
| Cheng‐Ting Tsai, MD | ||||
| Chun‐Chieh Liu, MD | ||||
| Fa‐Chang Yu, MD | ||||
| Yueh‐Hung Lin, MD | ||||
| Wei‐Ren Lan, MD | ||||
| Chih‐Hsuan Yen, MD | ||||
| Jui‐Peng Tsai, MD | ||||
| Kuo‐Tzu Sung, MD | ||||
| South Africa (7)* | ||||
| Mpiko Ntsekhe, MD | Cape Town | Groote Schuur Hospital/University of Cape Town (7) | ||
| Shaheen Pandie, MD | Constance Philander (Nee Talliard), ND | |||
| Charle A Viljoen, MD | Noloyiso Mtana, RN | |||
| Marianne De Andrade, MD | ||||
| Switzerland (7)* | ||||
| Country Leader | ||||
| Aldo P. Maggioni, MD | ||||
| Tiziano Moccetti, MD | Adriana Anesini, RN | Lugano | Cardiocentro (7) | |
| M.Grazia Rossi, MD | Simona Maspoli, RN | |||
| Manuela Mombelli, RN | ||||
| Egypt (6) | ||||
| Magdy Abdelhamid, MD | Ahmed Talaat, MD | Cairo | Cairo University (6) | |
| Ahmed Adel, MD | ||||
| Ahmed Kamal, MsC | ||||
| Hossam Mahrous, MD | ||||
| Sameh El Kaffas, MD | ||||
| Hussien El Fishawy, MD | ||||
| Romania (5) | ||||
| Calin Pop, MD, PhD | Bucharest | Emergency County Hospital Baia Mare (4) | ||
| Matei Claudia, MD, PhD | ||||
| Bogdan A. Popescu, MD, PhD | Bucharest | Emergency Institute of Cardiovascular Diseases “Prof. Dr C. C. Iliescu” (1) | ||
| Carmen Ginghina, MD, PhD | Monica Rosca, MD, PhD | |||
| Dan Deleanu, MD, PhD | Carmen C. Beladan, MD, PhD | |||
| Vlad A. Iliescu, MD, PhD | ||||
| Saudi Arabia (5)* | ||||
| Mouaz H. Al‐Mallah, MD MSc | Sarah Zahrani, RN | Central Province | King AbdulAziz Cardiac Center (5) | |
| Ahmed Aljzeeri, MD | ||||
| Hani Najm, MD | ||||
| Ali Alghamdi, MD | ||||
| Peru (4)* | ||||
| Walter Enrique Mogrovejo Ramos, MD | Marco Antonio Monsalve Davila, RN | Mirafloes | Instituto Neuro Cardiovascular De Las Americas (4) | |
| Thailand (3) | ||||
| Country Leader | ||||
| Harvey Douglas White, MD | ||||
| Country Coordinator | ||||
| Caroline Alsweiler | ||||
| Srun Kuanprasert, MD | Chiang Mai | Maharaj Nakorn Chiang Mai Hospital (2) | ||
| Arintaya Prommintikul, MD | ||||
| Weerachai Nawarawong, MD | Supatchara Khwakhong, RN | |||
| Surin Woragidpoonpol, MD | Anong Chaiyasri, RN | |||
| Thitipong Tepsuwan, MD | Warangkana Mekara, RN | |||
| Noppon Taksaudom, MD | Supap Kulthawong, RN | |||
| Chataroon Rimsukcharoenchai, MD | Anong Amaritakomol, RN | |||
| Juntima Euathrongchit, MD | ||||
| Yutthaphan Wannasopha, MD | ||||
| Sukit Yamwong, MD | Pachara Panpunuan, RN | Bangkok | Ramathibodi Hospital (1) | |
| Piyamitr Sritara, MD | ||||
| Suthara Aramcharoen, MD | ||||
| Krissada Meemuk, MD | ||||
| Malaysia (2)* | ||||
| Country Leader | ||||
| Harvey Douglas White, MD | ||||
| Country Coordinator | ||||
| Caroline Alsweiler | ||||
| Ahmad Khairuddin, MD | Noor Syamira Mokhtar, RN | Kuala Lumpur | Institut Jantung Negara (2) | |
| Hafidz Abd Hadi, MD | Nor Asiah Basri, RN | |||
| Shaiful Azmi Yahaya, MD | Irni Yusnida, RN | |||
| Humayrah Hashim | ||||
Countries participated in Economics Quality of Life Questionnaires.
This site received 1 participant in transfer who was randomized at another site.
NHS, National Health Service; NIH, National Institutes of Health; PI, Primary Investigator; UAB, University of Alabama Birmingham; VA, Veterans Affairs; VAMC, Veterans Affairs Medical Center.
This article was sent to Saket Girotra, MD, SM, Associate Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.122.029850
For Sources of Funding and Disclosures, see page 45.
