Abstract
Introduction
Large-scale implementation of the Health Extension Program (HEP) has enabled Ethiopia to make significant progress in health services coverage and health outcomes. However, evidence on equity and disparities in the implementation of the HEP is limited. The aim of this study was to examine disparities in the implementation of the HEP in Ethiopia.
Methods
We used data from the 2019 National HEP assessment which was conducted between Oct 2018 and Sept 2019 in nine regions in the country. Data were collected from 62 districts, 343 Health posts, 179 Health centres, 584 Health Extension Workers (HEWs), and 7043 women from 7122 Households. This study focused on selected input, service delivery, and coverage indicators. We used rate differences, rate ratios and index of disparity to assess disparities in HEP implementation across regions.
Results
We found wide inter-regional disparities in HEP implementation. Developing regional states (DRS) had significantly lower availability of qualified HEWs (Rate Ratio (RR) = 0.54), proportion of households visited by Health Extension workers (RR = 0.40), and proportion of mothers who received education on child nutrition (RR = 0.45) as compared national average. There were also significant disparities in HEP implementation among DRS in the proportion of households visited by HEWs in the past 12 months (Index of disparity = 1.58) and proportion of adolescents who interacted with HEWs (Index of disparity = 1.43). Despite low overall coverage of health services in DRS, the contribution of the HEP for maternal health services was relatively high.
Conclusion
There were significant inter-regional disparities in the implementation HEP in Ethiopia. The level of disparity among DRS was also remarkable. To achieve Universal Health Coverage, it is important that these disparities are addressed systematically and strategically. We recommend a tailored approach in HEP implementation in DRS.
Keywords: Disparities, Health extension program, Family health
1. Introduction
The Sustainable Development Goals (SDGs) through its pledge of “leave no one behind” affirmed the global commitment of nations to achieving the development needs of people by addressing avoidable disparities. SDG 3 (To ensure healthy lives and promote well-being for all at all ages) aims to achieve Universal Health Coverage (UHC) which seeks equitable access of healthcare to all people [1]. Promoting health equity has been a global agenda widely promoted by national and global agencies, for several decades [[2], [3], [4]]. As a result, substantial progress has been made in improving health equity among various populations throughout the world. However, there are still significant health disparities within and between nations [5,6].
In the health sector, equity has been broadly defined as “the absence of avoidable, unfair, or remediable differences in health among subgroups of a population and/ or locations.” Operationally, health equity is measured and monitored in terms of the extent of disparities in access to healthcare services and health outcomes, including the occurrence of disease, disability, or death among populations in different socioeconomic, demographic, and geographic categories [7].
Universal Health Coverage has primary healthcare as its cornerstone[8]. Primary Healthcare is an approach to healthcare delivery and improvement of well-being centred on the needs of individuals, families and communities. Governments across low-income and middle-income countries have pledged to achieve universal health coverage by 2030 [9]. However, countries in sub-Saharan Africa are still long way behind achieving this goal. Strengthening primary healthcare systems, including training and deployment of community level health workers, is essential to achieve this goal [10].
Disparities in health service coverage and health outcomes remain to be a significant challenge in Ethiopia [[11], [12], [13], [14]]. Geographic disparities, which overlap substantially with disparities across regions and livelihood categories, have been the primary focus of programs that promote health equity in the country [15]. The difference between Economically Advanced Agrarian Regional States (EAARS: Tigray, Amhara, Oromia, SNNPR) and Developing Regional States (DRS: Afar, Somali, Benishangul Gumuz, Gambella) has been the major focus of the health system during the implementation of the Health Sector Development Program (HSDP) and Health Sector Transformation Plan (HSTP) [16,17].
The Health Extension Program (HEP), launched in 2003, is one of Ethiopia's major investments designed to improve the health of Ethiopians. The HEP is a community-based health program that was initially designed to deliver 16 packages of health services to agrarian communities [[18], [19], [20]]. Later, the program evolved in various ways, including adaptations for pastoralist and urban communities, making changes to existing packages, and including two additional packages and upgrading training of Health Extension Workers (HEWs) [21]. HEWs are female community health workers delivering community-based services at ‘Kebele’ (the smallest administrive unit) level. They are recruited from the community, have completed at least grade 10 and received a one-year training on HEP. Two HEWs are assigned at Health posts in each kebele and they spend 75% of their time making house-to-house visits [22]. In 2019, the program had more than 39,878 HEWs and 17,587 Health Posts (HPs) [23]. The program has been acknowledged as a flagship program and led to the recent gains in health outcomes in the country. This program has made a significant contribution in improving access to and coverage of basic health services in Ethiopia [24].
Despite remarkable improvements in health service coverage, evidence from the 2019 Mini-EDHS, [11] and the 2018 Service Availability and Readiness Assessment [25,26] indicated that there are substantial disparities between geographic regions; urban and rural areas; and agrarian and pastoralist settings [12,27,28]. Health indicators in DRSs are much lower than national averages. For instance, modern contraceptive use was 12.7% in Afar and 3.4% in Somali as compared to over 30% in agrarian regions. Only 11.1% and 31.1% of pregnant women in Afar and Somai regions, respectively, had four or more antenatal care visits during their recent pregnancies as compared to 64% in Tigray region and 51% in Amhara region. Similarly, only 20% of children in Afar and 18% of children in Somali region had received all basic vaccinations as compared to 83% in Addis Ababa, 73% in Tigray and 62% in Amhara [29].
Though disparities in health service coverage and health outcomes at population levels have been well investigated, there is limited evidence on equity and disparities in the implementation of HEP and their impacts on access to and coverage of basic health services across regions in Ethiopia. Therefore, the aim of this study was to examine geographic disparities in the implementation of HEP in Ethiopia. More specifically, the study examined disparities in availability of basic inputs of HEP, accessibility of selected HEP services to the target populations, and coverage of selected HEP services.
2. Methods
2.1. Study context
At the time of this study, Ethiopia has four agrarian regions – Tigray, Amhara, Oromia and SNNPR – and the urban regions/city administrations – Addis Ababa, Dire Dawa and Hareri– and four Developing Regional States (DRS) – Afar, Benishangul-Gumuz, Gambella and Somali regions. Since the adoption of the health policy of the transitional government of Ethiopia in 1993 [30], special attention has been given to health system strengthening in DRS in order to narrow the geographic disparities in terms of access to health services, uptake of essential services and health outcomes. Accordingly, HSDP and HSTP gave special attention to these regions. This study focused on examining disparities in HEP implementation in agrarian regions and DRS.
