Abstract
Background
Postoperative hyper-inflammation is a frequent event in patients with acute Stanford type A aortic dissection (ATAAD) after surgical repair. This study's objective was to determine which inflammatory biomarkers could be used to make a better formula for identifying postoperative hyper-inflammation, and which risk factors were associated with hyper-inflammation.
Methods
A total of 405 patients were enrolled in this study from October 1, 2020 to April 1, 2023. Of these patients, 124 exhibited poor outcomes. In order to investigate the optimal cut-off values for poor outcomes, logistic and receiver operating characteristic analyses were performed on the following parameters on the first postoperative day: procalcitonin (PCT), C-reactive protein (CRP), interleukin-6 (IL-6), and systemic immune-inflammation index (SII). These cut-off points were used to separate the patients into hyper-inflammatory (n = 52) and control (n = 353) groups. Finally, the logistic were used to find the risk factors of hyper-inflammatory.
Results
PCT, CRP, IL-6, and SII were independent risk factors of poor outcomes in the multivariate logistic model. Cut-off points of these biomarkers were 2.18 ng/ml, 49.76 mg/L, 301.88 pg/ml, 2509.96 × 109/L respectively. These points were used to define postoperative hyper-inflammation (OR 2.97, 95% CI 1.35–6.53, P < 0.01). Cardiopulmonary bypass (CPB) > 180 min, and deep hypothermia circulatory arrest (DHCA) > 40 min were the independent risk factors for hyper-inflammation.
Conclusions
PCT > 2.18, CRP > 49.76, IL-6 > 301.88, and SII < 2509.96 could be used to define postoperative hyper-inflammation which increased mortality and morbidity in patients after ATAAD surgery. Based on these findings, we found that CPB > 180 min and DHCA > 40 min were separate risk factors for postoperative hyper-inflammation.
Keywords: Hyper-inflammation, Acute Stanford type A aortic dissection, Cardiopulmonary bypass, Deep hypothermia circulatory arrest, Mortality, Morbidity
Introduction
Acute type-A aortic dissection (ATAAD) is a life-threatening disease that carries a high mortality risk. According to the findings of the international Registry of Acute Aortic Dissection (IRAD), the mortality rate among patients who underwent surgical repair ranged from 18 to 25%. In a word, despite the significant advancements in peri-operative strategies and surgical techniques over the past two decades, ATAAD remains a highly severe aortic condition [1]. Prolonged cardiopulmonary bypass (CPB), aortic cross-clamp (ACC) and deep hypothermia circulatory arrest (DHCA) were ordinary during ATAAD surgical repair, which lead to various components of the inflammatory response were documented [2–7]. Consequently, patients with ATAAD who underwent surgical repair often experienced postoperative hyper-inflammatory conditions compared with other common cardiac surgeries, such as myocardial ischemia–reperfusion injury, coagulopathy, hypotension or shock postoperative and acute lung injury or even acute respiratory distress syndrome (ARDS) [1, 8–10].
Over the past years, numerous clinical studies have been conducted to identify risk factors associated with poor outcomes in order to enable early diagnosis and treatment of ATAAD, which included hyper-inflammatory complications [8, 10, 11]. During CPB in ATAAD surgery, an amplified systemic inflammatory response, involving neutrophile, lymphocyte, platelet, C reactive protein (CRP), procalcitonin (PCT), and interleukin-6 (IL-6) in body, was demonstrated that had a significant association with unfavorable postoperative outcomes including coagulopathy, surgical bleeding, re-intubation and so on [2–5, 12]. It has been proven that an early-initiated anti-inflammatory strategy is a promising option after ATAAD surgery [6]. Therefore, early prediction of hyper-inflammation after ATAAD may be useful and valuable to decrease mortality and morbidity.
There was a large body of research investigating association between postoperative hyper-inflammation and adverse outcomes after ATAAD surgery [8, 10, 11]. Li et al. [11] conducted a study where they found that the systemic immune-inflammation index (SII), a reliable indicator of systemic inflammation based on peripheral lymphocyte, neutrophil, and platelet, could effectively predict the survival of patients following surgery. Their methodology interested us deeply in investigating the definition of postoperative hyper-inflammation. However, it may be biased to make a statistical model on an isolated variable due to interference of per-operative and surgical strategies, such as CPB, ACC, DHCA and so on. Therefore, we designed this retrospective cohort study to determine which inflammatory biomarkers could be used to make a better formula for identifying postoperative hyper-inflammation, and which risk factors were associated with hyper-inflammation.
Methods
Patients
This study received approval from the ethical committees of Nanjing Drum Tower Hospital (No.2020-185-01). It was not feasible to obtain informed consent from all patients due to the nature of the study. However, since this study posed no risk to the patients involved, the institutional ethics committee waived the requirement for informed consent. The study adhered strictly to the Declaration of Helsinki (seventh revision, 2013) and was conducted under the supervision of the ethics committee. After obtaining approval from the ethical committees, a review was conducted using hospital medical records, nursing records, laboratory data, and surgical databases at a tertiary hospital.
Inclusion criteria Adult patients (aged 18 years old and above) who underwent surgery for ATAAD at our center would be enrolled in this study. Exclusion criteria Patients would be excluded when they met any of the following criteria: experienced a cardiogenic shock at the conclusion of CPB (vasoactive inotropic score > 40, cardiac index < 2.2 L/min m2, mean arterial pressure < 65 mm Hg)[7]; diagnosis of inflammatory immune diseases, infectious diseases, or tumor diseases; previous treatment with immune-suppressing medications; initiation of extracorporeal membrane oxygenation (ECMO) or continuous renal replacement therapy (CRRT) before surgery; had mechanically ventilated before surgery; received DAVID procedure; pregnancy.
