Abstract
Multi-slice computed tomography (MSCT) is the primary method for the detection and visualization of foreign bodies in the pulmonary artery because it provides high sensitivity and accuracy. It is very difficult to diagnose a patient with a non-iatrogenic pulmonary artery foreign body who does not have a history of a penetrating trauma. This case report describes a 36-year-old male that presented with coughing and haemoptysis. Based on conventional coronal and cross-sectional CT, the foreign body was misdiagnosed as pulmonary tuberculosis and pulmonary artery thrombosis. During treatment of the bronchial artery embolization and anti-tuberculosis therapy, the patient continued to experience haemoptysis. After further analysis of the pulmonary artery CT angiography images and curved multiplane reconstruction, an approximately 6-cm long toothpick was identified in the pulmonary artery with an unclear entry route. After surgery to remove the toothpick, symptoms of coughing and haemoptysis were resolved. This current case demonstrated that multiplane reconstruction in MSCT can improve the detection and visualization of pulmonary artery foreign bodies, which can aid in the diagnosis of pulmonary artery diseases of unknown cause.
Keywords: Foreign body, pulmonary artery, computed tomography, multiplane reconstruction
Introduction
Iatrogenic foreign bodies in the pulmonary circulation have been reported, usually due to the fracture and embolism of central or peripheral venous catheters. 1 Non-iatrogenic cases are rare in the clinic, especially those with an unknown cause and unclear entry route. 1 Foreign body pulmonary embolisms are often difficult to diagnose because of their varied clinical presentation, the nature of the embolizing material and dubious radiological features.
Computed tomography (CT) is the primary advanced imaging technique to diagnose pulmonary artery disease. The post-processing techniques of curved multiplanar reformation (MPR) reconstruction can comprehensively observe the shapes from multiple angles and improve the characterization of foreign bodies. This current case report describes the use of MPR in multi-slice computed tomography (MSCT) for the diagnosis of a patient with a non-iatrogenic foreign body in the pulmonary artery.
Case report
On 4 August 2022, a 36-year-old male had an initial chest CT examination at Wuxuan People’s Hospital, Wuxuan, Guangxi, China which revealed inflammatory lesions in the left upper lobe of the lung. Despite in-patient treatment, there was no significant improvement. On 14 August 2022, the patient was transferred to the Liuzhou People’s Hospital Affiliated to Guangxi Medical University with a complaint of ‘cough accompanied by sputum containing blood for more than 10 days, without apparent inducement’. The patient presented with a fresh red complexion, without evident aversion to cold, chills, fever, dizziness, headache, nasal congestion, rhinorrhoea, sore throat, chest pain, night sweats, abdominal pain, bloating, vomiting, diarrhoea, orthopnoea or precordial oppression. There were no complaints of limb or joint pain. The patient had a lengthy medical history of ‘thalassaemia’ and a prior history of blood transfusion, but the details were unknown. Laboratory examination after admission observed the following: haemoglobin 75 g/l; O Rh (D) positive; T-SPOT positive; α-thalassemia; glucose-6-phosphate dehydrogenase deficiency. CT images showed irregular and indistinct opacities in the posterior segment of the left upper lobe tip, as well as localized areas of ground glass opacities and the presence of tree-in-bud signals. Punctate high-density lesions were observed in the mediastinal window CT images, which were initially diagnosed as inflammatory lesions and were possibly accompanied by alveolar haemorrhage (Figure 1). After undergoing a comprehensive consultation with the medical team, the patient underwent 1 week of anti-tuberculosis therapy as follows: 0.3 g isoniazid once a day, 0.75 g ethambutol once a day and 1 g pyrazinamide once a day, all administered orally. In addition, the patient underwent bronchial artery embolization treatment using 100 mg polyvinyl alcohol particles (350 μm) in combination with 10 ml iohexol (100 ml: 35 g [I]) formulated as a suspension. The suspension was administered intravascularly at a rate of 2 ml/min until vascular occlusion was achieved and confirmed by the retention of the contrast agent used for bronchial artery angiography (Figure 2). These treatments resulted in improvement, leading to his discharge from hospital. Unfortunately, after