Abstract
INTRODUCTION.
Among people with lower extremity peripheral artery disease (PAD), little is known about variation in response to supervised exercise therapy (SET). Clinical characteristics associated with greater responsiveness to SET have not been identified.
METHODS.
Data from participants with PAD in two randomized clinical trials comparing SET vs. non-exercising control were combined. The exercise intervention consisted of three times weekly supervised treadmill exercise. The control groups received lectures on health-related topics.
RESULTS.
Of 309 unique participants randomized (mean age 67.9 (standard deviation (SD) =9.3), 132 (42.7%) women, 185 (59.9%) black), 285 (92%) completed six-month follow-up. Compared to control, those randomized to SET improved six-minute walk distance by 35.6 meters (95% confidence interval (CI) = +21.4,+49.8, P<0.001). In the 95 (62.1%) participants who attended at least 70% of SET sessions, change in six-minute walk distance varied from 149.4 to +356.0 meters. Thirty-four (35.8%) had no six-minute walk distance improvement. Among all participants, age, sex, race, body mass index, prior lower extremity revascularization and other clinical characteristics did not affect the degree of improvement in six-minute walk distance after SET, relative to the control group. Participants with six-minute walk distance less than the median of 334 meters at baseline had greater percent improvement in six-minute walk distance compared to those with baseline six-minute walk distance above the median (+20.5% vs. +5.3%, P for interaction= 0.0107).
CONCLUSIONS.
Among people with PAD, substantial variability exists in walking improvement after SET. Shorter 6-minute walk distance at baseline was associated with greater improvement after SET, but other clinical characteristics, including age, sex, prior lower extremity revascularization, and disease severity, did not affect responsiveness to exercise therapy.
TABLE OF CONTENTS SUMMARY.
In a randomized study of 309 patients with peripheral artery disease (PAD) shorter six-minute walk distance at baseline was associated with greater improvement after supervised exercise therapy (SET). Age, sex, history of revascularization and PAD severity did not affect response to SET, suggesting that no patients with PAD should be excluded from SET referral.
Supervised treadmill exercise therapy (SET) significantly improves walking distances in people with lower extremity peripheral artery disease (PAD) and is recommended by clinical practice guidelines as first line therapy to improve walking impairment in people with PAD (1-7). While SET consistently improves mean walking distance in people with PAD, little is known about the degree of variability in improved walking distance following SET or about the proportion of people with PAD who participate in SET but do not improve their walking distance. Little is known about characteristics of people with PAD, such as older age, sex, or disease severity, that are associated with better vs. poorer response to SET. Defining the degree of variability in response to SET and identifying clinical characteristics that are associated with poorer response to SET will help clinicians better counsel patients with PAD and select the most optimal therapy for patients with PAD.
In this study, data were combined from two randomized clinical trials of supervised treadmill exercise therapy in PAD (6,7) to address the following primary specific aims. First, to describe the degree of variability in improvement in walking distance in response to SET in people with PAD. Second, to identify clinical characteristics associated with greater or lesser response to a supervised treadmill exercise intervention, relative to a control group. Additional analyses limited to participants randomized to SET studied the effects of age, sex, race, and other clinical characteristics on the degree of walking improvement following SET.
METHODS
Overview
Data from two randomized clinical trials of SET in participants with PAD were combined for analyses. The two studies were the Study in Leg Circulation (SILC) and the PROgenitor cell release Plus Exercise to improve functional performance in PAD: (the PROPEL Trial) (6,7). All participants provided written informed consent.
Summary of included trials
Methods for each trial have been published (6,7) and are summarized here. In SILC, 156 participants with PAD were randomized to one of three groups: supervised treadmill exercise, supervised lower extremity resistance training, or attention control for six months. Participants randomized to supervised resistance training were excluded from analyses reported here, since the current analyses focused on supervised treadmill exercise training (6). In PROPEL, 210 participants with PAD were randomized to one of four groups: SET + granulocyte macrophage colony stimulating factor (GM-CSF), SET + placebo, GM-CSF + attention control, or placebo + attention control. For PROPEL, participants randomized to GM-CSF were included, since the effect of GM-CSF was found to be clinically insignificant (7).
Participant Identification
In both trials, participants were identified from Chicago-area medical centers, through newspaper or radio advertisements, or from mailings to older people living in the Chicago area (5,6). People with PAD who previously participated in research with the principal investigator (MMM) and expressed interest in future research were contacted.
Inclusion criteria
The two studies had an inclusion criterion of ankle brachial index (ABI) ≤ 0.90 and ABI ≤ 0.95, respectively (6–8). In PROPEL, potential participants with an ABI > 0.90 at the baseline visit were eligible, if a hospital-affiliated vascular laboratory report or angiogram demonstrated PAD (7). In PROPEL, participants with an ABI of 0.90–1.00 at baseline and those with a normal ABI and prior lower extremity revascularization were eligible if their ABI dropped by 20% after a heel-rise test, consisting of fifty heel rises at a rate of one per second followed by repeat ABI (9).
Exclusion criteria
Potential participants with a below or above-knee amputation, wheelchair confinement, walking impairment for a reason other than PAD, foot ulcer or critical limb ischemia, or significant visual or hearing impairment were excluded (6,7). Both trials excluded potential participants who used a walking aid other than a cane. Both trials included a run-in, in which participants were asked to attend an exercise session and a control group session within a three week period, to demonstrate willingness and ability to participate in the intervention. Those who did not complete the run-in successfully were excluded. The same run-in criteria were required for both trials. Potential participants with major surgery, revascularization, or cardiac rehabilitation participation during the previous 3 months or planned during the next 6 months were excluded. People requiring oxygen with activity were excluded. Potential participants for whom exercise may be unsafe and those at risk for health deterioration were excluded. Those with a Mini-Mental Status Examination score < 23 were excluded (10).
MEASURES
The same methods were used in the two included trials for measurement of the ankle brachial index (ABI), six-minute walk distance, treadmill walking, questionnaire administration, and body mass index measurement and calculation.
Ankle-brachial index (ABI)
A handheld Doppler probe (Nicolet Vascular Pocket Dop II, Golden, CO) was used to measure systolic blood pressures in the right brachial, dorsalis pedis, and posterior tibial arteries and left dorsalis pedis, posterior tibial, and brachial arteries as previously described (8,11,12).
Six-Minute Walk Test
Six-minute walk distance is a well validated measure of walking endurance that predicts mortality, cardiovascular events, and mobility loss in people with PAD (13–17). Following a standardized protocol (6,7,13–17), participants walked up and down a 100-foot hallway for 6 minutes after instructions to cover as much distance as possible during the six-minutes. The distance completed after 6 minutes was recorded. Among participants with PAD, a small clinically meaningful change was defined as 12 meters and a large clinically meaningful change was defined as 34 meters (18).
Treadmill walking performance
Maximal treadmill walking distance was measured using the Gardner-Skinner protocol (6,7,19). Participants were not allowed to grip handrails. Participants began walking at 2.0 miles per hour at zero percent grade. Grade was increased two percent every two minutes. Participants unable to walk at 2.0 miles/hour began walking at 0.50 miles per hour (6,7,19), and treadmill speed was increased by 0.50 miles/hour every two minutes until 2.0 miles per hour was achieved. Subsequently, grade was increased two percent every two minutes. Protocols dictated that the same stress test (i.e. Gardner or modified Gardner) was performed at baseline and follow-up.
INTERVENTIONS
Supervised treadmill exercise therapy
The same SET protocol was used in both randomized trials. Participants attended exercise sessions three times weekly with an exercise physiologist for six months (6,7). Walking exercise time was increased during the intervention to 50 minutes/session, not including rest periods.
Control group
Participants in both trials randomized to the control group were asked to attend one-hour educational sessions led by Northwestern faculty and staff once per week for six months. Example topics in these sessions were nutrition, cancer screening, and immunizations.
Study injections in PROPEL
PROPEL participants were randomized to either granulocyte macrophage colony stimulating factor (GM-CSF) or placebo injected subcutaneously 3 times per week for the first 2 weeks after randomization, in a double-blinded manner (7).
Other Measures
Medical history, race, and demographics were obtained using patient report (6,7). Height and weight were measured. Body mass index (BMI) was calculated as weight (kg)/(height (meters))2.
Statistical analyses
Characteristics of participants randomized to SET vs. control were compared using analysis of variance and statistical tests of trend. Generalized linear models were used to compare 6-month changes in six-minute walk distance and maximal treadmill walking time between PAD participants randomized to SET vs. control. Models adjusted for study and whether the intervention included GM-CSF. Analyses were repeated in the subset of participants who attended at least 70% of exercise or attention control sessions. Tests for interaction were performed to determine the effects of the following clinical characteristics: age, sex, race, ABI > 0.65 vs. ABI < 0.65, presence vs. absence of specific comorbidities, BMI > 30 vs. < 30 kg/M2, current smoking status, prior lower extremity revascularization, adherence to study intervention sessions (both SET and attention control group sessions) and baseline walking performance (six-minute walk distance ≥334 vs. <334 meters and maximal treadmill walking time ≥6.3 vs. < 6.3 minutes) on change in six-minute walk distance and change in maximal treadmill walking time, respectively, relative to the control group. In analyses limited to participants randomized to exercise, the magnitude of improvement in six-minute walk distance and maximal treadmill walking time were evaluated according to the presence vs. absence of these baseline clinical characteristics, using linear and logistic regression models, adjusting for baseline six-minute walk distance and baseline maximal treadmill walking time, respectively. A p value of <0.05 was considered statistically significant, since the purpose of these post-hoc analyses was to increase sensitivity for identifying clinical characteristics that may influence responsiveness to SET in people with PAD.
