Abstract
Malnutrition is more prevalent among children with cerebral palsy and a major factor for child morbidity and mortality in children with different co-morbidity, especially in Sub-Saharan Africa: The main aim of this systematic review and meta-analysis was to estimate the burden of malnutrition among children with cerebral palsy in Sub-Saharan Africa. We searched PubMed, Web of Science, Google Scholar, Research Gate, and institutional repositories for papers that reported the proportion of malnutrition among children with cerebral palsy that were published between December 2010 and September 2023. Data were retrieved using the standardized JBI data extraction checklist through Microsoft Excel, and then exported to STATA 17 for further analysis. DerSimonian and Laird’s estimator was used to calculate the pooled effect size in the random-effects model. Statistics such as the Cochran Q test and I2 test were employed to measure heterogeneity. Egger's test and the funnel plot were used to look for publication bias. This systematic review and meta-analysis used 16 studies from Sub-Saharan Africa to estimate the proportion of malnutrition among 2,120 children with cerebral palsy. The pooled proportion of malnutrition among children with cerebral palsy in Sub-Saharan Africa by using random-effects model analysis was found to be 59.7% (95% CI; 49.8–69.6). The proportion of malnutrition was also estimated by sample sizes categorized as ≤ 120 and > 120, and the proportion of malnutrition was found to be 54.0 (95% CI: 44.7–63.3) and 64.5 (95% CI: 50.5–78.5). Moreover, the proportion of malnutrition was estimated by accounting for the difference in the year of publication. In this regard, the study classified before ≤ 2017 and > 2017, and the proportion of malnutrition was found to be 53.7 (95% CI: 38.0–69.3) and 62.5 (95% CI: 49.7–75.3) in Sub-Saharan Africa respectively. Malnutrition among children with cerebral in Sub-Saharan Africa was found to be very high. Hence, enhancing and developing strategic guidelines for malnutrition screening, prevention, and nutritional support are crucial among children with cerebral palsy. Furthermore, systematic review, randomized control trials, and qualitative studies are recommended to understand the burden more among children with cerebral palsy in the continent.
Keywords: Children with cerebral palsy, Malnutrition, Sub-Saharan Africa
Subject terms: Molecular medicine, Neurology, Risk factors
Introduction
Cerebral palsy is a neurological disorder cause a lifelong physical disability1. With an estimated incidence of 17 million persons globally, cerebral palsy affects around 1 in 500 newborns2.
Children with cerebral palsy have a higher risk of developing malnutrition than other children because CP affects the muscles and movements involved in chewing, swallowing, and feeding3,4. It is a double burden for children with cerebral palsy to develop malnutrition since the problems are worsening each other and add challenges5,6.
The prevalence of malnutrition among children with cerebral palsy was 7.9–71.46%5,7, and malnutrition is more prevalent among children with cerebral palsy and a major factor for child morbidity and mortality in children with different co-morbidity, especially in Sub-Saharan Africa8.
Children with cerebral palsy are more susceptible to both the long- and short-term effects of malnutrition. Malnutrition lowers quality of life and social engagement, raises susceptibility to illness, and health care utilization, and lowers chances of survival5,6,9.
Therefore, malnutrition prevention, management, and nutritional support are very crucial and the stakeholders, government, and non-governmental organizations should be included in planning and implementing a package for children with cerebral palsy5,10,11.
Although some research has been done on the prevalence of malnutrition among children with cerebral palsy in Sub-Saharan Africa in the past, the combined frequency is not well understood. This systematic review and meta-analysis aimed to determine the pooled prevalence of malnutrition among children with cerebral palsy in Sub-Saharan Africa. This study may also draw new evidence from different heterogeneity of studies. Hence, this research is of paramount importance in providing evidence to policymakers, researchers, and clinicians to recognize the burden and can help the development of strategic guidelines, and enhance clinical decision-making and monitoring by integrating the recommendations of the study.
Methods
Data sources and search strategies
Review question
The review question of this systematic review and meta-analysis is: What is the burden of malnutrition among children with cerebral palsy in Sub-Saharan Africa?
Study selection
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (“PRISMA checklist” was used in the formulation of the systematic review methodology12. A registration request for the review methodology has been made to the PROSPERO database.
Articles were evaluated based on the inclusion and exclusion criteria from the perspective of the outcome variable (i.e., are they reporting the prevalence or epidemiology of malnutrition among children with cerebral palsy or not).
Search strategy
We searched PubMed, Google Scholar, Web Science, Cochrane databases, and other source that were conducted on malnutrition among children with cerebral palsy, and were published between January 2010 and September 2023. Since research involves constantly testing the hypotheses, staying updated with the latest publications will help us estimate the recent and updated burden of the problem.
