Abstract
Background
Oral care is one of the fundamental nursing care procedures used to decrease oral colonization, dental plaque, respiratory infections, patient stay, and cost. The importance of good oral hygiene for patients in intensive care units (ICUs) is well recognized, however, the most effective way to achieve good oral care in the ICU is unclear. Therefore, the aim of this study was to assess the knowledge, attitude, and practice of nursing professionals regarding oral healthcare in ICUs among various medical institutes across India.
Materials and methods
A questionnaire-based multicentric cross-sectional survey was conducted among registered nursing professionals employed at ICUs of three government tertiary healthcare centers (THC) of India: THC-I, THC-II, and THC-III located in the eastern and northern parts of India between February 2022 and July 2022.
Results
A total of 150 nurses completed the questionnaire form (response rate: 62.5%) comprised of 49 (32.7%) males and 101 (67.3%) females with a mean age of 35.69 ± 7.7 years. Nursing officers’ knowledge surpassed that of staff nurses regarding the duration of toothbrushing (p = 0.033). Among interinstitutional comparisons, THC-I nurses showed the greatest knowledge regarding the duration of toothbrushing and the mechanism of preventing saliva accumulation to reduce microbial growth (p = 0.013 and p = 0.003, respectively). Based on total work experience, participants were segregated into three groups: Group I (<7 years), group II (7.1–13.9 years), and group III (>14 years). Group II surpassed the knowledge of denture removal during sleep, cleaning after every meal, and storing in personalized air-tight containers (p = 0.001 and p = 0.036, respectively). The majority from group II recommended plain saline as the material for oral hygiene maintenance in ICU patients (p = 0.008). Group III predominantly practiced the ideal handwashing technique pre- and post-patient contact which was statistically significant (p = 0.001).
Conclusion
This study observed that a knowledge gap exists among the nurses of the three institutes across India pertaining to the oral hygiene care of ICU patients. Nurse's education and implementation of the proper oral hygiene measures for intubated patients in ICU setup is an essential need.
How to cite this article
Kumar S, Singh B, Mahuli AV, Kumar S, Singh A, Jha AK. Assessment of Nursing Staff's Knowledge, Attitude and Practice Regarding Oral Hygiene Care in Intensive Care Unit Patients: A Multicenter Cross-sectional Study. Indian J Crit Care Med 2024;28(1):48–57.
Keywords: Critically ill, Intensive care unit, Nurses knowledge, Oral care, Oral hygiene, Ventilator-associated pneumonia
Highlights
This article gives an insight regarding the knowledge, attitude, and practice of nurses pertaining to oral hygiene care in intensive care units (ICUs).
This cross-sectional questionnaire based multicentric study focuses on the practices of oral hygiene in intubated patients, identifying the shortcomings with ways and measures to overcome the challenges in improving oral care in ICUs.
Introduction
Poor oral health or dysfunctions negatively affect nutritional status, affecting the general health and quality of life.1 Patients in the intensive care unit (ICU) require specific oral care need to prevent oral disease and nosocomial infections which may lead to increased mortality and morbidity. Ventilator-associated pneumonia (VAP), which is believed to affect 10–28% of ventilated patients, is the most prevalent and fatal nosocomial infection in patients receiving critical care.2 The ICU patients may be intubated, inserted with a nasogastric tube, profoundly sedated, or feverish, all of which may result in dehydration and require mouth breathing.3 In the hospital setting, the nurses provide daily comfort and hygiene care, including dental hygiene. It is a challenging task for a nurse or assistant to perform oral hygiene on a patient who is in a semiconscious and noncooperative state.4
If oral hygiene is neglected in hospitalized patients, the oropharynx and the biofilm (plaque) deposited, following the type and consistency of the food consumed, become a favorable reservoir for the growth of microorganisms in association with reduced saliva production. This situation may be exacerbated by the presence of other oral diseases such as periodontal disease, dental caries, pulp necrosis, mucosal injury, and trauma caused by dentures, installing remote infections and influencing the therapeutic characteristics of each. In the literature, there is a connection between aspiration pneumonia, cardiovascular abnormalities, and periodontal disease. However, research and in-depth analyses have shown that oral hygiene and plaque reduction are still infrequently implemented in ICUs.5
Although the majority of those in charge of this practice are aware of their obligations in terms of oral hygiene care, it is well known that information about oral health is frequently learned through experience because nurses were not academically trained for tasks related to oral healthcare. Additionally, there is a deficiency of proper processes and routines employed when the oral hygiene technique is used which compromises the needs of oral health. Another aggravating factor is the administration of drugs to diminish the local microbial flora that do not have the expected antiseptic effects.
The perception that oral care does not significantly improve health, insufficient nurse staffing, a lack of oral health-related supplies, and low priority of oral health needs are the principal barriers reported in providing hospitalized patients with effective oral healthcare.6 For ICU patients, it is crucial for healthcare providers to have a thorough understanding of oral hygiene procedures to at the very least undertake the necessary cleaning of the tongue, cheeks, gums, and teeth. Thus, the study's aim is to evaluate the knowledge, attitude, and practice of nursing professionals regarding oral healthcare in ICUs among various Medical Institutes across India because there is a paucity of such research in the Indian setting.
Materials and Methods
Study Design and Setting
A questionnaire-based multicentric cross-sectional survey was conducted among registered nursing professionals employed at ICUs of three Government Tertiary Healthcare Centers (THC) of India: THC-I, THC-II, and THC-III located in the eastern and northern parts of India between February 2022 to July 2022. The method employed followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines. The study was approved by the institutional ethical committee of THC-I (IEC402/29/12/2021).
