Abstract
Background:
Emergency Department (ED) visits are common among adults with intellectual and developmental disabilities (IDD). However, little is known about how ED use has varied over time in this population, or how it has been affected by recent Medicaid policy changes.
Objective:
To examine temporal trends in ED use among adult Medicaid members with IDD in eight states that ranged in the extent to which they had implemented state-level Medicaid policy changes that might affect ED use.
Methods:
We conducted repeated cross-sectional analyses of 2010–2016 Medicaid claims data. Quarterly analyses included adults ages 18–64 years with IDD (identified by diagnosis codes) who were continuously enrolled in Medicaid for the past 12 months. We assessed change in number of ED visits per 1000 member months from 2010 to 2016 overall and interacted with state level policy changes such as Medicaid expansion.
Results:
States with no Medicaid expansion experienced an increase in ED visits (linear trend coefficient: 1.13, p < 0.01), while states operating expansion via waiver had a much smaller (non-significant) increase, and states with ACA-governed expansion had a decrease in ED visits (linear trend coefficient: 1.17, p < 0.01). Other policy changes had limited or no association with ED visits.
Conclusions:
Medicaid expansion was associated with modest reduction or limited increase in ED visits compared to no expansion. We found no consistent decrease in ED visits in association with other Medicaid policy changes.
Keywords: Intellectual disability, Developmental disabilities, Emergency departments, Medicaid, Health policy
Individuals with intellectual and developmental disabilities (IDD) constituted 1–2% of the adult population of the United States in 2014.1 While the numbers of adults with IDD are small relative to the general population, their utilization of hospital-based health services — including emergency departments (EDs) — is high.2 High use of acute care services may be due in part to poorer health and greater complexity of health needs in the IDD population.3,4 However, recent research has found that nearly 20% of ED visits among adults with intellectual disabilities in South Carolina were for conditions for which timely outpatient care could potentially prevent the need for ED visits or inpatient hospitalization.5 Similarly, a study in a multi-state sample of adults with IDD found that many of the most common conditions for which adults with IDD visited EDs could potentially be managed through timely access to non-emergency care instead.6
Most adults with IDD rely on Medicaid for healthcare coverage.3 Medicaid programs in many states have implemented a variety of policy changes over the past several years intended to improve care coordination, access, and quality for Medicaid members as a whole, or for particular subgroups of Medicaid members. These changes include Medicaid expansion to provide coverage to previously ineligible people, transitions to managed care, and other delivery system reforms.7 Because substantial portions of ED visits among adults with IDD are potentially preventable,5,6 such policy changes could lead to lower ED use among adults with IDD. In fact, research in Illinois found a substantial decrease in ED visits among adult Medicaid members with IDD following the state’s transition to a managed care model.2 In other states, certain health care delivery policy changes such as implementation of Accountable Care Organizations and ED copayments have been associated with reductions in ED use in the general Medicaid population,8–10 but their impact on Medicaid members with IDD is unknown. Some research on ED use following Medicaid expansion has reported increased outpatient utilization in non-emergency settings and reduced ED use among low income adults.11 However, such changes may have been driven by a reduction in the proportion of the population that was uninsured rather than changes in the way health care was utilized by Medicaid members who were already enrolled prior to expansion. Indeed, multiple studies have found reductions in self-pay ED visits but an increase in ED visits covered by Medicaid following expansion.12–19 None of these Medicaid expansion studies have assessed impacts for adults with IDD. Therefore, the purpose of this study was to examine changes over time in ED visits among adult Medicaid members with IDD in eight states that ranged in the extent to which they had implemented state-level Medicaid policy changes that might affect ED use.
Methods
Study design
This study utilized a repeated cross-sectional design, analyzing data by quarter across the time period 2010–2016.
Data sources
Data were drawn from Medicaid claims in eight states participating in a larger project on healthcare utilization among individuals with IDD. These states were: Iowa, Kansas, Massachusetts, Michigan, Montana, New York, Oregon, and South Carolina. Analysts in each state obtained claims data from their state’s Medicaid agency. The study was reviewed and approved by the Medicaid agencies in each state. In some cases, the Institutional Review Board made a review and in other states this was not required.
Case definition of IDD
IDD is an umbrella term encompassing conditions (e.g., autism spectrum disorder, cerebral palsy, Down syndrome) that are typically present from birth and are expected to have long term impacts on physical, intellectual, and/or emotional development and functioning.20 We searched claims data for ICD-9-CM and ICD-10-CM codes related to IDD over the study period. The approach for identifying individuals with IDD has been described in detail elsewhere.21 In brief, Medicaid members who had one inpatient encounter with an IDD diagnosis code, or two outpatient non-pharmacy/non-laboratory service encounters with IDD diagnosis codes separated by at least one month, were categorized as having IDD. The list of applicable diagnosis codes was based on algorithms for potentially disabling conditions, available from the Chronic Conditions Data Warehouse of the Centers for Medicare and Medicaid Services. Because these are non-transient diagnoses, individuals identified as having IDD at any point within the study period (2010–2016) were considered to have IDD for the entire period.