The search was conducted using the following keywords: (Prevalence OR proportion OR Burden OR magnitude) AND (Children [MeSH Terms] OR Child OR infant OR Kids) AND (Cerebral palsy [MeSH Terms] OR Disability OR Impairment OR Special needs) AND (Sub-Saharan Africa) OR developing country OR resource-limited setting. The search terms were used separately and in combination using Boolean operators like “OR” or “AND”. The literature search conducted from April 01 to 17, 2023 by authors includes ESC, MAM, MAS, and SSC. All papers published until April 17, 2023, were included in this review.
Eligibility criteria
Inclusion criteria
Language: Articles published in English.
Study area: Only studies conducted in Sub-Saharan Africa were eligible for this study.
Study design: Observational studies (case-control, cohort, and cross-sectional study) that report the prevalence of malnutrition among children with cerebral palsy.
Publication year: Reports made from January 2010 onwards.
Publication condition: Peer-reviewed journal articles as well as articles from the university website.
Outcome of interests: Studies reported the prevalence of malnutrition among children with cerebral palsy in Sub-Saharan Africa was considered.
Exclusion criteria
Due to the inability to evaluate the quality of publications without access to the complete text and to estimate the outcome variable, articles that were not fully accessed were excluded. Furthermore, studies that did not distinguish between children with cerebral palsy and those with other special needs/disability were excluded from the study.
Outcome measurement among children with cerebral palsy
There is one key outcome variable in this systematic review, which is the prevalence of malnutrition among children with cerebral palsy. The prevalence of malnutrition among children with cerebral palsy was calculated by multiplying the total number of children with cerebral palsy who had malnutrition by 100 and dividing that number by the total number of children with cerebral palsy.
Study selection and data extraction
All Studies reported the prevalence of malnutrition among children with cerebral palsy in Sub-Saharan Africa were transferred to Zotero software, and duplicate articles were removed. The pertinent information, including the names of the authors, the study's design, sample size, study area, and the number of cases/proportions of malnutrition were independently extracted by four authors (ESC, NM, FDB, and GBM). Similar to the preceding step, disagreements were discussed during a consensus meeting with other reviewers (MAM, MAS, ECA, MMG, KDT, SSC, and YSK) for the final decision on which studies to include in the meta-analysis and systematic review.
Quality assessment
We evaluated the included studies' quality using the Joanna Briggs Institute Critical Appraisal instrument for use in JBI Systematic Reviews (JBI-MAStARI)13. For the cross-sectional, case–control, and cohort investigations, various items were used in the scale. This systematic review and meta-analysis study included five writers (TAD, WAB, AK, AMD, and MMA) who examined the included articles.
Statistical analysis
The authors verified the accuracy of the retrieved data in a Microsoft Excel sheet before exporting it into STATA 17 for further analysis. The STATA version 17 was used for all analyses in this study.
The degree of heterogeneity was evaluated using Cochrane Q-statistics and an I2 statistic with a p-value (< 0.05)14,15. The test for heterogeneity was high (75%) or moderate (50–74%)16. Using a random-effects model, the pooled prevalence of malnutrition among children with cerebral palsy was estimated.
Once we had determined that there was moderate or higher heterogeneity, we also looked into the cause of the heterogeneity using subgroup analysis and meta-regression17. Predetermined subgroups were taken into account for this, including the study sample size, study design, publication year, and study conditions.
The publication bias was estimated through a funnel plot and Egger test18 and sensitivity analysis was piloted to examine the effect of a single study on the overall estimation.
Results
Search result
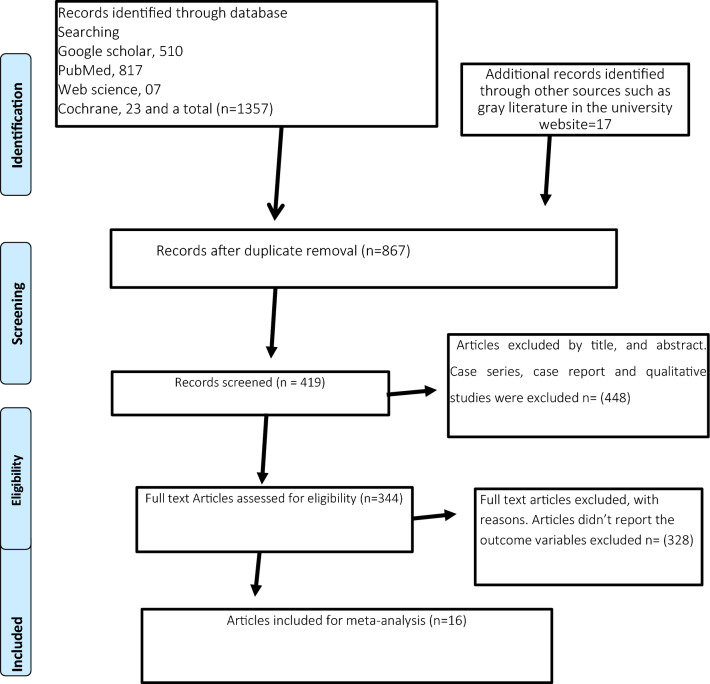
We found 1374 studies from PubMed, Google Scholar, Web Science, Cochrane databases, and other source. There were 507 studies were excluded due to duplication. Of the remaining 867 studies, 523 studies were excluded through title and abstract screening. From a total of 344 full-text articles, 328 were excluded due to the outcome variable wasn’t reported. A total of 16 studies were finally included from 09 Sub-Saharan Africa such as Nigeria, Ghana, Uganda, Kenya, Sudan, Cameroon, Tanzania, Botswana, and Zambia (Fig. 1).
