Abstract
Non-seminomatous germ cell tumors with structural components from all three cellular lineages are called teratomas. We report a rare case of a primary right adrenal teratoma in a postmenopausal female, presenting with abdominal pain. Ultrasound revealed a complex cystic shadow in the perihepatic region superior to the upper pole of the right kidney, which was suggestive of a complex supra-renal space-sequence-occupying lesion. Computerized tomography revealed a large-sized mature single multilobulated complex cystic lesion in the right hypochondrial lumbar region arising from the right adrenal gland. A right-sided transperitoneal adrenalectomy was performed. The resected mass (18 × 13 × 10 cm) was well encapsulated. Cut surfaces showed cystic mass filled with necrotic gray-white pultaceous material, along with a solid white gelatinous area. Microscopic sections showed a tumor which displayed differentiation along various tissue lineages. After immunohistochemical examinations, the tumor was confirmed to be a mature cystic teratoma. Mature teratomas show a good prognosis, and surgical resection and follow-up remain the standard approach.
Keywords: Adrenal teratoma, Mature cystic teratoma, Retroperitoneal mass, Germ cell tumor, Open adrenalectomy
Introduction
Teratomas are germ cell tumors having structural components from all three different cellular lineages. Teratomas may have different behavior, as they could be benign, well-differentiated cystic lesions (mature teratomas), or of indeterminate potential (immature teratomas), or as unequivocally malignant teratomas (usually admixed with another germ cell tumor component such as yolk sac tumor). They exhibit two peaks in incidence: the first at approximately 2 years of age and the second in late adolescence or early adulthood [1]. Teratomas usually originate from the gonads, but extragonadal tumors of the mediastinum, skull calvarium, sacrococcygeal spine, and retroperitoneum have been reported as well [2]. We report a rare case of a primary right adrenal teratoma in a 53-year-old female, presenting with abdominal pain. The preoperative diagnosis was primarily based on computerized tomography (CT) findings—heterogeneous lesion with fat components and scattered calcifications. A transperitoneal open adrenalectomy was performed.
Case Presentation
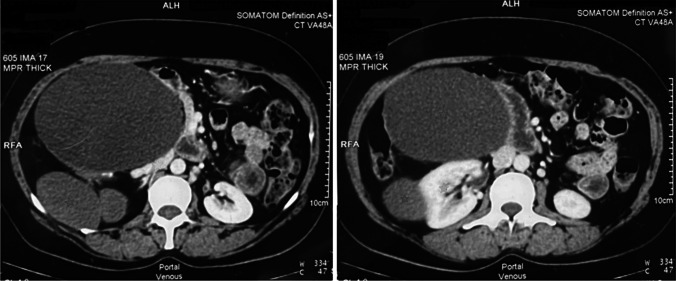
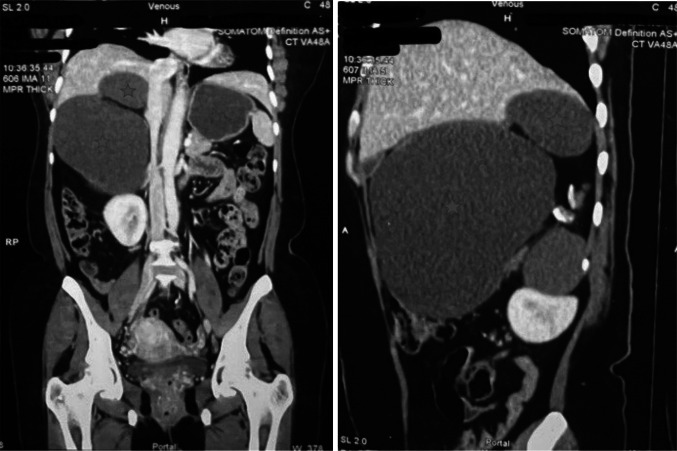
A 53-year-old female presented with complaints of pain in the abdomen for the last 6 months. Her general evaluation was essentially normal and non-conclusive. On abdominal examination, a firm and non-tender lump of size approximately 20 × 22 cm was palpated in the right hypochondrium, which did not move with respiration. Overnight dexamethasone suppression test revealed reduced cortisol levels, and urinary metanephrines and normetanephrines were within the normal range, thereby ruling out the possibility of Cushing’s syndrome or a pheochromocytoma. Contrast-enhanced computed tomography of the whole abdomen revealed a large-sized mature single multilobulated complex cystic lesion in the right hypochondrial lumbar region involving the right adrenal gland (Figs. 1 and 2). Ultrasonography of the whole abdomen revealed a complex cystic shadow in the perihepatic region superior to the upper pole of the right kidney, which was suggestive of a complex supra-renal space-sequence-occupying lesion.