Study populations
Our analyses focused on adults diagnosed with IDD, as described above. Because we did not have access to Medicare claims data, we included only those exclusively covered by Medicaid (47.2% of Medicaid-enrolled adults with IDD in the states participating in our study). To be included in the sample for a given quarter, an individual also needed to meet the following criteria:
Continuously enrolled in Medicaid for at least 12 months (all three months of the quarter, plus the preceding nine months); and
At least 18 years of age at the beginning of the quarter and not yet 65 years of age at the end of the quarter.
Identification of emergency department visits
We identified ED visits using current procedural terminology (CPT) codes, revenue codes, and place of service codes in each state’s Medicaid data. Then, we determined whether each ED visit resulted in an inpatient admission to a hospital. Because available data elements varied across states, we used one of the following two approaches, as applicable, to make this determination. The first approach identified ED visits as resulting in a hospitalization if a member had any inpatient claims on the same date of service or the following day. The second method relied on patient discharge status codes to identify visits that resulted in a hospital admission. ED visits without either of these indications of inpatient admission were categorized as outpatient visits.
Policy change variables
We defined three variables related to state Medicaid policy changes. The first, transition to managed care, was coded dichotomously. If states transitioned from fee-for-service to managed care during the study period, they were coded as 1 = yes. If baseline status (whether already managed care, a mix of managed care and fee-for-service, or entirely fee-for-service) remained unchanged during the study period, the state received a code of 0 = no change. Second, we grouped Medicaid expansion pursuant to the Affordable Care Act (ACA) into three categories: 0 = no expansion, 1 = expansion implemented through a Section 1115 waiver which allows states to operate their expansion program with greater flexibility than that allowed under the law (“expansion via waiver”), or 2 = expansion as set forth under the ACA (“full expansion”). Third, we created three categories indicating implementation of policies with potential to reduce ED visits within the Medicaid population: 0 = no applicable policy change, 1 = modest or targeted reforms, or 2 = major reforms. Major reforms included large-scale delivery system transformations aimed at improving health care delivery for the entire state Medicaid population, such as Oregon’s 1115 waiver reform which established Coordinated Care Organizations statewide with global budgets for integrating physical, mental, and oral health care delivery.22 Modest or targeted reforms included smaller scale efforts typically restricted to a particular Medicaid subpopulation (e.g., patients with serious mental illness). Categorization of states on each of the three policy changes variables is shown in Table 1.
Table 1.
Medicaid policy changes by state, 2010–2016.
| State | Transition to Managed Carea | Medicaid Expansionb | Healthcare Reforms to Reduce ED Visitsc |
|---|---|---|---|
| Iowa | Yes | Waiver | Modest/Targeted |
| Kansas | Yes | None | Modest/Targeted |
| Massachusetts | No | Full | Major |
| Michigan | No | Waiver | None |
| Montana | No | Waiver | Modest/Targeted |
| New York | Yes | Full | Major |
| Oregon | Yes | Full | Major |
| South Carolina | No | None | None |
States that transitioned from fee-for-service to managed care during the study period were coded as Yes. States with consistent status (whether already managed care, a mix of managed care and fee-for-service, or entirely fee-for-service) during the study period were coded as No.
Waiver = Medicaid expansion via waiver of certain requirements of the Affordable Care Act; Full = Medicaid expansion as set forth under the Affordable Care Act; None = No Medicaid expansion.
Major reforms included large-scale delivery system reforms aimed at improving health care delivery for the entire state Medicaid population. Modest or targeted reforms included smaller scale efforts typically restricted to a particular Medicaid subpopulation (e.g., patients with serious mental illness) or aspect of health care delivery (e.g., creation of health homes).
Data analyses
Each state supplied the following data for each calendar quarter from the beginning of 2010 through the end of 2016: 1) total number of unique members with IDD; 2) number of female versus male members with IDD; 3) number of members with IDD in each of the following age groups: 18–29 (reference group), 30–39, 40–49, 50–64; 4) total number of ED visits among adults with IDD; 5) number of ED visits leading to admission (inpatient ED visits); and 6) number of visits with patient treated in ED and released (outpatient ED visits). If available, states also supplied race/ethnicity data; however, not all states had this information. We reviewed trends by state and noted that one state exhibited a particularly dramatic increase in enrollment during the study period that did not correspond to the timing of Medicaid expansion. We examined demographic and disability characteristics of members before and after the increase and found minimal differences. To prevent the large change in numbers from skewing results, we included only those quarters after the increase (from first quarter of 2013 on) for this state.
