Abstract
Background:
Opioid misuse during pregnancy has been associated with adverse infant outcomes including preterm birth, stillbirth, and neonatal opioid withdrawal syndrome. The Pregnancy Risk Assessment Monitoring System (PRAMS) is an on-going state-based surveillance system of maternal behaviors, attitudes, and experiences prior to, during, and after pregnancy.
Methods:
We analyzed qualitative comments related to opioid use during pregnancy collected in 2016 from an open-ended prompt at the end of the PRAMS survey in 35 states (N = 40,408). Key word searches were conducted on the open-ended responses (n = 9,549) to identify opioid-related content with an automated function using Microsoft Excel. All responses from the initial screening (n = 1,035) were manually reviewed, and 69 responses were confirmed to relate to the respondent’s personal experience with opioid use during pregnancy. Content analysis was conducted by 3 independent coders; key themes were compiled, discussed, and finalized by the coding team.
Results:
Five key themes related to opioid use during pregnancy were identified: (1) gratitude for treatment, recovery, and healthy infants; (2) pregnancy as motivation to seek treatment; (3) difficulty finding prenatal care providers with training in substance use disorders; (4) concern about the effects of treatment on the infant; and (5) experiences of discrimination and stigma in the hospital around the time of delivery.
Conclusions:
Women may be aware of the potential impact of opioid use during pregnancy on the health of their infants and motivated to seek treatment. Findings may help inform new and ongoing initiatives designed to improve care and reduce stigma for women needing or seeking treatment.
Keywords: PRAMS, qualitative data, opioids, pregnancy, stigma
Introduction
The United States is facing an opioid crisis that affects individuals across the lifespan.1 The effects range from the increased incidence of neonatal abstinence syndrome (NAS) among newborns2 to an epidemic of opioid-involved overdose deaths.3 Opioid use disorder among pregnant women, as documented at hospital delivery, increased significantly from 1.5 per 1,000 delivery hospitalizations in 1999 to 6.5 per 1,000 delivery hospitalizations in 2014.4 The cost of treating infants diagnosed with NAS also increased from 1.6% of the hospital costs for all Medicaid births in 2004 to 6.7% in 2014.5 In 2016, the total in-hospital cost for treating infants diagnosed with NAS was $572.7 million with Medicaid shouldering the bulk (83%) of this cost.6
As national, state, and local leaders work to address the opioid crisis, the Centers for Disease Control and Prevention (CDC) has identified five strategies to guide the response to the opioid overdose epidemic. These strategies include conducting surveillance and research; building state, local, and tribal capacity; supporting providers, health systems, and payers; partnering with public safety; and empowering consumers to make safe choices.7 The Pregnancy Risk Assessment Monitoring System (PRAMS) survey data supports CDC’s surveillance and research strategy and is important to help identify effective prevention activities and guide resource allocation. PRAMS quantitative data were recently analyzed to examine prescription opioid pain reliever use during pregnancy.8 PRAMS also collects a limited amount of qualitative data which is also available for analysis and can complement quantitative findings.
Qualitative research offers a critical lens through which to view this issue as the methodology highlights beliefs, attitudes, and perspectives of those who have lived experiences and are most directly affected. Thus, qualitative studies are uniquely suited to improve understanding of the barriers and facilitators to treatment and recovery for opioid use during and around pregnancy. Qualitative research on opioid use among pregnant women has identified pregnancy as a change point and opportunity to develop self-efficacy and capacity for self-care,9 and drivers of rising drug use during pregnancy in Kenya.10
The objective of this study was to further contribute to these findings by using qualitative data from PRAMS to gain a better understanding of women’s experiences related to opioid use during pregnancy. The information extracted from comments related to opioid use may help inform future research and programs that seek to improve care, reduce stigma, and mitigate factors that prevent pregnant women from seeking, receiving, and maintaining treatment.
Methods
Data collection
We analyzed 2016 data from responses to an open-ended prompt collected on PRAMS. PRAMS is an ongoing, population-based surveillance system conducted by state, territorial, or city health departments in collaboration with the CDC. PRAMS collects information from women with a recent live birth about their behaviors and experiences before, during, and shortly after pregnancy. Women are randomly sampled from birth certificate records in each participating site between 2 to 6 months postpartum. PRAMS staff in each site send up to three mail questionnaires to each sampled woman and follow up to conduct a telephone interview with women who do not respond to mailings.11 The PRAMS study protocol has been approved by the Institutional Review Boards of CDC and each participating site. Per the data sharing agreement and procedures for approval for release of de-identified data in the PRAMS protocol, all PRAMS sites had the opportunity to review and comment on the analytic plan for this study.
