Abstract
Background
Chronic total occlusion rotational atherectomy (CTO RA) is an emerging intervention in coronary artery disease (CAD), although data comparing its outcomes and complications with non-CTO RA are scarce. We sought to evaluate the outcomes of RA in CTO lesions compared to those in non-CTO lesions by performing a meta-analysis.
Methods
We conducted a systematic review and meta-analysis of studies comparing the clinical outcomes and complications between CTO RA and non-CTO RA in patients with CAD. We searched PUBMED, CINAHL, EMBASE and Cochrane Central Register of Clinical Trials for any studies that compared the outcomes of RA in CTO and non-CTO lesions. The outcomes analyzed included in-hospital major adverse cardiovascular events (MACE), target vessel revascularization (TVR), angiographic success, procedural success, periprocedural complications, coronary perforation, and all-cause mortality.
Results
Four studies with a total of 1868 patients were included, spanning from 2018 to 2022, from Germany, Taiwan, and Korea. The median age of included patients was 71. The rate of the pooled results indicated a moderate, non-significant increase in in-hospital MACE and TVR for CTO RA compared to non-CTO RA. There was a small, non-significant decrease in angiographic and procedural success in CTO RA compared to non-CTO RA. CTO RA was associated with a non-significant increase in periprocedural complications and a significant increase in coronary perforation compared to non-CTO RA. All-cause mortality showed a non-significant increase in the CTO RA group.
Conclusion
This meta-analysis provides evidence that while CTO RA may be associated with a higher risk of coronary perforation, the risk of other outcomes including MACE, TVR, and all-cause mortality is not significantly different compared to non-CTO RA. More research is needed to further understand these relationships and to optimize treatment strategies in patients with CAD undergoing CTO RA.
Keywords: Rotational atherectomy, Chronic total occlusion, Non chronic total occlusion, Comparison of outcomes and complications, All-cause mortality
1. Introduction
Chronic total occlusion (CTO) is a common finding in patients with coronary artery disease (CAD), being present in approximately 18–52 % of individuals undergoing coronary angiography [[1], [2], [3]]. Intervention for CTO, which typically involves the use of percutaneous coronary intervention (PCI), can be technically challenging and is associated with higher rates of procedural complications compared to non-CTO coronary interventions [[4], [5], [6]].
Rotational atherectomy (RA) has emerged as a useful tool for the treatment of complex and heavily calcified coronary lesions, including CTOs [7,8]. It utilizes a high-speed rotational burr to modify the plaque, facilitating stent delivery and expansion [9]. However, the evidence on the comparative safety and efficacy of RA in CTO versus non-CTO lesions remains scarce, primarily due to the lack of large-scale, prospective trials [10,11]. Existing studies have reported conflicting results, with some suggesting higher rates of complications like coronary perforation and lower rates of procedural success in CTO lesions [12,13], while others have found comparable outcomes between CTO and non-CTO interventions [14,15]. Given these divergent findings and the clinical implications of this topic, a comprehensive analysis of the available literature is warranted.
This study aims to perform a systematic review and meta-analysis to compare the safety and efficacy of RA in CTO versus non-CTO lesions in CAD patients. To our knowledge, this is the first meta-analysis to directly address this important clinical question, providing valuable insights for clinicians in the management of patients with complex CAD [16].
