Abstract
The pseudoaneurysms of the cystic artery (CAP) are very uncommon. They usually develop as a result of an acute cholecystitis or after a cholecystectomy. Among the complications, we can find hemorrhaging, biliary blockage, and haemobilia. Limited understanding of the illness makes managing specific cases difficult. We describe a case of a cystic artery pseudoaneurysm complicating an acute cholecystitis that was successfully treated by transcatheter arterial embolization.
Keywords: Pseudoaneurysm, Cystic artery, Interventional radiology, Cholecystitis
Introduction
Cystic artery pseudoaneurysms (CAP) are rare, and happen most commonly secondary to acute cholecystitis, cholelithiasis, for patients who have undergone a cholecystectomy, or, less frequently, idiopathic [1]. Patients typically show signs of hemoperitoneum, upper gastrointestinal hemorrhage, right upper quadrant abdominal pain, and jaundice [2]. We report a case of a cystic artery pseudoaneurysm aggravating acute cholecystitis treated successfully with a transcatheter arterial embolization.
Case report
A 71-year-old woman, with no pathological history, was admitted in the surgical emergencies for upper right quadrant pain with anemic syndrome and deterioration of general condition. The patient at the admission had a Glasgow Coma Scale of 15, she had a blood pressure of 105/65 mmHg, heart rate of 95 beats/min, body temperature of 37.5 °C, and respiratory rate of 30 breaths/minutes. During the abdominal examination, there was a diffuse abdominal tenderness, more pronounced at the upper right quadrant, without muscle guarding. The initial laboratory investigations revealed a normal leukocytes count (white blood cell count of 9300/mm3), an elevated C-reactive protein (229 mg/L) and a procalcitonin of 142 ng/mL.
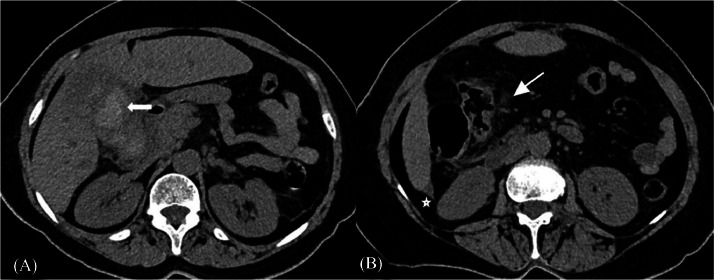
After stabilization of vital signs with fluid resuscitations, a dynamic abdominal computed tomography (CT) was performed. Unenhanced phase showed an enlarged heamorrahagic gallbladder (hyperdense) containing a lithiasis in the infundibulum. It also showed a low abondance intraperitoneal high-density effusion (Fig. 1).
Fig. 1.
Unenhanced computed tomography shows a large intravesicular hematoma. (A) (white arrow). It also demonstrates a peri-vesicular fatty infiltration (arrowhead) and minimal sub-hepatic fluid collection (white star) (B).
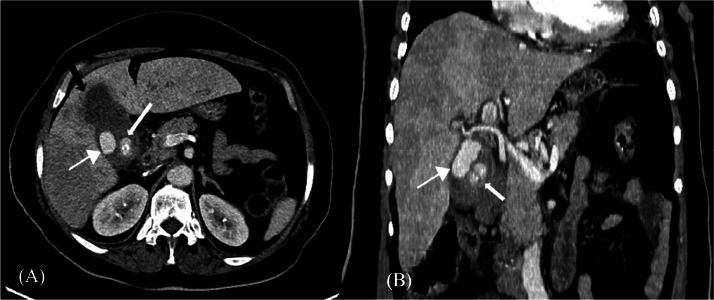
The arterial phase revealed a large cavity filled by contrast located inside the gallbladder and connected with the proximal segment of cystic artery. The portal phase displayed a thick gallbladder wall that showed no enhancement, with focal wall irregularity at the fundus, suggesting a pre-perforating gangrenous gallbladder (Fig. 2). These results suggested the presence of newly developed cystic artery pseudoaneurysm in conjunction with a possible cholecystitis.
