Abstract
Aim and background
Imaging is indispensable to the diagnostic and treatment process. By facilitating access to rapid timely image interpretation, teleradiology plays a prominent role in improving access, quality of critical care, and management of the patients in intensive care units (ICU). The aim of the study is to investigate the role of teleradiology in ICU patient care and management.
Materials and methods
In our study, a total of 22,081 studies of a cohort of 14,900 patients which had been transmitted from intensive care units of 80 hospitals located across the United States of America through a teleradiology reporting workflow, were interpreted by the American Board Certified Radiologists empanelled by a teleradiology service provider, located in India.
Results
Among all modalities, the highest percentage of studies performed were computed tomography scan (47%) followed by radiographs (37.22%). Out of 22,081 cases under the study, 16,582 cases were reported during nighttime with a mean turnaround time (TAT) of 46.66 minutes 95% CI (46.27–47.04) while 5,499 cases were reported during daytime with a mean TAT of 44.66 minutes 95% CI (45.40–43.92).
Conclusion
Setting up teleradiology service connectivity with a teleradiology service provider located in India, providing high-quality diagnostic interpretations and lower turnaround time with the ICUs in the US hospitals reduces the interval to intervention time and leads to efficient patient care management. Moreover, it also provides time advantage for US hospitals when on-site radiologists at night are unable to provide immediate coverage.
Clinical significance
The ICU teleradiology service model designed in the study would greatly help overcome the shortfall of radiologists in the hospitals, provide better patient management and care by quality reporting in short turnaround time, not only during daytime but also in the night hours or on holidays when on-site radiologists are unable to provide immediate coverage.
How to cite this article
Rao P, Mathur N, Kalyanpur A. Utilization of Teleradiology by Intensive Care Units: A Cohort Study. Indian J Crit Care Med 2024;28(1):20–25.
Keywords: Healthcare, Intensive care units, Radiologist, Teleradiology, Turnaround time
Highlights
Setting up teleradiology service connectivity with a teleradiology service provider located in India, providing high-quality diagnostic interpretations and lower turnaround time, with the intensive care units in the US hospitals lowers the interval to intervention time and leads to efficient patient care management. It also provides time advantage to the US hospitals.
The learnings of the international ICU teleradiology model system in this study could be leveraged for the deployment of ICU teleradiology services in India would greatly benefit smaller towns where the critical shortage of radiologists places an impediment in the path of care and management of critically ill patients.
Introduction
Teleradiology is a subset of telemedicine which has made a significant contribution to clinical patient care. By transmitting imaging studies over global networks from the site of origin to the location of the radiologist facilitates access to different categories of radiology subspecialists, such as neuroradiologists, pediatric radiologists, and msculoskeletal radiologists when the same are not available in the hospital of care.1 It also ensures that studies performed after hours when the radiologist may not be available within the hospital premises are interpreted contemporaneously. It is therefore a technology that has the potential to improve outcomes for critically ill patients by providing timely interpretation and advice regarding critical value findings detected on imaging.