Participants
The selection criteria included registered nursing (males and females) employees with more than six months of experience in the ICU field who have performed an ICU posting at least once among one of the selected institutes.
Data Sources/Measurement
A well-structured questionnaire was drafted with discussion among the nursing faculties and dental experts. The questionnaire validation was done after performing a pilot study on 10 nursing staff, which was omitted from the final analysis. Face validations were established by five nurse educators. The reliability of instruments was also checked by test–retest on 10 nurses at a 2-week interval (r = 0.82).
The self-administered questionnaire comprised 17 closed-ended questions, including demographic data (age, designation, work experience, and name of institution), perception, satisfaction, and experience of oral hygiene care among ICU patients. Participants were divided into three groups based on their total work experience in the ICU; group I had less than 7 years; group II comprising of 7.1–13.9 years whereas group III included 14 years and above. The questionnaire was distributed to 240 nursing participants across the three institutes. The study was explained in detail to each participant informed that their responses would be kept confidential and anonymous. Informed consent was obtained from those nurses who agreed to participate.
Bias
The participants were asked to complete the questionnaires during their break time to avoid disrupting the ICU routine duties in the investigator's presence. The investigators of each center were responsible for distributing and collecting the completed questionnaires.
Study Size Estimation
The sample size estimation was done using the formula N = (Z2 × P[1 × P])/e2 taking a proportion of the population who had knowledge about oral healthcare from previously available literature, at a 95% confidence interval and a 5% margin of error. A minimum sample size of 145 participants was calculated but 240 were considered.
Statistical Analysis
The gathered data was transferred to Microsoft Excel and analyzed using the statistical package for social sciences (SPSS, version 26, IBM Inc., Chicago, Illinois, USA) software to obtain the results. Descriptive statistics were used to calculate frequency distributions and the Chi-square test for relationships among variables and p < 0.05 was considered statistically significant.
Results
The sociodemographic characteristics of 150 nursing professionals who completed the questionnaire form (response rate: 62.5%) comprised of 49 (32.7%) males and 101 (67.3%) females with a mean age of 35.69 ± 7.7 years of which 110 (73.3%) were nursing officers and 40 (26.7%) were staff nurses. The distribution of study participants in different institutes is depicted in Figure 1.
Fig. 1.
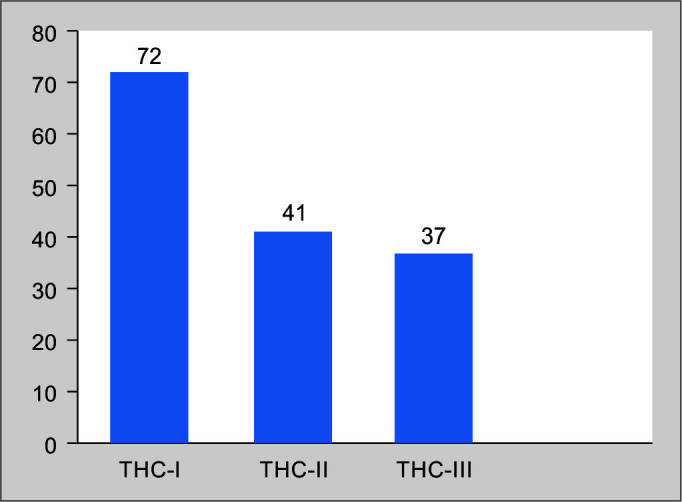
Distribution of study participants in different institutions
THC, tertiary healthcare center
Nursing officers’ knowledge surpassed that of staff nurses regarding the duration of toothbrushing (p = 0.033), recommended material used for oral care hygiene maintenance in ICU patients (p = 0.002) and technique of controlling saliva-associated microbial growth in intubated patients was statistically significant (p = 0.032) (Table 1).
Table 1.
Association with designation
| S. No. | Questions | Responses | Nursing officer | Staff nurse | χ2 | p-value |
|---|---|---|---|---|---|---|
| 1 | Recommended material used for oral care hygiene maintenance in ICU patients | Simple suction | 6 | 3 | 16.802 | 0.002 |
| Tap water | 8 | 2 | ||||
| Plain saline | 89 | 27 | ||||
| Chlorhexidine | 6 | 1 | ||||
| Toothbrush | 1 | 7 | ||||
| 2 | Is toothbrush recommended for maintenance of oral hygiene in ICU patients? | No | 42 | 8 | 4.364 | 0.037 |
| Yes | 68 | 32 | ||||
| 3 | Frequency of toothbrushing performed by nursing staff for each ICU patients daily | Once | 26 | 12 | 0.737 | 0.864 |
| Twice | 56 | 19 | ||||
| After every meal | 17 | 6 | ||||
| Not daily | 11 | 3 | ||||
| 4 | Duration of toothbrushing performed by nursing staff for each ICU patient | 3–4 minutes | 46 | 13 | 8.762 | 0.033 |
| 1–2 minutes | 53 | 16 | ||||
| 5 minutes | 3 | 1 | ||||
| Not sure | 8 | 10 | ||||
| 5 | Pooling of saliva in the mouth for intubated ICU patients leads to increased incidence of microbial growth. This can be controlled by | (A) Suctioning of oral fluids regularly | 46 | 10 | 6.865 | 0.032 |
| (B) Using cotton swabs to absorb | 10 | 1 | ||||
| Both (A) and (B) | 54 | 29 | ||||
| Not required | 0 | 0 | ||||
| 6 | Oral hygiene tools required in an ICU setup for oral hygiene maintenance | Toothbrush | 8 | 3 | 0.022 | 0.989 |
