Abstract
Objectives.
Less than 5% of eligible U.S. individuals undergo lung cancer screening (LCS). A significant barrier is lack of awareness; more effective outreach and education strategies are needed to achieve greater population LCS uptake. Tobacco Treatment Specialists (TTSs) are an untapped resource to assist and understanding TTS knowledge and perspectives about LCS and readiness and capacity to assist is a critical first step.
Methods.
A sequential explanatory mixed-methods study design was conducted to understand LCS knowledge, attitudes, beliefs, and practices of TTSs. A cross-sectional survey (N=147) was conducted supplemented with 3 focus groups (N=12).
Results.
TTSs lacked good working knowledge about LCS in general and screening guidelines, but think it is important for their patient population and open to routinely assessing and adding this educational component into their current workflow.
Conclusions.
Tobacco treatment offers a unique venue for LCS awareness and is a setting where there are experienced specialists trained in tobacco use assessment and treatment. Results highlight the unmet training needs required to facilitate integration of tobacco treatment and LCS.
Practice Implications.
TTSs are an expanding healthcare workforce. There is a strong need for current TTSs to receive additional training in the benefits of LCS.
INTRODUCTION
Although lung cancer screening (LCS) has the potential to reduce lung cancer-related mortality by up to 25%, fewer than 5% of eligible at-risk U.S. individuals with a history of smoking undergo LCS.1–2 Among the 34.1 million Americans who currently smoke cigarettes, it is estimated that approximately 15% are eligible to screen for lung cancer.3 Individuals are eligible for LCS if they are aged 50 to 80 years, have a 20-pack-year smoking history, and currently smoke or quit within the past 15 years.4 More effective strategies for outreach and education are necessary to realize the public health benefit of screening and achieve greater population uptake of LCS. Current efforts are public service and primary care based.5–6 However, an untapped yet promising resource are Tobacco Treatment Specialists (TTS). While several studies have examined the inclusion of tobacco treatment at the time of LCS as a potentially ‘teachable moment’ for cessation, to our knowledge, this is the first study to examine the knowledge and awareness about LCS among their screening-eligible patients.7–11 A TTS is specially trained to provide evidence-based tobacco treatment in a wide variety of community and health care settings. These clinicians attend a 3–5-day training program and develop knowledge and core competency skills to deliver tobacco dependence treatment.12 Collectively, accredited TTS training programs train about 2,000 TTSs every year.8 TTSs are trained in motivational interviewing and collaborative treatment planning and are particularly well positioned to educate individuals who smoke cigarettes and qualify for LCS about screening given their background. Nonetheless, TTSs need to have adequate knowledge about LCS including benefits and potential risks to realize this reach. Understanding the knowledge and perspectives of TTSs about LCS as well as their readiness and capacity to incorporate LCS awareness and education into their practice is an important component before engaging TTSs in efforts to increase LCS.
Purpose
The purpose of this study was to understand LCS knowledge, attitudes, and beliefs of TTSs as a foundational component for guiding the development of: (1) LCS-related training content, methodology and resources in the context of tobacco treatment training; and (2) a multilevel intervention to address knowledge and awareness of LCS among at-risk individuals who currently smoke. This paper addresses the following specific aims: 1) describe current LCS knowledge, attitudes, and beliefs among TTSs; 2) describe TTS current practices and perceived barriers to discussion of LCS with individuals who currently smoke; and 3) explore the viability of leveraging TTSs in the public health efforts of increasing LCS awareness among screening-eligible individuals including needed resources from the TTS perspective.
METHODS
Data for this study were collected as part of a sequential explanatory QUAN→qual mixed methods design13–14 to understand LCS knowledge, attitudes, beliefs, and current practices of TTSs. In this design, the quantitative portion (QUAN; Phase I) is implemented first, and the qualitative portion (qual; Phase II) follows and is used to explain/extend the quantitative findings.13–14 A QUAN→qual mixed methods design was chosen because while we understand knowledge, attitudes, and beliefs about LCS from other perspectives,6 we do not understand this topic from the TTS perspective. The qualitative component allowed us a more robust understanding of the quantitative data to better understand the knowledge, attitudes, and beliefs of TTSs on the topic of LCS. Quantitative and qualitative findings were fully integrated during data interpretation. Both study phases were approved by the Memorial Sloan Kettering Cancer Center Institutional Review Board; all research team members had human subjects training, and all participants provided informed consent.
Phase I: Quantitative
Recruitment Eligibility
The Association for the Treatment of Tobacco Use and Dependence (ATTUD) is the professional organization of TTSs with approximately 600 members to date; membership is broadly representative of TTSs practicing in the U.S. Study eligibility criteria included: 1) aged 18 years or older; 2) self-identified as a TTS; and 3) practicing in the U.S. We partnered with ATTUD leadership to assist with recruitment. Specifically, ATTUD members were sent an email from the ATTUD president introducing the survey.
