Abstract
Purpose:
American Heart Association recently published a set of seven cardiovascular (CV) health metrics for adults and children, emphasizing importance of preventing CV risk factors. Although CV disease risk factors have generally improved in adults, there is concern that this has not been true among adolescents. The present study examined trends and disparities of CV health metrics among U.S. adolescents.
Methods:
We used data from a series of National Health and Nutrition Examination Survey (1988–1994, 1999–2004, and 2005–2010) including 11,233 adolescents aged 12–17 years. We estimated prevalence and mean score of CV health metrics and examined the disparities in mean score by sex, race/ethnicity, educational attainment, and poverty-income ratio.
Results:
The prevalence of nonsmoking and healthy diet increased from 1988 through 2010, while the prevalence of normal body mass index and physical activity decreased, resulting in an unchanged distribution of overall CV health scores since 1988. The prevalence of adolescents meeting all seven CV health metrics was low, 3.5% (95% confidence interval [CI] 2.2–5.4), 4.0% (95% CI 3.3–4.8), and 4.0% (95% CI 2.9–5.3) in National Health and Nutrition Examination Survey 1988–1994, 1999–2004, and 2005–2010, respectively. The disparities in adjusted mean scores persisted between non-Hispanic whites and non-Hispanic blacks, families/households with >12 versus <12 years of education, and poverty-income ratio of >3 versus <3 (p < .05).
Conclusions:
The proportion of adolescents achieving all seven CV health metrics was low and remained unchanged during 1988–2010. The disparities in mean CV health score persisted among adolescents.
Keywords: Adolescents, Cardiovascular health, Trends of risk factors, Prevention, Health disparities
Cardiovascular disease (CVD) is the leading cause of death in the United States and accounts for estimated annual direct and overall costs of $192.1 billion and $312.6 billion, respectively [1]. CVD risk factors in youth—smoking, obesity, elevated blood pressure, undesirable lipid profiles, and metabolic syndrome—have been associated with accelerated atherosclerosis in youth [2] and often continue into adulthood [3–5]. The American Academy of Pediatrics recently updated its guidelines for CV health and risk reduction in children and adolescents and emphasized the importance of early, or primordial, prevention of CVD risk factors through various strategies, including promoting a healthy diet, greater participation in physical activity, and effective management of risk factors in children and adolescents [5]. In 2010, the American Heart Association (AHA) published recommendations aimed at improving CV health in United States by encouraging seven ideal CV health behaviors or factors (i.e., not smoking; being physically active; having normal weight, blood pressure, blood glucose, and total cholesterol levels; and eating a healthy diet) [6]. Several studies have examined the prevalence and trends in CV health metrics in adolescents and adult population [7–9], but recent information on trends in CV health metrics in adolescents is lacking. For the present study, we examined trends and disparities of CV health metrics among adolescents aged 12–17 years who participated in the National Health and Nutrition Examination Surveys (NHANESs) from 1988 through 2010.
Methods
National Health and Nutritional Examination Survey
NHANES consists of nationally representative sample surveys of the civilian, noninstitutionalized U.S. population. Data for NHANES were collected via household interviews and physical examinations. Detailed information is available elsewhere [10]. Before 1999, NHANESs were conducted on a periodic basis, but, beginning that year, the survey became continuous surveys. For the present study, we selected adolescents aged 12–17 years from NHANES 1988–1994, 1999–2004, and 2005–2010. Our analyses included 2,447 (1988–1994), 5,242 (1999–2004), and 3,544 (2005–2010) adolescents who were surveyed in Mobile Examination Centers (MECs), and for whom information was available on CV health metrics. In calculating CV health scores, we included all adolescents with complete information on all seven metrics (1,583 [1988–1994], 4,402 [1999–2004], and 2,892 [2005–2010], respectively). Figure 1 showed the flowchart of missing pattern for each CV health metric and selection of adolescents in the analysis. Adolescents who were excluded because of missing covariates for all seven metrics score analysis were in general similar to those included in the study in terms of age, sex, race/ethnicity, education, and poverty-income ratio (PIR; Supplementary Table 1). However, in NHANES III, a lower percentage of non-Hispanic white and adolescents with household head >12 years education was excluded, and in NHANES 2005–2010, a higher percentage of non-Hispanic black and a lower percentage of Mexican American were excluded from the study (p < .05).
Figure 1.
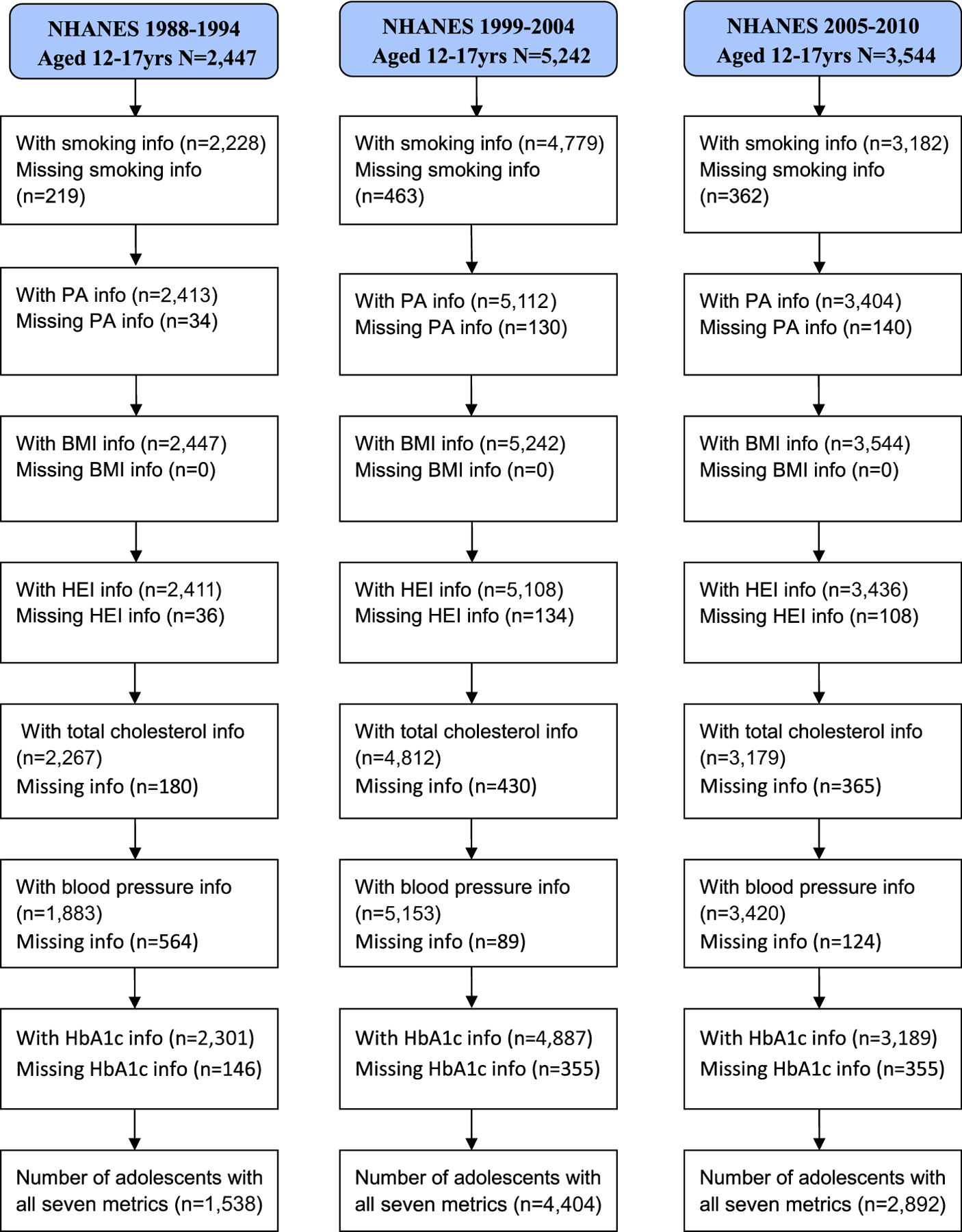
Flowchart describing missing pattern of CV health metrics and selection of adolescents aged 12–17 years in NHANES 1988–1994, 1999–2004, and 2005–2010.