RESULTS
361 unique people with PAD were randomized (205 in PROPEL and 156 in SILC). Of these, 52 participants randomized to resistance training in SILC were excluded, leaving 309 participants for analyses (153 randomized to exercise and 156 to control). Baseline characteristics of participants are shown in Table 1. Mean adherence to intervention sessions was 70.9% for participants randomized to SET and 69.7% for those randomized to control. Participants who attended <70% of their study intervention sessions were younger (66.7 years (standard deviation (SD):9.3 vs. 68.7, SD: 9.2, P=0.049), had a higher prevalence of prior lower extremity revascularization (38.5% vs. 27.1%, P=0.037) and a higher baseline maximal treadmill walking time (6.7 minutes, SD:4.5 vs. 7.7 minutes, SD: 4.5, P=0.047), than those who attended 70% or more of their SET sessions. Of the 309 randomized, 285 (92.2%) completed 6-month follow-up testing.
Table 1:
Baseline Characteristics of Participants with Peripheral Artery Disease
| Supervised Treadmill Exercise Therapy (SET) (N=153) | Attention Control (N=156) | |
|---|---|---|
| Age (years) | 68.31 (9.12) | 67.56 (9.50) |
| Female sex, N (%) | 66 (43.14) | 66 (42.31) |
| Black race, N (%) | 87 (56.86) | 98 (62.82) |
| Ankle brachial index | 0.66 (0.18) | 0.66 (0.18) |
| Body mass index (kg/M2) | 30.46 (6.31) | 30.33 (6.92) |
| Current smoker, N (%) | 51 (33.33) | 47 (30.13) |
| Diabetes mellitus, N (%) | 56 (36.60) | 62 (39.74) |
| Coronary artery disease, N (%) | 48 (31.37) | 39 (25.00) |
| Pulmonary disease, N (%)* | 15 (9.80) | 22 (14.29) |
| Heart failure, N (%)* | 13 (8.61) | 25 (16.03) |
| Classic Intermittent Claudication Symptoms, N (%) | 54 (35.29) | 47 (30.13) |
| Asymptomatic, N (%) | 8 (5.23) | 6 (3.85) |
| Prior lower extremity revascularization, N (%) | 50 (32.68) | 47 (30.13) |
| Baseline six minute walk distance (meters) | 335.28 (96.47) | 332.15 (92.58) |
| Baseline treadmill walking time (minutes) | 7.22 (4.85) | 7.46 (4.12) |
Unless otherwise specified, data shown are means and (standard deviations).
There are 2 participants in the Attention Control group missing baseline pulmonary disease data; there are 2 participants in the SET group missing baseline heart failure data.
Mean absolute changes in six-minute walk distance were +28.2 meters in the SET group vs. –7.4 meters in the control group (mean difference: +35.6 meters (95% Confidence Interval (CI) = 21.4, 49.8, P<0.001)). The mean percent change in six-minute walk distance was +12.4% in the SET group vs. −1.1% in the control group (mean difference: +13.5% (95% CI: 7.6%, 19.5%), P<0.001). Mean absolute changes in maximal treadmill walking time were +4.5 minutes in the SET group vs. +0.6 minutes in the control group (mean difference: +3.9 minutes (95% Confidence Interval (CI) = 3.1, 4.8, P<0.001)). Mean percent changes in maximal treadmill walking time were +101.4% in the SET group vs. 13.9% in the control group (mean difference: +87.5% (95% CI: 64.5%, 110.5%), P<0.001).
Change in six-minute walk distance and maximal treadmill walking time at 6-month follow-up varied substantially between participants (Table 2). For example, six-month change in six-minute walk distance ranged from −149.4 to +356.0 meters in the SET group and from −316.1 to +147.2 meters in the control group. Variability in change in maximal treadmill walking time ranged from –7.8 to +21.0 minutes in the SET group and from –7.8 to +12.6 minutes in the control group (Table 2). Results were similar when analyses were limited to participants who attended at least 70% of intervention sessions (Table 2).
Table 2.
Variation in change in six-minute walk distance and treadmill walking performance in people with PAD randomized to supervised treadmill exercise or control
| Group | N | Range of 6-month change in six-minute walk | Range of 6-month change in maximal treadmill walking time | Number (%) of participants with any improvement in six-minute walk | Number (%) of participants with any improvement in maximal treadmill walking time |
|---|---|---|---|---|---|
| Entire Cohort | |||||
| Supervised exercise therapy | 141 | −149 to +356 | −7.8 to 21.0 | 94 (66.7%) | 127 (91.4%) |
| Control | 142 | −316 to +147 | −7.8 to 12.6 | 67 (47.2%) | 76 (55.5%) |
| Subset of participants adherent to at least 70% of intervention sessions | |||||
| Supervised exercise therapy | 93 | −149 to +356 | −7.8 to +21.0 | 61 (65.6%) | 86 (92.5%) |
| Control | 95 | −118 to +137 | −7.8 to +12.6 | 49 (51.6%) | 51 (54.8%) |
Of 141 participants with PAD who were randomized to SET and had six-minute walk distance data at baseline and six-month follow-up, 47 (33.3%) declined in six-minute walk distance at six-month follow-up. PAD participants who declined in six-minute walk distance after SET had significantly higher baseline six-minute walk distance compared to those who did not decline after SET (375.4 meters (SD: 94.0) vs. 317.8 meters (SD: 91.0), P<0.01). Of 139 participants with PAD who were randomized to SET and had treadmill testing at baseline and six month follow-up, 12 (8.6%) declined in maximal treadmill walking time at six-month follow-up. Participants who declined in maximal treadmill walking time after SET had higher baseline treadmill walking time compared those who did not decline after SET (10.4 minutes (SD: 5.7) vs. 6.82 minutes (SD: 4.5)), P=0.01). There were no other baseline differences in characteristics of people who were randomized to SET and declined in six-minute walk distance or maximal treadmill walking time.
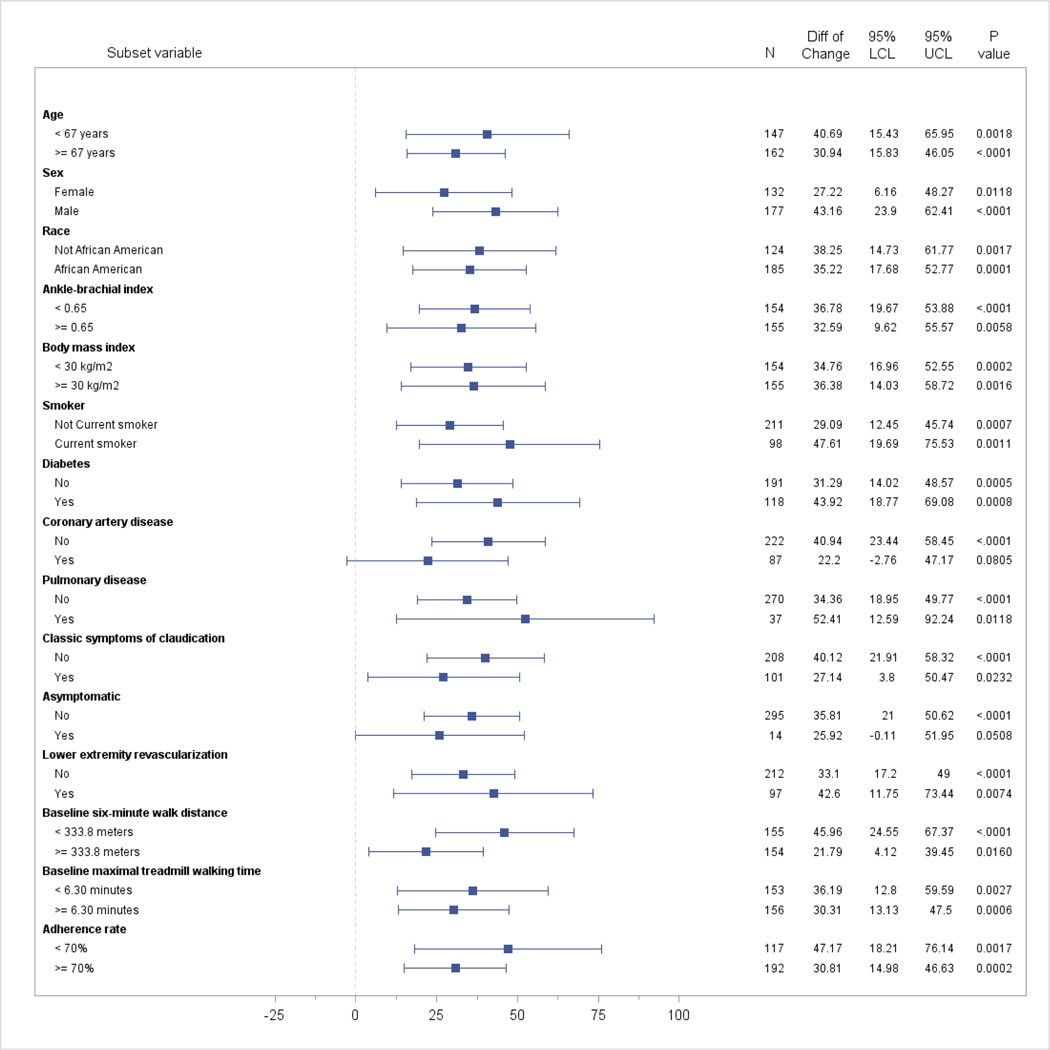
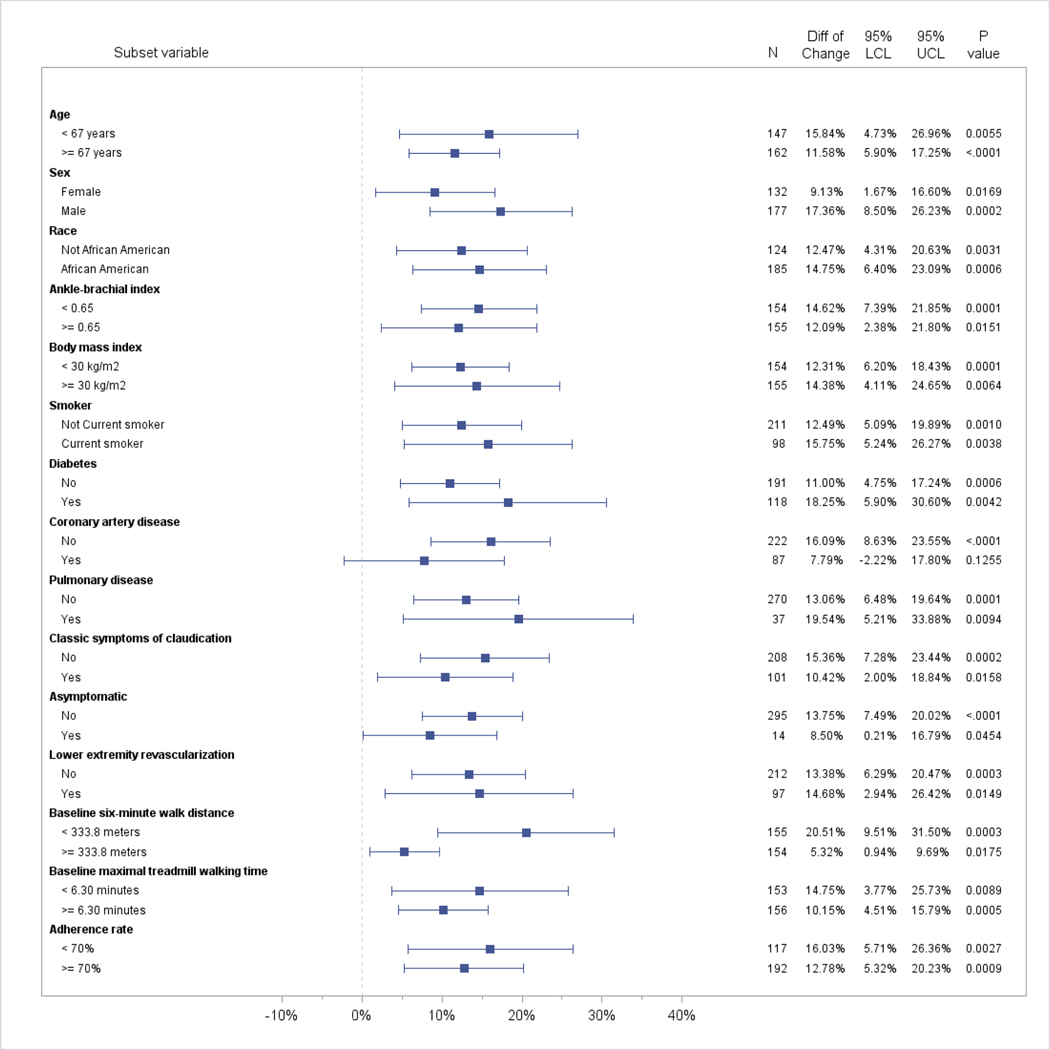