Fig. 2.
Contrast enhanced computed tomography scan showing a large cystic artery pseudoaneurysm (arrowhead) which is connected to the cystic artery associated with an infundibular gallstone (arrow) (A and B). Focal wall irregularity at the fundus suggesting a pre-perforating gallbladder (black arrows) (A).
Considering the hemodynamic stability and the operative bleeding risks, we chose to perform transcatheter arterial embolization (TAE) to prevent pseudoaneurysm rupture and the patient's death with hemorrhagic shock.
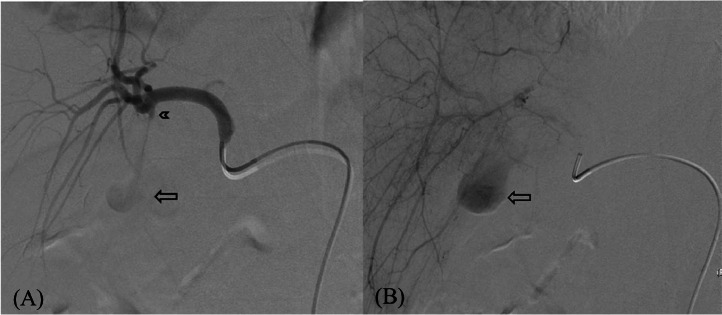
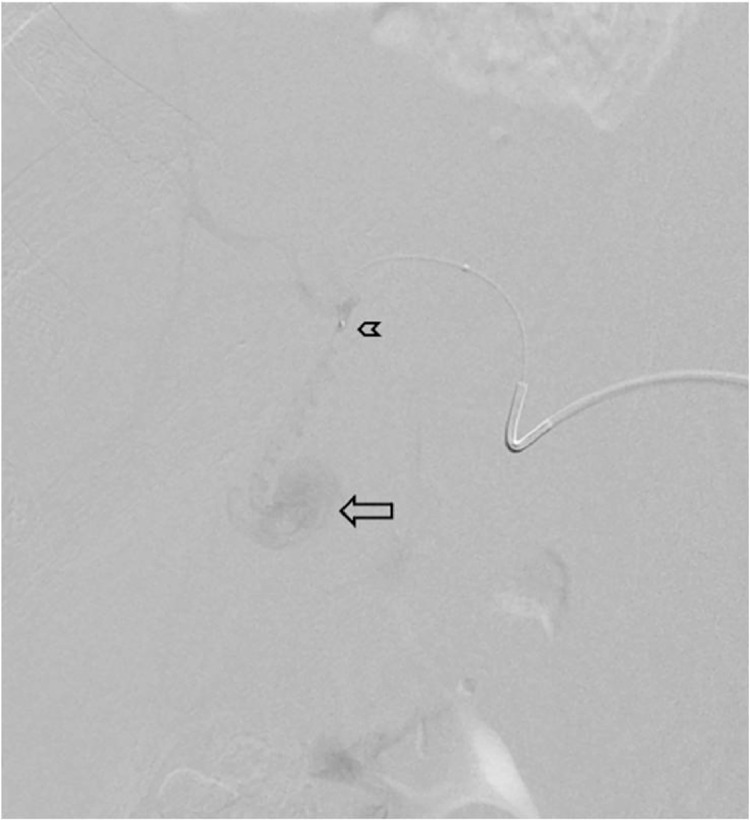
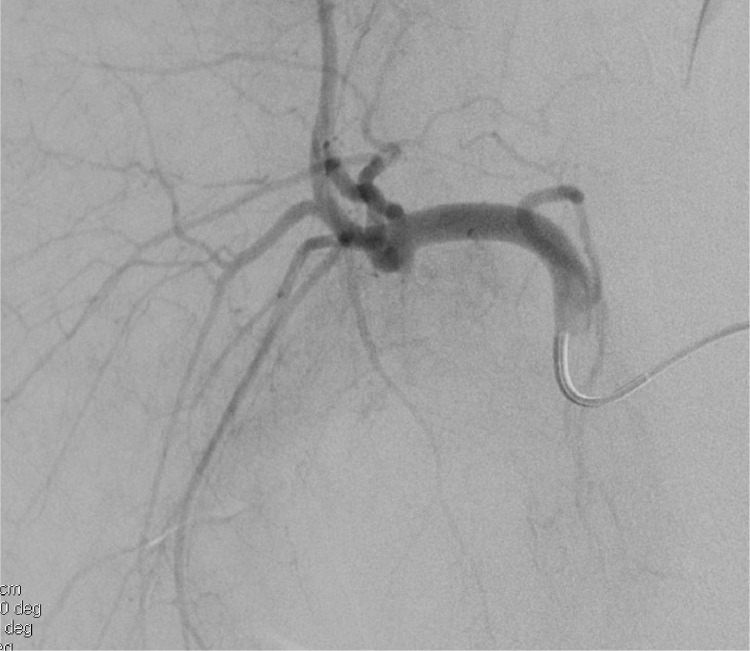
The angiogram confirmed a cystic artery pseudoaneurysm with progressive filling (Fig. 3). Through a 5 French (Fr) Cobra catheter placed on the hepatic artery, a microcatheter was inserted into the proximal part of the cystic artery (Fig. 4). Embolization was performed using glue (mixture of GLUBRANⓇ and LIPIODOLⓇ) at the pseudoaneurysm neck (proximal part of the cystic artery) (Fig. 5). The postembolization angiogram revealed CAP exclusion (Fig. 6). Our patient remained hemodynamically stable during and after the procedure. The patient was then hospitalized in the department of visceral surgery and benefited of a cholecystectomy.
Fig. 3.
Hepatic artery Angiogram shows a cystic artery pseudoaneurysm with a diameter of 3cm (arrow) with a narrow neck (arrowhead).
Fig. 4.
Microcatheterism of the cystic artery shows a cystic artery pseudoaneurysm with a diameter of 3 cm (arrow) with a narrow neck (arrowhead).
Fig. 5.
After embolization with glue, arterial inflow to the cystic artery is completely blocked.
Fig. 6.
The postembolization angiogram revealed CAP exclusion.
Discussion
