Abstract
While attention dysregulation is a promising early indicator of neurodevelopmental risk, in particular attention-deficit/hyperactivity disorder (ADHD), it is difficult to characterize clinical concern due to its developmental expectability at the transition to toddlerhood. Thus, explicating the typical:atypical continuum of risk indicators is among key future directions for research to promote early identification and intervention, and prevent decrements in attainment of developmental milestones into early childhood. In this paper, we present the Multidimensional Assessment Profiles – Attention Regulation Infant-Toddler (MAPS-AR-IT) Scale, a novel parent-report survey of dimensional, developmentally specified of attention (dys)regulation. We provide evidence of the validity of this measure in capturing the full typical:atypical spectrum via a longitudinal sample of typically developing children, at 12–18 months of age (baseline) via concurrent scores on well-validated temperament and clinical measures, as well as longitudinal stability and predictive validity via a clinical interview of ADHD symptoms at 24–30 months (follow-up). Item Response Theory was employed to characterize the typical:atypical spectrum of both normative and more concerning dysregulation (including the contexts in which behavior occurs). While not diagnostic, we present evidence of the utility of the MAPS-AR-IT in explicating individual neurodevelopmental risk and elucidating the broader typicality of behaviors related to attention (dys)regulation.
Keywords: developmental mechanisms, attention regulation, early mental health
1. Introduction
Attention dysregulation has been identified as a promising early indicator of neurodevelopmental risk (Diamond, 2013), particularly for attention-deficit/hyperactivity disorder (ADHD), a prevalent and impairing early-onset childhood syndrome tied to decrements in attainment of developmental milestones (Asherson, 2012; Blair & Raver, 2015). Given that a certain level of dysregulation in this domain is expectable, normative dysregulation during early childhood, characterizing the typical:atypical continuum of attention (dys)regulation to identify “when to worry” about young children’s attentional function is a key element of promoting earlier identification and prevention (Chacko et al., 2009; Wakschlag et al., 2019). A growing body of research has begun to pinpoint infant biobehavioral markers of attention (dys)regulation that are precursors to classic clinical presentation of ADHD (Miller, 2022). Given the potential for intervention to have the greatest impact at the vulnerability phase (Danielson et al., 2018; Willoughby et al., 2019), thereby slowing and reversing negative developmental cascades (Fuhs et al., 2013; Sonuga-Barke et al., 2011), increasing efforts in the past decade have sought to identify typical versus atypical behavioral expression and patterns in very early development. In support of this goal, we present the Multidimensional Assessment Profiles – Attention Regulation Infant-Toddler (MAPS-AR-IT) Scale, in order to foster earlier identification of neurodevelopmental risk via a developmentally specified, dimensional parent-report measure of attention (dys)regulation at the transition to toddlerhood.
1.1. Challenges to assessing early attention dysregulation
Assessment of attention dysregulation broadly, and ADHD-typical symptoms specifically, prior to preschool age has been hindered by difficulties in accounting for (1) typical developmental variation both between- and within-individuals, and (2) the unique contexts and concomitant demands relevant at the transition to toddlerhood (Sonuga-Barke & Halperin, 2010). Accordingly, a combined bottom-up and top-down approach to understanding the typical:atypical spectrum of indicators preceding the full ADHD phenotype is needed, alongside attempts at downward-extension of DSM-5 diagnostic criteria which tap the actual demands placed on children before they enter preschool settings (e.g., engaged in play with an adult for several minutes at a time, sitting still while engaged in a brief activity). Novel measures that “make sense” of the behaviors parents observe at home hold promise for improved accuracy of early identification. Simultaneously, lifespan coherence is made possible when measures downward extend ADHD-typical behaviors to developmentally feasible manifestations of target constructs (Blackwell et al., 2020; Wakschlag et al., 2010).
Assessment of attention regulation at the transition to toddlerhood along with making predictive judgments about infant capacities, is made all the more challenging by the potential transience of concerning behaviors as some children will naturally “grow out of” certain patterns as part of self-regulation acquisition. It is thus critical to develop means of reliably identifying children at heightened neurodevelopmental risk by examining the predictive strength of thresholds of concern. Consistent with our prior work, we aim to identify children whose behavior indicates concern, rather than ascribe diagnosis of psychopathology to children during the first two years of life (Krogh-Jespersen et al., 2022; Wakschlag et al., 2020).
1.2. Establishing the typical:atypical spectrum of attention (dys)regulation
In order to differentiate atypical (and potentially concerning) dysregulation from that which is developmentally typical, there is a need to first establish the full typical:atypical spectrum at the transition to toddlerhood. Attention (dys)regulation is a promising avenue for exploring neurodevelopmental risk at the earliest phase of the clinical sequence, as meaningful individual differences in attention regulation have been identified in the first year of life (Gurevitz et al., 2014; Morales et al., 2005), with relative stability beyond this developmental period (e.g., predicting to school-age ADHD diagnosis; Miller et al., 2018; Stephens et al., 2021; Miller et al., 2018; prevalence rates consistent from 2 years of age into school-age; Bufferd et al., 2012; Dougherty et al., 2015). While foundational to generating a science of early risk identification, this work has largely been conducted in small samples recruited via familial risk (e.g. Miller et al., 2018) or studied retrospectively via medical record (Gurevitz et al., 2014). Prior work measuring early attention (dys)regulation has also relied on intensive and/or costly methodologies, such as infant eye tracking (see also Goodwin et al., 2021). There has remained a need for more pragmatic and translational measurement, including developmentally meaningful parent surveys designed to capture the dimensional spectrum of behavior to support real world clinical feasibility.
Temperament approaches that characterize salient constructs such as “attention orienting” and “effortful control” have a long history. Measures such as the Infant Behavior Questionnaire (IBQ; Rothbart, 1981) and Early Childhood Behavior Questionnaire (ECBQ; Putnam et al., 2006) are particularly well-suited for assessing normative expression of attention (dys)regulation (Kaat et al.,2018). In contrast, surveys that take a quantitative approach to psychopathology like the Child Behavior Check List (CBCL; Achenbach & Rescorla, 2001) use a top-down method to capture symptoms across ages. Relative to a spectrum approach, we have previously shown that such measures have a floor effect that constrains capturing of normative variation (Wakschlag et al., 2020). Important advances have been made via developmentally based measures such as the ITSEA, which has translated problem behavior constructs into developmentally meaningful terms. However, there remains a gap in characterization of the typical:atypical spectrum of attention (dys) regulation that would enable identification of developmentally varying patterns and those children who are in gray areas of risk. Such measures have the potential to translate the importance of dimensional characterization of psychopathological patterns as developmentally unfolding, into measurable terms, to support earlier identification of risk (Casey, Oliveri, & Insel, 2014).