We calculated the overall number of ED visits per 1000 member months in each quarter in each state, as well as the number of visits per 1000 member months that led to hospital admission (inpatient ED visits) versus being treated in the ED and released (outpatient ED visits). We then averaged state-level ED visit prevalence per quarter across states. This approach weighted each state equally, as opposed to assigning higher weights to more populous states. We did not use weights because we conducted our analysis at the state-level, examining the association between policy changes and average state-level ED rates. We graphed the number of ED visits per 1000 member months in each quarter for all states combined, and sequentially stratified on the following variables: 1) Transition to managed care (no = 0, yes = 1); 2) Medicaid expansion status (0 = no expansion, 1 = expansion via waiver, 2 = full expansion; and 3) implementation of policies intended to reduce ED visits within the Medicaid population (0 = no applicable policy change, 1 = modest or targeted reforms, 2 = major reforms).
To assess the overall linear time trend across all participating states, we estimated the following regression equation:
where yst is the number of ED visits per 1000 member months for quarter t in state s; are patient characteristics consistently measured across states (percent female, percent of members in each age group); Fs are state-level fixed effects; t is the time relative to the first quarter of 2010 (i.e., t = 1 for 2010Q1, t = 2 for 2010Q2 … t = 28 for 2016Q4); and is the error term, assumed to be correlated at the state level. The coefficient measures the time trend. We included state fixed effects to control for level differences across states that may be associated with state policies. Not controlling for such level differences might bias trend estimates if outcome levels are systematically different in states characterized by different policy changes.
To explore how each of the state-level policy changes during the study period was associated with change in ED visits, we conducted three separate regression analyses. In the first (examining transition to managed care), we used the following regression equation:
where Policy is a binary variable indicating presence or absence of a transition to managed care during the study period. The coefficient δ measures the time trend among states with no transition and the coefficient θ measures the time trend among states that transitioned to managed care during the study period. We tested whether the time trend was identical in states with the policy change compared to states with no such policy change (i.e., whether θ = 0). If θ did not equal zero, this implied differential trends for the two groups of states.
For the remaining analyses, where the policy change variable included 3 categories rather than being binary, we used the following regression formula:
where Policy1 and Policy2 indicated expansion via waiver and full expansion, respectively, for Medicaid expansion; and modest/targeted reforms and major reforms, respectively, for policies intended to reduce ED visits within the Medicaid population.
The three regression analyses (one for each type of policy change) were conducted once for overall ED visits and then separately for visits leading to inpatient admissions versus outpatient ED visits. We conducted sensitivity analyses in which we additionally controlled for increases in Medicaid enrollment across the study period. Results changed only minimally, and these changes did not affect our conclusions; therefore, we report only the results of our main analyses. All analyses were conducted in R.23
Results
The total number of people with IDD in our sample increased from 53,751 in 2010 to 88,112 in 2016 (Table 2). This change included increases in each state as well as the addition of one state in 2013. At the beginning of the study period, slightly more than half of these members were male, 18–29 years old and recorded as White race. Seventy percent (70%) were recorded as non-Hispanic ethnicity. From 2010 to 2016, the proportions of male and young members increased slightly.
Table 2.
Demographic characteristics of Medicaid members ages 18–64 years with intellectual and developmental disabilities at beginning and end of study period— eight US states, 2010–2016.
| 2010 | 2016 | |||
|---|---|---|---|---|
|
|
|
|
||
| (N = 53,751) | (N = 88,112)a | |||
| Gender | ||||
| Female | 23,780 | 44.24% | 35,836 | 40.67% |
| Male | 29,971 | 55.76% | 52,276 | 59.33% |
| Age (years) | ||||
| 18–29 | 31,272 | 58.18% | 53,065 | 60.22% |
| 30–39 | 10,029 | 18.66% | 17,286 | 19.62% |
| 40–49 | 6609 | 12.29% | 8137 | 9.23% |
| 50–64 | 5841 | 10.87% | 9624 | 10.92% |
| Race | ||||
| White | 29,347 | 54.58% | 46,308 | 52.54% |
| Black | 12,368 | 23.00% | 19,728 | 22.38% |
| Other | 8495 | 15.80% | 14,021 | 15.91% |
| Unknownb | 3558 | 6.62% | 8080 | 9.17% |
| Ethnicity | ||||
| Hispanic | 6852 | 12.75% | 10,258 | 11.64% |
| Non-Hispanic | 37,609 | 69.97% | 64,770 | 73.51% |
| Unknownb | 9290 | 17.28% | 13,084 | 14.85% |
Enrollment increases from 2010 to 2016 reflect the addition of one state in 2013, as well as increases within each state.
Some states did not have race and/or ethnicity data recorded.
