Abstract
Minimally invasive surgery for hallux valgus correction, has been attracting great interests in the recent decades, due to the potential benefits of less pain, decreased recovery times, smaller scars with better cosmesis, and improved early post-operative range of motion. The most recent developments in minimally invasive surgery have evolved into the third generation with modifications of the chevron-type osteotomy. This evidence-based clinical guideline of the third generation minimally invasive surgery for hallux valgus is initiated and developed collectively by the Foot and Ankle Committee of Orthopedic Branch of Chinese Medical Doctor Association, Foot and Ankle Committee of Sports Medicine Branch of Chinese Medical Doctor Association, and Foot and Ankle Expert Committee of Orthopedic Branch of the Chinese Association of the Integrative Medicine. This clinical guideline provides recommendations for indications, contraindications, operative planning and techniques, post-operative management, management of complications, and prognosis of the third generation minimally invasive surgery for hallux valgus.
The Translational Potential of this Article This comprehensive guideline aims to establish standardized recommendations for the indications, contraindications, operative techniques, and post-operative management of the third generation minimally invasive surgery for hallux valgus. By adhering to this guideline, the success rate of the procedure could be maximized. This comprehensive guideline serves as a valuable reference for practitioners interested in or preparing to perform minimally invasive surgery for hallux valgus.
Keywords: Hallux valgus, Internal fixation, Minimally invasive surgery, Osteotomy, Technique
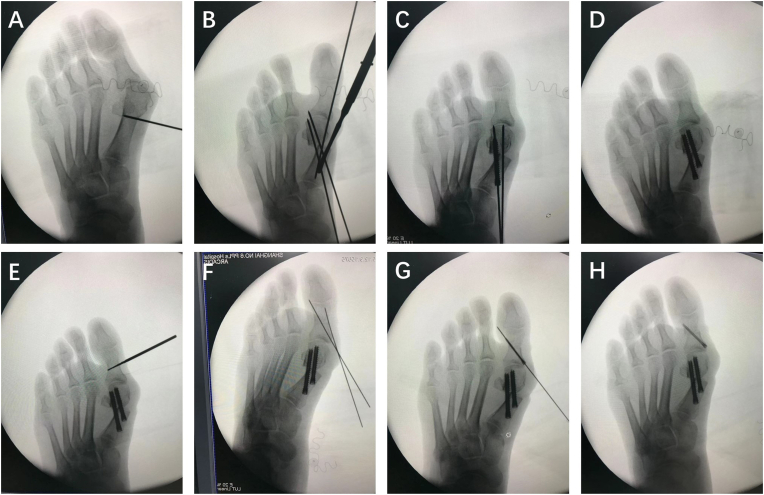
Graphical abstract
1. Background
Hallux valgus is a common progressive complex deformity of the first metatarsophalangeal joint, generally accompanied by pain or a bunion on the medial head of the first metatarsal. Traditionally, the severity of the deformity is graded based on the Hallux valgus angle (HVA): mild (15° < HVA <30°), moderate (30° < HVA <40°), or severe (HVA >40°). The angle between the first and second metatarsals, i.e. intermetatarsal angle (IMA), is also used to grade the severity of the condition: mild (IMA <10°), moderate (10° < IMA <15°), or severe (IMA >15°) [1].
When nonsurgical management fails to alleviate pain and there is a progression of deformity, surgery is indicated to reduce the deformity and correct underlying deforming forces [2]. There are hundreds of surgical treatment options available for the hallux valgus. Because of the potential perceived benefits of small incisions, minimal trauma, relative quicker recovery time, and reduced post-operative pain, minimally invasive surgery (MIS) has recently been preferred by more and more patients. At present, MIS hallux valgus surgery has evolved and advanced to the third generation with clinical evidences for achieving favorable outcomes through minimally invasive osteotomy and stable internal fixation. In order to reduce the incidence of associated complications, it is recommended for surgeons to get familiar with related surgical anatomy, gain enough experience on traditional open procedures before adoption of MIS surgery, and start extensive training of MIS hallux valgus surgery [3]. The main goal of this clinical guideline is to define and provide the details of the third generation MIS surgery for hallux valgus, in the purpose of improving clinical outcomes and reducing complication rates.
The evidence-based clinical guideline was based on a literature review and clinical expertise. A comprehensive literature search was done on the databases: Pubmed/Medline, EMBASE, Cochrane database, and Google Scholar. The following MESH terms were used: “hallux valgus”, “bunion”, “percutaneous”, “minimally invasive”, “MIS”, “MICA”, and “PERC”. The bibliographies of retrieved studies were examined to identify further articles. The search was limited to articles published in the English language.
2. History and evolution of minimally invasive surgery
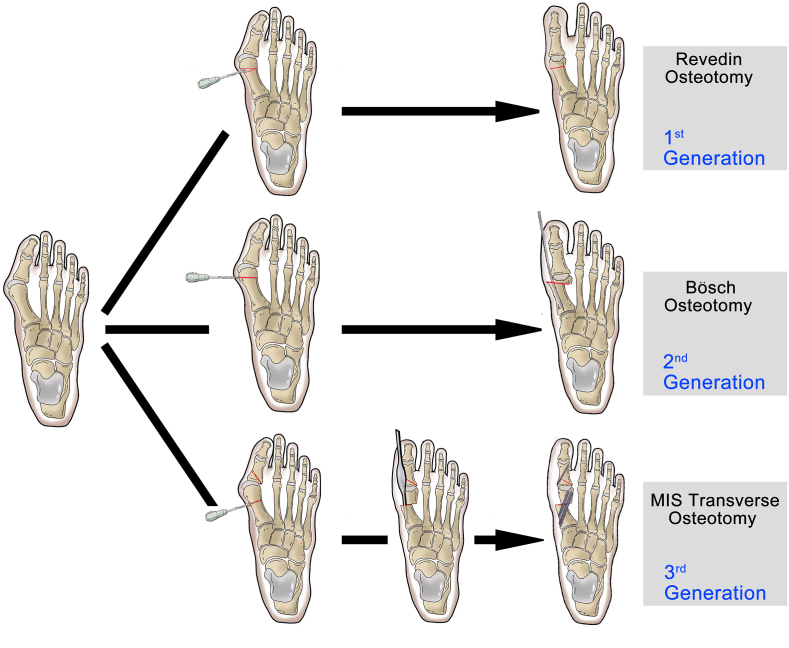
Revedin osteotomy, the first generation MIS hallux valgus surgery, is an intraarticular medial close wedge osteotomy of the head of the first metatarsal. When closing the wedge, osteoclasis of the preserved lateral cortex is achieved, adding intrinsic stability to the osteotomy without internal fixation [3,4]. Kirschner-wire is used in the Bösch osteotomy, a second generation MIS hallux valgus correction procedure, to temporarily fix the first metatarsal neck following transverse osteotomy [5,6]. The third generation MIS hallux valgus surgery has been evolved from the traditional Chevron osteotomy. Special percutaneous screw system is developed to fix and stabilize the first metatarsal osteotomy to correct the IMA, HVA, and distal metatarsal articular angle (DMAA). This procedure is carried out under fluoroscopic control through 3 to 4 small incisions with special minimally invasive power tools and Shannon burrs designed for MIS osteotomy. The third generation MIS osteotomies reported include Minimally Invasive Chevron-Akin (MICA), Percutaneous, Extra-Articular Reverse-L Chevron (PERC), Percutaneous Chevron-Akin, and Percutaneous Intra-Articular Chevron Osteotomy with variations on osteotomy sites, internal fixation types, and number of screws needed for fixation [3,7]. The third generation MICA technique has shown consistent clinical outcomes in broad applications compared to the first two generations of MIS technique. It is reported to treat some severe hallux valgus with success [8].