Definitions of cardiovascular health metrics
We used the modified AHA definitions of ideal, intermediate, and poor CV metrics because of changes in the questionnaires across NHANESs or lack of information for some metrics. Supplementary Table 2 provided the detailed information and explanation of the CV health metrics used in the present study.
Smoking status.
For adolescents aged ≥12 years, the questionnaires about smoking status changed substantially across the NHANESs; therefore, we used the gender- and race/ethnicity-specific cutoff points of cotinine concentrations to classify adolescents as noncurrent smokers versus nonsmokers [11]. For male adolescents, the cutoff points of cotinine concentrations were 8.78, 6.01, and 1.18 for non-Hispanic white, non-Hispanic black, and Mexican American, respectively. The corresponding cutoffs for female adolescents were 2.95, 2.81, and .66, respectively. The overall sensitivity of using cotinine to classify smoking status was 86.5% and specificity 93.1%.
Physical activity.
Physical activity questionnaires varied in collection of participation, frequency, and duration of physical activity across NHANES cycles. Questionnaires to assess the AHA recommended physical activity levels were not available; thus, physical activity was assessed at its most basic level: those reporting no activity (i.e., inactive) versus those reporting some activity over the assessed period. In NHANES 1988–1994, those with <1 time per week were categorized as inactive. In NHANES 1999–2006 and 2007–2010, the recall period varied, but information on participation, intensity, frequency, and duration of physical activity was available. Those reporting no physical activity or physical activity below minimum thresholds (<10 minutes in a typical week; <40 minutes in past 30 days) were categorized as inactive. We conducted additional sensitivity analyses across NHANES cycles, both with consistent physical activity assessment (1999–2004 and 2005–2006) and with physical activity removed from CV health metrics categories. The results are listed in Supplementary Table 3.
Body mass index.
Body mass index (BMI) was calculated as weight (kg)/height (m2). To account for variability by age and sex, we compared BMI in adolescents with age- and sex-specific reference values from the 2000 Centers for Disease Control and Prevention (CDC) growth charts [12]. BMI for age of ≥85th to <95th percentiles was defined as overweight, and ≥95% percentile as obese, and <85th percentile as ideal BMI.
Healthy diet score.
The AHA healthy diet score includes the following five components: consumption of fruits and vegetables (≥4.5 cups/day), fish (≥2 3.5-oz servings/week), fiber-rich whole grains (≥3 1-oz equivalent servings/day), sodium (<1,500 mg/d), and sugar-sweetened beverages (<36-oz/week). The NHANES Food Frequency Questionnaire, used to estimate the recommended healthy diet score, was not administered in NHANES 2007–2008 and 2009–2010. Therefore, we used the Healthy Eating Index-2010 (HEI-2010) that was designed to assess multiple aspects of diet quality as described by key recommendations of the 2010 Dietary Guidelines for Americans [13]. The HEI-2010 has 12 components representing all major food groups, including fruits, vegetables, grains, milk, meat and beans, oils, saturated fat, sodium, and calories from solid fats, alcoholic beverages, and added sugars. Food components are given maximum and minimum points per 1,000 calories, and the total score ranges from 0 to 100, a higher score indicating a more healthy diet. A detailed description of the HEI-2010 has been published previously [14]. We merged the NHANES 1988–1994 and 1999–2002 individual food files with the MyPyramid Equivalents Database (MPED) version 1 and NHANES 2003–2004 and 2005–2010 files with MPED version 2 to calculate HEI-2010 [15,16]. Of 5,440 unique United States Department of Agriculture (USDA) food codes in NHANES 2005–2010, 5,030 were also in MPED version 2. We matched the remaining 410 foods to the most similar foods. For example, the food code 21501350 (ground beef, 90%–94% lean, cooked) was matched to the nearest food code 21501300 (ground beef, 80%–84% lean, cooked). Dietary information was obtained from in-person 24-hour dietary recalls, and nutrient intake was estimated using the corresponding Food and Nutrient Databases for Dietary Studies from the USDA [17]. Twenty-four–hour dietary recalls are considered among the most precise methods of assessing diet and nutrients intake [18]. To examine the changes in HEI-2010 scores over time, we pooled all NHANES data together and estimated the top 10% of scores as having a healthy diet (cutoff point = 57.0 of possible 100) <top 10% and >50% (<57.0 but >39.3) as intermediate and ≤50% (<39.3) as poor diet [19]. We estimate the proportion of adolescents who were at different cutoff points in 1988–1994, 1999–2004, and 2005–2010.
