Abstract
Objectives:
Frequent sugar-sweetened beverage (SSB) intake is associated with weight gain in women, and pre-pregnancy overweight and excessive gestational weight gain are linked to adverse pregnancy outcomes. SSB intake information for women of reproductive age (WRA) is limited. We described SSB intake among non-pregnant and pregnant WRA and identified correlates of daily intake.
Methods:
Using 2017 Behavioral Risk Factor Surveillance System data, we analyzed SSB intake (regular soda, fruit drinks, sweet tea, sports/energy drinks) for 11,321 non-pregnant and 392 pregnant WRA (18–49 years) in 12 states and D.C. Adjusted odds ratios (aOR) for daily (≥1 time/day) SSB intake (reference: <1 time/day) by characteristics were estimated using multivariable logistic regression.
Results:
Overall, 27.3% of non-pregnant and 21.9% of pregnant women reported consuming SSBs ≥1 time/day; 12.6% and 9.7%, respectively, consumed SSBs ≥2 times/day. Among non-pregnant women, odds of daily SSB intake were higher for women who were non-Hispanic black (aOR=2.04, 95% CI=1.55–2.69) vs. non-Hispanic white; had ≤high school education (aOR=2.79, CI=2.26–3.44) or some college (aOR=1.85, CI=1.50–2.27) vs. college graduates; lived in nonmetropolitan counties (aOR=1.35, CI=1.11–1.63) vs. metropolitan; had no physical activity (aOR=1.72, CI=1.43–2.07) vs. some; were former (aOR=1.51, CI=1.17–1.94) or current (aOR=3.48, CI=2.82–4.28) smokers vs. nonsmokers. Among pregnant women, those not married had higher odds (aOR=2.81, CI=1.05–7.51) for daily SSB intake than married women.
Conclusions:
SSB intake information for WRA can inform efforts to promote healthy weight and appropriate gestational weight gain, potentially reducing the risk of adverse pregnancy outcomes.
Keywords: sugar-sweetened beverage intake, pregnancy, women of reproductive age, health behaviors, disparities
Introduction
Sugar-sweetened beverages (SSBs) are drinks with added sugars, which can include non-diet soda, fruit drinks that are not 100% fruit juice, sports drinks, energy drinks, and sweetened coffee or tea drinks. SSBs are a leading source of added sugars in the diet of U.S. adults (Drewnowski & Rehm, 2014). SSB intake is a public health issue, since frequent consumption is associated with poor diet quality and an increased risk of adverse health outcomes including weight gain, obesity, type 2 diabetes, and hypertension (Dhingra et al., 2007; Malik, Akram, Shetty, Malik, & Njike, 2014; Schulze et al., 2004; Sharkey, Johnson, & Dean, 2011). Surveillance of SSB intake through the National Health and Nutrition Examination Survey (NHANES) data has shown that 49.3% of U.S. adults consumed ≥1 SSBs on a given day (2011–2014) (Rosinger, Herrick, Gahche, & Park, 2017). Few studies have examined SSB intake among pregnant and non-pregnant women of reproductive age (Chen, Hu, Yeung, Willett, & Zhang, 2009; Cioffi, Figueroa, & Welsh, 2018; Gillman et al., 2017). A recent U.S. study that combined NHANES data from 2003–2012 to enable an adequate sample size, found that the average daily intake of added sugars from SSBs was 38.6 grams among pregnant women (n=650) and 39.6 grams among non-pregnant women of reproductive age (n=3,529) (Cioffi et al., 2018).
Information on SSB intake among pregnant and non-pregnant women of reproductive age is important, as frequent SSB intake is associated with weight gain in women (Schulze et al., 2004). Furthermore, pre-pregnancy overweight and obesity are associated with an increased risk of numerous adverse pregnancy and birth outcomes, including gestational diabetes, preeclampsia, pregnancy induced hypertension, large for gestational age (LGA) neonates, macrosomia, induction of labor, cesarean delivery, preterm delivery, and postpartum hemorrhage (Baeten, Bukusi, & Lambe, 2001; Li et al., 2013; Magann, Doherty, Sandlin, Chauhan, & Morrison, 2013; Sebire et al., 2001). Additionally, excessive gestational weight gain is associated with adverse outcomes such as LGA, macrosomia, preterm birth, cesarean delivery, pregnancy induced hypertension, and preeclampsia (Drehmer, Duncan, Kac, & Schmidt, 2013; Hutcheon et al., 2018; Li et al., 2013).
Given the potential adverse health consequences of pre-pregnancy overweight and obesity and excessive gestational weight gain, understanding current SSB intake patterns among women of reproductive age can be useful to inform interventions to reduce SSB intake in this population. The aims of the present analysis were to describe the frequency of SSB intake among non-pregnant and pregnant women of reproductive age and to identify sociodemographic and behavioral characteristics associated with daily intake of SSBs.
Methods
This analysis was performed using 2017 data from the Behavioral Risk Factor Surveillance System (BRFSS), a state-based, random–digit–dial telephone survey of U.S. adults aged ≥18 years. The BRFSS survey monitors health conditions and related behaviors, and is conducted annually by state and territorial health departments, with technical assistance from the U.S. Centers for Disease Control and Prevention. The multistage, stratified sampling strategy yields a representative sample of noninstitutionalized adults in all 50 states, the District of Columbia (D.C.), and selected U.S. territories. BRFSS data collection protocols are reviewed by the U.S. Center for Disease Control and Prevention’s Institutional Review Board (Protocol Number 2988) and the Office of Management and Budget (OMB No. 0920–1061 Exp. Date 3/31/2021). Secondary analyses of BRFSS data are not subject to Institutional Review Board approval because data are de-identified. Each year, BRFSS includes a core module of questions used by all states and territories and optional modules implemented by a subset of states. In 2017, an optional module containing SSB intake questions was used by D.C. and 12 states (Alaska, Arizona, Arkansas, Delaware, Hawaii, Iowa, New York, North Carolina, Ohio, Vermont, West Virginia, and Wisconsin); however, the small sample size for pregnant women precludes the provision of state-specific estimates. Using combined landline and cell phone data, these states had a median response rate of 43.0% (range: 32.9%–54.0%) (CDC, 2017). The analysis was restricted to women of reproductive age, defined as 18–49 years (n=14,356). Respondents who were missing data on pregnancy status (n=364, 2.5%) or SSB intake (n=2,279, 15.9%) were excluded from the analysis, leaving an analytic sample of 11,713 women, 11,321 of whom were non-pregnant and 392 of whom were pregnant. Compared to respondents who were excluded due to missing data, those retained in the analytic sample were older and more likely to be non-Hispanic white. No differences were found in education or marital status.