The intensive care unit (ICU) also known as an intensive therapy unit, is a multidisciplinary speciality in the hospital committed to cater to patients with severe or life-threatening illnesses and injuries, who require constant care and close supervision from life support equipment, and life-sustaining therapies or medication. Within the broader domain of intensive care, a neonatal intensive care unit (NICU) specializes in the care of ill or preterm newborn infants and surgical intensive care units specialize in the care of postoperative patients or critically ill surgical patients.2 The specialty of critical care emerged in the 1950s during the polio epidemic in the world. In India, during the early 1970s, the critical care units were designed and equipped dedicatedly to provide intensive care to patients with acute myocardial infarction and ischemic heart disease. Ventilator support was provided as a terminal treatment plan.3 However, gradually, in the later years, a significant improvement in the standard of care was observed in the larger teaching and private hospitals. Critical care or intensive care medicine has since been considered as a separate superspecialty. Taking into account of the need and merits of an ICU, regulatory bodies and Critical Care Medicine Societies across the world such as the Society for Critical Care Medicine (SCCM) in the US and the Medical Council of India (MCI) (later replaced by the National Medical Commission in India) and National Board of Examination and Indian Society for Critical Care Medicine (ISCCM) have designed well-structured training programs in critical care in order to award separate degrees/diploma/certificates to develop doctors called Intensivists.4 The intensivists are medical practitioners who are specialized and trained to cater to critically ill and multi- specialty patients in the intensive care unit (ICU).5
Despite the advances, the shortage of ICU units, ICU beds, clinicians, and radiologists has slowed the pace of treatment for critically ill patients. According to the annual survey of hospitals conducted by American Hospital Association in 2023, the total number of staffed beds in all US hospitals are 919,649.6 The ICU beds are reported to be 107,276 in number.7 A study by Kapoor et al. estimated that there are approximately 19 lakh hospital beds and 95,000 ICU beds in India which indicates a huge gap in a demand and supply for critical care facilities and providers of all levels. Telemedicine in the ICU emerged out of the necessity to bridge this gap.8 Teleradiology has been heralded as a promising solution and revolutionized the patient outcome by providing timely diagnostic services not only to critically ill patients in the ICU but also to emergency presentations during the night hours and under an unprecedented global situation such as the COVID-19 pandemic. Teleradiology permitted radiologists to work from home and minimized physical interaction with patients which resulted in diminishing the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) especially in healthcare settings. It also helps offset burnout, enhances productivity and bring out 24/7 access even to the rural areas that may not have additional full-time staff.9,10
With the advancement in imaging and data transfer techniques, teleradiologists have become an integral part of the patient's clinical team.11 In the ICU, where the patients are critically ill, many with support devices, the treatment cannot be delayed. In the case of critical nonavailability of on-site radiologists, the scans taken on ICU patients can be transmitted in real time to a teleradiologist who can interpret and report them remotely from anywhere at any time. Thus, the teleradiology system would be advantageous because of speedy and accurate reporting of clinical images, continuous availability of teleradiologists for consultation purposes, and a consequent decrease in the number of missed findings,12 rapid initiation of life-sustaining therapies, reduction in the mortality and ICU length of stay (LOS) and lowering the costs for critically ill patients.13 Teleradiology can also be a cost-effective solution for ICUs, particularly those with limited resources. ICUs can use teleradiology services on an as-needed basis rather than hiring a full-time radiologist, thereby cutting expenditures.
The scenario is gradually improving with the progress in teleradiology technology and expertise. The picture archiving and communication system (PACS) is a database used for acquiring, transporting, storing, and electronically displaying all imaging studies of the patients, which can be easily and immediately accessed by the clinician and a remotely located teleradiologist. It ensures automatic categorization, chronological ordering, correct orientation, and labeling of the images.14 The hospital and radiological information systems (HIS and RIS) provide access to patient information in real time to the radiologists, enhance the quality of patient care by reducing errors and help in clinical decision-making.15
Teleradiology has been utilized by ICUs to ease the challenges of geographic and nocturnal coverage. A further advantage of teleradiology is that it enables many smaller hospitals who struggle to maintain adequate off-hour and specialist coverage to quickly provide round the clock, high-quality interpretations. Teleradiology had a major impact in decreasing report turnaround time,16 and in improving service levels in ICUs. Turnaround time is the time interval between the images/scans of the patients are uploaded in the telereporting platform, accessed, read and interpreted by the radiologist and report is compiled and uploaded in the same telereporting platform or when the radiologist has signed off.
Aims and Objectives
The objective of this retrospective study is to investigate the role or benefits of teleradiology in ICU patient care and management.