2.2. Study design
The national HEP assessment was a cross-sectional study involving 343 Health posts, 179 Health centres, 584 Health Extension Workers (HEWs), and 7043 women from 7122 Households from 62 districts. This paper used data collected from the Health posts and households.
2.3. Data source
We used Health post and household level quantitative data that were collected as part of the National HEP assessment in Ethiopia. Details of the methods used in the national HEP assessment are presented elsewhere [31]. In brief, the national assessment of HEP was conducted from October 2018 to September 2019. All nine regional states and two city administrations were included. The assessment was guided by the Primary Health Care Performance Initiative (PHCPI) framework. Data were collected at all levels of the health system, including the Ministry of Health, Regional Health Bureaus (RHBs), District Health Offices, Health Centers (HCs), HPs, and communities.
2.4. Sampling strategy
In the National HEP assessment, a three-stage sampling strategy was applied to select the study woredas/districts, health facilities, and community members in both agrarian and pastoralist regions. The woredas in each region were further classified by their predominant means of livelihood to create 11 strata (seven agrarian and four pastoralist). Within each stratum, a predetermined number of woredas was selected and six kebeles were then selected randomly from each of these woredas. All Health posts in the selected kebeles were included in the Health post assessment, while the first three selected kebeles were included in the household survey. The sampling frame of households was obtained from the HEWs. A predetermined number of households (34–38) were randomly selected for the household survey. From each selected household, the household head, the wife of the head (if the household head was a man), and a youth girl (aged 15–24 years) were interviewed. Indicators of interest.
For this analysis, we purposively selected eight input, six process (access to HEP services) and six output (coverage of HEP services) indicators. The selection of the indicators was based on relevance and attributability to HEP and its packages and availability of representative data at regional level.
2.4.1. Input indicators
The input indicators assess availability of human resources, basic amenities and guidelines in health posts as well as adequacy of technical supervision by health centers. These included percentage of health posts with or having at least one level IV HEWs, improved water source, sanitation facilities, Cold box, Oral Rehydration Salt (ORS), HEP guidelines: Family Health, and adequate supervision from HC.
2.4.2. Process indicators
The process indicators focus on exposure of household members, especially women and young girls, to HEP services and adoption of HEP-targeted behaviors by women in the general population. These included percentage of household members exposed to HEP service, households ever been visited by HEWs, households visited by HEWs in the last year, women who interacted with HEWs, households that adopted HEP-targeted behaviour, and adolescents who interacted with HEWs.
2.4.3. Output indicators
The service coverage indicators included in this study focus on the widely implemented HEP services such as maternal health services, infant and young child feeding, sanitation and hygiene and treatment of sick people. These included percentage of Women received family planning services from HEWs/HP, women who attended their four antenatal visits at HPs, women who received postnatal care from HEWs, household which were visited by HEWs for Infant and Young Child Feeding, women educated on handwashing by HEWs, and sick people who sought treatment from HP/HEW.
2.5. Measurements
Data on input indicators were collected either by interview of HEWs or direct observation of Health Posts using a standardized checklist. The national HEP assessment collected data on access to and coverage of key HEP services through interview of women, men and young girls using a structured and pre-tested questionnaire. Indicator values, both at national and regional levels were computed as percentages. Indicators for agrarian regions were computed by aggregating individual level data from four national regional states (Tigray, Amhara, Oromia and SNNPR). Similarly, indicator data for DRS were computed from aggregated data representing four DRS (Afar, Benishangul-Gumuz, Gambella and Somali regions).
2.6. Data analysis
We used Stata 16.0 for analysis of data. The analysis of disparities in the implementation of HEP involved four stages. The first stage was direct comparison of HEP implementation indicator data among regions and between agrarian regions and DRS. In the second stage, we computed deviations of HEP implementation indicator values in DRS from national average and Agrarian average and best performing regions. This was done to examine the disparities among DRS relative to national average, agrarian regions and best performing regions. In the third stage, we examined disparities among Agrarian regions and DRS by comparing each region with agrarian regions and DRS averages. Finally, we considered aggregated HEP implementation indicators for DRS and examined its disparity from national and agrarian region averages and best performing regions.
We used both absolute (rate difference) and relative (relative rate and index of disparity) measures of disparity. Rate difference, as the absolute disparity between two health status indicators, was calculated as the simple arithmetic difference between two values of an indicator. The Rate Ratio was calculated by one rate by another. We calculated the Index of Disparity as the sum of the difference between several group rates and a reference rate, and the summed differences were expressed as a proportion of the reference rate [32].
3. Results
3.1. Study population
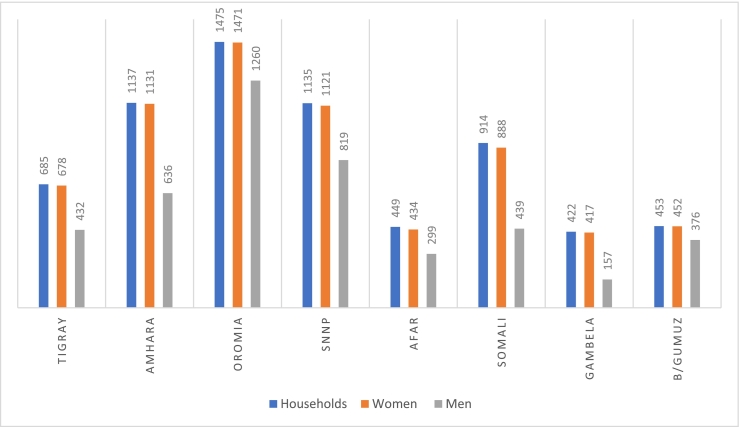
A total of 343 Health posts (235 from Agrarian regions – Tigray, Amhara, Oromia and SNNR regions- and 108 from DRS – Afar, Somali, Benishangul-Gumuz, and Gambella regions), 179 Health Centers (139 from Agrarian regions and 40 from DRS) and 584 HEWs (414 from Agrarian regions and 170 from DRS) from nine regions and 62 districts (42 from Agrarian regions and 20 from DRS) were involved in the national HEP assessment. A total of 7122 households (4854 from Agrarian regions and 2268 from DRS), 7122 women of child-bearing age (4821 from Agrarian regions and 2222 from DRS), 4805 men (3407 from Agrarian regions and 1398 from DRS) and 1020 young girls (746 from Agrarian regions and 274 from DRS) were also interviewed. The distribution of the study population by regions is presented in Fig. 1.