Based on statistical tests for interaction, relative to the control group, there were no significant differences in the degree of improvement in six-minute walk distance according to whether the participant was above or below the median age at baseline (≤ 67 vs. >67 years), or according to sex (male vs. female), race (black vs. white), median baseline ABI (≤0.65 vs. >0.65), median baseline BMI (≤30.0 kg/M2 vs. >30 kg/M2), presence vs. absence of specific comorbidities, smoking status (current smoker vs. not current smoker), leg symptoms (asymptomatic vs. not asymptomatic and classical intermittent claudication vs. not classical intermittent claudication), prior lower extremity revascularization vs. no prior revascularization, adherence to study intervention sessions (<70% vs. ≥70%) or above vs. below baseline median treadmill walking distance (<6.3 minutes vs. ≥ 6.3 minutes) (Table 3, Figure 1). However, relative to the control group, participants with a baseline six-minute walk distance below the median (i.e. <334 meters at baseline) had significantly greater improvement in percent change in six-minute walk distance at 6-month follow-up, compared to those with baseline six-minute walk distance above the median (i.e. ≥ 334 meters at baseline) (20.5% improvement vs. 5.3% improvement, P for interaction = 0.0107) (Figure 1b). Within each defined subgroup, participants randomized to SET had significantly greater improvement in absolute and percent change in six-minute walk distance relative to the control group, except that the 14 participants who were asymptomatic (i.e. reported no exertional leg symptoms) and the 82 participants with history of coronary artery disease did not significantly improve absolute or percent change in six-minute walk distance following SET, relative to control (Table 3, Figure 1). The lack of improvement in six-minute walk distance among those with no exertional leg symptoms and among those with coronary artery disease may have been due to small sample size.
Table 3:
Effects of clinical characteristics on change in six-minute walk distance and maximal treadmill walking time in response to supervised treadmill exercise vs. control in people with PAD*
| Subgroup | Change in six minute walk distance (meters) in the exercise group relative to the control group (changes by subgroup) | Change in maximal treadmill walk time (minutes) in the exercise group relative to the control group (changes by subgroup) | ||||||
|---|---|---|---|---|---|---|---|---|
| Absolute change | Percentage change | Absolute change | Percentage change | |||||
| Absolute change difference, (95% CI) | P value for interaction | Percentage change difference, (95% CI) | P value for interaction | Absolute change difference, (95% CI) | P value for interaction | Percentage change difference, (95% CI) | P value for interaction | |
| Age ≥67 vs. <67 years | −10.3 (−38.9, 18.4) | 0.48 | −4.8% (−16.8%, 7.3%) | 0.43 | +1.5 (−0.2, 3.3) | 0.084 | 2.0% (−44.2%, 48.2%) | 0.93 |
| Females vs. males | +15.8 (−12.8, 44.4) | 0.28 | 8.1% (−3.9%, 20.1%) | 0.18 | −0.5 (−2.2, 1.3) | 0.60 | 14.6% (−32.0%, 61.1%) | 0.54 |
| Blacks vs. whites | −1.1 (−30.3, 28.0) | 0.94 | 2.9% (−9.4%, 15.2%) | 0.64 | −0.7 (−2.5, 1.1) | 0.42 | 1.8% (−45.5%, 49.1%) | 0.94 |
| Ankle brachial index ≥0.65 vs. <0.65 | −4.0 (−32.5, 24.4) | 0.78 | −2.6% (−14.6%, 9.5%) | 0.68 | −0.3 (−2.1, 1.4) | 0.72 | −47.6% (−92.8%, −2.3%) | 0.039 |
| Body mass index (≥30 vs. <30 kg/m 2 ) | +1.5 (−27.1, 30.0) | 0.92 | 2.0% (−10.0%, 14.0%) | 0.74 | −1.8 (−3.5, −0.1) | 0.036 | −33.1% (−79.1%, 13.0%) | 0.16 |
| Current smoker | 20.9 (−10.4, 52.2) | 0.19 | 3.6% (−9.6%, 16.9%) | 0.59 | −0.2 (−2.1, 1.7) | 0.86 | 16.4% (−34.5%, 67.3%) | 0.53 |
| Diabetes | 12.6 (−16.8, 42.0) | 0.40 | 7.2% (−5.2%, 19.6%) | 0.25 | 1.4 (−0.4, 3.2) | 0.12 | 42.4% (−5.0%, 89.9%) | 0.080 |
| Coronary artery disease | −18.0 (−49.9, 13.8) | 0.27 | −8.0% (−21.4%, 5.4%) | 0.24 | −1.7 (−3.6, 0.2) | 0.082 | −38.5% (−89.2%, 12.2%) | 0.14 |
| Pulmonary disease | 19.3 (−26.8, 65.5) | 0.41 | 7.0% (−12.5%, 26.5%) | 0.48 | −1.3 (−4.1, 1.4) | 0.34 | −31.4% (−105.4%, 42.6%) | 0.40 |
| Heart Failure | −43.2 (−91.8, 5.4) | 0.081 | −14.9% (−35.4%, 5.6%) | 0.15 | 0.4 (−2.5, 3.2) | 0.81 | 0.3% (−76.1%, 76.7%) | 0.99 |
| Classic symptoms of intermittent claudication | −13.1 (−43.4, 17.3) | 0.40 | −5.0% (−17.8%, 7.8%) | 0.44 | 1.4 (−0.5, 3.2) | 0.15 | 27.3% (−21.6%, 76.3%) | 0.27 |
| Asymptomatic (report of no exertional leg symptoms) | 2.3 (−63.9, 68.6) | 0.95 | −1.8% (−29.8%, 26.1%) | 0.90 | −0.1 (−4.3, 4.1) | 0.96 | −63.9% (−175.0%, 47.1%) | 0.26 |
| History of lower extremity revascularization | 9.1 (−22.2, 40.3) | 0.57 | 1.0% (−12.1%, 14.2%) | 0.88 | −0.1 (−2.0, 1.8) | 0.92 | 26.2% (−24.4%, 76.8%) | 0.31 |
Figure 1a. Absolute change in six-minute walk distance between the supervised treadmill exercise vs. control groups, according to baseline characteristics.
*Groups for age, ankle brachial index, and body mass index were defined according to the baseline median value for each variable. P values shown represent the within-group statistical significance of change in the supervised exercise therapy group, relative to control.
Figure 1b. Percent change in six-minute walk distance between the supervised treadmill exercise vs. control groups, according to baseline characteristics.
*Groups for age, ankle brachial index, and body mass index were defined according to the baseline median value for each variable. P values shown represent the within-group statistical significance of change in the supervised exercise therapy group, relative to control.
**Point estimates represent the difference in change in six-minute walk distance between the SET and control groups at 6-month follow-up. Groups for age, ankle brachial index, and body mass index were defined according to the baseline median value for each variable. P values shown represent the within-group statistical significance of change in the supervised exercise therapy group, relative to control.