Total cholesterol.
Total cholesterol levels were based on samples taken regardless of fasting state. There were changes in methods, laboratories, and analyzers used to measure lipids from serum across surveys [20]. Despite such changes, the laboratory methods were essentially the same, and all laboratories participated in the CDC-National Heart, Lung, and Blood Institute Lipid Standardization Program. Detailed descriptions about blood collection and processing are provided in the NHANES laboratory/medical technologists procedures manual [21].
Adolescents were classified as having ideal, intermediate, or poor total cholesterol if their levels were <170, ≥170–<200, or ≥200 mg/dL, respectively [6].
Blood pressure.
Up to three blood pressure measurements were taken, using the proper cuff size, during visits to Mobile Examination Center after participants had rested quietly in a sitting position for at least 5 minutes. In 1988–1994, 1999–2004, and 2005–2010, 78%, 76%, and 79% of adolescents, respectively, had three blood pressure measurements. We classified adolescents as having ideal (normal), intermediate (prehypertension), or elevated blood pressure (hypertension) based on the age-, gender-, and height-specific blood pressure percentiles using the 2000 CDC growth charts [22]. Ideal (normal) was defined as systolic blood pressure (SBP) and diastolic blood pressure (DBP) <90th percentile for age, sex, and height, intermediate (prehypertension) as SBP or DBP ≥90th but <95th percentile or observed BP levels ≥120/80 mmHg. Elevated blood pressure (hypertension) was defined as SBP and/or DBP ≥95th percentile.
HbA1c.
HbA1c, a measure of average glucose concentration, was determined for all participants ≥12 years of age, regardless of fasting status, was used to classify glucose levels as desirable or undesirable (fasting glucose was not available for adolescents in NHANES 1988–1994). An HbA1c level of <5.7% and the absence of diabetes (self-reported or on diabetes medications) was desirable; an HbA1c level of ≥5.7% was undesirable [23].
Baseline covariates.
Demographic and descriptive information was self-reported by the participant or by proxy. Age, sex, race/ethnicity, and education attainment of head of household were obtained from the interview questionnaire. Race/ethnicity was classified as non-Hispanic white, non-Hispanic black, Mexican American, or other. Total annual family income, a socioeconomic status proxy, was used to calculate the PIR. PIR was derived by dividing the total annual family income by the established federal poverty level for the specific family size, accounting for the year and the state where the assessment took place [24]. We defined PIR <1.0 as poor, 1.0–<2.0 as near poor, 2.0–<3.0 as middle income, and ≥3.0 as high income.
Cardiovascular health score
Using the criteria for each CV health metric described above, we constructed a total CV health score, ranging from 0 to 7. The CV health score included never smoking (=1), some physical activity (=1), BMI <85% (=1), HEI-2010 ≥top 10% (score ≥ 57.0 = 1), total cholesterol <170 mg/dL (=1), blood pressure <90% (=1), and HbA1c <5.7% (=1). In calculating the total CV health score, we included all adolescents who had completed information on all seven metrics.
Statistical analysis
We estimated the weighted percentages of the selected covariates for NHANES 1988–1994, 1999–2004, and 2005–2010. We calculated the sex- and race-standardized prevalence and 95% confidence interval (CI) of the CV health metrics and the overall CV health score. We used logistic regression to test for linear trends in changes in CV health metrics. In the logistic regression models, each CV health metric or score was the dependent variable, the independent variables included a time variable corresponding to the midpoint of each surveys (1991 for 1988–1994, 2001 for 1999–2004, and 2007 for 2005–2010), and age, sex, and race/ethnicity. The time variable was used to assess the change of each CV health metric or score overtime. For disparities analysis, we used the logistic regression models to estimate the adjusted mean CV health scores and to test for differences in mean scores by the selected characteristics. Because of the limited number of participants in the categories at either end of the range, we combined the lower numbers (0–2) and the upper numbers (6–7) of achieved metrics to stabilize our estimates.
Data were analyzed using SAS version 9.3 and SUDAAN version 10 to account for the complex sampling design [25]. All tests were two sided, and a p value of <.05 was considered statistically significant.
Results
Demographic characteristics of the sample are listed in Table 1. The proportions of non-Hispanic white and non-Hispanic black adolescents decreased, while the proportion of adolescents of Mexican American and other races/ethnicities increased during 1988–2010. The percentage of adolescents living in higher PIR households or where the household heads reported >12 years of education also increased.
Table 1.
Characteristics of adolescents aged 12–17 years—NHANES 1988–1994, 1999–2004, and 2005–2010
| Characteristics | N | NHANES 1988–1994 % (95% CI) |
N | NHANES 1999–2004 % (95% CI) |
N | NHANES 2005–2010 % (95% CI) |
p Value for trenda |
|---|---|---|---|---|---|---|---|
| Sex | |||||||
| Male | 1,155 | 52.0 (48.3–55.7) | 2,647 | 50.9 (49.1–52.7) | 1,824 | 51.2 (49–53.4) | .814 |
| Female | 1,292 | 48.0 (44.3–51.7) | 2,595 | 49.1 (47.3–50.9) | 1,720 | 48.8 (46.6–51) | .814 |
| Race/ethnicity | |||||||
| Non-Hispanic white | 624 | 65.6 (60.9–70.0) | 1,331 | 61.1 (56.9–65.2) | 1,045 | 60.9 (56.6–65.1) | .058 |
| Non-Hispanic black | 870 | 15.9 (13.3–18.9) | 1,673 | 14.9 (12.3–17.8) | 1,000 | 14.4 (12.3–16.8) | .539 |
| Mexican American | 826 | 8.7 (6.9–10.9) | 1,819 | 10.9 (8.6–13.7) | 1,028 | 12.3 (10.0–14.9) | .017 |
| Other | 127 | 9.7 (7.0–13.5) | 419 | 13.1 (10.4–16.3) | 471 | 12.4 (10.1–15.2) | .122 |
| Education attainment of household head | |||||||
| <12 years | 1,025 | 25.7 (22.5–29.2) | 1,951 | 22.6 (20.3–25.2) | 1,069 | 19.4 (17.3–21.7) | <.001 |
| 12 years | 778 | 34.6 (31.1–38.2) | 1,234 | 26.7 (24.7–28.8) | 761 | 22.4 (20.1–24.9) | <.001 |
| >12 year | 638 | 39.7 (35.8–43.8) | 1,858 | 50.6 (47.8–53.5) | 1,569 | 58.2 (54.7–61.7) | <.001 |
| PIR | |||||||
| <1 (poor) | 830 | 22.2 (19.0–25.8) | 1,514 | 21.0 (19.2–22.8) | 933 | 18.7 (16.7–21.0) | .043 |
| ≥1–<2 (near poor) | 623 | 25.0 (21.5–28.8) | 1,290 | 22.6 (20.7–24.7) | 866 | 20.8 (18.7–23.1) | .096 |
| ≥2–<3 (middle income) | 403 | 24.0 (20.1–28.4) | 723 | 16.4 (14.6–18.3) | 538 | 17.2 (15.1–19.5) | .003 |
| ≥3 (high income) | 370 | 28.8 (24.0–34.1) | 1,297 | 40.1 (37.0–43.2) | 964 | 43.3 (39.2–47.4) | <.001 |
95% CI = 95% confidence interval; NHANES = National Health and Nutritional Examination Survey; PIR = poverty income ratio.
