Abstract
Though microdosing psychedelics has become increasingly popular, its long-term effects on cardiac health remain unknown. Microdosing most commonly involves ingesting sub-threshold doses of lysergic acid diethylamide (LSD), psilocybin, or other psychedelic drugs 2–4 times a week for at least several weeks, but potentially months or years. Concerningly, both LSD and psilocybin share structural similarities with medications which raise the risk of cardiac fibrosis and valvulopathy when taken regularly, including methysergide, pergolide, and fenfluramine. 3,4-Methylenedioxymethamphetamine, which is also reportedly used for microdosing, is likewise associated with heart valve damage when taken chronically. In this review, we evaluate the evidence that microdosing LSD, psilocybin, and other psychedelics for several months or more could raise the risk of cardiac fibrosis. We discuss the relationship between drug-induced cardiac fibrosis and the 5-HT2B receptor, and we make recommendations for evaluating the safety of microdosing psychedelics in future studies.
Keywords: Psychedelics, cardiology, psilocybin, serotonin
The practice of microdosing, which involves intermittently taking a sub-threshold dose of a psychedelic substance, has recently gained attention in both popular media and the scientific community (Kaypak and Raz, 2022). According to a 2020 survey of drug and alcohol users, 17% of participants reported microdosing psychedelics at some point in their lives, highlighting the public health importance of assessing the safety of this practice (Cameron et al., 2020). This is particularly true because some medications exhibiting a close chemical resemblance to psychedelics have been associated with the development of cardiac fibrosis and valvulopathy (Aronson, 2016). While psychedelics appear to be well-tolerated and safe when taken sparingly (Dos Santos et al., 2018), there are few scientific studies on the safety of microdosing over extended periods of time. One recent review concluded that there may be a significant risk of valvular heart disease (VHD) from chronic use of serotonergic psychedelics and MDMA (Tagen et al., 2023). The risk of VHD was primarily evaluated using data from in vitro functional assays, but also with reference to in vivo studies in both animals and humans, which all suggested that VHD is a potential risk of long-term microdosing that should be taken seriously (Tagen et al., 2023). The current review aims to expand the evaluation of the potential cardiac risks of microdosing serotoninergic psychedelics using comparisons to non-psychedelic substances already known to cause cardiac fibrosis and valvulopathy.
The practice of microdosing
The two primary substances used for microdosing are lysergic acid diethylamide (LSD) and psilocybin, which is found in psychedelic mushrooms; some users also report microdosing with 3,4-Methylenedioxymethamphetamine (MDMA) (Lea et al., 2020b). A microdose of LSD typically ranges from 10 to 20 μg, while a microdose of psilocybin-containing mushrooms ranges from 0.3 to 0.5 g of dried mushrooms (Kuypers, 2020). Microdoses are typically taken 2–4 times per week (Hutten et al., 2019) for at least several weeks and sometimes months or years (Kaertner et al., 2021; Lea et al., 2020a). Microdosing is intended to have minimal hallucinogenic effects (Anderson et al., 2019) and should not impair cognitive function (Rootman et al., 2022), though recent double-blind research has provided evidence for reduced cognitive performance in some individuals who microdosed with 0.5 g of psilocybin-containing mushrooms (Cavanna et al., 2022).
Self-reported outcomes of microdosing have identified several recurring themes, including changes in mood, work, and home life (Fadiman and Korb, 2019). Microdosers commonly report enhanced creativity, improved focus, better moods, and reduced anxiety (Kaertner et al., 2021; Liokaftos, 2021). Additionally, some people use microdosing to alleviate mental health problems, such as depression or anxiety, as well as headaches (Fadiman and Korb, 2019). Despite the positive nature of reported changes, the absence of a control group in many studies makes it difficult to determine the true effects of microdosing. Few double-blind, placebo-controlled studies on microdosing have thus far been done, and they often feature small sample sizes. One recent study investigating the impact of a 2 -month regimen of 0.7 g of dried psilocybin-containing Galindoi truffles, with 5–7 doses per 3 weeks and at least 1 day between doses, did not reveal a significant impact on interoceptive awareness, symptoms of depression or anxiety, or emotional processing (Marschall et al., 2022). Other studies suggest that many purported effects of microdosing might be placebo effects or a matter of regression to the mean (Cavanna et al., 2022).
The scientific interest in microdosing psychedelics is very recent: the oldest randomized controlled trial on microdosing was published in 2019 (Bershad et al., 2019), and as of this writing, there have only been a total of 11 randomized trials and one open-label study on microdosing. The results have been mixed thus far, and conclusions cannot be drawn due to the limited amount of data available. Despite the uncertainty surrounding the benefits and drawbacks of microdosing, the notion of ingesting psychedelic substances in small quantities over an extended period has piqued the interest of many (Lea et al., 2020a). There has also been interest in microdosing for the treatment of psychiatric disorders, particularly depression (Kuypers, 2020). Consequently, the safety of prolonged microdosing remains an important concern.
Presently, taking a single high dose of serotoninergic psychedelics is widely considered to be physically safe. This is also true for repeated high doses provided that sufficient time, for example, several months, elapses between doses (Nichols, 2004). However, the risks of chronic use (e.g. >2 times per week for at least several weeks) remain largely unknown. One concern is the potential risk of fibrosis and cardiac valvulopathy, which is known to be caused by substances which are chemically similar to psychedelics. Substances which share structural similarities with serotoninergic psychedelics, such as ergoline compounds, have been shown to cause cardiac fibrosis and valvulopathy when taken chronically (Reichmann et al., 2006).
Drug-induced cardiac valvulopathies
Drug-induced VHD typically involves impaired motion of the heart valves caused by abnormal valve thickening, also referred to as fibrosis (Andrejak and Tribouilloy, 2013). This results in valve regurgitation, which can cause arrhythmias or even heart failure if it becomes severe. Once established, fibrosis can be difficult to reverse (Kong et al., 2014). Drug-induced VHD is diagnosed by echocardiogram and was first described in the mid-1960s (Andrejak and Tribouilloy, 2013).