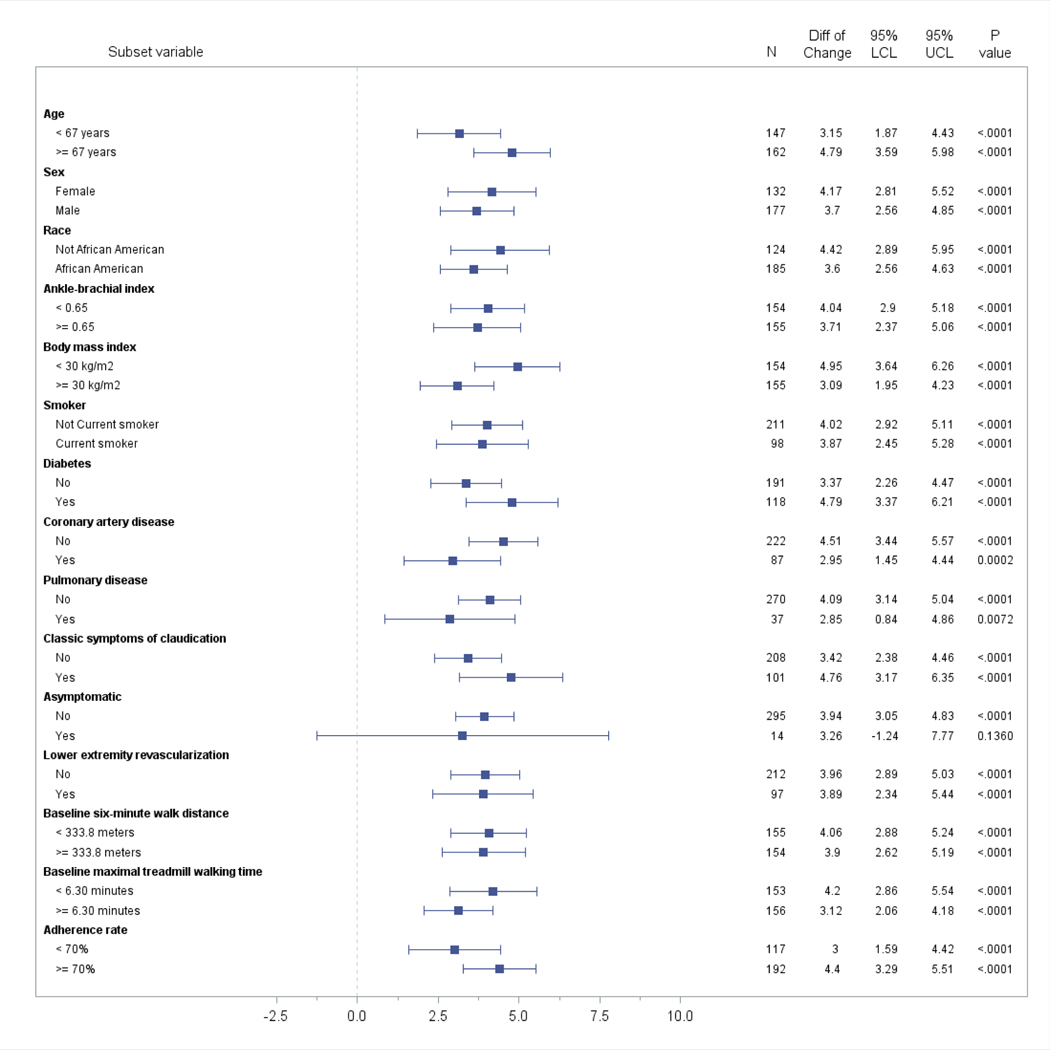
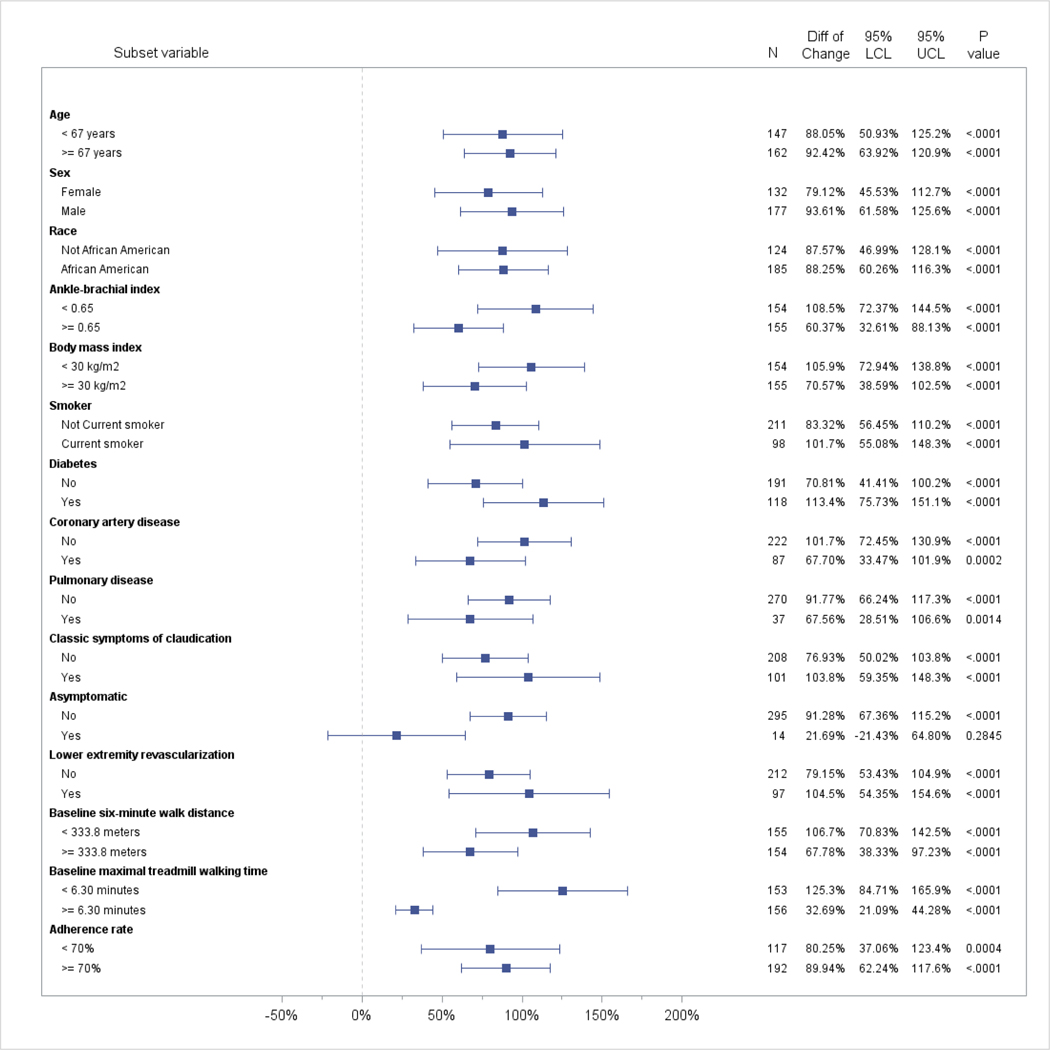
Based on statistical tests for interaction, relative to the control group, there were no significant differences in the degree of improvement in maximal treadmill walking distance by baseline age (<67 vs.≥ 67 years), sex (male vs. female), race (black vs. white), baseline ABI (≤0.65 vs. >0.65), comorbidities, smoking status, leg symptoms, prior lower extremity revascularization, adherence to study interventions (<70% vs. ≥70%), or baseline six-minute walk distance (Table 3, Figure 2). However, participants with a baseline BMI below the median (< 30 kg/M2) had a significantly greater absolute improvement in maximal treadmill walking time at 6-month follow-up, compared to those with BMI above the median (≥ 30 kg/M2) (4.95 vs. 3.09 minutes, P for interaction=0.036). In addition, participants with a baseline treadmill walking time below the median (i.e. < 6.3 minutes) had significantly greater improvement in percent change in maximal treadmill walking time at 6-month follow-up, compared to those with a higher maximal treadmill walking time at baseline (125.3% improvement in treadmill walking time vs. 32.7% improvement in treadmill walking time, P for interaction < 0.001) (Figure 2b). Within each defined subgroup, participants randomized to SET had significantly greater improvement in absolute and percent change in maximal treadmill walking time relative to the control group, except that the 14 participants who were asymptomatic did not significantly improve absolute or percent change in maximal treadmill walking time following SET, relative to the control group, perhaps due to small sample size (Table 3, Figure 1).
Figure 2a. Absolute change in treadmill walking time between the supervised treadmill exercise vs. control groups, according to baseline characteristics.
*Groups for age, ankle brachial index, and body mass index were defined according to the baseline median value for each variable. P values shown represent the within-group statistical significance of change in the supervised exercise therapy group, relative to control.
Figure 2b. Percent change in treadmill walking time between the supervised treadmill exercise vs. control groups, according to baseline characteristics.
*Groups for age, ankle brachial index, and body mass index were defined according to the baseline median value for each variable. P values shown represent the within-group statistical significance of change in the supervised exercise therapy group, relative to control.
* Point estimates represent the difference in change in treadmill walking time between the SET and control groups at 6-month follow-up. Groups for age, ankle brachial index, and body mass index were defined according to the baseline median value for each variable. P values shown represent the within-group statistical significance of change in the supervised exercise therapy.
In analyses limited to participants randomized to SET, men had significantly greater improvement in six-minute walk distance than women (+36.4 vs. +14.8, P=0.036) (Table 4). However, because women randomized to the control group had twice the rate of decline in six-minute walk distance compared to men randomized to the control group (Table 4), there was no statistically significant interaction for sex on the response to SET. Women and men randomized to SET, respectively, had significant improvement in six-minute walk distance relative to the control group (Table 4, Figure 1).