PRAMS qualitative data
At the end of the mail survey and telephone interview, respondents have the opportunity to provide additional information about their experiences. The following prompt is provided at the end of the mailed questionnaire: “Please use this space for any additional comments you would like to make about the health of mothers and babies in < STATE>”. At the end of the telephone interview, the following is read: “Is there anything you would like to say about your experiences around the time of your pregnancy or the health of mothers and babies in < STATE>?”. Responses are captured verbatim in a free text field by data entry staff (mail surveys) and telephone interviewers. Responses collected through general open questions at the end of structured surveys and interviews can provide further depth to data already collected, particularly when data found in open-ended questions provides new insight not already captured.12 This has been shown from previous research on postpartum experiences with PRAMS comment data.13
Analysis
All available comment data from 2016 were analyzed from 35 participating PRAMS sites that included the open-ended prompt on their survey (Figure 1). As the analysis was not focused on providing representative estimates, data were included for all available PRAMS sites who collected comment data, regardless of the annual weighted response rate in 2016 (range = 44.8% to 72.5%).
Figure 1.
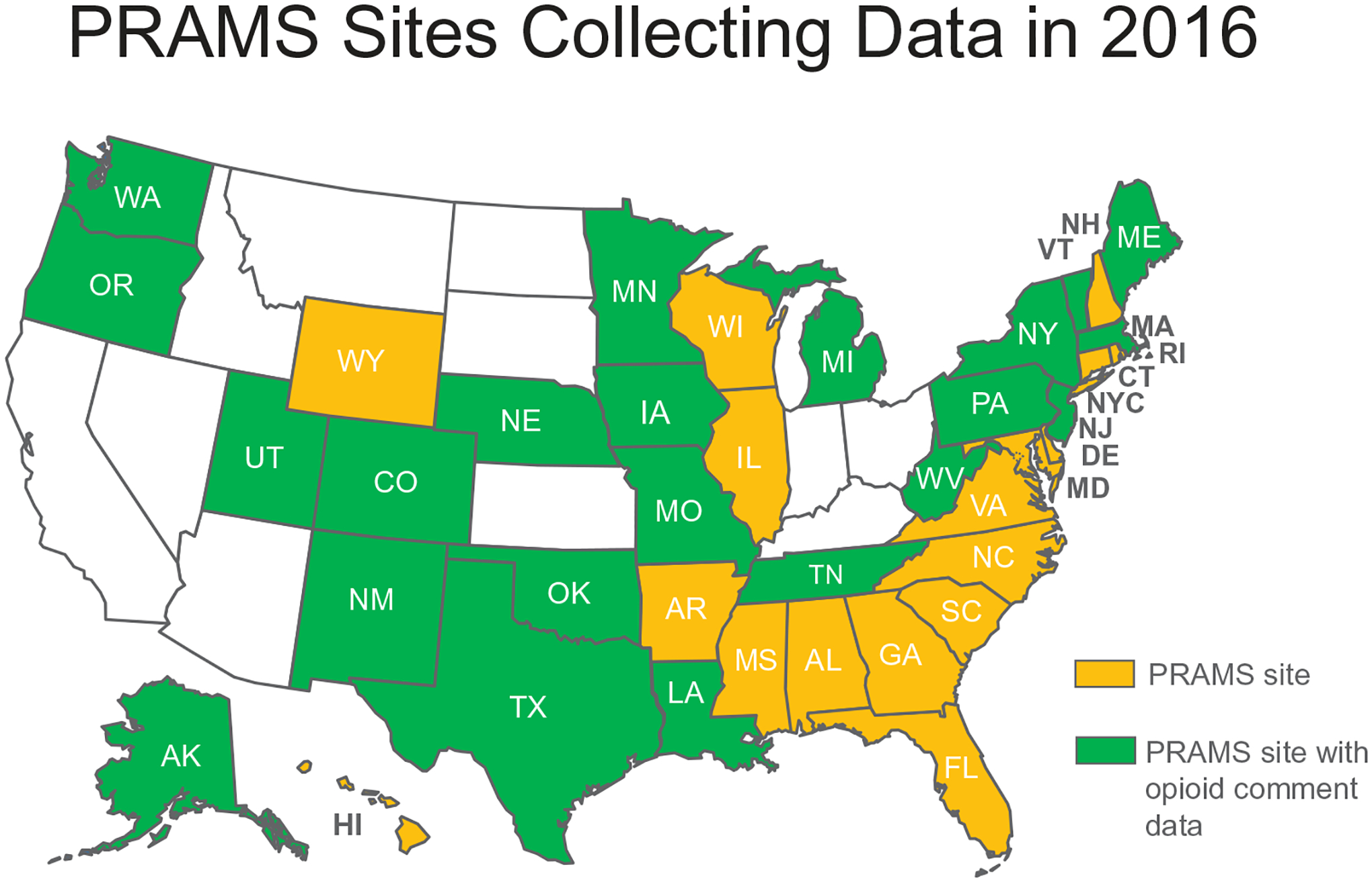
PRAMS sites collecting data, PRAMS 2016.