Figure 1.
The PRISMA flow diagram of searching process.
Study characteristics and participants
This systematic review and meta-analysis examined 16 studies conducted in Sub-Saharan Africa to determine the prevalence of malnutrition among 2,120 children diagnosed with cerebral palsy. The review included a total of 16 cross-sectional studies with study design19–34.
Out of sixteen studies in this review, five were from Nigeria19,21,23,25,26,, three were from Ghana), two studies were from Uganda22,28, and the remaining seven studies were from Kenya30, Sudan20, Cameroon29, Tanzania33, Botswana27, and Zambia31.
The review found that the highest proportion of malnutrition among children with cerebral palsy was 90%22, while the lowest proportion was 37.3%23. The sample sizes varied significantly, with the largest study including 388 participants from Nigeria25, and the smallest study including only 16 participants from Zambia31 (Table 1).
Table 1.
Distribution of malnutrition among children with cerebral palsy in Sub-Saharan Africa.
| First author/year | Country | Study design | Sample size | Cases | Malnutrition (%) | Quality status |
|---|---|---|---|---|---|---|
| Adamu et al 2018 | Nigeria | Cross sectional | 150 | 129 | 86 | Low risk |
| Ali et al. 2022 | Sudan | Cross sectional | 90 | 53 | 58.9 | Low risk |
| Badaru et al. 2023 | Nigeria | Cross sectional | 146 | 95 | 65.1 | Low risk |
| Bambi et al. 2021 | Uganda | Cross sectional | 224 | 202 | 90 | High risk |
| Chidomere et al. 2023 | Nigeria | Cross sectional | 169 | 63 | 37.3 | Low risk |
| Donkor et al. 2019 | Ghana | Cross sectional | 34 | 17 | 50 | Low risk |
| Duke et al 2021 | Nigeria | Cross sectional | 388 | 198 | 51 | Low risk |
| Iloeje et al. 2017 | Nigeria | Cross sectional | 100 | 37 | 38.1 | Low risk |
| Johnson et al. 2017 | Botswana | Cross sectional | 61 | 26 | 43 | Low risk |
| Kakooza- et al. 2015 | Uganda | Cross sectional | 135 | 57 | 42 | Low risk |
| Kana et al. 2022 | Cameroon | Cross sectional | 88 | 36 | 40.9 | Low risk |
| Koriata et al. 2012 | Kenya | Cross sectional | 140 | 98 | 70.3 | Low risk |
| Nawa et al. 2022 | Zambia | Cross sectional | 16 | 13 | 80.5 | Low risk |
| Polack et al. 2018 | Ghana | Cross sectional | 76 | 49 | 65 | Low risk |
| Sissya et al. 2010 | Tanzania | Cross sectional | 239 | 175 | 73.1 | Low risk |
| Zuurmond et al. 2018 | Ghana | Cross sectional | 64 | 40 | 63.1 | Low risk |
Meta-analysis
The pooled proportion of malnutrition among children with cerebral palsy in Sub-Saharan Africa by using random-effects model analysis was found to be 59.7% (95%CI; 49.8–69.6) and showed in (Fig. 2).
Figure 2.
Forest plot to test of malnutrition estimation among children with cerebral palsy in Sub-Saharan Africa.