| Gauze + tongue depressor | 40 | 15 | ||||
| Mouth rinse | 0 | 0 | ||||
| All | 62 | 22 | ||||
| 7 | Recommended toothpaste for children with teeth should contain | Fluoride | 62 | 22 | 2.080 | 0.353 |
| Sodium chloride | 43 | 18 | ||||
| Sodium bicarbonate | 0 | 0 | ||||
| Don't know | 5 | 0 | ||||
| 8 | Recommended oral rinse for ICU patients | 0.12% Chlorhexidine | 101 | 33 | 2.673 | 0.102 |
| Plain water | 9 | 7 | ||||
| Betadine | 0 | 0 | ||||
| Hydrogen | 0 | 0 | ||||
| Don't know | 0 | 0 | ||||
| 9 | Ideal handwashing practice to be followed by nursing staff in ICU | Precontact handwashing with tap water and soap | 0 | 0 | 0.408 | 0.523 |
| Pre- and post-contact handwashing with tap water and soap | 42 | 13 | ||||
| Pre- and post-contact handwashing with tap water and soap followed by alcohol rub | 68 | 27 | ||||
| Handwashing is not needed | 0 | 0 | ||||
| 10 | Denture hygiene of geriatric ICU patients comprises | Removal of dentures at night and cleaning it once a day | 11 | 6 | 2.108 | 0.349 |
| Removal of denture during sleep and cleaning it preferably after every meal | 95 | 34 | ||||
| No need for removal of denture from the mouth and external cleaning | 4 | 0 | ||||
| Intraoral cleaning with appropriate tools is sufficient | 0 | 0 | ||||
| 11 | Where do you store personalized oral hygiene tools for ICU patients? | (A) Personalized air-tight containers | 53 | 14 | 2.920 | 0.404 |
| (B) Along with their other personal belongings | 27 | 10 | ||||
| (A) or (B) | 30 | 16 | ||||
| Does not matter | 0 | 0 | ||||
| 12 | Maintenance of oral hygiene in infants before eruption of teeth in a pediatric ICU is done by | (A) Cotton swab to clean the gums | 75 | 24 | 1.923 | 0.382 |
| (B) Small soft toothbrush | 0 | 0 | ||||
| Both (A) and (B) | 33 | 16 | ||||
| No supporting cleaning required | 2 | 0 | ||||
| 13 | Did you receive assessment and provision of comprehensive oral care for ICU patients in basic nursing training? | No | 6 | 1 | 0.576 | 0.448 |
| Yes | 104 | 39 | ||||
| 14 | What is the ideal patient position for performing oral hygiene care in an unconscious ICU adult patient? | Position the patient in the supine position | 6 | 2 | 1.488 | 0.475 |
| Position the patient in the prone position | 0 | 0 | ||||
| Position the patient in the lateral decubitus | 69 | 21 | ||||
| Position the patient in elevated supine position | 35 | 17 | ||||
| Any position | 0 | 0 | ||||
| 15 | Do you think oral hygiene maintenance is necessary for ICU patients? | Yes | 110 | 40 | – | – |
| No | 0 | 0 | ||||
| 16 | Doctor's instruction for oral hygiene care documented in the checklist and your necessary documentation/record for the oral hygiene procedures will improve the practice of oral care by nursing staff | Yes | 110 | 40 | – | – |
| No | 0 | 0 | ||||
| 17 | Will the presence of a dental surgeon in the ICU will help in proper maintenance of oral hygiene in ICU patient? | No | 10 | 5 | 0.379 | 0.538 |
| Yes | 100 | 35 |
Among interinstitutional comparisons, THC-I showed the greatest (n = 24) knowledge regarding the duration of toothbrushing performed for each ICU patient while 29 participants knew the mechanism of controlling saliva accumulation in the mouth to prevent microbial growth (p = 0.013 and 0.003, respectively) (Table 2).
Table 2.
Association with institution
| S. No. | Questions | Responses | THC-I | THC-II | THC-III | χ2 | p-value |
|---|---|---|---|---|---|---|---|
| 1 | Recommended material used for oral care hygiene maintenance in ICU patients | Simple suction | 6 | 2 | 1 | 12.915 | 0.115 |
| Tap water | 4 | 4 | 2 | ||||
| Plain saline | 51 | 32 | 33 | ||||
| Chlorhexidine | 3 | 3 | 1 | ||||
| Toothbrush | 8 | 0 | 0 | ||||
| 2 | Is toothbrush recommended for maintenance of oral hygiene in ICU patients? | No | 21 | 12 | 17 | 3.516 | 0.172 |
| Yes | 51 | 29 | 20 | ||||
| 3 | Frequency of toothbrushing performed by nursing staff for each ICU patient daily | Once | 22 | 10 | 6 | 6.616 | 0.358 |
| Twice | 30 | 21 | 24 | ||||
| After every meal | 13 | 7 | 3 | ||||
| Not daily | 7 | 3 | 4 | ||||
| 4 | Duration of toothbrushing performed by nursing staff for each ICU patient | 3–4 minutes | 24 | 19 | 16 | 16.180 | 0.013 |
| 1–2 minutes | 39 | 20 | 19 | ||||
| 5 minutes | 2 | 2 | 3 | ||||
| Not sure | 16 | 0 | 4 | ||||
| 5 | Pooling of saliva in the mouth for intubated ICU patients leads to increased incidence of microbial growth. This can be controlled by | (A) Suctioning of oral fluids regularly | 29 | 9 | 18 | 15.855 | 0.003 |
| (B) Using cotton swabs to absorb | 2 | 8 | 1 | ||||
| Both (A) and (B) | 41 | 24 | 18 | ||||
| Not required | 0 | 0 | 0 | ||||