Tapping the developmental spectrum of behavior has the potential to inform our understanding of what constitutes atypical attention dysregulation (Dougherty et al., 2015). This approach is grounded in the previously articulated developmental specification framework and operationalized as multidimensional, developmental measurement of the typical:atypical spectrum of disruptive behavior via the Multidimensional Assessment Profiles – Disruptive Behavior (MAP-DB, formerly, Multidimensional Assessment of Preschool Disruptive Behavior) scale and its infant/toddler scale (MAP-DB-IT; Krogh-Jespersen et al., 2022), which captures irritability, noncompliance, and aggression. These measures include developmentally expectable behaviors at the transition to toddlerhood as well as indicators of concern, account for contextual variation, and use an objective frequency scale to aid in differentiation of normative behaviors most children do from those that are of concern (e.g., for high frequency of occurrence, or notably dysregulated expression). Such efforts help to identify those children at greater risk via models that “embrace rather than erase” valuable variation in differentiating typical:atypical behavior (Wakschlag et al., 2019). This approach is designed to inform decisions about “when to worry” within a developmental frame.
To this end, we introduce, and provide preliminary psychometric and validation evidence for, the Multidimensional Assessment Profiles – Attention Regulation Infant-Toddler (MAPS-AR-IT) scale as a novel measure of attention (dys)regulation starting at 12 months of age. The MAPS-AR-IT is a 12-item parent-report survey which provides a dimensional, developmentally specified means of capturing infant/toddler indicators of attention (dys)regulation by tapping not only the objective frequency of normative and less expectable forms of dysregulated behavior, but also the specific contexts in which dysregulation occurs (and whether behavior varies across settings). The scale was developed and refined by a team of experts in early childhood development, infant psychopathology, and early assessment of attention (dys)regulation following the same model of development, validation, and using the same measure as the authors of the well-validated MAP-DB scale, on which the MAPS-AR-IT is based (Wakschlag et al., 2012; Wakschlag et al., 2014). This team proposed items that would have coherence across early childhood development as well as behaviors that might be unique to the infant/toddler stage. The MAPS-AR-IT is intended to support identification of children whose attention dysregulation places them at greatest neurodevelopmental risk. In order to accomplish this, the aims of the present study are to (1) Model the typical:atypical spectrum of attention (dys)regulation of the MAPS-AR-IT using item response theory (IRT) methods, and (2) Examine the psychometric properties of the MAPS-AR-IT scale to establish its reliability and validity.
2. Method
2.1. Development of the Multidimensional Assessment Profiles of Attention Regulation – Infant-Toddler (MAPS-AR-IT) scale
To generate scale items, we convened 3 doctorate-level experts in early childhood development and developmental psychopathology, 1 practicing clinician with over 20 years of specialized experience in infant psychopathology, and 2 leading experts in early assessment of attention (dys)regulation, as well as a doctoral student whose research is focused on early risk indicators of attention-related disorders. Items were selected with the intention of representing normative types of dysregulation (based on the early childhood development literature) as well as possible risk factors for later attention-related disorders (e.g., poor sustained attention, restless and fidgety activity). Items were carefully selected to ensure developmental feasibility and language was adapted to represent the developmental contexts children occupy at this age (e.g., fidget restlessly during feedings or mealtimes). This measure was then administered to participants (see 2.2 below) in the When-to-Worry (W2W) Study. A few items were included with an eye toward developmental coherence, with versions of the measure designed for use at 24 and 36 months (e.g., “run or climb so dangerously that you couldn’t take your eyes of him/her”), in part meant to help determine the developmental point at which a normative behavior becomes atypical (e.g., “have trouble paying attention to a simple book or story for 5 minutes or longer”).
2.2. Participants
Participants were drawn from the When-to-Worry (W2W) Study, a socioeconomically and racially/ethnically diverse sample of children enrolled near the child’s first birthday (between 12 and 18 months of age, mean age at baseline = 14 months, N = 356), and their parents, who serve as the primary respondents. Primarily English-speaking (i.e., English used at home more than 50% of the time) Chicagoland families were recruited via diverse means (at pediatric clinics and through targeted ads on social media). For further details see prior published work in this sample as discussed in Krogh-Jesperson et al., 2022. Participating families completed an in-person assessment at baseline and follow-up with an interval of approximately 12 months, in order to examine predictive validity at ~24 months—the age at which the gold-standard clinical Preschool Age Psychiatric Assessment (PAPA) intervention has been validated (Egger et al., 1999). Surveys were also completed at these time points and repeated on a bimonthly basis between in-person assessments. The primary caregiver participating during the in-person assessments and all annual and bimonthly surveys was the child’s biological mother. Northwestern University’s Institutional Review Board approved the recruitment process and study design prior to the start of study activities (IRB# STU00202880).
Of the 356 children in the W2W study, 32 were excluded due to missing MAPS-AR-IT data at baseline. Thus, the total analytic sample N = 324. Approximately 2/3 of this sample (n = 202) provided clinical interview data at a follow-up visit that occurred near 24 months of age (participation was disrupted by COVID-19). Table 1 compared demographics between the sample at baseline (N = 324) and the excluded subsample whose data were not available for development of the MAPS-AR-IT (n = 32). The excluded subsample was more likely to be “poor” (i.e., at or below the Federal Poverty line as determined by income and household size), African American, or Hispanic. The analytic sample included a higher percentage of mothers with a Bachelor’s degree or higher, while over half of the mothers in the excluded subsample endorsed “some college” or less, though this did not reach the α = .05 level of significance. The two subsamples did not differ significantly by child’s sex assigned at birth.
Table 1.