2. Methodology
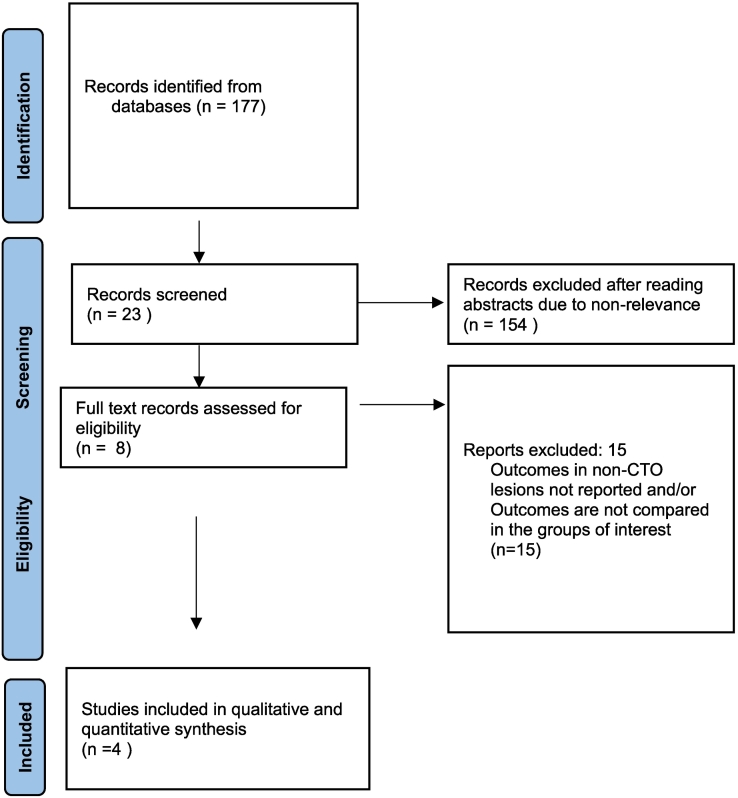
We followed PRISMA (Preferred Reporting Items for Systematic Reviews and Meta- Analyses) guidelines in reporting the results of the meta-analysis. Fig. 1 shows the PRISMA flow diagram of study selection. We conducted a search of electronic databases of PUBMED, CINAHL, EMBASE, Cochrane Central Register of Clinical Trials for English language references from inception through June 1, 2023, using the search terms “Chronic total occlusion” or “CTO coronary lesions” and “non chronic total occlusion lesions” or “non- CTO coronary lesions” and “rotational atherectomy” or Rotablation”. Three investigators (RRD, OQ and KP) independently conducted the database search and agreed on final article selection. Any disagreements were resolved by discussion between the three (RDD, OQ and KP). A manual search was performed for relevant references from the selected articles and published reviews. Any study that reported on the outcomes of rotational atherectomy in calcified CTO lesions compared to those in calcified non-CTO lesions were included if it involved ≥5 patients and reported on one of the outcomes of interest: all cause mortality, procedural complications, in-hospital major adverse cardiac events (MACE), target vessel revascularization (TVR), angiographic success, procedural success, periprocedural complications and coronary perforation.
Fig. 1.
shows the PRISMA flow diagram of study selection.
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: https://doi.org/10.1136/bmj.n71
Three investigators (RDD, SR and NG) independently extracted data from the selected studies in duplicate using standardized data-extraction form. Data was obtained on study characteristics that included study design, patient selection, inclusion and exclusion criteria, follow-up duration as applicable, number of patients, patients' demographic and baseline characteristics, and outcomes of interest reported in hospital and at follow up period as applicable.
We performed the statistical analysis (MSH) using random-effects REML model to compute overall effects. We also calculated the pooled risk ratio with 95 % confidence interval (CI) using the total number of events and patients as reported in the individual studies. Study heterogeneity was evaluated with I2 index and Cochrane's Q statistic. I2 estimates the proportion of the variance in study estimates that is due to heterogeneity (ref to be included) Significant heterogeneity was defined as I2 values >60 %. Meta-regression was not considered because the number of included studies were <10.
3. Outcome definition
All- cause mortality: death from any cause during the study period.
In-hospital MACE: Composite of all-cause death, periprocedural myocardial infarction, and target vessel revascularization.
Angiographic success: Rotational atherectomy followed by stent implantation with residual stenosis <30 % and TIMI 3 flow in the target vessel at the end of the procedure.
Procedure success: Angiographic success with the absence of in-hospital periprocedural complications (all cause death, periprocedural MI, recurrent angina requiring TVR with PCI or emergency CABG, and tamponade requiring pericardiocentesis or surgery).
Periprocedural complications: all cause death, periprocedural MI, recurrent angina requiring TVR with PCI or emergency CABG, and tamponade requiring pericardiocentesis or surgery.
Assessment of Publication bias: The funnel plot and Egger's test were used to evaluate publication bias. Funnel plot is a graphical representation of the size of the studies plotted against the effect size. It assumes that studies with high precision would lie on both sides of the average creating a funnel-shaped distribution. Deviation from this pattern indicates publication bias. For in-hospital MACE the funnel plot showed clear symmetry (Egger's test p = 0.9288). Similarly for other outcomes clear symmetry were found in funnel plot (for TVR Egger's test p = 0.8349, for Angiographic success Egger's test p = 1.00, for Procedural success Egger's test p = 0.922, for Periprocedural complications Egger's test p = 1.00, for Coronary Perforation Egger's test p = 0.3699, for all-cause mortality p = 0.8227). Assessment of publication bias did not show any clear evidence of bias for our outcomes of interest (supplementary file).