Materials and Methods
The study was carried out between March 2019 and August 2022 and involved the analysis of 22,081 imaging studies of a cohort of 14,900 patients, originating from ICU and NICU of 80 hospitals across the United States of America and interpreted by the American Board Certified Radiologists empanelled by a teleradiology service provider, headquartered in Bengaluru, India. The DICOM images of different modalities such as computed tomography (CT), magnetic resonance imaging (MRI), ultrasonography (US), radiography and nuclear medicine (NM) for various procedures of the ICU and NICU patients were uploaded onto the telereporting workflow platform “RADspa,” a cloud-based Radiology Information System (RIS)/Picture Archival and Communication System (PACS) system over a high-speed internet connection, generating a worklist. The radiologists interpreted the images and compiled the reports which were transmitted back to the client hospitals over the same workflow platform. The information about the patient demographics, prior reports, patient clinical and surgical history records, etc. were also uploaded into the RIS so that they were available to the radiologists along with the images. The patients who had registered in ICUs were included in the study. They were classified according to the demographic information such as age and gender and their clinical history. The mean age and turnaround time for reporting the cases were calculated. The total number of studies and the mean TAT for the cases transmitted from the US hospitals and telereported during night as well daytime were calculated. An approval has been taken from the institutional review board for this retrospective study.
Results
A retrospective study was carried out on a cohort of 14,900 patients over the duration of three and a half years starting from March 2019. A total of 22,081 studies of different imaging modalities of patients were transmitted from 80 hospitals across the United States of America through RADspa and interpreted by radiologists. Out of 14,900 patients, 14,000 were from ICU and 900 were from NICU. And 45.77 % were females and 54.23% were males.
The age of the patients in this study ranged from 1 day old to 103 years. The mean age of the cases was 59.65 years (22.84 SD) confidence interval CI (95%) (59.35–59.95). A significant number of patients (43.93%) were between 61 and 80 years of age (Fig. 1).
Fig. 1.

Age-group categorization of the ICU patients
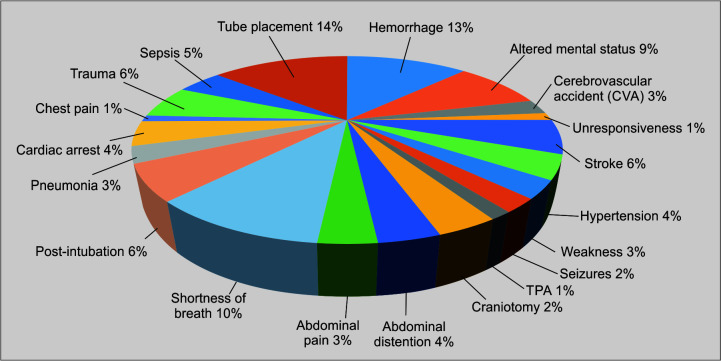
According to the diseases and complications, various imaging techniques were performed on the patients to help diagnosis and treatment decisions (Table 1). About 73.5% patients had undergone single imaging (NCCT or CTA or CT perfusion). About 5.5% patients had undergone concurrent multiple imaging studies while 21% patients had followed up. The patients had undergone various procedures under different modalities, the results are given in Table 1. Teleradiology services were provided to the patients under different clinical situations (Fig. 2). The findings of the scans interpreted by teleradiologists are given in Table 2. Prior images and reports were also loaded into the telereporting platform so that they were available to the radiologists along with the scans. Out of 22081 cases, prior images were available for 14056 cases and prior reports were available for 363 cases.
Table 1.
Breakdown of the number of studies for different procedures and modalities
| Modality procedure | NM | CT | Radiographs | MR | US |
|---|---|---|---|---|---|
| Abdomen | 57 | 2405 | 794 | 26 | 602 |
| Angiogram | – | 1532 | – | 229 | – |
| Brain/head/skull | 21 | 4963 | 7 | 1064 | 262 |
| Perfusion | – | 69 | – | – | – |
| Chest/Lung | 24 | 810 | 7132 | 1 | 14 |
| Neck | – | 51 | 1 | 3 | 69 |
| Soft neck tissue | – | 52 | – | – | 9 |
| Facial bones/maxillofacial | – | 52 | 6 | 2 | – |
| Lower extremities | – | 142 | 138 | 25 | 423 |
| Upper extremities | – | 36 | 8 | 4 | 128 |
| Spine | – | 225 | 10 | 256 | 6 |
| Venogram | – | 15 | – | 36 | – |
| Arteries | – | – | – | – | 3 |
| Brachial plexus | – | – | – | 5 | – |
| Pituitary | – | – | – | 1 | – |
| Venous Doppler | – | – | – | – | 181 |
| Babygram | – | – | 121 | – | – |
| Bone survey | – | – | 2 | – | – |
| Cytogram/urogram/KUB | – | 11 | – | – | – |
| Obstetrics | – | 18 | – | – | 30 |
| Total | 102 | 10381 | 8219 | 1652 | 1727 |
Fig. 2.