| 6 | Oral hygiene tools required in an ICU setup for oral hygiene maintenance | Toothbrush | 7 | 2 | 2 | 4.484 | 0.344 |
| Gauze + tongue depressor | 30 | 11 | 14 | ||||
| Mouth rinse | 0 | 0 | 0 | ||||
| All | 35 | 28 | 21 | ||||
| 7 | Recommended toothpaste for children with teeth should contain | Fluoride | 41 | 17 | 26 | 8.640 | 0.071 |
| Sodium chloride | 30 | 22 | 9 | ||||
| Sodium bicarbonate | 0 | 0 | 0 | ||||
| Don't know | 1 | 2 | 2 | ||||
| 8 | Recommended oral rinse for ICU patients | 0.12% Chlorhexidine | 62 | 36 | 36 | 3.348 | 0.188 |
| Plain water | 10 | 5 | 1 | ||||
| Betadine | 0 | 0 | 0 | ||||
| Hydrogen | 0 | 0 | 0 | ||||
| Don't know | 0 | 0 | 0 | ||||
| 9 | Ideal handwashing practice to be followed by nursing staff in ICU | Pre-contact handwashing with tap water and soap | 0 | 0 | 0 | 1.923 | 0.382 |
| Pre- and post-contact handwashing with tap water and soap | 25 | 13 | 17 | ||||
| Pre- and post-contact handwashing with tap water and soap followed by alcohol rub | 47 | 28 | 20 | ||||
| Handwashing is not needed | 0 | 0 | 0 | ||||
| 10 | Denture hygiene of geriatric ICU patients comprises | Removal of dentures at night and cleaning it once a day | 9 | 6 | 2 | 3.115 | 0.539 |
| Removal of denture during sleep and cleaning it preferably after every meal | 62 | 33 | 34 | ||||
| No need for removal of denture from the mouth and external cleaning | 1 | 2 | 1 | ||||
| Intraoral cleaning with appropriate tools is sufficient | 0 | 0 | 0 | ||||
| 11 | Where do you store personalized oral hygiene tools for ICU patients? | (A) Personalized air-tight containers | 27 | 22 | 18 | 7.658 | 0.264 |
| (B) Along with their other personal belongings | 17 | 9 | 11 | ||||
| (A) or (B) | 28 | 10 | 8 | ||||
| Does not matter | 0 | 0 | 0 | ||||
| 12 | Maintenance of oral hygiene in infants before eruption of teeth in a pediatric ICU is done by | (A) Cotton swab to clean the gums | 44 | 27 | 28 | 3.779 | 0.437 |
| (B) Small soft toothbrush | 0 | 0 | 0 | ||||
| Both (A) and (B) | 27 | 14 | 8 | ||||
| No supporting cleaning is required | 1 | 0 | 1 | ||||
| 13 | Did you receive assessment and provision of comprehensive oral care for ICU patients in basic nursing training? | No | 1 | 4 | 2 | 4.171 | 0.124 |
| Yes | 71 | 37 | 35 | ||||
| 14 | What is the ideal patient position for performing oral hygiene care in an unconscious ICU adult patient? | Position the patient in the supine position | 3 | 3 | 2 | 1.475 | 0.831 |
| Position the patient in the prone position | 0 | 0 | 0 | ||||
| Position the patient in the lateral decubitus | 41 | 26 | 23 | ||||
| Position the patient in the elevated supine position | 28 | 12 | 12 | ||||
| Any position | 0 | 0 | 0 | ||||
| 15 | Do you think oral hygiene maintenance is necessary for ICU patients? | Yes | 72 | 41 | 37 | – | – |
| No | 0 | 0 | 0 | ||||
| 16 | Doctor's instruction for oral hygiene care documented in the checklist and your necessary documentation/record for the oral hygiene procedures will improve the practice of oral care by nursing staff | Yes | 72 | 41 | 37 | – | – |
| No | 0 | 0 | 0 | ||||
| 17 | Will the presence of a dental surgeon in the ICU will help in proper maintenance of oral hygiene in ICU patient? | No | 8 | 3 | 4 | 0.454 | 0.797 |
| Yes | 64 | 38 | 33 |
THC, tertiary healthcare center
The majority (n = 35) of group I respondents knew that oral hygiene tools in an ICU setup must consist of a toothbrush, gauze with a tongue depressor and mouth rinse (p = 0.017). A bulk of group II (n = 48) opted for plain saline as the recommended material for oral hygiene maintenance in ICU patients (p = 0.008) while forty participants agreed that toothbrush is recommended for maintenance of oral hygiene in ICU patients (p = 0.011). Thirty-five among group I gave their consensus regarding the duration of toothbrushing to be 1–2 minutes for each ICU patient (p = 0.000). At the same time, 36 participants opted combined technique to eliminate pooled saliva (p = 0.002). Fluoride toothpaste for children was recommended by most of the group II participants (p = 0.011). Maintaining denture hygiene by its removal at sleep and cleaning post each meal of ICU patients were practiced by 50 of the group II participants (p = 0.036). They also stored their dentures in personalized airtight containers (p = 0.025). The majority (n = 56) of the participants had received comprehensive oral care for ICU patients in basic nursing training (p = 0.001). Maximum agreed that the presence of a dental surgeon in the ICU will aid in proper oral hygiene maintenance in ICU patients (p = 0.027). The ideal handwashing practice by nursing staff in the ICU was observed in majority by the group C (n = 35) participants (p = 0.001) (Table 3).
Table 3.