Contributor Information
Harmony R. Reynolds, Email: harmony.reynolds@nyulangone.org.
the ISCHEMIA Research Group:
Kreton Mavromatis, Jason Linefsky, Todd Miller, Subhash Banerjee, Harmony R. Reynolds, Jonathan D. Newman, Sripal Bangalore, Robert M. Donnino, Lawrence M. Phillips, Muhamed Saric, Khaled Abdul‐Nour, Peter H. Stone, James J. Jang, Gennie Yee, Steven Weitz, Suzanne Arnold, James Henry O’Keefe, Michael D. Shapiro, Mohammad El‐Hajjar, Mandeep S. Sidhu, Steven A. Fein, Mikhail T. Torosoff, Radmila Lyubarova, Sulagna Mookherjee, Krzysztof Drzymalski, Edward O. McFalls, Santiago A. Garcia, Stefan C. Bertog, Rizwan A. Siddiqui, Areef Ishani, Ronnell A. Hansen, Michel Georges Khouri, Jonathan L. Goldberg, Richard Goldweit, Ronny A. Cohen, Brooks Mirrer, Victor Navarro, David E. Winchester, Marvin Kronenberg, Philip Rogal, Christopher McFarren, John F. Heitner, Ira M. Dauber, Charles Cannan, Sriram Sudarshan, Puja K. Mehta, Michael McDaniel, Stamatios Lerakis, Arshed Quyyumi, Nanette K. Wenger, Chester M. Hedgepeth, Heather Hurlburt, Alan Rosen, Zakir Sahul, David Booth, Steve Leung, Ahmed Abdel‐Latif, Hassan Reda, Khaled Ziada, Sampoornima Setty, Rajat S. Barua, Fadi Hage, Christiano Caldeira, James E. Davies, Massoud Leesar, Jaekyeong Heo, Amy Iskandrian, Firas Al Solaiman, Satinder Singh, Khaled Dajani, Mohammad El‐Hajjar, Paul Der Mesropian, Joseph Sacco, Brian McCandless, Marisa Orgera, Mandeep S. Sidhu, Imran Arif, Hanan Kerr, Jorge F. Trejo (Gutierrez), Gerald Fletcher, Gary E. Lane, Lynn M. Neeson, Pragnesh P. Parikh, Peter M. Pollak, Brian P. Shapiro, Kevin Landolfo, Anthony Gemignani, Daniel O’Rourke, Judith L. Meadows, Jason T. Call, Joseph Hannan, Robert Bojar, Deepti Kumar, John Mukai, Edward T. Martin, Gabriel Vorobiof, Alec Moorman, Scott Kinlay, Robert J. Hamburger, Thomas P. Rocco, Deepak L. Bhatt, Kevin Croce, Jacquelyn A. Quin, Jati Anumpa, Marco Zenati, David P. Faxon, Glenn Rayos, Ashraf Seedhom, Lance Sullenberger, Gregory Kumkumian, Steven P. Sedlis, Robert M. Donnino, Jeffrey Lorin, Jacqueline E. Tamis‐Holland, Robert Kornberg, Robert Leber, Souheil Saba, Michael W. Lee, Delano R. Small, Wassim Nona, Patrick B. Alexander, Iram Rehman, Umesh Badami, Kevin Marzo, Inga H. Robbins, Howard A. Levite, Sanjay Shetty, Mayuri Patel, Glenn S. Hamroff, Raymond W. Little, Brandi D. Zimbelman, Charles Y. Lui, Brigham R. Smith, Daniel P. Vezina, Lillian L. Khor, Josephine D. Abraham, David A. Bull, Stephen H. McKellar, David Booth, John Kotter, Ahmed Abdel‐Latif, Bob Hu, Arthur J. Labovitz, Michael Berlowitz, Philip Rogal, Christopher McFarren, Fadi Matar, Christiano Caldeira, David J. Maron, Fatima Rodriguez, Ingela Schnittger, William F. Fearon, Prakash Deedwania, Kiran Reddy, Joseph Sweeny, Christopher Spizzieri, Claudia P. Hochberg, William D. Salerno, Ray Wyman, Amer Zarka, Anil V. Shah, Thomas Haldis, Jeffrey A. Kohn, Saket Girotra, Omar Almousalli, Mayil S. Krishnam, Jeffrey C. Milliken, Pranav M. Patel, Arnold H. Seto, Kevin T. Harley, Michael A. Gibson, Byron J. Allen, Rita Coram, Sabu Thomas, Ronald G. Schwartz, Wei Chen, Mahfouz El Shahawy, James Stafford, William B. Abernethy, Andrew Zurick, Thomas M. Meyer, Ronald G. Morford, Bruce Rutkin, Sabahat Bokhari, Seth I. Sokol, Jay Meisner, Ihab Hamzeh, Arunima Misra, Matthew Wall, Veronica Lenges De Rosen, Mahboob Alam, Michael C. Turner, Thomas J. Mulhearn, Arnold P. Good, Nicolas W. Shammas, Robert Chilton, Patricia K. Nguyen, Matthew Jezior, Paul C. Gordon, Thomas Crain, Robert Stenberg, Ronald P. Pedalino, Joseph Wiesel, George J. Juang, Mohammed Al‐Amoodi, David Wohns, Ellis W. Lader, Michael Mumma, Lekshmi Dharmarajan, Joseph F. X. McGarvey, Thomas R. Downes, Gary J. Luckasen, Benjamin Cheong, Srinivasa Potluri, Ronald A. Mastouri, Jeffery A. Breall, George E. Revtyak, Jonathan W. Bazeley, Dayuan