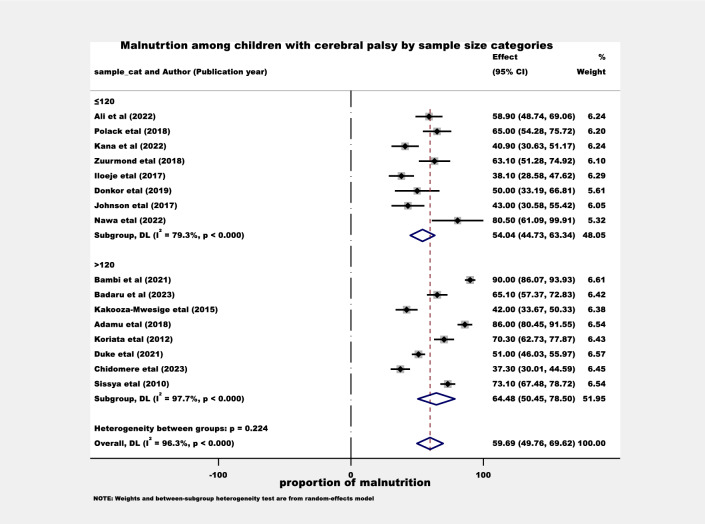
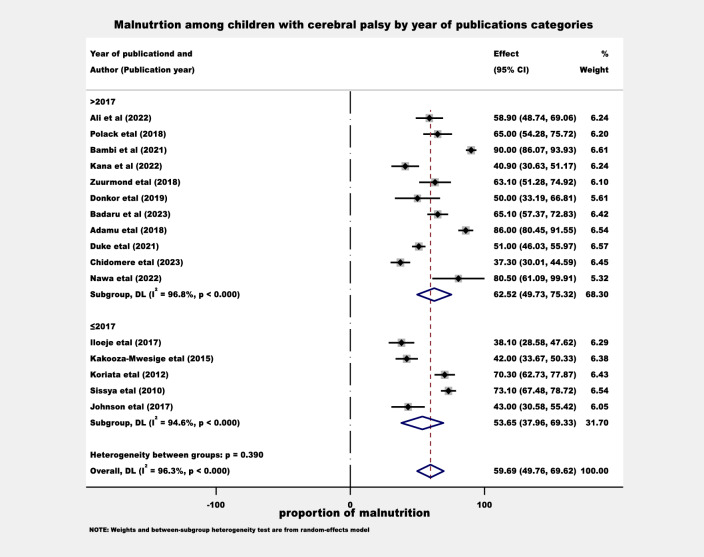
Estimation of malnutrition burden by sub group analysis among children with cerebral palsy
The proportion of malnutrition was also estimated by considering the sample size difference. The sample sizes were categorized as ≤ 120 and > 120, and the proportion of malnutrition was found to be 54.0 (95% CI: 44.7–63.3) and 64.5 (95% CI: 50.5–78.5) in Sub-Saharan Africa respectively (Fig. 3). Moreover, the proportion of malnutrition was estimated by accounting for the difference in the year of publication. In this regard, the study classified before ≤ 2017 and > 2017, and the proportion of malnutrition was found to be 53.7 (95% CI: 38.0–69.3) and 62.5 (95% CI: 49.7–75.3) in Sub-Saharan Africa respectively (Fig. 4).
Figure 3.
The proportion of malnutrition estimation among children with cerebral palsy by sample sizes categories.
Figure 4.
The proportion of malnutrition estimation among children with cerebral palsy by year of publications categories.
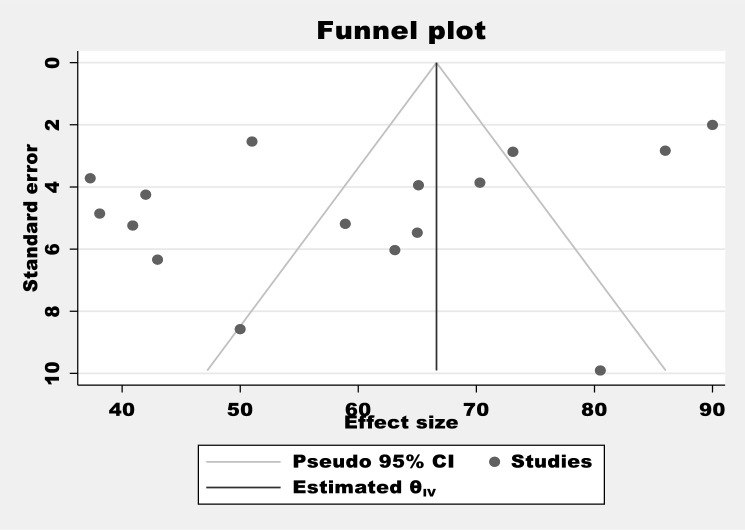
Publication bias
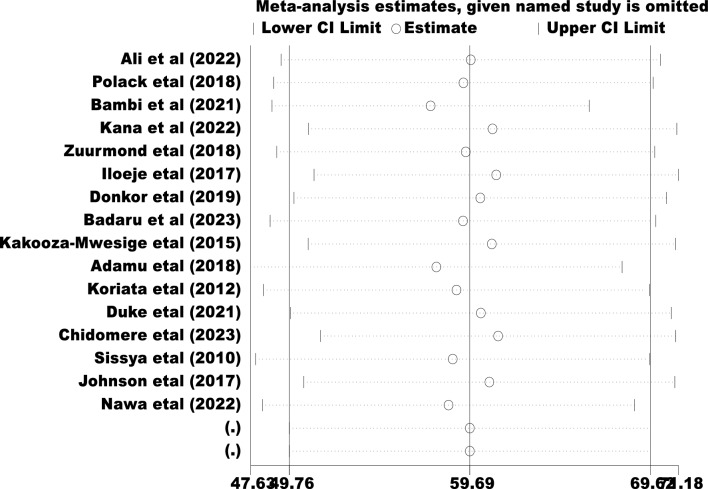
Egger's regression test value showed that there is a statistically significant publication bias in this study (p < 0.044) (Table 2). Besides, a funnel plot showed an asymmetrical distribution which indicated the presence of publication bias (Fig. 5)). Moreover, the results of sensitivity analyses using the random effect model suggested were estimated (Fig. 6).