One of the first drugs linked to fibrosis and VHD was methysergide, which incidentally was first synthesized from LSD by Sandoz in the same lab in which LSD was discovered (Koehler and Tfelt-Hansen, 2008). It is an effective treatment for cluster headaches and migraines but was linked to retroperitoneal fibrosis in the 1960s, especially cardiac and pulmonary fibrosis. Over a period of 5 years, 10 of 1000 patients who regularly took methysergide developed fibrosis (Graham, 1967). Additionally, it was found that discontinuing methysergide significantly reduced fibrosis and resuming it caused the fibrosis to return, confirming the connection with methysergide (Graham et al., 1966). It was later established that the active metabolite methylergonovine, rather than methysergide itself, is the cardiotoxic substance (Bhattacharyya et al., 2009). After these discoveries, methysergide was removed from the market in the United States and Canada (Mason et al., 1977; Ramírez Rosas et al., 2013). In other countries, it was still prescribed with instructions to discontinue use every 6 months for a period of 3–4 weeks in order to avoid fibrosis (Aronson, 2016).
Other ergolines have also been associated with the development of heart problems. Therapeutic doses of ergotamine, which shares structural similarities with LSD, have been associated with myocardial ischemia (Galer et al., 1991). Further links between ergotamine and VHD have been established based on both case reports and in vitro and in vivo experiments (Zajdel et al., 2015). Although ergotamine is still approved by the US Food and Drug Administration (FDA), daily administration is not recommended (U.S. Food and Drug Administration, 2002). Dihydroergotamine (DHE), another anti-migraine drug and ergot alkaloid, has also been linked to fibrosis. Out of 75 fibrosis cases reported by the marketing authorization holders, 50 were potentially caused by DHE (European Medicines Agency, 2013). The retroperitoneal type of fibrosis was the most reported, accounting for 36% of cases, followed by the cardiac type at 30% and the pleural type at 18%. Symptoms improved in the 57% of patients who discontinued the drug, though most of them also underwent heart valve replacement. As a result, in Europe, all medications containing DHE have been recalled, and their sale has been suspended due to severe cases of fibrosis and ergotism (European Medicines Agency, 2013).
Additionally, several medications used to treat Parkinson’s disease, such as cabergoline and pergolide, have been linked to fibrosis and VHD (Andersohn and Garbe, 2009; Newman-Tancredi et al., 2002). One case series describes 24 patients who developed fibrosis during pergolide treatment, with one of them developing pleural and parenchymal fibrosis while being treated with 7.5 mg/day of pergolide for 8 years (Agarwal et al., 2004). A meta-analysis has shown that less than 2 mg/day of pergolide was sufficient to increase risk of VHD by a factor of five when taken for several years (48 ± 18 months) (Corvol et al., 2007). Another study compared 634 Parkinson’s patients treated with cabergoline to 9120 Parkinson’s patients treated with a non-ergot dopamine decarboxylase inhibitor, concluding that valvular regurgitation was more frequent with the ones treated with cabergoline (De Vecchis et al., 2013). Another case reported pleural fibrosis after 7 months of cabergoline treatment, which resolved after de-challenge (Guptha and Promnitz, 2005). Pergolide has been withdrawn by the FDA due to its association with fibrosis and VHD (FDA Public Health Advisory, 2007), but cabergoline is still available to treat hyperprolactinemia at low doses of <4 mg per week, as these are not associated with clinically significant VHD (Bogazzi et al., 2008; Wakil et al., 2008).
A few substituted amphetamines, including MDMA, have also been associated with fibrosis and VHD. One such derivative is norfenfluramine, a metabolite of fenfluramine (Vickers et al., 2001), which was frequently used as an anorexic agent in combination with phentermine, another anti-obesity medication (Spencer et al., 2000). One study found 24 cases of VHD after using the fenfluramine-phentermine combination for an average of 12.3 months (Connolly et al., 1997). Another involved 223 patients who took fenfluramine during open-label trials from January 1994 to August 1997, with 53 developing cardiac valve abnormalities, compared to three in a control group. These diagnoses were independently confirmed by at least two cardiologists, usually using echocardiograms (Khan et al., 1998). A recent rabbit model study also found that dexfenfluramine, the d-enantiomer of fenfluramine, may also cause VHD (Oury et al., 2020). Although fenfluramine and dexfenfluramine were once used as anorexic agents, they have since been withdrawn (Li and Cheung, 2011). Fenfluramine is still used to treat seizures (Knupp et al., 2022).
Finally, although there are no studies on microdoses of MDMA, larger doses have been linked to valvular damage. This is particularly concerning because MDMA is almost never used daily, unlike many other drugs which have been associated with fibrosis. A study conducted on 33 individuals who took an average of 3.6 MDMA tablets per week for over 6 months found that 28% of them showed abnormal echocardiographic results based on FDA criteria, while no such results were observed in the gender- and age-matched control group (Droogmans et al., 2007). The valvular damage observed in those who used MDMA was less severe compared to that observed in people who took prescription drugs such as pergolide or phentermine-fenfluramine, presumably due to MDMA users taking breaks between doses (Droogmans et al., 2007).
5-HT2BR and cardiac valvulopathy
What do substances associated with drug-induced VHD have in common? Previous research has largely converged on overstimulation of 5-HT2BR as the primary cause of drug-induced cardiac valvulopathy (Cavero and Guillon, 2014; Elangbam et al., 2008). Nearly all drugs which induce VHD show agonist activity at 5-HT2BR or are metabolized to a substance that does, for example, methysergide, which is a pro-drug of the potent 5-HT2BR agonist methylergonovine (Andrejak and Tribouilloy, 2013; Huang et al., 2009; Rothman et al., 2000). This can be harmful because fibroblasts in the heart valves, whose proper functioning allows blood flow to proceed into the cardiac chambers and arteries in only one direction, show high expression levels of 5-HT2BR (Cavero and Guillon, 2014). Sustained overstimulation of 5-HT2BR can cause cardiac fibroblasts to proliferate and become deposited in abnormal quantities, causing cardiac valves to thicken and function abnormally, which can ultimately manifest as valve fibrosis and VHD (Gourdie et al., 2016; Newman-Tancredi et al., 2002).