The email described the study and explained what study participation involved as well as the study’s voluntary nature. Within one week of this email, the study principal investigator sent an email with a secure web-based link to the survey and an electronic informed consent document acknowledging their willingness to participate.
Data Collection
A 48-item self-report web-based survey was developed to measure knowledge, attitudes, beliefs, practice behaviors and barriers to LCS discussions in the patient population served by TTSs. These items included assessing sociodemographic characteristics (gender, age, race/ethnicity, education, practice setting, geographic practice location, professional licensure, national certification, professional organizational membership, years in practice, weekly work hours, average number of weekly patients, tobacco treatment type), knowledge about LCS and guidelines, attitudes, and beliefs about LCS, and barriers to LCS discussions with patients. Data were collected via a single web-based survey using REDCap (Research Electronic Data Capture), a secure web-based application for building and managing online surveys and databases. Embedded within the opening message was an informed consent document that was signed electronically by individuals who agreed to participate. A telephone number and study email address was provided for questions. Participants received a $25 Amazon gift card via email at survey completion.
Measures
Total knowledge was assessed with a 7-item scale adapted from Mukthinuthalapati et al. (2020) ranging from 1 (low knowledge) to 7 (high knowledge) about LCS criteria.15 In addition, knowledge of the U.S. Preventive Services Task Force (USPSTF) current LCS guidelines was assessed with five clinical scenarios presented containing patient age, pack-year history, and smoking status. Participants were asked to indicate which, if any, screening test they would recommend according to the clinical scenarios presented with potential responses of low dose computed tomography (LDCT) of the chest, chest x-ray, no screening, or not sure. LDCT of the chest is the only USPSTF recommended screening method for lung cancer. Therefore, scenarios within the age and pack-year criteria with responses choosing LDCT only were correct. Scores ranged from 0 (indicative of lack of knowledge of the USPSTF LCS guidelines) to 5 (indicative of high knowledge).
Attitudes and beliefs about LCS were assessed with five items rating beliefs about the evidence for LCS applying to their patient population, belief that LCS is safe, if patients ask about LCS, frequency of discussing LCS, and prior continuing education related to LCS. In addition, three Likert-response option items about the perception of benefits and importance of LCS for screening-eligible patients were assessed.
Barriers to LCS discussions were assessed with 10 items using a 4-point Likert-response option from strongly disagree to strongly agree. Finally, demographic characteristics were queried including professional practice history and practice specific characteristics.
Data Analyses
Participant survey responses were de-identified and assigned a participant ID code. Data were exported from REDCap into SAS version 9.4 (SAS Institute, Cary, NC) and cleaned by examining frequency tables and removing invalid data. Data were evaluated for outliers and to determine if the data were normally distributed. Because we were most interested in describing knowledge and perspectives, data were analyzed using descriptive statistics (relative frequencies, mean, standard deviation, and range).
Phase II: Qualitative
Phase II was a qualitative component in which focus groups were conducted via Zoom web-based platform with a sub-set of the Phase I participants. Focus groups were chosen because this method is recommended for collecting data involving perceptions in a defined area of interest in a nonjudgmental, non-threatening environment.16 Participants in Phase II were asked to expand on responses to items from the Phase I survey for a more robust understanding of the TTS perspective.
Sampling and Recruitment
Participants who completed the Phase I survey were asked at the survey end if they would be willing to participate in a follow-up focus group interview. Seventy-three (73; 49.7%) participants expressed willingness to do so. Selective sampling was used to recruit a subsample of 12 persons who represented both individuals with high and low LCS knowledge, as well as favorable and unfavorable attitudes and beliefs toward LCS.
Data Collection
Semi-structured focus group interview guides16 were developed from the Phase I survey items to assess knowledge about LCS, prior experience with patients related to LCS, barriers to discussing LCS with patients, information helpful to support TTS discussions about LCS, and thoughts about the 2021 USPSTF LCS criteria change (which lowered the age and pack-year eligibility to 50 years and 20 pack-years respectively).
Three focus groups were conducted, and the group interviews ranged from 45 to 54 minutes in duration. An experienced moderator led the focus group discussions using a semi-structured interview guide derived from a comprehensive literature review related to knowledge, attitudes, and beliefs about LCS. All participants were noted to be forthcoming with their thoughts and feelings about LCS discussions, potential role of the TTS, and challenges to integrating these types of conversation into their current practice. The interviews were digitally recorded and transcribed verbatim. Each transcript was given an identification number and participants referred to themselves by their speaker number during the interview. No identifying data were included in the transcripts. The first author (LCB) compared the transcripts to the audio recordings and made corrections as needed. The transcripts were reviewed independently by three researchers (LCB, LW, and VF).