4. Results
Our meta-analysis included four retrospective studies with a combined sample size of 1868 patients [[17], [18], [19], [20]]. The studies were conducted in Germany (Elbasha K et al., 2022 and Brinkmann C et al., 2018), Taiwan (Tsai T-C et al., 2022), and Korea (Lee SN et al., 2021). Table 1 presents the baseline patient and study characteristics, summarizing the demographic and clinical features across the studies. The patients' mean age varied between 63.9 and 72.5 years, and the majority were male (75 %–86.7 %). All studies reported a high prevalence of diabetes mellitus (32 %–61.9 %) and hypertension (70.5 %–92.5 %). Dyslipidemia, when reported, ranged from 64.8 % to 68 %. The rates of smoking varied from 30 % to 50 % in studies that provided this information. The type and length of coronary artery disease (CAD) lesions, as well as the specific vessels involved, were different among the studies. The right coronary artery (RCA) was the most frequently involved in two studies.
Table 1.
Baseline patient and study characteristics.
| Study/Year/Country | Study type | N | Mean Age years | Male (%) |
DM (%) |
HTN (%) |
Dyslipid -emia (%) |
Smoking (%) |
PAD (%) |
Hx of CABG (%) |
Hx of MI (%) |
Hx of PCI | CKD (%) |
mean LVEF | STEMI (%) |
NSTEMI (%) |
UA (%) |
Stable CAD (%) |
Dialysis (%) |
Lesion length(mm), mean | Ostial lesion (%) |
Bifurcation lesion (%) |
type of vessel (%) |
Burr Size (mm) |
Elective RA (%) |
Bailout RA (%) |
Vessels involved (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Elbasha K et al., 2022 Germany | Single center Retrospective study | 812 | 72.5 | 80 | 40 | 92.5 | 64.8 | 30 | N/A | 20 | 21.3 | 48.8 | 8.8 | 49.6 | 2.5 | 6.3 | 7.5 | 73.8 | 2.5 | 41.6 | 13.8 | 25 | CAD one 10 CAD two 21.3 CAD three 68.8 |
1.38 | 38.7 | 61.3 | LM 0 LAD 28.7 LCx 8.8 RCA 62.5 |
| Brinkmann C et al., 2018 Germany | Single center Retrospective study | 392 | 69.5 | 86.7 | 32 | 78.7 | 68 | N/A | 17.3 | 32 | 24 | 69.3 | N/A | 55 | N/A | N/A | N/A | N/A | N/A | 45.2 | N/A | N/A | CAD one 22.7 CAD two 18.7 CAD three 58.7 |
1.49 | N/A | N/A | LM 0 LAD 12 LCx 18.7 RCA 69.3 |
| Tsai T-C et al., 2022 Taiwan | Single center Retrospective study | 81 | 71.6 | 75 | 45.5 | 70.5 | N/A | N/A | 4.5 | 2.3 | N/A | N/A | N/A | 43.5 | 13.6 | 15.9 | 38.6 | N/A | N/A | N/A | 38.6 | 18.2 | CAD one 34.1 CAD two 20.5 CAD three 34.1 |
N/A | N/A | N/A | LM 11.4 LAD 47.7 LCx 9.1 RCA 27.3 |
| Lee SN et al., 2021 Korea | Multicenter Retrospective study | 583 | 63.9 | 83.3 | 61.9 | 76.2 | 50 | 23.8 | N/A | 11.9 | 14.3 | 40.5 | 21.4 | 52 | 9.5 | 7.1 | 9.5 | N/A | N/A | N/A | N/A | N/A | CAD one N/A CAD two N/A CAD three 85.7 |
N/A | N/A | N/A | LM 11.9 LAD N/A LCx N/A RCA N/A |
Note: PAD: Peripheral arterial disease; CAD: Coronary artery disease; RCA: Right coronary artery; CABG: Coronary artery bypass grafting; LM: Left main artery; N/A: Not reported.
5. Outcomes
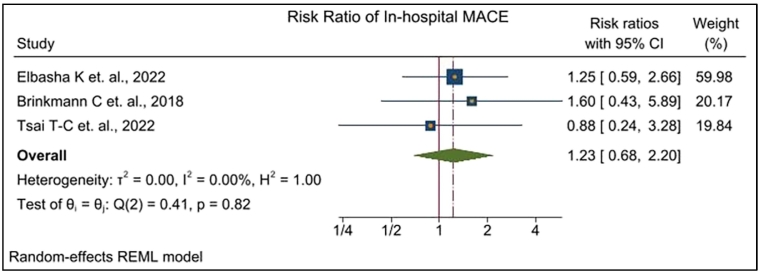
The meta-analysis included three studies: Elbasha K et al., 2022; Brinkmann C et al., 2018; and Tsai T-C et al., 2022. The overall analysis aimed to assess the risk of in-hospital MACE associated with CTO RA compared to Non-CTO RA.