Association with total experience
| S. No. | Questions | Responses | Group I | Group II | Group III | χ2 | p-value |
|---|---|---|---|---|---|---|---|
| 1 | Recommended material used for oral care hygiene maintenance in ICU patients | Simple suction | 7 | 2 | 0 | 20.658 | 0.008 |
| Tap water | 6 | 4 | 0 | ||||
| Plain saline | 35 | 48 | 33 | ||||
| Chlorhexidine | 4 | 1 | 2 | ||||
| Toothbrush | 2 | 1 | 5 | ||||
| 2 | Is toothbrush recommended for maintenance of oral hygiene in ICU patients? | No | 26 | 16 | 8 | 9.105 | 0.011 |
| Yes | 28 | 40 | 32 | ||||
| 3 | Frequency of toothbrushing performed by nursing staff for each ICU patient daily | Once | 16 | 15 | 7 | 11.765 | 0.067 |
| Twice | 28 | 26 | 21 | ||||
| After every meal | 3 | 9 | 11 | ||||
| Not daily | 7 | 6 | 1 | ||||
| 4 | Duration of toothbrushing performed by nursing staff for each ICU patient | 3–4 minutes | 13 | 30 | 16 | 34.182 | 0.000 |
| 1–2 minutes | 35 | 24 | 10 | ||||
| 5 minutes | 0 | 0 | 4 | ||||
| Not sure | 6 | 2 | 10 | ||||
| 5 | Pooling of saliva in the mouth for intubated ICU patients leads to an increased incidence of microbial growth. This can be controlled by | (A) Suctioning of oral fluids regularly | 29 | 15 | 12 | 16.628 | 0.002 |
| (B) Using cotton swabs to absorb | 6 | 5 | 0 | ||||
| (A) and (B) | 19 | 36 | 28 | ||||
| Not required | 0 | 0 | 0 | ||||
| 6 | Oral hygiene tools required in an ICU setup for oral hygiene maintenance | Toothbrush | 7 | 1 | 3 | 12.058 | 0.017 |
| Gauze + tongue depressor | 12 | 23 | 20 | ||||
| Mouth rinse | 0 | 0 | 0 | ||||
| All | 35 | 32 | 17 | ||||
| 7 | Recommended toothpaste for children with teeth should contain | Fluoride | 23 | 37 | 24 | 13.124 | 0.011 |
| Sodium chloride | 26 | 19 | 16 | ||||
| Sodium bicarbonate | 0 | 0 | 0 | ||||
| Don't know | 5 | 0 | 0 | ||||
| 8 | Recommended oral rinse for ICU patients | 0.12% chlorhexidine | 47 | 50 | 37 | 0.720 | 0.698 |
| Plain water | 7 | 6 | 3 | ||||
| Betadine | 0 | 0 | 0 | ||||
| Hydrogen | 0 | 0 | 0 | ||||
| Don't Know | 0 | 0 | 0 | ||||
| 9 | Ideal handwashing practice to be followed by nursing staff in ICU | Pre-contact handwashing with tap water and soap | 0 | 0 | 0 | 14.049 | 0.001 |
| Pre- and post-contact handwashing with tap water and soap | 26 | 24 | 5 | ||||
| Pre- and post-contact handwashing with tap water and soap followed by alcohol rub | 28 | 32 | 35 | ||||
| Handwashing is not needed | 0 | 0 | 0 | ||||
| 10 | Denture hygiene of geriatric ICU patients comprises | Removal of dentures at night and cleaning it once a day | 9 | 5 | 3 | 10.272 | 0.036 |
| Removal of the dentures during sleep and cleaning it preferably after every meal | 41 | 51 | 37 | ||||
| No need for the removal of dentures from the mouth and external cleaning | 4 | 0 | 0 | ||||
| Intraoral cleaning with appropriate tools is sufficient | 0 | 0 | 0 | ||||
| 11 | Where do you store personalized oral hygiene tools for ICU patients? | (A) Personalized air-tight containers | 21 | 29 | 17 | 14.412 | 0.025 |
| (B) Along with their other personal belongings | 20 | 13 | 4 | ||||
| (A) or (B) | 13 | 14 | 19 | ||||
| Does not matter | 0 | 0 | 0 | ||||
| 12 | Maintenance of oral hygiene in infants before the eruption of teeth in a pediatric ICU is done by | (A) Cotton swab to clean the gums | 35 | 42 | 22 | 5.562 | 0.234 |
| (B) Small soft toothbrush | 0 | 0 | 0 | ||||
| Both (A) and (B) | 18 | 13 | 18 | ||||
| No supporting cleaning is required | 1 | 1 | 0 | ||||
| 13 | Did you receive assessment and provision of comprehensive oral care for ICU patients in basic nursing training? | No | 7 | 0 | 0 | 13.054 | 0.001 |
| Yes | 47 | 56 | 40 | ||||
| 14 | What is the ideal patient position for performing oral hygiene care in an unconscious ICU adult patient? | Position the patient in the supine position | 5 | 1 | 2 | 8.262 | 0.082 |
| Position the patient in the prone position | 0 | 0 | 0 | ||||
| Position the patient in the lateral decubitus | 25 | 37 | 28 | ||||
| Position the patient in the elevated supine position | 24 | 18 | 10 | ||||
| Any position | 0 | 0 | 0 | ||||
| 15 | Do you think oral hygiene maintenance is necessary for ICU patients? | Yes | 54 | 56 | 40 | – | – |
| No | 0 | 0 | 0 | ||||
| 16 | Doctor's instruction for oral hygiene care documented in the checklist and your necessary documentation/record for the oral hygiene procedures will improve the practice of oral care by nursing staff | Yes | 54 | 56 | 40 | – | – |
| No | 0 | 0 | 0 | ||||
| 17 | Will the presence of a dental surgeon in the ICU help in the proper maintenance of oral hygiene in ICU patients? | No | 10 | 2 | 3 | 7.203 | 0.027 |
| Yes | 44 | 54 | 37 |
Group I, 0–7 years; group II, 7.1–13.9 years; group III, 14 years and above
Discussion