Fig. 1.
Study population by region.
3.2. Indicators of HEP implementation
Examination of indicator values by region showed a relatively higher availability of sanitation facilities and the tracer drug – oral rehydration therapy (ORS) in health posts. On the other hand, exposure of adolescents to HEP, delivery of IYCF services by HEWs and treatment of sick people at health posts were relatively lower. Benishangul-Gumuz region had higher values on most of HEP implementation indicators whereas Somali region had lower values on most of HEP implementation indicators. DRS have higher input indicators but low process and output indicators, except for coverage of maternal health services. Actually, DRS had higher coverage of maternal health services provided by HEWs. Health posts in DRS were more likely to receive adequate technical supervision by health centres. Details are shown in Table 1.
Table 1.
Indicators of HEP implementation (%) in Ethiopia stratified by administrative regions.
| Tigray | Amhara | Oromia | SNNPR | Afar | Somali | Gambela | B/Gumuz | EAARS | DRS | National | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Inputs: HP/HEWs | |||||||||||
| Average population served per HEW (number) | 2875 | 2834 | 3110 | 1966 | 1256 | 1268 | 424 | 935 | 2728 | 1361 | 2599 |
| HPs with at least one level IV HEWs (%) | 80.9 | 69.0 | 64.9 | 58.0 | 20.7 | 33.0 | 66.5 | 52.3 | 65.3 | 33.5 | 62.4 |
| HPs with improved water source (%) | 18.6 | 28.1 | 21.4 | 27.4 | 38.6 | 59.7 | 61.5 | 56.9 | 25.0 | 47.7 | 27.1 |
| HPs with sanitation facilities (%) | 93.1 | 85.4 | 86.8 | 93.9 | 97.2 | 66.4 | 94.9 | 82.2 | 89.3 | 69.2 | 87.4 |
| HPs having Cold box (%) | 62.4 | 39.8 | 39.0 | 36.2 | 42.8 | 40.0 | 55.0 | 40.8 | 45.8 | 31.4 | 41.8 |
| HPs having Oral Rehydration Salt (ORS) (%) | 100.0 | 98.9 | 86.0 | 74.9 | 72.9 | 60.6 | 85.9 | 90.9 | 91.0 | 69.0 | 86.0 |
| HPs with HEP guidelines: Family Health (%) | 78.2 | 78.8 | 59.1 | 65.2 | 22.5 | 54.9 | 30.6 | 48.4 | 65.2 | 53.7 | 64.6 |
| HPs with adequate supervision from HC (%) | 59.5 | 63.3 | 47.1 | 37.0 | 69.8 | 91.4 | 57.7 | 57.4 | 48.4 | 80.7 | 51.4 |
| Process: Service delivery | |||||||||||
| HH members exposed to HEP service (%) | 74.5 | 68.6 | 53.7 | 71.0 | 71.2 | 24.6 | 70.6 | 92.9 | 62.7 | 44.0 | 61.8 |
| HHs ever been visited by HEWs (%) | 67.2 | 64.9 | 52.8 | 49.4 | 31.8 | 5.5 | 51.6 | 90.6 | 56.6 | 22.3 | 55.1 |
| HHs visited by HEWs in the last year (%) | 39.5 | 41.7 | 25.4 | 30.4 | 25.2 | 4.8 | 45.3 | 76.4 | 32.0 | 14.7 | 31.2 |
| Women who interacted with HEWs (%) | 63.0 | 61.5 | 47.2 | 63.6 | 67.1 | 21.4 | 68.2 | 90.7 | 55.5 | 40.3 | 54.8 |
| HHs with adopted HEP-targeted behavior (%) | 53.7 | 57.7 | 49.9 | 44.1 | 39.0 | 39.2 | 42.0 | 60.7 | 51.3 | 38.4 | 50.8 |
| Adolescent who interacted with HEWs (%) | 37.5 | 27.3 | 12.3 | 26.7 | 44.7 | 8.5 | 58.0 | 50.8 | 22.1 | 16.7 | 21.9 |
| Output: Service coverage | |||||||||||
| Women received FP from HEWs/HP (%) | 40.4 | 51.6 | 54.9 | 66.7 | 49.3 | 0.0 | 43.9 | 54.6 | 56.5 | 67.7 | 56.7 |
| Women who attended their ANC-IV at HPs (%) | 9.5 | 9.9 | 38.8 | 54.2 | 32.4 | 94.4 | 36.0 | 21.5 | 31.8 | 56.2 | 32.2 |
| Women who received PNC from HEWs (%) | 73.6 | 36.2 | 40.8 | 39.9 | 7.2 | 50.0 | 39.5 | 89.9 | 43.1 | 46.1 | 43.2 |
| HHs visited by HEWs for IYCF (%) | 43.6 | 39.1 | 22.5 | 32.9 | 16.7 | 3.6 | 37.3 | 41.5 | 29.6 | 13.1 | 28.8 |
| Women educated on handwashing by HEWs (%) | 65.7 | 49.2 | 49.6 | 65.5 | 54.6 | 9.9 | 42.5 | 73.0 | 53.9 | 27.4 | 52.7 |
| Sick people who sought Rx from HP/HEW (%) | 10.6 | 4.6 | 10.4 | 15.7 | 78.7 | 34.8 | 54.6 | 33.6 | 10.3 | 29.2 | 10.8 |
HPs = Health Posts; HEWs = Health Extension Workers; HHS=Households; HEP=Health Extension Program; FP=Family Planning; PNC=Postnatal care; IYCF = infant and young child feeding; HC=Health Center; ANC = Antenatal care.