Li, Kenneth Giedd, Wayne Old, Francis Burt, Kozhaya Sokhon, Deepika Gopal, Uma S. Valeti, Jon Kobashigawa, Sajeev Chakanalil Govindan, Rajesh Gopalan Nair, Cholenahally Nanjappa Manjunath, Nagaraja Moorthy, Satvic Cholenahally Manjunath, Suryaprakash Narayanappa, Neeraj Pandit, Ranjit Kumar Nath, S. K. Dwivedi, V. S. Narain, Sharad Chandra, Gurpreet S. Wander, Rohit Tandon, Sarju Ralhan, Naved Aslam, Abhishek Goyal, Balram Bhargava, G. Karthikeyan, S. Ramakrishnan, Sandeep Seth, Rakesh Yadav, Sandeep Singh, Ambuj Roy, Neeraj Parakh, Sunil Kumar Verma, Rajiv Narang, Sundeep Mishra, Nitish Naik, Gautam Sharma, Shiv Kumar Choudhary, Chetan Patel, Gurpreet Gulati, Sanjeev Sharma, V. K. Bahl, Anoop Mathew, Eapen Punnoose, Milind Avdhoot Gadkari, Siddharth Gadage, Tapan Umesh Pillay, Santhosh Satheesh, Atul Mathur, Upendra Kaul, Johann Christopher, Rajeev Menon, Nirmal Kumar, Abraham Oomman, Robert Mao, Hilda Solomon, Sudhir Naik, Sajeeda Parveen Khan, Johann Christopher, Nirmal Kumar, Purvez Grant, Ranjan Kachru, V. K. Ajit Kumar, Sanjay Ganapathi, K. Jayakumar, Harikrishnan Sivadasanpillai, Bijulal Sasidharan, T. R. Kapilamoorthy, Johann Christopher, Praneeth Polamuri, Upendra Kaul, Roxy Senior, Ahmed Elghamaz, Sothinathan Gurunathan, Nikolaos Karogiannis, Benoy N. Shah, Richard HJ Trimlett, Michael B. Rubens, Edward D. Nicol, Tarun K. Mittal, Reinette Hampson, Reto Andreas Gamma, Mark A. de Belder, Jeet Thambyrajah, Thuraia Nageh, John R. Davies, Steven J. Lindsay, John Kurian, Haqeel Jamil, Osama Raheem, Angela Hoye, Patrick Donnelly, Bernardas Valecka, Anoop Chauhan, Craig Barr, Khaled Alfakih, Jonathan Byrne, Ian Webb, Peter Henriksen, Peter OKane, Ramesh de Silva, Dwayne S. G. Conway, Alexander A Sirker, Stephen P. Hoole, Fraser N. Witherow, Nicola Johnston, Mark Harbinson, Simon Walsh, Hanna Douglas, Matthew Luckie, Jolanta Sobolewska, Paramjit Jeetley, Niket Patel, Tushar Kotecha, Christopher Travill, Iqbal Karimullah, Mahmud Al‐Bustami, Denise Braganza, Robert Henderson, Kate Pointon, Surendra Naik, Thomas Mathew, Colin Berry, Damien Collison, Giles Roditi, Andrew J. Moriarty, Jason D. Glover, Jiwan Pradhan, Ghada Mikhail, Darrel P. Francis, Gilbert Gosselin, Ariel Diaz, Philippe Rheault, Miguel Barrero, Carl‐Éric Gagné, Yanek Pépin‐Dubois, Ricardo Costa, Ying Tung Sia, Catherine Lemay, Alejandro Gisbert, Pierre Gervais, Alain Rheault, Denis Carl Phaneuf, Gilbert Gosselin, Pallav Garg, Benjamin J. W. Chow, Renee C. Hessian, Rob S. Beanlands, Richard F. Davies, Kevin R. Bainey, Asim N. Cheema, Akshay Bagai, Ron Wald, Shaun Goodman, John Joseph Graham, Mark Peterson, Chi‐Ming Chow, Beth Abramson, Asim Nazir Cheema, Mohammad Tariq Vakani, James Cha, Andrew G Howarth, Graham Wong, Amar Uxa, Paul Galiwango, Saleem Kassam, Ashok Mukherjee, A. Joseph Ricci, Andy Lam, Shamir Mehta, Jacob Udell, Philippe Généreux, Adnan Hameed, Ledjalem Daba, Whady Hueb, Paulo Cury Rezende, Expedito Eustáquio Ribeiro Silva, Alexandre Ciappina Hueb, Paola Emanuela Poggio Smanio, Alexandre Schaan de Quadros, Renato Abdala Karam Kalil, José Luiz da Costa Vieira, Gabriel Grossmann, Pedro Píccaro de Oliveira, Leonardo Bridi, Simone Savaris, João V. Vitola, Rodrigo J. Cerci, Fabio R. Farias, Miguel M. Fernandes, José Antonio Marin‐Neto, André Schmidt, Moysés de Oliveira Lima Filho, Ricardo Mendes Oliveira, João Reynaldo Abbud Chierice, Carísi A. Polanczyk, Mariana V. Furtado, Luis F. Smidt, Antonio Carlos Carvalho, Gustavo Pucci, Flavio Lyra, Alvaro Rabelo Alves Junior, Marianna D. A. Dracoulakis, Rodolfo G. S. D Lima, Estevao Figueiredo, Paulo Ricardo Caramori, Rogerio Tumelero, Frederico Dall’Orto, Claudio T. Mesquita, Alexandre S. Colafranseschi, Amarino C. Oliveira, Luiz A. Carvalho, Isabella C. Palazzo, Andre S. Sousa, Expedito Eustáquio Ribeiro da Silva, Pedro Gabriel Melo de Barros, Luciana de Pádua