Abstract—
One method for managing anxiety, a highly prevalent modern mental health condition, is the calming touch sensations of deep pressure therapy (DPT). Solutions for administering DPT include the Automatic Inflatable DPT (AID) Vest, which we designed in past work. Although benefits of DPT are clear in a subset of the related literature, these benefits are not ubiquitous. There is limited understanding of what factors lead to DPT success for a given user. In this work, we present the findings of a user study (N = 25) that evaluates the effects of the AID Vest on anxiety. We compared physiological and self-reported measures of anxiety across Active (inflating) and Control (inactive) states of the AID Vest. In addition, we considered the presence of placebo effects and assessed participant comfort with social touch as a potential moderator. The results support our ability to reliably induce anxiety, and show that the Active AID Vest tended to reduce biosignals related to anxiety. We also found a significant relationship between comfort with social touch and reductions in self-reported state anxiety for the Active condition. Those who seek to successfully deploy DPT can benefit from this work.
Index Terms—: Wearable haptic devices, deep pressure sensations, anxiety management, assistive technology
I. Introduction
ANXIETY disorders are the most common mental health condition in the 21st century [1]. Sensory touch is known to lessen stereotypical physical responses to anxiety, and has been studied in a wide variety of applications [2]. The most prominent variant is deep pressure therapy (DPT), which provides relief through deep pressure sensations. Foundational work shows DPT to be a viable treatment for individuals with anxiety [3], including user groups with autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD) [4], [5]. However, these results are not universal; for example, other DPT research yielded disadvantageous effects of DPT [6], accidental encouragement of unwanted behavior via DPT [7], and inconsistent effects of DPT for child users with ASD [8]. It is evident that there are important questions about DPT that are yet to be answered, such as: is DPT effective in alleviating anxiety generally, is there a potential placebo effect of DPT, and how do individual differences shape experiences with DPT?
In our own past work in the DPT space, we designed a new device for delivering calming touch sensations as a complementary step for addressing broader DPT questions. We noticed that common DPT delivery solutions such as weighted blankets lacked portability [9], and portable options were limited to some extent by heat generation [10] or delays in pressure sensation delivery [11]. To address these limitations, we designed the Automatic Inflatable DPT (AID) Vest, as introduced in our previous work [12] and shown in Fig. 1. Our device is lined with soft inflatable actuators to offer faster and potentially more comfortable deep pressure sensations compared to similar systems. Additional details of the system hardware design appear in [12]. Initial evaluations of the system’s efficacy showed that we could reliably induce anxiety for the purpose of controlled user evaluations [12] and offered mixed results on the AID Vest’s influence on anxiety [13]. Although the core results were unclear, we noticed a potential relationship between participants’ social touch comfort and experiences with the vest.
Fig. 1.

Our study setup. On the left, a participant wears the AID Vest, a blue commercial fleece vest with custom inflatable actuators in its lining.
In the presented follow-on work in this paper, our central research goal was to investigate the anxiety-reducing effects of the AID Vest on a larger user group and explore how potential moderators, namely placebo and comfort with social touch, shape experiences with DPT. We first present related foundational work in Section II. Section III describes the methods of our study, during which we induced and reduced anxiety in a lab setting. We present the results of the study in Section IV and discuss insights, strengths, and limitations of the work in Section V. Key contributions of this paper include confirmation of reliable techniques for inducing anxiety in wearable electronics work, expanded results of the AID Vest’s influence on anxiety, and insights on the potential impact of key moderating factors in DPT work. This work can benefit others who seek to understand links between DPT and comfort with social touch, as well as how to successfully leverage DPT.
II. Related Work
To succeed in the proposed work, we needed a strong understanding of anxiety treatment, methods for administering DPT, and methods of measuring anxiety.
Anxiety and Touch:
The prevalence of anxiety is high, with a reported 264 million people living with anxiety disorders as of 2015 [14]. Although touch interactions are essential to human development [15], gaining this type of contact can be challenging for individuals with anxiety. For example, past work has shown that people with greater social anxiety tend to be less comfortable with touch [16]. Similarly, people with ASD, which often co-occurs with anxiety, benefit from touch sensations but can find interpersonal touch distressing [17]. Deep pressure therapy (DPT) is one solution for addressing this tension; DPT uses non-invasive pressure sensations, such as those provided by weighted vests, weighted blankets, and inflatable vests, to promote feelings of calmness [3].
DPT has been demonstrated to alleviate anxiety in selected past studies (e.g., [4], [9]). The positive impact of DPT, however, is not universal. For example, a review paper on the use of weighted vests by children with ASD showed that individual differences impact DPT benefits, and that factors like the method of engagement and duration of vest use can influence DPT success [8]. Further, long-term DPT use and DPT applied incorrectly can lead to adverse effects [6], [7]. Overall, it is apparent that DPT is well motivated and can be useful, but that factors impacting its efficacy require further study. We aim to address this gap in our work by evaluating the usefulness of the AID Vest for reducing anxiety and exploring the impact of likely moderating factors on responses to inflatable vest-based DPT.