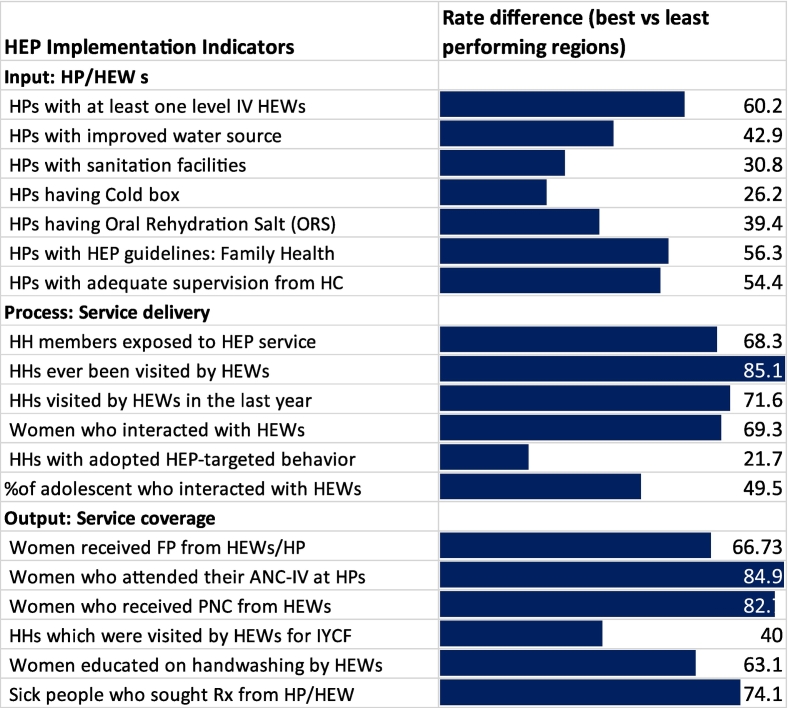
3.3. Interregional disparities
As shown in Fig. 2, disparities between best performing and least performing regions were highest for percentage of households ever visited by HEWs, percentage of women who attended four ANC visits at health posts and percentage of women who received PNC services from HEWs. Relatively lower disparities were observed in the adoption of HEP-targeted behaviour, availability of cold box in health posts, and availability of sanitation facilities in health posts. Further examination of best and least performing regions showed that Benishangul-Gumuz and Somali regions had best and least performance, respectively, in process (access to health services) indicators.
Fig. 2.
Disparities between best and least performing regions.
3.4. Disparities in Developing regional states
Table 2 shows deviations of HEP implementation indicators in DRS from national average, Agrarian average and best performing region. Analysis of status of HEP implementation indicators in individual DRS as compared to national and Agrarian averages showed a mixed pattern. While regions like Benishangul-Gumuz and Gambella have many HEP implementation indicators above the national and Agrarian averages, Somali region had only a few HEP implementation indicators at or above the national and Agrarian averages. However, DRS have significantly lower HEP implementation indicators as compared to best performing regions.
Table 2.
Disparities of DRS from national average and Agrarian average and best performing region.
| RD from national average |
RD from Agrarian average |
RD from best performing region |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Afar | Somali | Gambela | B/Gumuz | Afar | Somali | Gambela | B/Gumuz | Afar | Somali | Gambela | B/Gumuz | |
| Inputs: HP/HEWs | ||||||||||||
| Average population served per HEW (%) | −105 | −1331 | −2175 | −1664 | −1472 | −1460 | −2304 | −1793 | −1854 | −1842 | −2686 | −2175 |
| HPs with at least one level IV HEWs (%) | −13 | −29.4 | 4.1 | −10.1 | −44.6 | −32.3 | 1.2 | −13 | −60.2 | −47.9 | −14.4 | −28.6 |
| HPs with improved water source (%) | −9.1 | 32.6 | 34.4 | 29.8 | 13.6 | 34.7 | 36.5 | 31.9 | −22.9 | −1.8 | 0 | −4.6 |
| HPs with sanitation facilities (%) | 28 | −21 | 7.5 | −5.2 | 7.9 | −22.9 | 5.6 | −7.1 | −2.8 | −33.6 | −5.1 | −17.8 |
| HPs having Cold box (%) | 11 | −1.8 | 13.2 | −1 | −3.04 | −5.8 | 9.2 | −5 | −19.6 | −22.4 | −7.4 | −21.6 |
| HPs having Oral Rehydration Salt (ORS) (%) | 3.9 | −25.4 | −0.1 | 4.9 | −18.1 | −30.4 | −5.1 | −0.1 | −27.1 | −39.4 | −14.1 | −9.1 |
| HPs with HEP guidelines: Family Health (%) | −31 | −9.7 | −34 | −16.2 | −42.7 | −10.3 | −34.6 | −16.8 | −56.3 | −23.9 | −48.2 | −30.4 |
| HPs with adequate supervision from HC (%) | −11 | 40 | 6.3 | 6 | 21.4 | 43 | 9.3 | 9 | −21.6 | 0 | −33.7 | −34 |
| Process: Service delivery | ||||||||||||
| HH members exposed to HEP service (%) | 27 | −37.2 | 8.8 | 31.1 | 8.5 | −38.1 | 7.9 | 30.2 | −21.7 | −68.3 | −22.3 | 0.0 |
| HHs ever been visited by HEWs (%) | 9.5 | −49.6 | −3.5 | 35.5 | −24.8 | −51.1 | −5 | 34 | −58.8 | −85.1 | −39 | 0.0 |
| HHs visited by HEWs in the last year (%) | 11 | −26.4 | 14.1 | 45.2 | −6.8 | −27.2 | 13.3 | 44.4 | −51.2 | −71.6 | −31.1 | 0.0 |
| Women who interacted with HEWs (%) | 27 | −33.4 | 13.4 | 35.9 | 11.6 | −34.1 | 12.7 | 35.2 | −23.6 | −69.3 | −22.5 | 0.0 |
| HHs with adopted HEP-targeted behavior (%) | 0.6 | −11.6 | −8.8 | 9.9 | −12.3 | −12.1 | −9.3 | 9.4 | −21.7 | −21.5 | −18.7 | 0.0 |
| Adolescent who interacted with HEWs (%) | 28 | −13.4 | 36.1 | 28.9 | 22.6 | −13.6 | 35.9 | 28.7 | −13.3 | −49.5 | 0.0 | −7.2 |
| Output: Service coverage | ||||||||||||
| Women received FP from HEWs/HP (%) | −18 | −56.7 | −12.7 | −2.08 | −7.21 | −56.52 | −12.59 | −1.95 | −18.4 | −67.7 | −23.7 | −13.1 |
| Women who attended their ANC-IV at HPs (%) | −24 | 62.2 | 3.8 | −10.7 | 0.6 | 62.6 | 4.2 | −10.3 | −62 | 0 | −58.4 | −72.9 |
| Women who received PNC from HEWs (%) | −39 | 6.8 | −3.7 | 46.7 | −35.9 | 6.9 | −3.6 | 46.8 | −82.7 | −39.9 | −50.4 | 0.0 |
| HHs which were visited by HEWs for IYCF (%) | 3.6 | −25.2 | 8.5 | 12.7 | −12.9 | −26 | 7.7 | 11.9 | −26.9 | −40 | −6.3 | −2.1 |
| Women educated on handwashing by HEWs (%) | 27 | −42.8 | −10.2 | 20.3 | 0.7 | −44 | −11.4 | 19.1 | −18.4 | −63.1 | −30.5 | 0.0 |
| Sick people who sought Rx from HP/HEW (%) | 50 | 24 | 43.8 | 22.8 | 68.4 | 24.5 | 44.3 | 23.3 | 0 | −43.9 | −24.1 | −45.1 |
RD = Rate Difference.