Silva Baptista, Marcelo Jamus Rodrigues, Marcos Valério Coimbra de Resende, Jose Francisco Saraiva, Costantino Costantini, Marcin Demkow, Radoslaw Pracon, Cezary Kepka, Anna Teresinska, Karolina Kryczka, Jan Henzel, Mateusz Solecki, Edyta Kaczmarska, Tomasz Mazurek, Jaroslaw Drozdz, Bartosz Czarniak, Malgorzata Frach, Konrad Szymczyk, Iwona Niedzwiecka, Sebastian Sobczak, Tomasz Ciurus, Piotr Jakubowski, Magdalena Misztal‐Teodorczyk, Dawid Teodorczyk, Aleksandra Fratczak, Marcin Szkopiak, Patrycja Lebioda, Michal Wlodarczyk, Anna Plachcinska, Jacek Kusmierek, Magdalena Miller, Halina Marciniak, Karolina Wojtczak‐Soska, Katarzyna Luczak, Tomasz Tarchalski, Anna Cichocka‐Radwan, Hanna Szwed, Grazyna Anna Szulczyk, Adam Witkowski, Krzysztof Kukula, Malgorzta Celinska‐Spodar, Joanna Zalewska, Grzegorz Gajos, Krzysztof Bury, Piotr Pruszczyk, Marek Roik, Krystyna Loboz‐Grudzien, Leszek Sokalski, Barbara Brzezinska, Maciej Lesiak, Magdalena Lanocha, Krzysztof W. Reczuch, Zbigniew Kalarus, Andrzej Swiatkowski, Mariola Szulik, Wlodzimierz J. Musial, Leo Bockeria, Karen Petrosyan, Tatiana Trifonova, Alexander M. Chernyavskiy, Evgeniy I. Kretov, Igor O. Grazhdankin, Leonid L. Bershtein, Sergey A. Sayganov, Anastasia M. Kuzmina‐Krutetskaya, Elizaveta V. Zbyshevskaya, Nana O. Katamadze, Elena A. Demchenko, Pavel S. Kozlov, Vikentiy Y. Kozulin, Ekaterina I. Lubinskaya, Jose Lopez‐Sendon, Almudena Castro, Elena Refoyo Salicio, Gabriela Guzman, Gabriel Galeote, Silvia Valbuena, Jesús Peteiro, María Dolores Martínez‐Ruíz, Ruth Pérez‐Fernández, José J. Cuenca‐Castillo, Xacobe Flores‐Ríos, Óscar Prada‐Delgado, Gonzalo Barge‐Caballero, Jose Ramon Gonzalez Juanatey, Miguel Souto Bayarri, Virginia Pubull Nuñez, Raymundo Ocaranza Sanchez, Belen Cid Alvarez, Carlos Peña Gil, Amparo Martinez Monzonis, Alessandro Sionis, Montserrat Vila Perales, Josep Maria Padró, Antonio Serra Peñaranda, Joan García Picart, Antonino Ginel Iglesias, Xavier Garcia‐Moll Marimon, Guillem Pons Lladó, Francesc Carreras Costa, Vicente Miro, Jose L. Diez, Pilar Calvillo, F. Marin Ortuño, M. Valdés Chávarri, A. Tello Montolliu, E. Pinar Bermudez, G. De La Morena, Montserrat Gracida Blancas, Jose Enrique Castillo Luena, Francisco Fernandez‐Aviles, Jiyan Chen, Yongjian Wu, Yitong Ma, Yining Yang, Zheng Ji, Xinchun Yang, Wenhua Lin, Hesong Zeng, Xin Fu, Bin Yang, Songtao Wang, Gong Cheng, Yulan Zhao, Xuehua Fang, Qiutang Zeng, Xi Su, Qingxian Li, Shao‐ping Nie, Qin Yu, Jian’an Wang, Shuyang Zhang, Zhenyu Liu, Gian Piero Perna, Marco Marini, Gabriele Gabrielli, Stefano Provasoli, Edoardo Verna, Lorenzo Monti, Barbara Nardi, Antonio Di Chiara, Andrea Mortara, Marcello Galvani, Filippo Ottani, Marco Sicuro, Paolo Calabro, Tiziana Formisano, Giuseppe Tarantini, Umberto Cucchini, Anto Luigi Andres, Emanuela Racca, Carlo Briguori, Roberto Amati, William Vergoni, Aldo Russo, Raffaele Fanelli, Kian‐Keong Poh, Ping Chai, Titus Lau, Joshua P. Loh, Edgar L. Tay, Kristine Teoh, Lynette L. Teo, Ching‐Ching Ong, Raymond C. Wong, Poay‐Huan Loh, Theodoros Kofidis, Wan Xian Chan, Koo Hui Chan, David Foo, Jason Loh Kwok Kong, Ching Min Er, Fahim Haider Jafary, Terrance Chua, Rolf Doerr, Juergen Stumpf, Klaus Matschke, Gregor Simonis, Clemens T. Kadalie, Udo Sechtem, Peter Ong, P. Christian Schulze, Bjoern Goebel, Karsten Lenk, Georg Nickenig, Herwig Schuchlenz, Stefan Weikl, Irene Marthe Lang, Kurt Huber, Gabriele Jakl‐Kotauschek, Andras Vertes, Albert Varga, Geza Fontos, Bela Merkely, Gabor Kerecsen, Sasa Hinic, Marija Zdravkovic, Vladan Mudrenovic, Bogdan Crnokrak, Branko D. Beleslin, Nikola N. Boskovic, Marija T. Petrovic, Milan R. Dobric, Zeljko Z. Markovic, Ana S. Mladenovic, Nada Cemerlic‐Adjic, Goran Davidovic, Rada Vucic, Milica Nikola Dekleva, Goran Stankovic, Svetlana Apostolovic, Jorge Escobedo, Rubén Baleón‐Espinosa, Arturo