Haemobilia is rarely caused by vascular diseases. The hepatic artery or one of its branches is the primary site of aneurysms or pseudoaneurysms. Haemobilia resulting from cystic artery vascular diseases is extremely uncommon and usually follows iatrogenic trauma, such as a laparoscopic cholecystectomy. Non-traumatic pseudoaneurysms of the cystic artery are infrequent and usually result from gallbladder inflammation. Because of their proximity, these processes induce vascular lesions that might lead to a fistula between the gallbladder and the artery. The inflammatory process weakens the vessel wall by causing thrombosis of the vasa vasorum and damaging the vascular adventitia. Large gallstones that press up against the cystic artery can directly cause erosion, which is another mechanism at work [3]. It may seem odd that cystic artery pseudoaneurysm is so rare given that cholecystitis is a customary manifestation. Other authors have reported that the inflammatory response influences the pseudoaneurysm to early thrombosis, limiting its hemorrhagic rupture and associated sequelae [4], [5].
Quincke's triad—upper quadrant discomfort (biliary colic), obstructive jaundice, and gastrointestinal bleeding—is the classic presentation of hemomobilia [6].
As is the situation with our patient, 38% of patients with cystic artery pseudoaneurysm were not jaundiced, according to a recent case analysis of 16 patients by Akatsu and colleagues. According to the cases that have been recorded, the pseudoaneurysm was found inside the gallbladder in 56% of the cases and had a size range of 0.2 to 4 cm. In our case, the pseudoaneurysm was of 3 cm in diameter and was highly vulnerable to rupture. Eight cases had a single gallstone, while four cases had numerous stones [6]. In our current case, the pseudoaneurysm and the impacted gallstone coexisted. Furthermore, there's a chance that significant harm to the gallbladder wall accelerated the pseudoaneurysm's formation.