Administering DPT:
While weighted blankets are the most well-known form of applying DPT, other options exist in the form of wearables, such as hugging vests [18], weighted vests [19], and inflatable vests [11]. Across these devices, most have key design limitations for on-demand day-to-day use, such as discomforting heat generation, heavy weight, and limited portability. Other DPT systems are portable, but are slow to activate [10], [11]. These gaps led us to previously design the AID Vest, a lightweight, portable device for timely deep pressure sensations [12]. To create this device, we lined a commercial fleece vest with soft inflatable actuators that provide deep pressure sensation on the abdomen, chest, and back. The actuators can fully inflate to an internal pressure of 2.2 psi and deflate in under one minute.
Measuring Anxiety:
Monitoring anxiety in reasonable ways was important to our study design. Anxiety is commonly measured by tracking changes in related biosignals, especially electrodermal activity (EDA), heart rate (HR), and heart rate variability (HRV) [20], [21]. Stress and anxiety, although different, are often referred to interchangeably when it comes to biosignal tracking. Stress is an umbrella term that includes emotions and stressors such as fear, nervousness, or sadness. Exposure to stressors often leads to generalized anxiety [22]. Thus, common measurement techniques for social anxiety include the use of biosignals such as EDA and HR, which are also used to monitor for stress [22], [23], [24]. EDA and HR can be tracked relatively easily with either electrical activity-monitoring electrocardiogram (ECG) or optical photoplethysmography (PPG) sensors. HRV requires ECG readings for accurate calculation [25]. Since optical sensors (i.e., the Polar Verity Sense [26]) seemed to be most appropriate in our study scenario, we accordingly gauged HR, rather than HRV, in our work. Self-reported anxiety via the State Trait Anxiety Inventory (STAI) is also a strongly validated method of anxiety measurement [27], [28]. Hence, we considered EDA, HR, and STAI-based self-reported anxiety in our study.
III. Methods
We conducted a within-subjects study to confirm our ability to induce anxiety, clarify vest effects, and consider possible mitigating factors of DPT success. Our university ethics board approved this work under protocol #IRB-2020–0616.
Anxiety-Affecting Activities:
To conduct the proposed research, we needed methods for inducing anxiety and returning participants to a more relaxed state between conditions.
We used Trier Social Stress Test (TSST) [29] activities for inducing anxiety in participants, namely:
Mental Math: counting back from 1022 by 13. A buzzer sounded and the participant started over upon any error.
Mock Interview: pitching themselves for their dream job to a mock panel, with no preparation time.
We selected these activities because they induced more anxiety than other TSST tasks during earlier experimental evaluation [12]. The participants faced a panel of confederates from our research lab while performing the TSST activities. To enhance the effectiveness of the anxiety-inducing activities, these confederates were instructed to convey equipoise and avoid conversing with participants throughout the study.
To help return participants to baseline anxiety levels between study activities, we administered the following:
4–7-8 Breathing: completing the following cycle four times: breathe in for four counts, hold breath seven counts, breathe out eight counts [30].
Study Design:
Participants performed both TSST activities, with one possible state of the AID Vest per activity:
Active State: vest inflated at activity halfway point.
Control State: vest remained inactive throughout activity.
The order of the TSST activities and combination of activity and vest state was counterbalanced across participants. The AID Vest remained in the deflated Control state during all instances of the 4–7-8 breathing exercise. Fig. 2 shows the overall flow of the study design.
Fig. 2.
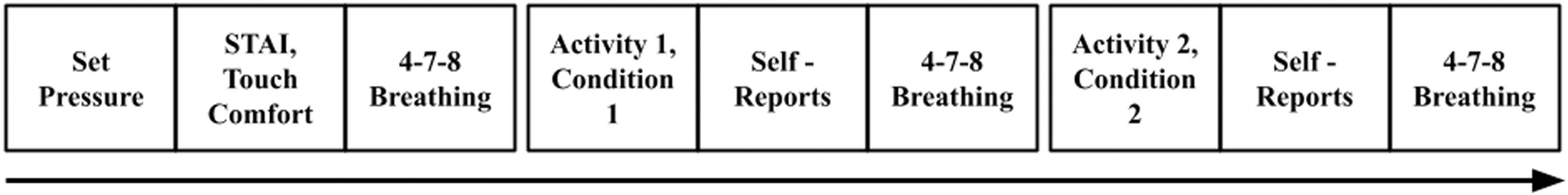
The schematic flow of the study procedure. The order and crossing of each activity and condition was counterbalanced across participants.
Hypotheses:
Our investigated hypotheses were as follows:
H1: Users will experience anxiety during the TSST activities, as indicated in their respective biosignals.
H2: Users will show a decrease in anxiety during Active state of the AID Vest, compared to the Control state.
H3: The relationship between AID Vest sensations and anxiety will be moderated by social touch comfort.
Measures:
Measures included objective and self-reported data. To gauge biosignals related to anxiety [22], we used:
Electrodermal Activity (EDA): recorded at 4 Hz in microsiemens using the Empatica E4 wristband [31].
Heart Rate (HR): recorded at 1 Hz in beats per minute using the Polar Verity Sense optical sensor [26].