The connection to 5-HT2BR has been confirmed in preclinical studies. Chronic treatment with nordexfenfluramine, which has been associated with VHD in humans, results in mitral valve lesions in mice; this effect can be blocked by either a 5-HT2BR antagonist or by genetic ablation of 5-HT2BR (Ayme-Dietrich et al., 2017). Antagonism of 5-HT2BR has also blocked drug-induced valvulopathy in rats (Droogmans et al., 2007). In line with this, many 5-HT2AR antagonists lack links to fibrosis, including lisuride (Hofmann et al., 2006; Zajdel et al., 2015) and metergoline (Falsetti et al., 1983). Some 5-HT2BR antagonists, for example, terguride, may even protect against fibrosis (Dees et al., 2011). Though other mechanisms may also play a role, including 5-HT2AR (Ayme-Dietrich et al., 2017) and dopaminergic receptors (Byrne et al., 2022), there is widespread consensus that 5-HT2BR stimulation is necessary to cause drug-induced VHD. This is concerning for microdosing because LSD, psilocybin, and MDMA also have agonist activity at 5-HT2BR (Halberstadt and Geyer, 2011; McCorvy et al., 2018).
Importantly, though 5-HT2BR agonism seems necessary for drug-induced VHD, some relatively weak 5-HT2BR agonists have not been associated with fibrosis or VHD. The anti-Parkinson drug ropinirole and the weight-loss drug lorcaserin are two such examples. One study compared ropinirole with the pro-fibrotic drugs cabergoline and pergolide, as well as a control group, using a VHD scoring system and transthoracic echocardiography to diagnose cardiovascular symptoms. As expected, the results showed significant symptoms of cardiovascular disease and VHD in the pergolide and cabergoline groups, but there was no such association found in the ropinirole group (Junghanns et al., 2007). Lorcaserin, though it was removed from the market due to increased cancer risk, was also not associated with valvulopathy in a study of 7190 patients (Greenway et al., 2016).
Because of these exceptions, the fact that serotoninergic psychedelics share similarities with fibrosis-inducing drugs does not immediately mean that chronic microdosing is dangerous. To gain more clues about the potential risk, we can investigate the differences between 5-HT2BR agonists, which do and do not cause fibrosis, and then evaluate the characteristics of LSD, psilocybin, and MDMA in comparison.
Characteristics of 5-HT2BR agonists associated with valvulopathy
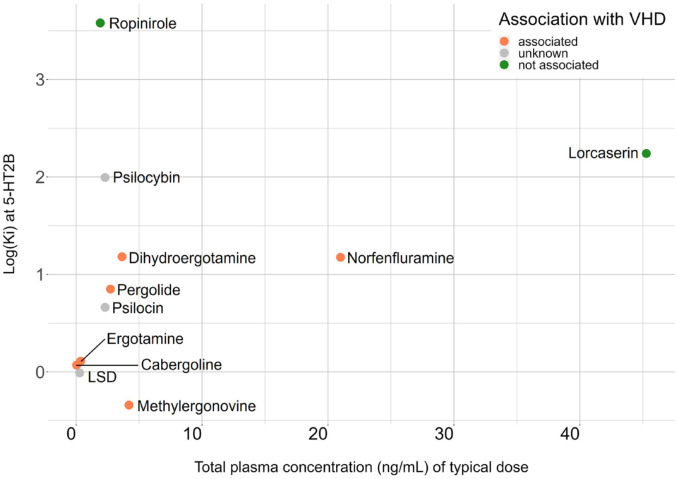
Previous research strongly suggests that agonists with a greater affinity for 5-HT2BR may pose the most risk of VHD. The affinity of a ligand for a receptor, expressed as the dissociation constant Ki, indicates the tightness of the binding interaction, though it is a limited indicator of functional efficacy. Though no single biomarker predicts VHD risk with complete accuracy, previous studies have established that 5-HT2BR agonists linked to fibrosis and VHD tend to have a Ki of below 15nM, including methylergonovine, ergotamine, pergolide, DHE, and several others discussed above (Table 1) (Papoian et al., 2017). Ropinirole and lorcaserin, which have not been associated with VHD, have Ki values of 4000 nM and 174 nM, respectively. In contrast, based on the 15 nM affinity threshold, the risk of VHD would be substantial for both LSD and psilocybin: LSD has a Ki value of 0.98 nM at 5-HT2BR, and psilocybin’s active metabolite psilocin has a Ki of 4.6 nM at 5-HT2BR (Figure 1) (Dinis-Oliveira, 2017; McKenna and Peroutka, 1989). Importantly, LSD and psilocin exert most of their psychoactive effects via 5-HT2AR (Vollenweider and Preller, 2020). The affinity of LSD at 5-HT2BR is similar to its affinity at 5-HT2AR, while psilocin shows even greater affinity for 5-HT2BR than 5-HT2AR, suggesting that both substances likely stimulate 5-HT2BR at any psychoactive dose (Tagen et al., 2023). Finally, MDMA’s relatively high affinity of 500 nM has not prevented it from causing cardiac abnormalities, although this exception might be explained by MDMA’s ability to potently release 5-HT (Mlinar and Corradetti, 2003); excessive amounts of 5-HT can also promote fibrotic signaling (Smith et al., 2009a, 2009b).
Table 1.