Fig. 1.
Axial computerized tomography sections of the abdomen. Right retroperitoneal adrenal mass (red star), compressed inferior vena cava (green star), and the right kidney (sky-blue star)
Fig. 2.
Coronal (left) and sagittal (right) sections of computerized tomography of the abdomen. Adrenal mass in red star
The patient was planned for surgical resection, and a transperitoneal open adrenalectomy was conducted under general anesthesia. Intraoperative and preoperative course was uneventful with no history of fluctuation in blood pressure. A single right adrenal vein was clipped. The resected mass (18 × 13 × 10 cm) was sent for histopathological examination. The mass was described grossly as having a smooth outer surface and being well encapsulated. Cut surfaces of the tumor showed cystic spaces filled with necrotic gray-white pultaceous material. A zone of solid white gelatinous area was identified with no signs of normal adrenal parenchyma (Fig. 3).
Fig. 3.
Gross view of the resected specimen. The specimen measured 18.0 × 13.0 × 10.0 cm. The outer surface was nodular and well encapsulated. The cut surface showed multiple cysts filled with necrotic and pultaceous material with areas of fat and gelatinous material.
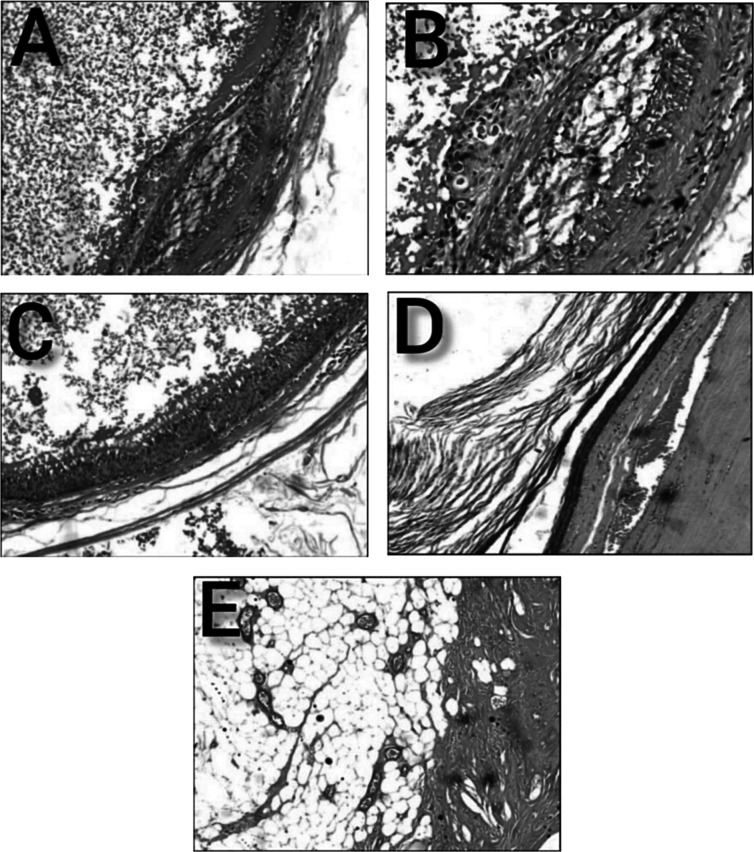
Microscopic sections showed a tumor which displayed differentiation along various tissue lineages. Multiple cystically dilated spaces were identified, lined by mature keratinizing stratified squamous and columnar epithelia. Scattered foci of lymphoid tissue and fibrocollagenous elements were also seen. The focal area showed a cluster of small cells with round hyperchromatic nuclei. No immature elements were identified in multiple sections after examination (Fig. 4). Immunohistochemistry findings were positive for pan-cytokeratin (CK), CK-7, and p40 in the lining epithelium, whereas leukocyte common antigen, synaptophysin, and chromogranin were negative. Hence, the tumor was confirmed to be a mature cystic teratoma.