3.5. Disparities within Agrarian regions and DRS
Table 3 shows disparities within Agrarian regions and DRS. There were lower disparities within Agrarian regions than within DRS. Within Agrarian regions disparity was higher for output indicators whereas within DRS disparity was higher for process indicators. For input indicators of HEP implementation, the average index of disparity within DRS was almost six times higher than the average index of disparity within Agrarian regions. The average index of disparity of process indicators within DRS was about 12 times higher than the average index of disparity within DRS than in Agrarian regions. Similarly, the average index of disparity within DRS for output indicators of HEP implementation was nearly six times higher than the average index of disparity in Agrarian regions.
Table 3.
Disparities within Agrarian regions and DRS.
| RD from Agrarian average |
RD from DRS average |
ID within Agrarian | ID within DRS | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tigray | Amhara | Oromia | SNNPR | Afar | Somali | Gambela | B/Gumuz | |||
| Inputs: HP/HEWs | ||||||||||
| HPs with at least one level IV HEWs (%) | 15.6 | 3.7 | −0.4 | −7.3 | −12.8 | −0.5 | 33 | 18.8 | 0.04 | 0.29 |
| HPs with improved water source (%) | −6.4 | 3.1 | −3.6 | 2.4 | −9.1 | 12 | 13.8 | 9.2 | 0.05 | 0.14 |
| HPs with sanitation facilities (%) | 3.8 | −3.9 | −2.5 | 4.6 | 28 | −2.8 | 25.7 | 13 | 0.01 | 0.23 |
| HPs having Cold box (%) | 16.6 | −6 | −6.8 | −9.6 | 11.36 | 8.6 | 23.6 | 9.4 | 0.03 | 0.42 |
| HPs having Oral Rehydration Salt (ORS) (%) | 9 | 7.9 | −5 | −16.1 | 3.9 | −8.4 | 16.9 | 21.9 | 0.01 | 0.12 |
| HPs with HEP guidelines: Family Health (%) | 13 | 13.6 | −6.1 | 0 | −31.2 | 1.2 | −23.1 | −5.3 | 0.08 | 0.27 |
| HPs with adequate supervision from HC (%) | 11.1 | 14.9 | −1.3 | −11.4 | −10.9 | 10.7 | −23 | −23.3 | 0.07 | 0.14 |
| Process: Service delivery | ||||||||||
| HH members exposed to HEP service (%) | 11.8 | 5.9 | −9 | 8.3 | 27.2 | −19.4 | 26.6 | 48.9 | 0.07 | 0.47 |
| HHs ever been visited by HEWs (%) | 10.6 | 8.3 | −3.8 | −7.2 | 9.5 | −16.8 | 29.3 | 68.3 | 0.03 | 1.01 |
| HHs visited by HEWs in the last year (%) | 7.5 | 9.7 | −6.6 | −1.6 | 10.5 | −9.9 | 30.6 | 61.7 | 0.07 | 1.58 |
| Women who interacted with HEWs (%) | 7.5 | 6 | −8.3 | 8.1 | 26.8 | −18.9 | 27.9 | 50.4 | 0.06 | 0.53 |
| HHs with adopted HEP-targeted behavior (%) | 2.4 | 6.4 | −1.4 | −7.2 | 0.6 | 0.8 | 3.6 | 22.3 | 0.00 | 0.18 |
| Adolescent who interacted with HEWs (%) | 15.4 | 5.2 | −9.8 | 4.6 | 28 | −8.2 | 41.3 | 34.1 | 0.17 | 1.43 |
| Output: Service coverage | ||||||||||
| Women received FP from HEWs/HP (%) | −16.16 | −4.89 | −1.59 | 10.21 | −18.36 | −67.67 | −23.74 | −13.1 | 0.05 | 0.45 |
| Women who attended their ANC-IV at HPs (%) | −22.3 | −21.9 | 7 | 22.4 | −23.8 | 38.2 | −20.2 | −34.7 | 0.12 | 0.18 |
| Women who received PNC from HEWs (%) | 30.5 | −6.9 | −2.3 | −3.2 | −38.9 | 3.9 | −6.6 | 43.8 | 0.10 | 0.01 |
| HHs which were visited by HEWs for IYCF (%) | 14 | 9.5 | −7.1 | 3.3 | 3.6 | −9.5 | 24.2 | 28.4 | 0.17 | 0.89 |
| Women educated on handwashing by HEWs (%) | 11.8 | −4.7 | −4.3 | 11.6 | 27.2 | −17.5 | 15.1 | 45.6 | 0.07 | 0.64 |
| Sick people who sought Rx from HP/HEW (%) | 0.3 | −5.7 | 0.1 | 5.4 | 49.5 | 5.6 | 25.4 | 4.4 | 0.00 | 0.73 |
ID=Index of Disparity; RD = Rate Difference.
3.6. Aggregated DRS
When the four DRS are taken together, DRS had significantly lower HEP implementation in all indicators included in this study. Input indicators, process and output indicators were on average 27, 49, and 35 percentage points lower than best performing regions, respectively. Further assessment using average index of disparity from best performing region, however, showed that disparities in DRS were higher for output indicators followed by process indicators and input indicators. Relative rates of HEP implementation indicators in DRS to Agrarian average for percentage of HPs with improved water source, adequacy of supervision by Health centre, percentage of women received family planning, ANC and PNC services from HEWs and percentage of sick people who sought treatment from HPs were above 1. Details of disparity measures for DRS are shown in Table 4.