In total, there were 9,549 comments across all 35 sites. Initially, a list of keywords was compiled based on opioid use and treatment-related words identified through a literature review on opioid use and treatment as well as an internet search for “street names” of opioids and common misspellings (Figure 2). Using an automated function in Microsoft Excel, 1,035 comments containing keywords were identified. A three-person team (MC, DD, MO) read these comments and applied inclusion and exclusion criteria to identify comments related to substance use (Figure 3). The remaining 8,514 comments that did not include keywords were reviewed by the three-person team to confirm exclusion. A codebook was initially created using deductive codes, or codes developed from previous literature searches, and hypothesized a priori to be of importance.14,15 Inductive codes were created based on the themes identified during coding process and added to the codebook. After the codebook was developed, four randomly selected sites (Delaware, Georgia, Illinois, and Wisconsin) representing 10% of the comments were reviewed by 2 independent coders (MC, MO). Application of codes was then compared between the 2 coders and agreement was high (Inter-Rater Reliability [IRR] = 100% agreement between coders on 98% of codes); any discrepancies were resolved by consensus. Following this review, the codebook was finalized, and no further changes were made to the codes. The final analysis was conducted by dividing up the 35 states among three independent coders.
Figure 2.

List of common words and misspellings included in keyword search to identify opioid related open-ended comments from the Pregnancy Risk Assessment Monitoring System in 2016.
Figure 3.

Selection of PRAMS records for inclusion in qualitative analysis of experiences with opioid use around the time of pregnancy.
We identified 241 substance-use related comments, which included narratives around opioid use, tobacco use, marijuana use, alcohol use, partner substance use, polysubstance use, and “negative cases” (occurrences when women mentioned substances, only to say that she didn’t use them). From the substance-use related comments, the team eliminated non-opioid related comments and negative cases resulting in 69 opioid-related comments for the final analysis. Polysubstance use comments were included if opioid use was mentioned. Comments ranged in length from 22 characters to 3,970 characters. The final 69 comments were analyzed for themes using a content analysis approach.16 All coding and textual analysis was done using Microsoft Excel software.
To examine characteristics of the population of women who had live births in the sample, we also analyzed quantitative data on demographic and other selected characteristics from the linked birth certificate file. Characteristics were examined to observe similarities and differences between the following 3 groups: all PRAMS respondents, PRAMS respondents who provided comments, and those who provided opioid-specific comments. Descriptive statistical analyses on the quantitative data were conducted using SAS v9.4 software.
Results
Overall, there were 40,408 respondents to the PRAMS survey in the 35 sites in 2016 (Table 1). Among all respondents, 23.6% (N = 9,549) provided a comment (i.e. responded to the open-ended prompt) on any topic. Less than one percent of respondents who provided comments (0.7%, N = 69) included a comment specific to opioid use. About half of all respondents (47.2%) and respondents providing comments (48.2%) were white. Approximately 60% of all respondents and those providing comments were married (60.0 and 61.9%, respectively) and had private health insurance coverage for prenatal care (58.6 and 60.0%, respectively). Among women who provided a comment on opioid use, the majority were white (75.4%), were not married (66.2%), and reported their prenatal care was covered by Medicaid (73.4%). A larger proportion of opioid-related comments (87.0%) were provided via the mail questionnaire compared to the phone survey (13.0%). When coding the results, the codes most commonly applied related to experiences finding and using treatment and negative health care provider experiences (39 and 34 codes, respectively); least commonly applied were codes related to positive health care provider experiences and interaction with child protective services (11 codes each).
Table 1.
Characteristics of respondents by contribution of comments on the Pregnancy Risk Assessment Monitoring System (PRAMS) survey, 35 sites*, 2016.