Table 4.
Change in six-minute walk distance within groups of participants randomized to exercise and control, respectively
| N | Baseline six-minute walk, mean (STD) | 6-month six-minute walk, mean (STD) | Within group change in six-minute walk distance, mean (95% CI) | Between group change in six-minute walk distance, mean (95% CI) | P value | |
|---|---|---|---|---|---|---|
| Age | ||||||
| Participants randomized to exercise | ||||||
| ≤ 67 years | 64 | 345.84 (98.83) | 379.52 (90.67) | 33.69 (18.69, 48.68) | Reference | 0.2154 |
| > 67 years | 77 | 329.63 (92.91) | 350.54 (86.54) | 20.91 (7.23, 34.58) | −12.78 (−33.07, 7.52) | |
| Participants randomized to control | ||||||
| ≤ 67 years | 78 | 356.42 (85.57) | 348.18 (102.30) | −8.24 (−21.87, 5.39) | Reference | 0.9427 |
| > 67 years | 64 | 310.84 (95.24) | 301.87 (94.66) | −8.98 (−24.02, 6.07) | −0.74 (−21.04, 19.56) | |
| Sex | ||||||
| Participants randomized to exercise | ||||||
| Female | 63 | 336.95 (91.52) | 351.71 (86.96) | 14.76 (−0.20, 29.72) | Reference | 0.0355 |
| Male | 78 | 337.01 (99.44) | 373.37 (90.54) | 36.36 (22.92, 49.81) | 21.60 (1.49, 41.72) | |
| Participants randomized to control | ||||||
| Female | 59 | 301.72 (83.88) | 289.27 (94.33) | −12.46 (−28.10, 3.20) | Reference | 0.5225 |
| Male | 83 | 360.16 (91.22) | 354.34 (97.76) | −5.81 (−19.01, 7.38) | 6.64 (−13.83, 27.10) | |
| Race | ||||||
| Participants randomized to exercise | ||||||
| Not African American | 61 | 349.32 (91.40) | 373.48 (87.92) | 24.17 (8.73, 39.61) | Reference | 0.6667 |
| African American | 80 | 327.58 (98.28) | 356.23 (90.17) | 28.64 (15.16, 42.12) | 4.47 (−16.02, 24.97) | |
| Participants randomized to control | ||||||
| Not African American | 52 | 331.12 (104.54) | 319.61 (118.14) | −11.52 (−28.20, 5.16) | Reference | 0.6615 |
| African American | 90 | 338.62 (85.39) | 331.75 (90.51) | −6.87 (−19.55, 5.81) | 4.65 (−16.30, 25.60) | |
| ABI | ||||||
| Participants randomized to exercise | ||||||
| ≤ 0.65 | 76 | 303.09 (80.29) | 336.46 (75.07) | 33.36 (19.62, 47.11) | Reference | 0.1607 |
| > 0.65 | 65 | 376.62 (97.45) | 395.54 (94.49) | 18.93 (4.07, 33.79) | −14.44 (−34.68, 5.80) | |
| Participants randomized to control | ||||||
| ≤ 0.65 | 66 | 313.48 (84.31) | 309.45 (91.50) | −4.03 (−18.81, 10.75) | Reference | 0.4075 |
| > 0.65 | 76 | 355.33 (95.52) | 342.81 (107.22) | −12.52 (−26.29, 1.26) | −8.49 (−28.69, 11.71) | |
| BMI | ||||||
| Participants randomized to exercise | ||||||
| ≤ 30 kg/m2 | 64 | 359.93 (92.15) | 384.13 (82.80) | 24.20 (9.13, 39.27) | Reference | 0.6567 |
| > 30 kg/m2 | 77 | 317.91 (94.86) | 346.71 (91.44) | 28.79 (15.05, 42.53) | 4.60 (−15.80, 24.99) | |
| Participants randomized to control | ||||||
| ≤ 30 kg/m2 | 74 | 359.99 (88.60) | 349.56 (100.67) | −10.42 (−24.41, 3.56) | Reference | 0.7054 |
| > 30 kg/m2 | 68 | 309.64 (90.22) | 303.09 (96.92) | −6.55 (−21.14, 8.04) | 3.87 (−16.34, 24.08) | |
| Current smoker | ||||||
| Participants randomized to exercise | ||||||
| No | 96 | 341.06 (101.56) | 365.49 (92.59) | 24.43 (12.13, 36.72) | Reference | 0.5176 |
| Yes | 45 | 328.29 (81.99) | 359.86 (82.71) | 31.57 (13.61, 49.53) | 7.14 (−14.62, 28.91) | |
| Participants randomized to control | ||||||
| No | 103 | 326.90 (92.82) | 322.79 (102.68) | −4.11 (−15.88, 7.67) | Reference | 0.1549 |
| Yes | 39 | 359.59 (88.74) | 339.23 (97.71) | −20.36 (−39.49, −1.22) | −16.25 (−38.72, 6.22) | |
DISCUSSION
Among 309 people with PAD randomized into a clinical trial of SET, there was wide variation in degree of change in six-minute walking distance and maximal treadmill walking time following SET. Despite this variability in response to SET, most clinical characteristics, including age, sex, race, PAD severity, comorbidities, presence of baseline leg symptoms, and prior lower extremity revascularization did not significantly affect the degree of improvement in six-minute walk distance or treadmill walking time following SET, relative to the control group. Compared to participants with baseline six-minute walk distance above the median value of 334 meters, baseline six-minute walk distance below the median of 334 meters value was associated with significantly greater percent change improvement but not with greater absolute improvement in six-minute walk distance following SET, relative to the control group. Compared to participants with maximal treadmill walking time above the median value at baseline (6.3 minutes), those with maximal treadmill walking time below the median had significantly greater improvement in percent change in treadmill walking time, relative to the control group. In addition, compared to participants with baseline BMI values above the median value of 30 kg/M2 at baseline, participants with baseline BMI values below the median had greater improvement in maximal absolute treadmill walking time, relative to the control group. Despite these three statistical interactions, within each subgroup evaluated (i.e. those with baseline BMI above and below the median, those with baseline absolute treadmill walking time above and below the median, and those with six-minute walk distance above vs. below the median) there were statistically significant improvements in six-minute walk distance and treadmill walking time within each of these subgroups, relative to the control group.
The clinical implications of these results are as follows. First, clinicians should advise people with PAD that the degree of responsiveness to SET varies between individuals. Second, clinicians should monitor patients with PAD for responsiveness to exercise interventions since, in general, patient characteristics (such as age, sex, race, history of revascularization or severity of PAD) did not identify patients more likely to respond favorably. Clinicians can potentially monitor response to SET by performing a six-minute walk test at clinic visits, since a six-minute walk test can be performed in the clinician’s office relatively easily and inexpensively. Patients with PAD who do not show improvement in six-minute walk distance after 6 months of SET could be evaluated for alternative therapies. Third, based on results reported here, clinicians could advise patients with PAD that people with higher baseline walking ability (i.e. a baseline six-minute walk distance > 333.8 meters or a baseline maximal treadmill walking time of > 6.3 minutes) may have a more modest response to SET than patients with poorer baseline walking performance. However, even participants within these higher categories of baseline walking performance significantly improved six-minute walk distance and maximal treadmill walking time in response to SET, relative to a control group.
Prior studies of older people without PAD also demonstrated variability in response to exercise interventions that was not explained by age, sex, or race (21–25). However, to our knowledge, no prior studies have evaluated the degree of change in six-minute walk distance and treadmill walking distance according to baseline clinical characteristics in a large number of participants with PAD.
This study has limitations. First, individuals who were unable or unwilling to attend on-site supervised exercise sessions three times a week were excluded, thereby reducing the generalizability of the results. Second, this study focused on supervised treadmill exercise therapy. Further study is needed to determine whether these findings apply to home-based exercise therapy in PAD. However, prior trials of home exercise reported that baseline characteristics of study participants did not affect response to home-based exercise (25,26). Third, the exercise interventions in this study were six months duration. These results may not apply to exercise interventions of shorter or longer duration. Fourth, data were not available on effort expended during exercise activities. Fifth, multiple comparisons were made to evaluate the effects of multiple participant characteristics on response to SET. Analyses were not pre-specified and no adjustments were made for multiple comparisons. Further study is needed to confirm our findings regarding the effects of baseline walking performance on response to SET. Sixth, our analyses assessing whether prior history of lower extremity revascularization affected the degree of improvement in walking performance in response to SET is pertinent to individuals with lower extremity revascularization at least three months previously. However, these clinical trial data could not assess whether combining lower extremity revascularization with SET improves walking performance more than SET alone. This question has been evaluated in prior randomized trials (27,28). Seventh, we did not collect data on location of lower extremity atherosclerosis.
In conclusion, substantial variability in responsiveness to SET exists among people with PAD. However, clinical characteristics do not appear to identify which patients with PAD are more likely to respond to SET. Further research is needed to determine whether biologic markers can identify patients who are more likely to have a significant improvement in walking ability following an exercise intervention.