discharge, the patient began experiencing haemoptysis again, without any clear underlying cause on 10 September 2022. Laboratory examination hinted at acute immune haemolysis. CT angiography revealed a persistent patchy lesion in the posterior segment of the left upper lobe apex (Figures 3a and 3b). There was no significant change in the high-density lesion in the posterior segment of the left upper lobe apex; and no improvement in haemoptysis and pulmonary embolism. The lesion was located in the pulmonary artery at the proximal end, with surrounding thrombosis and inflammatory tissue wrapping at the distal end (Figures 3c–3e). A curved reconstruction technique was used to visualize a linear high-density lesion of 6 cm length in the area of the pulmonary artery running along the posterior segment of the left upper lobe apex (Figures 3f–3h). A potential foreign body in the pulmonary artery was suspected, but there was insufficient diagnostic basis for pulmonary tuberculosis. Consequently, the administration of anti-tuberculosis drugs was discontinued and surgical treatment was decided. However, before the surgery, laboratory examination hinted at acute immune haemolysis. After repeated blood transfusions and related treatments, re-examination of the haemoglobin level (27 g/l) on 19 September 2022 showed that the infusion of washed red blood cells had been ineffective. The patient appeared to be having a haemolytic crisis. The patient’s condition was improved after undergoing three plasmapheresis treatments. On 11 October 2022, the patient underwent a follow-up CT examination. The absorption of the exudate lesion in the posterior segment of the left upper lobe was reduced and a local cavity was formed (Figure 4a). A high-density shadow at the lung window was located inside the cavity (Figure 4b). MPR curved reconstruction showed a distinct linear high-density shadow running along the pulmonary artery branch and passing through the cavity (Figure 4c). The proximal end was located inside the pulmonary artery with peripheral thrombosis (Figure 4d). On 20 October 2022, during the surgery, a complete toothpick of 6 cm length and proximal massive thrombus were discovered in the main pulmonary artery at the posterior segment of the left upper lung apex (Figure 5). By 27 July 2023, the left pleural effusion has completely absorbed and the left lower lobe of the lung was fully dilated (Figure 6).
Figure 1.
Axial and coronal computed tomography images of a 36-year-old male who presented with coughing and haemoptysis showed that the focus was patchy, a local tree-in-bud sign was present (a, b, c, d) and the pulmonary artery had mural thrombus (e, f, g, h).
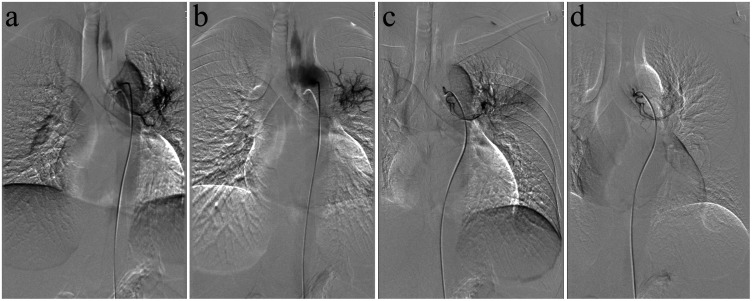
Figure 2.
Bronchial artery embolization in a 36-year-old male who presented with coughing and haemoptysis. The left bronchial artery was observed from the right wall of the thoracic aorta, exhibiting thickening and twisting. Within the upper lobe of the left lung, a large number of disorderly arranged clusters and reticular vessels were observed (a). Small areas of contrast medium overflow staining were seen in the parenchymal phase, along with the presence of a bronchial artery-pulmonary artery shunt (b). After embolization, the responsible blood vessel was occluded and the original contrast agent overflow staining disappeared (c, d).
Figure 3.
Computed tomography angiography images of a 36-year-old male who presented with coughing and haemoptysis. Persistent patchy lesion in the posterior segment of the left upper lobe apex (a, b). The lesion was located in the pulmonary artery at the proximal end, with surrounding thrombosis and surrounding inflammatory tissue wrapping at the distal end (c, d, e). Linear high-density lesion in the area of the pulmonary artery running along the posterior segment of the left upper lobe apex (f, g, h).
Figure 4.
Axial and coronal computed tomography images of a 36-year-old male who presented with coughing and haemoptysis showed a local cavity with a high-density shadow within the cavity (a, b). Curved multiplanar reformation reconstruction images showed a distinct linear high-density shadow running along the pulmonary artery branch and passing through the cavity (c, d).
Figure 5.
Intraoperative photography of a 36-year-old male who presented with coughing and haemoptysis. A complete toothpick approximately 6 cm in length (a) and a proximal massive thrombus (b) were discovered in the main pulmonary artery at the posterior segment of the left upper lung apex. The colour version of this figure is available at: http://imr.sagepub.com.