| Characteristics | Percent | ||
|---|---|---|---|
| All respondents (n = 40,408)** | Respondents who provided any comment (n = 9,549)** | Respondents who provided opioid-related comments (n = 69)** | |
| Age | |||
| <20 | 5.2 | 5.1 | 1.4 |
| 20–24 | 19.1 | 19.4 | 18.8 |
| 25–34 | 58.0 | 56.4 | 68.1 |
| >=35 | 17.8 | 19.2 | 11.6 |
| Race/ethnicity | |||
| White Non-Hispanic | 47.2 | 48.2 | 75.4 |
| Black Non-Hispanic | 18.2 | 15.0 | 5.8 |
| Other Non-Hispanic | 15.4 | 12.9 | 13.0 |
| Hispanic | 19.3 | 24.0 | 5.8 |
| Education | |||
| Less than high school | 13.7 | 14.3 | 11.9 |
| High school | 24.0 | 22.8 | 23.9 |
| More than high school | 62.3 | 62.9 | 64.2 |
| Parity | |||
| Nulliparous | 39.4 | 40.5 | 29.0 |
| Multiparous | 60.6 | 59.5 | 71.0 |
| Marital status | |||
| Married | 60.0 | 61.9 | 33.8 |
| Not married | 40.0 | 38.1 | 66.2 |
| Insurance coverage for prenatal care | |||
| Private | 58.6 | 60.0 | 25.0 |
| Medicaid | 39.1 | 37.2 | 73.4 |
| None | 2.3 | 2.8 | 1.6 |
| WIC during pregnancy | |||
| Yes | 41.1 | 40.5 | 47.8 |
| No | 58.9 | 59.5 | 52.2 |
| Timing of PNC entry | |||
| 1st Trimester | 85.8 | 84.6 | 78.3 |
| After 1st trimester | 14.2 | 15.4 | 21.7 |
| Infant birth weight | |||
| Normal birthweight (>=2500 grams) | 76.5 | 73.3 | 58.0 |
| Low birthweight (<2500 grams) | 23.5 | 26.7 | 42.0 |
PRAMS sites that captured comment data and had a 2016 dataset available for analysis: AK, AL, AR, CO, CT, DE, IA, IL, LA, MA, MD, ME, MI, MN, MO, MS, NC, NE, NJ, NM, NY, NYC, OK, OR, PA, RI, TN, TX, UT, VA, VT, WA, WI, WV, WY.
Unweighted sample size.
Women described experiences with opioid use that indicated use disorder as well as receipt of treatment for opioid use disorder around the time of pregnancy. Content analysis resulted in five overarching themes: (1) gratitude for treatment, recovery, and healthy infants; (2) pregnancy as a motivation to seek treatment; (3) difficulty finding appropriately trained prenatal care providers; (4) concerns about the effects of treatment on the infant; and (5) experiences of discrimination and stigma in the hospital around the time of delivery. Comments from each theme are provided as examples.
Gratitude for treatment, recovery, and healthy infants
One common theme was an expression of happiness, gratitude for treatment, and relief for healthy infant outcomes. Women talked about receiving treatment in a variety of settings including inpatient and outpatient facilities. These comments included an acknowledgement of the positive role of healthcare providers, as well as encouragement to others about the benefits of getting help.
I was suffering from an opioid addiction during my pregnancy and went through a 26-day inpatient treatment with other pregnant woman and I want to say it’s important to get the word out that there is help and resources out there if you have a problem, don’t be afraid to ask for help. Don’t think you’re going to get in trouble or anything, people are there to help you. I’ve been able to maintain my sobriety and am happy I got help.
30 years old, West
My addiction caused me to use drugs during my pregnancy. If you’re struggling please get help! … By the grace of God, I’m clean and sober and my baby is now healthy after 4 months of help from doctors and nurses. Thank you for your help.
26 years old, Mid-Atlantic
Pregnancy as motivation to seek treatment
The timing in which women received help for their drug dependence ranged from right when they found out they were pregnant to throughout their pregnancy. During pregnancy, women sought treatment at methadone clinics, from their medical providers, and inpatient facilities. Women most frequently cited their motivation to seek treatment was due to their pregnancy:
I was using pain pills when I found out I was pregnant so I got myself in a program to stop. They prescribed Subutex I used during pregnancy. My baby was born perfect … Now we are happy and healthy at home with her little sister who is 3–1/2 years old.
29 years old, Northeast
I was addicted to drugs before my pregnancy. Subutex helped me stay clean and have a healthy baby. Subutex should be encouraged if need be.
24 years old, Midwest
I am proof that having a baby on methadone doesn’t make you a monster. My child truly changed me. There are no positive stories out there about this situation. I was scared my whole pregnancy about my baby having to stay in the NICU, and he came out perfect. Other women should know this, so they won’t be scared like I was.
29 years old, South
Difficulty finding prenatal care providers with training in substance use disorders
Another common theme was frustration for women with experiences trying to find prenatal care providers willing to accept them as patients, providers who were able to appropriately advise them on treatment options, and providers who could connect them to other needed services.
When I got pregnant, I was addicted to opiate pain pills. I tried many places & services begging for help to get clean. Nobody was willing to help me at all because I was pregnant. There should be options available for mothers to access to be able to receive drug treatment if they seek it … At the very end of my pregnancy, I found a doctor willing to treat me with suboxone.
32 years old, South
I was on Methadone before, during, and after my pregnancy and I have been sober for 2 years now. It was extremely hard finding a doctor who would take me.