Pseudoaneurysms can be diagnosed with ultrasound, particularly color-Doppler ultrasonography, and arterial phase contrast-enhanced computed tomography scan [6]. For patients who are contraindicated for intravenous contrast agent administration, magnetic resonance imaging (MRI) offers an alternative [1].
When pseudoaneurysms are diagnosed, it's a serious medical emergency that needs to be treated quickly and aggressively since a rupture could result in exsanguination, which is potentially fatal. Ruptures of pseudoaneurysms in the hepatic artery have been linked to a death rate of 21%-33%. In the past, surgery was the main method used to treat pseudoaneurysms. This procedure included resecting the pseudoaneurysm and ligaturing the right hepatic artery or cystic artery stump. Nonetheless, because of major advancements in catheter-based therapies, TAE is now the main treatment for pseudoaneurysms. This is achieved by occluding the sac or feeding vessel with coils, N-butyl cyanoacrylate, also known as glue (GlubranⓇ, HistoacrylⓇ), and ethylvinyl alcool copolymere (OnyxⓇ, SquidⓇ). Using real-time ultrasound and Doppler guidance, multiple researchers have reported successfully managing pseudoaneurysms by directly injecting thrombin into the pseudoaneurysm. However, this method of embolization may not be selective, leading to potentially dangerous side effects as bowel and liver infarctions [7].
TAE should be viewed as a temporary treatment before cholecystectomy for pseudoaneurysms linked to cholecystitis [6] or in cases where the endovascular approach is not successful. It is however thought to be a definitive therapy for cystic artery pseudoaneurysm that forms after cholecystectomy [1].
In conclusion, even though cystic artery pseudoaneurysm is uncommon, it is crucial to include it in the differential diagnosis of hemomobilia. It is thought that dynamic CT is the most effective diagnostic instrument. Before performing a cholecystectomy and ligaturing the cystic artery, embolization should be used to treat the pseudoaneurysm while guaranteeing the patient's safety. It is however thought to be a final treatment, or a temporary one (for pseudoaneurysms secondary to cholecystitis).
Patient consent
Informed written consent was obtained from the patient for publication of the Case Report and all imaging studies.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Taghavi SMJ, Jaya Kumar M, Damodaran Prabha R, Puhalla H, Sommerville C. Cystic artery pseudoaneurysm: Current review of aetiology, presentation, and management. Surg Res Pract. 2021;2021:1–6. doi: 10.1155/2021/4492206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.R.Berry JH, Kardashian AA, LaRusso NF, Tabibian JH. Hemobilia: etiology, diagnosis, and treat- ment. Liver Res. 2018;2(4):200–208. doi: 10.1016/j.livres.2018.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Velázquez RM, Pérez JAC, Mérida MAA, Gómez JM. Non traumatic pseudoaneurysm of the cystic artery as a cause of haemobilia. Gastroenterol Hepatol. 2018;41(4):257–259. doi: 10.1016/j.gastrohep.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Barba CA, Bret PM, Hinchey J. Pseudoaneurysm of the cystic artery: a rare cause of hemobilia. Can J Surg. 1994;37(1):64. [PubMed] [Google Scholar]
- 5.Hall TC, Sprenger De Rover W, Habib S, Kumaran M. Cystic artery pseudoaneurysm secondary to acute cholecystitis: an unusual cause for haemobilia. BJR Case Rep. 2016;2(2) doi: 10.1259/bjrcr.20150423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akatsu T, Tanabe M, Shimizu T, Handa K, Kawachi S, Aiura K, et al. Pseudoaneurysm of the cystic artery secondary to cholecystitis as a cause of hemobilia: report of a case. Surg today. 2007;37(5):412–417. doi: 10.1007/s00595-006-3423-2. [DOI] [PubMed] [Google Scholar]
- 7.Machado NO, Al-Zadjali A, Kakaria AK, Younus S, Rahim MA, Al-Sukaiti R. Hepatic or cystic artery pseudoaneurysms following a laparoscopic cholecystectomy: literature review of aetiopathogenesis, presentation, diagnosis, and management. Sultan Qaboos University Med J. 2017;17(2):e135. doi: 10.18295/squmj.2016.17.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]