Vernois et al. reported HVA correction from 33.7° pre-operatively to 7.3° post-operatively and IMA correction from 14.5° pre-operatively to 5.5° post-operatively, with an overall satisfaction rate of 95 % [9]. A randomized controlled study on the treatment of hallux valgus deformity revealed comparable therapeutic effect of minimally invasive and open Chevron osteotomy for hallux valgus [10]. There were no significant differences in clinical outcomes including the Visual Analogue Scale (VAS), the forefoot scoring system of the American orthopedic foot and ankle society (AOFAS), patient satisfaction, imaging results, joint degeneration, and range of motion within 5 years post-operatively.
3. Indications and contraindications
Indication: Mild, moderate, and selected severe hallux valgus cases are indicated for MIS. In general, surgery is indicated when conservative treatment fails to manage the deformity and alleviate associated symptoms, such as pain and difficulty with shoe wear. Individuals who have relapsed symptoms and recurred deformity after previous hallux valgus surgery without any obvious first metatarsophalangeal joint degeneration, may also be indicated for MIS [11,12].
Relative contraindications: MIS procedure may not be recommended for certain patient populations, including those with advanced age and severe osteoporosis, as well as individuals with mild to moderate hallux rigidus or hallux valgus accompanied by severe metatarsal adduction. Additionally, clinical signs of instability of the first tarsometatarsal joint may also be considered as a relative contraindication for this procedure.
Contraindications: It is contraindicated to operate on patients with severe heart and lung disorders, severe peripheral vascular neuropathy, diabetes mellitus, and acute infectious diseases. It is not advised to use MIS technique to operate on patients with severe rheumatoid arthritis, severe gouty arthritis, severe metatarsophalangeal joint mismatch, severe metatarsophalangeal joint arthritis or severe hallux stiffness for reasons other than arthritis. Additional contraindications for MIS procedure include patients who are unable to comply with perioperative restrictions or have an unclear diagnosis. Furthermore, extra caution should be exercised when considering surgical intervention for patients with psychiatric disorders [13].
4. Minimally invasive surgery techniques
4.1. Pre-operative preparation
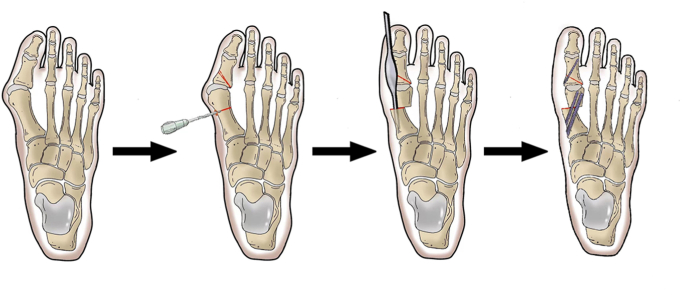
MIS requires specialized tools and instruments (Fig. 1), including regular C-arm or mini C-arm imaging equipment, specific power system for MIS, MIS Shannon burrs, MIS reduction tools, miniature rasps and periosteum elevators, standard instrument sets for orthopedic foot surgery and Kirschner-wires [14,15].
Fig. 1.
MIS instruments and tools. A. Specific power system for MIS, with different attachment options; B. Beaver blade, MIS reduction tools, miniature rasps (from left to right) C. MIS Shannon burrs.
Pre-operative preparation is critical for successful MIS. Patient is positioned in a supine position with operated foot situated at or beyond the edge of the operating table for easy access and intra-operative imaging assessment. The use of tourniquet is optional as it may increase the chances of thermal damage due to rapid rotation speed of the Shannon burr. Operating without tourniquets has the advantage of utilizing the cooling effect of blood flow to reduce potential thermal damage [16]. However, some experts believe that tourniquet may be beneficial for the surgeons during their initial learning curve. Copious saline irrigation should be used to reduce heat effect in this situation. C-arm is conventionally employed for the surgical procedure. The operated foot is usually positioned in a supine position on the radiolucent table with C-arm situated over the side of foot. Alternatively, the operated foot can be positioned directly on the C-arm image intensifier. The surgeon positions him or herself at the medial side of the operated foot for easy access [14,17].
MIS requires sufficient power to facilitate a quick and safe osteotomy with relative low speed and high torque in power setting [18]. Shannon burrs are usually utilized for osteotomy in MIS procedures. It is recommended that Shannon burrs with appropriate diameters (1.8, 2.0, and 2.5 mm) and cutting lengths (8–20 mm) be used. Additionally, a flushing cooling irrigation should be applied to prevent thermal damage resulting in local bone necrosis and impaired healing.
4.2. Operative techniques of MIS
Minimally invasive Chevron-Akin osteotomy (MICA) and percutaneous minimally invasive metatarsal transverse osteotomy are the two most frequently utilized osteotomy procedures for the third generation MIS. Compared to the traditional Chevron osteotomy, the location of the osteotomy in MICA is extracapsular and located in close proximity to the first metatarsal neck. The extra-articular osteotomy may offer advantages over the intra-articular osteotomy in several key aspects [[18], [19], [20]]: (1) The extra-articular osteotomy procedure minimizes capsular trauma, in which efforts are made to preserve the proximal attachment of the capsule intact. (2) The intra-articular osteotomy created with a Shannon burr inevitably generates bony debris, which may persist within the joint despite thorough irrigation. The residual debris could potentially result in postoperative arthrofibrosis, discomfort, and stiffness. (3) The extra-articular osteotomy allows for greater translation and rotational correction, as the capital fragment mobility is not restricted by capsular tightness.