The number of total ED visits per 1000 member months ranged from less than 25 visits to more than 125 visits per 1000 member months (Fig. 1). The average number of total and outpatient ED visits increased steadily over time, with the trend being statistically significant for outpatient visits (linear trend coefficient [δ]: 0.48; p < 0.05) (Table 3). Inpatient ED visits did not exhibit a linear time trend. Adjusting for demographic characteristics resulted in more negative linear time trends for all outcomes, suggesting that changes in the study population over time contributed to some of the increase in total and outpatient ED visits (details available in Supplemental Data). For inpatient ED visits, the adjusted linear time trend was negative and statistically significant (δ: 0.33; p < 0.05).
Fig. 1.
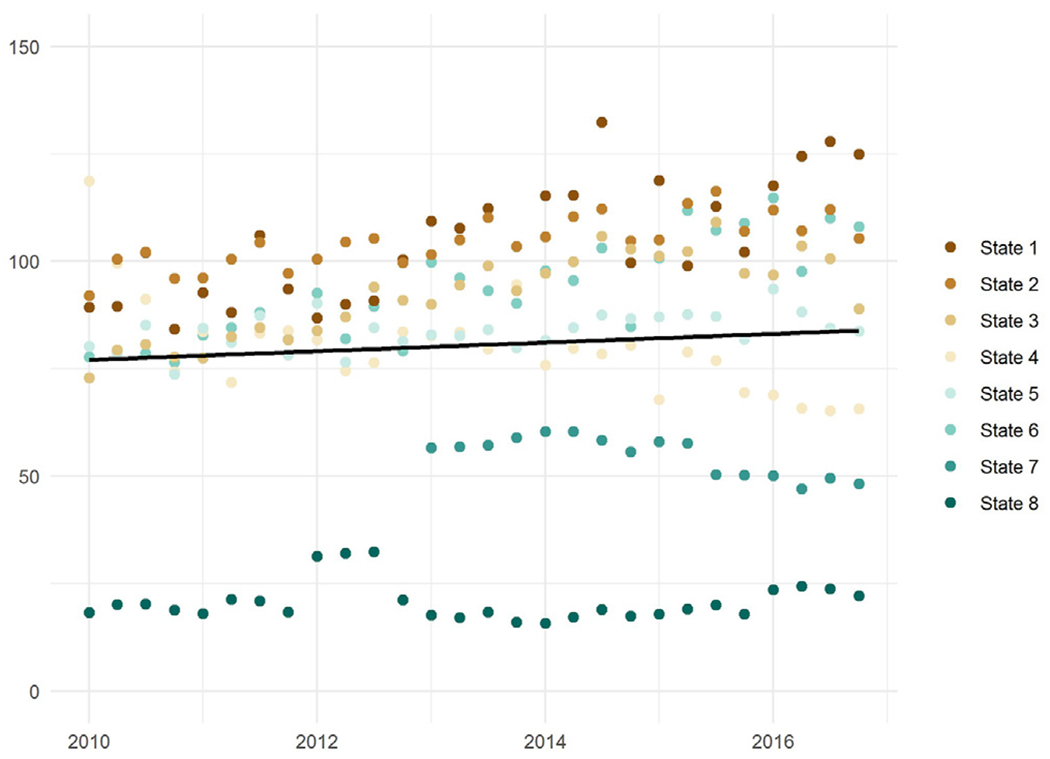
Total emergency department visits for adults with intellectual and developmental disabilities, by state and quarter— eight US states, 2010–2016.
Table 3.
Unadjusted and adjusted linear trends in total, outpatient, and inpatient emergency department visits for adults with intellectual and developmental disabilities, by policy change— eight US states, 2010–2016.
| Total | Outpatient | Inpatient | ||||
|---|---|---|---|---|---|---|
|
|
|
|
|
|||
| Reform | Unadj. | Adjusted | Unadj. | Adjusted | Unadj. | Adjusted |
| Trends across states | ||||||
| 0.45 | −0.31 | 0.48* | 0.02 | −0.03 | −0.33* | |
| Managed care transition | ||||||
| No | −0.13 | −0.23 | 0.06 | 0.11 | −0.19 | −0.34 |
| Yes | 0.63 | −0.24 | 0.37 | −0.31 | 0.27 | 0.04 |
| Medicaid expansion | ||||||
| No | 1.13** | 0.54 | 1.03** | 0.75 | 0.09 | −0.17 |
| Waiver | −0.80 | −0.96 | −0.79 | −0.85 | −0.01 | −0.07 |
| Full | −1.17** | −1.07** | −0.90* | −0.93* | −0.28 | −0.19 |
| Healthcare reform | ||||||
| No | −0.27 | 0.32 | −0.08 | 0.68 | −0.20 | −0.32* |
| Large | 0.23 | −0.74 | 0.21 | −0.76 | 0.01 | −0.03 |
| Small | 1.11 | −0.04 | 0.75 | −0.22 | 0.37*** | 0.19 |
Notes: Numbers show coefficients of linear trends (for no policy change) and interaction terms between linear trends and policy indicators. Adding the estimate for the interaction term to that for the linear trend yields the estimated direction and magnitude of change in ED visits associated with the applicable policy change (e.g., −0.80 + 1.13 = 0.33 for Medicaid expansion via waiver [unadjusted]). Regressions for unadjusted trends include the intercept, time trend, and policy indicators. Regression for adjusted trends also include state fixed effects and demographic characteristics (age; sex).