Sample demographics.
| Analytic Sample (n = 324) | Excluded from Sample (n = 32) | ||||
|---|---|---|---|---|---|
| Freq. (%) | Freq. (%) | χ2 | df | p | |
| Child sex assigned at birth: female | 147 (45.4) | 16 (50.0) | .3 | 1 | .616 |
| Child race/ethnicity | |||||
| Hispanic | 80 (24.8) | 12 (37.5) | 16.2 | 3 | .001 |
| Non-Hispanic African-American | 66 (20.4) | 14 (43.8) | |||
| Non-Hispanic White/Caucasian | 144 (44.6) | 5 (15.6) | |||
| Non-Hispanic Non-White or | |||||
| African-American | 33 (10.2) | 1 (3.1) | |||
| Household at or below Federal | 12.0 | 1 | |||
| Poverty line | 65 (20.1) | 15 (46.9) | <.001 | ||
| Mother’s education level | |||||
| Less than high school | 2 (0.6) | 0 (0.0) | 3.1 | 1 | .077a |
| High school or GED | 24 (7.4) | 1 (5.6) | |||
| Associate’s degree/Trade School | 30 (9.3) | 2 (11.1) | |||
| Some college (no degree) | 57 (17.6) | 7 (38.9) | |||
| Bachelor’s degree | 96 (29.7) | 6 (33.3) | |||
| Graduate degree (MA, PhD, MD, JD) | 114 (35.3) | 2 (11.1) |
Test to compare Bachelor’s or Graduate degree versus others; p = .135 from Fisher’s exact test with all categories
2.3. Measures
2.3.1. Multidimensional Assessment Profiles of Attention Regulation – Infant-Toddler (MAPS-AR-IT) scale
All parent participants in the W2W Study were asked to complete the 12-item MAPS-AR-IT as part of a larger survey battery. Each item was scored on a 6-point scale, which assesses objective frequency of a target behavior (responses range from “0 - Never” to “5 - Many times each day”). These items tapped developmentally specified expressions of attentional control, with a subset of items tapping broad activity (dys)regulation within the specific contexts in which it might occur, ranging from more developmentally expectable (“when tired, hungry, or sick”) to less typical (“no matter what is going on around him/her”).
2.4. Construct Validation Measures
2.4.1. Infant-Toddler Social and Emotional Assessment (ITSEA) – Activity/Impulsivity and Attention subscales
The well-validated ITSEA Activity/Impulsivity problems and Attention competency subscales were used (Church et al., 2020; Thurm et al., 2018). The ITSEA Attention subscale is positively scored for attentional capacity whereas on the ITSEA Activity/Impulsivity, with a larger score indicating greater impulsivity and activity dysregulation. Thus, we anticipated a negative correlation between ITSEA Attention and MAPS-AR-IT scores, and positive correlations between the ITSEA Activity/Impulsivity and MAPS-AR-IT. ITSEA scores were available for 299 children in the analytic sample. Cronbach’s alpha was 0.61 for Activity/Impulsivity and 0.67 for Attention.
2.4.2. Early Childhood Behavior Questionnaire (ECBQ) – Effortful Control subscale
The ECBQ is a parent-report measure of child temperament from 18 to 36 months of age. On the effortful control subscale, high scores indicate higher levels of self-regulation, which is derived from items indexing a child’s ability to control and shift attention (Putnam et al., 2006). As the Effortful Control subscale of the ECBQ is a competence scale, we anticipated a negative relationship with the MAPS-AR-IT. Scores were available for 302 children in the analytic sample. Cronbach’s alpha was 0.72.
2.4.3. Preschool Age Psychiatric Assessment (PAPA) – Attention Deficit/Hyperactivity Disorder domain
The PAPA is a well-validated semi-structured parent interview of developmentally specified behaviors indicative of clinical concerns in early childhood (Egger et al., 1999). The ADHD domain contains 20 items describing the child’s ADHD-related behavior. Symptoms of each of the 20 items are scored as absent (= 0) or present (= 1) based on trained interviewer interpretations, and the total number of symptoms present was used in analysis (possible range: 0 to 20). we treated symptoms continuously. Scores on the ADHD domain were available at follow up for 202 children.
2.5. Analysis Plan
2.5.1. Patterns of response distribution
We examined the distribution of frequency responses to each behavior captured by the MAPS-AR-IT. This approach is consistent with prior work on the MAP-DB (Krogh-Jespersen et al., 2022; Wakschlag et al., 2014), and serves as a basis for understanding patterns of variation of attention (dys)regulation behaviors.
2.5.2. Factor generation
We employed Mokken scaling to ascertain whether our data represent a unified construct (i.e., attention (dys)regulation) or multiple dimensions. Consistent with the literature on handling skewness in data, Mokken scaling is an appropriate non-parametric test of item relatedness and latent construct identification (Watson et al., 2012). Goodness-of-fit and number of Mokken scales was investigated via application of an automated item selection procedure (AISP), which partitions items into Mokken scales, excluding any items that are unscalable according to a hierarchical clustering approach (van der Ark, 2012). We assessed item relatedness via Loevinger’s coefficient (H), an indicator of the scalability of items in a measure or item set (van der Ark, 2011). When H exceeds 0.5, the scale is considered strong.
2.5.3. Item Response Theory (IRT)
We used IRTPRO version 4.2 to fit a single-factor graded response model, which is appropriate for ordinal item responses, and obtain IRT scores of MAPS-AR-IT responses (Paek & Han, 2013). Because each item has 6 ordered response categories, 5 threshold parameters (i.e., location) and 1 unique slope parameter (i.e., discrimination) were estimated per item. Threshold parameters for a certain category refer to the point along the latent trait value θ scale at which individuals have a 0.50 probability of responding in or above this category. A single location index i, defined as the mean of the five threshold parameters (bi1 to bi5), was then calculated (Ali et al., 2015). The item slope parameters refer to the strength of the relation each item has with the latent trait value θ of attention (dys)regulation (higher slopes indicating stronger relations; Toland, 2014). Expected a posteriori scoring (EAP) was employed to generate a score representing an individual’s attention dysregulation level on the scale of the latent trait (i.e., IRT scores). We arranged individuals’ IRT scores from high to low and defined “atypical” responses as falling at 95th percentile or above, a cut-off that reflects the severe/atypical nature of clinically concerning behavior. This is consistent with approaches in similar prior work (Wakschlag et al., 2014). We then assessed goodness of fit of the IRT modeling overall via the scale’s root-mean-square error of approximation (RMSEA); RMSEA < 0.05 indicates goodness of model fit for categorical response data (Maydeu-Olivares, 2013; Maydeu-Olivares & Joe, 2014). Calibration was performed using the baseline data, and parameters were applied to the follow-up data to generate IRT scores in the follow-up wave. A paired t-test and Pearson correlation were conducted to examine the relationship between the two waves of MAPS-AR-IT IRT scores.
2.5.4. Reliability and validity
As there is no gold standard measure for attention regulation at this age, we used a nomological net of well-validated measures capturing constructs highly related to attention and self-regulation in infancy. Test-retest reliability of MAPS-AR-IT estimated IRT scores was conducted using the two observations closest in time (i.e., less than two months apart) and between 12 and 18 months of age, n = 189, mean = 1.65 months, SD = 0.29). At baseline, we conducted Pearson correlations between IRT scores and related-construct measures, using the ITSEA Activity/Impulsivity and Attention subscales, and Effortful Control via the ECBQ. Longitudinal stability was assessed via Pearson correlations between the MAPS-AR-IT at baseline and follow up (n = 202, mean = 27.5 months, SD = 1.6 months). We also predicted ADHD symptomology from MAPS-AR-IT IRT scores one year later via the PAPA to assess predictive convergent validity.