Measures
The outcome variable in this analysis was frequency of daily SSB intake. The 2017 BRFSS optional module included two food frequency questionnaire (FFQ)-style screener questions that measured SSB intake: 1) “During the past 30 days, how often did you drink regular soda or pop that contains sugar? Do not include diet soda or diet pop.” and 2) “During the past 30 days, how often did you drink sugar-sweetened fruit drinks (such as Kool-aid and lemonade), sweet tea, and sports or energy drinks (such as Gatorade and Red Bull)? Do not include 100% fruit juice, diet drinks, or artificially sweetened drinks.” SSB intake was reported as the number of times per day, week, or month, and these data were converted to daily intake for both questions and then summed to calculate total daily SSB intake. The outcome of daily SSB intake was then categorized as <1 time/day and ≥1 time/day (Lundeen, Park, Pan, & Blanck, 2018; Park, Xu, Town, & Blanck, 2016).
We examined the association between frequency of daily SSB intake and selected sociodemographic and behavioral characteristics. Sociodemographic characteristics included age (18–29 years, 30–49 years), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic other), highest level of education completed (≤high school graduate, some college, ≥college graduate), marital status (married/domestic partnership, not married [including widowed]), and metropolitan status (metropolitan/nonmetropolitan). U.S counties were categorized as: metropolitan (large central metro, large fringe metro, medium metro, and small metro) and nonmetropolitan (micropolitan and noncore). The nonmetropolitan designation is used to classify counties with small populations (<50,000) (Ingram & Franco, 2014). Behavioral characteristics included leisure-time physical activity (had physical activity/exercise, no physical activity/exercise) in the past 30 days, smoking status (nonsmoker, former smoker, current smoker), and daily fruit and vegetable intake (<5 times/day, ≥5 times/day). A nonsmoker was defined as someone who has never smoked or smoked less than one hundred cigarettes in their life; a former smoker was defined as someone who has smoked at least one hundred cigarettes in their entire life but does not currently smoke cigarettes; a current smoker was defined as someone who has smoked at least one hundred cigarettes in their entire life and currently smokes every day or some days. Fruit and vegetable intake was calculated based on six FFQ-style screener questions that measured intake of fruits, 100% fruit juice, dark green vegetables, fried and non-fried potatoes, and other vegetables. Similar to SSBs, intake was converted to daily intake for all questions and then summed to calculate total daily fruit and vegetable intake. Respondents also self-reported their pregnancy status (currently pregnant or not currently pregnant), and this was used as a stratification variable in the analyses.
Statistical Analysis
Frequency of daily SSB intake is presented overall and by sociodemographic and behavioral characteristics. All analyses were stratified by pregnancy status. Chi-square tests were used to examine whether SSB intake varied within sociodemographic and behavioral characteristics (significant at p<0.05). Multivariable logistic regression was used to estimate adjusted odds ratios (aOR) and 95% confidence intervals (CI) for SSB intake ≥1 time/day (reference: <1 time/day), with all characteristics included in the model (i.e. age, race/ethnicity, education, marital status, metropolitan status, fruit and vegetable intake, physical activity, and smoking status). Analyses were performed using SAS-callable SUDAAN (version 9.3), and accounted for complex survey design variables (strata and primary sampling units) and sampling weights.
Results
A description of the sociodemographic and behavioral characteristics of pregnant and non-pregnant women of reproductive age in this study is shown in Table 1. Compared to non-pregnant women, a higher proportion of pregnant women were 18–29 years (51.1% vs. 36.2%; p<0.01), married (58.3% vs. 44.8%; p=0.01), nonsmokers (72.0% vs. 67.8%; p<0.01), and had ≤high school education (49.7% vs. 36.3%; p=0.03). A higher proportion of non-pregnant women, compared to pregnant women, had some leisure-time physical activity in the past 30 days (75.5% vs. 62.4%; p=0.02).
Table 1.
Characteristics of women of reproductive age (18–49 years), 12 states and District of Columbia, Behavioral Risk Factor Surveillance System, 2017
| Characteristic | All women %a | Women of reproductive age, by pregnancy status %a (95% confidence interval) |
p-valueb | |
|---|---|---|---|---|
| Non-pregnant women (n=11,321) | Pregnant women (n=392) | |||
|
| ||||
| Age (n=11,713) | ||||
| 18–29 years | 36.8 | 36.2 (34.4, 38.0) | 51.1 (41.5, 60.6) | <0.01 |
| 30–49 years | 63.2 | 63.8 (62.0, 65.6) | 48.9 (39.4, 58.5) | |
| Race/ethnicity (n=11,557) | ||||
| White, non-Hispanic | 61.6 | 62.1 (60.4, 63.8) | 51.3 (41.6, 61.0) | 0.21 |
| Black, non-Hispanic | 14.1 | 13.8 (12.5, 15.2) | 20.2 (12.1, 31.9) | |
| Hispanic | 14.0 | 13.8 (12.7, 15.0) | 18.1 (12.3, 26.0) | |
| Other, non-Hispanic | 10.3 | 10.3 (9.2, 11.5) | 10.3 (6.1, 16.8) | |
| Education (n=11,693) | ||||
| ≤High school | 36.9 | 36.3 (34.6, 38.1) | 49.7 (40.2, 59.3) | 0.03 |
| Some college | 33.0 | 33.2 (31.6, 34.9) | 27.8 (19.7, 37.8) | |
| ≥College graduate | 30.1 | 30.4 (29.0, 31.9) | 22.4 (16.6, 29.6) | |
| Marital status (n=11,666) | ||||
| Married/domestic partnership | 45.4 | 44.8 (43.1, 46.5) | 58.3 (48.7, 67.3) | 0.01 |
| Not marriedc | 54.6 | 55.2 (53.5, 56.9) | 41.7 (32.7, 51.3) | |
| Metropolitan status (n=11,713) | ||||
| Metropolitan | 82.1 | 82.1 (80.9, 83.2) | 83.8 (77.3, 88.7) | 0.56 |
| Nonmetropolitan | 17.9 | 17.9 (16.8, 19.1) | 16.2 (11.3, 22.7) | |
| Fruit and vegetable intake (n=11,284) | ||||
| <5 times/day | 79.1 | 79.4 (77.9, 80.8) | 71.0 (61.2, 79.1) | 0.08 |
| ≥5 times/day | 20.9 | 20.6 (19.2, 22.1) | 29.0 (20.9, 38.8) | |
| Leisure-time physical activityd (n=11,702) | ||||
| Had physical activity/exercise | 75.0 | 75.5 (74.0, 77.0) | 62.4 (52.2, 71.7) | 0.02 |
| No physical activity/exercise | 25.0 | 24.5 (23.0, 26.0) | 37.6 (28.3, 47.8) | |
| Smoking status (n=11,665) | ||||
| Nonsmoker | 68.0 | 67.8 (66.2, 69.3) | 72.0 (63.8, 79.0) | <0.01 |
| Former smoker | 15.3 | 15.0 (13.8, 16.2) | 22.2 (15.9, 30.2) | |
| Current smoker | 16.7 | 17.2 (16.0, 18.5) | 5.7 (3.4, 9.6) | |
Weighted percentages may not add to 100% because of rounding.
