Abstract
About 65.5 % of the Indians live in rural areas while availability of healthcare is biased towards urban setups. Medicine in undergraduates is taught in ivory towers of medical colleges, a paradigm shift in teaching bedside medicine from these ivory towers to community level is required. Hence a new competency-based medical education for undergraduate course was adopted with family adoption program as a vital component, which provides an opportunity for undergraduates to get sensitised to problems and social dynamics at grass root level. We propose an integrated holistic health team model to implement family adoption program so as to address needs of community and build consensus amongst graduate students from various health disciplines to work in integrated team approach and result in enhanced learning. A five pronged strategy is implemented by forming an integrated team comprising of students from medical, aental, ayurveda, and physiotherapy & nursing streams. The institutions that have undergraduate program for any two to five of these disciplines can adopt proposed approach. Expected outcomes of utilising this model is to create holistic health team thereby inculcating in budding graduates team spirit, mutual cooperation & respect for other disciplines of health sciences and thereby holistic healthcare to community.
Keywords: Family adoption program, National medical commission, Integrated health care
About 65.5 % of the Indian population live in rural areas while availability of healthcare facilities are biased towards urban areas and has been a major concern for public health in India. Issues spanning from access, affordability and health illiteracy, are some of the major determinants which acts as barriers in timely management of health issues and serves as limitations in health related awareness and quality healthcare which leads to a scenario called as ‘Scarcity in abundance’. To make healthcare facilities more approachable to the needy population there is a need to take necessary measures such as imparting community oriented training to the medical undergraduates [1] (see Fig. 1).
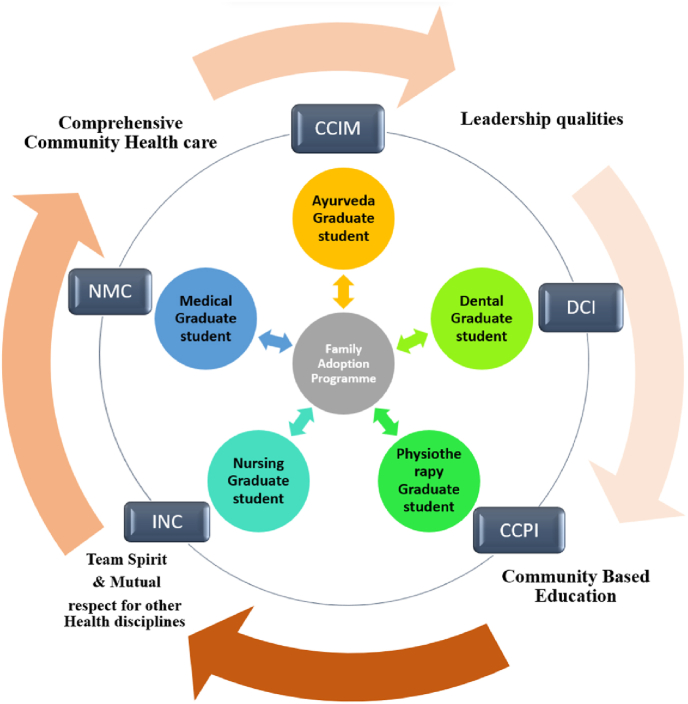
Fig. 1.
Implementation of Family adoption Program with a Holistic and Integrated Model. NMC-National Medical Commission,CCIM-Central council of Indian Medicine, DCI-Dental council of India, CCPI-Central council of Physiotherapy, India, INC-Indian Nursing Council. (Self-made).
Most of the medicine in undergraduate medical course is taught in ivory towers of medical colleges and tertiary hospitals and a paradigm shift in teaching bedside/clinical medicine from these ivory towers to community and district hospitals must be considered. Healthcare is teamwork, and several groups of workers operate in cohesion for effective delivery of healthcare hence exposure to community settings is important to budding health sciences graduates [2].
One of the goals of the undergraduate medical education is to make services of medical professionals accessible to all citizens across geographical boundaries. To achieve this every medical college allots about five households in a village to all the first MBBS students under ‘Family Adoption Programme’ during their entire undergraduate program so as to groom medical students as ‘complete doctors' with qualities such as confidence, empathy and leadership in socio health fronts [3].