p Value for trends across the surveys using logistic regression model adjusted for age, sex, and race/ethnicity; all tests two tailed.
The prevalence of current smoking declined from 17.2% (95% CI 14.9–19.9) during 1988–1994 to 11.4% (95% CI 10.0–12.8) during 2005–2010, and the prevalence of those with a high HEI-2010 score (≥57.0) increased significantly over time (p < .05 for trend). There was suggestive evidence of an increased prevalence of ideal total cholesterol (<170 mg/dL; p = .061). The prevalence of obesity increased from 11.2% (95% CI 9.2–13.6) to 18.5% (95% CI 16.6–20.5). Physical inactivity, assessed differently across cycles, appeared to increase over the assessment period (Table 2). Within consistent assessment periods (1999–2006), physical inactivity appeared to be declined from 1999–2004 to 2005–2006 (Supplementary Table 3). In additional analysis removing physical activity from the CV health composite score, similar trends and distribution across the number of CV health metrics were noted (Supplementary Table 3). About 4% of adolescents achieved all seven CV health metrics, however, and the distribution of the number of ideal CV health metrics remained largely unchanged since the 1988–1994 NHANES.
Table 2.
Sex- and race-standardized prevalence of CV health metrics in adolescents aged 12–17 years—NHANES, 1988–1994, 1999–2004, and 2005–2010
| CV health metricsa | N | NHANES 1988–1994 % (95% CI) |
N | NHANES 1999–2004 % (95% CI) |
N | NHANES 2005–2010 % (95% CI) |
p Value for trendb |
|---|---|---|---|---|---|---|---|
| Smoking statusc | |||||||
| Noncurrent smoker | 1,877 | 82.8 (80.1–85.1) | 4,179 | 86.1 (84.1–88.0) | 2,827 | 88.7 (87.2–90.0) | <.001 |
| Current smoker | 351 | 17.2 (14.9–19.9) | 600 | 13.9 (12.1–15.9) | 355 | 11.4 (10.0–12.8) | <.001 |
| Physical activityd | |||||||
| Some activity | 2,123 | 90.4 (88.5–92) | 4,401 | 88.5 (87.3–89.6) | 2,904 | 86.6 (84.9–88.1) | .003 |
| Inactive | 290 | 9.6 (8.0–11.5) | 711 | 11.5 (10.4–12.7) | 500 | 13.4 (11.9–15.1) | .003 |
| BMIe | |||||||
| <85th percentile | 1,704 | 72.4 (69.0–75.5) | 3,314 | 67.3 (64.7–69.8) | 2,179 | 65.6 (63.6–67.6) | <.001 |
| 85th–95th percentile | 396 | 16.4 (14.2–18.9) | 882 | 15.9 (14.2–17.7) | 585 | 15.9 (14.6–17.3) | .680 |
| >95th percentile | 347 | 11.2 (9.2–13.6) | 1,046 | 16.8 (15.3–18.6) | 780 | 18.5 (16.6–20.5) | <.001 |
| HEIf | |||||||
| ≥Top 10th percentile (≥57.0) | 225 | 8.4 (6.9–10.2) | 454 | 10.0 (8.6–11.7) | 370 | 11.3 (9.4–13.6) | .030 |
| <Top 10th and >50th percentile (<57.0 but >39.3) | 999 | 40.3 (37.4–43.3) | 2,033 | 38.2 (36.3–40.2) | 1,459 | 41.5 (38.7–44.4) | .748 |
| ≤50th percentile (<39.3) | 1,187 | 51.3 (47.9–54.7) | 2,621 | 51.7 (49.1–54.3) | 1,607 | 47.2 (43.5–50.9) | .146 |
| Total serum cholesterol (mg/dL) | |||||||
| <170 mg/dL | 1,407 | 66.5 (63.2–69.7) | 3,148 | 65.2 (63.1–67.1) | 2,228 | 70.9 (68.5–73.1) | .061 |
| 170–199 mg/dL | 600 | 24.1 (21.1–27.4) | 1,193 | 25.5 (23.6–27.5) | 732 | 22.8 (20.9–24.8) | .563 |
| ≥200 mg/dL | 260 | 9.4 (7.6–11.6) | 471 | 9.4 (8.1–10.8) | 219 | 6.4 (5.3–7.7) | .030 |
| Blood pressure (mmHg)g | |||||||
| <90th percentile | 1,573 | 84.9 (82.2–87.2) | 4,288 | 84.3 (82.7–85.8) | 2,888 | 85.3 (83.4–87.0) | .133 |
| 90th–95th percentile or SBP ≥120 or DBP ≥80 mmHg | 248 | 11.8 (9.9–14.1) | 674 | 12.0 (10.8–13.4) | 426 | 11.7 (10.4–13.2) | .121 |
| >95th percentile | 62 | 3.3 (2.2–5.1) | 191 | 3.7 (2.9–4.5) | 106 | 3.0 (2.3–3.9) | .636 |
| HbA1c | |||||||
| <5.7 | 2,159 | 96.4 (95.1–97.4) | 4,721 | 97.3 (96.7–97.8) | 2,973 | 95.2 (94.2–96.0) | .214 |
| ≥5.7 | 142 | 3.6 (2.7–5.0) | 166 | 2.7 (2.2–3.3) | 216 | 4.8 (4.0–5.8) | .214 |
| Number of CV health metricsh | |||||||
| 0–2 | 23 | 1.4 (.7–2.8) | 100 | 1.8 (1.3–2.4) | 48 | 1.3 (.9–1.9) | .358 |
| 3 | 137 | 6.6 (5.1–8.5) | 367 | 7.0 (6–8.2) | 234 | 7.4 (6.2–8.8) | .919 |
| 4 | 345 | 19.9 (16.9–23.2) | 947 | 21.3 (19.6–23.1) | 629 | 19.9 (17.7–22.3) | .613 |
| 5 | 576 | 36.7 (33.1–40.4) | 1,538 | 34.2 (32–36.4) | 998 | 34.3 (31.7–37) | .444 |
| 6 | 462 | 32.0 (28.4–35.8) | 1,305 | 31.7 (29.3–34.3) | 880 | 33.2 (30.6–35.9) | .276 |
| 7 | 40 | 3.5 (2.2–5.4) | 147 | 4.0 (3.3–4.8) | 103 | 4.0 (2.9–5.3) | .551 |
| 6–7 | 502 | 35.5 (31.5–39.7) | 1,452 | 35.7 (33–38.5) | 983 | 37.2 (34.5–39.9) | .219 |
AHA = American Heart Association; BMI = body mass index; CDC = Centers for Disease Control and Prevention; 95% CI = 95% confidence interval; CV = cardiovascular; DBP = diastolic blood pressure; HEI = Healthy Eating Index; NHANES = National Health and Nutritional Examination Survey; SBP = systolic blood pressure.