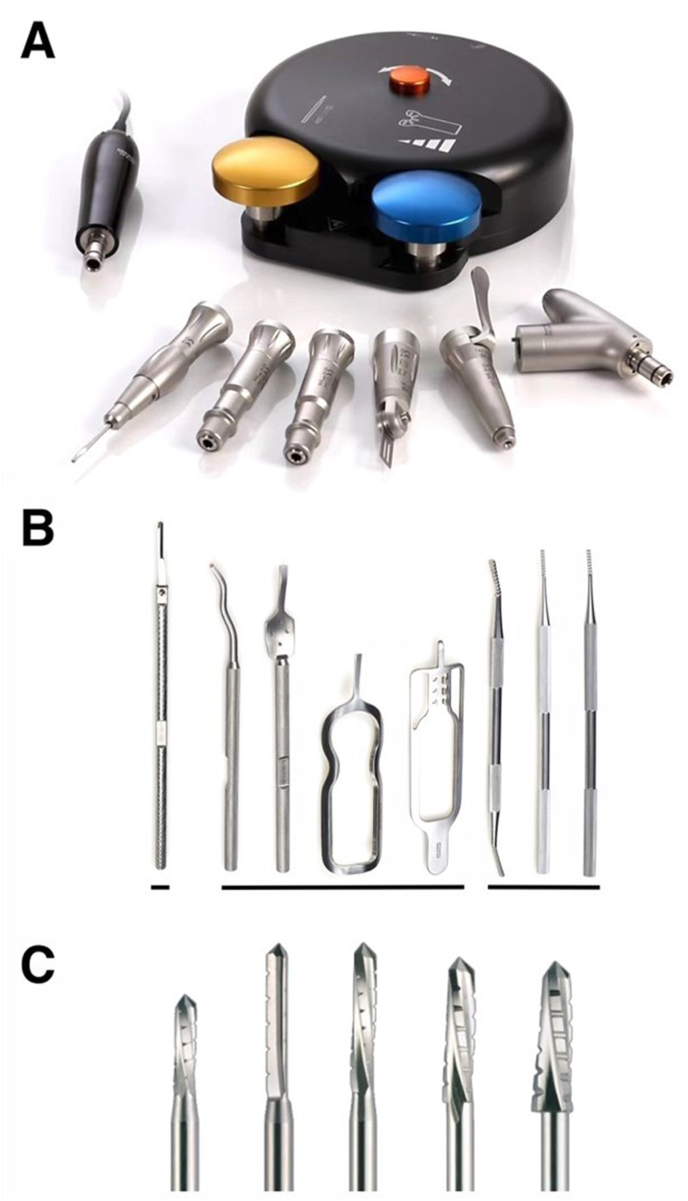
The use of a guide pin before osteotomy helps with further reduction and fixation after osteotomy [14]. The guide pin is usually inserted at the midpoint in dorsal plantar dimension of the medial base of the first metatarsal and advanced to penetrate the lateral cortex just proximal to the distal osteotomy site. Bi-cortical fixation is essential to maintain the stability of the osteotomized fragments in the desirable reduced position [21,22]. A periosteum elevator is utilized to release and protect the surrounding soft tissue prior to osteotomy. After identifying the planned V-shaped osteotomy apex, the surgeon may proceed MICA with a Shannon burr in dorsal and plantar-proximal directions [10,23]. Proper orientation of the osteotomy is critical to achieve the desired correction and to avoid alignment complications including excessive shortening or lengthening of the metatarsal axially, or sagittal elevation or depression of the metatarsal head. Percutaneous minimally invasive metatarsal transverse osteotomy, is another minimally invasive surgical technique that utilizes the same anatomical landmark for osteotomy as MICA, with the difference being a transverse osteotomy [14]. Radiographs demonstrating key operative steps of the percutaneous transverse osteotomy combined with Akin osteotomy, are shown in Fig. 2. Biomechanical studies on the two MIS hallux valgus correction procedures revealed no significant variations in terms of the ultimate load, yield load, and fixation strength [21]. Recent studies have validated significant malrotation of the first metatarsal in hallux valgus deformity, emphasizing the importance of addressing this rotational component as part of the comprehensive deformity correction [24,25]. In the aspect of rotational correction, the transverse osteotomy might demonstrate potential superiority when compared to MICA [18].
Fig. 2.
Intra-operative fluoroscopy images demonstrating the key operative steps of the third generation percutaneous minimally invasive metatarsal transverse osteotomy (A) Transverse extra-articular osteotomy (B) Lateral translation of the first metatarsal head using a MIS reduction tool, and temporary fixation with Kirschner-wires to avoid loss of reduction (C) Insertion of the first full-threaded cannulated screw through the guide pin (D) Insertion of the second cannulated screw in a similar manner (E) Percutaneous Akin osteotomy (F) Placement of guide pin after Akin osteotomy (G) Percutaneous Akin osteotomy fixation (H) Final correction.
Reduction and realignment of the osteotomized first metatarsal is usually achieved with the aid of specialized reduction instruments, including release hooks and coronal plane translators. Lateral joint capsule and adjacent soft tissue can be selectively released creating space for lateral translation of the metatarsal head [3,26]. The first metatarsal head is translated laterally to correct HVA and IMA by inserting a translator into the medullary canal through the medial osteotomy site [27,28]. The hallux is kept in adduction to prevent lateral angulation. Pronation deformity can be corrected with a controlled metatarsal head rotation. Care should be taken to prevent excessive plantar translation of the first metatarsal head during reduction and realignment. Fluoroscopic assessment should be performed in key steps of the MIS procedure to ensure proper reduction. An ideal reduced position of 0° HVA and proper alignment of the first metatarsophalangeal joint should be strived for in the anteroposterior view radiograph. In the lateral view, the distal cortex of the first metatarsal should be lined up in parallel to the proximal cortex along the metatarsal longitudinal axis [3,26]. In cases where it is challenging to reach a 0° reduction of HVA after metatarsal osteotomy, adjunctive Akin osteotomy or lateral soft tissue release may be indicated. After a satisfactory reduction and realignment, temporary fixation with Kirschner-wires are used to avoid loss of reduction.
The core of the third generation MIS technique is the use of specialized internal fixation system following osteotomy reduction. This approach enables early weight-bearing and motion, which has been shown to reduce the risk of joint stiffness post-operatively [3]. The placement of the first metatarsal shaft screw is a critical step. A preset guide pin is advanced into the metatarsal head from the medial base of first metatarsal after reduction. It is crucial to obtain an “in–out-in” trajectory of guide pin from the medial base of first metatarsal through the osteotomy site and to the realigned metatarsal head. The guide pin is to be placed parallel to the long axis of the first metatarsal in the sagittal position [17]. Fluoroscopic guidance should be used to monitor the guide pin passing through the medial and lateral cortex of the proximal osteotomy, and reaching the lateral cortex of the metatarsal head. The first full-threaded cannulated screw is inserted through the guide pin without compression. In many cases, a second cannulated screw is placed in a similar manner parallel to the first cannulated screw for additional stability [26,29].