S. Campos‐Santaolalla, Elihú Durán‐Cortés, José M. Flores‐Palacios, Andrés García‐Rincón, Moisés Jiménez‐Santos, Joaquín V. Peñafiel, José A. Ortega‐Ramírez, Aquiles Valdespino‐Estrada, Erick Alexánderson Rosas, Joseph B. Selvanayagam, Majo X. Joseph, Suku T. Thambar, John F. Beltrame, Graham S. Hillis, Christophe Thuaire, Téodora Dutoiu, Philippe Gabriel Steg, Jean‐Michel Juliard, Michel S. Slama, Rami El Mahmoud, Eric Nicollet, Pascal Goube, Gilles Barone‐Rochette, Alain Furber, Loïc Bière, Aleksandras Laucevicius, Jelena Celutkiene, Elvin Kedhi, Jorik Timmer, Rik Hermanides, Eliza Kaplan, Robert K. Riezebos, Pouneh Samadi, Elise van Dongen, Sander R. Niehe, Harry Suryapranata, Stijn van Vugt, Ruben Ramos, Duarte Cacela, Ana Santana, Antonio Fiarresga, Lidia Sousa, Hugo Marques, Lino Patricio, Luis Bernanrdes, Pedro Rio, Ramiro Carvalho, Rui Ferreira, Tiago Silva, Ines Rodrigues, Pedro Modas, Guilherme Portugal, Jose Fragata, Fausto J. Pinto, Miguel Nobre Menezes, Guilhermina Cantinho Lopes, Ana Gomes Almeida, Pedro Canas Silva, Angelo Nobre, Ana Rita Francisco, Nuno Ferreira, Ricardo L. Lopes, Luis Guzman, Julio César Figal, Oscar Méndiz, Claudia Cortés, Roberto René Favaloro, Carlos Alvarez, Javier Courtis, Gabriela Zeballos, Lilia Schiavi, Mariano Rubio, Gerard Patrick Devlin, Raewyn Fisher, Ralph Alan Huston Stewart, Harvey Douglas White, Jocelyne Benatar, Sasko Kedev, Irena Peovska Mitevska, Elizabeta Srbinovska Kostovska, Hristo Pejkov, Claes Held, Kai Eggers, Gunnar Frostfelt, Nina Johnston, Maciej Olsowka, Axel Åkerblom, Inga Soveri, Johannes Aspberg, Tali Sharir, Dan Elian, Arthur Kerner, Samia Massalha, Keiichi Fukuda, Shun Kohsaka, Satoshi Yasuda, Shigeyuki Nishimura, Kaatje Goetschalckx, Frans Van de Werf, Kathleen Claes, Chung‐Lieh Hung, Chun‐Ho Yun, Charles Jia‐Yin Hou, Jen‐Yuan Kuo, Hung‐I Yeh, Ta‐Chuan Hung, Jiun‐Yi Li, Chen‐Yen Chien, Cheng‐Ting Tsai, Chun‐Chieh Liu, Fa‐Chang Yu, Yueh‐Hung Lin, Wei‐Ren Lan, Chih‐Hsuan Yen, Jui‐Peng Tsai, Kuo‐Tzu Sung, Mpiko Ntsekhe, Shaheen Pandie, Charle A. Viljoen, Marianne De Andrade, Tiziano Moccetti, M. Grazia Rossi, Magdy Abdelhamid, Ahmed Adel, Ahmed Kamal, Hossam Mahrous, Sameh El Kaffas, Hussien El Fishawy, Calin Pop, Matei Claudia, Bogdan A. Popescu, Carmen Ginghina, Dan Deleanu, Vlad A. Iliescu, Mouaz H. Al‐Mallah, Ahmed Aljzeeri, Hani Najm, Ali Alghamdi, Walter Enrique Mogrovejo Ramos, Srun Kuanprasert, Arintaya Prommintikul, Weerachai Nawarawong, Surin Woragidpoonpol, Thitipong Tepsuwan, Noppon Taksaudom, Chataroon Rimsukcharoenchai, Juntima Euathrongchit, Yutthaphan Wannasopha, Sukit Yamwong, Piyamitr Sritara, Suthara Aramcharoen, Krissada Meemuk, Ahmad Khairuddin, Hafidz Abd Hadi, and Shaiful Azmi Yahaya
References
- 1. Jespersen L, Hvelplund A, Abildstrøm SZ, Pedersen F, Galatius S, Madsen JK, Jørgensen E, Kelbæk H, Prescott E. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012;33:734–744. doi: 10.1093/eurheartj/ehr331 [DOI] [PubMed] [Google Scholar]
- 2. Sharaf B, Wood T, Shaw L, Johnson BD, Kelsey S, Anderson RD, Pepine CJ, Merz CN. Adverse outcomes among women presenting with signs and symptoms of ischemia and no obstructive coronary artery disease: findings from the National Heart, Lung, and Blood Institute‐sponsored Women's ischemia syndrome evaluation (WISE) angiographic core laboratory. Am Heart J. 2013;166:134–141. doi: 10.1016/j.ahj.2013.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hemingway H, McCallum A, Shipley M, Manderbacka K, Martikainen P, Keskimäki I. Incidence and prognostic implications of stable angina pectoris among women and men. J Am Med Assoc. 2006;295:1404–1411. doi: 10.1001/jama.295.12.1404 [DOI] [PubMed] [Google Scholar]
- 4. Sedlak TL, Lee M, Izadnegahdar M, Merz CNB, Gao M, Humphries KH. Sex differences in clinical outcomes in patients with stable angina and no obstructive coronary artery disease. Am Heart J. 2013;166:38–44. doi: 10.1016/j.ahj.2013.03.015 [DOI] [PubMed] [Google Scholar]