Distribution of cases based on patients’ clinical presentation and symptoms
Table 2.
Finding-wise segregation of ICU cases of different modalities
| Modality | Procedure | Indications | No. of cases |
|---|---|---|---|
| NCCT | Head | Hemorrhage | 2024 |
| Fracture | 156 | ||
| Midline shift | 869 | ||
| Mass effect | 849 | ||
| Dense MCA | 57 | ||
| Infarct | 529 | ||
| Abdomen | Aneurysm | 97 | |
| Bowel obstruction | 137 | ||
| Radiographs | Chest | Opacities | 3411 |
| Edema | 1829 | ||
| Pneumonia | 5333 | ||
| Pleural effusion | 2555 | ||
| Atelectasis | 1842 | ||
| Cardiomegaly | 1851 | ||
| Consolidation | 1088 | ||
| Pneumothorax | 386 | ||
| USG | Abdomen | Cholelithiasis | 63 |
| Venous Doppler | Deep vein thrombosis | 66 | |
| Head | Hemorrhage | 55 |
The mean turnaround time (TAT) for the report to reach the client hospital once the images had been received on the worklist with the use of teleradiology is indicated in Tables 3 and 4. The total number of cases from different modalities and the mean TAT for reporting them during night as well daytime were calculated (Table 3). Comparison of the number of studies telereported during pre-COVID, COVID, and post-COVID times and during night and daytime and their mean TAT values was also done (Table 4).
Table 3.
Breakdown of cases from different modalities and mean TAT for reporting during night and daytime from teleradiology service provider located in India
| Modality | Night reporting | Day reporting | ||
|---|---|---|---|---|
| Number of studies | Mean TAT | Number of studies | Mean TAT | |
| NM | 71 | 43.42 min 95% CI (39.11–47.73) | 31 | 48.67 min 95% CI (40.79–56.56) |
| CT | 8716 | 46.66 min 95% CI (46.07–47.25) | 1665 | 46.44 min 95% CI (45.38–47.49) |
| Radiographs | 5365 | 46.94 min 95% CI (46.40–47.48) | 2854 | 43.07 min 95% CI (41.89–44.24) |
| MR | 1178 | 52.49 min 95% CI (51.09–53.89) | 474 | 53.11 min 95% CI (50.87–55.35) |
| US | 1252 | 41.64 min 95% CI (40.53–42.74) | 475 | 41.06 min 95% CI (39.19–42.92) |
| Total | 16582 | 46.66 min 95% CI (46.04–47.27) | 5499 | 44.66 min 95% CI (43.92–45.39) |
Table 4.