List of 5-HT2BR agonists which have been investigated for links to fibrosis and VHD, as well as their Ki values at the 5-HT2BR and peak total plasma concentrations of a typical dose or microdose. Data from four common microdosing drugs (LSD, psilocybin and psilocin, and MDMA) is included for comparison, and no controlled studies have yet assessed the risk of VHD in chronic microdosers. Data from cloned human 5-HT2BR receptors taken from the database of the U.S. National Institute of Mental Health (NIMH) Psychoactive Drug Screening Program (Roth et al., 2000) (http://pdsp.med.unc.edu) with additional references when applicable.
| Drug | Ki at 5-HT2BR (nM) | Peak plasma concentration of typical (micro)dose (ng/mL) | Associated with VHD? |
|---|---|---|---|
| Methylergonovine (metabolite of methysergide) | 0.457 (Knight et al., 2004) | 4.2 (Bredberg et al., 1986) | Yes |
| LSD | 0.977 (Knight et al., 2004) | 0.281 (Hutten et al., 2020) | Unknown |
| Cabergoline | 1.175 (Millan et al., 2002) | 0.04 (Andreotti et al., 1995) | Yes |
| Ergotamine | 1.288 (Knight et al., 2004) | 0.36 (Perrin, 1985) | Yes |
| Psilocin | 4.6 (Bredberg et al., 1986) | 2.3 (Madsen et al., 2019) | Unknown |
| Pergolide | 7.079 (Millan et al., 2002) | 2.73 (Blin, 2003) | Yes |
| DHE | 15.2 (Setola et al., 2003) | 3.648 (Shrewsbury et al., 2008) | Yes |
| Norfenfluramine | 52.1 (Rothman et al., 2000) | 21 (Caccia et al., 1985) | Yes |
| Psilocybin | 98.7 (Roth et al., 2000) | — | Unknown |
| Lorcaserin | 174 (Thomsen et al., 2008: 200) | 45.28 (SR Smith et al., 2009a, 2009b) | No |
| MDMA | 500 (Setola et al., 2003) | — | Yes |
| Ropinirole | 3802 (Wainscott et al., 1996) | 1.92 (Kaye and Nicholls, 2000) | No |
Figure 1.
Affinity at the 5-HT2BR and plasma concentrations of typical doses for drugs which have been investigated for links to fibrosis and VHD, as well as for LSD, psilocin, and psilocybin, for which the risk of VHD has not yet been investigated in controlled studies.
Because of the small doses used in microdosing, it is also worth considering whether these doses reach a high enough concentration in the bloodstream to overstimulate 5-HT2BR. The peak total LSD plasma concentration was 0.28 ng/mL after administration of a single dose of 0.01 mg of LSD base, which is a typical microdose (Hutten et al., 2020). Plasma concentrations of LSD are below the limit of detection with 6–8 h of administration, and thus plasma levels should not exceed this peak even with daily dosing (Family et al., 2022). A typical dose of cabergoline (1 mg p.o.), which has a similar affinity for the 5-HT2BR receptor to LSD, reaches a plasma concentration of only 0.04 ng/mL, and daily intake of this dose has been associated with VHD (Andreotti et al., 1995). Thus, it appears that a microdose of LSD may indeed be large enough to raise the risk of VHD. Similarly, a small dose of 3 mg psilocybin raises plasma concentrations of psilocin to 2.3 ng/mL (Madsen et al., 2019), comparable to the levels seen after the pro-fibrotic drug pergolide, which has a somewhat weaker affinity (Table 1). This suggests that the typical doses used in microdosing could potentially be enough to trigger fibrosis or VHD in a similar manner to other drugs. However, the lack of data specifically addressing this risk of VHD from microdosing underscores the need for further research in this area.
Though high affinity for 5-HT2BR seems to be a good indicator of the risk for VHD, several studies have also evaluated functional and molecular markers of pro-fibrotic activity. It has been theorized that 5-HT2BR stimulation activates pro-fibrotic pathways via activation of phospholipase C-β, protein kinase C, Src-P, and transforming growth factor-β1 (Reid et al., 2013). Mitogen-activated protein kinase (MAPK) signaling may also be involved: MAPK signaling pathways can stimulate the activation of cardiac fibroblasts, leading to increased production of extracellular matrix proteins, and activation of ERK and p38 MAPK pathways has been shown to induce fibroblasts (Oury et al., 2020). Notably, however, research comparing various readouts of 5-HT2BR activation in several 5-HT2BR agonists concluded that VHD risk was not associated with one specific marker of 5-HT2BR activation but rather with general potency across a variety of markers, including calcium flux, ERK2 phosphorylation, and arrestin recruitment (Huang et al., 2009). This potency was much lower for ropirinole, which has weak 5-HT2BR affinity, than for drugs with strong 5-HT2BR affinity (Huang et al., 2009). Concerningly, in calcium flux assays, psilocin appears to be about as potent at 5-HT2BR as methylergonovine and several other valvulopathic drugs, suggesting that it may have a similar potential to cause VHD (Klein et al., 2020).
Finally, a promising molecular marker downstream from 5-HT2BR appears to be transforming growth factor-beta (TGF-β), which is upregulated via 5-HT2BR activity and promotes fibroblast growth (Bhattacharyya et al., 2009; Orton et al., 2012). If TGF-β signaling is not properly controlled in humans, it can lead to various cardiovascular diseases and vascular pathologies, including arteriovenous malformations, atherosclerosis, aneurysms, and valve fibrosis (Dees et al., 2011). Among the substances used for microdosing, MDMA has been associated with increased TGF-β signaling in humans, although studies thus far have all used larger doses than microdoses (Pacifici et al., 2001). To the best of our knowledge, there is no research yet on how LSD or psilocybin affects TGF-β signaling.
Conclusion and future directions
Taking all this information into consideration, it is possible that chronic microdosing may carry a risk of fibrosis and VHD, which should be assessed in future studies. There is converging evidence that simulation of the 5-HT2BR over several months may lead to the development of fibrosis. Duration of intake plays a major role in drug-induced VHD, even if the substance is not taken daily (Connolly et al., 1997; Schade et al., 2007). Indeed, the data on MDMA demonstrate that even weekly use can lead to valvulopathy if it is done for several years (Dawson and Moffatt, 2012). Furthermore, potency at 5-HT2BR appears to be the best predictor of potential for drug-induced VHD, and it is possible that even microdoses are indeed large enough to raise the risk of fibrosis when taken regularly (Huang et al., 2009).