- 5. Reynolds HR, Farkouh ME, Lincoff AM, Hsu A, Swahn E, Sadowski ZP, White JA, Topol EJ, Hochman JS. Impact of female sex on death and bleeding after fibrinolytic treatment of myocardial infarction in GUSTO V. Arch Intern Med. 2007;167:2054–2060. doi: 10.1001/archinte.167.19.2054 [DOI] [PubMed] [Google Scholar]
- 6. Reynolds HR, Forman SA, Tamis‐Holland JE, Steg PG, Mark DB, Pearte CA, Carvalho AC, Sopko G, Liu L, Lamas GA, et al. Relationship of female sex to outcomes after myocardial infarction with persistent total occlusion of the infarct artery: analysis of the occluded artery trial (OAT). Am Heart J. 2012;163:462–469. doi: 10.1016/j.ahj.2012.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dillinger JG, Ducrocq G, Elbez Y, Cohen M, Bode C, Pollack C Jr, Petrauskiene B, Henry P, Dorobantu M, French WJ, et al. Sex differences in ischemic and bleeding outcomes in patients with non‐ST‐segment‐elevation acute coronary syndrome undergoing percutaneous coronary intervention: insights from the TAO trial. Circ Cardiovasc Interv. 2021;14:e009759. doi: 10.1161/CIRCINTERVENTIONS.120.009759 [DOI] [PubMed] [Google Scholar]
- 8. Bairey Merz CN, Shaw Leslee J, Reis Steven E, Bittner V, Kelsey Sheryl F, Olson M, Johnson BD, Pepine Carl J, Mankad S, Sharaf Barry L, et al. Insights from the NHLBI‐sponsored Women's ischemia syndrome evaluation (WISE) study. J Am Coll Cardiol. 2006;47:S21–S29. doi: 10.1016/j.jacc.2004.12.084 [DOI] [PubMed] [Google Scholar]
- 9. Guimarães PO, Granger CB, Stebbins A, Chiswell K, Held C, Hochman JS, Krug‐Gourley S, Lonn E, Lopes RD, Stewart RAH, et al. Sex differences in clinical characteristics, psychosocial factors, and outcomes among patients with stable coronary heart disease: insights from the STABILITY (stabilization of atherosclerotic plaque by initiation of Darapladib therapy) trial. J Am Heart Assoc. 2017;6:e006695. doi: 10.1161/JAHA.117.006695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tamis‐Holland JE, Lu J, Bittner V, Magee MF, Lopes N, Adler DS, Kip KE, Schwartz L, Groenewoud YA, Jacobs AK, et al. Sex, clinical symptoms, and angiographic findings in patients with diabetes mellitus and coronary artery disease (from the bypass angioplasty revascularization investigation [BARI] 2 diabetes trial). Am J Cardiol. 2011;107:980–985. doi: 10.1016/j.amjcard.2010.11.020 [DOI] [PubMed] [Google Scholar]
- 11. Acharjee S, Teo KK, Jacobs AK, Hartigan PM, Barn K, Gosselin G, Tanguay JF, Maron DJ, Kostuk WJ, Chaitman BR, et al. Optimal medical therapy with or without percutaneous coronary intervention in women with stable coronary disease: a pre‐specified subset analysis of the clinical outcomes utilizing revascularization and aggressive druG evaluation (COURAGE) trial. Am Heart J. 2016;173:108–117. doi: 10.1016/j.ahj.2015.07.020 [DOI] [PubMed] [Google Scholar]
- 12. Ferrari R, Abergel H, Ford I, Fox KM, Greenlaw N, Steg PG, Hu D, Tendera M, Tardif JC, Investigators C. Gender‐ and age‐related differences in clinical presentation and management of outpatients with stable coronary artery disease. Int J Cardiol. 2013;167:2938–2943. doi: 10.1016/j.ijcard.2012.08.013 [DOI] [PubMed] [Google Scholar]