Comparison of number of studies telereported during Pre-COVID, COVID, and Post-COVID times during night and daytime and their mean TAT values
| Time period | Nighttime reporting | Daytime reporting | ||
|---|---|---|---|---|
| Number of studies | Mean TAT | Number of studies | Mean TAT | |
| Pre-COVID (Mar 2019–Feb 2020) | 5688 | 51.09 min 95% CI (50.52–51.66) | 2026 | 49.43 min 95% CI (48.40–50.46) |
| COVID (Mar 2020–Feb 2022) | 8678 | 43.99 min 95% CI (43.43–44.55) | 2927 | 41.36 min 95% CI (40.27–42.45) |
| Post-COVID (Mar 2022–Aug 2022) | 2216 | 47.29 min 95% CI (46.36–48.21) | 546 | 47.11 min 95% CI (45.25–48.98) |
| Total | 16582 | 46.66 min 95% CI (46.27–47.04) | 5499 | 44.66 min 95% CI (43.92–45.39) |
Discussion
Intensive care units frequently deal with challenging situations that call for quick action such as those involving severely ill patients or cases of trauma and or situations where specialized knowledge, such as in neuroimaging or musculoskeletal imaging is required. The concept of electronic ICU or eICU or tele-ICU has emerged as a novel paradigm to cater to critical care patients where the telemedicine services are utilized to gain from medical expertise and provide 24/7 proactive care by intensivist-led teams of ICU carers.17,18 With the aid of teleradiology, a subset of telemedicine, ICUs can quickly and accurately evaluate radiological images with immediate access to experienced and subspecialty trained radiologists with great expertise in particular fields.
Imaging is indispensable for quick and accurate patient management decisions in the intensive care unit (ICU) setting. The different types of imaging modalities used in critical care are plain radiography (CR/DR), CT, ultrasound, magnetic resonance imaging (MRI) and nuclear medicine resonance (NMR).
The radiograph is the most commonly requested imaging examination for initial evaluation and essential for decision-making process in ICU. The chest radiograph is essential especially for the patients who are suffering from cardiopulmonary disorders or are on a ventilator. Abdominal radiographs are usually conducted for ICU patients that are suspected to have bowel obstruction based on abdominal distension.19 In our study, a total of 8219 radiographic studies were received (Table 1). The number of chest radiographs (7132) were far higher than the abdominal radiographs (794). 292 abdominal and 2172 chest radiographs were performed to monitor the positioning of nasogastric tube and endotracheal tubes. Generally, these are done to prevent the malpositioning and complications related to the regular insertion and use of endotracheal and nasogastric tubes, intravenous catheters, chest drains, pacemakers, and pleural aspiration. In this study, 6582 studies were performed to monitor central line position and endotracheal tube positions. About 737 chest radiographs indicated malpositioning. This is marked as critical finding and also conveyed over direct verbal communication when immediate urgent action is warranted. The radiographs are evaluated to monitor the patients with clinical symptoms of respiratory distress, pneumonia, cardiac arrest, chest pain, sepsis, hemorrhage, altered mental status, hypertension/hypotensive, seizures, unresponsiveness and abdominal pain, distention/bowel obstruction (Fig. 2).20 Out of 7132 chest radiographs performed, 5333 (75%) had positive findings for pneumonia, 1829 (25%) cases were positive for pulmonary edema and 386 (5.44%) cases showed positive results for pneumothorax (Table 2).
Computed tomography is preferred for complex and challenging clinical situations. However, CT has become a mainstay of imaging in the ICU for critically ill patients to diagnose and monitor the progression of certain conditions. In our study, among all modalities, the highest percentage of studies received were CT scans (47%) followed by radiographs (37.22%) as depicted in Tables 1 and 2. CT scans of the head, abdomen, chest, neck, spine, pelvis, upper and lower extremities were received. CT head were performed for the patients having clinical history of weakness, altered mental status, trauma and stroke (Fig. 2). Out of 4963 head CTs performed, 40% (2024) of the cases had positive finding for hemorrhage which is a medical emergency and needed immediate neurosurgical attention. And 17% (869) of the cases showed midline shift while 10% of the cases showed positive findings for infarct on the head CT scan. About 97 out of 2405 CT abdomen scans showed aneurysms while 137 scans had positive findings for bowel obstruction (Table 2).
In terms of being an effective modality in triaging patients, Ultrasound is also increasingly included into the intensive care management. During our study, 1727 ultrasonography (USG) studies (abdomen, chest, neck, upper and lower extremities) were performed (Table 1). About 20% of USG abdomen scans were positive for cholecystitis while 11% were positive for deep vein thrombosis (DVT) (Table 2).