Fig. 4.
Microphotographs of the mature cystic teratoma in the adrenal gland. A–B Whole of the adrenal gland was replaced by cystic spaces lined by mature ectodermal tissue composed of stratified squamous epithelium and unremarkable compressed adrenal parenchyma was seen at the periphery (hematoxylin and eosin ×50, ×100). C–D Mature stratified squamous epithelium with keratinous debris (hematoxylin and eosin ×100). E Areas of fibroadipose tissue (hematoxylin and eosin ×100)
Discussion
Teratomas are non-seminomatous germ cell tumors originating from totipotent germ cells, which include tissue structures from all three germ layers and they might be either malignant or benign. They account for only 4% of all primary teratomas and 0.13% of all adrenal tumors. Retroperitoneal lesions are rare and about 10–20% of these tumors occur in adults more than 30 years of age [2].
Our patient presented with a history of non-specific abdominal pain and fullness, and on palpation was found to have a right hypochondrial lump. An encased mass was visualized using CT, which was resected by an open transperitoneal adrenalectomy. The resected mass had components of fatty tissues, calcifications, and a few foci of lymphoid cells. PAN-CK, CK-7, and p40 were positive.
Teratomas usually do not present with any clinical manifestations, unless the tumor grows large enough to impinge onto major abdominal organs or vessels. Hence, the presenting range of clinical features is quite non-specific and may include abdominal discomfort, lumbar pain, nausea, weight loss, urinary retention, intestinal obstruction and even swelling of the lower limbs or genitalia following lymphatic obstruction. As a result, gross tumor dimensions can be directly correlated with the presenting complaints of the patient [3].
Adrenal hormone marker tests and nuclear medicine scans are of little value, due to inconclusive findings and their failure to distinguish from other tumors. It becomes imperative to evaluate computerized tomography and magnetic resonance imaging data to ensure the tumor’s location as well as its relationship to the surrounding organs and tissues [4]. It is very difficult to ascertain a benign tumor from a malignant one using radio-imaging techniques as they both show irregular marginalization and localized invasion with areas of uneven distribution of high density [5]. Malignant transformation and the size of the tumor have been found to have a direct relationship [6].
Surgical removal is the most preferable option, since teratomas show minimal response to chemotherapy and radiotherapy. The aim of surgery is to completely resect the tumor while preserving the adjacent organs. Laparoscopic adrenalectomy is the gold standard of treatment due to its minimal invasive small incision size, less blood loss, fewer complications, short hospital stay, and faster recovery. Both transperitoneal and retroperitoneal approaches are used in laparoscopic adrenalectomy. The retroperitoneal approach is preferred because it preserves the potency of the abdominal organs. The surgical procedure is complicated because mature adrenal teratomas are frequently entangled with vital blood vessels with thin walls, making complete resection extremely difficult. The complicating blood vessels should be resected, followed by end-to-end anastomosis, if necessary. Prognosis after excision is usually great; however, patients are still requested to appear for timely follow-ups in order to remove the incertitude of malignant transformations [3].
A review of the literature was conducted in PubMed using the keywords “adrenal” AND “teratoma[MeSH],” using filters for case reports, from which we selected studies in the English language reporting cases of adults. The search produced 12 results, which have been depicted in Table 1 [3, 7–17].
Table 1.