To support the analysis outlined later, EDA and HR levels were tagged (i.e., recorded via button press on the device) at the start and end of the following events:
Pressure selection: before the anxiety-affecting activities, participants selected a preferred max vest pressure.
Baselining: the first instance of the 4–7-8 breathing exercise prior to commencing the TSST activities.
TSST Activities: each TSST activity used in the study.
Return to Baseline: instances of the 4–7-8 breathing after each TSST activity.
Percentage decline of EDA and HR for each TSST activity was computed to assess the effects of vest conditions.
The self-reported measures were as follows:
State Trait Anxiety Inventory (STAI) Test: measured general anxiety levels with the full Trait test, and reactive anxiety levels with a modified State test [28]. The six-item short form of the State test was administered after each TSST activity [32]
Attitude Self-Assessment Manikin (AdSAM): captured affective state while using the AID Vest [33].
Modified Quantitative Affect Scale (QAS): captured emotional responses and feeling intensity [34].
Modified Interpersonal Touch Comfort Scale: we used the six questions from a relevant inventory [35], which covered comfort with touch generally, receiving touch from others, touch in social situations, and touch in the form of hugs. The questions were chosen for their focus on comfort with social touch; these scales combined yielded each participant’s social touch comfort score.
Custom DPT Questions: captured participant belief in DPT effectiveness (on a 5-point scale from very low to very high) and experience with DPT.
Procedure:
Participants began the study by signing a consent form. Next, they donned the Empatica E4 on their dominant wrist and the Polar Verity Sense sensor on their forearm. We collected participants’ demographic information, including the Trait test, short-form State test, Touch Comfort Scale, and DPT questions. The Empatica E4 required 15 minutes to calibrate, so participants next completed an unrelated computer-based survey of sufficient length to fill this time. Participants donned the AID Vest and were asked to identify a comfortable inflated pressure level that felt like a tight hug. The vest was then deflated, and participants proceeded to complete the first (baselining) 4–7-8 breathing exercise. Next, participants performed the first TSST activity while experiencing one state (randomized) of the vest. Upon completion of the activity, participants answered the short-form State test, AdSAM, and modified QAS survey. They then completed the second instance (return to baseline) of the 4–7-8 breathing exercise. Next came the second TSST activity with the remaining vest state, followed by the same post-activity surveys. Lastly, participants completed the breathing exercise for the third time (return to baseline). After a post-study interview, participants were paid $15 US for the hour-long study.
Participants:
We recruited 25 participants (20 male, 5 female) aged 18–30 years (M = 22.82, SD = 3.10). Based on standard STAI Trait test scoring [27], 13 participants reported having generally high anxiety, six reported having moderate anxiety, and six reported having low anxiety. Seven participants reported being highly comfortable with social touch, 12 moderately comfortable, and six uncomfortable. 14 participants reported a high belief in DPT, three reported a very high belief, and eight were neutral. Finally, five participants had prior experience with DPT via weighted blankets.
Analysis:
Induction of anxiety was computed as the percentage increase in biosignal readings (i.e., EDA, HR) from the TSST activity start to the peak reading during that TSST activity, as shown by the yellow and green circles, respectively, in the illustrative examples in Figs. 3 and 4. We used a one-sample t-test to assess whether anxiety increased in the EDA and HR signals. Reduction in anxiety was computed as the percentage decline in biosignal readings from the peak during the TSST activity to the starting value of the return to baseline (i.e., breathing exercise), as shown by the green and red circles in Fig. 3, respectively. On the individual level, we considered whether each participant experienced a greater decline in each anxiety measure with the Control or Active condition. We determined individual differences for anxiety measures using repeated measures ANOVA (rANOVA) tests. Due to our small sample size, normality assumptions may not be satisfied; however, previous work supports our selection of an ANOVA test even when normality assumptions are not met [36], [37]. To evaluate whether placebo effects or touch comfort were potential moderating factors, ANCOVA tests were conducted with each potential factor and each anxiety measure. All tests used an α = 0.05 significance level. Thematic qualitative analysis was performed on participants’ post-study interviews. For brevity, in this paper we present results from biosignals, self-reported data excluding the AdSAM and QAS, and thematic analysis.
Fig. 3.