χ2 tests were used for each variable to examine differences by pregnancy status.
Single, widowed, divorced, separated, or never married.
Leisure-time physical activity was categorized as 1) participating in any or 2) not participating any physical activity or exercise during the past 30 days other than their regular job.
Overall, 27.3% of non-pregnant women reported consuming SSBs ≥1 time/day (Table 2); 12.6% of non-pregnant women consumed SSBs ≥2 times/day (data not shown). In unadjusted analyses of non-pregnant women, the prevalence of daily SSB intake differed by race/ethnicity (p=0.0001), education (p=0.0000), marital status (p=0.0000), metropolitan status (p=0.0002), leisure-time physical activity/exercise (p=0.0000), and smoking status (p=0.0000; χ2 tests). Age and fruit and vegetable intake were not significantly associated with daily SSB intake in unadjusted analyses of nonpregnant women. Within sociodemographic and behavioral characteristics where there was a significant difference in SSB intake across groups, the proportion of non-pregnant women with SSB intake ≥1 time/day was highest among non-Hispanic Black women (38.3%), unmarried women (31.0%), those who lived in nonmetropolitan counties (32.8%), current smokers (52.6%), those with ≤high school education (38.7%), and those with no physical activity/exercise in the past 30 days (39.1%). In adjusted analyses among non-pregnant women, odds of consuming SSBs ≥1 time/day were higher for women who were non-Hispanic black (aOR=2.04, 95% CI=1.55–2.69) compared to non-Hispanic white; had ≤high school education (aOR=2.79, CI=2.26–3.44) or some college (aOR=1.85, CI=1.50–2.27) vs. college graduates; lived in nonmetropolitan counties (aOR=1.35, CI=1.11–1.63) vs. metropolitan counties; had no physical activity/exercise (aOR=1.72, CI=1.43–2.07) vs. some; were former (aOR=1.51, CI=1.17–1.94) or current (aOR=3.48, CI=2.82–4.28) smokers vs nonsmokers.
Table 2.
Factors associated with sugar-sweetened beverage (SSB)a intake among non-pregnant women of reproductive age, 12 states and District of Columbia, Behavioral Risk Factor Surveillance System, 2017
| Characteristic | Bivariate analysisb SSB intake |
Multivariable logistic regression analysisc SSB intake ≥1 time/day |
||||
|---|---|---|---|---|---|---|
| <1 time/day |
≥1 time/day |
p-valued | ||||
| n | % (95% CI) | n | % (95% CI) | aOR (95% CI) | ||
|
| ||||||
| All non-pregnant women (n=11,321) | 8315 | 72.7 (71.2, 74.2) | 3006 | 27.3 (25.8, 28.8) | - | - |
| Age (n=11,321) | ||||||
| 18–29 years | 2027 | 71.6 (68.7, 74.4) | 866 | 28.4 (25.6, 31.3) | 0.3261 | 1.07 (0.88–1.30) |
| 30–49 years | 6288 | 73.3 (71.5, 75.0) | 2140 | 26.7 (25.0, 28.5) | 1.00 [Reference] | |
| Race/ethnicity (n=11,174) | ||||||
| White, non-Hispanic | 5157 | 74.9 (73.1, 76.6) | 1703 | 25.1 (23.4, 26.9) | 0.0001 | 1.00 [Reference] |
| Black, non-Hispanic | 870 | 61.7 (56.5, 66.7) | 488 | 38.3 (33.3, 43.5) | 2.04 (1.55–2.69) | |
| Hispanic | 991 | 73.1 (68.8, 77.0) | 368 | 26.9 (23.0, 31.2) | 1.10 (0.85–1.42) | |
| Other, non-Hispanic | 1186 | 73.2 (67.4, 78.3) | 411 | 26.8 (21.7, 32.6) | 1.20 (0.85–1.70) | |
| Education (n=11,303) | ||||||
| ≤High school graduate | 1990 | 61.3 (58.2, 64.3) | 1327 | 38.7 (35.7, 41.8) | 0.0000 | 2.79 (2.26–3.44) |
| Some college | 2275 | 72.5 (69.8, 75.1) | 951 | 27.5 (24.9, 30.2) | 1.85 (1.50–2.27) | |
| ≥College graduate | 4037 | 86.5 (84.8, 88.0) | 723 | 13.5 (12.0, 15.2) | 1.00 [Reference] | |
| Marital status (n=11,276) | ||||||
| Married/domestic partnership | 4308 | 77.2 (75.1, 79.2) | 1172 | 22.8 (20.8, 24.9) | 0.0000 | 1.00 [Reference] |
| Not marriede | 3969 | 69.0 (66.7, 71.1) | 1827 | 31.0 (28.9, 33.3) | 1.15 (0.96–1.39) | |
| Metropolitan status (n=11,321) | ||||||
| Metropolitan | 6072 | 73.9 (72.1, 75.6) | 2061 | 26.1 (24.4, 27.9) | 0.0002 | 1.00 [Reference] |
| Nonmetropolitan | 2243 | 67.2 (64.1, 70.2) | 945 | 32.8 (29.8, 35.9) | 1.35 (1.11–1.63) | |
| Fruit and vegetable intake (n=10,907) | ||||||
| <5 times/day | 6241 | 72.6 (70.8, 74.3) | 2306 | 27.4 (25.7, 29.2) | 0.3668 | 0.91 (0.73–1.13) |
| ≥5 times/day | 1814 | 74.4 (70.7, 77.8) | 546 | 25.6 (22.2, 29.3) | 1.00 [Reference] | |
| Leisure-time physical activityf (n=11,310) | ||||||
| Had physical activity/exercise | 6687 | 76.5 (74.8, 78.2) | 1933 | 23.5 (21.8, 25.2) | 0.0000 | 1.00 [Reference] |
| No physical activity/exercise | 1620 | 60.9 (57.5, 64.2) | 1070 | 39.1 (35.8, 42.5) | 1.72 (1.43–2.07) | |
| Smoking status (n=11,276) | ||||||
| Nonsmoker | 5830 | 78.9 (77.1, 80.6) | 1591 | 21.1 (19.4, 22.9) | 0.0000 | 1.00 [Reference] |
| Former smoker | 1418 | 73.9 (69.7, 77.7) | 413 | 26.1 (22.3, 30.3) | 1.51 (1.17–1.94) | |