34 years old, Southwest
I feel there should be more programs available for addicted (opiate) mothers to be. My OB-GYN did very little to help me decide the best course of action for my situation …
30 years old, Northeast
Concern about the effects of treatment on the infant
Fear of witnessing their infants experience withdrawal symptoms was another recurrent theme. Although women mentioned different types of medication-assisted treatment (MAT), comments noted a desire to avoid methadone, in particular, because of fear that it would make withdrawal symptoms worse for the infant and lead to an extended infant hospital stay. There were also feelings of being uninformed about all treatment options and therefore being unable to select the option least likely to cause suffering in their infant.
I had twins so I was high risk! I never told my doctors that I was prescribed subutex ‘cause I knew that my babies would be fine and they were when they was born. I didn’t tell them ‘cause I did NOT want my babies to be put on methadone!
23 years old, Mid-Atlantic
I told my OBGYN [about addiction] and he just gave me the # to the methadone clinic which I really wanted to avoid. Although I’ve never been on methadone maintenance I am aware that the withdrawal is 4x longer than any opiate withdrawal.
30 years old, Northeast
Before I got pregnant, I was dependent on drugs (heroin). I got on methadone 2 months before I got pregnant. At the clinic I attend there are a lot of women whom are pregnant, and we had tons of questions. I relied on other people who had babies on methadone, and I heard a lot of different things, some of which scared me, for instance my baby will have tremors, my baby will spend 1–2 months in the hospital for withdrawals, and the nurses will treat me terrible, and a lot more, which really scared me.
26 years old, Northeast
Experiences of discrimination and stigma in the hospital and around the time of delivery
Women also described experiences of discrimination based on their opioid use and treatment status during their delivery hospitalization. Comments in this theme focused on negative health care provider interactions, being misunderstood, being treated poorly, and being made to feel that they were a bad or negligent parent.
A nurse treated me very poorly at the hospital because of the Subutex. She made me think that my baby would go to the NICU if she had withdrawals. She scared me and made me feel like a bad mom. I was doing the right thing for my baby. I got off of heroin & got into treatment. Apparently, that woman has never walked in my shoes, and has lived a perfect life.
24 years old, Mid-Atlantic
I had some issues after my son was born at the hospital … I had narcotic medicines that I was told I had to take during my pregnancy by my doctor and it was in my medical records that I had to take them. When the baby was born … they treated me like a drug addict they wouldn’t let my baby come home and they made me leave.
29 years old, Northeast
There is a lot of babies born addicted to illegal drugs in [STATE] … and the way the staff at the hospital treats you when they find out … is crazy. They treat you bad and judge you from the door.
30 years old, Mid-Atlantic
Discussion
PRAMS qualitative data from the open-ended prompt provide a unique opportunity to examine some of the challenges of managing opioid misuse and opioid use disorder during pregnancy directly through the words of women who have lived through this experience. While women who provided comments do not constitute a representative sample of women with opioid use or opioid use disorder, the demographic characteristics of these women, (most were White, unmarried, with Medicaid coverage for prenatal care) align with other studies that found the majority of pregnant women reporting opioid- and non-opioid illegal drug use were White,17 and that White women were more likely to receive medication for opioid use disorder compared to Black and Hispanic women,18 Although findings are not representative of any region, there were comments from across the United States. We did not observe differences in themes by region or by mode of participation (mail or phone).
Qualitative findings from other studies have identified sentiments of gratitude for empathetic and caring providers, medication treatment,19 and group therapy for opioid use disorder20 in the general population. However, there is scant research around sentiments of gratitude for healthcare providers and treatment for opioid use disorder around the time of pregnancy. Some women expressed relief and gratitude for healthy infants, their decision to seek and maintain treatment, and appreciation to facilities and providers who helped them. Other studies have demonstrated the positive effects of gratitude on mood, coping ability, reported quality of life, and the reduction of depressive symptoms in a variety of contexts.21–23
PRAMS participants who commented on opioid use during pregnancy also expressed concern for their infants. They discussed their awareness of the potential for poor outcomes for their infants and noted that pregnancy was the reason for starting treatment. When describing their experiences, some noted their infant was perfect and healthy while reflecting on their gratitude for providers and treatment programs. Women shared their desire to ensure the best possible outcome for their infant and some shared their frustration in finding relevant care. Barriers fell into several categories: difficulty finding a provider during pregnancy, feeling uninformed about the full range of options that might help their infants avoid withdrawal symptoms, and experiences or perceptions of being treated poorly or stigmatized for their opioid use in the hospital. Recognition that women are concerned about the possible effects of opioid use and treatment on the health of their infants may help inform public health efforts designed to make appropriate care more accessible, reduce negative stereotypes, and encourage women to seek help.