Primary outcome of this study was a composite of unfavorable morbidity following surgery that called “the poor outcome”. Morbidity was considered present if any of the following postoperative conditions were observed: in-hospital death, ECMO or CRRT use, tracheal re-intubation, severe pneumonia, mechanical ventilation time > 72 h, and malperfusion syndrome. Secondary endpoints included preoperative and postoperative inflammatory indicators such as SII, CRP, PCT and IL-6; observed surgical duration (CPB, ACC, DHCA runs).
Surgical intervention
Upon diagnosis of ATAAD, patients were promptly transferred to the intensive care unit. Central repair surgery was performed within 24 h of symptom onset. Patients experiencing critical conditions such as cardiac tamponade, cardiogenic shock, cerebrovascular accident, stroke, coma, myocardial ischemia, acute renal failure, or mesenteric ischemia would experience emergency surgery. The surgical approach involved a standard median sternotomy, with cannulation of the femoral artery, right axillary artery, and right atrium for CPB circulation. Antegrade cerebral perfusion was ensured via cannulation of the right axillary artery. Systemic temperature was maintained between 32 and 34 °C, and CPB was arrested once the desired hypothermic circulatory arrest temperature (22–24 °C) was reached. The initial volume of the antegrade cold blood cardioplegia solution, in a 4:1 ratio, was administered to achieve complete cessation of all cardiac electrical activity, with a minimum requirement of 20 ml/kg. To maintain cardiac arrest, retrograde infusion of 10 ml/kg of blood cardioplegia solution was repeated every 15 min after 30 min of initial antegrade infusion. If retrograde infusion was used three times, the antegrade strategy would be implemented accordingly.
The choice of distal surgical method depends on the location of the intimal tear and the extent of dissection. In cases where the primary tear is in the ascending aorta and the dissection is limited (arch dilation < 50 mm) [13], an ascending aortic replacement + hemi-arch replacement without antegrade stent-implantation is feasible. Otherwise, alternatives include ascending aortic replacement + total arch replacement + a frozen elephant trunk (FET) (MicroPort Medical Co Ltd) or ascending aortic replacement + an arched fenestrated stent graft (FSG) (Yuhengjia Sci-Tech Corp Ltd) implantation intraoperatively [14, 15]. For proximal segments, root reinforcement reconstruction or double jacket wrapping [16] were routinely performed. In situations where the dissection involves the coronary ostia, aortic valve, and aortic root aneurysm, the Bentall procedure and Wheat's procedure would be employed. If the dissection impairs the coronary artery, coronary artery bypass grafting (CABG) would be performed.
Data collection and definition
Baseline characteristics, laboratory features, operative details, and outcome data were collected from our electronic medical record database. The biomarkers of inflammation, including Neutrophile, Lymphocyte, Platelet, CRP, PCT, as well as IL-6 levels on the first postoperative day (POD1) were also collected. The formula of SII is as follows: platelet count × neutrophil to lymphocyte ratio [11]. Pre-operative ischemia (Table 1) could be considered if met the following condition: the presence of impaired blood flow in brain, coronary artery, limb and bowel as seen on radiographs; significant clinical symptoms, such as changes of pupillary size and light reaction pain, vomiting, bloody stool, abdominal pain, pallor, paresthesia, poikilothermia, or paralysis, etc. Malperfusion syndrome was defined as the presence of any organ malperfusion prior to surgery. According to our previous report, it includes cardiac malperfusion, cerebral malperfusion, renal malperfusion, mesenteric malperfusion, lower limb malperfusion [10].
Table 1.
Baseline characteristics
| Variables | Control (n = 281) | Poor outcome (n = 124) | P value |
|---|---|---|---|
| Age(year) | 53.8 ± 13.4 | 55.3 ± 13.5 | 0.371 |
| Gender male n (%) | 217 (77.2) | 93 (75.0) | 0.626 |
| BMI(kg/m2) | 25.4 (23.3–28.4) | 25.2 (20.9–27.7) | 0.570 |
| Medical history n (%) | |||
| Hypertension | 271 (96.4) | 116 (93.5) | 0.193 |
| Diabetes mellitus | 50 (17.8) | 30 (24.2) | 0.136 |
| COPD | 98 (34.9) | 45 (36.3) | 0.784 |
| Smoking | 135 (48.0) | 58 (46.8) | 0.814 |
| Heavy alcohol drinking | 41 (14.6) | 17 (13.7) | 0.816 |
| Liver diseases | 12 (4.3) | 1 (0.8) | 0.068 |
| Marfan syndrome | 14 (5.0) | 6 (4.8) | 0.951 |
| Cerebral infarction | 12 (4.3) | 5 (4.0) | 0.912 |
| Chronic renal failure | 3 (1.1) | 1 (0.8) | 0.806 |
| Ascending aortic diameter (cm) | 4.7 (4.4–5.4) | 5.1 (4.5–5.5) | 0.003 |
| Pre-operative PCT (ng/ml) | 0.01 (0.01–0.1) | 0.01 (0.01–0.1) | 0.207 |
| Pre-operative CRP (mg/L) | 3.52 (1.14–7.8) | 3.6 (1.5–6.0) | 0.984 |
| Pre-operative IL-6 (pg/ml) | 34.7 (11.9–60.0) | 40 (17.4–61.6) | 0.205 |
| Pre-operative SII | 546 (153–1326) | 539 (152–1512) | 0.874 |
| Pre-operative Neutrophile (× 109/L) | 4.3 (1–9.2) | 9.2 (4.8–13.0) | 0.822 |
| Pre-operative Lymphocyte (× 109/L) | 1.0 (0.7–1.4) | 0.9 (0.8–1.3) | 0.556 |
| Pre-operative Platelet (× 109/L) | 155 (116–190) | 153 (121–176) | 0.776 |
| Preoperative conditions n (%) | |||