Table 4.
Disparity in DRS (aggregate) as compared to EAARS, national and best performing region.
| Rate difference |
Index of disparity |
RR: DRS/Agrarian | |||||
|---|---|---|---|---|---|---|---|
| From national | From Agrarian | From best | From national | From Agrarian | From best | ||
| Inputs: HP/HEWs | |||||||
| HPs with at least one level IV HEWs (%) | −28.9 | −31.8 | −47.4 | 0.19 | 0.34 | 0.47 | 0.51 |
| HPs with improved water source (%) | 20.6 | 22.7 | −13.8 | 0.81 | 1.17 | 0.12 | 1.91 |
| HPs with sanitation facilities (%) | −18.2 | −20.1 | −30.8 | 0.03 | 0.05 | 0.15 | 0.77 |
| HPs having Cold box (%) | −10.4 | −14.4 | −31 | 0.13 | 0.03 | 0.28 | 0.69 |
| HPs having Oral Rehydration Salt (ORS) (%) | −17 | −22 | −31 | 0.05 | 0.15 | 0.22 | 0.76 |
| HPs with HEP guidelines: Family Health (%) | −10.9 | −11.5 | −25.1 | 0.35 | 0.40 | 0.50 | 0.82 |
| HPs with adequate supervision from HC (%) | 29.3 | 32.3 | −10.7 | 0.20 | 0.43 | 0.24 | 1.67 |
| Process: Service delivery | |||||||
| HH members exposed to HEP service (%) | −17.8 | −18.7 | −48.9 | 0.12 | 0.03 | 0.30 | 0.70 |
| HHs ever been visited by HEWs (%) | −32.8 | −34.3 | −68.3 | 0.04 | 0.21 | 0.50 | 0.39 |
| HHs visited by HEWs in the last year (%) | −16.5 | −17.3 | −61.7 | 0.35 | 0.19 | 0.50 | 0.46 |
| Women who interacted with HEWs (%) | −14.5 | −15.2 | −50.4 | 0.19 | 0.11 | 0.32 | 0.73 |
| HHs with adopted HEP-targeted behavior (%) | −12.4 | −12.9 | −22.3 | 0.05 | 0.12 | 0.25 | 0.75 |
| Adolescent who interacted with HEWs (%) | −5.2 | −5.4 | −41.3 | 0.91 | 0.83 | 0.30 | 0.76 |
| Output: Service coverage | |||||||
| Women received FP from HEWs/HP (%) | 11 | 11.15 | 0.00 | 0.40 | 0.35 | 0.45 | 1.20 |
| Women who attended their ANC-IV at HPs (%) | 24 | 24.4 | −38.2 | 0.24 | 0.45 | 0.51 | 1.77 |
| Women who received PNC from HEWs (%) | 2.9 | 3 | −43.8 | 0.06 | 0.08 | 0.48 | 1.07 |
| HHs which were visited by HEWs for IYCF (%) | −15.7 | −16.5 | −30.5 | 0.00 | 0.16 | 0.43 | 0.44 |
| Women educated on handwashing by HEWs (%) | −25.3 | −26.5 | −45.6 | 0.03 | 0.17 | 0.38 | 0.51 |
| Sick people who sought Rx from HP/HEW (%) | 18.4 | 18.9 | −49.5 | 3.24 | 3.90 | 0.36 | 2.83 |
4. Discussion
The HEP has been a flagship community-based program of the Ethiopian Health system [20]. Our findings indicated that there are significant disparities in the implementation of HEP between DRS and Agrarian regions. Disparities in program inputs between DRS and national average seems to be associated with the disparities in process and output indicators. For instance, there was a substantial disparity in proportion of health posts with level IV HEWs in DRS as compared to national average. Consequently, process indicators such as number of households visited by HEWs and proportion of women educated on infant and young child feeding and handwashing practices by HEWs were very low in these regions.
Even within DRS, there were considerable disparities in the implementation of HEP. Benishangul-Gumuz region, considered as one of the DRS, had relatively higher values of HEP implementation indicators while Somali region had a relatively lower performance in most of the HEP indicators considered in this study. While DRS had low performance in many aspects of HEP implementation, there were some key areas where DRS were performing better. These include availability of sanitation facilities at health posts, adequacy of supervision of HEWs, proportion of maternal health service received at health posts and treatment of sick people at health posts.
There were remarkable but non-uniform improvements in health status over the past few decades across regions in Ethiopia (, 2022 #63). This study has shown that DRS in Ethiopia had lower overall health system performance in many of the HEP implementation indicators. This is also true for other health and health-related indicators. These regions have “hard-to-reach” populations for health service delivery [33]. Access to health services in these regions is also challenging due to distance and lifestyle of the population that involves mobility. Lack of awareness about benefits of HEP [34] also adds the problem. Moreover, HEP was introduced in DRS five to six years later in 2010 [19]. There were also some differences in the recruitment and training of HEWs in DRS. These factors, along with differences in leadership and governance and support from development partners could have contributed to the disparities between DRS and Agrarian regions, and even within DRS, in terms of HEP implementation indicators.
As there is still a significant disparity in HEP between DRS and Agrarian regions in most of HEP implementation indicators, there is a need to strengthen the current efforts that are targeted to ensure equitable implementation of HEP in DRS. The current policy direction of ensuring equity needs to be implemented as a priority. The findings of this study also imply that the implementation of HEP need to be tailored to the specific DRS. Moreover, further studies that consider a longitudinal approach are needed to explore and monitor trends in the implementation and outcomes of HEP in DRS.
Although, HEP indicators of access to and coverage of health services in DRS were relatively low, DRS were performing better in a few indicators, such as proportion of health posts with improved water source, proportion of health posts with adequate proportion and proportion of mothers who received family planning services from HEWs. In addition, the percentage share of HEP in access to and coverage of health services was relatively larger in DRS than in Agrarian regions. These differences may be due to better access of the population in Agrarian regions to other health service delivery options, including health centres, hospitals and private health facilities.