Results of the review of literature, which was conducted in PubMed using the keywords “adrenal” AND “teratoma[MeSH],” using filters for case reports, from which we selected studies in English language reporting cases in adults (F female, M male, NA not available, ? method of resection unclear, cm centimeters, + present, − absent, ↑ increase)
| Study no. | Study title | Authors (year of publication) | Case presentation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Sex/age | Side | Clinical features | Surgery | Tumor dimensions (cm) | Calcification, fat components | Lab markers | |||
| 1 | Primary adrenal teratoma: Clinical characteristics and retroperitoneal laparoscopic resection in five adults [7] | Li S et al (2015 Nov) | F/21 | Right | Incidentally discovered | Retroperitoneal laparoscopic adrenalectomy | 8.5 (mean diameter) | +, + | NA |
| F/16 | Right | Incidentally discovered | Retroperitoneal laparoscopic adrenalectomy | 9.0 (mean diameter) | +, + | NA | |||
| F/43 | Left | Incidentally discovered | Retroperitoneal laparoscopic adrenalectomy | 4.9 (mean diameter) | −, − | NA | |||
| F/49 | Left | Incidentally Discovered | Retroperitoneal laparoscopic adrenalectomy | 5.3 (mean diameter) | +, + | NA | |||
| F/51 | Right | Incidentally Discovered | Retroperitoneal laparoscopic adrenalectomy | 2.4 (mean diameter) | NA, NA | NA | |||
| 2 | Primary adrenal teratoma: A case series and review of the literature [3] | Zhou L et al (2018 Oct) | F/69 | Left | Abdominal mass | Retroperitoneal laparoscopic adrenalectomy | 10.0 × 6.0 × 4.0 | +, + | NA |
| F/29 | Left | Incidentally discovered | Retroperitoneal laparoscopic adrenalectomy | 2.5 × 2.1 × 0.5 | +, NA | NA | |||
| 3 | Primary adrenal teratoma: An unusual tumor - Challenges in diagnosis and surgical management [8] | Ramakant P et al (2018 Apr) | F/25 | Right | Abdominal pain, weight loss | Open transperitoneal adrenalectomy | 19 × 15 | +, + | NA |
| 4 | Clinical Characteristics and Surgical Management of Adult Adrenal Teratoma: A 15-year Experience and Systematic Review of the Literature [9] | Zhong W et al (2020 Jan) | F/59 | Left | Flank pain | Open transperitoneal adrenalectomy | 10.6 (maximum diameter) | +, + | NA |
| F/54 | Right | Asymptomatic | Open transperitoneal adrenalectomy | 10.2 (maximum diameter) | +, + | NA | |||
| F/22 | Right | Abdominal pain | Open transperitoneal adrenalectomy | 10.0 (maximum diameter) | +, + | NA | |||
| F/48 | Right | Asymptomatic | Retroperitoneal laparoscopic adrenalectomy | 9.6 (maximum diameter) | +, + | NA | |||
| M/26 | Right | Flank Pain | Retroperitoneal laparoscopic adrenalectomy | 4.0 (maximum diameter) | +, + | NA | |||
| F/18 | Right | Abdominal Pain | Retroperitoneal laparoscopic adrenalectomy | 8.8 (maximum diameter) | +, + | NA | |||
| F/55 | Left | Asymptomatic | Open transperitoneal adrenalectomy | 14.0 (maximum diameter) | −, + | NA | |||
| F/28 | Right | Asymptomatic | Retroperitoneal laparoscopic adrenalectomy | 4.5 (maximum diameter) | +, + | NA | |||
| F/29 | Right | Asymptomatic | Retroperitoneal laparoscopic adrenalectomy | 7.8 (maximum diameter) | +, + | NA | |||
| F/29 | Left | Asymptomatic | Retroperitoneal laparoscopic adrenalectomy | 7.0 (maximum diameter) | +, + | NA | |||
| F/72 | Right | Asymptomatic | Open transperitoneal adrenalectomy | 6.0 (maximum diameter) | −, − | NA | |||
| F/28 | Left | Asymptomatic | Open transperitoneal adrenalectomy | 9.5 (maximum diameter) | +, + | NA | |||
| F/41 | Left | Asymptomatic | Open transperitoneal adrenalectomy | 18.0 (maximum diameter) | +, + | NA | |||