Although imaging is absolutely fundamental for the patient management in the ICU, the shortage and unavailability of on-site radiologists presents an impediment to early diagnosis. The few available radiologists may work proficiently during daytime but it is difficult and expensive to recruit radiologists for nighttime working hours as the number of studies performed is low and their productivity cannot be maintained at the same levels as during the day. It is difficult to maintain round the clock radiology services in a single hospital unit as recruiting more radiologists would mean more higher salaries. Offshore teleradiology services by the US Board certified radiologists has the potential to address this problem by delivering quality and timely radiological interpretations in his/her daytime help providing time advantage for the US hospitals when on-site radiologists at night are unable to provide immediate coverage.21 Furthermore, offshore night-hawk teleradiology services provide support in the radiological interpretation during the US daytime. The utilization of teleradiology services increases accessibility,22 shortens the turnaround time for reports23,24 but also brings down the diagnostic error rate, lowers the reporting and patient travel cost,25,26 and improves the quality-of-life and workload distribution for staff.27 In this retrospective study, out of 22081 cases, 16582 cases were reported at nighttime from India with a mean turnaround time (TAT) of 46.66 minutes 95% CI (46.27–47.04) while 5499 cases were reported at daytime with a mean TAT of 44.66 minutes 95% CI (45.40–43.92).
The mean turnaround time (TAT) for the report to reach the client hospital once the images had been received on the worklist for radiographs was 45.87 minutes 95% CI (45.42–46.32), CT studies was 46.86 minutes 95% CI (46.45–47.27), MR studies was 52.71 minutes 95% CI (51.52–53.89), NM studies was 44.95 minutes 95% CI (41.18–48.73), USG studies was 41.51 minutes 95% CI (40.56–42.46) and for all the studies was 46.39 minutes 95% CI (46.11–46.67). Further, mean TAT for reporting cases from different modalities during night and daytime was calculated.
The teleradiology services helped in coping up with COVID-19 pandemic by organizing radiologists’ work pressure, enhancing effectiveness and quality of radiological services, providing their around-the-clock accessibility and thus improving patients outcomes. In this retrospective study, an 52.56% increase was observed in the number of studies which were telereported during COVID pandemic with a mean TAT of 43.99 min 95% CI (43.43–44.55) as compared with the pre-COVID times when mean TAT was 51.09 min 95% CI (50.52–51.66) (Table 4).
In the case of critical findings where urgent patient management is required, referring physicians were made aware of these findings either by direct telephonic communication with the radiologist or the call center team of the teleradiology service provider.28 In our study, a total of 3792 calls were done. Out of these, 206 direct calls were made between the radiologist and the referring physician while 216 calls were done by call center team to report some positive finding and 26 calls for some negative findings. Besides these, 1298 calls were incomplete or partially successful during verbal communication due to the referring physician being busy. Further, 1384 calls were done for the verbal communication of important findings to the assistants at hospitals who ensured further actions.
Some of the challenges faced during telereporting of a few cases where interpretation time exceeded the limits of compliance were primarily process-bound and included the lack of pertinent prior images, slow image transmission, an unexpected surge of cases, complex studies with multiple findings necessitating more interpretation time, errors in the order entry that needed to be corrected, delayed order entry, and calls that were put on hold from the client hospital during verbal communication.
Conclusion
Teleradiology is a state-of-the-art technology to streamline the workflow of interpreting and reporting the scans of the patients transmitted from a distant location. Setting up teleradiology service connectivity with a teleradiology service provider located in India, providing high diagnostic quality standards with the intensive care units in the US hospitals lowers the interval to intervention time and leads to efficient patient care management. The international ICU teleradiology model detailed in this study provides teleradiology services to the US hospitals, help providing time advantage for US hospitals when on-site radiologists at night are unable to provide immediate coverage. This paves the way to start a similar teleradiology system in India. It is of utmost importance to understand about how the technology of teleradiology can be applied best and leveraged to maximize its value and effectiveness. The success of this telehealth model for ICU care depends on the degree of collaboration between remote service provider and clinicians. The learnings of the international ICU teleradiology model system in this study could be leveraged for the deployment of ICU teleradiology service system in India even without the time zone advantage, as volumes in individual hospitals may be low and teleradiologists covering multiple hospitals in a single night shift would offset radiologist shortage issue and increase cost-effectiveness. It would greatly benefit smaller towns where the critical shortage of radiologists places an impediment in the path of care and management of critically ill patients.