Significance codes:
p < 0.05;
p < 0.01;
p < 0.001.
Source: State Medicaid claims and enrollment records, 2010–2016.
States that transitioned to managed care during the study period did not show a differential linear trend in total, outpatient, or inpatient ED visits compared to states without such transitions. States with no Medicaid expansion had a strong increase in total and outpatient ED visits (δ for total ED visits: 1.13; p < 0.01; δ for outpatient ED visits: 1.03, p < 0.01). Multiplying these estimates by the number of quarters (28) implies an increase in total and outpatient ED visits of approximately 29–32 visits per 1000 member months over the course of the study period, although the effects were attenuated when we adjusted for demographic characteristics. In contrast, states that implemented Medicaid expansion via waiver had a much smaller and non-significant increase, and states with a full Medicaid expansion experienced a slight decrease in total ED visits and outpatient ED visits (Fig. 2). Linear trends in inpatient ED visits were similar across states that did or did not expand Medicaid.
Fig. 2.
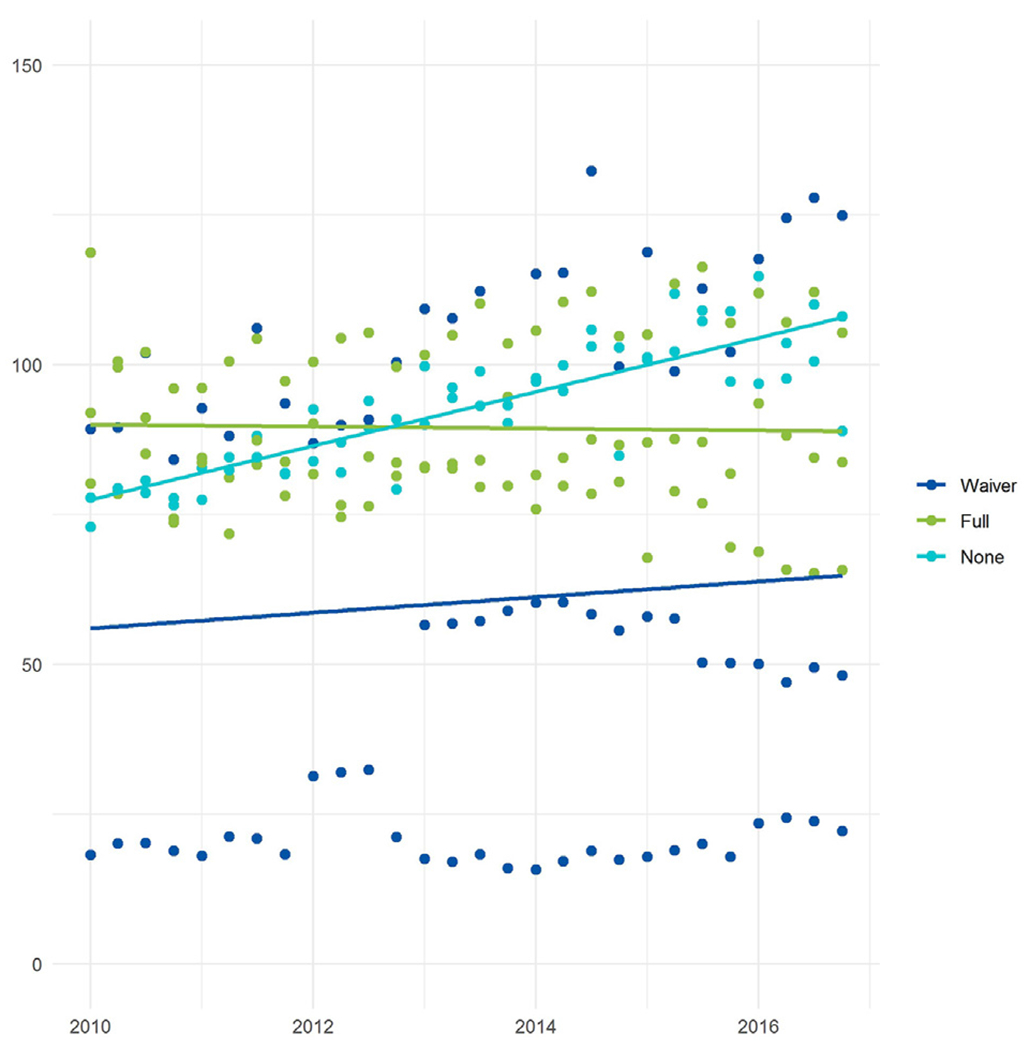
Total emergency department visits for adults with intellectual and developmental disabilities, by Medicaid expansion status — eight US states, 2010–2016. Note: Waiver = Medicaid expansion via waiver of certain requirements of the Affordable Care Act; Full = Medicaid expansion as set forth under the Affordable Care Act; None = No Medicaid expansion.