| Bowel ischemia | 0 | 7 (5.6) | < 0.001 |
| Cerebral ischemia | 0 | 42 (10.4) | < 0.001 |
| Limb ischemia | 0 | 51 (41.1) | < 0.001 |
| Coronary artery involvement | 7 (2.5) | 6 (4.8) | 0.217 |
| Arch surgery n (%) | 0.702 | ||
| Total arch replacement | 183 (65.2) | 86 (69.4) | |
| Hemi arch replacement | 40 (14.2) | 16 (12.9) | |
| Arch stent | 58 (20.6) | 22 (17.7) | |
| Root surgery n (%) | 0.304 | ||
| Bentall procedure | 144 (51.2) | 65 (52.4) | |
| Wheat’s procedure | 56 (25.7) | 36 (29.0) | |
| Reconstruction | 81 (23.1) | 23 (18.6) | |
| Concomitant CABG n (%) | 7 (2.5) | 6 (4.8) | 0.217 |
| CPB time (min) | 182 (158.5–220.5) | 188 (163–228) | 0.233 |
| ACC time (min) | 133 (110.5–169.0) | 135 (120–175) | 0.099 |
| DHCA time (min) | 33 (26–41) | 31 (25–43) | 0.594 |
Median (Interquartile range); BMI Body mass index, COPD Chronic obstructive pulmonary disease, PCT Procalcitonin, CRP C-reactive protein, IL-6 interleukin-6, SII Systemic immune-inflammation index, CABG Coronary artery bypass graft, CPB Cardiopulmonary bypass, ACC Aortic cross-clamp, DHCA Deep hypothermia circulatory arrest
Statistical analysis
Statistical analysis was conducted using IBM SPSS Statistics for Windows (version 24, IBM Corporation, Armonk, NY, USA). Continuous variables were generally described as mean ± SD or median with interquartile ranges (IQR), while categorical variables were expressed as frequencies (n, %). The Student t-test was utilized for normally distributed continuous variables, while the Mann–Whitney U nonparametric method was employed for non-normally distributed continuous variables. Categorical data were compared using either the chi-square test or Fisher exact test. The receiver operating characteristic (ROC) curve and Youden index were employed to assess the predictive values and cut-off points of SII, PCT, CRP and IL-6 on POD1 for poor outcomes, which were used to defined hyper-inflammation. The areas under the ROC curves (AUC) were used to determine predictive accuracy. Logistic regression analyses were performed to identify independent risk factors for poor outcomes and hyper-inflammation. Covariates reaching statistical significance (P ≤ 0.10) in the univariate analysis and those considered clinically relevant were entered into a multivariable logistic regression model. Collinearity and calibration were assessed for each multivariable logistic model using the variance inflation factor (VIF) and Hosmer–Lemeshow test, respectively. A two-sided P-value of < 0.05 was considered statistically significant.
Results
A total of 426 patients underwent surgery for ATAAD at our hospital between October 1, 2020, and April 1, 2023. Among these patients, 405 individuals met the specified inclusion and exclusion criteria, and 124 exhibited poor outcomes which included in-hospital death (n = 43), ECMO (n = 5), tracheal re-intubation (n = 9), mechanical ventilation > 72 h (n = 54), severe pneumonia (n = 9), malperfusion syndrome (n = 97), and CRRT (n = 45). The detailed demographic and baseline data were provided in Table 1. Compared with the control, poor outcome group had higher level of ascending aortic diameter (median: 4.7 cm, IQR 4.4–5.4 cm vs. Median: 5.1 cm, IQR 4.5–5.5 cm, P = 0.003), and higher rate of pre-operative bowel ischemia (0 vs. 5.6%, P < 0.001), cerebral ischemia (0 vs. 10.4%, P < 0.001) and limb ischemia (0 vs. 41.1%, P < 0.001). Comparison of postoperative data revealed that poor outcome group had higher level of PCT (P < 0.001), CRP (P < 0.001) and IL-6 (P < 0.001), and lower level of SII (P < 0.001) compared with control group.
In multivariate analysis (Table 3), PCT, CRP, IL-6 and SII were independent risk factors of poor outcomes. Therefore, the PCT, CRP, IL-6 and SII were put into the ROC model. The cut-off points of these variables were 2.18 ng/ml (AUC: 0.61, sensitivity: 0.86, specificity: 0.38), 49.76 mg/L (AUC: 0.61, sensitivity: 0.85, specificity: 0.32), 301.88 pg/ml (AUC: 0.64, sensitivity: 0.44, specificity: 0.81), and 2509.96 × 109/L (AUC: 0.69, sensitivity: 0.58, specificity: 0.76), respectively. Then, these cut-off points were used to define hyper-inflammation which increased the risk of poor outcome (Table 2: 5.3% vs. 29.8%, P < 0.001). After collinearity analysis, the multivariable regression model (Table 3) also showed that hyper-inflammation was an independent risk factor of poor outcomes (OR 2.97, 95% CI 1.35–6.53, P < 0.01). However, after regression adjustment, liver diseases, ascending aortic diameter and ACC time did not display a significant correlation with the poor outcomes.
Table 3.
Multivariable logistic regression for poor outcomes
| Variables | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Liver diseases | 0.21 | 0.03–1.71 | 0.177 |
| Ascending aortic diameter | 1.01 | 1.00–1.01 | 0.068 |
| ACC time | 1.00 | 0.97–1.03 | 0.273 |
| PCT on POD1 | 1.50 | 1.03–2.17 | 0.035 |
| CRP on POD1 | 1.01 | 1.00–1.01 | 0.027 |
| IL-6 on POD1 | 1.00 | 1.00–1.01 | 0.042 |
| SII on POD1 | 1.00 | 1.00–1.01 | 0.002 |
| Hyper-inflammation | 2.97 | 1.35–6.53 | 0.007 |
CI Confidence interval, ACC Aortic cross-clamp, POD1 The first postoperative day, PCT procalcitonin, CRP C-reactive protein, IL-6 Interleukin-6, SII Systemic immune-inflammation index
Table 2.