Difficulty finding care or prenatal care providers knowledgeable about their condition was a common theme mentioned among the opioid use related comments. Screening and referral for substance use disorder is a recommended routine part of prenatal care by the American College of Obstetricians and Gynecologists24. However, findings from some provider surveys align with the comments from our study, reporting a lack of training and confidence to screen, refer, and treat women with these conditions.25 Efforts to improve training and resources for providers include the multidisciplinary work by the National Network of Perinatal Quality Collaboratives to improve maternal and child health outcomes and health systems at the state level.26 Another example is CDC’s partnership with the Association of State and Territorial Health Officials (ASTHO) to develop the Opioid Use Disorder, Maternal Outcomes, and Neonatal Abstinence Syndrome Initiative Learning Community (OMNI LC) to build state and local capacity. OMNI LC members identified five focus areas including access to and coordination of quality services and provider awareness and training.27
Experiences of discrimination for opioid use and treatment for opioid use disorder during pregnancy was commonly reported by women and has been well-documented in other qualitative studies.28,29 Negative provider interactions and fear of stigma are documented barriers to successful treatment for opioid use disorder during pregnancy.30,31 The comments shared in this study reinforce the importance of addressing stigma and discrimination so that women are not reluctant to seek treatment and support findings suggesting that nonjudgmental and positive provider interactions may be key to successful treatment and recovery in this population.32,33 Developing ethical, legal, and social considerations of strategies to address opioid use disorder among pregnant and postpartum women is another focus area of the OMNI LC. Specifically, supporting and training providers on the use of non-stigmatizing messaging and antidiscrimination and unconscious bias practices.27
Although many mothers who commented expressed a desire to find providers for treatment during pregnancy, an interesting finding of this study was the desire among some women to avoid methadone treatment, in particular, due to their perception that infants born to mothers who used methadone suffered worse withdrawal symptoms. These sentiments are supported by research suggesting infants exposed to methadone in utero are more likely to experience NAS than those exposed to buprenorphine.34 Women talked about methadone in a variety of ways, including warning or being warned by others not to use it, hiding their opioid use to avoid methadone treatment for fear of their infants experiencing withdrawal symptoms, and feeling they had not been fully informed of the potential outcomes of or alternatives to methadone. Given that MAT for pregnant women with methadone or buprenorphine is a recommended clinical practice and that infant withdrawal symptoms are expected,35,36 our findings support the work currently being done to improve provider awareness and training around caring for this population to ensure women receive accurate information regarding the recommended treatment options, including implications and plans for their infants at birth.27
Qualitative data collection methods may involve use of open-ended questions,12 and the statement used to solicit responses for the PRAMS qualitative data analyzed in this study is one such example. Only a small proportion of all PRAMS respondents in our study (0.17%; 69 of 40,408) provided an opioid-related qualitative comment in response to the general prompt at the end of the survey. However, this is not surprising given the absence of a specific probe inquiring about opioid use, the location of the prompt at the end of the survey, the sensitive nature of the topic (87% of opioid comments were from the mail survey rather than the telephone survey interview suggesting potential discomfort disclosing information to an interviewer), and the small proportion the population who uses opioids during pregnancy. PRAMS quantitative data from 2019 showed that 6.6% of respondents reported any prescription opioid pain reliever use during pregnancy,8 and 2018 National Survey on Drug Use and Health found 3.6% of the U.S. population misused prescription pain relievers.37 We were not able to assess whether comment data on opioid use correlated with opioid misuse or use disorder from quantitative data on PRAMS in 2016 because the PRAMS survey did not ask questions about this topic in detail until 2019.
The findings of this analysis are not generalizable to all women who used opioids or received treatment for opioid use disorder around the time of pregnancy, and are not intended to be interpreted as representative of the population of women with a live birth in the study sites. Our findings may lack the depth other qualitative research on this population are able to provide due to the brevity of the comments and inability to probe respondents.20,38 Nevertheless, this study provides valuable insights on women’s attitudes, perceptions, and experiences around opioid use during pregnancy that may inform prevention and treatment strategies designed to improve care and reduce stigma for women needing or seeking treatment, as well as future analyses of PRAMS data.