Health care reform efforts were not clearly associated with lower total or outpatient ED use among Medicaid-enrolled adults with IDD. States with no health care reform had a significant decline in adjusted inpatient ED visits (δ: 0.32; p < 0.05). States with small-scale health care reform efforts had a significantly more positive unadjusted time trend than states with no such reform (δ: 0.37; p < 0.001), but the estimate was not significant after accounting for demographic changes (Table 3).
Discussion
Although prior research has examined effects of Medicaid policy changes on ED use in the general adult Medicaid population,8–10,12–19 few previous studies have examined possible changes for adults with IDD. Overall, there was a steady increase in ED visits over time in our multi-state sample of adults with IDD. We found minimal association between ED use and health care reform efforts or transition to managed care. However, total and outpatient ED visits decreased slightly in states with full Medicaid expansion and showed no significant change in states with Medicaid expansion via waiver while increasing significantly in non-expansion states. This is in contrast to several studies reporting increased ED use by Medicaid members as a whole following expansion.12–19 In those studies, many of the newly enrolled Medicaid members had previously been uninsured and may have had significant health challenges.19 Conversely, because most adults with IDD were eligible for Medicaid prior to expansion, those with the most significant health care needs may have already had coverage; new members with IDD in expansion states may therefore have been healthier or had less severe disabilities, as suggested by other research.24 Additional research is needed to determine whether the changes in ED utilization among adults with IDD are correlated with their health status; receipt of primary care, clinical preventive services, and coordinated care; and overall health care costs. In addition, other research has linked expansion to improvements in health for the overall Medicaid population11,25 but has not explored health changes for Medicaid members with IDD.
Medicaid enrollment for people with IDD increased during the study period in every state in our sample, but increases were more abrupt and typically larger in states that expanded Medicaid. These increases in Medicaid enrollment may be attributed at least in part to the “welcome mat” effect, in which enrollment of previously eligible individuals increased due to publicity about coverage expansions under the ACA.17,26 There were statistically significant post-ACA increases in Medicaid enrollment for people with disabilities in both Medicaid expansion and non-expansion states, but increases were larger in expansion states.24,26 Prior to expansion, most people with disabilities wishing to qualify for Medicaid coverage first had to apply for Supplemental Security Income (SSI) and go through a disability determination process that required them to declare they could not engage in substantial work.27 SSI beneficiaries remain eligible for traditional Medicaid in both expansion and non-expansion states. However, Medicaid expansion under the ACA may allow some people with IDD to qualify for Medicaid on the basis of income alone, thereby making the enrollment process easier in those states.24,27 Ease of enrollment may have encouraged more adults with IDD to enroll in Medicaid when they had not previously taken that step.27,28 It is possible that new enrollees with IDD in expansion states may have differed in important ways from Medicaid members with IDD during pre-expansion time periods and in non-expansion states.24 Further research is needed regarding the socioeconomic and health characteristics of new Medicaid members with IDD in expansion states, and how these characteristics could potentially be associated with differences in ED use.
Limitations
The repeated cross-sectional design of our study provides information about patterns of ED use in entire population groups at multiple points in time rather than longitudinal data for specific individuals. Thus, the changes in ED use we observed may reflect changes in the composition and health characteristics of adult Medicaid members with IDD during our study period. We did not control for health characteristics such as comorbidities, which would be relevant to examine in future research. Our study also was not able to control for differences in race and ethnicity because not all states had these data available. Further, our study utilized data from eight states participating in a larger study of healthcare utilization among individuals with IDD. As such, our findings may not be representative of the broader U.S. population of adults with IDD or the effects of similar policy changes in other states. In particular, our sample included only one southern state and it was one that had not participated in Medicaid expansion. Given evidence that health is generally worse in the southeast than in other parts of the country,29 these broader patterns may have confounded our findings regarding the association between lack of Medicaid expansion and increases in ED visits. Our findings may also be unrepresentative of Medicaid-enrolled adults with IDD who are also enrolled in Medicare, given that we excluded dual enrollees because we did not have access to Medicare claims data. In light of existing research pertaining to the general Medicaid population, we focused our analyses on adults with IDD only. As part of furthering the evidence base, future research could focus on direct comparisons between ED use of adults with IDD and comparable adults without IDD in the Medicaid population. Moreover, we focused our analyses specifically on ED use. Additional investigation is needed into the possibility of corresponding changes in outpatient care among adults with IDD in relation to Medicaid expansion.
