ABSTRACT
Here we report the case of a 71-year-old woman who complained of lower back and left leg pain due to rod fracture following instrumented fusion using the lateral lumbar interbody fusion and multi-rod technique to treat adult spinal deformity. Radiographic images revealed bilateral rod fractures at L4-5 and pseudoarthrosis at L2-5; lower lumbar lordosis was minimal, but upper lumbar hyperlordosis was noted. The patient underwent revision surgery, which included posterior spinal instrument replacement, L3-4 and L4-5 lateral lumbar interbody fusion cage removal, and L4 vertebral body replacement via the anterior approach. This is a rare case of reoperation with the multi-rod technique. Revision surgery should be performed in consideration of the proportion of lumbar lordosis and anterior bony fusion as the posterior component is resected and bony fusion can only be achieved anteriorly.
Key Words: adult spinal deformity, rod fracture, multi-rod technique, pseudarthrosis, revision surgery
INTRODUCTION
Adult spinal deformity (ASD) is a form of spinal deformity that increases with age and causes pain and functional disability.1 As poor sagittal alignment is associated with symptoms such as lower back and leg pain, surgical treatment is used to achieve proper alignment. Anterior fixation using lateral lumbar interbody fixation (LLIF) or other methods, followed by posterior fixation to correct global alignment, is commonly used; however, several postoperative complications, such as pseudoarthrosis have been reported.2 Thus, the use of a multi-rod technique for stronger initial fixation to prevent rod fractures has been reported.3-5 However, there have been few reports on reoperation following rod fracture using the multi-rod technique, and it is unclear how the spine should be reconstructed for anterior bony fusion when the rod count is already multiple and sufficient.
Herein, we report a case of ASD reoperation due to pseudarthrosis and rod fracture after LLIF and posterior fusion using the multi-rod technique. This case report was approved by the Institutional Review Board (Approval No. 2016-0177) of our center, and was conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinski.
CASE REPORT
A 71-year-old female patient was admitted to our institution due to reported back pain and bilateral leg pain that had gradually worsened over the prior two years. The patient’s past medical history included diabetes and hypertension. On examination, the manual muscle testing of the left tibialis anterior muscle and gastrocnemius muscle was graded as 3/5. The straight leg raise test was positive on the left side, femoral nerve stretch testing was negative on both sides, and bilateral patellar and Achilles tendon reflexes were normal. No urinary or bowel issues were reported.
Radiographs showed that the global alignment error with the pelvic incidence (PI) was 53°, lumbar lordosis (LL) was 16°, lower lumbar lordosis (LLL) was 5°, C7-SVA was 125 mm, and the degenerative scoliosis with the degree of lumber scoliosis was 33° (Fig. 1A, B). CT myelography and MRI revealed severe endplate degeneration, spondylolisthesis, and spinal canal stenosis of the L3/4 and L4/5 (Fig. 1C, D). The patient underwent LLIF followed by posterior fusion from T12 to the iliac, total laminectomy from the L2 to the sacrum, and grade 2 osteotomy from the L2/3 to L5/sacrum. Pure titanium rods (6 mm) were used, while additional rods were used to increase the posterior fixation strength. Rib bone and β-TCP were used as grafted bones in the LLIF cages (Fig. 2).
Fig. 1.
Preoperative radiographs, CT myelography, and MRI
Fig. 1A, 1B: Standing posteroanterior (A) and lateral (B) radiographs.
Fig. 1C: Sagittal view of CT myelography.
Fig. 1D: Sagittal view of T2-weighted MRI.
PI: pelvic incidence
PT: pelvic tilt
SS: sacral slope
TK: thoracic kyphosis
LL: lumbar lordosis
LLL: lower lumbar lordosis
SVA: sagittal vertical axis
Fig. 2.