Table 2.
Egger's test of the study of malnutrition among children with cerebral palsy in Sub-Saharan Africa.
| Std_Eff Coefficient | SE | T | P > t | [95% CI] | ||
|---|---|---|---|---|---|---|
| Slope | 89.32553 | 11.1347 | 8.02 | 0.000 | 65.44397 | 113.2071 |
| Bias | −6.563965 | 2.965408 | −2.21 | 0.044 | −12.92413 | −0.2037975 |
| Test of H0: no small-study effects P = 0.044, Root MSE = 4.62, Number of Studies = 16 | ||||||
Figure 5.
Funnel plot tests for the proportion of malnutrition among children with cerebral palsy in Sub-Saharan Africa.
Figure 6.
The sensitivity test for the proportion of malnutrition among children with cerebral palsy in Sub-Saharan Africa.
Discussion
This systematic review and meta-analysis study provides representative data on the estimation of malnutrition among children with CP in Sub-Saharan Africa.
The study suggests that an estimated pooled malnutrition burden among children with cerebral in Sub-Saharan Africa was found to be 57.4% (95% CI; 46.7–68.2).
The finding of this review, the proportion of malnutrition among children with CP is higher than the study conducted in Saudi Arabia11, U.S.A7, Argentine10, Bangladesh35, Nepal36, Turkey37, Vietnam38, and systematic review and meta-analysis Asia 40%39.
This difference might be due to the limited healthcare services, healthcare providers, infrastructure, and limited social support for the optimization of health among children with cerebral palsy by preventing, controlling, and managing malnutrition in Sub-Saharan Africa as compared to other continents40,41.
Moreover, food insecurity, overpopulation, low educational status, and wars can contribute to malnutrition is too high, particularly in resource-limited settings and vulnerable groups such as children with cerebral play in Sub-Saharan Africa40–43.
However, the proportion of malnutrition is lower than in the study conducted in Colombia9, and a Systematic Review and Meta-Analysis Arabic speaking countries5. This difference might be due to the reference standards cut-off point to diagnosis malnutrition in Colombian and Arabic-speaking countries were included mild, modern, and severe classifications, whereas this study included moderate and severe to declare malnutrition only among children with cerebral palsy5,9.
The finding of this review will inform the burden of malnutrition among children with cerebral palsy in Sub-Saharan Africa for the planners, policymakers, healthcare providers, government and non-governmental organizations, and researchers’ up-to-date data. Additionally, this finding shows the impact of malnutrition in children with cerebral, so prevention and management through the integration of the recommendations to develop guidelines and improve the quality of service is very crucial for children with cerebral palsy in the continent.
The subgroup analysis conducted in this review aimed to estimate the proportion of malnutrition among children with cerebral palsy in various categories within the Sub-Saharan Africa region. One aspect that was examined was the difference in sample sizes, with participants categorized as ≤ 120 and > 120. The estimated proportions of malnutrition were found to be 54.0% (95% CI: 44.7–63.3) and 64.5% (95% CI: 50.5–78.5), respectively. Another factor considered was the variation in the year of publication, with studies classified as published before ≤ 2017 and > 2017. The estimated proportions of malnutrition were found to be 53.7% (95% CI: 38.0–69.3) and 62.5% (95% CI: 49.7–75.3), respectively. Taking into account the significance of a large sample size for accuracy, it is conceivable that the proportion of malnutrition among children with cerebral palsy in Sub-Saharan Africa might be higher than the findings of this study suggest. Moreover, recent studies focusing on this population in the region have shown that, there is an increment in the prevalence of malnutrition among children with cerebral palsy. It is crucial to take these subgroup analysis findings into account to avoid misleading conclusions influenced by confounding factors44.