Postoperative outcomes
| Variables | Control (n = 281) | Poor outcome (n = 124) | P value |
|---|---|---|---|
| Poor outcomes | |||
| In-hospital death n (%) | – | 43 (34.7) | – |
| ECMO n (%) | – | 5 (4.0) | – |
| Re-intubation n (%) | – | 9 (7.3) | – |
| MV > 72 h n (%) | – | 54 (43.5) | – |
| Sever pneumonia n (%) | – | 9 (7.3) | – |
| CRRT n (%) | – | 45 (36.3) | – |
| Malperfusion syndrome n (%) | – | 97 (78.2) | – |
| PCT on POD1 (ng/ml) | 3.04 (2.03–5.6) | 4.07 (2.6–6.6) | < 0.001 |
| CRP on POD1 (mg/L) | 77 (43.0–106.2) | 99 (66–125) | < 0.001 |
| IL-6 on POD1 (pg/ml) | 154.7 (54.6–270.7) | 239.3 (115.3–438.9) | < 0.001 |
| SII on POD1 | 2963.9 (1634.5–5220.4) | 1608.8 (876.9–2495.5) | < 0.001 |
| Neutrophile on POD1 (× 109/L) | 9.1 (6.2–10.6) | 9.15 (6.2–11.0) | 0.422 |
| Lymphocyte on POD1 (× 109/L) | 0.3 (0.2–0.3) | 0.5 (0.3–0.7) | < 0.001 |
| Platelet on POD1 (× 109/L) | 102 (76–125) | 94 (68–123) | 0.071 |
| Hyper-inflammation n (%) | 15 (5.3) | 37 (29.8) | < 0.001 |
Median (Interquartile range); ECMO Extracorporeal membrane oxygenation, MV Mechanical ventilation, CRRT Continuous renal replacement therapy, PCT Procalcitonin, CRP C-reactive protein, IL-6 Interleukin-6, SII Systemic immune-inflammation index, POD1 The first postoperative day
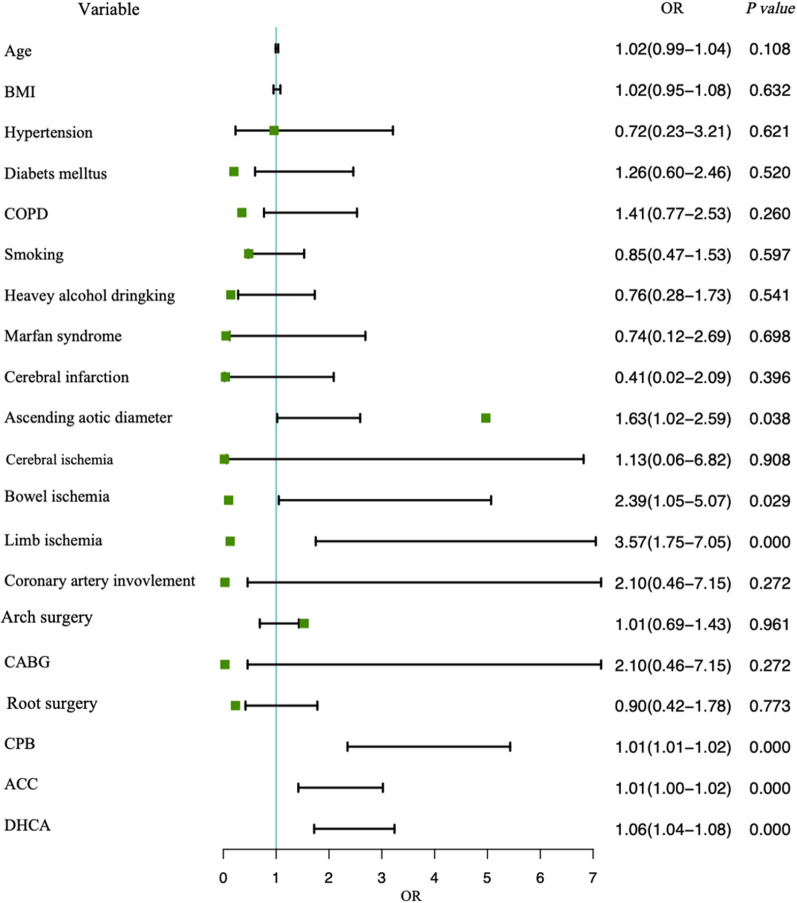
Subsequently, the study cohort was divided into two groups: the hyper-inflammation group (n = 52) and the control group (n = 353) (Table 4). Contrast to the control group, the hyper-inflammatory group demonstrated a greater proportion of preoperative cerebral ischemia [10 (19.23) vs. 32 (9.07), p = 0.025] and limb ischemia [15 (28.85) vs. 36 (10.20), p < 0.001]. In the hyper-inflammatory group, patients tended to suffer longer CPB [218.00 (195.50–269.00) vs. 163.00 (140.00–196.00), p < 0.001], ACC [158.50 (133.75–207.50) vs. 134.00 (113.00–168.00), p < 0.001] and DHCA duration [46.00 (38.00–56.25) vs. 32.00 (25.00–41.00), p < 0.001]. Consistently as before, inflammatory fators on the first postoperative day were also significantly elevated in the high inflammation group. Notably, mortality was significantly higher in the population of hyper-inflammation group [16 (30.77) vs. 27 (7.65)]. In univariable analysis (Fig. 1), ascending aortic diameter, pre-operative bowel ischemia, pre-operative limb ischemia, CPB, ACC, and DHCA were associated with an increased incidence of postoperative hyper-inflammation. In the ROC model (Fig. 2), cut-off points of CPB, ACC and DHCA were 176.6≈180 min (AUC: 0.82, sensitivity: 0.88, specificity: 0.63), 127.5 min≈130 min (AUC: 0.70, sensitivity: 0.88, specificity: 0.44), and 37.7≈40 min (AUC: 0.77, sensitivity: 0.81, specificity: 0.66), respectively. In Table 5, the further multivariate regression model showed that pre-operative bowel ischemia (P = 0.004), pre-operative limb ischemia (P = 0.001), CPB > 180 min (P < 0.001), and DHCA > 40 min (P < 0.001) were independent risk factor of postoperative hyper-inflammation. The ACC > 130 min could not significantly increase the rate of postoperative hyper-inflammation (P = 0.397).