In order to prevent potential soft tissue irritation after fixation, the utilization of beveled headless cannulated screws may be considered. The diameter of 4.0–5.0 mm could be chosen for the first proximal cannulated screw, while a smaller diameter (3.0–4.0 mm) screw is indicated for the second distal one [12,16]. Bioabsorbable screws can be used for internal fixation. However, there are reports of removal difficulty due to its tendency to expand [30]. While metal intramedullary plates can be used as an alternative fixation method during MIS for hallux valgus correction, there are concerns regarding the limited displacement of the metatarsal head that can be achieved with these plates due to design restrictions.
A minimally invasive Akin osteotomy is commonly used in conjunction of the MIS first metatarsal osteotomy. It is a medial closed wedge osteotomy of the proximal phalangeal shaft through a medial small incision with a Shannon burr [31]. The osteotomy is usually fixed and stabilized by a 2.0–3.0 mm cannulated screw.
The necessity of lateral soft tissue release in MIS is still a topic of debate [30]. The congruency of the first metatarsophalangeal joint and lateral soft tissue tension should always be evaluated before closure [32,33]. Lateral release is suggested when there is persistent deformity or inadequate reduction of the sesamoids [14].
Collectively, MIS is anticipated to yield improved results with minor soft tissue complications and reduced stiffness, due to the smaller medial scar, limited operative exposure, and the extra-articular osteotomy [12,18,34,35]. The surgical protocols mentioned above have been illustrated in a flow diagram, which specifically displays the details of the percutaneous minimally invasive metatarsal transverse osteotomy procedure (Fig. 3). Distinguished surgical techniques of the generation MIS hallux valgus correction procedures, are also demonstrated in the diagram for comparison.
Fig. 3.
Representation of key steps in the first, second and third generation MIS for hallux valgus correction.
4.3. Post-operative management
Specialized protocol of post-operative dressing is an important component of MIS for hallux valgus. Standardized dressing techniques are essential for preserving post-operative soft tissue balance and preventing recurrence [5]. Sterile gauzes are placed in the first web space. A constant pressure to maintain the neutral position of the hallux at the first metatarsophalangeal joint is applied during the wrapping of forefoot surgical wound. The rest of the toe web space are also separated with sterile gauzes and wrapped, with the hallux in a staggered fashion and stabilized with bandages extending beyond the osteotomy area to reinforce strength of dressing. Toes and nails need to be exposed at the distal ends of the bandage to facilitate early active range of motion and observation of blood supply [13].
Post-operative care and rehabilitation are important for the success of MIS [36]. Immediately after the procedure, patients are advised to wear forefoot offloading shoes or walking boots with partial weight bearing as tolerated. The operated limb should be kept in elevation when possible. Usual exercises are advised to prevent joint stiffness in the hip, knee, ankle, and toe joints. Active muscle activities are also encouraged to prevent muscle atrophy and reduce swelling [37]. Sutures are usually removed in 2 weeks post-operatively. Physiotherapy can commence once the surgical wound has healed. During the next six weeks of the recovery period, the hallux should be checked weekly for maintenance of a neutral position with regular dressing or customized brace. Patients with severe pre-operative deformities may benefit from a prolonged use of a toe spacer placed in the first web space. After six weeks, patients can usually be allowed to start exercises of swimming or cycling in sneakers with wide forefeet toe box for the following three to six months. Full weight bearing without restriction and sport activities can resume four to six months post-operatively, based on clinical and imaging evaluation for complete bone healing. Weight bearing radiographs are recommended for clinical evaluation at six weeks, three months, six months, and one year post-operatively [1,12].
4.4. Complications
In general, the spectrum of potential complications in MIS is similar to that in traditional open surgery [38]. However, MIS procedures may introduce specific complications absent in open surgery, such as damage to soft tissue structures not directly visible or thermal lesions of the skin. Third generation MIS for hallux valgus has been reported with a post-operative complication rate of 10 % [34]. The most common reported complications include recurrence, malunion, delayed or nonunion, transfer metatarsalgia, intractable foot pain, superficial or deep infection, deep vein thrombosis, local sensation deficits, joint stiffness, osteoarthritis, and implant failures [38]. The incidence of deformity recurrence in MICA surgery is 0.9 %, with the probability of nerve and tendon injury ranging from 0 % to 5 %, wound-related complications occurring in approximately 4 % of cases, and post-operative first metatarsophalangeal joint pain with a probability of 1.5 % [27].
To avoid the recurrence of hallux valgus, it is essential to achieve proper correction of the proximal articular set angle and realign the forces of tendons [39,40]. Consequently, in most cases, it is advisable to consider an additional Akin procedure. Another critical factor in recurrence prevention lies in the thoughtful selection of the appropriate osteotomy for correcting the first metatarsal. If the lack of plantarization or excessive shortening of the first metatarsal/overlength of the lesser rays are observed intra-operatively, percutaneous distal metatarsal metaphyseal osteotomy (DMMO) or Weil osteotomy of the lesser metatarsals is advisable to lower the incidence of transfer metatarsalgia [38,41].
Due to small incisions in MIS, infection rate is reported to be significantly lower than that in open surgery [42]. Specifically, extra caution should be taken in the utilization of Shannon burrs for osteotomy to avoid thermal damage of the skin and bone tissue, which could further lower the infection incidence. Thermal damage of the bone tissue could also lead to the delayed union or nonunion. Several recommendations are advocated to reduce the risk of iatrogenic thermal injury, including use of sharp burrs, an irrigated micromotor with high torque and low speed, shorter burr time and absence of a tourniquet [18,38]. While transient post-operative dysesthesia caused by soft tissue swelling or bruising is frequently observed, the occurrence of persistent paresthesia attributed to nerve injury is rare in MIS [43,44]. Knowledge of a safe-zone medially and laterally to the extensor hallucis longus tendon, is critical to precisely perform these procedures, avoiding the nerve and tendon injury [45]. Despite the theoretical advantages of extra-articular osteotomy aforementioned, a recent systematic review reported stiffness of the first metatarsophalangeal joint in 9.8 % of cases [46]. To maintain mobility, it is advisable to initiate active and passive mobilization of the metatarsophalangeal joint as soon as one week post-operatively.
In the management of complications, it is paramount to adhere to established principles, similar to those employed in open surgery [38]. Initially, nonoperative treatment should be tried. Should nonoperative approaches prove unfeasible, a surgical intervention is imperative. The choice between percutaneous or open techniques is contingent upon the specific case and the proficiency of the surgeon. It is crucial to underscore that rigorous training is pivotal in reducing complications, including cadaveric training and visiting experienced colleagues.