All adolescents with available CV health metrics were included in trend analyses for each specific metric; therefore, the sample size might vary for each CV health metric.
p Value for trends across the surveys using logistic regression model adjusted for age, sex, and race/ethnicity; all tests two tailed.
We used gender- and race/ethnicity-specific cutoff points of cotinine concentrations to classify adolescents as current smokers versus nonsmokers [1].
During 1988–1994 (NHANES III), adolescents were asked how many times they had any physical activity that made them sweat and breathe hard in the past week. We defined those who had <1 time of physical activity in the past week as inactive. In NHANES 1999–2006, participants were asked if they did any moderate- or vigorous-intensity activities for at least 10 minutes in the last 30 days and, in NHANES 2007–2010, they were asked if they did any moderate- or vigorous-intensity physical activity for at least 10 minutes in a typical week. We defined the participants as inactive if they reported no physical activity, <40 minutes of physical activity in the last 30 days in NHANES 1999–2006, or <10 minutes physical activity in a typical week in NHANES 2007–2010.
BMI is calculated as weight in kilograms divided by height in meters squared. BMI in adolescents is compared with age- and sex-specific reference values from the 2000 CDC growth charts (http://www.cdc.gov/growthcharts/cdc_charts.htm). BMI for age ≥85th–<95th percentile is defined as overweight and BMI for age ≥95% percentile as obese.
HEI-2010 consists of 12 components representing all major food groups found in MyPyramid, including total fruit, total vegetables, total grains, milk, meat and beans, oils, saturated fat, sodium, and calories from solid fats, alcoholic beverages, and added sugars. Each component is given maximum and minimum points per 1,000 calories, and the total score ranges from 0 to 100, a higher score indicating a more healthy diet. Using NHANES data, we estimated a cutoff point of the top 10% of scores as having a healthy diet (63 for adolescents), then used this cutoff to estimate the proportion of children who were at or above the cutoff point during 1988–1994, 1999–2004, and 2005–2010.
We classified adolescents as having ideal (normal), intermediate (prehypertension), or elevated blood pressure (hypertension) based on the age-, sex-, and height-specific blood pressure percentiles, using the reference population of the 2000 CDC growth charts (http://www.cdc.gov/growthcharts/cdc_charts.htm). Ideal blood pressure = SBP and DBP <90th percentile for age-, sex-, and height-specific blood pressure; intermediate blood pressure (prehypertension) = average SBP or DBP ≥90th–95th percentile or observed BP levels ≥120/80 mmHg, even if systolic and diastolic percentiles were <90%. Elevated blood pressure (hypertension) = SBP and/or DBP ≥95th percentile.
To calculate the total CV health score, we included all participants with complete information for all seven CV health metrics. The score was calculated by recoding the seven metrics as dichotomous variables (using one point for the AHA ideal or proxy category vs. zero points for the other categories): score = ([never smoking (1 point)] + [some physical activity (1 point)] + [BMI <85th percentile (1 point)] + [HEI-2010 ≥top 10% (1 point)] + [total cholesterol <170 mg/dL (1 point)] + [blood pressure <90th percentile (1 point)] + [HbA1c <5.7% (1 point)]).
We found no evidence of significant changes in the mean CV health scores over time by sex, race/ethnicity, and PIR; however, the mean score increased marginally from 4.61 in 1988–1994 to 4.81 in 2005–2010 among adolescents whose head of household had <12 years of education (p = .082; Figure 2, Supplementary Table 4). The adjusted mean scores were significantly higher among non-Hispanic whites compared with non-Hispanic blacks (p = .003), among heads of households with >12 years compared with <12 years of education (p < .001), and among those with a PIR ≥ 3 compared with a PIR < 3 (p < .001; Figures 2B–D, Supplementary Table 4).
Figure 2.