Figure 6.
Postoperative follow-up computed tomography images of a 36-year-old male who presented with coughing and haemoptysis. The left pleural effusion has completely absorbed (a, b) and the left lower lobe of the lung was fully dilated (c, d).
This case report was approved by the Ethics Committee of the Liuzhou People’s Hospital (no. KY-E-02). The patient was informed about the whole procedure. He provided written informed consent for treatment and publication of this case report. This case report conformed to CARE guidelines. 2
Discussion
Multi-slice CT serves as the primary modality for the examining and diagnosing pulmonary artery foreign bodies. CT has high sensitivity and accuracy in detecting these foreign bodies, but they might still be misdiagnosed or missed. Repeated CT examination and MRP curved reconstruction can improve the diagnostic confidence.
This current case report presents a rare instance of a pulmonary foreign body. This patient initially presented with haemoptysis and the pulmonary lesion was located in the posterior segment of the upper lobe tip of the left lung. Axial and conventional coronal reconstruction showed that the focus was patchy and presented with a local tree-in-bud sign. The tree-in-bud sign is a CT manifestation of early tuberculosis infection spread through the bronchi, which is a common sign of active pulmonary tuberculosis. 3 Tuberculosis often presents with various lesion morphologies and is prone to calcification. Due to the high oxygen tension in the upper lungs, 4 secondary pulmonary tuberculosis is more likely to occur in the apical posterior segment. Pulmonary tuberculosis was suspected because Guangxi Zhuang Autonomous Region is a high-incidence area for tuberculosis and the patient had a lesion in the apical posterior segment, which is the most common site for tuberculosis. In addition, the patient did not have a clear history of foreign-body ingestion. The foreign body appeared as punctate high-density shadows on routine axial and coronal images. The inflammatory lesions in apical and posterior images blurred the spot-like slightly high-density shadow of the foreign body due to the volume effect, which was misinterpreted as tuberculosis calcification, especially in the absence of metal artifacts. 5 Notably, this coincided with a positive result in the detection of Mycobacterium tuberculosis-specific T cells, along with clinical symptoms such as cough and expectoration. In addition, this patient had thalassaemia and was also prone to fungal infections such as aspergillus infection. Patients with aspergillus infection often show haemoptysis and the focus shows a tree-in-bud sign, which is consistent with an infection originating from the airway. Aspergillus infection can easily become calcified because of the absorption of minerals such as ferromanganese from the air. The cavity that appeared during the later stages of treatment could be potentially misdiagnosed as aspergillus infection. The postoperative diagnosis was a toothpick in the pulmonary artery. The entry route of the toothpick was not completely clear.
Pulmonary artery foreign bodies are relatively rare and most of the pulmonary circulation foreign bodies reported in the literature are iatrogenic, including fragments of catheter materials and intravascular devices;6,7 as well as various shrapnel and metals dissociated to blood vessels after trauma. 8 Reports of pulmonary artery foreign bodies caused by non-iatrogenic toothpicks are rare and even rarer is the case where the entry route of the toothpick foreign bodies was unclear. 5 Because of the different clinical manifestations and different properties of foreign bodies, it can be relatively difficult to diagnose foreign-body pulmonary embolism. Generally, foreign-body-induced pulmonary embolism is associated with a clear history of penetrating trauma. However, this patient lacked a history of foreign-body penetration, which brought difficulties to the diagnosis. The foreign body was relatively regular and linear, which lead to speculation that it was a medical injection needle. But the patient made it clear that he had not been transfused since 7 years of age. At the time of diagnosis, the patient was 36 years old and had not experienced any symptoms of discomfort during the period. The possibility was small but could not be completely ruled out. Considering the patient’s previous history of drunkenness and falls, there was also speculation that he had swallowed a fishbone. There are three normal physiological strictures of the oesophagus, with the second constriction situated at the intersection of the oesophagus and trachea, where the oesophagus is adjacent to the trachea, left and right main bronchi, left and right pulmonary arteries, veins and aorta and. It is possible to pierce the oesophagus and break into the pulmonary artery. Throughout the whole course of the disease, there were no clear symptoms of oesophageal foreign body obstruction such as swallowing discomfort or chest pain. Similarly, there were no related symptoms such as oesophageal mediastinal fistula and oesophageal pulmonary artery fistula. Consequently, it was inferred