4.5. Prognosis
Consistent with other studies [26,40], our experience showed that the third generation MIS technique for correcting hallux valgus could achieve similar deformity correction and clinical outcomes compared to traditional open methods, while also presenting its own distinct set of complications. MIS for hallux valgus correction has been reported so far to be an effective surgical option with likely improved imaging and clinical outcomes (Fig. 4), as demonstrated by a recent meta-analysis [47]. As a specific MIS technique, the transverse osteotomy exhibits comparable efficacy as other MIS techniques, such as MICA and PERC. Prognostic indicators being utilized to evaluate the efficacy of MIS include the post-operative function of the affected limb (AOFAS forefoot score), traditional radiographic parameters (HVA and IMA), post-operative complications, post-operative pain (visual analogue scale VAS score), patient satisfaction, wound healing, and reoperation rate [14,47]. It is important to note that the learning curve of surgeons is also closely related with the prognosis [29]. The efficacy of MIS may be compromised when a surgeon does not fully appreciate the significance of comprehensive training and understanding the potential limits inherent to the technique.
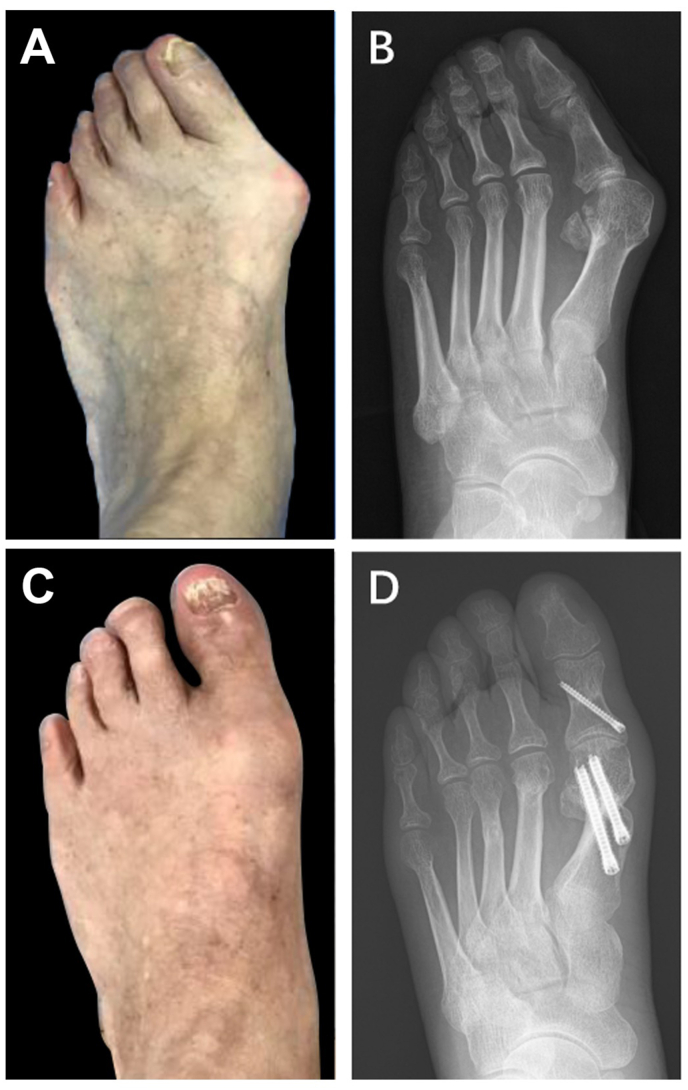
Fig. 4.
Preo-perative and 10-month post-operative condition of a patient who underwent the third generation MIS procedure (A) Pre-operative clinical photograph (B) Pre-operative radiograph (C) 10-month post-operative clinical photograph (D) 10-month posto-perative radiograph.
5. Disadvantages of MIS
While MIS has gained recognition as an effective and safe approach for hallux valgus correction with increased popularity, it is important to acknowledge certain disadvantages of MIS when compared to traditional open surgery. These limits include: (1) Radiation exposure is increased in MIS procedure [48,49]. The utilization of a mini C-arm might be beneficial in percutaneous foot surgery. (2) There is insufficient precision in controlling osteotomy position and shortening of the first metatarsal [44,50]. Thickness of the burr and absence of intrinsic stability of the osteotomy entails bone loss which leads to excessive shortening of the metatarsal. Dorsal or plantar malalignment has also been reported in previous literature [51]. (3) MIS technique often requires an extensive learning curve [3,49]. Learning curve demonstrated a consistent improvement in terms of surgery duration and amount of fluoroscopy shots. Specific cadaveric training and intensive practice is strongly recommended, which is vital in minimizing the learning curve. (4) Neurovascular and tendinous structures are at risk of iatrogenic injury, due to indirect visualization during the procedure [38,45]. A sound knowledge of relative anatomical structures and safety zones is paramount. (5) Despite promising clinic outcomes of MIS in the treatment of severe hallux valgus reported in some studies [[52], [53], [54], [55]], MIS technique has been classically indicated for mild to moderate hallux valgus [43,56]. The main concern in the correction of a larger deformity is the insufficient bony contact between the head and shaft [57]. In addition, pre-operative HVA (≥40°) and post-operative tibial sesamoid position were reported to be closely associated with deformity recurrence [52].
6. Conclusion
The adoption of minimally invasive hallux valgus surgery has been on a consistent rise in the recent years, with higher acceptance rate among patients and surgeons. According to the clinical guideline, the use of third generation minimally invasive hallux valgus technique should be standardized. Specifically, a summary of relevant recommendations is addressed and outlined (Table 1). Surgical indications should be strictly controlled and observed. Surgeons are advised to undergo extensive training to get familiar with relevant anatomy, and become proficient in performing MIS osteotomy and internal fixation techniques to achieve improved the clinical outcomes.
Table 1.
Summary of Recommendations on the third generation minimally invasive surgery for hallux valgus.