The meta-analysis yielded a pooled risk ratio of 1.23 (95 % CI 0.683 to 2.201) for in-hospital MACE (Fig. 2). These results suggest that there is a moderate increase (23 %) in the risk of in-hospital MACE associated with CTO RA compared to non-CTO RA. However, the result was not statistically significant. There were no heterogeneity presents in the study (I2 statistic = 0.00 %, Cochran's Q statistic = 0.41, p = 0.82).
Fig. 2.
shows pooled risk ratios for In-hospital MACE.
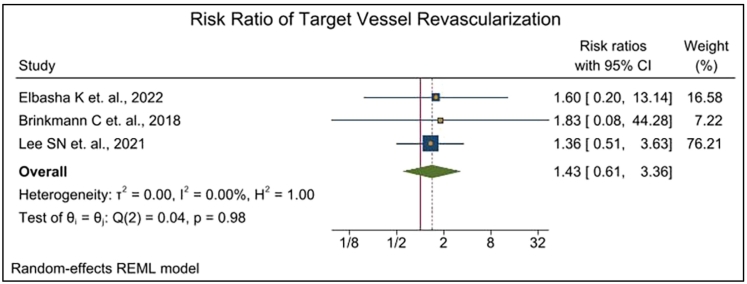
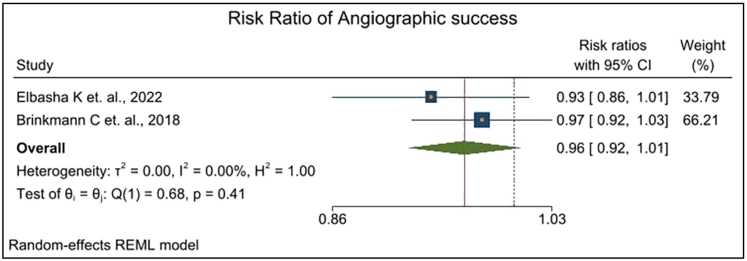
Fig. 3 represented the result of the meta-analysis for the outcome of target vessel revascularization (TVR). The overall analysis identified that the risk ratio of 1.43 (95 % CI: 0.61 to 3.36) for TVR. These suggest that CTO RA group were 43 % more in risk of TVR than non-CTO RA group. These findings were also not statistically significant. As a result, we could not conclude the significant difference between CTO RA and non-CTO RA in terms of TVR. Also, there were no heterogeneity presents among the studies (I2 statistic = 0.00 %, Cochran's Q statistic = 0.04, p = 0.98). The overall result of the meta-analysis for the outcome of angiographic success is presented in Fig. 4. The meta-analysis included two studies: Elbasha K et al., 2022, and Brinkmann C et al., 2018. The overall result suggests that CTO RA groups are 4 % (RR:96 %, CI 0.92 to 1.01) less chance of angiographic success than non-CTO RA. It shows the baseline significance so there may exist little difference between CTO RA and non-CTO RA. There was also no heterogeneity present among the studies (I2 statistic = 0.00 %, Cochran's Q statistic = 0.68, p = 0.41).
Fig. 3.
shows pooled risk ratios for target vessel revascularization.
Fig. 4.
shows pooled risk ratios for angiographic success.
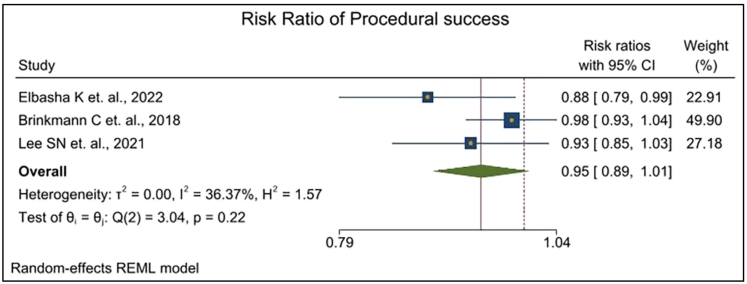
Also, in terms of procedural success (Fig. 5) it has been evident that CTO RA were 5 % (RR:0.95, 95 % CI: 0.89, 1.01) lower chance to have procedural success compared to that of the non-CTO RA group. Also, it shows the baseline significance so there may also exist little difference between CTO RA and non-CTO RA. The study found little heterogeneity in this case, but it was not that important (I2 statistic = 36.37 %, Cochran's Q statistic = 3.04, p = 0.22).