The subgroup analysis findings emphasize the urgent requirement for interventions and targeted strategies to tackle the rising prevalence of malnutrition among children with cerebral palsy.
Limitations of the study
This systematic review and meta-analysis have some limitations. Firstly, the study did not assess the specific causes of malnutrition among children with cerebral palsy. Secondly, only quantitative observational studies published in English were included in the analysis, potentially excluding relevant studies in other languages. Thirdly, studies that did not differentiate between children with cerebral palsy and those with other disabilities were not considered in the analysis.
Conclusion
Malnutrition among children with cerebral in Sub-Saharan Africa was found to be very high. Hence, enhancing and developing strategic guidelines for malnutrition screening, prevention, and nutritional support are crucial among children with cerebral palsy. Furthermore, systematic review, randomized control trials, and qualitative studies are recommended to understand the burden more among children with cerebral palsy in the continent.
Supplementary Information
Acknowledgements
We would like to thank all authors of the studies included in this systematic review and meta-analysis.
Abbreviation
- CP
Cerebral palsy
Author contributions
E.S.C., N.M., F.D.B., G.B.M., M.M.F., L.Y.B., D.T.A., M.A.Z., N.A.G., G.A.A., G.A.K., M.A.M., M.A.S., E.C.A., and S.S.C. developed the protocol and involved in the design, selection of study, and data extraction. Moreover, E.S.C., M.M.G., K.D.T., Y.S.K., B.B., S.F.F., T.A.D., W.A.B., A.K., A.M.D., and MMA performed the statistical analysis and developed the initial drafts of the manuscript. All authors prepared, read, and approved the final draft of the manuscript.
Data availability
All data generated or analyzed during this study are included in this published article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-55730-1.
References
- 1.CDC. Centers for Disease Control and Prevention. 2023 [cited 2023 Dec 7]. What is cerebral palsy? | CDC. Available from: https://www.cdc.gov/ncbddd/cp/facts.html
- 2.Graham HK, Rosenbaum P, Paneth N, Dan B, Lin JP, Damiano DL, et al. Cerebral palsy. Nat. Rev. Dis. Primer. 2016;2(1):1–25. doi: 10.1038/nrdp.2015.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cerebral Palsy Guidance [Internet]. [cited 2023 May 19]. Cerebral Palsy and Malnutrition. Available from: https://www.cerebralpalsyguidance.com/cerebral-palsy/associated-disorders/malnutrition/
- 4.Failure to Thrive [Internet]. 2019 [cited 2023 May 19]. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/failure-to-thrive
- 5.Silva D, da Cunha M, Santana A, Alves AMD, Pereira M. Malnutrition and nutritional deficiencies in children with cerebral palsy: a systematic review and meta-analysis. Public Health. 2022;24(205):192. doi: 10.1016/j.puhe.2022.01.024. [DOI] [PubMed] [Google Scholar]
- 6.Reyes FI, Salemi JL, Dongarwar D, Magazine CB, Salihu HM. Prevalence, trends, and correlates of malnutrition among hospitalized children with cerebral palsy. Dev. Med. Child Neurol. 2019;61(12):1432–1438. doi: 10.1111/dmcn.14329. [DOI] [PubMed] [Google Scholar]
- 7.Jahan I, Muhit M, Hardianto D, Laryea F, Amponsah SK, Chhetri AB, et al. Epidemiology of malnutrition among children with cerebral palsy in low- and middle-income countries: Findings from the global LMIC CP register. Nutrients. 2021;13(11):3676. doi: 10.3390/nu13113676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herrera-Anaya E, Angarita-Fonseca A, Herrera-Galindo VM, Martínez-Marín RDP, Rodríguez-Bayona CN. Association between gross motor function and nutritional status in children with cerebral palsy: A cross-sectional study from Colombia. Dev. Med. Child Neurol. 2016;58(9):936–941. doi: 10.1111/dmcn.13108. [DOI] [PubMed] [Google Scholar]
- 9.de las Ruiz Brunner M, Cieri ME, Rodriguez Marco MP, Schroeder AS, Cuestas E. Nutritional status of children with cerebral palsy attending rehabilitation centers. Dev. Med. Child Neurol. 2020;62(12):1383–1388. doi: 10.1111/dmcn.14667. [DOI] [PubMed] [Google Scholar]
- 10.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2022;10(1):89. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Critical Appraisal Tools | JBI [Internet]. [cited 2023 May 6]. Available from: https://jbi.global/critical-appraisal-tools