Data Analysis
Data were analyzed using conventional thematic content analysis, an inductive process that allows codes and categories to emerge from the data rather than a deductive process confirming or refining a pre-existing theoretical structure.17 To address the aims, we focused primarily on the participants’ direct responses to the interviewer’s initial query to knowledge about LCS (i.e., What do you know about lung cancer screening as it relates to smoking?). It was important to examine participant unprompted knowledge about LCS before delving into specifics around the TTS role in LCS.
Three research team members experienced in qualitative data analysis (LCH, LW, and VF) coded each transcript individually. Data were extracted and divided into text units (i.e., words/phrases/sentences/short passages capturing a single thought). Each text unit was labeled with a short code capturing its essence.17 The codes were then entered into a data display table. The tables were constructed by assigning a row to each participant and group labelling it with their group number followed by their study ID number. The table had two columns—one displayed each participant’s basic demographic information and one displayed all the codes associated with that participant.
Information was summarized on the tables using a process of discussion and consensus by the research team. Because the analysis involved a low level of interpretation, analytic disagreements were few and easily resolved by a re-examination of the data. The research team determined that the focus group interviews yielded ample data to provide a robust description of knowledge, attitudes and beliefs, barriers to LCS discussions, and practice behaviors among TTSs. A narrative description of each category was prepared and reviewed by the team.
RESULTS
Phase I (Quantitative) Results
Sample Description
598 invitations were sent to ATTUD members practicing in the U.S. with a 24.6% response rate (n=147). Of those who responded by clicking the link to read the introduction to the survey opportunity (n=232), there was a 63.4% completion rate (n=147). Consistent with ATTUD membership, participants were mostly female (79%; n=122), white (84%; n=129), and ranged in age from 25–72 years with a mean age of 47.1 (SD 13.2). Most participants identified as having attained the National Certificate for Tobacco Treatment Practice (91%; n=140) and represented a variety of health professions. A full description of participant sociodemographic and practice characteristics are reported in Table 1.
Table 1.
Participant Sociodemographic and Practice Characteristics
| Variable | Group | n (%) |
|---|---|---|
| Gender | Female | 122 (79%) |
| Male | 25 (16%) | |
| Hispanic ethnicity | No | 142 (92%) |
| Race | White | 129 (84%) |
| Black | 9 (6%) | |
| Asian | 3 (2%) | |
| Indian or Indian American | 1 (1%) | |
| Native Hawaiian or Alaskan Native | 1 (1%) | |
| Other | 4 (3%) | |
| Education Level | Some College | 8 (5%) |
| Undergraduate Degree | 44 (29%) | |
| Master’s Degree | 76 (49%) | |
| Doctoral Degree | 23 (15%) | |
| Geographic Area of Practice | Rural | 38 (25%) |
| Suburban | 38 (25%) | |
| Urban | 73 (47%) | |
| Practice Setting | * Other | 42 (27%) |
| Hospital | 38 (25%) | |
| Cancer Center | 19 (12%) | |
| University or Academic Setting | 18 (12%) | |
| Medical Office | 17 (11%) | |
| Community Center | 7 (5%) | |
| State Quitline | 6 (4%) | |
| Lung Cancer Screening Program | 2 (1%) | |
| Dental Office | 1 (1%) | |
| Professional Identity | Tobacco Treatment Specialist | 69 (45%) |
| Social Worker | 18 (12%) | |
| Nurse Practitioner | 14 (9%) | |
| Nurse | 13 (8%) | |
| Addictions Counselor | 12 (8%) | |
| Respiratory Therapist | 10 (6%) | |
| Pharmacist | 5 (3%) | |
| Physician | 3 (2%) | |
| Psychologist | 4 (3%) | |
| Completion of the National Certificate in Tobacco Treatment Practice (NCTTP) | Yes | 140 (91%) |
| Variable | Mean (SD) | |
| Age (n=147) | 47.1 (13.2) | |
| Years in Practice (n=146) | 6.7 (7.8) | |
| Number of Hours Practicing per Week (n=147) | 20 (15.4) | |
| Number of Patients Seen Daily (n=144) | 12.7 (21) | |
Other represents a variety of practice settings including remote/telehealth, pharmacy services, area health education center, government, homeless shelter, nonprofit public health organization, and county jail.
Knowledge, Attitudes, and Beliefs
Participants reported relatively little knowledge of USPSTF LCS guidelines with a total mean score of 2.7 (SD 1.4) (range 1=low knowledge to 7=high knowledge). Nearly all (96.2%; n=141) reported they agree that LCS would be beneficial for most of their screening-eligible patients; 96.8% (n=142) reported they agree that it is important for all eligible patients to be made aware of the option to screen. Nearly all (96.8%; n=142) reported agreement that it is important for all eligible patients to have a discussion with their primary care clinician about the option to screen for lung cancer.