Clinical Significance
The ICU teleradiology service model designed in the study would greatly help overcome the shortfall in the number of radiologists in the hospitals. It would also help address burnout issues, amend workload distribution, and enhance the quality-of-life for the on-site radiologists, provides better patient management and care by quality reporting in short turnaround time. Further, the utilization of teleradiology services delivered by Board certified radiologists would also benefit in night hours or on holidays when on-site radiologists are unable to provide immediate coverage. Teleradiology also help in providing super-specialist access in ICUs.
Orcid
Pallavi Rao https://orcid.org/0009-0009-7777-2504
Neetika Mathur https://orcid.org/0009-0002-8884-2060
Arjun Kalyanpur https://orcid.org/0000-0003-2761-7273
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Improvement of patient care through teleradiology. Smart Teleradiology June 2, 2021. https://smartteleradiology.com/improvement-of-patient-care-through-teleradiology/ Available at:
- 2.Neonatal Intensive Care, Primary Health Care: Open Access. https://www.iomcworld.org/medical-journals/neonatal-intensive-care-56251.html ISSN-2167-1079. Available at:
- 3.Yeolekar ME, Mehta S. ICU care in India – status and challenges. J Assoc Physicians India. 2008;56:221–222. 18702381 [PubMed] [Google Scholar]
- 4.Rungta N, Zirpe KG, Dixit SB, Mehta Y, Chaudhry D, Govil D, et al. Indian Society of Critical Care Medicine Experts Committee Consensus Statement on ICU Planning and Designing, 2020. Indian J Crit Care Med. 2020;24(Suppl 1):S43–S60. doi: 10.5005/jp-journals-10071-G23185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.https://en.wikipedia.org/wiki/Intensivist
- 6.Fast Facts on U.S. Hospitals. 2023. https://www.aha.org/statistics/fast-facts-us-hospitals
- 7.https://www.nlsql.com/blog/post/number-of-icu-beds-in-the-us/
- 8.Kapoor G, Hauck S, Sriram A, Joshi J, Schueller E, Frost I, et al. Health Policy. 2020. State-wise estimates of current hospital beds, intensive care unit (ICU) beds and ventilators in India: are we prepared for a surge in COVID-19 hospitalizations? [DOI] [Google Scholar]
- 9.Rackimuthu S, Hasan MM, Ray I, Sahito AM, Chawla P, Ghosh D. Teleradiology in India during the COVID-19 pandemic: merits, pitfalls and future perspectives. Health Policy Plan. 2022;37(9):1203–1206. doi: 10.1093/heapol/czac045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalyanpur A. 2020 April 19. 4 Benefits of teleradiology in the coronavirus pandemic.https://www.auntminnie.com/imaging-informatics/enterprise-imaging/pacs-vna/article/15625706/4-benefits-of-teleradiology-in-the-coronavirus-pandemic Available from: [Google Scholar]
- 11.Trotman-Dickenson B. Radiology in the intensive care unit (part 2) J Intensive Care Med. 2003;18(5):239–252. doi: 10.1177/0885066603254087. [DOI] [PubMed] [Google Scholar]
- 12.Huda W, Honeyman JC, Palmer CK, Frost MM, Staab EV. Computed radiography and film digitizer inputs to an intensive care unit teleradiology system: An image quality comparison. Acad Radiol. 1996;3(2):110–114. doi: 10.1016/s1076-6332(05)80375-7. [DOI] [PubMed] [Google Scholar]