3. Results
3.1. Patterns of response distribution
Response patterns were reviewed as indicators of both the atypicality of a particular behavior (i.e., whether it is something very few reported) and the frequency of occurrence of these behaviors based on descriptive analysis (see Table 2; see also Supplementary Figure 1 for histogram presentation of these data). Consistent with prior work on the original MAP-DB-IT measure that inspired this one, we sought to determine whether there were frequency markers that distinguished the atypical from the typical (Krogh-Jespersen et al., 2022). In general, items appeared to capture behaviors that either were not endorsed by a large portion of the sample (or endorsed at the lowest frequency if at all), while others were endorsed by most of the sample at a broad distribution of frequencies. For example, “fidget restlessly during feedings or mealtime,” was reported as 0/Never (43%) or 1/Rarely (28%). Meanwhile, “jump quickly from one toy or activity to another without really playing with any of the toys” was endorsed by 93% of the sample as occurring at some frequency, however, only 9% of parents reported that this occurred “many times each day or higher.” We note that a behavioral frequency of “many times each day or higher” was reported in < 10% of responses across all items, in contrast with other versions of the MAP-DB tapping irritability, which have identified daily occurrence as an important threshold (Krogh-Jespersen et al., 2022; Wakschlag et al., 2014). This high frequency could represent a concrete threshold for screening in clinical settings, where IRT scoring is less feasible. In general, trends of item endorsement at baseline resembled those at follow-up, with similar percentages of children scoring “Never” across both time points; however, patterns of item endorsement above a 0 differed at follow up (see Supplementary Table 1), with fewer parents endorsing behaviors at the higher end of the spectrum (i.e., daily or more occurrence).
Table 2.
MAPS-AR-IT 12-month IRT Estimates with Severity Threshold
| Category Thresholds | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| Never | Rarely (Less than Some (1–3) days of Most (4–6) days of lx/week) the week the week or higher | Every day of the week or higher | Many times each day or higher | |||||||||
|
|
||||||||||||
| Freq. | Percentage | |||||||||||
| In the oast month, how often did vour child… | ||||||||||||
| 1. Jump quickly from one toy or activity to another without really playing with the toys | 20 | 6.56% | 68 | 22.30% | 105 | 34.43% | 51 | 16.72% | 33 | 10.82% | 28 | 9.18% |
| 2. Have trouble paying attention to a simple book or story for 5 minutes or longer | 26 | 8.52% | 71 | 23.28% | 81 | 26.56% | 55 | 18.03% | 41 | 13.44% | 31 | 10.16% |
| 3. Seem easily distracted by things that were happening around him/her | 13 | 4.26% | 68 | 22.30% | 102 | 33.44% | 59 | 19.34% | 32 | 10.49% | 31 | 10.16% |
| 4. Have trouble sitting still even for a few minutes | 38 | 12.46% | 85 | 27.87% | 78 | 25.57% | 55 | 18.03% | 20 | 6.56% | 29 | 9.51% |
| 5. Run or climb so dangerously that you couldnť take your eyes off him/her | 101 | 33.11% | 71 | 23.28% | 59 | 19.34% | 31 | 10.16% | 26 | 8.52% | 17 | 5.57% |
| 6. Fidget restlessly during feedings or mealtime | 132 | 43.28% | 88 | 28.85% | 51 | 16.72% | 19 | 6.23% | 10 | 3.28% | 5 | 1.64% |
| 7. Demand your attention without being able to wait | 47 | 15.41% | 79 | 25.90% | 90 | 29.51% | 38 | 12.46% | 29 | 9.51% | 22 | 7.21% |
| In the past month, how often did vour child have trouble Davina attention, keeping still or waiting… | ||||||||||||
| 8. When frustrated, angry, or upset | 34 | 11.15% | 68 | 22.30% | 96 | 31.48% | 50 | 16.39% | 43 | 14.10% | 14 | 4.59% |
| 9. During daily routines such as mealtime, bedtime, or getting dressed | 47 | 15.41% | 96 | 31.48% | 85 | 27.87% | 40 | 13.11% | 25 | 8.20% | 12 | 3.93% |
| 10. No matter what is going on around him/her | 94 | 30.82% | 116 | 38.03% | 53 | 17.38% | 17 | 5.57% | 20 | 6.56% | 5 | 1.64% |
| 11. When excited | 63 | 20.66% | 94 | 30.82% | 89 | 29.18% | 27 | 8.85% | 23 | 7.54% | 9 | 2.95% |
| 12. When tired, hungry, or sick | 33 | 10.82% | 74 | 24.26% | 108 | 35.41% | 46 | 15.08% | 30 | 9.84% | 14 | 4.59% |
The mean (and standard deviation) on the MAPS-AR-IT IRT scores at follow up (i.e., ~24 months) was −0.35 (0.85) for 295 W2W participants for whom data were available (note that modeling of the MAPS-AR-IT at 24–30 months of age included participants who did not have data at baseline and thus are not included in the larger analytic sample). A paired t-test between baseline and follow up indicated that the difference in the two scores (n = 202) was significant—mean difference = 0.45 (SD = 0.83), t(201) = 7.68, p < .0001. Given that the scoring parameters were generated from the baseline data (i.e., a score of 0.00 is the expected value at 12–14 months), these score distributions suggest that, on average, attention dysregulation is higher during infancy and decreases during the second year of life.
3.2. Mokken scaling
Application of AISP selected all items in the MAPS-AR-IT to represent a unidimensional latent construct. Mokken scaling on this measure yielded an H of 0.56, suggesting strong construct unity. Accordingly, all items were determined to belong within the scale and were included during IRT norming.