Barriers to Lung Cancer Screening Discussions
Several barriers to LCS discussions were identified (Figure 1). Nearly half (44.2%; n=68) reported they did not know enough about LCS to effectively discuss it with their patients, and over one-third (36.4%; n=56) believed patients were unlikely to adhere to LCS and follow-up recommendations. A smaller, but significant number of participants (11.0%; n=17) believed that LCS may expose patients to harm. However, most did not have concerns that bringing up LCS would interfere with their tobacco treatment efforts and did not identify inadequate time as a barrier to addressing LCS in their practice. Figure 1 provides more details about potential barriers to LCS discussions.
Figure 1.
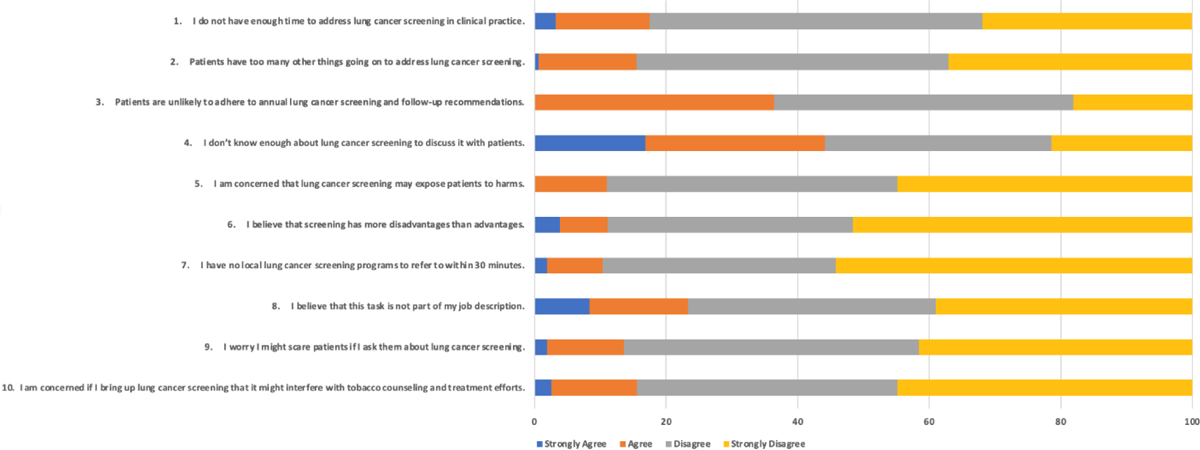
Potential Barriers to Lung Cancer Screening Discussions in Tobacco Treatment.
Practice Behaviors
Over half of participants (62.6%; n=97) indicated that patients rarely or never ask about LCS. When asked how frequently they discuss LCS with their screening-eligible patients, 38.1% (n=59) reported most or all of the time, 29.7% (n=46) reported occasionally, and 32.3% (n=50) reported rarely or never.
Phase II (Qualitative) Results
As we explored the primary areas of inquiry more robustly, nine themes arose across (1) knowledge, attitudes, and beliefs, (2) barriers to lung screening discussions, and (3) practice behaviors among TTSs. Themes are discussed below organized by the three areas. Table 2 details focus group participant sociodemographic characteristics.
Table 2.
Focus Group Participant Sociodemographic Characteristics
| Variable | Group | n (%) |
|---|---|---|
| Gender | Female | 8 (66.7%) |
| Male | 4 (33.3%) | |
| Hispanic ethnicity | No | 11 (91.7%) |
| Race | White | 9 (75.0%) |
| Black | 2 (16.7%) | |
| Native Hawaiian or Alaskan Native | 1 (8.3%) | |
| Education Level | Undergraduate Degree | 1 (8.3%) |
| Master’s Degree | 9 (75.0%) | |
| Doctoral Degree | 2 (16.7%) | |
| Geographic Area of Practice | Rural | 4 (33.3%) |
| Suburban | 4 (33.3%) | |
| Urban | 4 (33.3%) | |
| Type of Practice Setting | Hospital | 4 (33.3%) |
| Cancer Center | 2 (16.7%) | |
| University or Academic Setting | 4 (33.3%) | |
| Community Center | 2 (16.7%) | |
| Profession | Tobacco Treatment Specialist | 6 (50.0%) |
| Social Worker | 3 (15.8%) | |
| Nurse Practitioner | 1 (5.3%) | |
| Pharmacist | 1 (5.3%) | |
| Addictions Counselor | 1 (5.3%) | |
| Variable | Mean (SD) | Range |
| Age (n=14) | 51.5 (12.8) | 25 – 70 |
| Years in Practice (n=146) | 7.9 (7.6) | 0.5 – 31 |
Knowledge, Attitudes, and Beliefs
When asked about knowledge, attitudes, and beliefs related to LCS, two primary themes were identified among TTSs: (a) lack of knowledge; and (b) belief in a teachable moment. TTS participants discussed lack of knowledge with statements such as “my awareness of lung screening is quite limited…I realize there’s alot I don’t know (Group 2, Participant 3)” and “I just don’t feel I have detailed knowledge of what is involved and all the different steps and what they do [to] have a meaningful discussion (Group 1, Participant 4)”.