- 13. Hochman JS, Reynolds HR, Bangalore S, O'Brien SM, Alexander KP, Senior R, Boden WE, Stone GW, Goodman SG, Lopes RD, et al. Baseline characteristics and risk profiles of participants in the ISCHEMIA randomized clinical TrialBaseline characteristics of participants in the ISCHEMIA StudyBaseline characteristics of participants in the ISCHEMIA study. JAMA Cardiol. 2019;4:273–286. doi: 10.1001/jamacardio.2019.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Reynolds HR, Shaw LJ, Min JK, Spertus JA, Chaitman BR, Berman DS, Picard MH, Kwong RY, Bairey‐Merz CN, Cyr DD, et al. Association of sex with Severity of coronary artery disease, ischemia, and symptom burden in patients with moderate or severe ischemia: secondary analysis of the ISCHEMIA randomized clinical trial. JAMA Cardiol. 2021;6:980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Blankstein R, Ward RP, Arnsdorf M, Jones B, Lou Y‐B, Pine M. Female gender is an independent predictor of operative mortality after coronary artery bypass graft surgery. Circulation. 2005;112:I‐323–I‐327. doi: 10.1161/CIRCULATIONAHA.104.525139 [DOI] [PubMed] [Google Scholar]
- 16. Arif R, Farag M, Gertner V, Szabó G, Weymann A, Veres G, Ruhparwar A, Bekeredjian R, Bruckner T, Karck MJPO. Female gender and differences in outcome after isolated coronary artery bypass graft surgery: does age play a role? PLoS One. 2016;11:e0145371. doi: 10.1371/journal.pone.0145371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Filardo G, Hamman BL, Pollock BD, da Graca B, Sass DM, Phan TK, Edgerton J, Prince SL, Ring WSJOH. Excess short‐term mortality in women after isolated coronary artery bypass graft surgery. Open Heart. 2016;3:e000386. doi: 10.1136/openhrt-2015-000386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Duvernoy CS, Smith DE, Manohar P, Schaefer A, Kline‐Rogers E, Share D, McNamara R, Gurm HS, Moscucci MJ. Gender differences in adverse outcomes after contemporary percutaneous coronary intervention: an analysis from the blue cross blue shield of Michigan cardiovascular consortium (BMC2) percutaneous coronary intervention registry. Am Heart J. 2010;159:677–683. doi: 10.1016/j.ahj.2009.12.040 [DOI] [PubMed] [Google Scholar]
- 19. Magee MF, Tamis‐Holland JE, Lu J, Bittner VA, Brooks MM, Lopes N, Jacobs AKJI. Sex, prescribing practices and guideline recommended, blood pressure, and LDL cholesterol targets at baseline in the BARI 2D trial. Int J Endocrinol. 2015;2015:610239. doi: 10.1155/2015/610239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Newman JD, Alexander KP, Gu X, O'Brien SM, Boden WE, Govindan SC, Senior R, Moorthy N, Rezende PC, Demkow M, et al. Baseline predictors of low‐density lipoprotein cholesterol and systolic blood pressure goal attainment after 1 year in the ISCHEMIA trial. Circ Cardiovasc Qual Outcomes. 2019;12:e006002. doi: 10.1161/CIRCOUTCOMES.119.006002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Blumenthal DM, Howard SE, Searl Como J, O'Keefe SM, Atlas SJ, Horn DM, Wagle NW, Wasfy JH, Yeh RW, Metlay JP. Prevalence of angina among primary care patients with coronary artery disease. JAMA Network Open. 2021;4:e2112800. doi: 10.1001/jamanetworkopen.2021.12800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Beltrame JF, Weekes AJ, Morgan C, Tavella R, Spertus JA. The prevalence of weekly angina among patients with chronic stable angina in primary care practices: the coronary artery disease in general practice (CADENCE) study. Archiv Intern Med. 2009;169:1491–1499. doi: 10.1001/archinternmed.2009.295 [DOI] [PubMed] [Google Scholar]
- 23. Shah ASV, Griffiths M, Lee KK, McAllister DA, Hunter AL, Ferry AV, Cruikshank A, Reid A, Stoddart M, Strachan F, et al. High sensitivity cardiac troponin and the under‐diagnosis of myocardial infarction in women: prospective cohort study. BMJ. 2015;350:g7873. doi: 10.1136/bmj.g7873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Eggers KM, Johnston N, James S, Lindahl B, Venge P. Cardiac troponin I levels in patients with non–ST‐elevation acute coronary syndrome—the importance of gender. American Heart Journal. 2014;168:317–324.e1. doi: 10.1016/j.ahj.2014.06.006 [DOI] [PubMed] [Google Scholar]