Conclusion
The experiences described related to opioid use and treatment for opioid use disorder around the time of pregnancy are consistent with items addressed in CDC’s recommended strategies to prevent opioid-related harms, including supporting providers and health systems, empowering consumers to make safe choices, and increasing provider awareness and training on ethical, legal and social considerations.7 These data indicate a need for increased knowledge and capacity of providers to screen, refer, and provide appropriate, nonjudgmental prenatal care and support for women who use opioids around the time of pregnancy. This is especially critical for prenatal care providers as many women described pregnancy as a motivation to seek and maintain treatment and stigma and discrimination as a barrier to do so.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors acknowledge Dr. Jean Ko for her input and review of the first draft of the manuscript and the PRAMS Working Group: Kristen Johnson, Alabama Department of Public Health; Enid Quintana-Torres, Arizona Department of Health Services; Ashley Juhl, Colorado Department of Public Health & Environment; Jennifer Morin, Connecticut Department of Public Health; Fern Johnson-Clarke, District of Columbia Department of Health; Jerri Foreman, Florida Department of Health; J. Michael Bryan, Georgia Department of Public Health; Joyce Prince, Illinois Department of Public Health; Brittany Reynolds, Indiana State Department of Health; Jennifer Pham, Iowa Department of Public Health; Lisa Williams, Kansas Department of Health and Environment; Tracey Jewell, Kentucky Department for Public Health; Rosaria Trichilo, Louisiana Department of Health; Laurie Kettinger, Maryland Department of Health; Emily Lu, Massachusetts Department of Public Health; Rebecca Lander, Missouri Department of Health and Senior Services; Tami Conn, Nevada Department of Health and Human Services; Sara Riordan, NH Department of Health & Human Services; Anne Radigan, New York State Department of Health; Grace Njau, North Dakota Department of Health; Tina Kent, Oregon Department of Human Services; Sara E. Thuma, Pennsylvania Department of Health; Wanda Hernández Virella, Puerto Rico Department of Health; Karine Monteiro, Rhode Island Department of Health; Harley T. Davis, South Carolina Department of Health and Environmental Control; Linda Ahrendt, South Dakota State Department of Health; Uvonne Leverett, Tennessee Department of Health; Barbara Algarin, Utah Department of Health; John Davy, Vermont Department of Health; Linda Lohdefinck, Washington Department of Health; Monica Pegram, West Virginia Bureau for Public Health; Lorie Wayne Chesnut, Wyoming Department of Health.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
References
- [1].U.S. Department of Health & Human Services. HHS Acting Secretary Declares Public Health Emergency to Address National Opioid Crisis. 2017. https://www.hhs.gov/about/news/2017/10/26/hhs-acting-secretary-declares-public-health-emergency-address-national-opioid-crisis.html. Published October 26, 2017. Accessed August 8, 2019.
- [2].Leech AA, Cooper WO, McNeer E, Scott TA, Patrick SW. Neonatal abstinence syndrome in the United States, 2004–16. Health Aff. 2020;39(5):764–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wilson N, Kariisa M, Seth P, Smith H, Davis NL. Drug and opioid-involved overdose deaths – United States, 2017–2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):290–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization – United States, 1999–2014. MMWR Morb Mortal Wkly Rep. 2018;67(31):845–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Winkelman TNA, Villapiano N, Kozhimannil KB, Davis MM, Patrick SW. Incidence and costs of neonatal abstinence syndrome among infants with Medicaid. Pediatrics. 2018;141(4): e20173520–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Strahan AE, Guy GP Jr., Bohm M, Frey M, Ko JY. Neonatal abstinence syndrome incidence and health care costs in the United States. JAMA Pediatr. 2020;174(2):200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Centers for Disease Control and Prevention. America’s drug overdose epidemic: putting data to action; 2020. https://www.cdc.gov/injury/features/prescription-drug-overdose/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fopioids%2Fstrategy.html. Accessed August 8, 2019.
- [8].Ko JY, D’Angelo DV, Haight SC, et al. Vital signs: prescription opioid pain reliever use during pregnancy – 34 U.S. Jurisdictions, 2019. MMWR Morb Mortal Wkly Rep. 2020; 69(28):897–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Goodman DJ, Saunders EC, Wolff KB. In their own words: a qualitative study of factors promoting resilience and recovery among postpartum women with opioid use disorders. BMC Pregnancy Childbirth. 2020;20(1):178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Mburu G, Ayon S, Mahinda S, Kaveh K. Determinants of women’s drug use during pregnancy: perspectives from a qualitative study. Matern Child Health J. 2020;24(9):1170–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Shulman HB, D’Angelo DV, Harrison L, Smith RA, Warner L. The Pregnancy Risk Assessment Monitoring System (PRAMS): overview of design and methodology. Am J Public Health. 2018; 108(10):1305–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].O’Cathain A, Thomas KJ. “Any other comments?” Open questions on questionnaires – a bane or a bonus to research? BMC Med Res Methodol. 2004;4:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kanotra S, D’Angelo D, Phares TM, Morrow B, Barfield WD, Lansky A. Challenges faced by new mothers in the early postpartum period: an analysis of comment data from the 2000 Pregnancy Risk Assessment Monitoring System (PRAMS) survey. Matern Child Health J. 2007;11(6):549–558. [DOI] [PubMed] [Google Scholar]