Taking cognisance of this, the undergraduate Medical Education Board of National Medical Commission implemented a new competency-based medical education for undergraduate course curriculum with the main objective of covering the three domains of learning - Cognitive, Affective & Psychomotor learning. The aim of the program is to provide medical graduates early community exposure and learning opportunities for community based health systems so that they are groomed as socially relevant physicians.
Family adoption program is recommended under this curriculum starting from the first professional year of medical course. This program shall include villages which are not covered under the Rural Health training centre of each medical college. Apart from this, every college may organise a health screening & referral medical camp in the villages with help of community participation where in identification of local health problems and basic curative, preventive, promotive and needful referral services will be provided by the medical college hospital and if possible, treatment provided should be offered under government schemes, subsidized rates or waived off. Along with that, environment friendly activities like tree plantation/medicinal plant plantation are also to be promoted and conducted by National service scheme (NSS) units [1].
Guidelines under graduate medical education regulation 2023 superseded all the previous guidelines and it intends to take the learner to provide health care to the evolving needs of the nation and the world. Family adoption program as an important component of this recent guidelines which focuses on an integrated approach towards other clinical disciplines, public health services, NGOs, environmental sciences, social sciences, management, hospital administration, research, etc. to impart training to enable the graduate to work at all levels of health care. It states that the teaching should be aligned and integrated horizontally and vertically in order to allow the learner to understand the impact of environment, society and national health priorities as they relate to the promotion of health and prevention and cure of disease [4].
Several studies envisaged the advantages of learning in ‘the community as a classroom’ as achieving communication skills; understanding the customs and cultural beliefs of the rural population, learning to be humane and develop empathy; inculcate leadership skill; working as primary consultants for the households; and learning basic skills of diagnosing and managing health problems [3,5,6].
Stakeholders in “Family Adoption Program” are undergraduate students, faculty& staff from departments of Community medicine, village head/gram sabha members and families of adopted households. It shall provide an opportunity for all stakeholders to get sensitised to the problems and understand social dynamics existing at community level thereby providing a platform to understand the social determinants of health at grass root level.
The successful implementation of the programme depends on a work plan with team efforts from all the stakeholders from the institutional level to execution level in the form of human resources, availability of logistics, transport facilities and involvement of the department of community medicine in training of the medical graduates [3].
Experience from Australia and Canada has also showed that through Longitudinal Integrated Clerkships (LICs) a year-long community-based placements help medical students hone the soft skills in the domain of communication, clinical reasoning and health managerial skills which they described as ‘Meaningful personal learning experiences [7].
Considering the various constraints in implementing the Community based Education (CBE) Program a Generic guideline would not be sufficient to ensure impact as expected hence a detailed recommendation on systematic CBE learning characteristics for different levels of undergraduate medical curriculum (macro, meso, and micro levels) has been proposed by Claramita M et al. named as the ‘CBE-tree’ framework. They opined that the lessons learned may be significantly more beneficial for the students, faculty members, and participating community [8].
Ayurveda is a traditional Indian system of medicine dating back to the late 1000- 500 B.C. In Ayurveda, the approach to training was integrated and holistic. So, the concept of the approach can be referred back to the late Vedic period.
In 1977, in India, in collaboration with World health organisation Southeast Asian Region (WHO SEARO), a significant initiative, Reorientation of Medical Education (ROME), was undertaken. Every medical college was responsible for comprehensive health care in three primary health centres and gradually extended its coverage to the entire district. For this purpose, each medical college was to establish a well-knit rural referral system. To achieve the purpose of community-based training, outreach activities such as community postings of medical students, mobile clinics and involvement of the entire faculty of the medical college was done.
The challenges faced during the implementation of this ROME Scheme such as lack of logistics, the unenthusiastic medical faculty in participation in community-based training, and the lack of intensive effort and institutional mechanisms for its implementation were equated to its partial success. Even though it has been relaunched as a family adoption program the same challenges still persist and need to be addressed [9].
Since 1977 till now, almost all medical colleges ceased its implementation except the Mahatma Gandhi Institute of Medical Sciences, Sewagram, which continued to implement the ROME scheme for medical undergraduates with appropriate alterations and a set of recommendations based on the “Edinburgh Declaration” of World Federation for Medical Education (WFME) [10].
Integrated Holistic Health Team approach is an integrated system of care intended to fulfil the health needs of the individuals, families in their local settings through an interdisciplinary program which simultaneously provides an educational platform for students [11].