Barriers to Lung Screening Discussions
Five themes arose when asked about barriers to discussing LCS with patients including: (a) patient fear, worry and fatalism; (b) worried about scaring the patient; (c) knowledge barriers; (d) worry about scope of practice; and (e) lack of resources.
Patient Fear, Worry and Fatalism
Patient fear, worry and fatalism were identified as barriers to engaging in discussions with comments like, “It is what it is…God’s providence. There’s not much to be done. So, some people would rather not know…it’s a death sentence. Typically, most people think of it that way (Group 1, Participant 1)” and “there are patients that should get screened that just won’t because I think they’re worried about that result (Group 3, Participant 4)”.
Worried About Scaring the Patient
Some worried about scaring the patient noting, “I don’t want to scare them….I don’t know how the providers will be with me and say, well, you have to stop…letting these people know, or referring them to get lung screening, because you’re scaring them (Group 2, Participant 4)”.
Knowledge Barriers
Knowledge barriers highlighted issues such as feeling like the patient’s doctor might not know about LCS eligibility criteria as well as the complexity of navigating the healthcare system and not knowing how to navigate their patients to screening. Illustrative comments included, “I don’t think every physician knows the guidelines or knows how to have these conversations about the risks and benefits (Group 3, Participant 4)”, and “I still feel like the challenge is it has to come from that person’s doctor to get the order in and get it set up and covered by insurance (Group 1, Participant 5)”, and “it’s such a challenge for TTSs because we can only do so much to get the provider to act (Group 2, Participant 3)”.
Worry About Scope of Practice
Many TTSs described worry about scope of practice and the uncertainty of LCS discussions being within their scope of practice noting this “really should be a conversation for the primary care provider (Group 2, Participant 2)”. However, many went on to say they believe increasing awareness about LCS among eligible individuals is important, thought the tobacco treatment setting was appropriate for the topic, but expressed frustration with the lack of high-quality, customizable educational tools to support this type of patient conversation.
Lack of Resources
Lack of resources as a barrier was captured in comments such as “I don’t really have a paper pamphlet or fact sheet, but I should probably make a slide. Maybe I should make a slide that speaks to this [lung screening] because I think I can do a better job (Group 2, Participant 1)”. Another TTS said, “I remember looking about six months ago and could not find just a one-page general fact sheet. I need something maybe from the national level that’s very basic and I have never seen this (Group 1, Participant 2)”. Another explained that she created her own to address the lack of a formal teaching tool, “I just created a flowchart and have it in front of me and we do it together. I bring a highlighter. And so, we do it together and it’s okay if we only get one tick and we’re like, oh, this doesn’t apply to you and then we move on to something different. But it’s just a way to kind of go through and let people see how we’re getting to that – that plan of saying, oh, it looks like you are eligible to…get that lung low-dose CT (Group 3, Participant 4)” but noted formal resources would be welcomed. Finally, another TTS noted he thinks “it needs to be built into our workflow (Group 2, Participant 3)” so there is consistency with assessing all patients for eligibility criteria and providing high-quality LCS education to those who qualify. It is difficult if the process is not built into the workflow as illustrated by a TTS in a midwestern hospital-based tobacco treatment program, “there are issues with tobacco use that almost subsume talking about lung screening. I mean, I think that applies to me because I’m always completely absorbed in the issue at hand and I don’t have a little flag built in to say hey, remember to mention this person’s eligible for lung cancer screening (Group 1, Participant 2)”.
Practice Behaviors
Two primary themes were identified when we explored practice behaviors among TTSs about LCS: (a) opportunity to advocate for screening; and (b) never asked and never had a patient ask. Several participants spoke about tobacco treatment encounters with patients being an opportunity to advocate for the patient’s health through screening with comments such as “we have been able to identify people and get them into early treatment and we’d like to think that’s the reason why they’re still here (Group 3, Participant 1)” and “on the probability that (with screening) they could get some reassurance that they haven’t already, that it’s not too late, is kind of how that’s come in to my practice (Group 1, Participant 5)”. In addition, many stated, “I’ve never had a patient ask me about it (Group 2, Participant 2)” and “I have never asked a patient about it (Group 3, Participant 2)” as clearly illustrative of practice behaviors that are not currently aligned with LCS awareness and education.