Table 4.
Comparison of population with and without postoperative hyper-inflammation
| Variables | Control (n = 353) | Hyper-inflammation (n = 52) | P value |
|---|---|---|---|
| Age(year) | 53.84 ± 13.59 | 57.06 ± 12.30 | 0.107 |
| Gender male n (%) | 273 (77.34) | 37 (71.15) | 0.326 |
| BMI(kg/m2) | 25.37 (23.32–27.91) | 24.83 (22.20–28.53) | 0.769 |
| Medical history n (%) | |||
| Hypertension | 387 (95.56) | 338 (95.75) | 0.892 |
| Diabetes mellitus | 68 (19.26) | 12 (23.08) | 0.519 |
| COPD | 121 (34.28) | 22 (42.31) | 0.258 |
| Smoking | 170 (48.16) | 23 (44.23) | 0.596 |
| Heavy alcohol drinking | 52 (14.73) | 6 (11.54) | 0.540 |
| Liver diseases | 13 (3.68) | 0 (0.00) | 0.325 |
| Marfan syndrome | 18 (5.10) | 2 (3.85) | 0.963 |
| Cerebral infarction | 16 (4.53) | 1 (1.92) | 0.613 |
| Chronic renal failure | 4 (1.13) | 0 (0.00) | 1.000 |
| Ascending aortic diameter (cm) | 4.80 (4.40–5.50) | 4.90 (4.50–5.53) | 0.020 |
| Pre-operative PCT (ng/ml) | 0.01 (0.01–0.10) | 0.01 (0.01–0.10) | 0.877 |
| Pre-operative CRP (mg/L) | 3.52 (1.14–7.77) | 3.92 (1.14–16.10) | 0.596 |
| Pre-operative IL-6 (pg/ml) | 34.70 (11.68–52.71) | 39.85 (17.40–107.75) | 0.063 |
| Pre-operative SII | 531.84 (153.00–1400.00) | 615.55 (184.46–1400.00) | 0.669 |
| Preoperative conditions n (%) | |||
| Bowel ischemia | 6 (1.70) | 1 (1.92) | 1.000 |
| Cerebral ischemia | 32 (9.07) | 10 (19.23) | 0.025 |
| Limb ischemia | 36 (10.20) | 15 (28.85) | < 0.001 |
| Coronary artery involvement | 10 (2.83) | 3 (5.77) | 0.484 |
| Arch surgery n (%) | 0.941 | ||
| Total arch replacement | 235 (66.57) | 34 (65.38) | |
| Hemi arch replacement | 48 (13.60) | 8 (15.38) | |
| Arch stent | 70 (19.83) | 10 (19.23) | |
| Root surgery n (%) | 0.461 | ||
| Bentall procedure | 185 (52.41) | 24 (46.15) | |
| Wheat’s procedure | 81 (22.95) | 11 (21.15) | |
| Reconstruction | 87 (24.65) | 17 (32.69) | |
| Concomitant CABG n (%) | 10 (2.83) | 3 (5.77) | 0.484 |
| CPB time (min) | 163.00 (140.00–196.00) | 218.00 (195.50–269.00) | < 0.001 |
| ACC time (min) | 134.00 (113.00–168.00) | 158.50 (133.75–207.50) | < 0.001 |
| DHCA time (min) | 32.00 (25.00–41.00) | 46.00 (38.00–56.25) | < 0.001 |
| PCT on POD1 (ng/ml) | 3.04 (2.03–5.48) | 6.34 (3.57–6.90) | < 0.001 |
| CRP on POD1 (mg/L) | 79.00 (44.00–113.00) | 104.00 (69.00–125.50) | < 0.001 |
| IL-6 on POD1 (pg/ml) | 154.70 (54.62–253.52) | 438.86 (329.28–1039.78) | < 0.001 |
| SII on POD1 | 2698.75 (1516.67–4891.25) | 1259.13 (714.77–1692.67) | < 0.001 |
| Death | 27 (7.65) | 16 (30.77) | < 0.001 |
Median (Interquartile range); BMI Body mass index, COPD Chronic obstructive pulmonary disease, PCT Procalcitonin, CRP C-reactive protein, IL-6 Interleukin-6, SII Systemic immune-inflammation index, CABG Coronary artery bypass graft, CPB Cardiopulmonary bypass, ACC Aortic cross-clamp, DHCA Deep hypothermia circulatory arrest
Fig. 1.
Univariable analysis for postoperative hyper-inflammation in patients with AAAD
Fig. 2.
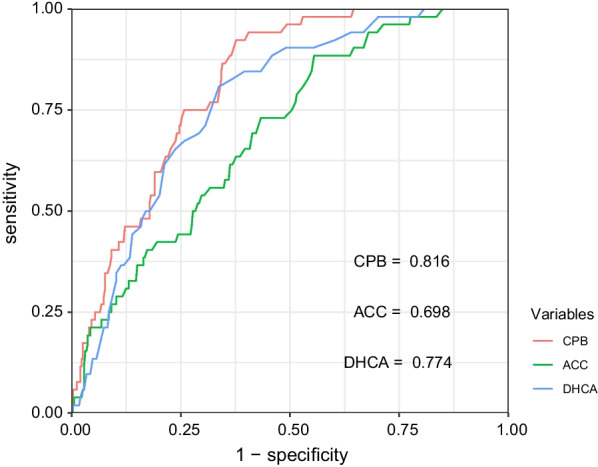
Receiver operating characteristic curve (ROC) analyses with the area under the curve, sensitivity and specificity of CPB, ACC, DHCA in predicting postoperative hyper-inflammation
Table 5.