Fig. 5.
shows pooled risk ratios for procedural success.
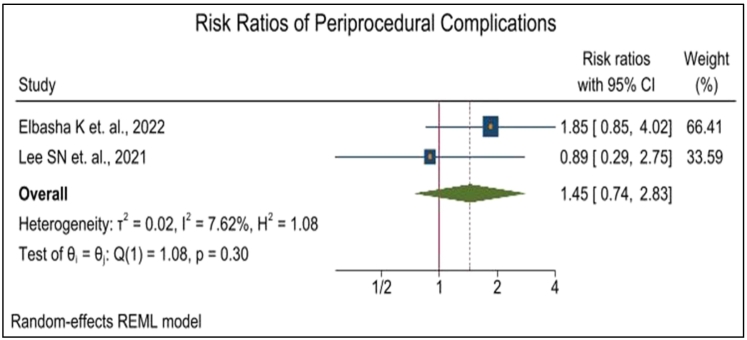
Furthermore, for periprocedural complications (Fig. 6) the overall risk ratio was 1.45 (95 % C·I: 0.74 to 2.83). These results suggest that the CTO RA groups were 45 % more at risk of periprocedural complications than non-CTO RA though the finding was not statistically significant. Also, there existed minimal heterogeneity in this outcome (I2 statistic = 7.62 %, Cochran's Q statistic = 1.08, p = 0.30).
Fig. 6.
shows pooled risk ratios for periprocedural Complications.
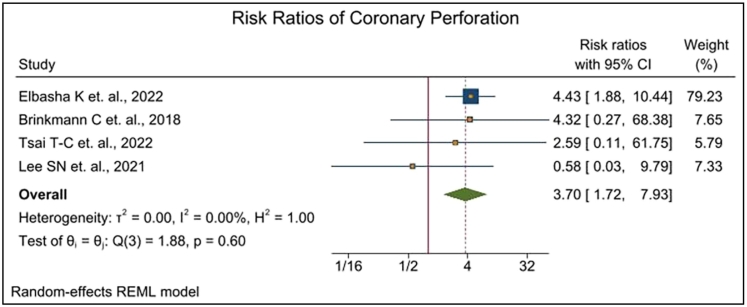
For coronary perforation (Fig. 7) the overall risk ratio was 3.70 (95 % C·I: 1.72 to 7.93). These results indicate that the CTO RA groups were 3.70 times more at risk of coronary perforation than non-CTO RA and the finding is statistically significant. So, we may conclude that there exists strong difference between CTO RA and non-CTO RA groups in terms of coronary perforation. There were also no heterogeneity presents among the study (I2 statistic = 0.00 %, Cochran's Q statistic = 1.88, p = 0.60).
Fig. 7.
shows pooled risk ratios for coronary Perforation.
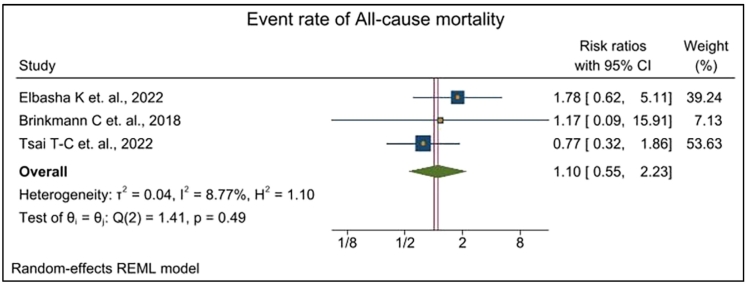
Finally in terms of all-cause mortality (Fig. 8) the overall risk ratio was 1.10 (95 % C·I: 0.55 to 2.23) which indicates that CTO RA groups were 10 % higher risk of mortality than non-CTO RA group though the finding was not statistically significant. Also, there existed minimal heterogeneity among studies (I2 statistic = 8.77 %, Cochran's Q statistic = 1.41, p = 0.49).
Fig. 8.
shows pooled risk ratios for All-cause mortality.
In assessing the pooled results of the four studies as evident from Table 2, several key points become apparent. First, while the in-hospital major adverse cardiovascular events (MACE), target vessel revascularization, and all-cause mortality showed a non-significant increase in the chronic total occlusion rotational atherectomy (CTO RA) groups compared to the non-CTO RA groups, it's important to note that this increase, while not statistically significant, may still suggest a trend of potential clinical relevance. The risk ratios for these outcomes were above 1, indicating a higher occurrence in the CTO RA groups, even though this did not reach statistical significance.