Implementation of HEP among DRS also varied significantly. Somali and Afar regions had lower levels of input indicators as compared to Benishangul-Gumuz and Gambella regions. In line with this, Benishangul-Gumuz and Gambella regions had better status of process and output indicators of HEP implementation. With regard to HEP implementation, Benishangul-Gumuz was similar to Agrarian regions as it had better status of implementation as compared to the other DRS.
Previous studies have explored the various factors that affect the utilization of health services in these regions. Demand side factors such as lack of awareness about the benefits health services, nomadic lifestyle, lack of trust in health workers and easy access to traditional healers were the main barriers to health service unitization in Afar region [34]. As health system related factors are critical in Somali region, the priority is health system strengthening [35]. Low literacy and negative attitude to health services were the main factors affecting health services utilization in Gambella region [36]. Similarly, poor health facility readiness, costs of health services, inaccessibility to health facilities, and cultural and traditional practices were barriers to health service utilization in Benishangul-Gumuz region [37].
The differences in HEP implementation and factors affecting health service utilization imply that a “one-size-fits-all” approach wouldn't be appropriate for the implementation of HEP in DRS. Benishangul-Gumuz region which had higher values of HEP implementation indicators would need a different approach as compared to other DRS regions. Somali region, with very low family planning coverage but relatively better proportion of ANC delivered by HEP would need a different approach in optimization of HEP implementation. Therefore, there needs to be a more contextualized approach that considers differences between regions and differences between indicators.
The implementation HEP in Ethiopia enabled the country to achieve significant improvements in access to and coverage of basic health promotion and disease prevention services [19]. The program was also found to be cost-effective in delivering community health services [18]. However, the disparities in the implementation would affect the benefits and the costs of the program across regions. A study conducted among Accredited Social Health Activists (ASHAs) in India has shown that work of ASHAs led to some positive health changes in the community though their capacities were limited by various health system and community factors [38]. Overall, community health programs improve healthcare access and equity in low- and middle-income countries [39]. To ensure this benefit, disparities in their implementation need to be reduced.
There are some limitations associated with this study. Firstly, the HEP assessment was a cross-sectional study and reflects the state of the indicators only at the time of the assessment. It didn't capture the variation in the pattern of the indicators across time. Secondly, most of the information collected from household members was self-reported and the possibility of social desirability bias cannot be ruled out. Thirdly, we have focused on selected indicators of implementation of HEP in Ethiopia and these may not reflect the implementation of HEP as a whole. Finally, the focus of this study was at regional levels and this may not reflect sub-regional differences in HEP implementation.
5. Conclusion
We found substantial interregional disparities in the implementation of HEP in Ethiopia. There are also significant disparities in the implementation of HEP between DRS and Agrarian regions. The level of disparity among DRS was also considerable. To achieve UHC, it is important that these disparities are addressed systematically and strategically with more attention on improving the implementation of HEP in DRS. Moreover, tailored approach to implementation need to be considered in DRS as the four DRS vary substantially. Further studies with a longitudinal data collection are needed to monitor the improvments in the implementation of HEP in Ethiopia.
Ethics approval and consent to participate
Ethical clearance to conduct the national HEP assessment was obtained from Ethiopian Public Health Institute. Informed consent to participate in the study was obtained from all the participants.
Consent for publication
Not applicable.
Availability of data and materials
Data used for this study are available from Ministry of Health, Ethiopia, subject to approval by Ministry of Health.
Funding
The national HEP assessment was funded by Bill and Melinda Gates Foundation.
Authors' contributions
TNH, YKA and AMT conceptualized the study and prepared the proposal. TNH and MAW conducted data analysis. TNH, YKA and MAW wrote the manuscript. All other authors provided substantial inputs into the manuscript. All authors approved the manuscript for submission.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to acknowledge the Ministry of Health, Bill and Melinda Gates Foundation, the study team and all study participants.
References
- 1.United Nations . 2015. Transforming Our World: 2030 Agenda for Sustainable Development. [Google Scholar]
- 2.WHO . International Conference on Primary Health Care; Alma-Ata, USSR: 1978. Declaration of Alma-Ata. [Google Scholar]
- 3.WHO Commission on Social Determinants of Health. and World Health Organization . Switzerland, World Health Organization, Commission on Social Determinants of Health; Geneva: 2008. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health : Commission on Social Determinants of Health Final Report. [Google Scholar]
- 4.World Health Organization . World Health Organization; Geneva: 1981. Global Strategy for Health for All by the Year 2000. [Google Scholar]
- 5.WHO . 2019. Global Health Observatory Data Repository: Health Equity Monitor Database. [Google Scholar]
- 6.World Health Organization . World Health Organization; Geneva: 2020. World Health Statistics 2020: Monitoring Health for the SDGs, Sustainable Development Goals. [Google Scholar]
- 7.Whitehead M. The concepts and principles of equity and health. Int J Health Serv. 1992;22(3):429–445. doi: 10.2190/986L-LHQ6-2VTE-YRRN. [DOI] [PubMed] [Google Scholar]
- 8.De Maeseneer J., Li D., Palsdottir B., Mash B., Aarendonk D., Stavdal A., et al. Universal health coverage and primary health care: the 30 by 2030 campaign. Bull World Health Organ. 2020;98(11):812–814. doi: 10.2471/BLT.19.245670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friebel R., Molloy A., Leatherman S., Dixon J., Bauhoff S., Chalkidou K. Achieving high-quality universal health coverage: a perspective from the National Health Service in England. BMJ Glob Health. 2018;3(6) doi: 10.1136/bmjgh-2018-000944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tulenko K., Møgedal S., Afzal M.M., Frymus D., Oshin A., Pate M., et al. Community health workers for universal health-care coverage: from fragmentation to synergy. Bull World Health Organ. 2013;91(11):847–852. doi: 10.2471/BLT.13.118745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.EPHI, MoH . 2019. Ethiopia Mini-Demographic and Health Survey Key Indicators. [Google Scholar]