Multivariable logistic regression for postoperative hyper-inflammation
| Variables | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Ascending aortic diameter > 5 cm [20] | 1.14 | 0.58–2.26 | 0.703 |
| Pre-operative bowel ischemia | 4.19 | 1.59–11.03 | 0.004 |
| Pre-operative limb ischemia | 4.07 | 1.78–9.29 | 0.001 |
| Cardiopulmonary bypass time > 180 min | 14.16 | 4.10–48.82 | < 0.001 |
| Aortic cross-clamping time > 130 min | 0.61 | 0.19–1.92 | 0.397 |
| DHCA time > 40 min | 4.11 | 2.03–8.31 | < 0.001 |
CI Confidence interval, CPB Cardiopulmonary bypass, ACC Aortic cross-clamp, DHCA Deep hypothermia circulatory arrest
Discussion
The hyper-inflammatory diseases, which usually result in poor prognosis, are common complications in patients after ATAAD surgery [8, 10, 11]. However, it had no large-sample-sized study to demonstrate the identification of postoperative hyper-inflammation in patients with ATAAD. Based on our center's cohort of ATAAD patients October 1, 2020 to April 1, 2023, we found that ① an easy formula could be used to define postoperative hyper-inflammation (PCT > 2.18 ng/ml & CRP > 49.76 mg/L & IL-6 > 301.88 pg/ml & SII < 2509.96 × 109/L); ② The morbidity of hyper-inflammation was about 12.83% in patients after ATAAD surgery, which was significantly associated with high mortality and morbidity; ③ the pre-operative bowel ischemia, pre-operative limb ischemia, CPB > 180 min and DHCA > 40 min were independent risk factors for postoperative hyper-inflammation.
To our best known, postoperative hyper-inflammatory diseases in patients with ATAAD include acute lung injury, malperfusion syndrome, and severe pneumonia [8, 10, 11]. The systemic inflammatory response could induce acute lung injury which could significantly increase in-hospital death [6, 17]. The malperfusion syndrome which is actually an ischemia–reperfusion injury (I/R injury), is caused by an immune-inflammatory response, which has been proven the lethal factor of in-hospital death [1, 10]. Severe pneumonia which is significantly associated with poor outcome, result in systemic inflammatory response syndrome (SIRS) or septic shock [18]. We, therefore, defined poor outcomes based on these poor inflammation-related endpoints, including in-hospital death, ECMO, tracheal re-intubation, mechanical ventilation > 72 h, severe pneumonia, malperfusion syndrome, and CRRT. For example, prolonged MV time and tracheal re-intubation are well-recognized factors of pneumonia. The ECMO can cause SIRS and represent a poor prognosis [19]. The CRRT usually results from renal malperfusion in patents after ATAAD surgery [20].
The predisposed poor outcomes may effectively help us to investigate the definition of postoperative hyper-inflammation. That was the reason why cut-off points of PCT, CRP, IL-6, and SII were easily found. Based on these points, we defined postoperative hyper-inflammation. In univariable analysis, the definable hyper-inflammation is significantly associated with poor outcomes (OR 7.54, 95% CI 3.95–14.40, P < 0.001). And this definable hyper-inflammation is an independent risk factor of poor outcomes in multivariate analysis (Table 3). There are reasons to believe that our definition of hyper-inflammation is acceptable, useful and reliable. It will help clinicians to quickly and easily predict postoperative hyper-inflammation.
Based on our definition, we divided the study population into hyper-inflammation group and control group. After univariate and multivariable analysis, the pre-operative bowel ischemia, pre-operative limb ischemia, CPB > 180 min and DHCA > 40 min were independent risk factors for postoperative hyper-inflammation. Pre-operative bowel ischemia and pre-operative limb ischemia are unsurprised to be risk factors of hyper-inflammation. Because pre-operative limb and bowel ischemia had an inflammatory related pathophysiologic process of I/R injury during the period of ATAAD surgery. Previous studies also reported that limb and bowel ischemia, identified as high-risk factors of hyper-inflammation, could significantly increase in-hospital mortality [10, 11]. ATAAD surgery required prolonged CPB and DHCA, which allowed the release of huge inflammatory indicators in body, including PCT, CRP, and IL-6, and therefore they have been widely recognized as independent risk factors of hyper-inflammation [21, 22]. However, to our best knowledge, there were no large-sample sized studies to demonstrate which cut-off points of CPB and DHCA time could lead to hyper-inflammation in patients who underwent ATAAD surgery. The ATAAD,a rare and critical disease, is scattered far and wide across the country. It has to implement a multi-center cohort to collect the study population. Our hospital is a regional cardiovascular center, due to which many ATAAD cases accumulated. We built a cohort that enrolled 405 patients with ATAAD, and calculated that cut-off points of CPB and DHCA time were 180 min and 40 min, respectively. This is the first study to report the conclusion of time thresholds that CPB > 180 min and DHCA > 40 min were significantly associated with postoperative hyper-inflammation. In general, this work will more rigorously suggest surgeons should try their best to reduce the operative time, which might be the only way for any patient to have a positive prognosis.
Study limitation
The current study had certain inherent limitations. Our study approach incorporates one center's experiences, which is a limitation of retrospective observational research. Retrospective observational studies are highly prone to bias. And other centers may have different results compared with our hospital. Our conclusions need these centers’ data to further test. Besides, due to limited research funding, we are unable to provide dynamic inflammatory indicators trends, which has an impact on our outcomes. However, according to previous findings in the literature, the inflammatory indexes on the first postoperative day were also highly suggestive of prognosis, and the conclusions of this study are indeed consistent with the previous literature [23]. Finally, our research population is the Chinese Han, which is noticeably different from the populations of the United States and Europe. The cut-off points may be different in the population from the US and Europe.