| M/45 | Left | Asymptomatic | Retroperitoneal laparoscopic adrenalectomy | 6.8 (maximum diameter) | +, + | NA | |||
| 5 | Teratoma of the adrenal gland: clinical experience and literature review [10] | He C et al (2020 Aug) | F/17 | Right | Tuberculosis in upper and middle lobes of right lung, and upper lobe of left lung | Retroperitoneal laparoscopic adrenalectomy | 7.0 × 2.5 × 2.0 | +, + | NA |
| 6 | A giant primary retroperitoneal mature cystic teratoma in right adrenal region in a 39-year-old female [11] | Tang DD et al (2014 Jun) | F/39 | Right | Tender abdominal mass, dizziness, hypertension | ? Surgical resection | 22.5 × 17 × 7 | +, + | Anti-HBs (+), anti-HBc (+), CEA ↑, CA 19-9 ↑ |
| 7 | Retroperitoneal Adrenal Teratoma Presenting as Trichoptysis [12] | Bhatia V et al (2016 Jul) | F/24 | Left | Abdominal pain, cough with occasional expectoration of hairlike strands | ? Surgical resection with splenectomy | 7.6 × 6.5 (contrast-enhanced CT) | +, + | NA |
| 8 | Malignant Transformation of a mature teratoma of the adrenal gland: A rare case report and literature review [13] | Niu M et al (2017 Dec) | F/36 | Right | Incidentally discovered | Retroperitoneal laparoscopic adrenalectomy | 9.0 × 6.0 × 7.5 | +, + | Cortisol ↑, ACTH ↑, aldosterone ↑, vanillyl mandelic acid ↑ |
| 9 | Laparoscopic simultaneous resection of bilateral giant primary mature retroperitoneal teratoma of the adrenal region [14] | Wang J et al (2019 Oct) | F/22 | Right and left (bilateral) | Incidentally discovered | Retroperitoneal laparoscopic adrenalectomy | 10.4 × 10.1 × 13.2 (left), 12.3 × 10.5 × 12.5 (right) | −, + | NA |
| 10 | Adult Retroperitoneal Mature Cystic Teratoma Masquerading as Non-Endocrine Primary Adrenal Tumor [15] | Shakir FTZ et al (2021 Nov) | F/31 | Left | Food indigestion, abdominal pain, vomiting following meals | Exploratory laparotomy with complete mass excision | 7.9 × 7.9 × 9.7 | +, + | NA |
| 11 | Laparoscopic resection of a huge mature cystic teratoma of the right adrenal gland through retroperitoneal approach: a case report and literature review [16] | Li H et al (2015 Nov) | M/49 | Right | Incidentally discovered | Retroperitoneal laparoscopic adrenalectomy | 5.7 × 4.9 × 4.3 | +, + | NA |
| 12 | Adrenal Teratoma: a Case Series and Review of the Literature [17] | Kuo EJ et al (2017 Jan) | M/26 | Right | Abdominal pain | Open transperitoneal adrenalectomy | 8.5 × 5.5 × 4.8 | −, + | NA |
| F/29 | Left | Incidentally discovered | Retroperitoneal laparoscopic adrenalectomy | 2.5 × 2.1 × 0.5 | +, − | NA | |||
| F/24 | Left | Abdominal pain | Retroperitoneal laparoscopic adrenalectomy | 11.5 × 9 × 3 | −, + | NA | |||
Lab markers: plasma adrenocorticotrophic (ACTH) hormone, renin, angiotensin II, aldosterone, plasma cortisol, urinary catecholamines
Conclusions
Primary retroperitoneal teratomas rarely appear in adult patients and are usually asymptomatic. Symptoms (if present) arise as a result of compression of organs and adjoining vessels and resulting in radiating pain, which often leads to their detection. A differential diagnosis can be made preoperatively with the help of radiographic imaging modalities and a definitive one can be arrived at, via histopathological examination. Mature teratomas show a good prognosis, and surgical resection and follow-up remain the standard approach. Incomplete surgery in immature teratoma is the group at greatest risk of relapse.
Author Contribution
Patient treatment: K. G., A. A., A. A. S. First draft: U. S., S. R. All authors read and approved the final draft.
Data Availability
All data underlying the results are available as part of the article and no additional source data are required.