Table 3:
Clinical characteristics and effects on change in six-minute walk distance and maximal treadmill walking time in participants with PAD randomized to supervised treadmill exercise vs. control (continued)
| Subgroup | Change in six minute walk distance (meters) | Maximal treadmill walk time (minutes) | ||||||
|---|---|---|---|---|---|---|---|---|
| Absolute change | Percentage change | Absolute change | Percentage change | |||||
| Absolute change difference, (95% CI) | P value for interaction | Percentage change difference, (95% CI) | P value for interaction | Absolute change difference, (95% CI) | P value for interaction | Percentage change difference, (95% CI) | P value for interaction | |
| Baseline six-minute walk distance (≥334 vs. <334 meters) | −24.0 (−51.4, 3.4) | 0.086 | −15.0% (−26.5%, −3.5%) | 0.011 | −0.1 (−1.9, 1.6) | 0.88 | −38.3% (−84.2%, 7.7%) | 0.10 |
| Baseline maximal treadmill walking time (≥6.3 vs. <6.3 minutes) | −5.1 (−33.6, 23.5) | 0.73 | −4.3% (−16.3%, 7.6%) | 0.48 | −1.0 (−2.7, 0.7) | 0.24 | −91.1% (−131.7%, −50.6) | <.001 |
| Adherence to study intervention sessions (≥70% vs. ≤70%) | −15.8 (−45.8, 14.3) | 0.30 | −2.9% (−15.7%, 9.8%) | 0.65 | 1.4 (−0.4, 3.3) | 0.14 | 9.4% (−40.0%, 58.8%) | 0.71 |
Data shown represent changes in six-minute walk distance or treadmill walking time in participants randomized to exercise relative to the control group by subgroup. For example, in the first row of data, participants age 67 and older randomized to supervised exercise therapy gained 10.3 meters less and 4.8% less on the six-minute walk test relative to control compared to participants less than age 67. However, these differences between those age 67 and older vs. those less than age 67 were not statistically significant, since the p value for interaction was not < 0.05.
Table 4.
Associations of clinical characteristics with change in six-minute walk among participants randomized to exercise and control, respectively (continued)
| N | Baseline six-minute walk, mean (STD) | 6-month six-minute walk, mean (STD) | Change of six-minute walk within group, mean (95% CI) | Change of six-minute walk between groups, mean (95% CI) | P value | |
|---|---|---|---|---|---|---|
| Diabetes | ||||||
| Participants randomized to exercise | ||||||
| No | 90 | 344.64 (95.69) | 369.88 (90.96) | 25.24 (12.53, 37.95) | Reference | 0.7043 |
| Yes | 51 | 323.48 (94.98) | 352.78 (86.08) | 29.30 (12.42, 46.19) | 4.07 (−17.07, 25.20) | |
| Participants randomized to control | ||||||
| No | 87 | 345.48 (91.75) | 340.77 (103.27) | −4.71 (−17.57, 8.16) | Reference | 0.3414 |
| Yes | 55 | 320.69 (92.66) | 306.01 (95.05) | −14.69 (−30.86, 1.49) | −9.98 (−30.65, 10.69) | |
| Coronary artery disease | ||||||
| Participants randomized to exercise | ||||||
| No | 97 | 348.03 (95.13) | 377.05 (80.97) | 29.02 (16.79, 41.25) | Reference | 0.5042 |
| Yes | 44 | 312.65 (93.27) | 334.25 (100.18) | 21.61 (3.45, 37.77) | −7.42 (−29.31, 14.48) | |
| Participants randomized to control | ||||||
| No | 106 | 338.60 (91.89) | 327.44 (101.38) | −11.15 (−22.81, 0.51) | Reference | 0.3858 |
| Yes | 36 | 327.86 (95.40) | 326.90 (102.35) | −0.97 (−20.97, 19.04) | 10.19 (−12.97, 33.35) | |
| Pulmonary disease | ||||||
| Participants randomized to exercise | ||||||
| No | 128 | 340.13 (94.78) | 364.15 (88.77) | 24.02 (13.46, 34.59) | Reference | 0.1003 |
| Yes | 13 | 306.07 (102.45) | 359.20 (98.00) | 53.13 (19.99, 86.27) | 29.10 (−5.68, 63.89) | |
| Participants randomized to control | ||||||
| No | 122 | 339.19 (95.47) | 329.47 (105.63) | −9.72 (−20.68, 1.23) | Reference | 0.6458 |
| Yes | 18 | 315.01 (73.40) | 312.40 (72.68) | −2.61 (−31.12, 25.91) | 7.12 (−23.43, 37.66) | |
| Heart failure | ||||||
| Participants randomized to exercise | ||||||
| No | 129 | 336.88 (95.07) | 364.46 (89.73) | 27.58 (16.98, 38.18) | Reference | 0.2952 |
| Yes | 10 | 364.54 (95.46) | 371.12 (86.85) | 6.58 (−31.49, 44.65) | −21.00 (−60.52, 18.52) | |
| Participants randomized to control | ||||||
| No | 122 | 340.26 (94.36) | 328.99 (104.40) | −11.27 (−22.10, −0.44) | Reference | 0.1910 |
| Yes | 20 | 309.11 (77.51) | 317.02 (80.93) | 7.91 (−18.84, 34.66) | 19.18 (−9.68, 48.04) | |
| Symptoms of classic intermittent claudication | ||||||
| Participants randomized to exercise | ||||||
| No | 90 | 335.65 (96.76) | 364.28 (87.69) | 28.63 (15.92, 41.34) | Reference | 0.6196 |
| Yes | 51 | 339.34 (94.54) | 362.66 (92.94) | 23.31 (6.43, 40.19) | −5.32 (−26.45, 15.81) | |
| Participants randomized to control | ||||||
| No | 98 | 337.71 (95.71) | 327.62 (105.07) | −10.09 (−22.24, 2.06) | Reference | 0.6584 |
| Yes | 44 | 331.80 (86.08) | 326.61 (93.38) | −5.20 (−23.33, 12.94) | 4.89 (−16.94, 26.72) | |
| Asymptomatic (no exertional leg symptoms) | ||||||
| Participants randomized to exercise | ||||||
| No | 133 | 333.81 (94.36) | 361.64 (88.79) | 27.83 (17.40, 38.26) | Reference | 0.3741 |
| Yes | 8 | 389.72 (108.00) | 397.80 (96.95) | 8.08 (−34.46, 50.62) | −19.75 (−63.55, 24.05) | |
| Participants randomized to control | ||||||
| No | 136 | 334.68 (93.15) | 326.90 (102.42) | −7.78 (−18.08, 2.52) | Reference | 0.4597 |
| Yes | 6 | 362.97 (80.33) | 336.40 (76.34) | −26.57 (−75.61, 22.47) | −18.79 (−68.90, 31.32) | |
Table 4.
Associations of clinical characteristics with change in six-minute walk among participants randomized to exercise and control, respectively (continued)
| N | Baseline six-minute walk, mean (STD) | 6-month six-minute walk, mean (STD) | Change of six-minute walk within group, mean (95% CI) | Change of six-minute walk between groups, mean (95% CI) | P value | |
|---|---|---|---|---|---|---|
| Lower extremity revascularization | ||||||
| Participants randomized to exercise | ||||||
| No | 97 | 347.03 (89.77) | 371.99 (78.87) | 24.97 (12.73, 37.21) | Reference | 0.6151 |
| Yes | 44 | 314.85 (105.17) | 345.40 (107.60) | 30.55 (12.38, 48.72) | 5.58 (−16.33, 27.50) | |
| Participants randomized to control | ||||||
| No | 101 | 344.36 (93.43) | 337.15 (99.11) | −7.21 (−19.18, 4.76) | Reference | 0.6756 |
| Yes | 41 | 314.98 (88.06) | 303.05 (103.64) | −11.93 (−30.72, 6.85) | −4.73 (−27.00, 17.55) | |
| Baseline six-minute walk | ||||||
| Participants randomized to exercise | ||||||
| ≤ 333.8 meters | 73 | 265.23 (57.68) | 313.00 (72.66) | 47.77 (34.60, 60.94) | Reference | <0.0001 |
| > 333.8 meters | 68 | 414.02 (62.51) | 418.11 (72.00) | 4.10 (−9.55, 17.75) | −43.67 (−62.64, −24.70) | |
| Participants randomized to control | ||||||
| ≤ 333.8 meters | 64 | 255.02 (57.65) | 257.23 (79.58) | 2.21 (−12.64, 17.05) | Reference | 0.0549 |
| > 333.8 meters | 78 | 402.22 (55.50) | 384.81 (78.50) | −17.41 (−30.86, −3.96) | −19.62 (−39.65, 0.42) | |
| Baseline maximal treadmill walking time | ||||||
| Participants randomized to exercise | ||||||
| ≤6.30 minutes | 75 | 305.80 (84.70) | 340.26 (83.37) | 34.46 (20.66, 48.26) | Reference | 0.1069 |
| > 6.30 minutes | 66 | 372.42 (95.59) | 390.32 (88.93) | 17.90 (3.19, 32.61) | −16.56 (−36.73, 3.62) | |
| Participants randomized to control | ||||||
| ≤6.30 minutes | 62 | 297.74 (77.45) | 294.29 (85.46) | −3.45 (−18.69, 11.80) | Reference | 0.3774 |
| > 6.30 minutes | 80 | 365.44 (92.93) | 352.89 (105.56) | −12.54 (−25.96, 0.88) | −9.10 (−29.41, 11.21) | |
Table 5.