Future clinical studies of microdosing should both design protocols which minimize the risk of fibrosis and screen for signs of pro-fibrotic signaling. Microdosing studies thus far have spanned several weeks rather than several months, but there is also clear interest in microdosing for the treatment of psychiatric disorders, which would likely involve longer microdosing regimens (Kuypers, 2020). Any future work considering longer microdosing regimens should incorporate breaks and regularly screening for vascular abnormalities, which is most easily done using an echocardiogram. Additionally, chronic microdosers could be screened for evidence of VHD in cross-sectional studies using echocardiograms, similar to previous studies of MDMA users (Droogmans et al., 2007). Previous work using in silico models has also been useful in estimating the risk of drug-induced valvulopathy, and has not yet been applied to microdosing.(Reid et al., 2013) Finally, large survey studies such as the Global Drug Survey, the world’s largest survey on drug use, could be used to assess the self-reported prevalence of cardiac symptoms and diagnoses in microdosers, though this would not replace data from controlled trials (Winstock et al., 2021). Though the risk of fibrosis and VHD is uncertain at this point, it is important to investigate potential adverse effects seriously as microdosing gains in popularity.
Acknowledgments
We would like to thank Dr. Patrizia Malagutti, cardiologist at the Department of Cardiology, Inselspital Bern, University of Bern, Switzerland, for reviewing the manuscript and for helpful comments.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This article was supported by the University of Fribourg.
ORCID iD: Gregor Hasler  https://orcid.org/0000-0002-8311-0138
https://orcid.org/0000-0002-8311-0138
References
- Agarwal P, Fahn S, Frucht SJ. (2004) Diagnosis and management of pergolide-induced fibrosis. Mov Disord 19: 699–704. [DOI] [PubMed] [Google Scholar]
- Andersohn F, Garbe E. (2009) Cardiac and noncardiac fibrotic reactions caused by ergot-and nonergot-derived dopamine agonists. Mov Disord 24: 129–133. [DOI] [PubMed] [Google Scholar]
- Anderson T, Petranker R, Rosenbaum D, et al. (2019) Microdosing psychedelics: Personality, mental health, and creativity differences in microdosers. Psychopharmacology 236: 731–740. [DOI] [PubMed] [Google Scholar]
- Andrejak M, Tribouilloy C. (2013) Drug-induced valvular heart disease: An update. Arch Cardiovasc Dis 106: 333–339. [DOI] [PubMed] [Google Scholar]
- Andreotti AC, Pianezzola E, Persiani S, et al. (1995) Pharmacokinetics, pharmacodynamics, and tolerability of cabergoline, a prolactin-lowering drug, after administration of increasing oral doses (0.5, 1.0, and 1.5 milligrams) in healthy male volunteers. J Clin Endocrinol Metabol 80: 841–845. [DOI] [PubMed] [Google Scholar]
- Aronson JK. (ed.) (2016) Methysergide. In: Meyler’s Side Effects of Drugs, 16th edn. Oxford: Elsevier, pp. 973–974. Available at: https://www.sciencedirect.com/science/article/pii/B9780444537171010702 (accessed 15 June 2023). [Google Scholar]
- Ayme-Dietrich E, Lawson R, Côté F, et al. (2017) The role of 5-HT2B receptors in mitral valvulopathy: Bone marrow mobilization of endothelial progenitors. Brit J Pharmacol 174: 4123–4139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bershad AK, Schepers ST, Bremmer MP, et al. (2019) Acute subjective and behavioral effects of microdoses of lysergic acid diethylamide in healthy human volunteers. Biol Psychiatr 86: 792–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharyya S, Schapira AH, Mikhailidis DP, et al. (2009) Drug-induced fibrotic valvular heart disease. Lancet 374: 577–585. [DOI] [PubMed] [Google Scholar]
- Blin O. (2003) The pharmacokinetics of pergolide in Parkinson’s disease. Curr Opin Neurol 16: S9–S12. [DOI] [PubMed] [Google Scholar]
- Bogazzi F, Buralli S, Manetti L, et al. (2008) Treatment with low doses of cabergoline is not associated with increased prevalence of cardiac valve regurgitation in patients with hyperprolactinaemia. Int J Clin Pract 62: 1864–1869. [DOI] [PubMed] [Google Scholar]
- Bredberg U, Eyjolfsdottir GS, Paalzow L, et al. (1986) Pharmacokinetics of methysergide and its metabolite methylergometrine in man. Eur J Clin Pharmacol 30: 75–77. [DOI] [PubMed] [Google Scholar]
- Byrne SE, Vishwakarma N, Sriramula S, et al. (2022) Dopamine receptor 3: A mystery at the heart of cardiac fibrosis. Life Sci 308: 120918. [DOI] [PubMed] [Google Scholar]
- Caccia S, Conforti I, Duchier J, et al. (1985) Pharmacokinetics of fenfluramine and norfenfluramine in volunteers given d- and dl-fenfluramine for 15 days. Eur J Clin Pharmacol 29: 221–224. [DOI] [PubMed] [Google Scholar]
- Cameron LP, Nazarian A, Olson DE. (2020) Psychedelic microdosing: Prevalence and subjective effects. J Psychoactive Drugs 52: 113–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanna F, Muller S, de la Fuente LA, et al. (2022) Microdosing with psilocybin mushrooms: A double-blind placebo-controlled study. Transl Psychiatr 12: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavero I, Guillon J-M. (2014) Safety Pharmacology assessment of drugs with biased 5-HT2B receptor agonism mediating cardiac valvulopathy. J Pharmacol Toxicol Meth 69: 150–161. [DOI] [PubMed] [Google Scholar]