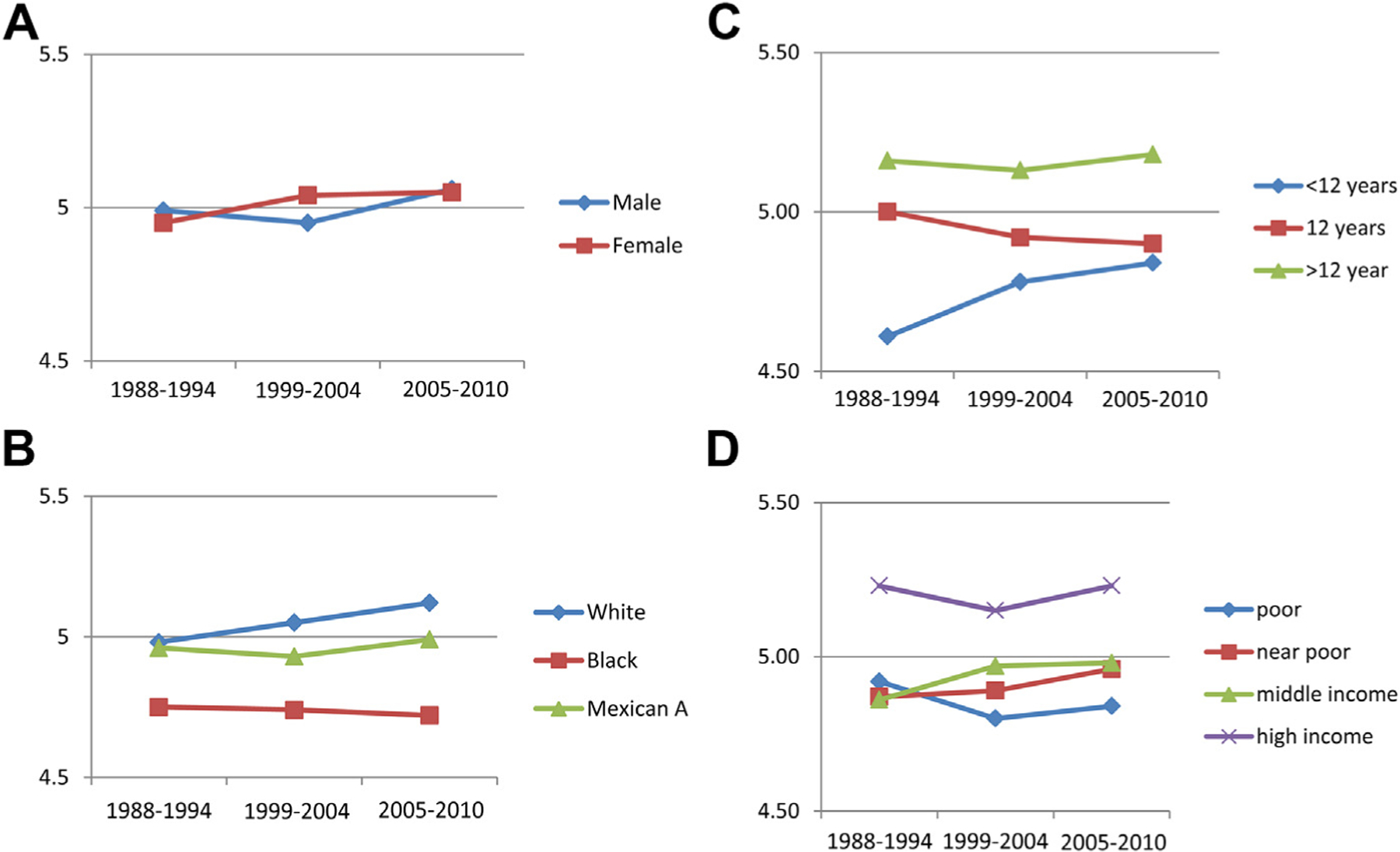
Trends of adjusted mean number of CV health metrics by sex (A), race/ethnicity (B), education of head of household (C), and PIR (D) in adolescents 12–17 years of age—NHANES 1988–1994, 1999–2004, and 2005–2010. The mean score was adjusted for sex and race/ethnicity in panel (A), for age and sex in panel (B), and for age, sex, and race/ethnicity in panels (C) and (D). The adjusted mean scores were significantly higher among non-Hispanic whites compared with non-Hispanic blacks (p = .003), education attainments of households >12 years compared with <12 years (p < .001), and PIR ≥3 (high income) compared with <3 (poor, near poor, or middle income; p < .001; see Supplementary Table 2).
Discussion
Many studies have examined trends of specific CVD risk factors, such as weight classification, lipid profile, smoking status, physical activity, fruit and vegetable consumption, and blood pressure among children, and adolescents [20,26–29]. Others have examined the joint distribution of multiple CVD risk factors or metabolic syndrome [30–32], but none has examined trends and disparities of individual CV health metrics among U.S. adolescents. Using a series of nationally representative samples of adolescents, the findings in our study indicate that the prevalence of nonsmoking and of choosing a healthy diet (HEI-2010 score ≥57.0) improved from 1988 to 2010. However, the prevalence of obesity and physical inactivity increased as well. The effects of increased prevalence of nonsmoking and healthy eating appeared to be offset by the increased prevalence of obesity and physical inactivity, thus leaving the number of adolescents achieving six or seven CV health metrics largely unchanged from 1988 to 2010. The prevalence of meeting seven ideal CV health metrics among adolescents is low, consistent with the findings of a recent study [8], and has remained low since 1988. In addition, the disparities in adjusted mean CV health scores by race/ethnicity, education, and PIR persisted among adolescents during 1988–2010. Compared with the results from the Cardiovascular Risk in Young Finns Study cohort of adolescents aged 12–18 years, the prevalence of the ideal level of nonsmoking and fasting glucose (measured by HbA1c) was similar. The prevalence of the ideal level of BMI and healthy diet was higher, and the prevalence of the ideal level of total cholesterol and physical activity was lower among adolescent Finns compared with our results [33]. The findings of a recent study including five international cohorts of young adults from United States, Finland, and Australia (average age 34 years) suggested that the prevalence of seven ideal CV health metrics was about 1% that was lower than that of our estimate. The lower estimate was mainly attributed to the lower level of ideal diet in the international cohort study. The prevalence of the ideal level of total cholesterol, nonsmoking, and fasting glucose (HbA1c in our study) appeared to be comparable. However, the ideal level of BMI and blood pressure was lower than our estimate, that is, 46% versus 66% for BMI and 52% versus 85% for blood pressure, respectively [34]. Maintaining a healthy diet and increasing physical activity are the main recommendations for reducing childhood obesity in the United States [5]. Although the prevalence of high HEI-2010 scores (≥top 10%) increased over time, the prevalence of physical inactivity appeared to increase as well, which were consistent with the findings of other studies [27]. In the sensitivity analysis of NHANES 1999–2006 data on physical activity, fewer than half of the adolescents engaged in ideal level of physical activity as recommended by the AHA (Supplementary Table 3). There are strong and consistent evidence that healthy eating and regular physical activities play important role in reducing the CVD risk factors and in decreasing the risk of developing CVDs in children and adolescents. Continued efforts should be made at the national, local levels, and schools to promote the healthy eating and physical activities among adolescents, such as outlined by the School Health Guidelines to Promote Healthy Eating and Physical Activity [35].