Associations of clinical characteristics with change in maximal treadmill walking time among participants randomized to exercise and control, respectively
| N | Baseline maximal treadmill walking time, mean (STD) | 6-month maximal treadmill walking time, mean (STD) | Within group change in maximal treadmill walking time, mean (95% CI) | Between group change in maximal treadmill walking time, mean (95% CI) | P value | |
|---|---|---|---|---|---|---|
| Age | ||||||
| Participants randomized to exercise | ||||||
| ≤ 67 years | 64 | 6.58 (4.74) | 10.89 (5.14) | 4.31 (3.26, 5.35) | Reference | 0.6561 |
| > 67 years | 75 | 7.60 (4.58) | 12.22 (5.78) | 4.63 (3.66, 5.59) | 0.32 (−1.10, 1.74) | |
| Participants randomized to control | ||||||
| ≤ 67 years | 76 | 7.40 (3.69) | 8.47 (4.34) | 1.08 (0.42, 1.74) | Reference | 0.0259 |
| > 67 years | 61 | 7.58 (4.08) | 7.53 (4.14) | −0.05 (−0.79, 0.69) | −1.13 (−2.12, −0.14) | |
| Sex | ||||||
| Participants randomized to exercise | ||||||
| Female | 65 | 6.82 (4.28) | 11.54 (5.60) | 4.72 (3.69, 5.76) | Reference | 0.5234 |
| Male | 74 | 7.40 (5.00) | 11.67 (5.48) | 4.26 (3.29, 5.24) | −0.46 (−1.88, 0.96) | |
| Participants randomized to control | ||||||
| Female | 57 | 6.94 (4.04) | 7.49 (4.41) | 0.55 (−0.22, 1.33) | Reference | 0.9453 |
| Male | 80 | 7.86 (3.70) | 8.45 (4.14) | 0.59 (−0.07, 1.25) | 0.04 (−0.98, 1.05) | |
| Race | ||||||
| Participants randomized to exercise | ||||||
| Not African American | 60 | 8.15 (4.98) | 13.04 (6.30) | 4.88 (3.81, 5.96) | Reference | 0.3255 |
| African American | 79 | 6.35 (4.29) | 10.52 (4.59) | 4.17 (3.23, 5.11) | −0.71 (−2.14, 0.72) | |
| Participants randomized to control | ||||||
| Not African American | 50 | 8.46 (4.72) | 9.05 (5.10) | 0.59 (−0.33, 1.42) | Reference | 0.9582 |
| African American | 87 | 6.92 (3.14) | 7.48 (3.61) | 0.56 (−0.07, 1.20) | −0.03 (−1.07, 1.02) | |
| ABI | ||||||
| Participants randomized to exercise | ||||||
| ≤ 0.65 | 75 | 5.51 (3.25) | 10.24 (4.15) | 4.73 (3.77, 5.70) | Reference | 0.4475 |
| > 0.65 | 64 | 9.03 (5.34) | 13.21 (6.45) | 4.18 (3.14, 5.23) | −0.55 (−1.97, 0.87) | |
| Participants randomized to control | ||||||
| ≤ 0.65 | 64 | 6.44 (3.51) | 7.11 (4.05) | 0.67 (−0.06, 1.40) | Reference | 0.7273 |
| > 0.65 | 73 | 8.39 (3.94) | 8.89 (4.30) | 0.49 (−0.20, 1.18) | −0.18 (−1.18, 0.83) | |
| BMI | ||||||
| Participants randomized to exercise | ||||||
| ≤ 30 kg/m2 | 62 | 7.43 (5.00) | 12.98 (5.97) | 5.55 (4.52, 6.58) | Reference | 0.0068 |
| > 30 kg/m2 | 77 | 6.89 (4.40) | 10.50 (4.88) | 3.62 (2.69, 4.55) | −1.93 (−3.32, −0.54) | |
| Participants randomized to control | ||||||
| ≤ 30 kg/m2 | 70 | 8.16 (4.26) | 8.78 (4.79) | 0.62 (−0.08, 1.33) | Reference | 0.8462 |
| > 30 kg/m2 | 67 | 6.77 (3.27) | 7.30 (3.52) | 0.52 (−0.19, 1.24) | −0.10 (−1.10, 0.91) | |
| Current smoker | ||||||
| Participants randomized to exercise | ||||||
| No | 95 | 7.72 (4.94) | 12.27 (5.91) | 4.55 (3.69, 5.40) | Reference | 0.7881 |
| Yes | 44 | 5.84 (3.76) | 10.18 (4.28) | 4.34 (3.08, 5.60) | −0.21 (−1.73, 1.32) | |
| Participants randomized to control | ||||||
| No | 99 | 7.65 (3.99) | 8.27 (4.39) | 0.62 (0.03, 1.21) | Reference | 0.7794 |
| Yes | 38 | 7.03 (3.50) | 7.49 (3.93) | 0.46 (−0.49, 1.41) | −0.16 (−1.28, 0.96) | |
Table 5.
Associations of clinical characteristics with change in maximal treadmill walking time among participants randomized to exercise and control, respectively (continued)
| N | Baseline maximal treadmill walking time, mean (STD) | 6-month maximal treadmill walking time, mean (STD) | Within group change in maximal treadmill walking time, mean (95% CI) | Between group change in maximal treadmill walking time, mean (95% CI) | P value | |
|---|---|---|---|---|---|---|
| Diabetes | ||||||
| Participants randomized to exercise | ||||||
| No | 87 | 7.47 (5.13) | 11.83 (5.85) | 4.36 (3.46, 5.25) | Reference | 0.6591 |
| Yes | 52 | 6.56 (3.75) | 11.25 (4.94) | 4.68 (3.53, 5.84) | 0.33 (−1.14, 1.79) | |
| Participants randomized to control | ||||||
| No | 85 | 7.69 (4.19) | 8.70 (4.59) | 1.01 (0.38, 1.63) | Reference | 0.0286 |
| Yes | 52 | 7.13 (3.26) | 7.00 (3.45) | −0.13 (−0.93, 0.67) | −1.14 (−2.15, −0.12) | |
| Coronary artery disease | ||||||
| Participants randomized to exercise | ||||||
| No | 94 | 7.26 (5.15) | 12.30 (5.83) | 5.04 (4.19, 5.89) | Reference | 0.0233 |
| Yes | 45 | 6.86 (3.50) | 10.17 (4.53) | 3.31 (2.09, 4.54) | −1.73 (−3.22, −0.24) | |
| Participants randomized to control | ||||||
| No | 102 | 7.59 (4.07) | 8.17 (4.32) | 0.58 (−0.003, 1.16) | Reference | 0.9793 |
| Yes | 35 | 7.15 (3.18) | 7.72 (4.13) | 0.56 (−0.43, 1.56) | −0.02 (−1.17, 1.14) | |
| Pulmonary disease | ||||||
| Participants randomized to exercise | ||||||
| No | 126 | 7.25 (4.77) | 11.84 (5.53) | 4.59 (3.85, 5.33) | Reference | 0.3422 |
| Yes | 13 | 5.91 (3.48) | 9.33 (5.01) | 3.42 (1.10, 5.73) | −1.17 −3.60, 1.26) | |
| Participants randomized to control | ||||||
| No | 118 | 7.63 (3.93) | 8.17 (4.37) | 0.55 (0.007, 1.09) | Reference | 0.9534 |
| Yes | 18 | 6.78 (3.33) | 7.37 (3.63) | 0.59 (−0.79, 1.98) | 0.04 (−1.44, 1.53) | |
| Heart failure | ||||||
| Participants randomized to exercise | ||||||
| No | 126 | 6.92 (4.53) | 11.55 (5.51) | 4.63 (3.90, 5.36) | Reference | 0.6563 |
| Yes | 11 | 9.05 (6.06) | 13.10 (5.81) | 4.05 (1.59, 6.51) | −0.58 (−3.14, 1.98) | |
| Participants randomized to control | ||||||
| No | 118 | 7.70 (4.00) | 8.41 (4.35) | 0.71 (0.17, 1.25) | Reference | 0.1823 |
| Yes | 19 | 6.12 (2.52) | 5.85 (2.92) | −0.27 (−1.61, 1.07) | −0.98 −2.42, 0.47) | |
| Symptoms of classic intermittent claudication | ||||||
| Participants randomized to exercise | ||||||
| No | 88 | 7.66 (4.88) | 11.80 (5.49) | 4.14 (3.25, 5.02) | Reference | 0.2100 |
| Yes | 51 | 6.22 (4.16) | 11.29 (5.60) | 5.07 (3.90, 6.23) | 0.93 (−0.53, 2.40) | |
| Participants randomized to control | ||||||
| No | 95 | 7.48 (3.71) | 8.21 (4.22) | 0.73 (0.13, 1.33) | Reference | 0.3660 |
| Yes | 42 | 7.48 (4.22) | 7.71 (4.40) | 0.23 (−0.67, 1.13) | −0.50 −1.58, 0.59) | |
| Asymptomatic (no exertional leg symptoms) | ||||||
| Participants randomized to exercise | ||||||
| No | 131 | 6.72 (4.26) | 11.21 (5.16) | 4.50 (3.76, 5.23) | Reference | 0.8544 |
| Yes | 8 | 13.86 (6.16) | 18.07 (7.40) | 4.21 (1.25, 7.17) | −0.28 (−3.33, 2.76) | |
| Participants randomized to control | ||||||
| No | 132 | 7.47 (3.87) | 8.05 (4.30) | 0.58 (0.07, 1.09) | Reference | 0.9319 |
| Yes | 5 | 7.70 (3.89) | 8.17 (3.45) | 0.46 (−2.17, 3.09) | −0.12 (−2.79, 2.56) | |
Table 5.