- 12.West SL, Gartlehner G, Mansfield AJ, Poole C, Tant E, Lenfestey N, et al. Table 7, Summary of common statistical approaches to test for heterogeneity [Internet]. Agency for Healthcare Research and Quality (US); 2010 [cited 2023 May 16]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK53317/table/ch3.t2/
- 13.Chang Y, Phillips MR, Guymer RH, Thabane L, Bhandari M, Chaudhary V. The 5 min meta-analysis: Understanding how to read and interpret a forest plot. Eye. 2022;36(4):673–5. doi: 10.1038/s41433-021-01867-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.9.5.2 Identifying and measuring heterogeneity [Internet]. [cited 2023 May 16]. Available from: https://handbook-5-1.cochrane.org/chapter_9/9_5_2_identifying_and_measuring_heterogeneity.htm
- 15.Spineli LM, Pandis N. Problems and pitfalls in subgroup analysis and meta-regression. Am. J. Orthod. Dentofacial. Orthop. 2020;158(6):901–904. doi: 10.1016/j.ajodo.2020.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Identifying publication bias in meta-analyses of continuous outcomes [Internet]. [cited 2023 May 6]. Available from: https://training.cochrane.org/resource/identifying-publication-bias-meta-analyses-continuous-outcomes
- 17.Adamu AS, Sabo UA, Gwarzo GD, Belonwu RO. Nutritional status in cerebral palsy: A cross-sectional comparative survey of children in Kano, Nigeria. Niger. Postgrad. Med. J. 2018;25(3):156–160. doi: 10.4103/npmj.npmj_67_18. [DOI] [PubMed] [Google Scholar]
- 18.Ali TAI, Ali SBA, Ali MAM. Assessment of nutritional status for Sudanese children with cerebral Palsy in two rehabilitation centers in Khartoum state, Sudan. J. Saudi Soc. Food Nutr. (JSSFN) 2022;15(1):87–96. [Google Scholar]
- 19.Badaru UM, Umar AL, Abdullahi A, Usman JS, Ogwumike OO. Influence of malnutrition and body composition on the gross motor function of children with cerebral palsy in Kano, Nigeria: a cross-sectional study. Bull. Fac. Phys. Ther. 2023;28(1):2. doi: 10.1186/s43161-022-00113-8. [DOI] [Google Scholar]
- 20.Bambi EN, Mwesige AK, Lekuya HM, Kasirye P, Idro R. Chronic pain among children with cerebral palsy attending a Ugandan tertiary hospital: a cross-sectional study. BMC Pediatr. 2021;21(1):456. doi: 10.1186/s12887-021-02928-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chidomere RI, Ukpabi IK, Chukwudi NK, Onyeonoro UU, Ojinnaka NC. Prevalence and pattern of feeding problems and relationship to motor function severity in children with cerebral palsy in Umuahia. West Afr. J. Med. 2023;40(1):55–59. [PubMed] [Google Scholar]
- 22.Donkor CM, Lee J, Lelijveld N, Adams M, Baltussen MM, Nyante GG, et al. Improving nutritional status of children with Cerebral palsy: a qualitative study of caregiver experiences and community-based training in Ghana. Food Sci. Nutr. 2019;7(1):35–43. doi: 10.1002/fsn3.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duke RE, Torty C, Okorie U, Kim MJ, Eneli N, Edadi U, et al. Pattern of comorbidities in school-aged children with cerebral palsy in Cross River State, Nigeria. BMC Pediatr. 2021;21(1):165. doi: 10.1186/s12887-021-02637-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iloeje SO, Ogoke CC. Factors associated with the severity of motor impairment in children with cerebral palsy seen in Enugu, Nigeria. South Afr. J. Child Health. 2017;11(3):112–116. doi: 10.7196/SAJCH.2017.v11i3.1246. [DOI] [Google Scholar]
- 25.Johnson A, Gambrah-Sampaney C, Khurana E, Baier J, Baranov E, Monokwane B, et al. Risk factors for malnutrition among children with cerebral palsy in Botswana. Pediatr. Neurol. 2017;70:50–55. doi: 10.1016/j.pediatrneurol.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 26.Kakooza-Mwesige A, Tumwine JK, Eliasson AC, Namusoke HK, Forssberg H. Malnutrition is common in Ugandan children with cerebral palsy, particularly those over the age of five and those who had neonatal complications. Acta Paediatr. 1992;104(12):1259–68. doi: 10.1111/apa.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kana CAN, Deugoue RB, Dongmo FN, Enyama D, Noukeu D, Mah E, et al. Comorbidities in children with cerebral palsy. Pediatr. Oncall. J. 2022 doi: 10.7199/ped.oncall.2022.37. [DOI] [Google Scholar]
- 28.Koriata NS. Nutritional status of children with cerebral palsy attending Kenyatta National Hospital [Internet] [Thesis]. University of Nairobi, Kenya; 2012 [cited 2023 Apr 22]. Available from: http://erepository.uonbi.ac.ke/handle/11295/8313