Although previously observed increases in obesity among children and adolescents appeared to be leveling off since mid-2000s [29], our results suggested that the increased prevalence of obesity among adolescents made the favorable trend in the distribution of CV health metrics over time nonsignificant. Many studies suggested that childhood obesity is associated with metabolic syndrome, high blood pressure, high cholesterol, and type 2 diabetes, and it tracks into adulthood [5,36,37]. Continuing efforts focusing on reducing childhood obesity through healthy eating and regular physical activity play an essential role in primordial prevention of CVDs and improving the overall health in general. The prevalence of adolescents with undesirable total cholesterol (≥200 mg/dL) declined significantly from 1988 to 2010, and these findings are consistent with other studies [20]. This decline might be attributable, in part, to the decline in consumption of trans fats and saturated fats and to an increase in the proportion of those reporting consuming a healthy diet (HEI-2010 index). Detailed analyses of the HEI-2010 index indicated that consumption of total fruits and vegetables has increased significantly, and consumption of saturated fat has decreased significantly since 1988 among adolescents (results not shown). The average HEI-2010 score increased from 39.9 in 1988–1994 to 41.4 in 2005–2010 (p = .017).
Despite many efforts to reduce health disparities, adjusted mean CV health scores were persistently lower among non-Hispanic blacks compared with non-Hispanic whites, among adolescents living with heads of households with lower educational attainment (<12 years) and in households with lower PIRs (<3.0). The existence and persistence of substantial disparities in mortality, morbidity, and risk factors among the entire U.S. population have been well documented [38]. Many national and local government programs, such as CDC’s Racial and Ethnic Approaches to Community Health program, are trying to address and eliminate racial and ethnic disparities in health [39]. However, there is insufficient evidence regarding the effectiveness of any particular intervention in reducing specific disparities among different segments of the population [39]. Our findings provide further evidence of the existence of persistent disparities in CV health metrics among adolescents. Until interventions are proven to be effective, continued efforts should be invested in increasing community awareness of health disparities; setting priorities among disparities to be addressed at the federal, state, tribal, and local levels; and expending resources to reduce and eliminate priority disparities [39].
Our study has major strengths, including the use of data from a series of nationally representative samples of U.S. adolescents, the analysis of trends and disparities in CV health metrics, and the applicability of data to all seven CV health metrics or proxy measures.
Our study also has several limitations: first, physical activity questionnaires were not consistent across NHANES cycles, and the observed trend in increased physical inactivity might have been influenced by changes in assessment method. However, in the sensitivity analysis excluding physical activity, we found that patterns of distribution and trends remained consistent with those using seven metrics (Supplementary Table 3). Second, we calculated the HEI-2010 to approximate the AHA healthy diet score and used the top 10% of scores as the cutoff point for a healthy diet [19], which might have overestimated the ideal healthy diet defined by the AHA [6]. Other studies of young adult or adult populations indicated that the prevalence of eating a healthy diet was very low [9,34]. Third, we used the gender- and race/ethnicity-specific cutoff points of cotinine concentrations to determine the smoking status among adolescents. Although this method has high sensitivity and specificity (>86%) for determining current smoking, it could not classify those of “never tried” from those of “former” smokers [11]. In addition, using cotinine concentrations to determine smoking status might miss intermittent smokers, and some of the “current smokers” might be passive smokers (exposed to second-hand smoking). Fourth, because of limited data on fasting glucose in NHANES, we used a hemoglobin A1c level of <5.7% to approximate the fasting glucose level of <100 mg/dL, the level suggested by the American Diabetes Association [40].
In summary, our findings indicated that the prevalence of meeting seven CV health metrics was low among U.S. adolescents. Declines in current smoking and elevated total cholesterol and an increasing prevalence of higher HEI-2010 scores were offset by an increasing prevalence of obesity, which resulted in limited changes to the overall CV health scores during 1988–2010. Reducing childhood obesity through healthy eating and regular physical activity is essential in primordial prevention of CVDs and improving the overall health in general among adolescents. Finally, disparities in the adjusted mean CV health scores persisted among adolescents over time.
Supplementary Material
IMPLICATIONS AND CONTRIBUTION.
Despite improvements in some cardiovascular health metrics, the prevalence of adolescents who achieve all metrics has remained low since the 1980s. To improve adolescents’ cardiovascular health, public health efforts should focus on promoting healthy dietary habits, increasing physical activity, and identifying cardiovascular health risks early.
Acknowledgments
All authors have read and approved submission of the manuscript. The manuscript has not been published elsewhere in whole or part, and neither is under review for publication elsewhere. There are no prior publications or submissions with any overlapping information, including studies and patients. There is no honorarium, grant, or other form of payment was given to anyone to produce the manuscript. Dr. Yang wrote the first draft and has full access to all the data and takes responsibility for the integrity of the data and the accuracy of the data analysis. He also conceptualized and designed the study, drafted the manuscript, and approved the final manuscript as submitted. Mr. Yuan carried out the initial analyses, reviewed the manuscript, and approved the final manuscript as submitted. Dr. Gregg, Dr. Loustalot, Dr. Fang, Dr. Hong, and Mr. Merritt all critically reviewed and revised the manuscript and approved the final manuscript as submitted.
Footnotes
There is no real or perceived conflict of interest.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Supplementary Data
Supplementary data related to this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jadohealth.2014.03.013
References
- [1].Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2013 update: A report from the American Heart Association. Circulation 2013;127:e6–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Berenson GS, Srinivasan SR, Bao W, et al. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med 1998;338:1650–6. [DOI] [PubMed] [Google Scholar]
- [3].Freedman DS, Khan LK, Dietz WH, et al. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: The Bogalusa Heart Study. Pediatrics 2001;108:712–8. [DOI] [PubMed] [Google Scholar]
- [4].Morrison JA, Friedman LA, Gray-McGuire C. Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: The Princeton lipid research clinics follow-up study. Pediatrics 2007;120:340–5. [DOI] [PubMed] [Google Scholar]
- [5].National Heart Lung and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics 2011;128(Suppl 5):S213–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- [7].Shay CM, Ning H, Allen NB, et al. Status of cardiovascular health in US adults: Prevalence estimates from the national health and nutrition examination surveys (NHANES) 2003–2008. Circulation 2012;125:45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Shay CM, Ning H, Daniels SR, et al. Status of cardiovascular health in US adolescents: Prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005–2010. Circulation 2013;127:1369–76. [DOI] [PubMed] [Google Scholar]
- [9].Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA 2012;307:1273–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].National Center for Health Statistics. National Health and Nutrition Examination Survey. Questionnaires, datasets, and related documentation. Available at http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Accessed January 2012.