- 25. Maron DJ, Hochman JS, O'Brien SM, Reynolds HR, Boden WE, Stone GW, Bangalore S, Spertus JA, Mark DB, Alexander KP, et al. International study of comparative health effectiveness with medical and invasive approaches (ISCHEMIA) trial: rationale and design. Am Heart J. 2018;201:124–135. doi: 10.1016/j.ahj.2018.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Califf RM, Phillips HR III, Hindman MC, Mark DB, Lee KL, Behar VS, Johnson RA, Pryor DB, Rosati RA, Wagner GS, et al. Prognostic value of a coronary artery jeopardy score. J Am Coll Cardiol. 1985;5:1055–1063. doi: 10.1016/S0735-1097(85)80005-X [DOI] [PubMed] [Google Scholar]
- 27. Franzone A, Taniwaki M, Rigamonti F, Heg D, Piccolo R, Roffi M, Tuller D, Muller O, Vuilliomenet A, Cook S, et al. Angiographic complexity of coronary artery disease according to SYNTAX score and clinical outcomes after revascularisation with newer‐generation drug‐eluting stents: a substudy of the BIOSCIENCE trial. EuroIntervention. 2016;12:e595–e604. doi: 10.4244/EIJV12I5A99 [DOI] [PubMed] [Google Scholar]
- 28. Chaitman BR, Alexander KP, Cyr DD, Berger JS, Reynolds HR, Bangalore S, Boden WE, Lopes RD, Demkow M, Perna GP, et al. Myocardial infarction in the ISCHEMIA trial. Circulation. 2021;143:790–804. doi: 10.1161/CIRCULATIONAHA.120.047987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452 [DOI] [Google Scholar]
- 30. John D, Kalbfleisch RLP. The Statistical Analysis of Failure Time Data. 2nd ed. Wiley; 2011. [Google Scholar]
- 31. Gray RJ. A class of K‐sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16:1141–1154. doi: 10.1214/aos/1176350951 [DOI] [Google Scholar]
- 32. Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O'Brien SM, Boden WE, Chaitman BR, Senior R, Lopez‐Sendon J, Alexander KP, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382:1395–1407. doi: 10.1056/NEJMoa1915922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shaw LJ, Miller DD, Romeis JC, Kargl D, Younis LT, Chaitman BR. Gender differences in the noninvasive evaluation and Management of Patients with suspected coronary artery disease. Ann Intern Med. 1994;120:559–566. doi: 10.7326/0003-4819-120-7-199404010-00005 [DOI] [PubMed] [Google Scholar]
- 34. Pagidipati NJ, Coles A, Hemal K, Lee KL, Dolor RJ, Pellikka PA, Mark DB, Patel MR, Litwin SE, Daubert MA, et al. Sex differences in management and outcomes of patients with stable symptoms suggestive of coronary artery disease: insights from the PROMISE trial. Am Heart J. 2019;208:28–36. doi: 10.1016/j.ahj.2018.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Beatty AL, Spertus JA, Whooley MA. Frequency of angina pectoris and secondary events in patients with stable coronary heart disease (from the heart and soul study). Am J Cardiol. 2014;114:997–1002. doi: 10.1016/j.amjcard.2014.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Eisen A, Bhatt DL, Steg PG, Eagle KA, Goto S, Guo J, Smith SC, Ohman EM, Scirica BM, Investigators RR. Angina and future cardiovascular events in stable patients with coronary artery disease: insights from the reduction of atherothrombosis for continued health (REACH) registry. J Am Heart Assoc. 2016;5:e004080. doi: 10.1161/JAHA.116.004080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mamudu HM, Paul TK, Veeranki SP, Budoff M. The effects of coronary artery calcium screening on behavioral modification, risk perception, and medication adherence among asymptomatic adults: a systematic review. Atherosclerosis. 2014;236:338–350. doi: 10.1016/j.atherosclerosis.2014.07.022 [DOI] [PubMed] [Google Scholar]
- 38. Reynolds HR, Shaw LJ, Min JK, Page CB, Berman DS, Chaitman BR, Picard MH, Kwong RY, O'Brien SM, Huang Z, et al. Outcomes in the ISCHEMIA trial based on coronary artery disease and ischemia severity. Circulation. 2021;144:1024–1038. doi: 10.1161/CIRCULATIONAHA.120.049755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Buuren S. Flexible Imputation of Missing Data. Chapman & Hall/CRC; 2012. doi: 10.1201/b11826 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