- 29.Nawa NM. The relationship between nutritional status and health in children with cerebral palsy in livingstone. [Internet] [Thesis]. Cavendish University; 2022 [cited 2023 Apr 22]. Available from: http://192.168.1.248:8080/xmlui/handle/123456789/757
- 30.Polack S, Adams M, O’banion D, Baltussen M, Asante S, Kerac M, et al. Children with cerebral palsy in Ghana: Malnutrition, feeding challenges, and caregiver quality of life. Dev. Med. Child Neurol. 2018;60(9):914–21. doi: 10.1111/dmcn.13797. [DOI] [PubMed] [Google Scholar]
- 31.Sissya HA. Prevalence of malnutrition and associated feeding problems among children with cebral pasly attending Muhimbili National Hospital, Dar es Salaam, Tanzania [Internet] [Thesis]. Muhimbili University of Health and Allied Sciences; 2010 [cited 2023 Apr 22]. Available from: http://dspace.muhas.ac.tz:8080/xmlui/handle/123456789/1200
- 32.Zuurmond M, O’Banion D, Gladstone M, Carsamar S, Kerac M, Baltussen M, et al. Evaluating the impact of a community-based parent training programme for children with cerebral palsy in Ghana. PloS One. 2018;13(9):e0202096. doi: 10.1371/journal.pone.0202096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jesmin H, Debnath B, Islam S, Rahman M. Nutritional status among children with cerebral palsy attended at Medical University Hospital of Bangladesh. J. Curr. Adv. Med. Res. 2022;9(1):42–7. doi: 10.3329/jcamr.v9i1.59744. [DOI] [Google Scholar]
- 34.Jahan I, Muhit M, Al Imam MH, Ghose R, Chhetri AB, Badawi N, et al. Nutritional status of children with cerebral palsy in Gorkha, Nepal: findings from the Nepal cerebral palsy register. Nutrients. 2021;13(8):2537. doi: 10.3390/nu13082537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aydin K, Kartal A, Alp E. High rates of malnutrition and epilepsy: two common comorbidities in children with cerebral palsy. Turk. J. Med. Sci. 2019;49(1):33–37. doi: 10.3906/sag-1803-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karim T, Jahan I, Dossetor R, Giang NTH, Van Anh NT, Dung TQ, et al. Nutritional status of children with cerebral palsy—Findings from prospective hospital-based surveillance in Vietnam indicate a need for action. Nutrients. 2019;11(9):2132. doi: 10.3390/nu11092132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Da Silva DCG, da Cunha MDSB, de Oliveira Santana A, dos Santos Alves AM, Santos MP. Malnutrition and nutritional deficiencies in children with cerebral palsy: a systematic review and meta-analysis. Public Health. 2022;205:192–201. doi: 10.1016/j.puhe.2022.01.024. [DOI] [PubMed] [Google Scholar]
- 38.Oguntade HA, Nishath T, Owusu PG, Papadimitriou C, Sakyi KS. Barriers to providing healthcare to children living with cerebral palsy in Ghana: A qualitative study of healthcare provider perspectives. PLOS Glob Public Health. 2022;2(12):e0001331. doi: 10.1371/journal.pgph.0001331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Manyuma D, Maluleke M, Raliphaswa NS, Masutha TC, Rangwaneni ME, Thabathi TE, et al. Caring for children with cerebral palsy: A challenge to caregivers in rural areas of South Africa. Children. 2023;10(3):440. doi: 10.3390/children10030440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bain LE, Awah PK, Geraldine N, Kindong NP, Sigal Y, Bernard N, et al. Malnutrition in Sub-Saharan Africa: Burden, causes and prospects. Pan Afr. Med. J. 2013;15:120. doi: 10.11604/pamj.2013.15.120.2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Militao EMA, Salvador EM, Uthman OA, Vinberg S, Macassa G. Food insecurity and health outcomes other than malnutrition in Southern Africa: A descriptive systematic review. Int. J. Environ. Res. Public Health. 2022;19(9):5082. doi: 10.3390/ijerph19095082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tanniou J, van der Tweel I, Teerenstra S, Roes KCB. Subgroup analyses in confirmatory clinical trials: Time to be specific about their purposes. BMC Med. Res. Methodol. 2016;16:20. doi: 10.1186/s12874-016-0122-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Subgroup analysis [Internet]. [cited 2023 May 14]. Available from: https://www.iwh.on.ca/what-researchers-mean-by/subgroup-analysis
- 44.Farrokhyar F, Skorzewski P, Phillips MR, Garg SJ, Sarraf D, Thabane L, et al. When to believe a subgroup analysis: revisiting the 11 criteria. Eye. 2022;36(11):2075–2077. doi: 10.1038/s41433-022-01948-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article.