Conclusion
According to your findings, the morbidity of hyper-inflammation was about 12.83% in patients after ATAAD surgery. It could lead to a poor prognosis. A combination of PCT > 2.18, CRP > 49.76, IL-6 > 301.88, and SII < 2509.96 could be used to define postoperative hyper-inflammation which increased mortality and morbidity in patients after ATAAD surgery. Moreover, pre-operative bowel ischemia, pre-operative limb ischemia, CPB > 180 min and DHCA > 40 min were independent risk factors for postoperative hyper-inflammation.
Acknowledgements
Not applicable
Abbreviations
- ATAAD
Acute type-A aortic dissection
- CPB
Cardiopulmonary bypass
- DHCA
Deep hypothermia circulatory arrest
- PCT
Procalcitonin
- IL-6
Interleukin-6
- CRP
C-reactive protein
- SII
Systemic immune-inflammation index
- ACC
Aortic cross-clamp
- POD1
First postoperative day
- CABG
Coronary artery bypass grafting
- MV
Mechanical ventilation
- ECMO
Extracorporeal membrane oxygenation
- CRRT
Continuous renal replacement therapy
Author contributions
All authors contributed to the study conception and design. Y-XL, Matniyaz Y, and Y-XT were responsible for drafting the article and contributed to the data acquisition. YJ and YX-X participated in the analysis and interpretation of data and made significant contributions to the data acquisition. KP, KL, Z-WF, KW, H-TZ, HZ, and W-ZW, L-ZK participated in data collection. D-JW, TP, and F-DF made substantial contributions to the conception and design of the study and were involved in critically revising it for important intellectual content. All authors have provided their final approval for the version to be published.
Funding
This work received support from the National Natural Science Foundation of China (82300459, 82241212, 82270346), Jiangsu Provincial Key Medical Discipline (to Dong-Jin Wang No. ZDXKA2016019), Jiangsu Province Capability Improvement Project through Science,Technology and Education, Jiangsu Provincial Medical Key Discipline (ZDXK202229) and The Health Commission of Nanjing (to Tuo Pan No. YKK22096).
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to patients did not signed consents about upload the data but are available from the corresponding author on reasonable request.
Declarations
Ethical approval and consent to participate
The study and protocol received approval from the Institutional Review Board (IRB) of Nanjing Drum Tower Hospital (approval number: 2020-293-02). The study adhered to the ethical principles stated in the “Declaration of Helsinki”, the International Conference on Harmonisation-Good Clinical Practice (ICH-GCP) guideline, as well as the “Quality Management Standards for Drug Clinical Trials” and “Medical Devices Clinical Trial Quality Management Standards” established by the Chinese Food and Drug Administration (CFDA). Additionally, it complied with the “Ethical Review Measures for Biomedical Research Involving Humans” issued by the National Health Commission of China, along with other pertinent national laws and regulations. Prior to their inclusion in the study, the study participant or a legally authorized representative provided informed consent.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yuan-Xi Luo, Yusanjan Matniyaz and Yu-Xian Tang contribute equally to this study.
Contributor Information
Tuo Pan, Email: pan_tuo@126.com.
Dong-Jin Wang, Email: dongjin_wang@126.com.
Fu-Dong Fan, Email: ffd19610169@126.com.
References
- 1.Evangelista A, Isselbacher EM, Bossone E, Gleason TG, Eusanio MD, Sechtem U, Ehrlich MP, Trimarchi S, Braverman AC, Myrmel T, et al. Insights from the international registry of acute aortic dissection: a 20-year experience of collaborative clinical research. Circulation. 2018;137(17):1846–1860. doi: 10.1161/CIRCULATIONAHA.117.031264. [DOI] [PubMed] [Google Scholar]
- 2.Li M, Xu S, Yan Y, Wang H, Zheng J, Li Y, Zhang Y, Hao J, Deng C, Zheng X, et al. Association of biomarkers related to preoperative inflammatory and coagulation with postoperative in-hospital deaths in patients with type A acute aortic dissection. Sci Rep. 2021;11(1):18775. doi: 10.1038/s41598-021-98298-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Erdolu B, As AK. C-reactive protein and neutrophil to lymphocyte ratio values in predicting inhospital death in patients with stanford type A acute aortic dissection. Heart Surg Forum. 2020;23(4):E488–E492. doi: 10.1532/hsf.3055. [DOI] [PubMed] [Google Scholar]
- 4.Ma M, Shi J, Feng X, Wang J, Liu L, Wei X. The elevated admission white blood cell count relates to adverse surgical outcome of acute Stanford type a aortic dissection. J Cardiothorac Surg. 2020;15(1):48. doi: 10.1186/s13019-020-1078-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen Z-R, Huang B, Lu H-S, Zhao Z-H, Hui R-T, Yang Y-M, Fan X-H. Admission white blood cell count predicts short-term clinical outcomes in patients with uncomplicated Stanford type B acute aortic dissection. J Geriatr Cardiol. 2017;14(1):49–56. doi: 10.11909/j.issn.1671-5411.2017.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pan T, Tuoerxun T, Chen X, Yang C-J, Jiang C-Y, Zhu Y-F, Li Z-S, Jiang X-Y, Zhang H-T, Zhang H, et al. The neutrophil elastase inhibitor, sivelestat, attenuates acute lung injury in patients with cardiopulmonary bypass. Front Immunol. 