- Connolly HM, Crary JL, McGoon MD, et al. (1997) Valvular heart disease associated with fenfluramine-phentermine. New Engl J Med 337: 581–588. [DOI] [PubMed] [Google Scholar]
- Corvol J-C, Anzouan-Kacou J-B, Fauveau E, et al. (2007) Heart valve regurgitation, pergolide use, and parkinson disease: An observational study and meta-analysis. Arch Neurol 64: 1721–1726. [DOI] [PubMed] [Google Scholar]
- Dawson P, Moffatt JD. (2012) Cardiovascular toxicity of novel psychoactive drugs: Lessons from the past. Progr Neuro-Psychopharmacol Biol Psychiatr 39: 244–252. [DOI] [PubMed] [Google Scholar]
- De Vecchis R, Esposito C, Ariano C. (2013) Cabergoline use and risk of fibrosis and insufficiency of cardiac valves. Herz 38: 868–880. [DOI] [PubMed] [Google Scholar]
- Dees C, Akhmetshina A, Zerr P, et al. (2011) Platelet-derived serotonin links vascular disease and tissue fibrosis. J Exp Med 208: 961–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinis-Oliveira RJ. (2017) Metabolism of psilocybin and psilocin: Clinical and forensic toxicological relevance. Drug Metabol Rev 49: 84–91. [DOI] [PubMed] [Google Scholar]
- Dos Santos RG, Bouso JC, Alcázar-Córcoles MÁ, et al. (2018) Efficacy, tolerability, and safety of serotonergic psychedelics for the management of mood, anxiety, and substance-use disorders: A systematic review of systematic reviews. Exp Rev Clin Pharmacol 11: 889–902. [DOI] [PubMed] [Google Scholar]
- Droogmans S, Cosyns B, D’haenen H, et al. (2007) Possible association between 3,4-methylenedioxymethamphetamine abuse and valvular heart disease. Am J Cardiol 100: 1442–1445. [DOI] [PubMed] [Google Scholar]
- Elangbam CS, Job LE, Zadrozny LM, et al. (2008) 5-hydroxytryptamine (5HT)-induced valvulopathy: Compositional valvular alterations are associated with 5HT2B receptor and 5HT transporter transcript changes in Sprague-Dawley rats. Exp Toxicol Pathol 60: 253–262. [DOI] [PubMed] [Google Scholar]
- European Medicines Agency (2013) New restrictions on use of medicines containing ergot derivatives. European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP). Available at: https://www.ema.europa.eu/en/news/new-restrictions-use-medicines-containing-ergot-derivatives (accessed 10 July 2023). [Google Scholar]
- Fadiman J, Korb S. (2019) Might microdosing psychedelics be safe and beneficial? An initial exploration. J Psychoactive Drugs 51: 118–122. [DOI] [PubMed] [Google Scholar]
- Falsetti L, Voltolini AM, Schimberni M, et al. (1983) Treatment of hyperprolactinaemia with metergoliie for periods up to 5 years: Clinical and biological tolerability. Curr Med Res Opin 8: 327–332. [DOI] [PubMed] [Google Scholar]
- Family N, Hendricks PS, Williams LT, et al. (2022) Safety, tolerability, pharmacokinetics, and subjective effects of 50, 75, and 100 µg LSD in healthy participants within a novel intervention paradigm: A proof-of-concept study. J Psychopharmacol (Oxford, England) 36: 321–336. [DOI] [PubMed] [Google Scholar]
- FDA Public Health Advisory: Pergolide (marketed as Permax) (2007). Available at: https://web.archive.org/web/20070408111551/https:/www.fda.gov/cder/drug/advisory/pergolide.htm (accessed 8 July 2023).
- Galer BS, Lipton RB, Solomon S, et al. (1991) Myocardial ischemia related to ergot alkaloids: A case report and literature review. Headache 31: 446–450. [DOI] [PubMed] [Google Scholar]
- Gourdie RG, Dimmeler S, Kohl P. (2016) Novel therapeutic strategies targeting fibroblasts and fibrosis in heart disease. Nat Rev. Drug Discov 15: 620–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham JR. (1967) Cardiac and pulmonary fibrosis during methysergide therapy for headache. Trans Am Clin Climatol Assoc 78: 79–92. [PMC free article] [PubMed] [Google Scholar]
- Graham JR, Suby HI, LeCompte PR, et al. (1966) Fibrotic disorders associated with methysergide therapy for headache. New Engl J Med 274: 359–368. [DOI] [PubMed] [Google Scholar]
- Greenway FL, Shanahan W, Fain R, et al. (2016) Safety and tolerability review of lorcaserin in clinical trials. Clin Obesity 6: 285–295. [DOI] [PubMed] [Google Scholar]
- Guptha SH, Promnitz AD. (2005) Pleural effusion and thickening due to cabergoline use in a patient with Parkinson’s disease. Eur J Intern Med 16: 129–131. [DOI] [PubMed] [Google Scholar]
- Halberstadt AL, Geyer MA. (2011) Multiple receptors contribute to the behavioral effects of indoleamine hallucinogens. Neuropharmacology 61: 364–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann C, Penner U, Dorow R, et al. (2006) Lisuride, a dopamine receptor agonist with 5-HT2B receptor antagonist properties: Absence of cardiac valvulopathy adverse drug reaction reports supports the concept of a crucial role for 5-HT2B receptor agonism in cardiac valvular fibrosis. Clin Neuropharmacol 29: 80–86. [DOI] [PubMed] [Google Scholar]
- Huang X-P, Setola V, Yadav PN, et al. (2009) Parallel functional activity profiling reveals valvulopathogens are potent 5-hydroxytryptamine2b receptor agonists: Implications for drug safety assessment. Mol Pharmacol 76: 710–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutten NRPW, Mason NL, Dolder PC, et al. (2019) Motives and side-effects of microdosing with psychedelics among users. Int J Neuropsychopharmacol 22: 426–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutten NRPW, Mason NL, Dolder PC, et al. (2020) Mood and cognition after administration of low LSD doses in healthy volunteers: A placebo controlled dose-effect finding study. Eur Neuropsychopharmacol 41: 81–91. [DOI] [PubMed] [Google Scholar]