Integration of Quantitative and Qualitative Data
Table 3 presents a data display integrating the quantitative and qualitative findings and associated implications for future interventions and/or training efforts. As we consider the quantitative results in the context of the qualitative results, there is a more robust understanding of TTS knowledge levels, barriers to discussions, and practice behaviors. Results provide a blueprint for future development of educational resources and clinical tools that can support these important conversations as the TTS leverages a potentially teachable moment to encourage patients to pursue deeper discussions with their primary care clinician about lung screening. Resources that offer both an increased understanding about LCS as well as how to engage effectively in this conversation within the context of tobacco treatment are essential. Educational resources should include information on LDCT of the chest, how it is performed, what patients should expect, potential benefits and harms, current USPSTF guidelines, and importance of early detection.
Table 3.
Data Display Integrating Phase I (QUAN) and Phase II (QUAL) Findings
| Variable | Phase I: Summary Statistic | Phase II: Categories | Interpretation | Opportunities for Future Intervention/Training |
|---|---|---|---|---|
| Knowledge | 2.7 (1.4); range 0–7 | Lack of knowledge; Teachable moment for tobacco treatment | Self-awareness of low knowledge regarding lung cancer screening with potential to impact self-efficacy to engage in a shared discussion with a patient about lung cancer screening |
|
| Barriers | 44.2% lack of knowledge 11.0% belief that LCS may expose patient to harms | a) patient fear, worry and fatalism; (b) worried about scaring the patient; (c) complexity of navigating the healthcare system; (d) lack of clinician knowledge about lung cancer screening; (e) cost; and (f) worry about scope of practice | Qualitative results expand understanding of potential barriers |
|
| Practice Behaviors | 62.6% patients rarely or never ask about LCS Highly variable results for TTS discussing LCS with their patients (38.1% most or always discuss; 32.3% rarely or never discuss | (a) opportunity to advocate for screening as important for the patient’s lung health; and (b) never had a patient ask and never asked a patient. | Bidirectional avoidance of topic of lung screening |
|
DISCUSSION AND CONCLUSION
Discussion
Overall, we found that TTSs lacked a good working knowledge about LCS in general as well as current USPSTF guidelines, but think it is important for their patient population and they are also generally open to routinely assessing and adding this educational component into their current workflow supporting the belief that LCS is beneficial for early detection of lung cancer. In fact, knowledge gaps about LCS are not unique to TTSs, but common across other healthcare disciplines. For example, for the subspecialty group most likely to ‘order’ LCS – internal medicine and family physicians – Kota et al. (2022) recently found that knowledge is only moderate about LCS criteria with room for clinical improvement.18 TTSs strongly endorsed the importance of patients both being made aware of the option to screen and encouraging patients to have a discussion with their primary care clinician about LCS. In addition, most respondents did not have concerns about integrating education about LCS into their tobacco treatment practice, and most did not think time was a barrier to discussing LCS in their practice. Therefore, if given the education, skills, incentives, and support to do so, TTSs are likely to incorporate education and discussion about LCS in their tobacco treatment practice.19 This is incredibly helpful as we consider the broader public health initiative of early detection of lung cancer. TTSs are an untapped resource who connect with screening-eligible individuals on a daily basis as part of their practice. However, several knowledge gaps exist and lack of high-quality patient educational tools to support the TTS workflow to engage in this type of conversation take precedence when considering implementing LCS education within the TTS setting. Ultimately, tobacco treatment offers a unique venue to raise awareness about this important topic and is also a setting in which there are experienced specialists trained in tobacco use assessment and treatment as well as motivational interviewing. Therefore, the likelihood of identifying screening-eligible individuals is high in this venue and self-efficacy for discussing tobacco use and treatment is already high. As we consider novel community-based outreach methods to reach screening-eligible patients and increase awareness about LCS, we must also consider how best to support clinicians providing the education with high-quality, accurate information about lung cancer risk, screening, and guidelines. The tobacco treatment context offers a unique opportunity to reach many screening-eligible individuals who are already thinking about their lung health. TTSs are trained in motivational interviewing and are able to empathically communicate with patients using a shared decision-making framework, essential to helping patients who may otherwise experience interactions within a healthcare context that may bring up feelings of shame, blame, guilt, and stigma – and at times, fatalism – about their smoking history and related health consequences. A recent study implementing clinician- and system-based changes helped maximize the reach of both tobacco treatment and LCS, particularly with racial and ethnic minorities.5
Limitations
Our response rate was relatively low, thus limiting our ability to draw conclusions about all TTSs in practice. At the time the survey invitation was sent, ATTUD launched a listserv platform change and some ATTUD members may not have seen the email announcement about the survey opportunity, thus potentially impacting the response rate. However, this response rate was higher than that obtained by Bloom et al. (2018) in a study that surveyed ATTUD members about billing practices.20 That sample includes a combined 131 ATTUD members and members of the Society for Research on Nicotine and Tobacco members.