3.3. IRT
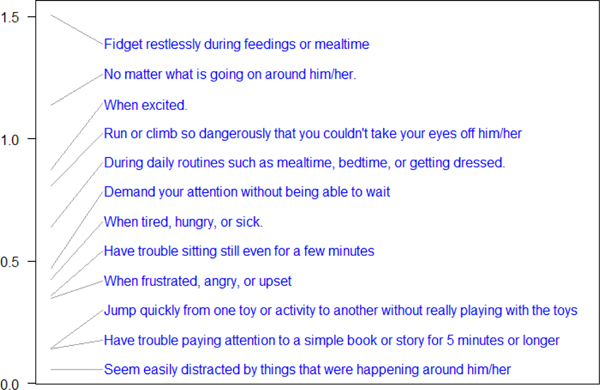
Item threshold estimates (bi1 to bi5) for each item are presented in Table 3. The 95th percentile is 1.72, therefore “atypical” responses, defined as having an item threshold of the 95th percentile or higher correspond to 1.72 or higher within our sample. For example, parent endorsement of “many times each day or higher” to item “Jump quickly from one toy or activity to another without really playing with the toys” (b5 = 2.02) falls in the 95th percentile of responses to that item. Similarly, “fidget restlessly…,” “have trouble paying attention to a simple book or story…,” and “demand your attention without being able to wait” are atypical behaviors at this age if they occur “many times each day or higher” but not otherwise. Of the MAPS-AR-IT items, ten represented behaviors that became atypical at the frequency of “many times each day or higher” (see Table 3), while “have trouble sitting still even for a few minutes” did not cross the atypicality threshold at any frequency of occurrence at baseline, although it became atypical at follow-up with occurring “every day of the week or higher.” None of the item threshold values were located above the 95th percentile, i.e., a parent endorsing the item as anything above a “0 – Never” in frequency is not atypical (see Figure 1).
Table 3.
MAPS-AR-IT 12-month IRT estimates with severity threshold
| Item Slope | Category Thresholds | Item Location | |||||
|---|---|---|---|---|---|---|---|
| Rarely (Less than 1x/week) or higher | Some (1–3) days of the week or higher | Most (4–6) days of the week or higher | Every day of the week or higher | Many times each day or higher | |||
|
|
|||||||
| a | b1 | b2 | b3 | b4 | b5 | mean (b) | |
|
| |||||||
| Attention Regulation (95th perc. score = 1.72) | |||||||
| In the past month, how often did your child… | |||||||
| Have trouble sitting still even for a few minutes | 2.19 | −1.38 | −0.31 | 0.5 | 1.25 | 1.71 | 0.36 |
| Seem easily distracted by things that were happening around him/her | 2.13 | −2.12 | −0.75 | 0.33 | 1.1 | 1.73 | 0.06 |
| Fidget restlessly during feedings or mealtime | 1.88 | −0.24 | 0.73 | 1.63 | 2.33 | 3.08 | 1.51 |
| Jump quickly from one toy or activity to another without really playing with the toys | 1.59 | −2.19 | −0.79 | 0.47 | 1.22 | 2.02 | 0.15 |
| Run or climb so dangerously that you couldn’t take your eyes off him/her | 1.83 | −0.64 | 0.14 | 0.89 | 1.44 | 2.21 | 0.81 |
| Have trouble paying attention to a simple book or story for 5 minutes or longer | 1.8 | −1.81 | −0.62 | 0.29 | 0.99 | 1.84 | 0.14 |
| Demand your attention without being able to wait | 1.79 | −1.41 | −0.34 | 0.67 | 1.31 | 2.11 | 0.47 |
| In the past month, how often did your child have trouble paying attention, keeping still or waiting… | |||||||
| No matter what is going on around him/her | 2.63 | −0.6 | 0.51 | 1.27 | 1.71 | 2.79 | 1.14 |
| When excited | 1.96 | −1.07 | −0.03 | 1.06 | 1.69 | 2.72 | 0.88 |
| During daily routines such as mealtime, bedtime, or getting dressed | 2.34 | −1.24 | −0.14 | 0.75 | 1.47 | 2.34 | 0.64 |
| When frustrated, angry, or upset | 2.37 | −1.44 | −0.51 | 0.41 | 1.08 | 2.2 | 0.35 |
| When tired, hungry, or sick | 2.48 | −1.45 | −0.5 | 0.58 | 1.3 | 2.19 | 0.43 |
Note: Items ordered by severity score with each item stem. Mean(b) is the average of the five theta/item threshold values. Theta values greater than 1.72 were bolded, indicating atypicality. Items are presented in the table in the order of administration.
Figure 1.
Severity spectrum of MAPS-AR-IT 12 mos. items
In comparing items at baseline with the IRT-derived severity continuum at follow-up, we found that patterns were broadly similar. However, we did identify items with threshold values above the 95th percentile at this older toddler timepoint (see Supplementary Table 2), indicating that certain behaviors that occur as frequently as “most days of the week” or “every day” were atypical in mature toddlers (e.g., “Have trouble paying attention to a simple book or story for 5 minutes or longer” and “Have trouble paying attention, keeping still or waiting no matter what was going on around him/her”), an unsurprising finding given increased developmental capacity at follow up.
3.4. Reliability and Validity
The MAPS-AR-IT had high internal consistency across all 12 items, indicated by a McDonald’s omega of 0.93. Test-retest reliability (across a two-month interval) was high, with a Pearson correlation coefficient of 0.76, and ICC = 0.76 (95% CI: .69, .81). Finally, metrics of validity indicate moderate to high concurrent and predictive convergent validity (see Table 4). Concurrent: The MAPS-AR-IT estimated IRT scores correlated strongly and positively with the ITSEA Activity/Impulsivity problem subscale and moderately and negatively with the ITSEA Attention subscale and ECBQ Effortful Control competency subscales. Longitudinal: MAPS-AR-IT longitudinal stability from baseline to follow-up was high and moderate-strength correlations to a sum score of PAPA ADHD symptoms at follow-up indicated predictive convergent validity.
Table 4.
Pearson correlations of attention regulation measures and MAPS-AR
| Concurrent | Longitudinal | ||||
|---|---|---|---|---|---|
|
|
|||||
| ITSEA: Activity & Impulsivity | ITSEA: Attention | ECBQ: Effortful Control | MAPS-AR-IT at follow up | PAPA: ADHD at ~24 mos Total | |
|
|
|||||
| MAPS-AR Baseline | 0.55*** | −0.30*** | −0.44*** | 0.57*** | 0.32*** |
| n | 297 | 297 | 300 | 202 | 197 |
Note: ITSEA Attention and ECBQ Effortful Control are both competence subscales that positively score related capacities for each child, rather than areas of deficit or concern.
p < .001
4. Discussion
A dimensional, developmentally specified measure of attention (dys)regulation that captures behaviors of normative attention dysregulation can bolster our understanding of how indicators of neurodevelopmental risk unfold during the first two years of life, when such capacities are rapidly developing (Richards et al., 2010). We here present the MAPS-AR-IT which we developed to address an extant gap in early assessment in the form of a validated parent-report measure that captures the typical:atypical spectrum of attention (dys)regulation within developmental and motivational contexts. Psychometric findings support the MAPS-AR-IT as a unidimensional measure of attention regulation at the transition to toddlerhood with moderate construct and convergent validity when correlated with both normative (i.e., temperament) and clinical measures of attention. Furthermore, the strong unidimensionality of the MAPS-AR-IT—notable for its inclusion of items that capture both attentional and activity-based dysregulation—informs our understanding of the developmental phenotype of attention (dys)regulation as expressed in young children. Calibration via IRT illustrates the promise of this measure in capturing the broader typical:atypical range of attention regulation in this population.