- [11].Benowitz NL, Bernert JT, Caraballo RS, et al. Optimal serum cotinine levels for distinguishing cigarette smokers and nonsmokers within different racial/ethnic groups in the United States between 1999 and 2004. Am J Epidemiol 2009;169:236–48. [DOI] [PubMed] [Google Scholar]
- [12].Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat 2002;11:1–190. [PubMed] [Google Scholar]
- [13].United States. Dept. of Health and Human Services., United States. Dept. of Agriculture., United States. Dietary Guidelines Advisory Committee. Dietary guidelines for Americans, 2010. 7th edition. Washington, D.C.: G.P.O; 2010. [Google Scholar]
- [14].Guenther PM, Casavale KO, Reedy J, et al. Update of the healthy eating Index: HEI-2010. J Acad Nutr Diet 2013;113:569–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Bowman SA, Friday JE, Moshfengh AJ. MyPyramid equivalents database, 2.0 for USDA survey foods, 2003–2004 [Online]. Beltsville, MD: U.S. Department of Agriculture, ARS. Available at http://wwwarsusdagov/research/publications/publicationshtm?seq_no_115=229527 Accessed October 2012. 2008. [Google Scholar]
- [16].Friday JE, Bowman SA. MyPyramid equivalents database for USDA survey food codes, 1994–2002, version 1.0. U.S. Department of Agriculture, Agriculture Research Service. Available at http://wwwarsusdagov/research/publications/publicationshtm?seq_no_115=201058 Accessed August 2012. 2006. [Google Scholar]
- [17].USDA Food and Nutrient Database for Dietary Studies, 1.0. Beltsville, MD: Agricultural Research Service, Food Surveys Research Group; 2004. Available at http://www.ars.usda.gov/Services/docs.htm?docid=12085. Accessed April 9, 2014. [Google Scholar]
- [18].Moshfegh AJ, Rhodes DG, Baer DJ, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88:324–32. [DOI] [PubMed] [Google Scholar]
- [19].Basiotis PP, Carlson A, Gerrior SA, et al. The healthy eating Index: 1999–2000. US Department of Agriculture, Center for Nutrition Policy and Promotion CNPP-12; 2002. [Google Scholar]
- [20].Kit BK, Carroll MD, Lacher DA, et al. Trends in serum lipids among US youths aged 6 to 19 years, 1988–2010. JAMA 2012;308:591–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Laboratory Protocol. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. http://wwwcdcgov/nchs/nhanes/nhanes_questionnaireshtm Accessed October 2012. [Google Scholar]
- [22].National High Blood Pressure Education Program Working Group on High Blood Pressure in Children. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004;114:555–76. [PubMed] [Google Scholar]
- [23].Fagot-Campagna A, Saaddine JB, Flegal KM, Beckles GL. Diabetes, impaired fasting glucose, and elevated HbA1c in U.S. adolescents: The Third National Health and Nutrition Examination Survey. Diabetes Care 2001;24:834–7. [DOI] [PubMed] [Google Scholar]
- [24].Dalaker J, Proctor BD. Poverty in the United States: 1999. Washington, DC: US Census Bureau; 2000. Current Population Reports Series P60, No. 210. Available at http://www.census.gov/hhes/www/poverty/publications/p60-210.pdf Accessed June 2011. [Google Scholar]
- [25].Shah VBBB, Bieler GS. SUDAAN User’s manual, Release 9. Research Triangle Park, NC: Research Triangle Institute; 2005. [Google Scholar]
- [26].Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation 2007;116:1488–96. [DOI] [PubMed] [Google Scholar]
- [27].Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance - United States, 2011. MMWR Surveill Summ 2012:1–162. [PubMed] [Google Scholar]
- [28].Lowry R, Lee SM, Fulton JE, Kann L. Healthy people 2010 objectives for physical activity, physical education, and television viewing among adolescents: National trends from the Youth Risk Behavior Surveillance System, 1999–2007. J Phys Act Health 2009;6(Suppl 1):S36–45. [DOI] [PubMed] [Google Scholar]
- [29].Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:483–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Cook S, Auinger P, Li C, Ford ES. Metabolic syndrome rates in United States adolescents, from the national health and nutrition examination survey, 1999–2002. J Pediatr 2008;152:165–70. [DOI] [PubMed] [Google Scholar]
- [31].Ford ES, Mokdad AH, Ajani UA. Trends in risk factors for cardiovascular disease among children and adolescents in the United States. Pediatrics 2004;114:1534–44. [DOI] [PubMed] [Google Scholar]
- [32].Katzmarzyk PT, Srinivasan SR, Chen W, et al. Body mass index, waist circumference, and clustering of cardiovascular disease risk factors in a biracial sample of children and adolescents. Pediatrics 2004;114:e198–205. [DOI] [PubMed] [Google Scholar]
- [33].Laitinen TT, Pahkala K, Magnussen CG, et al. Ideal cardiovascular health in childhood and cardiometabolic outcomes in adulthood: The cardiovascular risk in young Finns study. Circulation 2012;125:1971–8. [DOI] [PubMed] [Google Scholar]
- [34].Oikonen M, Laitinen TT, Magnussen CG, et al. Ideal cardiovascular health in young adult populations from the United States, Finland, and Australia and its association with cIMT: The international childhood cardiovascular cohort consortium. J Am Heart Assoc 2013;2:e000244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Centers for Disease C, Prevention. School health guidelines to promote healthy eating and physical activity. MMWR Recomm Rep 2011;60:1–76. [PubMed] [Google Scholar]
- [36].Freedman DS, Mei Z, Srinivasan SR, et al. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: The Bogalusa Heart Study. J Pediatr 2007;150:12–17.e2. [DOI] [PubMed] [Google Scholar]
- [37].Singh AS, Mulder C, Twisk JW, et al. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes Rev 2008;9:474–88. [DOI] [PubMed] [Google Scholar]
- [38].Centers for Disease Control and Prevention. CDC health disparities and inequalities report - United States, 2011. MMWR Surveill Summ 2011;60(Suppl:1). [PubMed] [Google Scholar]
- [39].Centers for Disease Control and Prevention. Racial and ethnic approaches to community health (REACH). http://wwwcdcgov/reach/ Accessed October 2012.
- [40].American Diabetes Association. Standards of medical care in diabetes–2010. Diabetes Care 2010;33(Suppl 1):S11–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