Associations of clinical characteristics with change in maximal treadmill walking time among participants randomized to exercise and control, respectively (continued)
| N | Baseline maximal treadmill walking time, mean (STD) | 6-month maximal treadmill walking time, mean (STD) | Within group change in maximal treadmill walking time, mean (95% CI) | Between group change in maximal treadmill walking time, mean (95% CI) | P value | |
|---|---|---|---|---|---|---|
| Lower extremity revascularization | ||||||
| Participants randomized to exercise | ||||||
| No | 96 | 7.30 (4.73) | 11.88 (5.71) | 4.58 (3.73, 5.43) | Reference | 0.6802 |
| Yes | 43 | 6.74 (4.57) | 11.00 (5.07) | 4.26 (2.98, 5.53) | −0.32 (−1.85, 1.21) | |
| Participants randomized to control | ||||||
| No | 97 | 8.05 (4.13) | 8.70 (4.30) | 0.65 (0.05, 1.24) | Reference | 0.6607 |
| Yes | 40 | 6.09 (2.67) | 6.49 (3.80) | 0.40 (−0.53, 1.33) | −0.25 (−1.35, 0.86) | |
| Baseline six-minute walk | ||||||
| Participants randomized to exercise | ||||||
| ≤ 333.8 meters | 73 | 5.18 (3.01) | 9.34 (4.09) | 4.16 (3.19, 5.14) | Reference | 0.3518 |
| > 333.8 meters | 66 | 9.28 (5.22) | 14.11 (5.83) | 4.83 (3.80, 5.86) | 0.67 (−0.75, 2.09) | |
| Participants randomized to control | ||||||
| ≤ 333.8 meters | 62 | 5.65 (2.83) | 5.78 (3.16) | 0.13 (−0.61, 0.87) | Reference | 0.1094 |
| > 333.8 meters | 75 | 8.99 (3.95) | 9.94 (4.16) | 0.94 (0.27, 1.62) | 0.81 (−0.19, 1.81) | |
| Baseline maximal treadmill walking time | ||||||
| Participants randomized to exercise | ||||||
| ≤6.30 minutes | 75 | 3.92 (1.46) | 9.50 (4.67) | 5.58 (4.66, 6.51) | Reference | 0.0007 |
| > 6.30 minutes | 64 | 10.89 (4.32) | 14.07 (5.44) | 3.19 (2.18, 4.19) | −2.40 (−3.76, −1.03) | |
| Participants randomized to control | ||||||
| ≤6.30 minutes | 59 | 4.17 (1.39) | 5.47 (3.27) | 1.30 (0.55, 2.05) | Reference | 0.0120 |
| > 6.30 minutes | 78 | 9.98 (3.18) | 10.01 (3.89) | 0.03 (−0.62, 0.68) | −1.28 (−2.27, −0.28) | |
ARTICLE HIGHLIGHTS.
Type of data.
Combined data from two randomized clinical trials.
Key Findings.
Among 306 participants with peripheral artery disease (PAD), there was substantial variability in six-minute walk distance improvement following supervised exercise therapy (SET). While age, sex, race, PAD severity, and prior revascularization did not affect response to SET, shorter six-minute walk distances at baseline were associated with significantly greater percent improvement in six-minute walk.
Take home message.
Among people with PAD, substantial variability exists in walking improvement after SET. These analyses further suggest that no patients should be excluded from SET referrals.
Footnotes
Clinical Trials Registration: NCT00106327 and NCT01408901
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, et al. 2016 AHA/ACC Guideline on the Management of Patients with Lower Extremity Peripheral Artery Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(12):e790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Society for Vascular Surgery Lower Extremity Guidelines Writing Group, Conte MS, Pomposelli FB, Clair DG, Geraghty PJ, McKinsey JF, et al. Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: management of asymptomaticdisease and claudication. J Vasc Surg 2015;61: 2S–41S. PMID: 25638515. [DOI] [PubMed] [Google Scholar]
- 3.Fakhry F, van de Luijtgaarden KM, Bax L, den Hoed PT, Hunink MG, Rouwet EV, et al. Supervised walking therapy in patients with intermittent claudication. J Vasc Surg. 2012;56(4):1132–42. [DOI] [PubMed] [Google Scholar]
- 4.McDermott MM, Kibbe MR. Improving Lower Extremity Functioning in Peripheral Artery Disease: Exercise, Endovascular Revascularization, or Both? JAMA. 2017;317(7):689–90. [DOI] [PubMed] [Google Scholar]
- 5.McDermott MM. Exercise rehabilitation for peripheral artery disease: A Review. J Cardiopulm Rehab 2018;38:63–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McDermott MM, Ades P, Guralnik JM, Dyer A, Ferrucci L, Liu K, et al. Treadmill exercise and resistance training in patients with peripheral arterial disease with and without intermittent claudication: a randomized controlled trial. JAMA 2009;301:165–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McDermott MM, Ferrucci L, Tian L, Guralnik JM, Lloyd-Jones D, Kibbe MR, et al. Effect of Granulocyte-Macrophage Colony-Stimulating Factor With or Without Supervised Exercise on Walking Performance in Patients with Peripheral Artery Disease: The PROPEL Randomized Clinical Trial JAMA 2017;318:2089–2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C, et al. American Heart Association Council on Peripheral Vascular Disease; Measurement and interpretation of the ankle-brachial index: A scientific statement from the American Heart Association. Circulation 2012;126:2890–909. [DOI] [PubMed] [Google Scholar]
- 9.Amirhamzeh MM, Chant JH, Rees JL, Hands LJ, Powell RJ, Campbell WB. A comparative study of treadmill tests and heel raising exercise for peripheral arterial disease. Eur J Vasc Endovasc Surg 1997; 13:301–305. [DOI] [PubMed] [Google Scholar]
- 10.Huen R, Papassotiropoulos A, Jennssen F. The validity of psychometric instruments for detection of dementia in the elderly general population. Int J Geriatr Psychiatry 1998;13:368–380. [DOI] [PubMed] [Google Scholar]
- 11.McDermott MM, Criqui MH, Liu K, Guralnik JM, Greenland P, Martin GJ, et al. Lower ankle/brachial index, as calculated by averaging the dorsalis pedis and posterior tibial arterial pressures, and association with leg functioning in peripheral arterial disease. J Vasc Surg 2000;32:1164–171. [DOI] [PubMed] [Google Scholar]
- 12.Shadman R, Criqui MH, Bundens WP, Fronek A, Denenberg JO, Gamst AC, et al. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol 2004; 44:618–23. [DOI] [PubMed] [Google Scholar]
- 13.McDermott MM, Greenland P, Liu K, Guralnik JM, Celic L, Criqui MH, et al. The ankle brachial index is associated with leg function and physical activity: the Walking and Leg Circulation Study. Ann Intern Med 2002;136:873–883. [DOI] [PubMed] [Google Scholar]
- 14.McDermott MM, Guralnik JM, Criqui MH, Liu K, Kibbe MR, Ferrucci L. Six-minute walk is a better outcome measure than treadmill walking tests in therapeutic trials of patients with peripheral artery disease. Circulation. 2014;130(1):61–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McDermott MM, Guralnik JM, Tian L, Ferrucci L, Liu K, Liao Y, et al. Baseline functional performance predicts the rate of mobility loss in persons with peripheral arterial disease. J Am Coll Card 2007;50:974–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McDermott MM, Greenland P, Tian L, Kibbe MR, Green D, Zhao L, et al. Association of 6minute walk performance and physical activity with incidence ischemic heart disease events and stroke in peripheral arterial disease. J Am Heart Assoc 2015;4(7). Pii: e001846. Doi: 10.1161/JAHA115.001846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDermott MM, Tian L, Liu K, Guralnik JM, Ferrucci L, Tan J, et al. Prognostic value of functional performance for mortality in patients with peripheral artery disease. J Am Coll Cardiol 2008;51(15):1482–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gardner AW, Montgomery PS, Wang M. Minimal clinically important differences in treadmill, 6-minute walk, and patient reported outcomes following supervised and home-based exercise in peripheral artery disease. Vasc Med 2018;23:349–357. Epub 2018 Apr 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gardner AW, Skinner JS, Cantwell BW, Smith LK. Progressive vs. single-stage treadmill tests for evaluation of claudication. Med Sci Sports Exerc 1991;23:402–408. [PubMed] [Google Scholar]
- 20.McDermott MM, Liu K, Greenland P, Guralnik JM, Criqui MH, Chan C, et al. Functional decline in peripheral arterial disease: associations with the ankle brachial index and leg symptoms. JAMA. 2004;292:453–461 [DOI] [PubMed] [Google Scholar]
- 21.Bouchard C, Rankinen T. Individual differences in response to regular physical activity. Med Sci Sports Exerc. 2001;33(6 Suppl):S446–51 [DOI] [PubMed] [Google Scholar]
- 22.Ahtiainen JP, Walker S, Peltonen H, Holviala J, Sillanpää E, Karavirta L, et al. Heterogeneity in resistance training-induced muscle strength and mass responses in men and women of different ages. Age. 2016;38(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karavirta L, Häkkinen K, Kauhanen A, Arija-Blazquez A, Sillanpää E, Rinkinen N, et al. Individual responses to combined endurance and strength training in older adults. Med Sci Sports Exerc. 2011;43(3):484–90. [DOI] [PubMed] [Google Scholar]
- 24.Bouchard C, Blair SN, Church TS, Earnest CP, Hagberg JM, Häkkinen K, et al. Adverse metabolic response to regular exercise: is it a rare or common occurrence? PLoS One. 2012;7(5):e37887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McDermott MM, Liu K, Guralnik JM, Criqui MH, Spring B, Tian L, et al. Home-Based Walking Exercise Intervention in Peripheral Artery Disease. A Randomized Clinical Trial. JAMA 2013;310:57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McDermott MM, Spring B, Berger JS, Treat-Jacobson D, Conte MS, Creager MA, et al. Effect of a Home-Based Exercise Intervention of Wearable Technology and Telephone Coaching on Walking Performance in Peripheral Artery Disease: The HONOR Randomized Clinical Trial. JAMA. 2018;319(16):1665–1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fakhry F, Spronk S, van der Laan L, Wever JJ, Teijink JA, Hoffman WH et al. Endovascular revascularization and supervised exercise for peripheral artery disease and intermittent claudication: A randomized clinical trial. JAMA 2015;314:1936–1944. [DOI] [PubMed] [Google Scholar]
- 28.Klaphake S, Buettner S, Ultee KH, van Rijn MJ, Hoeks SE, Verhagen HJ. Combination of endovascular revascularization and supervised exercise therapy for intermittent claudication: A systematic review and meta-analysis. J Cardiovasc Surg 2018;59:150–157. [DOI] [PubMed] [Google Scholar]