The advantage of the MAPS-AR-IT as presented in this paper is in the richness, dimensionality, and developmental sensitivity with which attention (dys)regulation behavior is captured. By design, this measure captures the spectrum of developmental expectability. While some items were included as developmentally typical expressions of attention dysregulation that were only atypical at the highest frequency (e.g., “Have trouble paying attention to a simple story or book for more than 5 minutes”), others keyed into more rare and unexpected forms of dysregulation (e.g., “Fidget restlessly during feedings or mealtimes”). A novel feature of this scale is its inclusion of context-specific items among specific attention (dys)regulation behaviors, particularly as this informs our understanding of the developmental expectability of certain behaviors. Not all contexts are equal in their demands for attention or regulation. In accounting for contextual variation, the MAPS-AR-IT taps critical information about the expectability of a child’s dysregulation. Difficulty paying attention or staying still might be expected when a child is tired or sick, but it may represent less typical attention (dys)regulation if it occurs when the child is excited, or happens no matter the context. In fact, contextual variability—and difficulty modulating behavior between contexts in which it is discouraged versus permitted—is its own promising indicator of dysregulation (Dirks et al., 2012). However, while invariability across contexts was the most severe “context-specific” item, we note that, as with our behavioral items, no single context item crossed the severity threshold at baseline. Rather, these manifestations of dysregulation become severe at the highest frequency of occurrence, and are severe at the item level when this measure is administered at the ~24 month follow-up. Thus, we propose that, unlike in our work with irritability, context items on the MAPS-AR-IT are not sufficient indicators on their own but instead part of a larger construct of dysregulation. Further, given the importance of capturing context, especially in traditional assessment and diagnosis of attention-related disorders, and the need for coherence with later iterations of the measures where certain contexts may yet prove to be singular severity indicators, we propose that there is utility in continuing to capture the many and varied contexts in which attention-dysregulated behaviors occur across the transition to toddlerhood.
Future directions for this research include extending our psychometric work to translate the MAPS-AR-IT to primary care and other clinical settings, beyond its application in clinical research, and calibrate the measure with yet more diverse samples. While the clinical applicability of an IRT-scored measure is constrained by the present sample size, replication of this psychometric work within a larger representative sample, such as has been successfully conducted with other MAPS scales (Krogh-Jespersen et al., 2022), will further advance this aim. Furthermore, with time and the establishment of item banks, advanced knowledge about item functioning could serve to translate the MAPS-AR-IT to pragmatic screening of neurodevelopmental risk in early childhood care and intervention settings (see work by Gibbons et al., 2012, 2014, 2019 on mental health assessments using computerized adaptive tests via IRT scoring methods). This would provide empirically-and developmentally-based parameters to identify children at high risk for problems in regulating attention as well as those in the “gray area” who may or may not benefit from intervention depending on their profile of risk and protective factors that may be derived from more in-depth developmental, clinical and family assessment. This is important to advance in future work. The development of clinical thresholds and probabilistic risk determination with this scale will be critical for clinical utility such as primary care and infant mental health settings. Assessment of risk during a period of rapid development must allow for the developmental change that can and will occur in the infant and toddler years, which the current version of the MAPS-AR-IT can help researchers meaningfully capture and characterize. However, given that much remains unknown about the developmental trajectories children will travel during this period, it is critical to avoid pathologizing individuals based on their MAPS-AR-IT scores and to contextualize the study of attention (dys)regulation within the larger story of rapid skill acquisition and transient perturbation (Wakschlag et al., 2019). We present the MAPS-AR-IT as a novel, dimensional, developmentally specified measure of neurodevelopmental risk that can improve our understanding of typical (versus clinically concerning) attention (dys)regulation and characterize early developmental trajectories in a manner designed to advance central objectives of the infant mental health field, i.e., early, developmentally based risk detection that can be leveraged for strengths-based self-regulation bolstering.
Supplementary Material
Key finding #1:
The MAPS-AR-IT forms a unidimensional measure of behaviors that span traditional “hyperactive” and “inattentive” clinical characterizations as well as normative dysregulation. This has implications for how we think about the underlying mechanisms of dysregulation in future studies, especially as behavioral indicators of both physical and cognitive (dys)regulation noted by parents may better be thought of as belonging to a single underlying capacity. This work informs our understanding of the developmental phenotype of attention (dys)regulation as expressed in young children.
Key finding #2:
Determination of the severity spectrum (via Item Response Theory) allows us to comment on the typicality of specific behaviors. While items were initially included on the basis of spanning a spectrum of typical:atypical attention (dys)regulation, the norming efforts of this study indicate that the frequency at which each behavior occurs is the most informative of relative severity when using this measure at 12–18 months of age. While no individual items crossed the predetermined severity threshold, we do find that manifestations of physical restlessness (e.g. “Fidget restlessly during feedings or mealtimes”) and dysregulation that occurs regardless of context (e.g., “no matter what is going on around him/her”) are the most severe items. This indicates the promise of capturing developmentally specified behaviors as well as the potential utility of noting broad dysregulation that occurs across contexts.
Key finding #3:
The developmentally based MAPS-AR-IT, while not a diagnostic tool, allows us to look earlier in the lifespan when considering atypicality of behavior and to look at the broad spectrum of these behaviors. A key novel contribution of this work is the developmental specification of attention (dys)regulation alongside cross-sectional and longitudinal validation when correlated with both normative (i.e., temperament) and clinical measures of attention. We propose that this is an appropriate complement to clinical assessments aimed at differentiating the typical from the atypical, as the MAPS-AR-IT serves a novel function in spanning the broader spectrum of severity and typicality at this early age.