ICU nurses’ oral care of ventilated patients has been the subject of numerous researches. Only 20% of ICU patients in Sudan had adequate oral hygiene practices, despite having a high degree of understanding (97.4%) about their value. The study highlighted the requirement for an oral care policy and training in ICUs.7 Only 20% of patient charts contained nurses’ notes about dental care, according to research of a similar nature conducted in Iran, where staff shortages and writing obligations meant oral care was not given priority.8 A pre- and post-test educational intervention in Dubai revealed a significantly higher level of awareness and oral hygiene usage among 6,016 participants.9 The results of this study showed that most nurses were aware of the relationship between oral health and systemic health in ICU patients. More than two-thirds of nursing officers were aware that chlorhexidine 0.12% is the recommended oral rinse for ICU patients which was in concordance with a study by Rodrigues et al. in which 75.6% of nurses were aware that chlorhexidine is the best substance for oral hygiene in hospitalized patients.10 Previous studies by Vilela MC et al. and Munro CL et al. recommended 0.12% chlorhexidine mouthwash as the most effective oral hygiene technique rather than teeth brushing in reducing VAP;11,12 however, in contrast, several studies have shown that mechanical interventions, particularly toothbrushing, are more effective than using swabs or an oral wash with chlorhexidine.13–16
Most of the participants in our study agreed that plain saline is the best substance to use when maintaining oral hygiene in ICU patients which was in accordance with studies by Adib-Hajbaghery M et al. and Wei et al. in which 69.2 and 82.7% of individuals used regular saline as their primary mouthwash, respectively.17,18 In contrast the findings of a few recent meta-analyses revealed that using mouthwashes containing povidone-iodine and chlorhexidine rather than saline effectively reduced the incidence of VAP in ICU patients.19–21 These findings support the need for greater dissemination of oral health knowledge and for improvement of Indian nurses’ capacity for evidence-based nursing.
A bulk of THC-I nurses (p = 0.013) in our study chose to brush each ICU patient's teeth for 1–2 minutes (n = 39) and 3–4 minutes (n = 24) which was contrary to a study by Gu WJ et al. that recommended brushing teeth for 1–2 minutes every 12 hours with sodium monofluorophosphate 0.7% paste. Additionally, it suggests using a standard toothbrush and applying 15 mL of 0.12% chlorhexidine solution while following the oral protocol (70–90% compliance); this lowers the rate of VAP from 5.2 to 2.4 infections/1000 ventilator days (p = 0.04).22
Intubated ICU patient exhibits frequent salivation resulting in microbial proliferation. The predominant THC-I nurses (p = 0.003) preferred swabbing and suctioning of the oral fluids, which was consistent with the findings discussed in the study by Wei et al. from 2 years earlier, which showed 91.9% of participants preferred the swabbing technique.18 In the present study, a bulk of group I chose toothbrush, gauze plus tongue depressor, and mouth rinse (p = 0.017) as the required equipment necessary to maintain oral hygiene in an ICU setting which was in contrast with Wei et al. which stated 86.1 and 69.9% of nurses, respectively, selected cotton pellets and cotton swabs as tools to clean the mouth, while less than 50% of nurses used a toothbrush with flushing and suction.18 A study by SM Ibrahim et al. showed that 98.7% of their participants used gauze and tongue depressor to perform oral care.7 These differences may be attributed to the availability of the tools in the government and private ICU setups and their improved knowledge regarding the usage of tools and aids for oral hygiene maintenance.
In a clinical investigation, Yao et al. found that cumulative VAP rates were considerably lower in the experimental group compared to the control group after 7 days of twice-daily teeth brushing with filtered water (17% vs 71%; p = 0.05). To reduce VAP and enhance oral hygiene, they subsequently recommended brushing teeth twice a day with filtered water.23 It appears that using an antibacterial mouthwash is necessary after brushing your teeth. The addition of manual toothbrushing to chlorhexidine oral care, on the contrary, was not helpful in the prevention of VAP according to a recent randomized controlled study.24 A recent review compared powered toothbrushes with manual toothbrushes and concluded that only powered toothbrushes with a rotation oscillation action were more effective at removing plaque and reducing gingivitis than manual brushing.25
Studies have demonstrated local decontamination with topical toothbrushing can eliminate dental plaque and related bacteria while brushing the teeth could also induce the risk of the number of organisms available for transfer from the mouth to subglottic secretions or the lung.26 Investigators have suggested meticulous handwashing for 10 seconds following every patient contact and wearing gloves while coming in physical contact with oral or endotracheal secretions.27 The American Association of Critical Care Nurses, the Centers for Disease Control, the Association for Professionals in Infection Control and Epidemiology, and the Institute for Healthcare Improvement have recommended the implementation of an authentic and comprehensive oral hygiene program a VAP prevention strategy.26 According to a research by Scannapieco et al. routine dental care incorporation into normal practice may reduce VAP by as much as 60%.28 Additional education among ICU nurses is necessary to practice protocol in relation to oral care for the overall wellbeing of patients in ICUs.29 Group II respondents in our study demonstrated adequate denture knowledge regarding their removal at night and proper storage which was in consensus with a study of Jablonski et al.30 in which the majority of the nursing assistants believed that dentures should be removed at night whereas Preston et al.31 showed a knowledge gap among their nursing participants in this context.