Table 2.
Summary of meta-analysis outcomes.
| Outcome | Pooled Risk Ratio (95 % Confidence Interval) | Significance | Heterogeneity (I2, Q statistic, p-value) |
|---|---|---|---|
| In-hospital MACE | 1.23 (0.683–2.201) | Not Significant | I2 = 0.00 %, Q = 0.41, p = 0.82 |
| Target vessel revascularization | 1.43 (0.61–3.36) | Not Significant | I2 = 0.00 %, Q = 0.04, p = 0.98 |
| Angiographic success | 0.96 (0.92–1.01) | Not Significant | I2 = 0.00 %, Q = 0.68, p = 0.41 |
| Procedural success | 0.95 (0.89–1.01) | Not Significant | I2 = 36.37 %, Q = 3.04, p = 0.22 |
| Periprocedural complications | 1.45 (0.74–2.83) | Not Significant | I2 = 7.62 %, Q = 1.08, p = 0.30 |
| Coronary Perforation | 3.70 (1.72–7.93) | Significant | I2 = 0.00 %, Q = 1.88, p = 0.60 |
| All-cause mortality | 1.10 (0.55–2.23) | Not Significant | I2 = 8.77 %, Q = 1.41, p = 0.49 |
Second, the angiographic and procedural success rates showed a minor decrease in the CTO RA groups. Although this decrease was also not statistically significant, it suggests that the CTO RA procedures might be slightly more challenging and may not achieve the same level of success as the non-CTO RA procedures.
Third, and most notably, there was a significantly higher risk of coronary perforation in the CTO RA groups with a risk ratio of 3.70, well above 1, and a 95 % confidence interval that did not cross 1 (1.72 to 7.93). This indicates a clear statistical significance. This finding underscores the fact that, while CTO RA procedures may be effective in managing certain patients, they also carry a significantly increased risk of this serious complication.
6. Discussion
Our study is the first to directly compare the cardiovascular outcomes of chronic total occlusion rotational atherectomy (CTO RA) and non-CTO RA. This is a new and important finding, as it provides valuable insights into the safety and efficacy of RA in these two groups, which have different levels of complexity. It is important to note that our comparisons are based on a baseline characteristic (CTO vs non-CTO coronary artery lesions) rather than on a treatment choice (rotational atherectomy vs non-atherectomy PCI), which is the decision faced by PCI operators. This is an important distinction, as it means that our findings should not be interpreted as a recommendation for or against RA in either of these groups.
Our findings suggest that CTO RA and non-CTO RA have similar cardiovascular outcomes, except for coronary perforation, which was significantly more common in the CTO RA group. This finding is consistent with previous studies, such as the study by Khand et al., which showed that the successful retrograde wiring of collateral channels in selected CTO patients undertaken by “CTO dedicated” operators can significantly enhance the chances of revascularization of complex CTOs with a low risk of acute serious complications [21]. The higher risk of coronary perforation in CTO RA procedures can be attributed to the inherent complexity of these lesions. CTOs are often long, tortuous, and have heavy calcification, making them more difficult to access and manipulate. Therefore, it is important to carefully select patients for CTO RA and to use the appropriate technique and equipment. Our findings also suggest that there are some important differences in the angiographic and procedural success rates of CTO RA and non-CTO RA. While the differences were slight, they are nonetheless important, as they highlight the challenges of CTO RA procedures. This underscores the importance of skillful operator technique, which is a critical factor in both the procedure's success and the patient's safety.
Sharma et al.'s review of the evolution of Rotational atherectomy (RA) techniques can provide valuable insights here [22]. Over the past three decades, RA techniques have matured and evolved with a focus on lesion modification to facilitate balloon angioplasty and stenting, contributing to improvements in procedural safety and the opportunity to use smaller caliber equipment and radial access. Such improvements might account for the comparable success rates we observed, despite the inherent complexity of CTO RA compared to Non-CTO RA. The heterogeneity that Sharma et al. note in RA utilization and technique may also provide a potential explanation for the differences we observed. Moreover, Sharma et al. emphasized the importance of being prepared to manage complications in RA, which aligns with our observation of a significantly higher risk of coronary perforation in the CTO RA group. This again stresses the importance of technical proficiency, experience, and meticulous procedural planning in performing these complex procedures. Overall, our study provides valuable insights into the safety and efficacy of CTO RA and non-CTO RA. Our findings suggest that CTO RA is a safe and effective procedure, but it is important to carefully select patients and to use the appropriate technique and equipment. It's conceivable that variability in practices across different institutions and operators could lead to differing outcomes, emphasizing the importance of standardizing techniques and strategies to ensure the best possible patient outcomes.