References
- Achenbach TM, & Rescorla L. (2001). Manual for the ASEBA school-age forms & profiles: An integrated system of multi-informant assessment. University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Ali US, Chang H-H, & Anderson CJ (2015). Location indices for ordinal polytomous items based on item response theory. ETS Research Report Series, 2015(2), 1–13. 10.1002/ets2.12065 [DOI] [Google Scholar]
- Asherson P. (2012). ADHD across the lifespan. Medicine, 40(11), 623–627. 10.1016/j.mpmed.2012.08.007 [DOI] [Google Scholar]
- Bibok MB, Carpendale JIM, & Müller U. (2009). Parental scaffolding and the development of executive function. New Directions for Child and Adolescent Development, 2009(123), 17–34. 10.1002/cd.233 [DOI] [PubMed] [Google Scholar]
- Blackwell CK, Wakschlag L, Krogh-Jespersen S, Buss KA, Luby J, Bevans K, Lai J-S, Forrest CB, & Cella D. (2020). Pragmatic health assessment in early childhood: The PROMIS® of developmentally based measurement for pediatric psychology. Journal of Pediatric Psychology, 45(3), 311–318. 10.1093/jpepsy/jsz094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair C, & Raver CC (2015). School readiness and self-regulation: A developmental psychobiological approach. Annual Review of Psychology, 66(1), 711–731. 10.1146/annurev-psych-010814-015221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bufferd SJ, Dougherty LR, Carlson GA, Rose S, & Klein DN (2012). Psychiatric disorders in preschoolers: Continuity from ages 3 to 6. American Journal of Psychiatry, 169(11), 1157–1164. 10.1176/appi.ajp.2012.12020268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter AS, Briggs-Gowan MJ, Jones SM, & Little TD (2003). The Infant-Toddler Social and Emotional Assessment (ITSEA): Factor structure, reliability, and validity. Journal of Abnormal Child Psychology, 31(5), 495–514. 10.1023/a:1025449031360 [DOI] [PubMed] [Google Scholar]
- Casey BJ, Oliveri ME, & Insel T. (2014). A neurodevelopmental perspective on the research domain criteria (RDoC) framework. Biological psychiatry, 76(5), 350–353. [DOI] [PubMed] [Google Scholar]
- Chacko A, Wakschlag L, Hill C, Danis B, & Espy K. (2009). Viewing preschool disruptive behavior disorders and ADHD through a developmental lens: What do we know and what do we need to know? Child and Adolescent Psychiatric Clinics of North America, 18, 627–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Church PT, Grunau RE, Mirea L, Petrie J, Soraisham AS, Synnes A, Ye XY, & O’Brien K. (2020). Family Integrated Care (FICare): Positive impact on behavioural outcomes at 18 months. Early Human Development, 151, 105196. 10.1016/j.earlhumdev.2020.105196 [DOI] [PubMed] [Google Scholar]
- Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, & Blumberg SJ (2018). Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents, 2016. Journal of Clinical Child & Adolescent Psychology, 47(2), 199–212. 10.1080/15374416.2017.1417860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond A. (2013). Executive functions. Annual Review of Psychology, 64(1), 135–168. 10.1146/annurev-psych-113011-143750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dirks MA, De Los Reyes A, Briggs‐Gowan M, Cella D, & Wakschlag LS (2012). Annual Research Review: Embracing not erasing contextual variability in children’s behavior–theory and utility in the selection and use of methods and informants in developmental psychopathology. Journal of Child Psychology and Psychiatry, 53(5), 558–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty LR, Leppert KA, Merwin SM, Smith VC, Bufferd SJ, & Kushner MR (2015). Advances and directions in preschool mental health research. Child Development Perspectives, 9(1), 14–19. 10.1111/cdep.12099 [DOI] [Google Scholar]
- Egger HL, Ascher BH, & Angold A. (1999). Preschool Age Psychiatric Assessment (PAPA). In. Durham, North Carolina: Duke University Medical Center. [Google Scholar]
- Fuhs MW, Farran DC, & Nesbitt KT (2013). Preschool classroom processes as predictors of children’s cognitive self-regulation skills development. School Psychology Quarterly, 28(4), 347–359. 10.1037/spq0000031 [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Weiss DJ, Pilkonis PA, Frank E, Moore T, Kim JB, & Kupfer DJ (2012). Development of a computerized adaptive test for depression. Archives of general psychiatry, 69(11), 1104–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons RD, Perraillon MC, & Kim JB (2014). Item response theory approaches to harmonization and research synthesis. Health Services and Outcomes Research Methodology, 14(4), 213–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons RD, & deGruy FV (2019). Without wasting a word: Extreme improvements in efficiency and accuracy using computerized adaptive testing for mental health disorders (CAT-MH). Current Psychiatry Reports, 21(8), 1–9. [DOI] [PubMed] [Google Scholar]
- Goodwin A, Hendry A, Mason L, Bazelmans T, Begum Ali J, Pasco G, Charman T, Jones E, & Johnson M. (2021). Behavioural measures of infant activity but not attention associate with later preschool ADHD traits. Brain Sciences, 11(5), 524. 10.3390/brainsci11050524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurevitz M, Geva R, Varon M, & Leitner Y. (2014). Early markers in infants and toddlers for development of ADHD. Journal of Attention Disorders, 18(1), 14–22. 10.1177/1087054712447858 [DOI] [PubMed] [Google Scholar]
- Hammond SI, Müller U, Carpendale JIM, Bibok MB, & Liebermann-Finestone DP (2012). The effects of parental scaffolding on preschoolers’ executive function. Developmental Psychology, 48(1), 271. 10.1037/a0025519 [DOI] [PubMed] [Google Scholar]
- Kaat AJ, Blackwell CK, Estabrook R, Burns JL, Petitclerc A, Briggs-Gowan MJ, Gershon RC, Cella D, Perlman SB, & Wakschlag LS (2018). Linking the Child Behavior Checklist (CBCL) with the Multidimensional Assessment Profile of Disruptive Behavior (MAP-DB): Advancing a Dimensional Spectrum Approach to Disruptive Behavior. Journal of Child and Family Studies, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krogh-Jespersen S, Kaat AJ, Petitclerc A, Perlman SB, Briggs-Gowan MJ, Burns JL, ... & Wakschlag LS (2022). Calibrating temper loss severity in the transition to toddlerhood: Implications for developmental science. Applied developmental science, 26(4), 785–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landau R, Avital M, Berger A, Atzaba-Poria N, Arbelle S, Faroy M, & Auerbach JG (2010). Parenting of 7-month-old infants at familial risk for attention deficit/hyperactivity disorder. Infant Mental Health Journal: Official Publication of The World Association for Infant Mental Health, 31(2), 141–158. 10.1002/imhj.20249 [DOI] [PubMed] [Google Scholar]