that it was unlikely that the foreign body had entered the pulmonary artery from the oesophagus. The toothpick was made of bamboo, sharp at both ends, and like a fishbone, it was unlikely to enter the pulmonary artery from the oesophagus. The patient had previously fallen and injured his left front chest wall-clavicle area. It is unlikely that the toothpick could have pierced into the chest wall without damaging a blood vessel. In the context of bamboo foreign body injury, CT is more valuable in the early stage.9,10 After repeated CT examinations, the linear suspicious foreign body running inside the pulmonary artery of the upper lobe of the left lung always remained and the diagnosis of a pulmonary artery foreign body was confirmed. The shape and type of lung foreign body are various; and their impact on the human body mainly depends on the shape, size, texture and retention site of the foreign body. Pulmonary foreign bodies can cause pulmonary embolism, septicaemia, infective endocarditis, septic pulmonary infarction, pulmonary infection and other serious complications.11,12
A previous report described a similar case. 1 A 46-year-old male presented with recurrent haemoptysis following coughing. 1 Chest CT revealed a linear high-density shadow in the right lower lobe basal segment pulmonary artery course, accompanied by surrounding infiltration. Due to an unclear diagnosis and consideration of possible infection, a multidisciplinary discussion led to the decision for surgical intervention. During the surgery, an approximately 7-cm long tubular wooden object was found within the pulmonary artery of the right lower lobe basal segment. According to the patient, it was identified as a pine needle from a Maritime Pine tree where he had run approximately 300 km and believes he could have easily inhaled a pine needle. The patient had no clear history of penetrating trauma and the mechanism by which the pine needle entered the pulmonary artery remained perplexing. The axial view of the patient’s CT scan clearly displayed a linear shadow along the course of the pulmonary artery, making the diagnosis relatively straightforward compared with the present case. Infections caused by foreign bodies often present as a hazy ground-glass opacities along the course of the pulmonary artery, similar to the findings in the current case, suggesting a chronic process. The current patient showed a favourable prognosis during follow-up.
Haemoptysis is an important clinical manifestation of patients with pulmonary embolism and plays an important role in evaluating the possibility of pulmonary embolism. Combined with the course of the disease and the volume of haemoptysis, the current patient was considered to have massive haemoptysis caused by a chronic pulmonary embolic event.13–16 Fibreoptic bronchoscopy showed active bleeding in the posterior segment of the upper lobe tip of the left lung during haemoptysis, which also suggested the possibility of pulmonary artery bronchial fistula. The foreign body may pierce or inflammatory factors spread to the adjacent bronchi to form pulmonary bronchial fistula. These clinical findings provide a reliable basis for an accurate aetiological diagnosis and also suggests the importance of dynamic CT re-examination.
The treatment of foreign bodies in the pulmonary artery is complicated. Interventional therapy and surgical treatment are selected according to the patient’s symptoms and possible complications. Interventional therapy is mostly due to iatrogenic foreign bodies, which is often used for immediate treatment of foreign bodies.17–19 Surgical resection is frequently used when the foreign body is located in the right pulmonary artery system and the guide catheter cannot be reached. When the foreign body is located in the main trunk or large branch of the left pulmonary artery, a blue catheter can be used to trap it, but due to its anatomical position, it cannot be placed directly into the pulmonary artery system. This current patient had a long disease course, severe pulmonary embolism and a complicated infection. Due to the particularity of the location of the foreign body, life-threatening complications may arise at any time. Therefore, surgical removal of foreign bodies from the pulmonary artery is the first treatment of choice.
In conclusion, this case of a foreign body in the pulmonary artery was extremely rare and the pathway of entry was not completely clear. There are few previous reports on the literature. When encountering similarly difficult cases in our work, multi-angle MPR reconstruction may be able to find a new way to observe the overall shape of foreign objects and improve the diagnosis of pulmonary artery diseases of unknown cause.
Acknowledgements
We thank Xiaomin Liu from Clinical & Technical Support, Philips Healthcare for editing the language of a draft of this manuscript.
Footnotes
Author contributions: Qinxiang Mao: writing – original draft preparation; Zheng Lv and Qiuli Han: image analysis; Wei Zhang: writing – review and editing. All authors have read and agreed to the published version of the manuscript.
The authors declare that there are no conflicts of interest.