| Current smoker | 1034 | 47.4 (43.5, 51.3) | 990 | 52.6 (48.7, 56.5) | 3.48 (2.82–4.28) | |
Abbreviations: sugar-sweetened beverage (SSB), confidence interval (CI), adjusted odds ratio (aOR).
Included non-diet soda, fruit drinks that are not 100% juice, sweet tea, sports drinks, and energy drinks.
Unweighted sample size and weighted percentage. Weighted percentages may not add to 100 because of rounding.
Multivariable logistic regression was performed to estimate adjusted odds ratios for SSB intake ≥1 time/day (reference: <1 time/day), with all characteristics included in the model (n=10,688). Bold indicates significance.
χ2 tests were used for each variable to examine differences by SSB intake categories.
Single, widowed, divorced, separated, or never married.
Leisure-time physical activity was categorized as 1) participating in any or 2) not participating any physical activity or exercise during the past 30 days other than their regular job.
Overall, 21.9% of pregnant women reported consuming SSBs ≥1 time/day (Table 3); 9.7% of pregnant women consumed SSBs ≥2 times/day (data not shown). In unadjusted analyses of pregnant women, the prevalence of daily SSB intake differed by education (p=0.0022), marital status (p=0.0040), and leisure-time physical activity/exercise (p=0.0319; χ2 tests). Within these characteristics, the proportion of pregnant women with SSB intake ≥1 time/day was highest among those with ≤high school education (29.2%), unmarried women (35.1%), and those with no physical activity/exercise in the past 30 days (33.3%). Age, race/ethnicity, metropolitan status, fruit and vegetable intake, and smoking status were not significantly associated with daily SSB intake in unadjusted analyses of pregnant women. In adjusted analyses among pregnant women, only marital status was significantly associated with odds of SSB intake ≥1 time/day. Pregnant women who were not married had higher odds for daily SSB intake (aOR=2.81, CI=1.05–7.51) than married women.
Table 3.
Factors associated with sugar-sweetened beverage (SSB)a intake among pregnant women of reproductive age, 12 states and District of Columbia, Behavioral Risk Factor Surveillance System, 2017
| Characteristic | Bivariate analysisb SSB intake |
Multivariable logistic regression analysisc SSB intake ≥1 time/day |
||||
|---|---|---|---|---|---|---|
| <1 time/day |
≥1 time/day |
p-valued |
||||
| n | % (95% CI) | n | % (95% CI) | aOR (95% CI) | ||
|
| ||||||
| All pregnant women (n=392) | 297 | 78.1 (70.1, 84.4) | 95 | 21.9 (15.6, 29.9) | - | - |
| Age (n=392) | ||||||
| 18–29 years | 117 | 73.0 (61.1, 82.3) | 56 | 27.0 (17.7, 38.9) | 0.1491 | 1.16 (0.34–3.96) |
| 30–49 years | 180 | 83.5 (72.0, 90.8) | 39 | 16.5 (9.2, 28.0) | 1.00 [Reference] | |
| Race/ethnicity (n=383) | ||||||
| White, non-Hispanic | 167 | 85.3 (77.2, 90.8) | 46 | 14.7 (9.2, 22.8) | 0.2252 | 1.00 [Reference] |
| Black, non-Hispanic | 27 | 71.7 (46.3, 88.2) | 17 | 28.3 (11.8, 53.7) | 2.15 (0.46–10.10) | |
| Hispanic | 51 | 66.9 (44.4, 83.7) | 13 | 33.1 (16.3, 55.6) | 3.32 (0.87–12.60) | |
| Other, non-Hispanic | 43 | 72.5 (49.3, 87.7) | 19 | 27.5 (12.3, 50.7) | 1.19 (0.32–4.44) | |
| Education (n=390) | ||||||
| ≤High school | 80 | 70.8 (57.1, 81.5) | 47 | 29.2 (18.5, 42.9) | 0.0022 | 3.13 (0.84–11.66) |
| Some college | 78 | 78.2 (63.8, 87.9) | 32 | 21.8 (12.1, 36.2) | 1.80 (0.60–5.44) | |
| ≥College graduate | 137 | 94.1 (87.2, 97.4) | 16 | 5.9 (2.6, 12.8) | 1.00 [Reference] | |
| Marital status (n=390) | ||||||
| Married/domestic partnership | 197 | 87.5 (79.3, 92.8) | 45 | 12.5 (7.2, 20.7) | 0.0040 | 1.00 [Reference] |
| Not marriede | 98 | 64.9 (50.9, 76.7) | 50 | 35.1 (23.3, 49.1) | 2.81 (1.05–7.51) | |
| Metropolitan status (n=392) | ||||||
| Metropolitan | 217 | 79.2 (70.0, 86.2) | 60 | 20.8 (13.8, 30.0) | 0.3567 | 1.00 [Reference] |
| Nonmetropolitan | 80 | 72.2 (57.2, 83.4) | 35 | 27.8 (16.6, 42.8) | 2.24 (0.92–5.48) | |
| Fruit and vegetable intake (n=377) | ||||||
| <5 times/day | 196 | 76.3 (66.2, 84.1) | 66 | 23.7 (15.9, 33.8) | 0.1567 | 1.61 (0.56–4.58) |
| ≥5 times/day | 93 | 86.9 (71.6, 94.6) | 22 | 13.1 (5.4, 28.4) | 1.00 [Reference] | |
| Leisure-time physical activityf (n=392) | ||||||
| Had physical activity/exercise | 221 | 85.0 (77.5, 90.2) | 57 | 15.0 (9.8, 22.5) | 0.0319 | 1.00 [Reference] |
| No physical activity/exercise | 76 | 66.7 (49.9, 80.1) | 38 | 33.3 (19.9, 50.1) | 1.87 (0.73–4.81) | |
| Smoking status (n=389) | ||||||
| Nonsmoker | 213 | 81.5 (71.4, 88.6) | 54 | 18.5 (11.4, 28.6) | 0.0911 | 1.00 [Reference] |
| Former smoker | 64 | 72.8 (56.3, 84.7) | 24 | 27.2 (15.3, 43.7) | 2.80 (0.88–8.97) | |
| Current smoker | 17 | 54.6 (30.5, 76.7) | 17 | 45.4 (23.3, 69.5) | 4.38 (0.99–19.28) | |