- Landry SH, Miller-Loncar CL, Smith KE, & Swank PR (2002). The role of early parenting in children’s development of executive processes. Developmental Neuropsychology, 21(1), 15–41. 10.1207/s15326942dn2101_2 [DOI] [PubMed] [Google Scholar]
- MacNeill LA, Zhang Y, Giase G, Nili A, Wiggins J, Allen NB, & Wakschlag LS (in prep). Multi-level indicators of irritability as transdiagnostic predictors of clinical liability in young children. [Google Scholar]
- Maydeu-Olivares A. (2013). Goodness-of-fit assessment of item response theory models. Measurement: Interdisciplinary Research and Perspectives, 11(3), 71–101. 10.1080/15366367.2013.831680 [DOI] [Google Scholar]
- Maydeu-Olivares A, & Joe H. (2014). Assessing approximate fit in categorical data analysis. Multivariate Behavioral Research, 49(4), 305–328. 10.1080/00273171.2014.911075 [DOI] [PubMed] [Google Scholar]
- Miller M. (2022). Editorial: Are we there yet? Identification and intervention for attention-deficit/hyperactivity disorder in the first years of life. Journal of the American Academy of Child and Adolescent Psychiatry, 61(2), 122–124. 10.1016/j.jaac.2021.05.010 [DOI] [PubMed] [Google Scholar]
- Miller M, Iosif A-M, Young GS, Hill MM, & Ozonoff S. (2018). Early detection of ADHD: insights from infant siblings of children with autism. Journal of Clinical Child & Adolescent Psychology, 47(5), 737–744. 10.1080/15374416.2016.1220314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales M, Mundy P, Crowson M, Neal AR, & Delgado C. (2005). Individual differences in infant attention skills, joint attention, and emotion regulation behaviour. International Journal of Behavioral Development, 29(3), 259–263. 10.1080/01650250444000432 [DOI] [Google Scholar]
- Paek I, & Han KT (2013). IRTPRO 2.1 for Windows (item response theory for patient-reported outcomes). Applied Psychological Measurement, 37(3), 242–252. 10.1177/0146621612468223 [DOI] [Google Scholar]
- Pauli-Pott U, Schloß S, & Becker K. (2018). Maternal responsiveness as a predictor of self-regulation development and attention-deficit/hyperactivity symptoms across preschool ages. Child Psychiatry & Human Development, 49(1), 42–52. 10.1007/s10578-017-0726-z [DOI] [PubMed] [Google Scholar]
- Putnam SP, Gartstein MA, & Rothbart MK (2006). Measurement of fine-grained aspects of toddler temperament: The Early Childhood Behavior Questionnaire. Infant Behavior and Development, 29(3), 386–401. 10.1016/j.infbeh.2006.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards JE, Reynolds GD, & Courage ML (2010). The neural bases of infant attention. Current Directions in Psychological Science, 19(1), 41–46. 10.1177/0963721409360003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbart MK (1981). Measurement of temperament in infancy. Child Development, 52, 569–578. [Google Scholar]
- Sonuga-Barke EJS, & Halperin JM (2010). Developmental phenotypes and causal pathways in attention deficit/hyperactivity disorder: Potential targets for early intervention? Journal of Child Psychology and Psychiatry, 51(4), 368–389. 10.1111/j.1469-7610.2009.02195.x [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Koerting J, Smith E, McCann DC, & Thompson M. (2011). Early detection and intervention for attention-deficit/hyperactivity disorder. Expert Review of Neurotherapeutics, 11(4), 557–563. 10.1586/ern.11.39 [DOI] [PubMed] [Google Scholar]
- Stephens RL, Elsayed HE, Reznick JS, Crais ER, & Watson LR (2021). Infant attentional behaviors are associated with ADHD symptomatology and executive function in early childhood. Journal of Attention Disorders, 25(13), 1908–1918. 10.1177/1087054720945019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurm A, Manwaring SS, Cardozo Jimenez C, Swineford L, Farmer C, Gallo R, & Maeda M. (2018). Socioemotional and behavior problems in toddlers with language delay. Infant Mental Health Journal, 39(5), 569–580. 10.1002/imhj.21735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toland MD (2014). Practical guide to conducting an item response theory analysis. The Journal of Early Adolescence, 34(1), 120–151. 10.1177/0272431613511332 [DOI] [Google Scholar]
- van der Ark LA (2012). New developments in Mokken scale analysis in R. Journal of Statistical Software, 48(5), 1–27. 10.18637/jss.v048.i05 [DOI] [Google Scholar]
- Wakschlag LS, Briggs-Gowan MJ, Choi SW, Nichols SR, Kestler J, Burns JL, ... & Henry D. (2014). Advancing a multidimensional, developmental spectrum approach to preschool disruptive behavior. Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), 82–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Choi SW, Carter AS, Hullsiek H, Burns J, McCarthy K, ... & Briggs‐Gowan MJ (2012). Defining the developmental parameters of temper loss in early childhood: implications for developmental psychopathology. Journal of Child Psychology and Psychiatry, 53(11), 1099–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Krogh-Jespersen S, Estabrook R, Hlutkowsky CO, Anderson EL, Burns JL, Briggs-Gowan MJ, Petitclerc A, & Perlman SB (2020). The Early Childhood Irritability-Related Impairment Interview (E-CRI): A novel method for assessing young Children’s Developmentally Impairing Irritability. Behavior Therapy, 51(2), 294–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Roberts MY, Flynn RM, Smith JD, Krogh-Jespersen S, Kaat AJ, Gray L, Walkup J, Marino BS, Norton ES, & Davis MM (2019). Future directions for early childhood prevention of mental disorders: A road map to mental health, earlier. Journal of Clinical Child and Adolescent Psychology, 48(3), 539–554. 10.1080/15374416.2018.1561296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Tolan PH, & Leventhal BL (2010). Research Review: ‘Ain’t misbehavin’: Towards a developmentally-specified nosology for preschool disruptive behavior. Journal of Child Psychology and Psychiatry, 51(1), 3–22. 10.1111/j.1469-7610.2009.02184.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson R, van der Ark LA, Lin LC, Fieo R, Deary IJ, & Meijer RR (2012). Item response theory: How Mokken scaling can be used in clinical practice. Journal of Clinical Nursing, 21, 2736–2746. 10.1111/j.1365-2702.2011.03893.x [DOI] [PubMed] [Google Scholar]
- Willoughby MT, Wylie AC, & Blair CB (2019). Using repeated-measures data to make stronger tests of the association between executive function skills and attention deficit/hyperactivity disorder symptomatology in early childhood. Journal of Abnormal Child Psychology, 47(11), 1759–1770. 10.1007/s10802-019-00559-w [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.