- Junghanns S, Fuhrmann JT, Simonis G, et al. (2007) Valvular heart disease in Parkinson’s disease patients treated with dopamine agonists: A reader-blinded monocenter echocardiography study. Mov Disord 22: 234–237. [DOI] [PubMed] [Google Scholar]
- Kaertner LS, Steinborn MB, Kettner H, et al. (2021) Positive expectations predict improved mental-health outcomes linked to psychedelic microdosing. Sci Rep 11: 1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye CM, Nicholls B. (2000) Clinical pharmacokinetics of ropinirole. Clin Pharmacokinet 39: 243–254. [DOI] [PubMed] [Google Scholar]
- Kaypak AC, Raz A. (2022) Macrodosing to microdosing with psychedelics: Clinical, social, and cultural perspectives. Transcult Psychiatry 59: 665–674. [DOI] [PubMed] [Google Scholar]
- Khan MA, Herzog CA, St. Peter JV, et al. (1998) The prevalence of cardiac valvular insufficiency assessed by transthoracic echocardiography in obese patients treated with appetite-suppressant drugs. New Engl J Med 339: 713–718. [DOI] [PubMed] [Google Scholar]
- Klein AK, Chatha M, Laskowski LJ, et al. (2020) Investigation of the structure–activity relationships of psilocybin analogues. ACS Pharmacol Transl Sci 4: 533–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight AR, Misra A, Quirk K, et al. (2004) Pharmacological characterisation of the agonist radioligand binding site of 5-HT2A, 5-HT2B and 5-HT2C receptors. Naunyn-Schmiedeberg’s Arch Pharmacol 370: 114–123. [DOI] [PubMed] [Google Scholar]
- Knupp KG, Scheffer IE, Ceulemans B, et al. (2022) Efficacy and safety of fenfluramine for the treatment of seizures associated with lennox-gastaut syndrome: A randomized clinical trial. JAMA Neurol 79: 554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koehler P, Tfelt-Hansen P. (2008) History of methysergide in migraine. Cephalalgia 28: 1126–1135. [DOI] [PubMed] [Google Scholar]
- Kong P, Christia P, Frangogiannis NG. (2014) The pathogenesis of cardiac fibrosis. Cell Mol Life Sci 71: 549–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuypers KPC. (2020) The therapeutic potential of microdosing psychedelics in depression. Ther Adv Psychopharmacol 10: 2045125320950567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lea T, Amada N, Jungaberle H, et al. (2020. a) Microdosing psychedelics: Motivations, subjective effects and harm reduction. Int J Drug Policy 75: 102600. [DOI] [PubMed] [Google Scholar]
- Lea T, Amada N, Jungaberle H, et al. (2020. b) Perceived outcomes of psychedelic microdosing as self-managed therapies for mental and substance use disorders. Psychopharmacology 237: 1521–1532. [DOI] [PubMed] [Google Scholar]
- Li M-F, Cheung BM. (2011) Rise and fall of anti-obesity drugs. World J Diabetes 2: 19–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liokaftos D. (2021) Sociological investigations of human enhancement drugs: The case of microdosing psychedelics. Int J Drug Policy 95: 103099. [DOI] [PubMed] [Google Scholar]
- Madsen MK, Fisher PM, Burmester D, et al. (2019) Psychedelic effects of psilocybin correlate with serotonin 2A receptor occupancy and plasma psilocin levels. Neuropsychopharmacology 44: 1328–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marschall J, Fejer G, Lempe P, et al. (2022) Psilocybin microdosing does not affect emotion-related symptoms and processing: A preregistered field and lab-based study. J Psychopharmacol (Oxford, England) 36: 97–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason JW, Billingham ME, Friedman JP. (1977) Methysergide-induced heart disease: A case of multivalvular and myocardial fibrosis. Circulation 56: 889–890. [DOI] [PubMed] [Google Scholar]
- McCorvy JD, Wacker D, Wang S, et al. (2018) Structural determinants of 5-HT2B receptor activation and biased agonism. Nat Struct Mol Biol 25: 787–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenna DJ, Peroutka SJ. (1989) Differentiation of 5-hydroxytryptamine2 receptor subtypes using 125I-R- (-)2,5-dimethoxy-4-iodo-phenylisopropylamine and 3H-ketanserin. J Neurosci 9: 3482–3490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millan MJ, Maiofiss L, Cussac D, et al. (2002) Differential actions of antiparkinson agents at multiple classes of monoaminergic receptor. I. A multivariate analysis of the binding profiles of 14 drugs at 21 native and cloned human receptor subtypes. J Pharmacol Exp Ther 303: 791–804. [DOI] [PubMed] [Google Scholar]
- Mlinar B, Corradetti R. (2003) Endogenous 5-HT, released by MDMA through serotonin transporter- and secretory vesicle-dependent mechanisms, reduces hippocampal excitatory synaptic transmission by preferential activation of 5-HT1B receptors located on CA1 pyramidal neurons. Eur J Neurosci 18: 1559–1571. [DOI] [PubMed] [Google Scholar]
- Newman-Tancredi A, Cussac D, Quentric Y, et al. (2002) Differential actions of antiparkinson agents at multiple classes of monoaminergic receptor. III. Agonist and antagonist properties at serotonin, 5-HT(1) and 5-HT(2), receptor subtypes. J Pharmacol Exp Ther 303: 815–822. [DOI] [PubMed] [Google Scholar]
- Nichols DE. (2004) Hallucinogens. Pharm Ther 101: 131–181. [DOI] [PubMed] [Google Scholar]
- Orton EC, Lacerda CMR, MacLea HB. (2012) Signaling pathways in mitral valve degeneration. J Veter Cardiol 14: 7–17. [DOI] [PubMed] [Google Scholar]