Abbreviations: sugar-sweetened beverage (SSB), confidence interval (CI), adjusted odds ratio (aOR).
Included non-diet soda, fruit drinks that are not 100% juice, sweet tea, sports drinks, and energy drinks.
Unweighted sample size and weighted percentage. Weighted percentages may not add to 100 because of rounding.
Multivariable logistic regression was performed to estimate adjusted odds ratios for SSB intake ≥1 time/day (reference: <1 time/day), with all characteristics included in the model (n=366). Bold indicates significance.
χ2 tests were used for each variable to examine differences by SSB intake categories.
Single, widowed, divorced, separated, or never married.
Leisure-time physical activity was categorized as 1) participating in any or 2) not participating any physical activity or exercise during the past 30 days other than their regular job.
Discussion
We found that among women of reproductive age in 12 states and D.C., one in four non-pregnant women and one in five pregnant women consumed SSBs at least once per day. Sociodemographic and behavioral characteristics associated with daily SSB intake were identified for non-pregnant and pregnant women. Among non-pregnant women, characteristics associated with daily SSB intake in the unadjusted analyses included race/ethnicity, education, marital status, metropolitan status, physical activity, and smoking status; with the exception of marital status, all of these characteristics were also predictive in the adjusted analysis. Among non-pregnant women, sociodemographic factors associated with higher odds of daily SSB intake in the adjusted analysis included being non-Hispanic black, having less than a college education, and living in nonmetropolitan counties. Behavioral characteristics that were significant in the adjusted model included being a former or current smoker and having no physical activity/exercise in the past month. A previous examination of pregravid women in the Nurses Health Study II found that 31.3% of women consumed ≥5 servings/week of SSBs, and that this higher quantity of SSB intake was associated with younger age, current smoking, fewer hours of physical activity per week, and consumption of less fruits and vegetables (Chen et al., 2009). Additionally, more recent studies of adults in the U.S.—both female and male—have resulted in similar findings of higher odds of daily SSB intake among non-Hispanic black adults, those with less than a college education, nonmetropolitan county residents, current smokers, and those who are physically inactive (Lundeen et al., 2018; Park, Pan, Sherry, & Blanck, 2014).
We found that in unadjusted analyses of pregnant women, frequency of SSB intake significantly differed by education, marital status, and leisure-time physical activity/exercise. In the adjusted analysis, marital status was the only factor that was significantly associated with daily SSB intake. In the present study, among pregnant women, those who were not married had 2.8 times higher odds for consuming SSBs at least once per day than married women. Although the magnitude of other odds ratios was similar to that for non-pregnant women, the few significant results could have been the result of a relatively small sample size for pregnant women that limited statistical power. A prospective pre-birth cohort study in the U.S. called Project Viva published a similar finding that around one in five pregnant women are daily SSB consumers. This study showed that 19.8% of women in the second trimester of pregnancy consume ≥1 serving/day of SSBs, and that correlates of higher SSB intake during pregnancy include younger maternal age, nonwhite race/ethnicity, smoking during pregnancy, lower education and household income, and higher pre-pregnancy body mass index (Gillman et al., 2017; Wright, Rifas-Shiman, Oken, Litonjua, & Gold, 2018).
Efforts to promote maintenance of a healthy weight among all women of reproductive age can help more women begin pregnancy at a healthy weight and potentially reduce the risk of these adverse outcomes. One public health strategy may be working with physicians, dieticians, and other healthcare providers who can provide counseling to women of reproductive age about the role of limiting SSB intake in achieving a healthy pre-pregnancy weight and appropriate weight gain during pregnancy. Currently, 53.3% of births in the U.S. are to women with pre-pregnancy overweight or obesity (body mass index ≥25 kg/m2) (Martin, Hamilton, Osterman, Driscoll, & Drake, 2018). Additionally, among women with full-term, singleton births in the U.S., 32% had gestational weight gain within the recommended range and 48% gained more weight than the Institute of Medicine Recommendations (CDC, 2016).