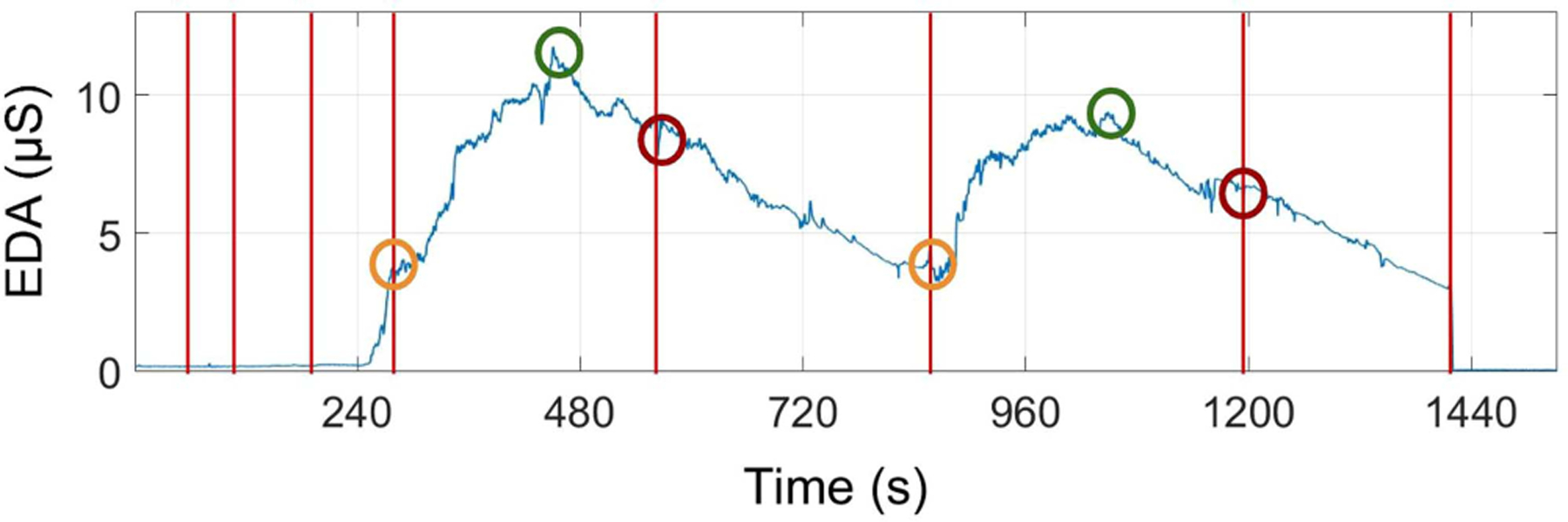
Illustrative EDA reading for one participant depicting tagged events (vertical lines) and key data points for later analysis computations (circles).
Fig. 4.
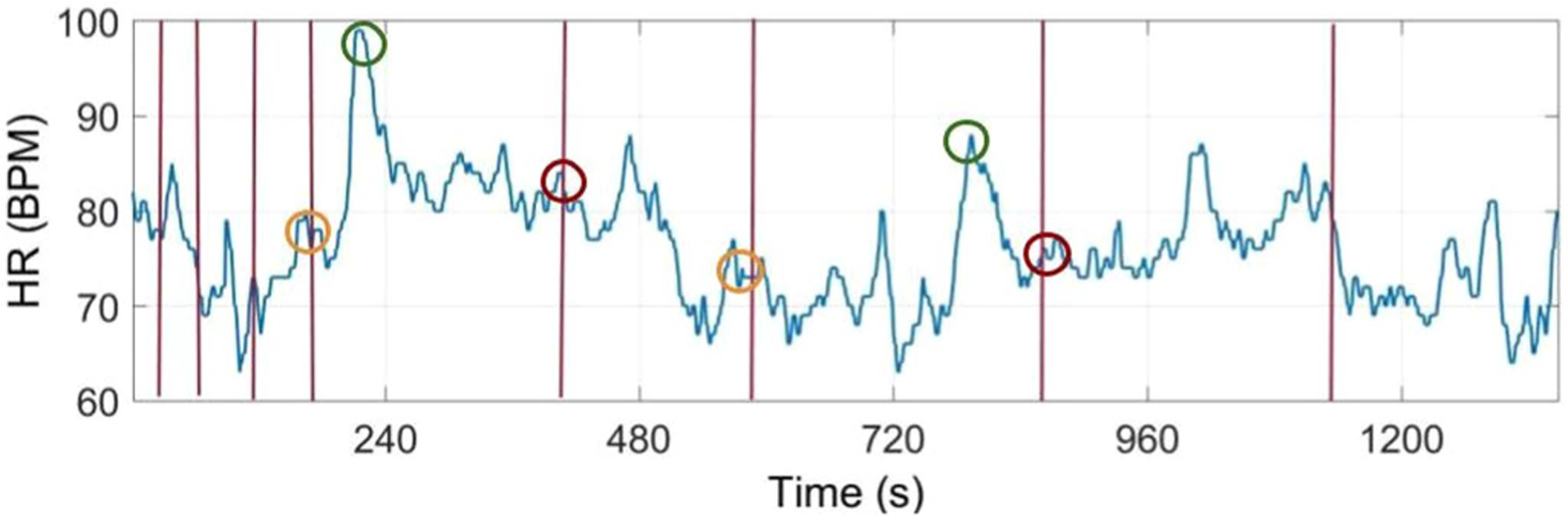
Illustrative HR reading for one participant depicting tagged events (vertical lines) and key data points for later analysis computations (circles).
IV. Results
All 25 participants successfully completed the study. All data mentioned in the methods was successfully recorded other than one participant’s post-study interview data, which failed to save correctly. The corresponding results are presented in the following subsections, which are organized to help address our core hypotheses and research questions.