Conclusions
The study findings suggest that Medicaid expansion may affect ED utilization by adults with IDD somewhat, whereas managed care transitions and other health reforms may have little or no impact. Interventions specifically targeted to the needs of the IDD population may be needed to ensure appropriate non-emergency management of medical conditions among adults with IDD. Recent research indicates that primary care is underutilized by population groups with the most potential to benefit from it, including people with developmental disabilities.30 Improving receipt and continuity of quality health care and disability inclusive health promotion services early in the life course (e.g., during transition from pediatric to adult care) could have substantial impact on public health and downstream health care costs.31 Previously, increases in the Medicaid payment rate have been associated with greater availability of primary care appointments without increased wait times.32 Clinicians could be further incentivized to provide outpatient care to patients with IDD if metrics around reducing ED use were risk adjusted to support clinicians caring for patients with predictably higher use.30 In addition, while the number of medical, nursing, and dental schools that provide specific educational experiences about care of people with IDD is growing, more such education is needed, along with continuing education and training for practicing clinicians.33 Increasing providers’ knowledge and skills sets could enhance preventive care, disease management, and communication between healthcare providers, patients with IDD, and their caregivers.33–36 These approaches need development, evaluation, and dissemination in the literature so best practices in outpatient medicine are available to people with IDD and their providers, thereby potentially reducing the use of the ED.
Supplementary Material
Acknowledgments
The authors thank Julie Royer for assistance with variable creation and analysis design.
Funding
This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Hu[1] man Services (HHS) under grant number R41MC39340 and R40 Maternal and Child Health Field-initiated Innovative Research Studies Program.
Footnotes
Disclaimer
This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
Supplementary material
Supplementary data to this article can be found online at https://doi.org/10.1016/j.dhjo.2021.101225.
Presentation
Findings from this study were previously presented at the American Public Health Association virtual annual meeting in October of 2020.
References
- 1.Taylor DM. Americans with Disabilities: 2014. Current Population Reports. P70–152. Washington, DC: U.S. Census Bureau; 2018. [Google Scholar]
- 2.Yamaki K, Wing C, Mitchell D, Owen R, Heller T. The impact of Medicaid Managed Care on health service utilization among adults with intellectual and developmental disabilities. Intellect Dev Disabil. 2019;57(4):289–306. [DOI] [PubMed] [Google Scholar]
- 3.Ervin DA, Merrick J. Intellectual and developmental disability: healthcare financing. Frontiers in Public Health. 2014;2:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krahn GL, Fox MH. Health disparities of adults with intellectual disabilities: what do we know? What do we do? J Appl Res Intellect Disabil. 2014;27(5):431–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDermott S, Royer J, Mann JR, Armour BS. Factors associated with ambulatory care sensitive emergency department visits for South Carolina Medicaid members with intellectual disability. J Intellect Disabil Res. 2018;62(3):165–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lauer E, Lindgren S, Momany E, et al. Health service utilization patterns among Medicaid insured adults with intellectual and developmental disabilities: implications for access needs in outpatient community-based medical services. J Ambul Care Manag. 2021;4(2):138–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Snyder L, Rudowitz R. Trends in State Medicaid Programs: Looking Back and Looking Ahead. Kaiser Family Foundation; 2016. [Google Scholar]
- 8.McConnell KJ, Renfro S, Chan BKS, et al. Early performance in Medicaid accountable care Organizations: a comparison of Oregon and Colorado. JAMA Internal Medicine. 2017;177(4):538–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rutledge RI, Romaire MA, Hersey CL, Parish WJ, Kissam SM, Lloyd JT. Medicaid accountable care Organizations in four states: implementation and early impacts. Milbank Q. 2019;97(2):583–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sabik LM, Gandhi SO. Copayments and emergency department use among adult Medicaid enrollees. Health Econ. 2016;25(5):529–542. [DOI] [PubMed] [Google Scholar]
- 11.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid Expansion or expanded private insurance. JAMA Internal Medicine. 2016;176(10):1501–1509. [DOI] [PubMed] [Google Scholar]
- 12.Pines JM, Zocchi M, Moghtaderi A, et al. Medicaid expansion in 2014 did not increase emergency department use but did change insurance payer mix. Health Affairs (Project Hope). 2016;35(8):1480–1486. [DOI] [PubMed] [Google Scholar]