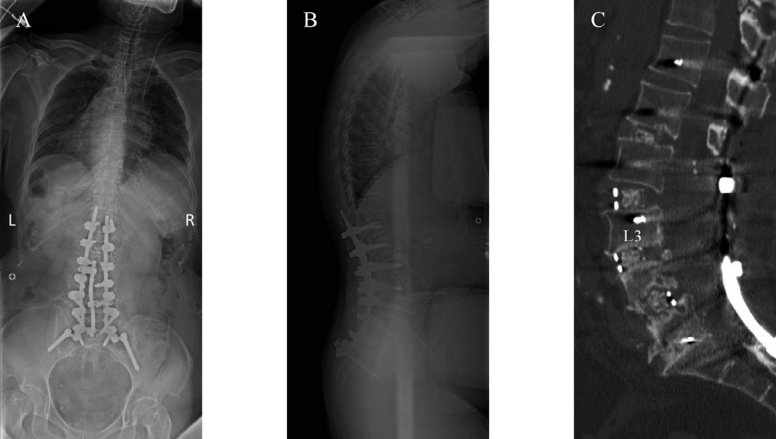
Postoperative radiographs and CT
Fig. 2A, 2B: Intraoperative prone posteroanterior (A) and lateral (B) radiograph.
Fig. 2C: Sagittal view of CT.
One month later, a T12 compression fracture occurred, resulting in a proximal junctional fracture (Fig. 3A, B). Therefore, the posterior fixation was extended to the T4, and T12 vertebral body replacement was performed using the left anterior approach. The local and rib bones were used for grafting. The PI was 49°, LL was 42°, and LLL was 9° (Fig. 3 C, D).
Fig. 3.
Radiographs after proximal junctional fracture and revision surgery
Fig. 3A, 3B: Standing posteroanterior (A) and lateral (B) radiograph, black arrow showed proximal junctional fracture.
Fig. 3C, 3D: Standing posteroanterior (C) and lateral (D) radiograph.
PI: pelvic incidence
PT: pelvic tilt
SS: sacral slope
TK: thoracic kyphosis
LL: lumbar lordosis
LLL: lower lumbar lordosis
SVA: sagittal vertical axis
Two years later, the patient was admitted to our institution with severe back and left leg pain, accompanied by an inability to ambulate. Radiographs revealed bilateral rod fractures at the L4/5 level where rod reinforcement was in place, and clear zones were observed at L2/3 and 4/5 around the LLIF cage (Fig. 4A, B). Computed tomography revealed pseudoarthrosis at the L2/3, 3/4, and 4/5 vertebrae, and endplate injury at the inferior L4 and superior L5 vertebral bodies (Fig. 4C, D). Magnetic resonance imaging showed fluid accumulation and mild spinal canal stenosis between the L4/5 vertebrae (Fig. 4E).
Fig. 4.
X-ray, CT, and MRI two years after initial surgery
Fig. 4A: Posteroanterior radiograph showing bilateral rod fracture at the L4/5 level.
Fig. 4B: Lateral radiograph showing L2/3, 4/5 clear zone around cages.
Fig. 4C, 4D: Sagittal (C) and coronal (D) computed tomography images showing pseudoarthrosis and endplate injury.
Fig. 4E: Sagittal T2-weighted magnetic resonance imaging showed fluid accumulation (black arrow).
A two-stage surgery was planned to rectify the rod fracture caused by pseudoarthrosis. Posterior fixation was performed during the first revision surgery. An incision was made caudally through the connector, and the rods and screws were removed. Metallosis was observed, especially around the connector, suggesting implant loosening (Fig. 5). The L1/2 and L4/5 facets were refreshed bilaterally, and the bone was grafted from the iliac crest because of pseudarthrosis. The screws were replaced with thicker and longer screws, and the pure titanium rods (6 mm) were replaced with cobalt-chrome rods (6 mm) to strengthen the fixation force for re-fixing. Intraoperative bleeding was 447 mL over a total operation time of 4 h and 38 min. No complications were noted.