Anxiety Induction:
To assess the influence of the anxiety-inducing activities, we considered the increases of anxiety observed in the biosignals across the experienced ordering and experienced TSST activity. This was an important first check, since if anxiety was not induced, the influence of the AID Vest would be unclear. Results of the t-tests on anxiety induction data showed that percent increase in anxiety was significantly greater than zero in both the EDA (p = 0.026) and the HR (p< 0.001) data, indicating that anxiety was consistently induced. For 49 of the 50 participant-activity pairings, EDA signals showed an increase in anxiety; the same was true for HR readings in 47 of 50 cases. In every activity (50 of 50 possible), either EDA or HR increased.
Anxiety Reduction with the AID Vest:
To evaluate the effects of the AID Vest on reducing anxiety, we compared decline in biosignals across the experienced ordering, experienced TSST activity, and experienced vest condition. We observed no evidence of ordering-based or TSST activity-based effects; the experience (i.e., first or second activity experienced; Mental Math or Mock Interview) with more anxiety reduction was always split evenly across these cases (i.e., 12 or 13 of the 25 total participants). rANOVA tests confirmed that there were no significant differences across ordered experience or TSST activity (all p > 0.187). There was some evidence of a vest condition effect; the majority of participants (15 out of 25) experienced a greater decline in EDA with the Active vest, compared to the Control condition. The Active condition also led to a greater decline in HR for the majority of users (14 out of 25). However, rANOVA tests showed no statistically significant differences in EDA or HR decline between Active and Control vest conditions (all p > 0.492).
Self-reported anxiety from the State tests were also analysed. As with the biosignals, the results of the State test showed no evidence of ordering-based effects; the experience (i.e., first or second activity experienced) with lower self-reported anxiety at the conclusion was evenly split. rANOVA tests confirmed this inference; there were no significant differences across ordered experience (p = 0.978). On the other hand, there was evidence of possible TSST activity-based and AID Vest condition-based effects. For the former, a majority of participants reported having higher anxiety after experiencing the Mock Interview (16 out of 25), and this effect was statistically significant (p = 0.047). For the latter, and in contrast with the biosignal reading trends, the majority of participants reported experiencing higher anxiety with the Active vest condition (14 out of 25); however, this difference was not statistically significant (p = 0.329).
In summary, as also reflected in the results roundup in Table I, we found no reliable effect of the AID Vest reducing anxiety in the Active condition more than the Control condition. There were substantial individual differences: the majority of participants showed meaningful reductions in anxiety, but some did not show any change in anxiety, and a few even showed increased anxiety. Our findings align with past research showing inconsistent benefits of DPT (and other pressure-based treatments) for individuals with anxiety [8]. We posit the inconsistent benefits of DPT demonstrated here and in previous work suggest the presence of one or more variables moderating the effect of pressure on anxiety relief.
TABLE I.
Statistical Analysis Results for Anxiety Reduction-Related Tests and Tests of Potential Covariates
| EDA | HR | State | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| df | F | η | p | df | F | η | p | df | F | η | p | |
|
| ||||||||||||
| Order-based Effects | 1 | 0.744 | 0.013 | 0.397 | 1 | 1.628 | 0.030 | 0.214 | 1 | <0.001 | <0.001 | 0.978 |
| Activity-based Effects | 1 | 0.208 | 0.004 | 0.652 | 1 | 1.846 | 0.034 | 0.187 | 1 | 4.399 | 0.045 | *0.047 |
| Condition-based Effects | 1 | 0.488 | 0.008 | 0.492 | 1 | 0.268 | 0.005 | 0.609 | 1 | 0.995 | 0.011 | 0.329 |
| Touch Comfort ANCOVA | 15 | 0.601 | 0.215 | 0.853 | 1 | 1.477 | 0.614 | 0.230 | 15 | 2.837 | 0.563 | *0.006 |
| Belief in System ANCOVA | 15 | 2.261 | 0.131 | 0.109 | 2 | 1.727 | 0.070 | 0.189 | 2 | 1.038 | 0.053 | 0.352 |
Belief in System and Touch Comfort as Potential Moderators:
One potential moderator we considered was participants’ belief in DPT technologies, since a strong prior belief in DPT could produce a placebo effect. We found that a majority of participants reported having either high or very high belief in DPT effectiveness, but there was no clear trend between these ratings and performance with the AID Vest. To statistically verify this result, ANCOVAs including this belief in DPT factor were conducted on EDA declines, HR declines, and State test scores across vest condition. No significant relationship was found (all p > 0.109); hence, a placebo effect was not observed.
Based on connections between DPT use and touch comfort in the related literature, ANCOVAs were likewise conducted to evaluate touch comfort as a potential moderator of the effect of the AID Vest on anxiety reduction. Although all participants with low touch comfort experienced a greater decline in EDA for the Active vest condition, this effect was not statistically significant. In fact, there were no significant relationships between EDA or HR decline and touch comfort across vest conditions (all p> 0.230), as shown in Table I. There was, however, a significant difference in State test scores across vest condition when including touch comfort as a covariate (p = 0.006). Those who reported high touch comfort experienced a greater reduction in anxiety in the Active condition relative to those who reported low touch comfort. This result led us to pursue an exploratory analysis of participant self-reports to try to identify the user group who might benefit most consistently from DPT technologies.