- 13.Barakat MT, Mithal A, Huang RJ, et al. Affordable Care Act and healthcare delivery: a comparison of California and Florida hospitals and emergency departments. PLoS One. 2017;12(8), e0182346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klein EY, Levin S, Toerper MF, et al. The effect of Medicaid expansion on utilization in Maryland emergency departments. Ann Emerg Med. 2017;70(5):607–614. e601. [DOI] [PubMed] [Google Scholar]
- 15.Nikpay S, Freedman S, Levy H, Buchmueller T. Effect of the Affordable Care Act Medicaid Expansion on emergency department visits: evidence from state-level emergency department databases. Ann Emerg Med. 2017;70(2):215–225. e216. [DOI] [PubMed] [Google Scholar]
- 16.Sabik LM, Cunningham PJ, Tehrani AB. Changes in emergency department utilization after early Medicaid expansion in California. Med Care. 2017;55(6). [DOI] [PubMed] [Google Scholar]
- 17.Garthwaite C, Graves J, Gross T, Karaca Z, Marone V, Notowidigdo M. All Medicaid Expansions Are Not Created Equal: The Geography and Targeting of the Affordable Care Act. NBER Working Paper; 2019. No. 26289. [Google Scholar]
- 18.Janke AT, Danagoulian S, Venkatesh AK, Levy PD. Medicaid expansion and resource utilization in the emergency department. Am J Emerg Med. 2020;38(12):2586–2590. [DOI] [PubMed] [Google Scholar]
- 19.Moghtaderi A, Black B, Zocchi M, Klauer K, Pilgrim R, Pines JM. The three-year effect of Medicaid expansion on emergency department visits and admissions. Ann Emerg Med. 2021;77(1):76–81. [DOI] [PubMed] [Google Scholar]
- 20.Eunice Kennedy Shriver National Institute on Child Health and Human Development. Intellectual and Developmental Disabilities (IDDs): Condition Information; 2016. https://www.nichd.nih.gov/health/topics/idds/conditioninfo/default. Accessed November 20, 2020. Accessed.
- 21.McDermott S, Royer J, Cope T, et al. Using Medicaid data to characterize persons with intellectual and developmental disabilities in five U.S. states. Am J Intellect Dev Disabil. 2018;123(4):371–381. [DOI] [PubMed] [Google Scholar]
- 22.Kushner J KT, Lind B, Renfro S, Rowland R, McConnell KJ. Evaluation of Oregon’s 2021-2018 Medicaid Waiver. Portland, OR: Center for Health Systems Effectiveness; 2017. [Google Scholar]
- 23.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. [Google Scholar]
- 24.Stimpson JP, Kemmick Pintor J, McKenna RM, Park S, Wilson FA. Association of Medicaid expansion with health insurance coverage among persons with a disability. JAMA Network Open. 2019;2(7), e197136. e197136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel MR, Tipirneni R, Kieffer EC, et al. Examination of changes in health status among Michigan Medicaid expansion enrollees from 2016 to 2017. JAMA Network Open. 2020;3(7), e208776. e208776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guth M, Garfield R, Rudowitz R. The Effects of Medicaid Expansion under the ACA: Updated Findings from a Literature Review. Kaiser Family Foundation; 2020. [Google Scholar]
- 27.Hall JP, Shartzer A, Kurth NK, Thomas KC. Medicaid expansion as an employment incentive program for people with disabilities. Am J Publ Health. 2018;108(9):1235–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Soni A, Burns ME, Dague L, Simon KI. Medicaid expansion and state trends in Supplemental Security Income program participation. Health Aff. 2017;36(8):1485–1488. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. Division of heart disease and stroke prevention. Quick maps of heart disease. Stroke, and Socio-economic Conditions; 2021. https://www.cdc.gov/dhdsp/maps/quick-maps/index.htm. Accessed September 3, 2021. Accessed.
- 30.Lines LM, Li NC, Mick EO, Ash AS. Emergency department and primary care use in Massachusetts 5 years after health reform. Med Care. 2019;57(2):101–108. [DOI] [PubMed] [Google Scholar]
- 31.Khavjou OA, Anderson WL, Honeycutt AA, et al. National health care expenditures associated with disability. Med Care. 2020;58(9):826–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Polsky D, Richards M, Basseyn S, et al. Appointment availability after increases in Medicaid payments for primary care. N Engl J Med. 2015;372(6):537–545. [DOI] [PubMed] [Google Scholar]
- 33.Ervin DA, Hennen B, Merrick J, Morad M. Healthcare for persons with intellectual and developmental disability in the community. Frontiers in Public Health. 2014;2:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilkinson J, Dreyfus D, Cerreto M, Bokhour B. Sometimes I feel overwhelmed”: educational needs of family physicians caring for people with intellectual disability. Intellect Dev Disabil. 2012;50(3):243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agaronnik N, Campbell EG, Ressalam J, Iezzoni LI. Exploring issues relating to disability cultural competence among practicing physicians. Disabil Health J. 2019;12(3):403–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boardman L, Bernal J, Hollins S. Communicating with people with intellectual disabilities: a guide for general psychiatrists. Adv Psychiatr Treat. 2014;20(1): 27–36. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