| Recommendations | |
|---|---|
| Indications & Contraindication | 1. Third generation MIS technique is an effective modality for surgical correction of patients with mild to moderate hallux valgus. |
| 2. For patients with severe hallux valgus, the surgical planning and strategy should be assessed on a case-by-case basis considering the patient's individual pathology and the expertise of the surgeon. | |
| Pre-Operative | 1. Radiation protection precautions for both patients and surgeons are necessary, despite the relative low dose of radiation. |
| 2. It is preferable and advisable to use a specialized power system that meets the requirements of low speed and high torque power setting. | |
| 3. Selection of an appropriate type and size of Shannon burr is crucial for achieving optimal outcomes during osteotomy procedures. | |
| Intra-Operative | 1. Third generation MIS adopts an extracapsular osteotomy site proximal to the neck of the first metatarsal. |
| 2. The direction and angle of the osteotomy should be carefully planned and executed to achieve the desired correction while minimizing the complications. | |
| 3. Specialized reduction tools are recommended for effective reduction. | |
| 4. It is important to note that there is a learning curve in achieving reliable osteotomy, reduction and internal fixation. | |
| 5. The severity of hallux valgus is closely related to the degree of lateral translation required for metatarsal head realignment. | |
| 6. Guide pins for fixation screws should be inserted before osteotomy. | |
| 7. The “in–out-in” technique is critical when inserting screws to achieve sufficient stability. | |
| 8. Fully threaded cannulated screws are advocated to enhance stability. | |
| 9. It is still controversial whether lateral soft tissue release is necessary in MIS for hallux valgus. | |
| Post-Operative | 1. Standard dressing technique or a special brace to maintain the hallux in a neutral position is recommended post-operatively for 4–6 weeks. |
| 2. It is crucial to implement standardized functional rehabilitation program to maintain the surgical outcome and prevent complications such as joint stiffness. | |
| 3. It is important to note the risks of post-operative complications in MIS for hallux valgus despite its advocated advantages of a less invasive approach than the traditional open osteotomy surgery. |
Declaration of competing interest
All authors declare no conflicts of interest. This clinical guideline was published in Chinese first in Zhongguo Gu Shang Za Zhi (China Journal of Orthopaedics and Traumatology) in September 2022 (https://doi.org/10.12200/j.issn.1003-0034.2022.09.003) [58], this English edition was published with modifications from the published Chinese version, with full permission granted from the China Journal of Orthopaedics and Traumatology (Zhongguo Gu Shang Za Zhi).
Declaration of AI and AI-assisted technologies
No authoritative AI and AI-assisted technologies were used in manuscript drafting, production of figures, images and artworks.
Declaration of competing interest
All authors declare no conflicts of interest. This clinical guideline was published in Chinese first in Zhongguo Gu Shang Za Zhi (China Journal of Orthopaedics and Traumatology) in September 2022, this English edition was published with slight modifications from the published Chinese version, with full permission granted from the China Journal of Orthopaedics and Traumatology (Zhongguo Gu Shang Za Zhi).
Acknowledgement
No funding was used in this work.
Contributor Information
Zhongmin Shi, Email: liuyuanzuhuai@163.com.
Xin Ma, Email: maxinshhs@126.com.
References
- 1.Easley M.E., Trnka H.J. Current concepts review: hallux valgus part 1: pathomechanics, clinical assessment, and nonoperative management. Foot Ankle Int. 2007;28(5):654–659. doi: 10.3113/FAI.2007.0654. [DOI] [PubMed] [Google Scholar]
- 2.Shi G.G., Whalen J.L., Turner N.S., 3rd, Kitaoka H.B. Operative approach to adult hallux valgus deformity: principles and techniques. J Am Acad Orthop Surg. 2020;28(10):410–418. doi: 10.5435/JAAOS-D-19-00324. [DOI] [PubMed] [Google Scholar]
- 3.Del Vecchio J.J., Ghioldi M.E. Evolution of minimally invasive surgery in hallux valgus. Foot Ankle Clin. 2020;25(1):79–95. doi: 10.1016/j.fcl.2019.10.010. [DOI] [PubMed] [Google Scholar]
- 4.Biz C., Fosser M., Dalmau-Pastor M., Corradin M., Roda M.G., Aldegheri R., et al. Functional and radiographic outcomes of hallux valgus correction by mini-invasive surgery with Reverdin-Isham and Akin percutaneous osteotomies: a longitudinal prospective study with a 48-month follow-up. J Orthop Surg Res. 2016;11(1):157. doi: 10.1186/s13018-016-0491-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maffulli N., Longo U.G., Oliva F., Denaro V., Coppola C. Bosch osteotomy and scarf osteotomy for hallux valgus correction. Orthop Clin N Am. 2009;40(4):515–524. doi: 10.1016/j.ocl.2009.06.003. ix-x. [DOI] [PubMed] [Google Scholar]
- 6.Radwan Y.A., Mansour A.M. Percutaneous distal metatarsal osteotomy versus distal chevron osteotomy for correction of mild-to-moderate hallux valgus deformity. Arch Orthop Trauma Surg. 2012;132(11):1539–1546. doi: 10.1007/s00402-012-1585-5. [DOI] [PubMed] [Google Scholar]
- 7.Lam K.-L.K., Kong S.-W., Chow Y.-H. Percutaneous chevron osteotomy in treating hallux valgus: Hong Kong experience and mid-term results. J Orthopaed Trauma Rehabil. 2015;19(1):25–30. [Google Scholar]
- 8.Trnka H.J. Percutaneous, MIS and open hallux valgus surgery. EFORT Open Rev. 2021;6(6):432–438. doi: 10.1302/2058-5241.6.210029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vernois J., Redfern D.J. Percutaneous surgery for severe hallux valgus. Foot Ankle Clin. 2016;21(3):479–493. doi: 10.1016/j.fcl.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 10.Kaufmann G., Mortlbauer L., Hofer-Picout P., Dammerer D., Ban M., Liebensteiner M. Five-year follow-up of minimally invasive distal metatarsal chevron osteotomy in comparison with the open technique: a randomized controlled trial. J Bone Joint Surg Am. 2020;102(10):873–879. doi: 10.2106/JBJS.19.00981. [DOI] [PubMed] [Google Scholar]