Fig. 5.

Intraoperative photograph
Fig. 5A: Photograph after implant exposure, white arrows indicate rod fracture site.
Fig. 5B: Photograph after rod removal shows significant metallosis.
One week later, a second revision surgery was performed. L2/3 intervertebral fusion and L4 vertebral body replacement were performed using the left approach on the opposite side of the first surgery. LLIF cage removal was difficult because of fibrous fusion, and removing the implant while carefully breaking the area around the implant with a chisel took time. L4 vertebral body replacement was performed, and the ribs and local bones were used for bone grafting. Intraoperative bleeding was measured at 1105 mL over a total of 4 h and 40 min. Peritoneal injury was observed during surgery. On follow-up assessment after one year, the patient noted that the lower back pain recurred occasionally, but the patient was able to walk already with an aid of a walker. Radiographs showed that the lumbar region was well aligned with no implant failure; however, proximal junctional kyphosis had occurred. Computed tomography revealed a bony union from the L2 to L5 (Fig. 6).
Fig. 6.

X-ray and CT at final follow-up
Fig. 6A, 6B: Whole-spine standing posteroanterior (A) and lateral (B) radiograph show maintaining global alignment.
Fig. 6C, 6D: Sagittal (C) and coronal (D) computed tomography show bone union.
PI: pelvic incidence
PT: pelvic tilt
SS: sacral slope
TK: thoracic kyphosis
LL: lumbar lordosis
SVA: sagittal vertical axis
DISCUSSION
ASD is a three-dimensional degenerative change that occurs predominantly in the lumbar spine and thoracolumbar transition region. This disease is common in Japan, which has a hyper-aged society, and Schwab et al reported a 68% incidence of ASD in the elderly over 60 years of age.1
LLIF has become a standard of minimally invasive surgery for degenerative lumbar spinal diseases due to minimally invasive access to the spine, less blood loss compared to open procedures, and less postoperative pain.6 However, in Japan the complication rate is 18%, and the re-operation rate in 2.2%.7 Further, Pojskic et al reported an 11% incidence of pseudoarthrosis.2 In recent years, there have been many reports on the use of the multi-rod technique to strengthen the posterior fixation to prevent rod fracture. Rod fracture in ASD has been reported to occur in 6.8–14.9% of patients, whereas the rod fracture rate decreased to 0–3% using the multi-rod technique, thereby indicating the feasibility of this specific technique.3-5 Pseudarthrosis is also the cause of rod fracture when using the multi-rod technique3; however, few papers have reported on the etiological factors that lead to pseudoarthrosis and on the optimal way to reoperate.
In the present case, there are two factors that contributed to the development of pseudoarthrosis and subsequent rod fracture, including a lack of cage contact area due to improper sagittal alignment and bone grafting material. Specifically, LLL after primary surgery is smaller than ideal, although total LL is appropriate. Recently, there have been several reports on the ratio of LLL to LL. Barrey et al reported that the lordosis angle from L4 to S1 accounts for 2/3 of the LL.8 Yilgor et al proposed the Global Alignment and Population (GAP) score, which suggests that LLL is appropriate for 50–80% of LL.9 In the present case, radiography after the primary surgery revealed that an LL of 42° was sufficient for a PI of 49°, but LLL was insufficient at 9°, and the upper intervertebral disc was used to acquire lordosis. Thus, the upper LL and segmental lordosis were larger, which may be related to the minimal contact area between the cage and the vertebral endplate resulting in pseudoarthrosis. Secondly, increasing or modifying the graft bone could have prevented pseudarthrosis, even though the bone graft matrix was lost due to the posterior element resected for lumbar spinal canal stenosis and osteotomies of multiple facet joints to form lumbar lordosis. In recent years, bone grafting materials such as demineralized bone matrix have become available, and have shown good results,10 and the use of such materials may be effective for bone union.