We propose an integrated holistic health team model to implement the family adoption program so as to address needs of the community & build a consensus amongst graduate students from various health disciplines to work in a team approach leading to enhanced learning from community based education and integrated & holistic health care for community.
This model proposes a five pronged strategy by forming an “Integrated Holistic health team” comprising undergraduate students from medical, dental, ayurveda, physiotherapy and nursing Colleges. While Universities having two to five of the above mentioned disciplines or if other discipline colleges are present in same town/city can make their teams accordingly as we believe team approach is better than individual approach.
.
The department of community medicine from medical colleges, department of public health dentistry from dental colleges, department of swasthavritta from Ayurveda colleges, department of community physiotherapy from physiotherapy colleges and department of Community Health Nursing from Nursing college can be designated as apex departments to conduct the family adoption program.
There shall be one undergraduate student from each stream to make a team of 5 students, number of teams will depend on the total intake capacity of the institute and the ratio of students from any discipline can be increased depending on the number of students in that discipline over and above one student from each stream in one team.
Apart from National Medical Commission which is statutory body regulating medical education in India, The National Commission for Indian System of Medicine, Dental Council of India, Central Council of Physiotherapy and Indian Nursing council regulate the education curriculum for Ayurveda, Dental Physiotherapy and Nursing education in country. On lines with the National medical commission the other councils need to take up the early clinical exposure in form of family adoption program and inculcate in revised curriculum so as to ensure that all the streams can participate in the envisaged model in uniformity. The discussion among all stakeholders can be initiated on this regards. There is need of political commitment and beurocratic and technocratic decisions required in this regards. As of now the colleges can start the program on pilot mode on free days in morning hours without disturbing the existing curriculum.
Perceived benefits of integrated holistic team model to students
-
1.
Family adoption program gives them early community exposure to hone their skills in rapport building, communication skills and Introduce and orient them to community whom they are expected to serve after graduation.
-
2.
Insights regarding socio-cultural and economic determinants of health & disease in rural communities.
-
3.
Develop a team spirit by collaborating and coordinating with graduates from other disciplines.
-
4.
Understand pros & cons of each discipline of health sciences and develop mutual respect.
-
5.
Imbibe leadership qualities in them by helping solve issues of the villagers by acting as a bridge between community & tertiary care hospitals.
Benefits of integrated holistic team model to community
-
1.
Availability of health sciences graduates for guidance regarding any health issues and conduction of health camps for curative needs
-
2.
Hand holding by team members when they visit hospitals for curative treatment
-
3.
Health awareness and preventive strategies sensitisation by information, education and communication and behavioural change communication strategies through skit/role plays done by students.
-
4.
Query solving & removing myths regarding health & diseases.
-
5.
Improved communication with health sciences students will remove their mistrust & misunderstanding for any issues regarding health care sector.
Planning & method of implementation of family adoption program essentially remains the same while adopting the integrated holistic health team strategy and model instead of medical graduates going alone the “TEAM” goes to the villages.
The students should visit the village as per their academic schedule. Half of such teams shall visit the adopted village on a scheduled day while students from remaining half teams shall stay back for classroom teaching. It can be planned and linked in a manner that students are oriented and sensitized about learning objectives for the next family visit during the preceding classroom teaching.
Feedback from all stakeholders: families from adopted communities, students and staff from health sciences university to be conducted at the end of each academic year to get insights on perceived usefulness of this model and improvements if any required as per inputs of evaluation.
We expect to improve the doctor-patient communication and thereby decrease the conflicts that have increased due to lack of rapport and miscommunication between Health care sector and Community as this shall make students socially aware & relevant to the settings they intend to serve in near future.
Perceived challenges & proposed measures for way ahead
The National Medical Commissions document on family adoption program explains the basics and rational of the program along with its aim, objectives and implementation plan and phase wise competencies to acquire along Teaching learning method to utilise and proposed outcomes.
The document fails to address some ground level implementation difficulties in form of faculty acceptance and motivation levels, logistics requirements, and stakeholder's perception for successful implementation of the program and lacks mention on how the horizontal or vertical integration can be done to make the program more holistic [12].
As with any new initiative, family adoption program could face multiple challenges like availability of transport facilities, faculty shortage and motivation levels among all stakeholders. Challenges in implementation may include the acceptance of proposed health team by adopted family members, security of the team and relevance of health team in interventions required during crises. Other challenge in implementation is in regards to family members of adopted families expecting curative treatment in form of medicines/prescription from students of team which they are not eligible to prescribe.