- 11.Lam P., Lee M., Xing J., Di Nallo M. Percutaneous surgery for mild to moderate hallux valgus. Foot Ankle Clin. 2016;21(3):459–477. doi: 10.1016/j.fcl.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 12.Brogan K., Voller T., Gee C., Borbely T., Palmer S. Third-generation minimally invasive correction of hallux valgus: technique and early outcomes. Int Orthop. 2014;38(10):2115–2121. doi: 10.1007/s00264-014-2500-1. [DOI] [PubMed] [Google Scholar]
- 13.Schipper O.N., Day J., Ray G.S., Johnson A.H. Percutaneous techniques in orthopedic foot and ankle surgery. Orthop Clin N Am. 2020;51(3):403–422. doi: 10.1016/j.ocl.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Neufeld S.K., Dean D., Hussaini S. Outcomes and surgical strategies of minimally invasive chevron/akin procedures. Foot Ankle Int. 2021;42(6):676–688. doi: 10.1177/1071100720982967. [DOI] [PubMed] [Google Scholar]
- 15.Ferreira G.F., Nunes G.A., Mattos E.D.M.C., Pedroso J.P., Lewis T.L., Lam P., et al. Technique Tip: medial prominence bone spur resection in the third-generation percutaneous Chevron-Akin Osteotomy Technique (PECA) for hallux valgus correction. Foot Ankle Surg. 2022;28(4):460–463. doi: 10.1016/j.fas.2021.11.004. [DOI] [PubMed] [Google Scholar]
- 16.Lee M., Walsh J., Smith M.M., Ling J., Wines A., Lam P. Hallux valgus correction comparing percutaneous chevron/akin (PECA) and open scarf/akin osteotomies. Foot Ankle Int. 2017;38(8):838–846. doi: 10.1177/1071100717704941. [DOI] [PubMed] [Google Scholar]
- 17.Toepfer A., Strassle M. 3rd generation MICA with the "K-wires-first technique" - a step-by-step instruction and preliminary results. BMC Muscoskel Disord. 2022;23(1):66. doi: 10.1186/s12891-021-04972-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewis T.L., Lau B., Alkhalfan Y., Trowbridge S., Gordon D., Vernois J., et al. Fourth-generation minimally invasive hallux valgus surgery with metaphyseal extra-articular transverse and Akin osteotomy (META): 12 Month clinical and radiologic results. Foot Ankle Int. 2023;44(3):178–191. doi: 10.1177/10711007231152491. [DOI] [PubMed] [Google Scholar]
- 19.Lucas y, Hernandez J., Golano P., Roshan-Zamir S., Darcel V., Chauveaux D., et al. Treatment of moderate hallux valgus by percutaneous, extra-articular reverse-L Chevron (PERC) osteotomy. Bone Joint Lett J. 2016;98-B(3):365–373. doi: 10.1302/0301-620X.98B3.35666. [DOI] [PubMed] [Google Scholar]
- 20.Chin K.M., Richardson N.S., Campbell J.T., Jeng C.L., Christian M.W., Cerrato R.A. The hallux metatarsophalangeal capsule: an anatomic study with respect to percutaneous hallux valgus correction. Foot Ankle Int. 2022;43(1):86–90. doi: 10.1177/10711007211027262. [DOI] [PubMed] [Google Scholar]
- 21.Aiyer A., Massel D.H., Siddiqui N., Acevedo J.I. Biomechanical comparison of 2 common techniques of minimally invasive hallux valgus correction. Foot Ankle Int. 2021;42(3):373–380. doi: 10.1177/1071100720959029. [DOI] [PubMed] [Google Scholar]
- 22.Lewis T.L., Ray R., Robinson P., Dearden P.M.C., Goff T.J., Gordon D., et al. Letter regarding: biomechanical comparison of 2 common techniques of minimally invasive hallux valgus correction. Foot Ankle Int. 2021;42(3):381–382. doi: 10.1177/1071100721992753. [eng] [DOI] [PubMed] [Google Scholar]
- 23.Redfern D. Minimally invasive chevron Akin (MICA) for correction of hallux valgus. Tech Foot Ankle Surg. 2020;19(3):132–141. [Google Scholar]
- 24.Steadman J., Barg A., Saltzman C.L. First metatarsal rotation in hallux valgus deformity. Foot Ankle Int. 2021;42(4):510–522. doi: 10.1177/1071100721997149. [eng] [DOI] [PubMed] [Google Scholar]
- 25.Najefi A.A., Katmeh R., Zaveri A.K., Alsafi M.K., Garrick F., Malhotra K., et al. Imaging findings and first metatarsal rotation in hallux valgus. Foot Ankle Int. 2022;43(5):665–675. doi: 10.1177/10711007211064609. [eng] [DOI] [PubMed] [Google Scholar]
- 26.Holme T.J., Sivaloganathan S.S., Patel B., Kunasingam K. Third-generation minimally invasive chevron Akin osteotomy for hallux valgus. Foot Ankle Int. 2020;41(1):50–56. doi: 10.1177/1071100719874360. [DOI] [PubMed] [Google Scholar]
- 27.Malagelada F., Sahirad C., Dalmau-Pastor M., Vega J., Bhumbra R., Manzanares-Cespedes M.C., et al. Minimally invasive surgery for hallux valgus: a systematic review of current surgical techniques. Int Orthop. 2019;43(3):625–637. doi: 10.1007/s00264-018-4138-x. [DOI] [PubMed] [Google Scholar]
- 28.Tay A.Y.W., Goh G.S., Koo K., Yeo N.E.M. Third-generation minimally invasive chevron-akin osteotomy for hallux valgus produces similar clinical and radiological outcomes as scarf-akin osteotomy at 2 Years: a matched cohort study. Foot Ankle Int. 2022;43(3):321–330. doi: 10.1177/10711007211049193. [DOI] [PubMed] [Google Scholar]
- 29.Jowett C.R.J., Bedi H.S. Preliminary results and learning curve of the minimally invasive chevron Akin operation for hallux valgus. J Foot Ankle Surg. 2017;56(3):445–452. doi: 10.1053/j.jfas.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Del Vecchio J.J., Cordier G., Dealbera E.D., Slullitel G., Lopez V., Manzanares-Cespedes M.C., et al. Correction power of percutaneous adductor tendon release (PATR) for the treatment of hallux valgus: a cadaveric study. J Foot Ankle Surg. 2021;60(6):1103–1109. doi: 10.1053/j.jfas.2021.02.012. [DOI] [PubMed] [Google Scholar]
- 31.Liszka H., Gadek A. Percutaneous transosseous suture fixation of the Akin osteotomy and minimally invasive chevron for correction of hallux valgus. Foot Ankle Int. 2020;41(9):1079–1091. doi: 10.1177/1071100720935036. [DOI] [PubMed] [Google Scholar]
- 32.Silver D. The operative treatment of hallux valgus. J Bone Joint Surg Am. 1923;5:225–232. [Google Scholar]
- 33.Hromadka R., Bartak V., Bek J., Popelka S., Jr., Bednarova J., Popelka S. Lateral release in hallux valgus deformity: from anatomic study to surgical tip. J Foot Ankle Surg. 2013;52(3):298–302. doi: 10.1053/j.jfas.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 34.Jeyaseelan L., Malagelada F. Minimally invasive hallux valgus surgery-A systematic review and assessment of state of the art. Foot Ankle Clin. 2020;25(3):345–359. doi: 10.1016/j.fcl.2020.05.001. [DOI] [PubMed] [Google Scholar]