The limitations of the study include that the results are not very generalizable because the respondents were only chosen from one Indian province. The representativeness may have been insufficient due to the exclusion of many respondents to improve the data's accuracy and the low percentage of questionnaire completion (62.5%). The use of retrospective and self-reporting in data collection may have led to individuals overestimating their behaviors.
Recommendations
Intensive care nurses can improve the oral care for ICU patients by
Obtaining adequate education and mastering oral care skills,
Enhancing their perceptions and attitudes in oral care for critical patients,
Implementing written standards, guidelines, or protocols that are handy in their work area, and
Based on the existing classification of critical care patients, oral healthcare should be integrated with critical care.
Conclusion
The standard oral hygiene care protocol of patients in ICUs mainly depends on the patient's condition and the nursing staff's awareness and knowledge. The participating nurses knew the importance of oral care however there were knowledge and practice gap observed which requires amendments and should be of concern to the administrators. There are several differences in oral care and procedures for intubated patients in ICU and research shows that there is no consensus. There is a necessity to address ICU patients’ oral health issues with proper protocol. It is urged to conduct studies with larger sample sizes and different hospital settings to better understand the problems of patients and device standard operating procedures for oral healthcare in critically ill patients.
Orcid
Surender Kumar https://orcid.org/0000-0002-2112-3451
Bishnupati Singh https://orcid.org/0000-0002-3762-8606
Amit Vasant Mahuli https://orcid.org/0000-0002-4746-5935
Sanjay Kumar https://orcid.org/0000-0001-5688-4376
Ankita Singh https://orcid.org/0000-0002-6072-505X
Awanindra Kumar Jha https://orcid.org/0000-0003-4793-337X
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Furr LA, Binkley CJ, McCurren C, Carrico R. Factors affecting quality of oral care in intensive care units. J Adv Nurs. 2004;48(5):454–462. doi: 10.1111/j.1365-2648.2004.03228.x. [DOI] [PubMed] [Google Scholar]
- 2.Loesche WJ. Association of the oral flora with important medical diseases. Curr Opin Periodontol. 1997;4:21–28. 9655017 [PubMed] [Google Scholar]
- 3.Li X, Kolltveit KM, Tronstad L, Olsen I. Systemic diseases caused by oral infection. Clin Microbiol Rev. 2000;13(4):547–558. doi: 10.1128/CMR.13.4.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scannapieco FA, Stewart EM, Mylotte JM. Colonization of dental plaque by respiratory pathogens in medical intensive care patients. Crit Care Med. 1992;20(6):740–745. doi: 10.1097/00003246-199206000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Berry AM, Davidson PM, Masters J, Rolls K. Systematic literature review of oral hygiene practices for intensive care patients receiving mechanical ventilation. Am J Crit Care. 2007;16(6):552–562. 17962500 quiz 563. [PubMed] [Google Scholar]
- 6.Faragalla AI, Almaki EJ, Asiri HA. Knowledge, attitude and practice of nurses to oral health care for hospitalized patients in Abha city—Saudi Arabia. Acta Scientific Dental Sci. 2018;2(5):16–23. https://actascientific.com/ASDS/pdf/ASDS-02-0115.pdf Available from: [Google Scholar]
- 7.Ibrahim SM, Mudawi AM, Omer O. Nurses’ knowledge, attitude and practice of oral care for intensive care unit patients. Open J Stomatol. 2015;5(7):179–186. doi: 10.4236/ojst.2015.57023. [DOI] [Google Scholar]
- 8.Javadinia SA, Kuchi Z, Saadatju A, Tabasi M, Adib–Hajbaghery M. Oral care in trauma patients admitted to the ICU: Viewpoints of ICU nurses. Trauma Mon. 2014;19(2):e15110. doi: 10.5812/traumamon.15110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cherian S, Karkada S. Effect of education related to oral care practices on nurses’ knowledge, practice and clinical outcomes of mechanically ventilated patients in Dubai. Int J Nurs Res. 2015;2(1):9–14. https://www.researchgate.net/publication/280561131_Effect_of_education_related_to_oral_care_practices_on_nurses'_knowledge_practice_and_clinical_outcomes_of_mechanically_ventilated_patients_in_Dubai Available from: [Google Scholar]
- 10.da Silva Rodrigues S, Caminha MD, Ferraz MG, de Arruda MA, da Rocha Kozmhinshy VM, de Moraes Guerra CA, et al. Knowledge, attitude and practice of the nursing team regarding oral health care in intensive care units in a reference hospital of Recife, Brazil. Pesqui Bras Odontopediatria Clin Integr. 2016;16(1):129–139. doi: 10.4034/PBOCI.2016.161.14. [DOI] [Google Scholar]
- 11.Vilela MCN, Ferreira GZ, da Silva Santos PS, de Rezende NPM. Oral care and nosocomial pneumonia: A systematic review. Einstein (Sao Paulo) 2015;13(2):290–296. doi: 10.1590/S1679-45082015RW2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Munro CL, Grap MJ, Jones DJ, McClish DK, Sessler CN. Chlorhexidine, toothbrushing, and preventing ventilator-associated pneumonia in critically ill adults. Am J Crit Care. 2009;18(5):428–437. doi: 10.4037/ajcc2009792. quiz 438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeKeyser Ganz F, Fink NF, Raanan O, Asher M, Bruttin M, Nun MB, et al. ICU nurses’ oral-care practices and the current best evidence. J Nurs Scholarsh. 2009;41(2):132–138. doi: 10.1111/j.1547-5069.2009.01264.x. [DOI] [PubMed] [Google Scholar]