7. Limitation
Our meta-analysis has several limitations. The major limitations include:
-
■
Potential bias for greater operators' experience with RA in calcified CTO lesions
-
■
Selection bias
-
■
Small sample sizes
We were not able to do subgroup analysis by CTO lesion types based on JCTO scores. J-CTO (Japanese Chronic Total Occlusion) score is an angiographic scoring system used to predict the likelihood of successful guidewire crossing within 30 min. Therefore, it is not clear if RA outcomes in calcified CTO lesions are similar in all subsets of CTO lesions. Other potential limitations include a variable follow-up duration in some studies where it was reported and endpoints. Not all studies reported on each of the outcomes of interest. Additionally, as with all observational studies, unmeasured confounding factors may have influenced the results. For a more definitive understanding of the risks and benefits of CTO RA procedures, prospective randomized controlled trials are necessary. This would provide higher quality evidence to guide clinical decision-making in the treatment of patients with chronic total occlusions.
8. Conclusion
Our meta-analysis found that CTO RA procedures, while potentially effective in treating patients with chronic total occlusions, carry an increased risk of coronary perforation. Additionally, although not statistically significant, we observed a trend towards more complications and lower success rates.
The significantly higher risk of coronary perforation is of particular concern, given the severe consequences this complication can have. Physicians must therefore consider this risk when deciding to perform CTO RA and should ensure that patients are fully informed about the potential risks and benefits of the procedure.
The observation of increased complications and decreased success rates, even though not statistically significant, may suggest a need for further enhancement in procedural techniques, operator experience, or patient selection. This could potentially improve the outcomes of CTO RA procedures.
Our study underscores the need for further research into these treatments. In line with Sharma et al.'s call for continual evolution and improvement in RA strategies and techniques [22], our findings highlight areas for further exploration, such as refining the procedural approach and post-procedural management strategies. Ultimately, the goal is to optimize treatment strategies and improve outcomes for patients undergoing RA for CTO lesions.
The following are the supplementary data related to this article.
Funnel plots for all the outcomes of interest to evaluate publication bias of the studies analysed.
CRediT authorship contribution statement
Rakesh Reddy Devireddy: Conceptualization, Methodology, data curation, writing-Original draft preparation. Omar Qaqish: Data curation, Writing-Review and Editing. Kurian Pannikottu, Swetha Ramireddy, Nathan George: Data curation. Chadi Saad, Sujata Kambhatla, Awaneesh Kumar: Writing- Review & Editing. Ashok Kondur: Supervision. Md Sakibur Hassan: Formal analysis.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this article.
References
- 1.Fefer P., Knudtson M.L., Cheema A.N., et al. Current perspectives on coronary chronic total occlusions: the Canadian multicenter chronic total occlusions registry. J. Am. Coll. Cardiol. 2012;59(11):991–997. doi: 10.1016/j.jacc.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 2.Werner G.S., Martin-Yuste V., Hildick-Smith D., et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur. Heart J. 2018;39(26):2484–2493. doi: 10.1093/eurheartj/ehy220. [DOI] [PubMed] [Google Scholar]
- 3.Claessen B.E., Dangas G.D., Weisz G., et al. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3-year results from the HORIZONS-AMI trial. Eur. Heart J. 2012;33(6):768–775. doi: 10.1093/eurheartj/ehr471. [DOI] [PubMed] [Google Scholar]
- 4.Brilakis E.S., Banerjee S., Karmpaliotis D., et al. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (National Cardiovascular Data Registry) JACC Cardiovasc. Interv. 2015;8(2):245–253. doi: 10.1016/j.jcin.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Michael T.T., Karmpaliotis D., Brilakis E.S., et al. Procedural outcomes of revascularization of chronic total occlusion of native coronary arteries (from a multicenter United States registry) Am. J. Cardiol. 2013;112(4):488–492. doi: 10.1016/j.amjcard.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Joyal D., Afilalo J., Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am. Heart J. 2010;160(1):179–187. doi: 10.1016/j.ahj.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 7.Abdel-Wahab M., Richardt G., Joachim Büttner H., et al. High-speed rotational atherectomy before paclitaxel-eluting stent implantation in complex calcified coronary lesions: the randomized ROTAXUS (rotational Atherectomy prior to Taxus stent treatment for complex native coronary artery disease) trial. JACC Cardiovasc. Interv. 2013;6(1):10–19. doi: 10.1016/j.jcin.2012.07.017. [DOI] [PubMed] [Google Scholar]