- 35.Redfern D., Vernois J. Letter regarding: stiffness and range of motion after minimally invasive chevron-akin and open scarf-akin procedures. Foot Ankle Int. 2019;40(8):987–989. doi: 10.1177/1071100719863710. [eng] [DOI] [PubMed] [Google Scholar]
- 36.Ling S.K.K., Wu Y.M., Li C., Lui T.H., Yung P.S. Randomised control trial on the optimal duration of non-weight-bearing walking after hallux valgus surgery. J Orthop Translat. 2020;23:61–66. doi: 10.1016/j.jot.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qin Y.-X., Xia Y., Muir J., Lin W., Rubin C.T. Quantitative ultrasound imaging monitoring progressive disuse osteopenia and mechanical stimulation mitigation in calcaneus region through a 90-day bed rest human study. J Orthopaed Transl. 2019;18:48–58. doi: 10.1016/j.jot.2018.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hochheuser G. Complications of minimally invasive surgery for hallux valgus and how to deal with them. Foot Ankle Clin. 2020;25(3):399–406. doi: 10.1016/j.fcl.2020.04.002. [DOI] [PubMed] [Google Scholar]
- 39.Chan C.X., Gan J.Z., Chong H.C., Rikhraj Singh I., Ng S.Y.C., Koo K. Two year outcomes of minimally invasive hallux valgus surgery. Foot Ankle Surg. 2019;25(2):119–126. doi: 10.1016/j.fas.2017.09.007. [eng] [DOI] [PubMed] [Google Scholar]
- 40.Kaufmann G., Dammerer D., Heyenbrock F., Braito M., Moertlbauer L., Liebensteiner M. Minimally invasive versus open chevron osteotomy for hallux valgus correction: a randomized controlled trial. Int Orthop. 2019;43(2):343–350. doi: 10.1007/s00264-018-4006-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miranda M.A.M., Martins C., Cortegana I.M., Campos G., Pérez M.F.M., Oliva X.M. Complications on percutaneous hallux valgus surgery: a systematic review. J Foot Ankle Surg. 2021;60(3):548–554. doi: 10.1053/j.jfas.2020.06.015. [eng] [DOI] [PubMed] [Google Scholar]
- 42.Yassin M., Bowirat A., Robinson D. Percutaneous surgery of the forefoot compared with open technique - functional results, complications and patient satisfaction. Foot Ankle Surg. 2020;26(2):156–162. doi: 10.1016/j.fas.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 43.Bauer T., de Lavigne C., Biau D., De Prado M., Isham S., Laffenétre O. Percutaneous hallux valgus surgery: a prospective multicenter study of 189 cases. Orthop Clin N Am. 2009;40(4):505–514. doi: 10.1016/j.ocl.2009.05.002. ix. [eng] [DOI] [PubMed] [Google Scholar]
- 44.De Prado M. Complications in minimally invasive foot surgery. Fuß Sprunggelenk. 2013;11(2):83–94. [Google Scholar]
- 45.Malagelada F., Dalmau-Pastor M., Fargues B., Manzanares-Céspedes M.C., Peña F., Vega J. Increasing the safety of minimally invasive hallux surgery-An anatomical study introducing the clock method. Foot Ankle Surg. 2018;24(1):40–44. doi: 10.1016/j.fas.2016.11.004. [eng] [DOI] [PubMed] [Google Scholar]
- 46.Bia A., Guerra-Pinto F., Pereira B.S., Corte-Real N., Oliva X.M. Percutaneous osteotomies in hallux valgus: a systematic review. J Foot Ankle Surg. 2018;57(1):123–130. doi: 10.1053/j.jfas.2017.06.027. [eng] [DOI] [PubMed] [Google Scholar]
- 47.Ji L., Wang K., Ding S., Sun C., Sun S., Zhang M. Minimally invasive vs. Open surgery for hallux valgus: a meta-analysis. Front Surg. 2022;9 doi: 10.3389/fsurg.2022.843410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Torrent J., Baduell A., Vega J., Malagelada F., Luna R., Rabat E. Open vs minimally invasive scarf osteotomy for hallux valgus correction: a randomized controlled trial. Foot Ankle Int. 2021;42(8):982–993. doi: 10.1177/10711007211003565. [DOI] [PubMed] [Google Scholar]
- 49.Toepfer A., Strässle M. The percutaneous learning curve of 3rd generation minimally-invasive Chevron and Akin osteotomy (MICA) Foot Ankle Surg. 2022;28(8):1389–1398. doi: 10.1016/j.fas.2022.07.006. [DOI] [PubMed] [Google Scholar]
- 50.Bauer T. Percutaneous forefoot surgery. J Orthop Traumatol: Surg Res. 2014;100(1):S191–S204. doi: 10.1016/j.otsr.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 51.Trnka H.J., Krenn S., Schuh R. Minimally invasive hallux valgus surgery: a critical review of the evidence. Int Orthop. 2013;37(9):1731–1735. doi: 10.1007/s00264-013-2077-0. [eng] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Castellini J.L.A., Grande Ratti M.F., Gonzalez D.L. Clinical and radiographic outcomes of percutaneous third-generation double first metatarsal osteotomy combined with closing-wedge proximal phalangeal osteotomy for moderate and severe hallux valgus. Foot Ankle Int. 2022;43(11):1438–1449. doi: 10.1177/10711007221118568. [eng] [DOI] [PubMed] [Google Scholar]
- 53.de Carvalho K.A.M., Baptista A.D., de Cesar Netto C., Johnson A.H., Dalmau-Pastor M. Minimally invasive chevron-akin for correction of moderate and severe hallux valgus deformities: clinical and radiologic outcomes with a minimum 2-year follow-up. Foot Ankle Int. 2022;43(10):1317–1330. doi: 10.1177/10711007221114123. [eng] [DOI] [PubMed] [Google Scholar]
- 54.Lewis T.L., Ray R., Gordon D.J. Minimally invasive surgery for severe hallux valgus in 106 feet. Foot Ankle Surg. 2022;28(4):503–509. doi: 10.1016/j.fas.2022.01.010. [eng] [DOI] [PubMed] [Google Scholar]
- 55.Lewis T.L., Ray R., Robinson P., Dearden P.M.C., Goff T.J., Watt C., et al. Percutaneous chevron and Akin (PECA) osteotomies for severe hallux valgus deformity with mean 3-year follow-up. Foot Ankle Int. 2021;42(10):1231–1240. doi: 10.1177/10711007211008498. [eng] [DOI] [PubMed] [Google Scholar]
- 56.Iannò B., Familiari F., De Gori M., Galasso O., Ranuccio F., Gasparini G. Midterm results and complications after minimally invasive distal metatarsal osteotomy for treatment of hallux valgus. Foot Ankle Int. 2013;34(7):969–977. doi: 10.1177/1071100713481453. [eng] [DOI] [PubMed] [Google Scholar]
- 57.Redfern D., Vernois J., Legré B.P. Percutaneous surgery of the forefoot. Clin Podiatr Med Surg. 2015;32(3):291–332. doi: 10.1016/j.cpm.2015.03.007. [eng] [DOI] [PubMed] [Google Scholar]
- 58.Zhang H., Wang X., Yang Y.F., Tao X., Guo Q.W., Xu H.L., et al. [Expert consensus of the third-generation minimally invasive technical specification for hallux valgus] Zhong Guo Gu Shang. 2022;35(9):812–817. doi: 10.12200/j.issn.1003-0034.2022.09.003. [DOI] [PubMed] [Google Scholar]