Conclusion
While leveraging novel settings to increase awareness about LCS, it is essential that training is offered that improves both the readiness and capacity for engaging screening-eligible individuals in a discussion about LCS.9 Given that nearly half of our study participants reported that they did not know enough about LCS to effectively discuss it with their patients, the need for high-quality, accurate information about LCS and how to incorporate it in their practice is needed. Training might be offered as continuing education but could also be added to current accredited TTS training programs as part of the updated core competencies. Ultimately, lung cancer kills more people than breast, colorectal, prostate, and pancreatic cancers combined,21 and early detection of lung cancer through screening has the potential to move the needle toward decreasing lung cancer-related mortality. However, LCS remains essentially an unknown screening modality among eligible individuals. Therefore, we must address this public health challenge at multiple levels to support increasing awareness, delivering high-quality education, and providing patient-centric supportive resources. TTSs respect autonomy and have daily discussions with patients about the pros and cons of various tobacco treatments, for example, providing detailed discussion and psychoeducation about the safety, potential adverse effects, and efficacy of FDA-approved quitting medications, and help patients come to their own decision to use or not use in their quitting efforts. Similarly, TTSs are well-qualified to have discussions of the risks and benefits of LCS and given their scope of work are unlikely to simply provide some LCS education and refer without further discussion.
Practice Implications
As public health efforts advance to increase LCS awareness in appropriate, high-risk individuals, TTSs represent a novel, yet untapped workforce with a significant reach into the cigarette smoking population who have the foundational skills to engage screening-eligible individuals in discussions about LCS. Acquiring the specific skills to identify eligible individuals and engage them in meaningful discussion might also provide a unique opportunity for the TTSs to forge collaborations with LCS programs and facilities. Results of this study provide insight into the unmet training needs of TTSs to facilitate the integration of tobacco treatment and LCS9,19 and provide a foundation for more in-depth research and discussion of the feasibility of adding TTSs to the workforce designated to discuss LCS and connect individuals who are eligible for LCS services. Future research might pilot test implementation of systematic evaluation for LCS in TTS practice as well as examine systems-level and policy-level changes that might facilitate the incorporation of decision-making about LCS in TTS practice.
Ethics Approval and Consent to Participate
This submission is the authors’ own original work, which has not been previously published elsewhere. This paper is not currently being considered for publication elsewhere. The paper reflects the authors’ own research and analysis in a truthful and complete manner. The paper properly credits the meaningful contributions of co-authors and co-researchers. The results are appropriately placed in the context of prior and existing research. All sources used are properly disclosed. All authors have been personally and actively involved in substantial work leading to the paper and will take public responsibility for its content. In addition, this study was reviewed and approved by the Institutional Review Board of Memorial Sloan Kettering Cancer Center prior to any research activities commencing.
Highlights.
Tobacco Treatment Specialists think lung cancer screening is important for their patient population and are open to adding this educational component to their workflow.
Results highlight the unmet training needs required to facilitate integration of tobacco treatment and lung screening among Tobacco Treatment Specialists in the U.S.
Tobacco treatment offers a unique opportunity to reach screening-eligible individuals.
Acknowledgements
We would like to extend our sincere appreciation to Dr. Maher Karam-Hage, Past President of the Association for the Treatment of Tobacco Use and Dependence (ATTUD), for his support of this study and recruitment efforts of the ATTUD membership. We would also like to thank Ms. Katie Lynch and Mr. Nicholas Emard at Memorial Sloan Kettering Cancer Center for assisting with moderation of the focus groups.
Funding
This work was supported in part by funding from the National Cancer Institute (P30CA008748). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Competing Interest
There are no financial or non-financial competing interests for any of the authors.
Availability of Data and Materials
The quantitative datasets generated and analyzed during the current study are available from the corresponding author on reasonable request. The qualitative transcripts are not available secondary to concerns for participant privacy.
References
- 1.Fedewa SA, Kazerooni EA, Studts JL, Smith R, Bandi P, Sauer AG, et al. State Variation in Low-Dose CT Scanning for Lung Cancer Screening in the United States. J Natl Cancer Inst. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landy R, Young CD, Skarzynski M, Cheung LC, Berg CD, Rivera MP, et al. Using Prediction-Models to Reduce Persistent Racial/Ethnic Disparities in Draft 2020 USPSTF Lung-Cancer Screening Guidelines. J Natl Cancer Inst. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jemal A, Fedewa SA. Lung Cancer Screening With Low-Dose Computed Tomography in the United States-2010 to 2015. JAMA Oncol. 2017;3:1278–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United States Preventive Services Task Force. Final recommendation statement: Lung cancer screening. http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/lung-cancer-screening. Accessed May 28, 2023.