- 12.Gebre E., Worku A., Bukola F. Inequities in maternal health services utilization in Ethiopia 2000-2016: magnitude, trends, and determinants. Reprod health. 2018;15(1) doi: 10.1186/s12978-018-0556-x. 119–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ministry of Health [Ethiopia] 2016. State of Inequity in the Ethiopian Health Sector. [Google Scholar]
- 14.Woldemichael A., Takian A., Akbari Sari A., Olyaeemanesh A. Inequalities in healthcare resources and outcomes threatening sustainable health development in Ethiopia: panel data analysis. BMJ Open. 2019;9(1) doi: 10.1136/bmjopen-2018-022923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Habtemariam M.K., Semegn S.T. Setting health sector priorities: a brief overview of Ethiopia's experience. Cost Effect Resource Allocat. 2018;16(Suppl. 1):46. doi: 10.1186/s12962-018-0117-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ministry of Health Ethiopia . Addis Ababa; Ethiopia, MOH: 2016. Health Sector Transformation Plan. [Google Scholar]
- 17.Norheim O.F. Ethical priority setting for universal health coverage: challenges in deciding upon fair distribution of health services. BMC Med. 2016;14:75. doi: 10.1186/s12916-016-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Assebe L.F., Belete W.N., Alemayehu S., Asfaw E., Godana K.T., Alemayehu Y.K., et al. Economic evaluation of Health Extension Program packages in Ethiopia. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0246207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Assefa Y., Gelaw Y.A., Hill P.S., Taye B.W., Van Damme W. Community health extension program of Ethiopia, 2003-2018: successes and challenges toward universal coverage for primary healthcare services. Global Health. 2019;15(1) doi: 10.1186/s12992-019-0470-1. 24–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Banteyerga H. Ethiopia's health extension program: improving health through community involvement. MEDICC Rev. 2011;13(3):46–49. doi: 10.37757/MR2011V13.N3.11. [DOI] [PubMed] [Google Scholar]
- 21.Medhanyie A., Spigt M., Kifle Y., Schaay N., Sanders D., Blanco R., et al. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res. 2012;12:352. doi: 10.1186/1472-6963-12-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mengesha W., Steege R., Kea A.Z., Theobald S., Datiko D.G. Can mHealth improve timeliness and quality of health data collected and used by health extension workers in rural Southern Ethiopia? J Public Health. 2018;40(suppl_2):ii74-ii86. doi: 10.1093/pubmed/fdy200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ministry of Health Ethiopia . Addis Ababa; Ethiopia, MOH: 2020. Realizing Universal Health Coverage Through Primary Health Care: A Roadmap for Optimizing the Ethiopian Health Extension Program 2020–2035. [Google Scholar]
- 24.Fetene N., Linnander E., Fekadu B., Alemu H., Omer H., Canavan M., et al. The ethiopian health extension program and variation in health systems performance: what matters? PLoS One. 2016;11(5):e0156438. doi: 10.1371/journal.pone.0156438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Calabrese S.K., Meyer I.H., Overstreet N.M., Haile R., Hansen N.B. Exploring discrimination and mental health disparities faced by black sexual minority women using a minority stress framework. Psychol Women Quart. 2015;39(3):287–304. doi: 10.1177/0361684314560730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.EPHI . 2018. Services Availability and Readiness Assessment (SARA) [Google Scholar]
- 27.Bobo F.T., Yesuf E.A., Woldie M. Inequities in utilization of reproductive and maternal health services in Ethiopia. Int J Equity Health. 2017;16(1):105. doi: 10.1186/s12939-017-0602-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yesuf E.A., Calderon-Margalit R. Disparities in the use of antenatal care service in Ethiopia over a period of fifteen years. BMC Pregnancy Childbirth. 2013;13(1):131. doi: 10.1186/1471-2393-13-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ethiopian Public Health Institute (EPHI) [Ethiopia] and ICF . Rockville; Maryland, USA, EPHI and ICF: 2019. Ethiopia Mini Demographic and Health Survey 2019: Key Indicators. [Google Scholar]
- 30.FMOH . 1993. Health Policy of the Transitional Government of Ethiopia. Addis Ababa. [Google Scholar]
- 31.Ministry of Health Ethiopia . Addis Ababa; Ethiopia, MoH: 2019. The National Assessment of the Health Extension Program. [Google Scholar]
- 32.Keppel K., Pamuk E., Lynch J., Carter-Pokras O., Kim I., Mays V., et al. Methodological issues in measuring health disparities. Vital Health Stat Series 2, Data Eval Methods Res. 2005;141:1–16. [PMC free article] [PubMed] [Google Scholar]
- 33.Gammino V.M., Diaz M.R., Pallas S.W., Greenleaf A.R., Kurnit M.R. Health services uptake among nomadic pastoralist populations in Africa: A systematic review of the literature. PLoS Negl Trop Dis. 2020;14(7):e0008474. doi: 10.1371/journal.pntd.0008474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ibrhim M.A., Demissie M., Medhanyie A.A., Worku A., Berhane Y. Reasons for low level of skilled birth attendance in Afar pastoralist community, North East Ethiopia: a qualitative exploration. Pan Afr Med J. 2018;30 doi: 10.11604/pamj.2018.30.51.14420. 51–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Warsame A., Handuleh J., Patel P. Prioritization in Somali health system strengthening: a qualitative study. Int Health. 2015;8(3):204–210. doi: 10.1093/inthealth/ihv060. [DOI] [PubMed] [Google Scholar]
- 36.Mitiku A.A., Dimore A.L., Mogas S.B. Determinants of home delivery among mothers in abobo district, gambella region, ethiopia: a case control study. Int J Reprod Med. 2020;2020:8856576. doi: 10.1155/2020/8856576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Agajie M., Abera S., Yimer E., Yaregal G., Muhidin A., Kelbessa W., et al. Barriers to maternal and child health care service uptake in assosa zone, benishangul gumuz region, ethiopia: a qualitative study. Int J Reprod Med. 2021;2021:5154303. doi: 10.1155/2021/5154303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sarin E., Lunsford S.S. How female community health workers navigate work challenges and why there are still gaps in their performance: a look at female community health workers in maternal and child health in two Indian districts through a reciprocal determinism framework. Hum Resour Health. 2017;15(1):44. doi: 10.1186/s12960-017-0222-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Javanparast S., Windle A., Freeman T., Baum F. Community Health Worker Programs to Improve Healthcare Access and Equity: Are They Only Relevant to Low- and Middle-Income Countries? Int J Health Policy Manag. 2018;7(10):943–954. doi: 10.15171/ijhpm.2018.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data used for this study are available from Ministry of Health, Ethiopia, subject to approval by Ministry of Health.