In conclusion, rod fracture can occur if bone union is not achieved even with implant augmentation and surgical planning, considering where bony union will be achieved is necessary.
ACKNOWLEDGEMENT
We would like to thank Editage (www.editage.com) for English language editing.
CONFLICTS OF INTEREST STATEMENT
The authors declare that there are no conflicts of interest in this study and no specific funding was achieved to support this work.
Abbreviations
- ASD
adult spinal deformity
- LL
lumbar lordosis
- LLIF
lateral lumbar interbody fusion
- LLL
lower lumbar lordosis
REFERENCES
- 1.Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 2005;30(9):1082–1085. doi: 10.1097/01.brs.0000160842.43482.cd. [DOI] [PubMed]
- 2.Pojskic M, Saß B, Völlger B, Nimsky C, Carl B. Extreme lateral interbody fusion (XLIF) in a consecutive series of 72 patients. Bosn J Basic Med Sci. 2021;21(5):587–597. doi: 10.17305/bjbms.2020.5261. [DOI] [PMC free article] [PubMed]
- 3.Hyun SJ, Lenke LG, Kim YC, Koester LA, Blanke KM. Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976). 2014;39(22):1899–1904. doi: 10.1097/BRS.0000000000000556. [DOI] [PubMed]
- 4.Merrill RK, Kim JS, Leven DM, Kim JH, Cho SK. Multi-Rod Constructs Can Prevent Rod Breakage and Pseudarthrosis at the Lumbosacral Junction in Adult Spinal Deformity. Global Spine J. 2017;7(6):514–520. doi: 10.1177/2192568217699392. [DOI] [PMC free article] [PubMed]
- 5.Gupta S, Eksi MS, Ames CP, et al. A novel 4-rod technique offers potential to reduce rod breakage and pseudarthrosis in pedicle subtraction osteotomies for adult spinal deformity correction. Oper Neurosurg (Hagerstown). 2018;14(4):449–456. doi: 10.1093/ons/opx151. [DOI] [PMC free article] [PubMed]
- 6.Ohba T, Ebata S, Haro H. Comparison of serum markers for muscle damage, surgical blood loss, postoperative recovery, and surgical site pain after extreme lateral interbody fusion with percutaneous pedicle screws or traditional open posterior lumbar interbody fusion. BMC Musculoskelet Disord. 2017;18(1):415. doi: 10.1186/s12891-017-1775-y. [DOI] [PMC free article] [PubMed]
- 7.Fujibayashi S, Kawakami N, Asazuma T, et al. Complications Associated With Lateral Interbody Fusion: Nationwide Survey of 2998 Cases During the First 2 Years of Its Use in Japan. Spine (Phila Pa 1976). 2017;42(19):1478–1484. doi: 10.1097/BRS.0000000000002139. [DOI] [PubMed]
- 8.Barrey C, Darnis A. Current strategies for the restoration of adequate lordosis during lumbar fusion. World J Orthop. 2015;6(1):117–126. doi: 10.5312/wjo.v6.i1.117. [DOI] [PMC free article] [PubMed]
- 9.Yilgor C, Sogunmez N, Boissiere L, et al. Global Alignment and Proportion (GAP) Score : Development and Validation of a New Method of Analyzing Spinopelvic Alignment to Predict Mechanical Complications After Adult Spinal Deformity Surgery. J Bone Joint Surg Am. 2017;99(19):1661–1672. doi: 10.2106/JBJS.16.01594. [DOI] [PubMed]
- 10.Ricart PH, Gandhi SD, Geisinger J, Baker K, Park DK. Clinical and CT Analysis of Lumbar Spine Arthrodesis: β-Tricalcium Phosphate Versus Demineralized Bone Matrix. J Am Acad Orthop Surg Glob Res Rev. 2018;2(9):e024. doi: 10.5435/JAAOSGlobal-D-18-00024. [DOI] [PMC free article] [PubMed]