- 5.Presant CA, Salgia R, Kulkarni P, Tiep BL, Sanani S, Leach B, Ashing K, Sandoval J, Sedrak MS, Landau S, Yeung S, Raz D, Subbiah S. Implementing Lung Cancer Screening and Prevention in Academic Centers, Affiliated Network Offices and Collaborating Care Sites. J Clin Med. 2020;9:1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duong DK, Shariff-Marco S, Cheng I, Naemi H, Moy LM, Haile R, Singh B, Leung A, Hsing A, Nair VS. Patient and primary care provider attitudes and adherence towards lung cancer screening at an academic medical center. Prev Med Rep. 2017;6:17–22. doi: 10.1016/j.pmedr.2017.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park ER, Neil JM, Noonan E, Howard SE, Gonzalez I, Marotta C, et al. Leveraging the Clinical Timepoints in Lung Cancer Screening to Engage Individuals in Tobacco Treatment. JNCI Cancer Spectr. 2022. Nov 1;6(6):pkac073. doi: 10.1093/jncics/pkac073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galiatsatos P, Schreiber R, Green K, Shah R, Lee H, Feller-Kopman D, et al. Improving lung cancer screening: An equitable strategy through a tobacco treatment clinic. Prev Med Rep. 2021. Sep 17;24:101558. doi: 10.1016/j.pmedr.2021.101558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fucito LM, Czabafy S, Hendricks PS, Kotsen C, Richardson D, Toll BA; Association for the Treatment of Tobacco Use and Dependence/Society for Research on Nicotine and Tobacco Synergy Committee. Pairing smoking-cessation services with lung cancer screening: A clinical guideline from the Association for the Treatment of Tobacco Use and Dependence and the Society for Research on Nicotine and Tobacco. Cancer. 2016. Apr 15;122(8):1150–9. doi: 10.1002/cncr.29926. Epub 2016 Feb 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shelley D, Wang VH, Taylor K, Williams R, Toll B, Rojewski A, et al. Accelerating integration of tobacco use treatment in the context of lung cancer screening: Relevance and application of implementation science to achieving policy and practice. Transl Behav Med. 2022. Nov 21;12(11):1076–1083. doi: 10.1093/tbm/ibac076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heffner JL, Coggeshall S, Wheat CL, Krebs P, Feemster LC, Klein DE, et al. Receipt of Tobacco Treatment and One-Year Smoking Cessation Rates Following Lung Cancer Screening in the Veterans Health Administration. J Gen Intern Med. 2022. May;37(7):1704–1712. doi: 10.1007/s11606-021-07011-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheffer CE, Al-Zalabani A, Aubrey A, et al. The Emerging Global Tobacco Treatment Workforce: Characteristics of Tobacco Treatment Specialists Trained in Council-Accredited Training Programs from 2017 to 2019. Int J Environ Res Public Health. 2021;18(5):2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Creswell JW, Plano Clark VL, Gutman ML, Hanson WE. Advanced mixed methods design. Thousand Oaks, CA: SAGE Publications; 2003. [Google Scholar]
- 14.Creswell JW, Klassen AC, Plano Clark VL, Smith KC. Best practices for mixed methods research in the health sciences. Washington, DC: Office of Behavioral and Social Sciences Research; 2011. [Google Scholar]
- 15.Mukthinuthalapati VVPK, Putta A, Farooq MZ, Singh SRK, Gupta S, Smith S. Knowledge, Attitudes, and Practices Pertaining to Lung Cancer Screening Among Primary Care Physicians in a Public Urban Health Network. Clin Lung Cancer. 2020;21:450–4. [DOI] [PubMed] [Google Scholar]
- 16.Krueger R Focus Groups: A Practical Guide for Applied Research. Thousand Oaks, CA: Sage Publications, 1988. [Google Scholar]
- 17.Neuendorf KA. The Content Analysis Guidebook. Thousand Oaks, CA: Sage Publications, 2002. [Google Scholar]
- 18.Kota KJ, Ji S, Bover-Manderski MT, et al. Lung cancer screening knowledge and perceived barriers among physicians in the United States. JTO Clin Res Rep. 2022;3:100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roughgarden KL, Toll BA, Tanner NT, Frazier CC, Silvestri GA, Rojewski AM. Tobacco Treatment Specialist Training for Lung Cancer Screening Providers. Am J Prev Med. 2021;61:765–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bloom EL, Burke MV, Kotsen C, et al. Billing practices among US tobacco use treatment providers. J Addict Med. 2018;12:381–386. [DOI] [PubMed] [Google Scholar]
- 21.American Cancer Society. Cancer Facts & Figures 2022. In. American Cancer Society. Atlanta: 2022. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The quantitative datasets generated and analyzed during the current study are available from the corresponding author on reasonable request. The qualitative transcripts are not available secondary to concerns for participant privacy.