Reducing SSB intake may be an important strategy for promoting healthy pre-pregnancy weight and preventing excessive weight gain during pregnancy, thereby reducing the risk of adverse birth outcomes. Pregnancy is a critical time when it is particularly important that caloric intake be rich in healthful nutrients rather than the nutrient-poor calories provided by added sugars. Most healthy, normal weight pregnant women require no additional calories during the first trimester, an additional 340 calories during the second trimester, and 450 additional calories during the third trimester to support the metabolic demands of pregnancy (IOM, 2005). Pregnant women may reduce the risks of excessive weight gain and adverse outcomes by getting adequate physical activity and having a balanced diet that is high in whole grains, fruits, vegetables, low-fat dairy, and lean protein, and that limits added sugars and saturated fats (CDC, 2019; USDA, 2019).
Frequent intake of SSBs, both before and during pregnancy, is associated with several adverse health outcomes. An examination of thousands of women prior to pregnancy in the Nurses Health Study II found that higher intake of sugar-sweetened cola (≥5 servings/week) was associated with an increased risk of gestational diabetes mellitus, even after controlling for pre-pregnancy body mass index (BMI) (Chen et al., 2009). During pregnancy, frequent intake of SSBs is associated with an increased risk of preeclampsia and preterm delivery, even when adjusting for pre-pregnancy BMI (Borgen et al., 2012; Englund-Ogge et al., 2012; Petherick, Goran, & Wright, 2014). Furthermore, maternal SSB intake during pregnancy is positively associated with the offspring’s BMI and fat mass in early- and mid-childhood, independent of the child’s SSB intake (Gillman et al., 2017; Jen et al., 2017); higher maternal pregnancy SSB intake has also been linked to increased odds of the offspring experiencing asthma in mid-childhood, independent of maternal pre-pregnancy BMI (Wright et al., 2018), and maternal SSB intake has been shown to be inversely associated with offspring cognitive scores at mid-childhood (Cohen, Rifas-Shiman, Young, & Oken, 2018).
Some evidence suggests that attitudes toward SSB intake may be an important lever to influence intake behaviors. A previous study surveyed families participating in the Special Supplemental Nutrition Program for Women, Infants and Children, including both pregnant women and male and female parents of children under 2 years (Woo-Baidal et al., 2018). Parents were asked to rate the extent to which they agreed or disagreed with statements such as “It is okay to drink sugary drinks while pregnant” and “Drinking sugary drinks increases the risk of gaining too much weight.” The researchers found that pregnant women and parents who had more negative attitudes toward SSB intake consumed fewer SSB calories (Woo-Baidal et al., 2018). During in-depth interviews, women showed motivation to change beverage consumption patterns during pregnancy, stating a strong desire to promote infant health (Morel et al., 2019).
To our knowledge, the present study is one of only two U.S. studies to examine SSB intake in pregnant women using population-based survey data collected from multiple states throughout the U.S. The data on sociodemographic characteristics and health-related behaviors in BRFSS allowed us to determine risk factors for daily SSB intake among pregnant and nonpregnant women of reproductive age, thereby identifying women who may be at risk for higher SSB intake before and during pregnancy. However, the present study is subject to several limitations. SSB intake data in BRFSS are self-reported, and can potentially be influenced by recall or social desirability bias (Gibson, 2005), although the degree of this potential bias is unknown. The findings in this report might not be generalizable to the entire U.S. population of women of reproductive age, as the analysis included only 12 states and D.C., which used the optional SSB module in 2017. Furthermore, this analysis included only four of the ten U.S. states with the highest prevalence of adult obesity and over sixty percent of the sample was non-Hispanic white, and thus the findings may not represent the dietary intake of racial and ethnic groups with the highest obesity prevalence (CDC, 2018). The small sample size for pregnant women in this analysis may have limited the statistical power to detect associations. However, given the relatively small proportion of the population of women in the U.S. who experience pregnancy each year, national surveys that assess dietary intake are limited by a small sample size for pregnant women, if they do not oversample pregnant women or combine data across multiple years. The present study cannot estimate the amount or calorie intake from SSBs, because SSB intake was captured in frequency rather than volume. Information on trimester of pregnancy was not available for pregnant women, limiting comparisons to other studies of SSB intake in pregnant women. Finally, the measurement of SSB intake used in this study did not capture consumption of sweetened coffee drinks.
Conclusions
Daily intake of SSBs is common among both non-pregnant and pregnant women of reproductive age. Information on the correlates of daily SSB intake among women of reproductive age can be used by a variety of public health and healthcare professionals to identify women who may be at risk for higher SSB intake before and during pregnancy. This information can be used to tailor interventions to promote healthy pre-pregnancy weight and gestational weight gain.
Figure 1.