Appropriate permissions from gram panchayat, discussion of their concerns in gram sabha, making provisions of stand by ambulance if required in case of crises and provision of mini health camps for basic curative care for community members are some of the interventions proposed to address the above challenges.
Yalamanchili VK et al. has raised concerns about families' cooperation and adjustment to the academic schedule. The most significant motivating factor was interactive sessions by spending time with village people in the field. This program may improve the limited patient satisfaction regarding rural health services provided by tertiary care medical colleges [13].
We propose this integrated model of implementing the family adoption program wherever possible & feasible so as to enhance the learning experience of budding health sciences graduates and thereby benefiting the adopted communities in a holistic manner.
Sources of funding
None.
Author contributions
AM conceptualised the idea, JR was responsible for the writing initial draft for manuscript and AM edited the manuscript and both authors (AM, JR) read and approved the final manuscript.
Declaration of competing interest
None
Acknowledgements
The authors are grateful to Public health departments of all constituent units of University for the contribution in implementing the strategy.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.National Medical Commission. U.11026/1/2022 UGMEB dated 31st March 2022. Implementation of new competency based medical education for undergraduate course curriculum. Retrieved from https://www.nmc.org.in/MCIRest/open/getDocument?path=/Documents/Public/Portal/LatestNews/Implementation.pdf accessed on 10th March 2023.
- 2.Suhas Satish, Gangadhar B.N., Vanikar Aruna V., Malik Yogender, Girish N., Kumar Vijayendra, et al. Undergraduate medicine curriculum in India: untying the gordian knot. Ind J Prev & Soc Med. 2022;53(2) [Google Scholar]
- 3.Vanikar A.V., Kumar Vijayendra. The family adoption programme: taking Indian medical undergraduate education to villages. Ind J Prev & Soc Med. 2021;52(3) [Google Scholar]
- 4.NMC . National Medical Commission (Undergraduate Medical Education Board); 2023. Guidelines under graduate medical education regulation 2023. [Google Scholar]
- 5.Diab P., Flack P. Benefits of community-based education to the community in South African health science facilities. Afr J Prim Health Care Fam Med. 2013;5(1):474. [Google Scholar]
- 6.Amalba A., van Mook W.N.K.A., Mogre V., Scherpbier A.J.J.A. The perceived usefulness of community based education and service (COBES) regarding students’ rural workplace choices. BMC Med Educ. 2016;16(1):130. doi: 10.1186/s12909-016-0650-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelly L., Walters L., Rosenthal D. Community-based medical education: is success a result of meaningful personal learning experiences? Educ Health. 2014;27(1):47–50. doi: 10.4103/1357-6283.134311. [DOI] [PubMed] [Google Scholar]
- 8.Claramita M., Setiawati E.P., Kristina T.N., Emilia O., van der Vleuten C. Community-based educational design for undergraduate medical education: a grounded theory study. BMC Med Educ. 2019;19(1) doi: 10.1186/s12909-019-1643-6. 1-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma S., Sharma G. Medical education in India. Ann Natl Acad Med Sci (India) 2017;53(4):179–193. [Google Scholar]
- 10.Dongre A.R., Deshmukh P.R., Gupta S.S., Garg B.S. An evaluation of ROME Camp: forgotten innovation in medical education. Educ Health. 2010;23(1):363. [PubMed] [Google Scholar]
- 11.Leal Filho W., Marisa Azul A., Brandli L., GökçinÖzuyar P., Wall T., editors. Sustainable cities and communities. Springer International Publishing; Cham: 2020. Zero hunger. 981–981. [DOI] [Google Scholar]
- 12.National Medical Commission . National Medical commission(Undergraduate Medical Education Board); 2022. Implementation of new Competency-based Medical Education for undergraduate course curriculum. [Google Scholar]
- 13.Yalamanchili Vijay K., Uthakalla Vijaya K., Naidana Sarathy P., Kalapala Abhilash, Venkata Prasanna K., Yendapu Rajasekhar. Family adoption programme for medical undergraduates in India – the way ahead: a qualitative exploration of stakeholders’ perceptions. Indian J Community Med. 2023;48(1):142–146. doi: 10.4103/ijcm.ijcm_831_22. [DOI] [PMC free article] [PubMed] [Google Scholar]