- 13.Vranas KC, Slatore CG, Kerlin MP. Telemedicine coverage of intensive care units: A narrative review. Annals ATS. 2018;15(11):1256–1264. doi: 10.1513/AnnalsATS.201804-225CME. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strickland NH. PACS (picture archiving and communication systems): filmless radiology. Arch Dis Child. 2000;83(1):82–86. doi: 10.1136/adc.83.1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lingamallu K, Nayakvadi S. Role of HIS and RIS in improving quality of patient care. Int J Collab Res Intern Med Public Health. 2018;9(7):725–734. Corpus ID: 52022798. [Google Scholar]
- 16.Kalyanpur A. The role of teleradiology in emergency radiology provision. Radiol Manage. 2014;36(3):46–49. 25004687 [PubMed] [Google Scholar]
- 17.Celi LA, Hassan E, Marquardt C, Breslow M, Rosenfeld B. The eICU: it's not just telemedicine. Crit Care Med. 2001;29(8 Suppl):N183–N189. doi: 10.1097/00003246-200108001-00007. [DOI] [PubMed] [Google Scholar]
- 18.Shahpori R, Hebert M, Kushniruk A, Zuege D. Telemedicine in the intensive care unit environment – A survey of the attitudes and perspectives of critical care clinicians. J Crit Care. 2011;26(3):328.e9–e15. doi: 10.1016/j.jcrc.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 19.Porté F, Basit R, Howlett D. Imaging in the intensive care unit. Surgery (Oxford) 2009;27(11):496–499. doi: 10.1016/j.mpsur.2009.09.002. [DOI] [Google Scholar]
- 20.Ganapathy A, Adhikari NK, Spiegelman J, Scales DC. Routine chest x-rays in intensive care units: a systematic review and meta-analysis. Crit Care. 2012;16(2):R68. doi: 10.1186/cc11321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burute N, Jankharia B. Teleradiology: The Indian perspective. Indian Journal of Radiology and Imaging. 2009;19(01):16–18. doi: 10.4103/0971-3026.45337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Char A, Kalyanpur A, Puttanna Gowda VN, Bharathi A, Singh J. Teleradiology in an inaccessible area of northern India. J Telemed Telecare. 2010;16(3):110–113. doi: 10.1258/jtt.2009.009007. [DOI] [PubMed] [Google Scholar]
- 23.Kennedy S, Bhargavan M, Sunshine JH, Forman HP. The effect of teleradiology on time to interpretation for CT pulmonary angiographic studies. J Am Coll Radiol. 2009;6(3):180–189.e1. doi: 10.1016/j.jacr.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 24.Zabel AOJ, Leschka S, Wildermuth S, Hodler J, Dietrich TJ. Subspecialized radiological reporting reduces radiology report turnaround time. Insights Imaging. 2020;11(1):114. doi: 10.1186/s13244-020-00917-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Plathow C, Walz M, Essig M, Engelmann U, Schulz-Ertner D, Delorme S, et al. Teleradiology: Economic research analysis of CT investigations in a small hospital. Rofo. 2005;177(7):1016–1026. doi: 10.1055/s-2005-858265. [DOI] [PubMed] [Google Scholar]
- 26.Johansen I, Breivik E. Is teleradiology service in primary health care cost-effective? Tidsskr Nor Laegeforen. 2004;124(19):2490–2492. 15477888 [PubMed] [Google Scholar]
- 27.Coppola F, Bibbolino C, Grassi R, Pierotti L, Silverio R, Lassandro F, et al. Results of an Italian survey on teleradiology. Radiol Med. 2016;121(8):652–659. doi: 10.1007/s11547-016-0640-7. [DOI] [PubMed] [Google Scholar]
- 28.Honig SE, Honig EL, Babiarz LB, Lewin JS, Berlanstein B, Yousem DM. Critical findings: Timing of notification in neuroradiology. AJNR Am J Neuroradiol. 2014;35(8):1485–1492. doi: 10.3174/ajnr.A3918. [DOI] [PMC free article] [PubMed] [Google Scholar]