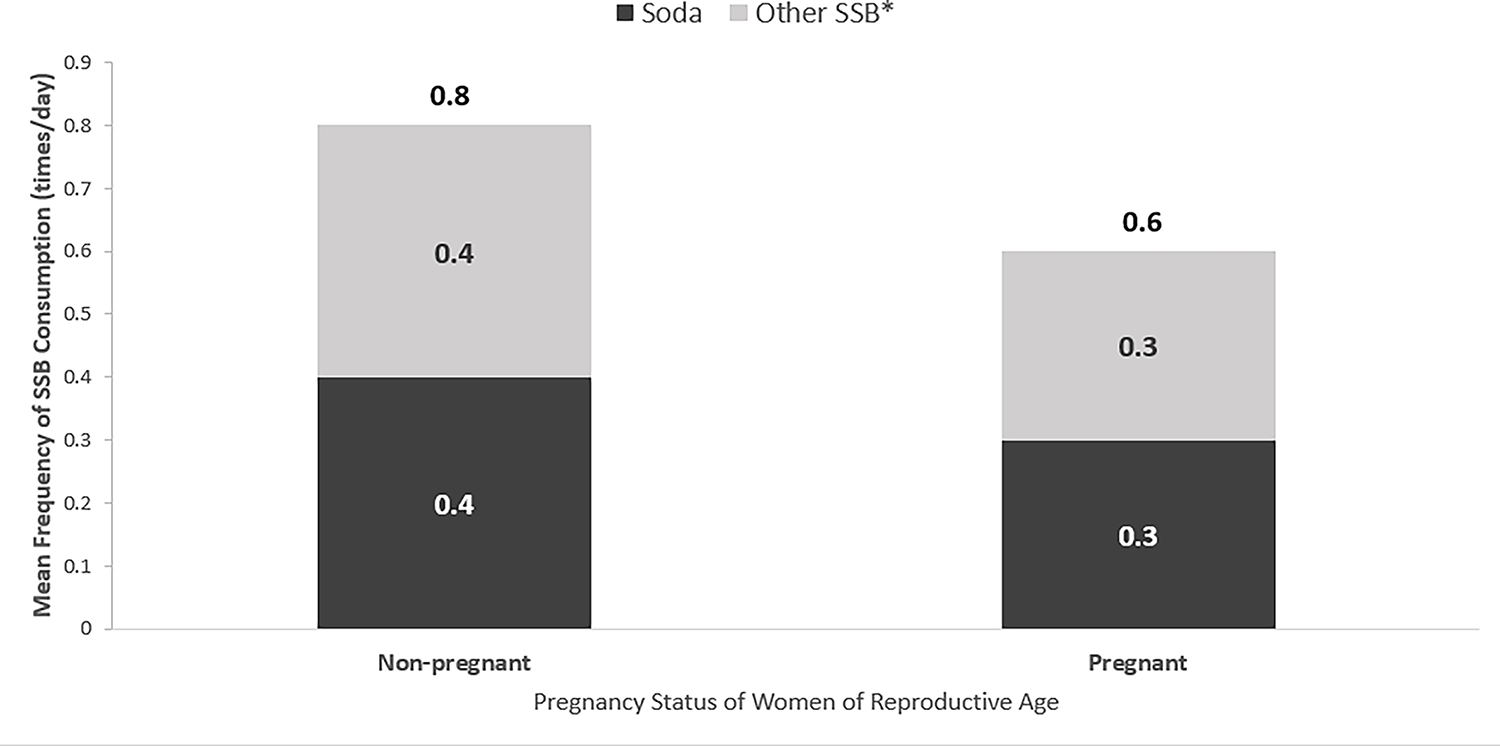
Mean frequency (times/day) of total sugar-sweetened beverage (SSB) consumption and the contribution of each beverage type: soda and other SSB (*fruit drinks, sweet tea, sports drinks, energy drinks). Data presented are from non-pregnant (n=11,321) and pregnant women (n=392) who participated in the 2017 U.S. Behavioral Risk Factor Surveillance System.
Significance.
What is already known on this subject?
Frequent sugar-sweetened beverage (SSB) intake is associated with weight gain, obesity, type 2 diabetes, and cardiovascular disease. Pre-pregnancy overweight and obesity and excessive gestational weight gain are linked to adverse maternal and infant health outcomes.
What this study adds?
Among women of reproductive age (WRA), one in four non-pregnant women and one in five pregnant women consumed SSBs at least once per day. Sociodemographic and behavioral correlates of daily SSB intake were identified for non-pregnant and pregnant women. Information on SSB intake and correlates of daily intake among WRA can aid in designing interventions to promote healthy weight and appropriate gestational weight gain.
Acknowledgements:
The authors would like to acknowledge Suzianne Garner for her assistance with the optional module and state BRFSS staff for data collection. There is no funding to disclose.
Footnotes
Conflicts of Interest: The authors declare that they have no conflict of interest.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Elizabeth A. Lundeen, Division of Nutrition, Physical Activity and Obesity (DNPAO), National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP), Centers for Disease Control and Prevention (CDC); Address: 4770 Buford Highway NE, Mail Stop F77, Atlanta, GA 30341..
Sohyun Park, DNPAO, NCCDPHP, CDC.
Jennifer A. Woo Baidal, Division of Pediatric Gastroenterology, Hepatology, and Nutrition, Department of Pediatrics, Columbia University Medical Center; Address: 622 W. 168th Street, PH-17, New York, NY 10032..
Andrea J. Sharma, DNPAO, NCCDPHP, CDC, and a Commander in the U.S. Public Health Service Commissioned Corps..
Heidi M. Blanck, DNPAO, NCCDPHP, CDC, and a Captain in the U.S. Public Health Service Commissioned Corps..
References
- Baeten JM, Bukusi EA, & Lambe M (2001). Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health, 91(3), 436–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgen I, Aamodt G, Harsem N, Haugen M, Meltzer H, & Brantsæter A (2012). Maternal sugar consumption and risk of preeclampsia in nulliparous Norwegian women. Eur J Clin Nutr, 66(8), 920–925. [DOI] [PubMed] [Google Scholar]
- CDC. (2016). QuickStats: Gestational Weight Gain Among Women with Full-Term, Singleton Births, Compared with Recommendations — 48 States and the District of Columbia, 2015. MMWR Morb Mortal Wkly Rep, 65, 1121. doi: 10.15585/mmwr.mm6540a10 [DOI] [PubMed] [Google Scholar]
- CDC. (2017). Centers for Disease Control and Prevention. The Behavioral Risk Factor Surveillance System 2017 Summary Data Quality Report. Accessed January 28, 2019 at: https://www.cdc.gov/brfss/annual_data/2017/pdf/2017-sdqr-508.pdf
- CDC. (2018). Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion, Division of Nutrition, Physical Activity, and Obesity. Data, Trends and Maps [online]. Accessed Mar 11, 2019 at : https://www.cdc.gov/nccdphp/dnpao/data-trends-maps/index.html. [Google Scholar]
- CDC. (2019). U.S. Centers for Disease Control and Prevention. Weight Gain During Pregnancy. Accessed January 28, 2019 at: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-weight-gain.htm. [Google Scholar]
- Chen L, Hu FB, Yeung E, Willett W, & Zhang C (2009). Prospective study of pre-gravid sugar-sweetened beverage consumption and the risk of gestational diabetes mellitus. Diabetes Care, 32(12), 2236–2241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cioffi CE, Figueroa J, & Welsh JA (2018). Added Sugar Intake among Pregnant Women in the United States: National Health and Nutrition Examination Survey 2003–2012. J Acad Nutr Diet, 118(5), 886–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JF, Rifas-Shiman SL, Young J, & Oken E (2018). Associations of Prenatal and Child Sugar Intake With Child Cognition. Am J Prev Med, 54(6), 727–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhingra R, Sullivan L, Jacques PF, Wang TJ, Fox CS, Meigs JB, . . . Vasan RS. (2007). Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation, 116(5), 480–488. [DOI] [PubMed] [Google Scholar]
- Drehmer M, Duncan BB, Kac G, & Schmidt MI (2013). Association of second and third trimester weight gain in pregnancy with maternal and fetal outcomes. PLoS One, 8(1), e54704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A, & Rehm CD (2014). Consumption of added sugars among US children and adults by food purchase location and food source. Am J Clin Nutr, 100(3), 901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englund-Ogge L, Brantsæter AL, Haugen M, Sengpiel V, Khatibi A, Myhre R, . . . Jacobsson B. (2012). Association between intake of artificially sweetened and sugar-sweetened beverages and preterm delivery: a large prospective cohort study. Am J Clin Nutr, 96(3), 552–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson RS (2005). Measurement Errors in Dietary Assessment. In Principles of Nutritional Assessment (Vol. Second Edition, pp. 105–128). New York, New York: Oxford University Press. [Google Scholar]