Declarations
Ethics Approval
Not applicable
Informed Consent
Written informed consent was taken to publish the patient data and photographs in an anonymous format.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kumar V, Abbas AK, Aster JC. Robbins and Cotran pathologic basis of disease. Philadelphia, PA: Elsevier/Saunders; 2015. [Google Scholar]
- 2.Bedri S, Erfanian K, Schwaitzberg S, Tischler AS. Mature cystic teratoma involving adrenal gland. Endocr Pathol. 2002;13(1):59–64. doi: 10.1385/ep:13:1:593. [DOI] [PubMed] [Google Scholar]
- 3.Zhou L, Pan X, He T, Lai Y, Li W, Hu Y, Ni L, Yang S, Chen Y, Lai Y. Primary adrenal teratoma: a case series and review of the literature. Mol Clin Oncol. 2018;9(4):437–442. doi: 10.3892/mco.2018.1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chuan-Yu S, Yat-Faat H, Wei-Hong D, Yuan-Cheng G, Qing-Feng H, Ke X, Bin G, Guo-Wei X. Laparoscopic adrenalectomy for adrenal tumors. Int J Endocrinol. 2014;2014:241854. doi: 10.1155/2014/241854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernini GP, Miccoli P, Moretti A, Vivaldi MS, Iacconi P, Salvetti A. Sixty adrenal masses of large dimensions: hormonal and morphologic evaluation. Urology. 1998;51(6):920–925. doi: 10.1016/s0090-4295(98)00026-0. [DOI] [PubMed] [Google Scholar]
- 6.Sturgeon C, Shen WT, Clark OH, Duh QY, Kebebew E. Risk assessment in 457 adrenal cortical carcinomas: how much does tumor size predict the likelihood of malignancy? J Am Coll Surg. 2006;202(3):423–430. doi: 10.1016/j.jamcollsurg.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 7.Li S, Li H, Ji Z, Yan W, Zhang Y. Primary adrenal teratoma: clinical characteristics and retroperitoneal laparoscopic resection in five adults. Oncol Lett. 2015;10(5):2865–2870. doi: 10.3892/ol.2015.3701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramakant P, Rana C, Singh KR, Mishra A. Primary adrenal teratoma: an unusual tumor - challenges in diagnosis and surgical management. J Postgrad Med. 2018;64(2):112–114. doi: 10.4103/jpgm.JPGM_588_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhong W, Ma R, Cheng S, Tian J, Wang H, Wang T, Zhang Z, Li X, Lu J, Ma L, Zhou L. Clinical characteristics and surgical management of adult adrenal teratoma: a 15-year experience and systematic review of the literature. Urology. 2020;135:71–75. doi: 10.1016/j.urology.2019.05.032. [DOI] [PubMed] [Google Scholar]
- 10.He C, Yang Y, Yang Y, Wang F, Hu J, Zhang J, Yin Y, Zeng L, Zhang T, Liu H. Teratoma of the adrenal gland: clinical experience and literature review. Gland Surg. 2020;9(4):1056–1064. doi: 10.21037/gs-20-648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tang DD, Zhang XS, Hao ZY, Zhou J, Liang CZ (2014) A giant primary retroperitoneal mature cystic teratoma in right adrenal region in a 39-year-old female. Int J Clin Exp Med 7(6):1611–1613 Available from https://pubmed.ncbi.nlm.nih.gov/25035788/. Accessed 2 Apr 2023 [PMC free article] [PubMed]
- 12.Bhatia V, Sharma S, Sood S, Mardi K, Venkat B. Case 231: retroperitoneal adrenal teratoma presenting as trichoptysis. Radiology. 2016;280(1):317–321. doi: 10.1148/radiol.2016140459. [DOI] [PubMed] [Google Scholar]
- 13.Niu M, Liu A, Zhao Y, Feng L. Malignant transformation of a mature teratoma of the adrenal gland: a rare case report and literature review. Medicine (Baltimore) 2017;96(45):e8333. doi: 10.1097/MD.0000000000008333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang J, Zhang J, Xiao C, Fan C. Laparoscopic simultaneous resection of bilateral giant primary mature retroperitoneal teratoma of the adrenal region: a case report. Medicine (Baltimore) 2019;98(44):e17836. doi: 10.1097/MD.0000000000017836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shakir FTZ, Sultan R, Siddiqui R, Shah MZ, Javed A. Adult retroperitoneal mature cystic teratoma masquerading as non-endocrine primary adrenal tumor. J Coll Physicians Surg Pak. 2021;31(11):1351–1353. doi: 10.29271/jcpsp.2021.11.1351. [DOI] [PubMed] [Google Scholar]
- 16.Li H, Zhao T, Wei Q, Yuan H, Cao D, Shen P, Liu L, Zeng H, Chen N. Laparoscopic resection of a huge mature cystic teratoma of the right adrenal gland through retroperitoneal approach: a case report and literature review. World J Surg Oncol. 2015;13:318. doi: 10.1186/s12957-015-0734-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuo EJ, Sisk AE, Yang Z, Huang J, Yeh MW, Livhits MJ. Adrenal teratoma: a case series and review of the literature. Endocr Pathol. 2017;28(2):152–158. doi: 10.1007/s12022-017-9468-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data underlying the results are available as part of the article and no additional source data are required.