Participant-Identified Themes:
We conducted a thematic analysis of the post-study interviews. Key codes derived from this process were as follows: descriptions of the vest as helpful, descriptions of the DPT as calming or comforting, positive notes about the pressure from the system, descriptions of the vest as awkward, notes about feeling hot, and descriptions of the vest as distracting. These codes seemed to fall into two natural valence groupings: positive and negative themes.
We matched the participant-identified themes to biosignal data and found that, out of 11 participants who fell in the positive group when reporting on their Active vest experience, nine showed a greater decline in anxiety (as measured by biosignals) with the Active vest. Similarly, out of 10 participants who fell in the negative-valence group for Active vest experience, six experienced a greater decline in anxiety with the Control vest. The remaining three participants had neutral comments.
V. Discussion
In order to gain a better understanding of DPT with wearable devices, we conducted a user study evaluating the AID Vest’s effects on reducing anxiety. We sought to validate methods of inducing anxiety with a larger participant group than in our past work, compare reduction of anxiety between Active and Control vest conditions, and evaluate factors that may moderate participants’ experiences.
Physiological biosignal readings provide strong support of H1. The method of inducing anxiety via a modified TSST procedure appears to be repeatable, and we recommend it for reliable anxiety induction in the wearable electronics space. The Mock Interview task is particularly effective as a activity choice for yielding raised, and even prolonged raised, anxiety.
The expected reduction of anxiety in H2, however, was met by mixed results. Across the participant group, there were no significant differences in any of the anxiety measures between the Active and Control conditions. Since we recruited broadly for this study (not necessarily including, for example, only participants with anxiety disorders), we considered that the AID Vest may be useful for some (but not all) participants; thus, we examined anxiety change experiences on an individual level as well. We found that for all analyzed biosignals, a greater number of participants experienced a reduction in anxiety with the Active versus Control vest condition, irrespective of condition ordering or anxiety induction activity. However, the participants who experienced a greater decline in EDA levels with the Active vest, were not necessarily the same participants who experienced a greater decline in HR levels. Self-reported State anxiety tended in the opposite direction; a majority of participants reported higher anxiety at the end of the Active vest condition, compared to the Control vest condition. In all, it was necessary to consider moderating factors to try to gain a better understanding of how and whether DPT via the AID Vest can provide consistent benefits.
Analyses related to H3 helped us to better understand whether expected and unexpected moderating factors might be influencing the observed changes in anxiety. Our results did not support the idea of the placebo effect as a moderating factor. On the other hand, touch comfort seemed to play a role in anxiety reduction experiences. Participants with high touch comfort reported significantly more reduction in anxiety for the Active vest condition compared to those with low touch comfort. This experience could be due to similarities between the vest use experience and the experience of being hugged; three participants drew a parallel, describing the vest as feeling like a “warm hug” or “comforting hug,” and one user even mentioned “wish[ing] it would also cover the arms.”
Central design implications in this work mainly relate to the idea that DPT may be helpful to some individuals with anxiety, but is not a one-size-fits-all solution. Due to the prevalence of anxiety in modern society, the need for easy-to-access anxiety management solutions is pressing. At the same time, as evidenced in our past conversations with mental health professionals (discussed further in our past work [12]), it is clear that there is no one-size-fits-all anxiety management tool. Some individuals with anxiety may have the time and financial resources needed to access therapists, some may prefer (or prefer to avoid) medication-based solutions, and likewise, individuals may be drawn to (or repelled from) other newer anxiety management tools. In the case of DPT, for example, the deep pressure sensations may be comforting to someone who enjoys hugs, but stressful to someone who is claustrophobic. Along these lines, our findings support the idea that screening potential users of DPT using social touch comfort scales may help to identify users who would benefit most from this approach, although touch comfort is not the only factor that matters. Further work is required to solidify our understanding of the relationship between DPT and touch comfort, and to prescribe guidelines for successful DPT use.
One strength of this work is repeatable methods for reliably inducing anxiety in the wearable electronics field. While formulating this research, we tested the majority of approaches used for this purpose from the related DPT literature, and we have found the TSST to be the main repeatable method from this past work. Within our own work, we have found these effects to repeat across early testing [12] and a pilot version of the current study [13] previously. Our past evaluations involved only two participants [12]; thus, the larger study presented here substantially advanced our understanding of DPT delivery via the AID Vest. We propose the increased clarity on factors that may or may not be moderating DPT experience as a strength of the work. Although this question is not fully closed, compared to other work, we were able to provide more evidence that cases of success with DPT are not due to the placebo effect, and that touch comfort is an important moderating factor of DPT success. Based on this work, others who are interested in helping to expand the understanding of DPT can more quickly formulate ways to induce anxiety in in-lab studies and identify candidates who are likely to respond well to DPT-based treatment of anxiety.