- 14.Pedreira ML, Kusahara DM, de Carvalho WB, Núñez SC, Peterlini MA. Oral care interventions and oropharyngeal colonization in children receiving mechanical ventilation. Am J Crit Care. 2009;18(4):319–328. doi: 10.4037/ajcc2009121. quiz 329. [DOI] [PubMed] [Google Scholar]
- 15.Fields LB. Oral care intervention to reduce incidence of ventilator-associated pneumonia in the neurologic intensive care unit. J Neurosci Nurs. 2008;40(5):291–298. doi: 10.1097/01376517-200810000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Hajibagheri A, Fini IA. Mouth care in patients receiving mechanical ventilation: A systematic review. Nurs Midwifery Stud. 2012;1(2):51–61. doi: 10.5812/nms.8543. [DOI] [Google Scholar]
- 17.Adib-Hajbaghery M, Ansari A, Azizi–Fini I. Intensive care nurses’ opinions and practice for oral care of mechanically ventilated patients. Indian J Crit Care Med. 2013;17(1):23–27. doi: 10.4103/0972-5229.112154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wei X, Jing M, Zhang X, Li C, Li L. Nurses’ practice and educational needs in oral care for postoperative patients with oral cancer in ICUs: A multicenter cross-sectional study. BMC Oral Health. 2022;22(1):389. doi: 10.1186/s12903-022-02426-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang TT, Tang SS, Fu LJ. The effectiveness of different concentrations of chlorhexidine for prevention of ventilator-associated pneumonia: A meta-analysis. J Clin Nurs. 2014;23(11–12):1461–1475. doi: 10.1111/jocn.12312. [DOI] [PubMed] [Google Scholar]
- 20.Zhao T, Wu X, Zhang Q, Li C, Worthington HV, Hua F. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database Syst Rev. 2020;12(12):CD008367. doi: 10.1002/14651858.CD008367.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dale CM, Rose L, Carbone S, Smith OM, Burry L, Fan E, et al. Protocol for a multi-centered, stepped wedge, cluster randomized controlled trial of the de-adoption of oral chlorhexidine prophylaxis and implementation of an oral care bundle for mechanically ventilated critically ill patients: The CHORAL study. Trials. 2019;20(1):603. doi: 10.1186/s13063-019-3673-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gu WJ, Gong YZ, Pan L, Ni YX, Liu JC. Impact of oral care with versus without toothbrushing on the prevention of ventilator-associated pneumonia: A systematic review and meta-analysis of randomized controlled trials. Crit Care. 2012;16(5):R190. doi: 10.1186/cc11675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yao LY, Chang CK, Maa SH, Wang C, Chen CC. Brushing teeth with purified water to reduce ventilator-associated pneumonia. J Nurs Res. 2011;19(4):289–297. doi: 10.1097/JNR.0b013e318236d05f. [DOI] [PubMed] [Google Scholar]
- 24.Lorente L, Lecuona M, Jiménez A, Palmero S, Pastor E, Lafuente N, et al. Ventilator-associated pneumonia with or without toothbrushing: A randomized controlled trial. Eur J Clin Microbiol Infect Dis. 2012;31(10):2621–2629. doi: 10.1007/s10096-012-1605-y. [DOI] [PubMed] [Google Scholar]
- 25.Robinson PG, Deacon SA, Deery C, Heanue M, Walmsley AD, Worthington HV, et al. Manual versus powered toothbrushing for oral health. Cochrane Database Syst Rev. 2005;(2):CD002281. doi: 10.1002/14651858.CD002281.pub2. doi: 10.1002/14651858.CD002281.pub2. Update in: Cochrane Database Syst Rev. 2014;6:CD002281. [DOI] [PubMed] [Google Scholar]
- 26.Khezri HD, Zeydi AE, Firouzian A, Baradari AG, Mahmoodi G, Kiabi FH, et al. The importance of oral hygiene in prevention of ventilator-associated pneumonia (VAP): A literature review. Int J Caring Sci. 2014;7(1):12–23. http://internationaljournalofcaringsciences.org/docs/3.%20Darvishi-i-1.pdf Available from: [Google Scholar]
- 27.Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R, CDC; Healthcare Infection Control Practices Advisory Committee Guidelines for preventing health-care-associated pneumonia, 2003: Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep. 2004;53(RR-3):1–36. 15048056 [PubMed] [Google Scholar]
- 28.Scannapieco FA, Wang B, Shiau HJ. Oral bacteria and respiratory infection: Effects on respiratory pathogen adhesion and epithelial cell proinflammatory cytokine production. Ann Periodontol. 2001;6(1):78–86. doi: 10.1902/annals.2001.6.1.78. [DOI] [PubMed] [Google Scholar]
- 29.Miranda AF, de Paula RM, de Castro Piau CG, Costa PP, Bezerra AC. Oral care practices for patients in Intensive Care Units: A pilot survey. Indian J Crit Care Med. 2016;20(5):267–273. doi: 10.4103/0972-5229.182203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jablonski RA, Munro CL, Grap MJ, Schubert CM, Ligon M, Spigelmyer P. Mouth care in nursing homes: Knowledge, beliefs, and practices of nursing assistants. Geriatr Nurs. 2009;30(2):99–107. doi: 10.1016/j.gerinurse.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Preston AJ, Punekar S, Gosney MA. Oral care of elderly patients: Nurses’ knowledge and views. Postgrad Med J. 2000;76(892):89–91. doi: 10.1136/pmj.76.892.89. [DOI] [PMC free article] [PubMed] [Google Scholar]