- [14].Hotham ED, Ali RL, White JM. Analysis of qualitative data from the investigation study in pregnancy of the ASSIST Version 3.0 (the Alcohol, Smoking and Substance Involvement Screening Test). Midwifery. 2016;34:183–197. [DOI] [PubMed] [Google Scholar]
- [15].Meyer JP, Isaacs K, El-Shahawy O, Burlew AK, Wechsberg W. Research on women with substance use disorders: Reviewing progress and developing a research and implementation road-map. Drug Alcohol Depend. 2019;197:158–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
- [17].Metz VE, Brown QL, Martins SS, Palamar JJ. Characteristics of drug use among pregnant women in the United States: Opioid and non-opioid illegal drug use. Drug Alcohol Depend. 2018; 183:261–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Peeler M, Gupta M, Melvin P, et al. Racial and ethnic disparities in maternal and infant outcomes among opioid-exposed mother-infant dyads in Massachusetts (2017–2019). Am J Public Health. 2020;110(12):1828–1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Rawson RA, Rieckmann T, Cousins S, McCann M, Pearce R. Patient perceptions of treatment with medication treatment for opioid use disorder (MOUD) in the Vermont hub-and-spoke system. Prev Med. 2019;128:105785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Sokol R, Albanese C, Chaponis D, et al. Why use group visits for opioid use disorder treatment in primary care? A patient-centered qualitative study. Subst Abus. 2018;39(1):52–58. [DOI] [PubMed] [Google Scholar]
- [21].O’ Leary K, Dockray S, Hammond S. Positive prenatal well-being: conceptualising and measuring mindfulness and gratitude in pregnancy. Arch Womens Ment Health. 2016;19(4): 665–673. [DOI] [PubMed] [Google Scholar]
- [22].Leung CC, Tong EMW. Gratitude and drug misuse: role of coping as mediator. Subst Use Misuse. 2017;52(14):1832–1839. [DOI] [PubMed] [Google Scholar]
- [23].Millstein RA, Celano CM, Beale EE, et al. The effects of optimism and gratitude on adherence, functioning and mental health following an acute coronary syndrome. Gen Hosp Psychiatry. 2016;43:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Substance abuse in pregnancy. ACOG technical bulletin number 195–July 1994 (replaces No. 96, September 1986). Int J Gynaecol Obstet. 1994;47(1):73–80. [PubMed] [Google Scholar]
- [25].Ko JY, Tong VT, Haight SC, et al. Obstetrician-gynecologists’ practices and attitudes on substance use screening during pregnancy. J Perinatol. 2020;40(3):422–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Henderson ZT, Ernst K, Simpson KR, et al. The national network of state perinatal quality collaboratives: a growing movement to improve maternal and infant health. J Womens Health. 2018;27(2):123–127. [DOI] [PubMed] [Google Scholar]
- [27].Kroelinger CD, Rice ME, Cox S, et al. State strategies to address opioid use disorder among pregnant and postpartum women and infants prenatally exposed to substances, including infants with neonatal abstinence syndrome. MMWR Morb Mortal Wkly Rep. 2019;68(36):777–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Elms N, Link K, Newman A, Brogly SB, Kingston House of Recovery for Women and Children. Need for women-centered treatment for substance use disorders: results from focus group discussions. Harm Reduct J. 2018;15(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Fowler C, Reid S, Minnis J, Day C. Experiences of mothers with substance dependence: Informing the development of parenting support. J Clin Nurs. 2014;23(19–20):2835–2843. [DOI] [PubMed] [Google Scholar]
- [30].Frazer Z, McConnell K, Jansson LM. Treatment for substance use disorders in pregnant women: motivators and barriers. Drug Alcohol Depend. 2019;205:107652. [DOI] [PubMed] [Google Scholar]
- [31].Gartner K, Elliott K, Smith M, Pearson H, Hunt G, Martin RE. People in regular society don’t think you can be a good mother and have a substance use problem”: participatory action research with women with substance use in pregnancy. Can Fam Physician. 2018;64(7):e309–e316. [PMC free article] [PubMed] [Google Scholar]
- [32].Alexander K. A call for compassionate care. J Addict Nurs. 2017;28(4):220–223. [DOI] [PubMed] [Google Scholar]
- [33].van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1–2): 23–35. [DOI] [PubMed] [Google Scholar]
- [34].Lemon LS, Caritis SN, Venkataramanan R, Platt RW, Bodnar LM. Methadone versus buprenorphine for opioid use dependence and risk of neonatal abstinence syndrome. Epidemiology. 2018;29(2):261–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Klaman SL, Isaacs K, Leopold A, et al. Treating women who are pregnant and parenting for opioid use disorder and the concurrent care of their infants and children: literature review to support national guidance. J Addict Med. 2017;11(3): 178–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Ko JY, Wolicki S, Barfield WD, et al. CDC grand rounds: public health strategies to prevent neonatal abstinence syndrome. MMWR Morb Mortal Wkly Rep. 2017;66(9):242–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2019. [Google Scholar]
- [38].Leiner C, Cody T, Mullins N, Ramage M, Ostrach BMM. “The elephant in the room;” a qualitative study of perinatal fears in opioid use disorder treatment in Southern Appalachia. BMC Pregnancy Childbirth. 2021;21(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]