There are also key limitations of this work. The sensors used for collecting biosignal data are subject to motion artifacts, which had the potential for introducing errors in the biosignal data. One potential future method for addressing this would be using ECG recordings, which are less susceptible to motion artifacts, to gauge HR and HRV. Further, the participants recruited in this study did not necessarily have a clinical diagnosis of anxiety, and they thus are not wholly representative of users who would seek or benefit from systems like the AID Vest. Refinements to the recruiting process based on the moderating factors identified in this work, movement towards working with individuals with diagnosed or self-diagnosed anxiety, and better balancing of participant demographics (for example, gender-balancing participants) would support stronger findings in future research steps.
VI. Conclusion
This paper establishes the need to investigate DPT with respect to not only the method of administration, but the individual experiencing it. The results of the user study show that anxiety induction methods and subsequent reduction are repeatable with wearable devices, and show some potential of DPT administered with the AID Vest. The relationship of comfort with social touch provides promising insight, and calls the need for future studies exploring other factors that impact DPT. DPT can be used to provide calming sensation to those who lack access to sensory touch from others, whether by preference or circumstance. Understanding how to determine who benefits the most from DPT and how to optimize its effects is therefore essential.
Acknowledgment
We would like to thank David Kerr for his study design advice.
Footnotes
This paper was recommended for publication by Associate Editor Jan B.F. van Erp and Editor-in-Chief S. Choi upon evaluation of the reviewers’ comments.
This work involved human subjects or animals in its research. Approval of all ethical and experimental procedures and protocols was granted by the Oregon State University IRB under Application No. #IRB-2020-0616.
References
- [1].Bandelow B and Michaelis S, “Epidemiology of anxiety disorders in the 21st century,” Dialogues Clin. Neurosci, vol. 17, pp. 327–335, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Morrison I, “Keep calm and cuddle on: Social touch as a stress buffer,” Adaptive Hum. Behav. Physiol, vol. 2, pp. 344–362, 2016. [Google Scholar]
- [3].Krauss KE, “The effects of deep pressure touch on anxiety,” Amer. J. Occup. Ther, vol. 41, no. 6, pp. 366–373, 1987. [DOI] [PubMed] [Google Scholar]
- [4].Vasa RA et al. , “A systematic review of treatments for anxiety in youth with autism spectrum disorders,” J. Autism Devlop. Disord, vol. 44, no. 12, pp. 3215–3229, 2014. [DOI] [PubMed] [Google Scholar]
- [5].VandenBerg NL, “The use of a weighted vest to increase on-task behavior in children with attention difficulties,” Amer. J. Occup. Ther, vol. 55, no. 6, pp. 621–628, 2001. [DOI] [PubMed] [Google Scholar]
- [6].Bestbier L and Williams TI, “The immediate effects of deep pressure on young people with autism and severe intellectual difficulties Demonstrating individual differences,” Occup. Ther. Int, vol. 2017, 2017, Art. no. 7534972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Zissermann L, “The effects of deep pressure on self-stimulating behaviors in a child with autism and other disabilities,” Amer. J. Occup. Ther, vol. 46, no. 6, pp. 547–551, 1992. [DOI] [PubMed] [Google Scholar]
- [8].Stephenson J and Carter M, “The use of weighted vests with children with autism spectrum disorders and other disabilities,” J. Autism Devlop. Disord, vol. 39, no. 1, pp. 105–114, 2009. [DOI] [PubMed] [Google Scholar]
- [9].Chen H-Y, Yang H, Chi H-J, and Chen H-M, “Physiological effects of deep touch pressure on anxiety alleviation: The weighted blanket approach,” J. Med. Biol. Eng, vol. 33, pp. 463–470, 2013. [Google Scholar]
- [10].Foo E and Holschuh B, “Dynamic compression in affective haptics,” in Proc. ACM Int. Joint Conf. Int. Symp. Pervasive Ubiquitous Comput. Wearable Comput, 2018, pp. 577–583. [Google Scholar]
- [11].Reynolds S, Lane SJ, and Mullen B, “Effects of deep pressure stimulation on physiological arousal,” Amer. J. Occup. Ther, vol. 69, no. 3, pp. 1–5, 2015. [DOI] [PubMed] [Google Scholar]
- [12].Brown H, Shannon E, and Fitter NT, “Design and preliminary evaluation of the aid vest: An automatic inflatable wearable device for anxiety reduction,” in Proc. IEEE World Haptics Conf., 2021, pp. 745–750. [Google Scholar]
- [13].Bontula A, Preston RC, Shannon E, and Fitter NT, “Pilot human user evaluation of the automatic inflatable deep pressure therapy vest,” in Proc. Haptics Symp. Mentoring Forum, 2022, pp. 1–3. [Google Scholar]