- Gillman MW, Rifas-Shiman SL, Fernandez-Barres S, Kleinman K, Taveras EM, & Oken E (2017). Beverage Intake During Pregnancy and Childhood Adiposity. Pediatrics, 140(2), e20170031. doi: 10.1542/peds.2017-0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutcheon JA, Stephansson O, Cnattingius S, Bodnar LM, Wikström A-K, & Johansson K (2018). Pregnancy Weight Gain Before Diagnosis and Risk of Preeclampsia: A Population-Based Cohort Study in Nulliparous Women. Hypertension, 72(2), 433–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram DD, & Franco SJ (2014). 2013 NCHS urban–rural classification scheme for counties. National Center for Health Statistics. Vital Health Stat, 2(166). [PubMed] [Google Scholar]
- IOM. (2005). Institute of Medicine. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC: The National Academies Press. 10.17226/10490. [DOI] [Google Scholar]
- Jen V, Erler NS, Tielemans MJ, Braun KV, Jaddoe VW, Franco OH, & Voortman T (2017). Mothers’ intake of sugar-containing beverages during pregnancy and body composition of their children during childhood: the Generation R Study. Am J Clin Nutr, 105(4), 834–841. [DOI] [PubMed] [Google Scholar]
- Li N, Liu E, Guo J, Pan L, Li B, Wang P, . . . Hu G. (2013). Maternal prepregnancy body mass index and gestational weight gain on pregnancy outcomes. PLoS One, 8(12), e82310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundeen EA, Park S, Pan L, & Blanck HM (2018). Daily Intake of Sugar-Sweetened Beverages Among US Adults in 9 States, by State and Sociodemographic and Behavioral Characteristics, 2016. Prev Chronic Dis, 15, E154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magann EF, Doherty DA, Sandlin AT, Chauhan SP, & Morrison JC (2013). The effects of an increasing gradient of maternal obesity on pregnancy outcomes. Aust N Z J Obstet Gynaecol, 53(3), 250–257. [DOI] [PubMed] [Google Scholar]
- Malik AH, Akram Y, Shetty S, Malik SS, & Njike VY (2014). Impact of sugar-sweetened beverages on blood pressure. Am J Cardiol, 113(9), 1574–1580. [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, & Drake P (2018). Births: Final Data for 2017. Natl Vital Stat Rep, 67(8), Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Morel K, Nichols K, Nong Y, Charles N, Price S, Taveras E, . . . Baidal JAW. (2019). Parental and Provider Perceptions of Sugar-Sweetened Beverage Interventions in the First 1,000 Days: A Qualitative Study. Acad Pediatr, S1876-2859(19)30007-5. doi: 10.1016/j.acap.2019.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S, Pan L, Sherry B, & Blanck HM (2014). Consumption of sugar-sweetened beverages among US adults in 6 states: Behavioral Risk Factor Surveillance System, 2011. Prev Chronic Dis, 11, E65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S, Xu F, Town M, & Blanck HM (2016). Prevalence of Sugar-Sweetened Beverage Intake Among Adults--23 States and the District of Columbia, 2013. MMWR Morb Mortal Wkly Rep, 65(7), 169–174. [DOI] [PubMed] [Google Scholar]
- Petherick E, Goran M, & Wright J (2014). Relationship between artificially sweetened and sugar-sweetened cola beverage consumption during pregnancy and preterm delivery in a multi-ethnic cohort: analysis of the Born in Bradford cohort study. Eur J Clin Nutr, 68(3), 404–407. [DOI] [PubMed] [Google Scholar]
- Rosinger A, Herrick K, Gahche J, & Park S (2017). Sugar-sweetened Beverage Consumption Among U.S. Adults, 2011–2014. NCHS data brief, no 270. Hyattsville, MD: National Center for Health Statistics. . [Google Scholar]
- Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, Willett WC, & Hu FB (2004). Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA, 292(8), 927–934. [DOI] [PubMed] [Google Scholar]
- Sebire N, Jolly M, Harris J, Wadsworth J, Joffe M, Beard R, . . . Robinson S. (2001). Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord, 25(8), 1175–1182. [DOI] [PubMed] [Google Scholar]
- Sharkey JR, Johnson CM, & Dean WR (2011). Less-healthy eating behaviors have a greater association with a high level of sugar-sweetened beverage consumption among rural adults than among urban adults. Food Nutr Res, 55, doi: 10.3402/fnr.v55i0.5819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDA. (2019). United States Department of Agriculture. Nutritional Needs During Pregnancy. Accessed January 28, 2019 at: https://www.choosemyplate.gov/nutritional-needs-during-pregnancy.
- Woo-Baidal JA, Morel K, Nichols K, Elbel E, Charles N, Goldsmith J, . . . Taveras E. (2018). Sugar-Sweetened Beverage Attitudes and Consumption During the First 1000 Days of Life. Am J Public Health, 108(12), 1659–1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright LS, Rifas-Shiman SL, Oken E, Litonjua AA, & Gold DR (2018). Prenatal and Early Life Fructose, Fructose-Containing Beverages, and Midchildhood Asthma. Ann Am Thorac Soc, 15(2), 217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]