2023;14:1082830. doi: 10.3389/fimmu.2023.1082830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan T, Long G-F, Chen C, Zhang H-T, Wang J-X, Ahaskar A, Chen H-B, Wang D-J. Heparin-binding protein measurement improves the prediction of myocardial injury-related cardiogenic shock. BMC Cardiovasc Disord. 2020;20(1):124. doi: 10.1186/s12872-020-01406-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duan X-Z, Xu Z-Y, Lu F-L, Han L, Tang Y-F, Tang H, Liu Y. Inflammation is related to preoperative hypoxemia in patients with acute Stanford type A aortic dissection. J Thorac Dis. 2018;10(3):1628–1634. doi: 10.21037/jtd.2018.03.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larsson M, Zindovic I, Sjögren J, Svensson PJ, Strandberg K, Nozohoor S. A prospective, controlled study on the utility of rotational thromboelastometry in surgery for acute type A aortic dissection. Sci Rep. 2022 doi: 10.1038/s41598-022-23701-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu Z, Xue Y, Fan F, Cao H, Pan J, Zhou Q, Wang D. Malperfusion syndromes in acute type A aortic dissection do not affect long-term survival in Chinese population: a 10-year institutional experience. J Card Surg. 2021;36(6):1943–1952. doi: 10.1111/jocs.15464. [DOI] [PubMed] [Google Scholar]
- 11.Li Z, Zhang H, Baraghtha S, Mu J, Matniyaz Y, Jiang X, Wang K, Wang D, Xue YX. Short- and mid-term survival prediction in patients with acute type A aortic dissection undergoing surgical repair: based on the systemic immune-inflammation index. J Inflamm Res. 2022;15:5785–5799. doi: 10.2147/JIR.S382573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sultan I, Bianco V, Aranda-Michel E, Kilic A, Serna-Gallegos D, Navid F, Wang Y, Gleason TG. The use of blood and blood products in aortic surgery is associated with adverse outcomes. J Thorac Cardiovasc Surg. 2023;165(2):544–551.e543. doi: 10.1016/j.jtcvs.2021.02.096. [DOI] [PubMed] [Google Scholar]
- 13.Wu J, Zafar MA, Liu Y, Chen JF, Li Y, Ziganshin BA, Ellauzi H, Mukherjee SK, Rizzo JA, Elefteriades JA. Fate of the unoperated ascending thoracic aortic aneurysm: three-decade experience from the Aortic Institute at Yale University. Eur Heart J. 2023 doi: 10.1093/eurheartj/ehad148. [DOI] [PubMed] [Google Scholar]
- 14.Xue Y, Pan J, Cao H, Fan F, Luo X, Ge M, Chen Y, Wang D, Zhou Q. Different aortic arch surgery methods for type A aortic dissection: clinical outcomes and follow-up results. Interact Cardiovasc Thorac Surg. 2020;31(2):254–262. doi: 10.1093/icvts/ivaa095. [DOI] [PubMed] [Google Scholar]
- 15.Zhou Q, Xue Y, Cao H, Pan J, Wang Q, Fan F, Wang D. Novel arch fenestrated stent graft for acute Stanford Type A aortic dissection with open antegrade implantation. Interact Cardiovasc Thorac Surg. 2018;26(3):369–375. doi: 10.1093/icvts/ivx335. [DOI] [PubMed] [Google Scholar]
- 16.Xue Y, Zhou Q, Pan J, Cao H, Fan F, Zhu X, Wang D. "Double jacket wrapping" root reconstruction for acute type A aortic dissection. Ann Thorac Surg. 2020;110(3):1060–1062. doi: 10.1016/j.athoracsur.2020.03.081. [DOI] [PubMed] [Google Scholar]
- 17.Asimakopoulos G, Smith PL, Ratnatunga CP, Taylor KM. Lung injury and acute respiratory distress syndrome after cardiopulmonary bypass. Ann Thorac Surg. 1999;68(3):1107–1115. doi: 10.1016/S0003-4975(99)00781-X. [DOI] [PubMed] [Google Scholar]
- 18.Zhang H-T, Han X-K, Wang C-S, Zhang H, Li Z-S, Chen Z, Pan K, Zhong K, Pan T, Wang D-J. Diagnosis of infection after cardiovascular surgery (DICS): a study protocol for developing and validating a prediction model in prospective observational study. BMJ Open. 2021;11(9):e048310. doi: 10.1136/bmjopen-2020-048310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ge M, Pan T, Wang J-X, Chen Z-J, Wang D-J. Outcomes of early versus delayed initiation of extracorporeal life support in cardiac surgery. J Cardiothorac Surg. 2019;14(1):129. doi: 10.1186/s13019-019-0950-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Z, Ge M, Chen T, Chen C, Zong Q, Lu L, Wang D. Independent risk factors and the long-term outcomes for postoperative continuous renal replacement treatment in patients who underwent emergency surgery for type a acute aortic dissection. J Cardiothorac Surg. 2020;15(1):100. doi: 10.1186/s13019-020-01153-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paparella D, Yau TM, Young E. Cardiopulmonary bypass induced inflammation: pathophysiology and treatment. An update. Eur J Cardiothorac Surg. 2002;21(2):232–244. doi: 10.1016/S1010-7940(01)01099-5. [DOI] [PubMed] [Google Scholar]
- 22.Steinbrenner H, Bilgic E, Pinto A, Engels M, Wollschläger L, Döhrn L, Kellermann K, Boeken U, Akhyari P, Lichtenberg A. Selenium pretreatment for mitigation of ischemia/reperfusion injury in cardiovascular surgery: influence on acute organ damage and inflammatory response. Inflammation. 2016;39(4):1363–1376. doi: 10.1007/s10753-016-0368-5. [DOI] [PubMed] [Google Scholar]
- 23.Liu KD, Altmann C, Smits G, Krawczeski CD, Edelstein CL, Devarajan P, Faubel S. Serum Interleukin-6 and interleukin-8 are early biomarkers of acute kidney injury and predict prolonged mechanical ventilation in children undergoing cardiac surgery: a case-control study. Crit Care. 2009;13(4):R104. doi: 10.1186/cc7940. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to patients did not signed consents about upload the data but are available from the corresponding author on reasonable request.