- [14].Rosiar R, “Our daily friend in disguise: Anxiety in the 21st century–Part I,” Feb. 2021. [Online]. Available: https://www.cross-current.org/posts/anxiety-in-the-21st-century [Google Scholar]
- [15].Sonneveld MH and Schifferstein HN, “The tactual experience of objects,” in Product Experience New York, NY, USA: Elsevier, 2008, pp. 41–67. [Google Scholar]
- [16].Kashdan TB, Doorley J, Stiksma MC, and Hertenstein MJ, “Discomfort and avoidance of touch: New insights on the emotional deficits of social anxiety,” Cogn. Emotion, vol. 31, no. 8, pp. 1638–1646, 2017. [DOI] [PubMed] [Google Scholar]
- [17].Borgman S, “Touch and the autism spectrum,” Nov. 2011. [Online]. Available: https://www.psychologytoday.com/us/blog/spectrum-solutions/201111/touch-and-the-autism-spectrum [Google Scholar]
- [18].Duvall JC, Dunne LE, Schleif N, and Holschuh B, “Active “hugging” vest for deep touch pressure therapy,” in Proc. ACM Int. Joint Conf. Pervasive Ubiquitous Comput.: Adjunct, 2016, pp. 458–463. [Google Scholar]
- [19].Lin H-Y, Lee P, Chang W-D, and Hong F-Y, “Effects of weighted vests on attention, impulse control, and on-task behavior in children with attention deficit hyperactivity disorder,” Amer. J. Occup. Ther, vol. 68, no. 2, pp. 149–158, 2014. [DOI] [PubMed] [Google Scholar]
- [20].Naveteur J and Baque EFI, “Individual differences in electrodermal activity as a function of subjects’ anxiety,” Pers. Individual Differences, vol. 8, no. 5, pp. 615–626, 1987. [Google Scholar]
- [21].Licht CM, De Geus EJ, Van Dyck R, and Penninx BW, “Association between anxiety disorders and heart rate variability in The Netherlands study of depression and anxiety (NESDA),” Psychosomatic Med, vol. 71, no. 5, pp. 508–518, 2009. [DOI] [PubMed] [Google Scholar]
- [22].Giannakakis G, Grigoriadis D, Giannakaki K, Simantiraki O, Roniotis A, and Tsiknakis M, “Review on psychological stress detection using biosignals,” IEEE Trans. Affect. Comput, vol. 13, no. 1, pp. 440–460, Jan.–Mar. 2022. [Google Scholar]
- [23].Stein MB and Stein DJ, “Social anxiety disorder,” Lancet, vol. 371, no. 9618, pp. 1115–1125, 2008. [DOI] [PubMed] [Google Scholar]
- [24].Heimberg RG, Mueller GP, Holt CS, Hope DA, and Liebowitz MR, “Assessment of anxiety in social interaction and being observed by others: The social interaction anxiety scale and the social phobia scale,” Behav. Ther, vol. 23, no. 1, pp. 53–73, 1992. [Google Scholar]
- [25].Shaffer F and Ginsberg JP, “An overview of heart rate variability metrics and norms,” Front. Public Health, 2017, Art. no. 258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].“Polar verity sense,” 2023. [Online]. Available: https://www.polar.com/en [Google Scholar]
- [27].Metzger RL, “A reliability and validity study of the state-trait anxiety inventory,” J. Clin. Psychol, vol. 32, pp. 276–278, 1976. [Google Scholar]
- [28].Julian L, “Measures of anxiety: State-trait anxiety inventory (STAI), beck anxiety inventory (BAI), and hospital anxiety and depression scale-anxiety (HADS-A),” Arthritis Care Res, vol. 63, no. 11, pp. 467–472, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Birkett MA, “The trier social stress test protocol for inducing psychological stress,” J. Visualized Experiments, no. 56, 2011, Art. no. e3238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Zaccaro A et al. , “How breath-control can change your life: A systematic review on psycho-physiological correlates of slow breathing,” Front. Hum. Neurosci, vol. 12, 2018, Art. no. 353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].“E4 wristband: Real-time physiological signals. Wearable PPG, EDA, temperature, motion sensors,” 2023. [Online]. Available: https://www.empatica.com/research/e4/ [Google Scholar]
- [32].Marteau TM and Bekker H, “The development of a six-item short-form of the state scale of the spielberger state-trait anxiety inventory (STAI),” Brit. J. Clin. Psychol, vol. 31, no. 3, pp. 301–306, 1992. [DOI] [PubMed] [Google Scholar]
- [33].“Attitude self-assessment manikin survey,” 2020. [Online]. Available: https://adsam.com/survey/ [Google Scholar]
- [34].Block AE, “HuggieBot: An interactive hugging robot with visual and haptic perception,” Ph.D. dissertation, ETH Zurich, Zürich, Switzerland, 2021. [Google Scholar]
- [35].Webb A and Peck J, “Individual differences in interpersonal touch: On the development, validation, and use of the “comfort with interpersonal touch” (CIT) scale,” J. Consum. Psychol, vol. 25, no. 1, pp. 60–77, 2015. [Google Scholar]
- [36].Mena MJB et al. , “Non-normal data: Is ANOVA still a valid option?,” Psicothema, vol. 29, pp. 552–557, 2017. [DOI] [PubMed] [Google Scholar]
- [37].Feir-Walsh BJ and Toothaker LE, “An empirical comparison of the ANOVA f-test, normal scores test and kruskal-wallis test under violation of assumptions,” Educ. Psychol. Meas, vol. 34, no. 4, pp. 789–799, 1974. [Google Scholar]