- Oury C, Maréchal P, Donis N, et al. (2020) Dexfenfluramine and pergolide cause heart valve disease via valve metabolic reprogramming and ongoing matrix remodeling. Int J Mol Sci 21: 4003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacifici R, Zuccaro P, Hernandez López C, et al. (2001) Acute effects of 3,4-methylenedioxymethamphetamine alone and in combination with ethanol on the immune system in humans. J Pharm Exp Ther 296: 207–215. [PubMed] [Google Scholar]
- Papoian T, Jagadeesh G, Saulnier M, et al. (2017) Regulatory forum review*: Utility of in vitro secondary pharmacology data to assess risk of drug-induced valvular heart disease in humans: Regulatory considerations. Toxicol Pathol 45: 381–388. [DOI] [PubMed] [Google Scholar]
- Perrin VL. (1985) Clinical pharmacokinetics of ergotamine in migraine and cluster headache. Clin Pharmacokinet 10: 334–352. [DOI] [PubMed] [Google Scholar]
- Ramírez Rosas MB, Labruijere S, Villalón CM, et al. (2013) Activation of 5-hydroxytryptamine1B/1D/1F receptors as a mechanism of action of antimigraine drugs. Exp Opin Pharmacother 14: 1599–1610. [DOI] [PubMed] [Google Scholar]
- Reichmann H, Bilsing A, Ehret R, et al. (2006) Ergoline and non-ergoline derivatives in the treatment of Parkinson’s disease. J Neurol 253: iv36–iv38. [DOI] [PubMed] [Google Scholar]
- Reid T-E, Kumar K, Wang XS. (2013) Predictive in silico studies of human 5-hydroxytryptamine receptor subtype 2B (5-HT2B) and valvular heart disease. Curr Top Med Chem 13: 1353–1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rootman JM, Kiraga M, Kryskow P, et al. (2022) Psilocybin microdosers demonstrate greater observed improvements in mood and mental health at one month relative to non-microdosing controls. Sci Rep 12: 11091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth BL, Lopez E, Patel S, et al. (2000) The multiplicity of serotonin receptors: Uselessly diverse molecules or an embarrassment of Riches? Neuroscientist 6: 252–262. [Google Scholar]
- Rothman RB, Baumann MH, Savage JE, et al. (2000) Evidence for possible involvement of 5-HT(2B) receptors in the cardiac valvulopathy associated with fenfluramine and other serotonergic medications. Circulation 102: 2836–2841. [DOI] [PubMed] [Google Scholar]
- Schade R, Andersohn F, Suissa S, et al. (2007) Dopamine agonists and the risk of cardiac-valve regurgitation. New Engl J Med 356: 29–38. [DOI] [PubMed] [Google Scholar]
- Setola V, Hufeisen SJ, Grande-Allen KJ, et al. (2003) 3,4-Methylenedioxymethamphetamine (MDMA, “Ecstasy”) induces fenfluramine-like proliferative actions on human cardiac valvular interstitial cells in vitro. Mol Pharmacol 63: 1223–1229. [DOI] [PubMed] [Google Scholar]
- Shrewsbury SB, Cook RO, Taylor G, et al. (2008) Safety and pharmacokinetics of dihydroergotamine mesylate administered via a Novel (Tempo) inhaler. Headache 48: 355–367. [DOI] [PubMed] [Google Scholar]
- Smith SA, Waggoner AD, De Las Fuentes L, et al. (2009. a) Role of serotoninergic pathways in drug-induced valvular heart disease and diagnostic features by echocardiography. J Am Soc Echocardiogr 22: 883–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SR, Prosser WA, Donahue DJ, et al. (2009. b) Lorcaserin (APD356), a selective 5-HT(2C) agonist, reduces body weight in obese men and women. Obesity (Silver Spring, Md.) 17: 494–503. [DOI] [PubMed] [Google Scholar]
- Spencer DC, Hwang J, Morrell MJ. (2000) Fenfluramine–Phentermine (Fen-Phen) and seizures: Evidence for an association. Epilepsy Behav 1: 448–452. [DOI] [PubMed] [Google Scholar]
- Tagen M, Mantuani D, van Heerden L, et al. (2023) The risk of chronic psychedelic and MDMA microdosing for valvular heart disease. J Psychopharmacol (Oxford, England) 37: 876–890. [DOI] [PubMed] [Google Scholar]
- Thomsen WJ, Grottick AJ, Menzaghi F, et al. (2008) Lorcaserin, a Novel Selective Human 5-Hydroxytryptamine2C Agonist: In vitro and in vivo pharmacological characterization. J Pharm Exp Ther 325: 577–587. [DOI] [PubMed] [Google Scholar]
- U.S. Food and Drug Administration (2002) Cafergot suppositories approval letter. U.S. Food and Drug Administration, Center for Drug Evaluation and Research. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2002/09000_S022&S023_Cafergot_APPROVAL%20PACKAGE.pdf (accessed 10 July 2023). [Google Scholar]
- Vickers SP, Dourish CT, Kennett GA. (2001) Evidence that hypophagia induced by d-fenfluramine and d-norfenfluramine in the rat is mediated by 5-HT2C receptors. Neuropharmacology 41: 200–209. [DOI] [PubMed] [Google Scholar]
- Vollenweider FX, Preller KH. (2020) Psychedelic drugs: Neurobiology and potential for treatment of psychiatric disorders. Nat Rev Neurosci 21: 611–624. [DOI] [PubMed] [Google Scholar]
- Wainscott DB, Lucaites VL, Kursar JD, et al. (1996) Pharmacologic characterization of the human 5-hydroxytryptamine2B receptor: Evidence for species differences. J Pharmacol Exp Ther 276: 720–727. [PubMed] [Google Scholar]
- Wakil A, Rigby AS, Clark AL, et al. (2008) Low dose cabergoline for hyperprolactinaemia is not associated with clinically significant valvular heart disease. Eur J Endocrinol 159: R11–R14. [DOI] [PubMed] [Google Scholar]
- Winstock A, Timmerman C, Davies E, et al. (2021) 2020 pyschedelics key findings report. Glob Drug Survey. Epub ahead of print 2021. [Google Scholar]
- Zajdel P, Bednarski M, Sapa J, et al. (2015) Ergotamine and nicergoline – Facts and myths. Pharmacol Rep 67: 360–363. [DOI] [PubMed] [Google Scholar]