Funding: This research received no specific grant from funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Wei Zhang https://orcid.org/0000-0002-0544-786X
References
- 1.Ciarrocchi AP, Parisi AM, Campisi A, et al. A strange case of foreign body embolism in the right lower pulmonary artery. Gen Thorac Cardiovasc Surg 2021; 69: 894–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache 2013; 53: 1541–1547. [DOI] [PubMed] [Google Scholar]
- 3.Jin XJ, Kim JM, Kim HK, et al. Histopathology and TB-PCR kit analysis in differentiating the diagnosis of intestinal tuberculosis and Crohn’s disease. World J Gastroenterol 2010; 16: 2496–2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goodwin RA, Des Prez RM. Apical localization of pulmonary tuberculosis, chronic pulmonary histoplasmosis, and progressive massive fibrosis of the lung. Chest 1983; 83: 801–805. [DOI] [PubMed] [Google Scholar]
- 5.Qu PF, Bai BL, Duan T, et al. Multiple Pulmonary Infarction and Abscess Caused by a Bamboo Stick Accidentally Piercing into Chest: a Case Misdiagnosed as Pulmonary Tuberculosis. Chin Med Sci J 2021; 252–256. [DOI] [PubMed] [Google Scholar]
- 6.Dell’Amore A, Ammari C, Campisi A, et al. Peripheral venous catheter fracture with embolism into the pulmonary artery. J Thorac Dis 2016; 8: E1581–E1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee CJ, Joo HC, Won JY, et al. A Foreign Body Inside the Pulmonary Artery After Heart Transplantation. JACC Cardiovasc Interv 2016; 9: 1191–1192. [DOI] [PubMed] [Google Scholar]
- 8.Kawaguchi M, Yamamoto H, Yamada T, et al. Penetrating thoracic ice pick injury extending into pulmonary artery: Report of a case. Int J Surg Case Rep 2018; 52: 63–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakata H, Egashira K, Nakamura K, et al. Bamboo foreign bodies in lung parenchyma: CT features. Clin Imaging 1992; 16: 117–120. [DOI] [PubMed] [Google Scholar]
- 10.Kitajiri S, Tabuchi K, Hiraumi H. Transnasal bamboo foreign body lodged in the sphenoid sinus. Auris Nasus Larynx 2001; 28: 365–367. [DOI] [PubMed] [Google Scholar]
- 11.Pan GZ, Bastidas JG, Hasaniya NW, et al. Bullet embolization from an aorto-caval fistula to the heart. Interact Cardiovasc Thorac Surg 2013; 16: 710–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bach AG, Restrepo CS, Abbas J, et al. Imaging of nonthrombotic pulmonary embolism: biological materials, nonbiological materials, and foreign bodies. Eur J Radiol 2013; 82: e120–e141. [DOI] [PubMed] [Google Scholar]
- 13.Stein PD, Terrin ML, Hales CA, et al. Clinical, laboratory, roentgenographic, and electrocardiographic findings in patients with acute pulmonary embolism and no pre-existing cardiac or pulmonary disease. Chest 1991; 100: 598–603. [DOI] [PubMed] [Google Scholar]
- 14.Reesink HJ, Van Delden OM, Kloek JJ, et al. Embolization for hemoptysis in chronic thromboembolic pulmonary hypertension: report of two cases and a review of the literature. Cardiovasc Intervent Radiol 2007; 30: 136–139. [DOI] [PubMed] [Google Scholar]
- 15.Uzun O, Atasoy Y, Findik S, et al. A prospective evaluation of hemoptysis cases in a tertiary referral hospital. Clin Respir J 2010; 4: 131–138. [DOI] [PubMed] [Google Scholar]
- 16.Yang S, Wang J, Kuang T, et al. Efficacy and Safety of Bronchial Artery Embolization on Hemoptysis in Chronic Thromboembolic Pulmonary Hypertension: A Pilot Prospective Cohort Study. Crit Care Med 2019; 47: e182–e189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uflacker R, Lima S, Melichar AC. Intravascular foreign bodies: percutaneous retrieval. Radiology 1986; 160: 731–735. [DOI] [PubMed] [Google Scholar]
- 18.Pelage JP, El Hajjam M, Lagrange C, et al. Pulmonary artery interventions: an overview. Radiographics 2005; 25: 1653–1667. [DOI] [PubMed] [Google Scholar]
- 19.Schechter MA, O’Brien PJ, Cox MW. Retrieval of iatrogenic intravascular foreign bodies. J Vasc Surg 2013; 57: 276–281. [DOI] [PubMed] [Google Scholar]