- 8.Tomey M.I., Kini A.S., Sharma S.K. Current status of rotational atherectomy. JACC Cardiovasc. Interv. 2014;7(4):345–353. doi: 10.1016/j.jcin.2013.12.196. [DOI] [PubMed] [Google Scholar]
- 9.Benezet J., Díaz de la Llera L.S., Cubero J.M., Villa M., Fernández-Quero M., Sánchez-González A. Drug-eluting stents following rotational atherectomy for heavily calcified coronary lesions: long-term clinical outcomes. J. Invasive Cardiol. 2011;23(1):28–32. [PubMed] [Google Scholar]
- 10.Rathore S., Matsuo H., Terashima M., et al. Procedural and in-hospital outcomes after percutaneous coronary intervention for chronic total occlusions of coronary arteries 2002 to 2008: impact of novel guidewire techniques. JACC Cardiovasc. Interv. 2009;2(6):489–497. doi: 10.1016/j.jcin.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 11.Morino Y., Abe M., Morimoto T., et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (multicenter CTO registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc. Interv. 2011;4(2):213–221. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 12.Sianos G., Morel M.A., Kappetein A.P., et al. The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention J. Eur. Collab Work Group Interv. Cardiol. Eur. Soc. Cardiol. 2005;1(2):219–227. [PubMed] [Google Scholar]
- 13.Brilakis E.S., Grantham J.A., Rinfret S., et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc. Interv. 2012;5(4):367–379. doi: 10.1016/j.jcin.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Grantham J.A., Jones P.G., Cannon L., Spertus J.A. Quantifying the early health status benefits of successful chronic total occlusion recanalization: results from the FlowCardia’s approach to chronic total occlusion recanalization (FACTOR) trial. Circ. Cardiovasc. Qual. Outcomes. 2010;3(3):284–290. doi: 10.1161/CIRCOUTCOMES.108.825760. [DOI] [PubMed] [Google Scholar]
- 15.Maeremans J., Walsh S., Knaapen P., et al. The hybrid algorithm for treating chronic total occlusions in Europe: the RECHARGE registry. J. Am. Coll. Cardiol. 2016;68(18):1958–1970. doi: 10.1016/j.jacc.2016.08.034. [DOI] [PubMed] [Google Scholar]
- 16.Patel V.G., Brayton K.M., Tamayo A., et al. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc. Interv. 2013;6(2):128–136. doi: 10.1016/j.jcin.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 17.Elbasha K., Mankerious N., Alawady M., et al. Long-term outcomes after rotational atherectomy for calcified chronic total occlusion versus nonchronic total occlusion coronary lesions. J. Interv. Cardiol. 2022;2022:2593189. doi: 10.1155/2022/2593189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee K., Jung J.H., Lee M., et al. Clinical outcome of rotational atherectomy in calcified lesions in Korea-ROCK registry. Med. Kaunas Lith. 2021;57(7):694. doi: 10.3390/medicina57070694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brinkmann C., Eitan A., Schwencke C., Mathey D.G., Schofer J. Rotational atherectomy in CTO lesions: too risky? Outcome of rotational atherectomy in CTO lesions compared to non-CTO lesions. EuroIntervention J. Eur. Collab Work Group Interv. Cardiol. Eur. Soc. Cardiol. 2018;14(11):e1192–e1198. doi: 10.4244/EIJ-D-18-00393. [DOI] [PubMed] [Google Scholar]
- 20.Tsai T.C., Lo W.J., Chen W.J., et al. Rotational atherectomy for chronically and totally occluded coronary lesions: a propensity score-matched outcomes study. Front. Cardiovasc. Med. 2022:9. doi: 10.3389/fcvm.2022.1061812. Accessed October 10, 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khand A., Patel B., Palmer N., et al. Retrograde wiring of collateral channels of the heart in chronic total occlusions: a systematic review and meta-analysis of safety, feasibility, and incremental value in achieving revascularization. Angiology. 2015;66(10):925–932. doi: 10.1177/0003319715573902. [DOI] [PubMed] [Google Scholar]
- 22.Sharma S.K., Tomey M.I., Teirstein P.S., et al. North American expert review of rotational atherectomy. Circ. Cardiovasc. Interv. 2019;12(5) doi: 10.1161/CIRCINTERVENTIONS.118.007448. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Funnel plots for all the outcomes of interest to evaluate publication bias of the studies analysed.