Abstract
Background
COVID-19 disrupted the TB prevention programme in the UK, especially for TB infection (TBI) care. We explore whether experience of the COVID-19 pandemic impacted on patients' perceptions of TBI and its treatment.
Methods
Semi-structured interviews were conducted as part of the Research to Improve Detection and Treatment of TBI (RID-TB) programme, exploring perceptual and practical barriers to TBI treatment. Nineteen people diagnosed with TBI were interviewed between August 2020 and April 2021. Recordings were transcribed and analysed using a constant comparative approach, allowing for a dynamic and iterative exploration of themes. Themes are organised using the Perceptions and Practicalities Approach.
Findings
Some participants perceived TBI as a risk factor for increased susceptibility to COVID-19, while some thought that treatment for TBI might protect against COVID-19 or mitigate its effects. Adaptations to TB services (e.g., remote follow-up) and integrated practices during the COVID-19 restrictions (e.g., medication being posted) addressed some practical barriers to TBI treatment. However, we identified beliefs about TBI and COVID-19 that are likely to act as barriers to engagement with TBI treatment, including: interpreting service delays as an indication of TBI not being serious enough for treatment and concerns about contracting COVID-19 in TB clinics.
Interpretation
COVID-19 and TBI service delays influence people's perceptions and practical barriers to TBI treatment adherence. Failure to address these beliefs may lead to people's concerns about their treatment not being fully addressed. Utilised service adaptations like remote consultations to address practical barriers may be relevant beyond COVID-19.
Funding
NIHR RID-TB Program (RP-PG-0217-20009).
Keywords: tuberculosis, LTBI, Covid-19, perceptions, health beliefs
1. Background
In 2014, the World Health Organization (WHO) launched the End-TB Strategy, with a long-term vision to eliminate TB and a time-bound target to reduce the global incidence of TB disease (to less than one per million) by 2035 [1]. Based on around 25% of the world's population being thought to be infected by TBI and up to 10% developing TB disease during their lifetime, TBI detection and treatment are recognized as a crucial global target for TB control [1,2]. This has led to an increased global emphasis on TB prevention. In low TB incidence countries (<100 TB cases per 100,000 per annum) where this is easier to both initiate and identify [3], the WHO and European Respiratory Society provided a priority framework to achieve this goal. It includes the adoption of targeted screening for active TB and TB infection in TB contacts and selected high-risk groups including migrants [3]. The WHO European Region was on track to reach 2020 targets, with a 19% reduction of TB incidence between 2015 and 2019 [1]. However, the COVID-19 pandemic has caused significant disruptions to healthcare systems globally, impacting on TB control in many countries [4]. For example, TB case notifications have decreased between 31% to 48%, indicating nondetection of cases in the European region between 2019 and 2020 [5], including countries with a low TB incidence. Compared to the pre pandemic period, during the pandemic TB patients presented later and with higher rates of disseminated TB [6]. TB modelling studies have estimated that a 25% reduction in TB detection for three months could result in a 13% increase in TB deaths [7]. This is aggravated by a reduction of preventive services, which have previously been effective in raising awareness and early detection of active cases [8].
The UK's successful national migrant TBI screening program was suspended in March 2020, and screening was only performed on a case-by-case basis for high-risk individuals, including contacts of TB [9]. This was followed by the largest decrease (12·3%) in TB notifications since UK TB surveillance was established in 2000 [10]. Despite the decrease in cases, the UK had the highest number (2·4%) of drug resistant TB in 2020 since the time such data were available [11]. Thus, the COVID-19 pandemic has been linked to a reduction in detection of TB and TBI cases globally [12], and an overall decrease in healthcare utilization [13].
The success of any TBI program depends on service integrity and relies on the patient adhering to the full prescribed treatment cascade [14,15]. The much-needed optimisation of this critical cascade [8,9,14,15] has been the focus of significant research investment in the UK, including the RID-TB program, which aims to improve access to diagnosis and enhance treatment uptake and completion in individuals with or at risk of TBI. The UK National Institute for Health and Care Excellence (NICE) guideline (CG76) highlights the importance of the Perceptions and Practicalities Approach (PaPA) as a framework to address nonadherence to treatment [16]. The PaPA suggests that any decisions about taking treatment are based on both perceptual (e.g., how much someone thinks they need the treatment and how concerned they are about it) and practical (e.g., how easy/convenient it is to follow the recommendation) factors [14]. Understanding people's perceptions of TBI and TBI treatment, and any practical barriers to accessing or taking treatment, is the first step to developing a person-centered adherence support program [14]. These perceptual factors, including how a person perceives their condition or illness and how they evaluate their personal need for treatment, influences the type of coping behaviors they choose to help them manage the health threat or illness (e.g., attending a clinical appointment, accepting a test, or adhering to treatment) [14,17].
During the pandemic, fear of acquiring COVID-19 may have prevented patients, including those with active TB, from attending medical appointments [18], increasing risk of TB treatment delays. Further, perceptions around the risks of COVID-19 may influence perceptions regarding TBI. Evidence from other co-morbid conditions suggests that people hold multimorbid representations, and that the interactions between these can affect perceived priorities for self-management and coping behaviors [19]. Given the importance of timely TB care and TB awareness and prevention activities, there is a need to understand how conflicting health threats and risk perceptions, including from other infections, such as COVID-19 may influence people's perceptions and behaviors around TBI care. Accordingly, in line with the PaPA framework, this qualitative study aimed to explore the perceptions and practicalities around COVID-19 and TBI among people eligible for TBI treatment in the UK, and to explore whether these perceptions and practicalities influenced attitudes to TBI, treatment, and experience of TBI care.
2. Methods
The study was conducted and reported in line with the Standards for Reporting Qualitative Research [20].
2.1. Study design
This was an in-depth qualitative study (RID-TB Q), which is part of a wider programme of work, the RID-TB programme (NIHR RP-PG-0217-20009). Part of the wider RID-TB programme was aimed to explore perceptions of TBI and its treatment to inform the content of an adherence support package. This qualitative study (RID-TB Q) contributed to this and provided a unique opportunity to understand how people with TBI internalise information about COVID-19 and how this might influence their perceptions of TBI treatment.
This study was approved by the London – Brent Research Ethics Committee (REC reference 19/LO/1546).
2.2. Study inclusion/exclusion criteria
Adults (<65 years) who were due to start, currently on, or had completed TBI treatment within the last 12 months in the UK, were eligible for inclusion in RID-TB Q. Adults (> 65) who were not eligible for TBI treatment within the last 12 months in the UK were not eligible to take part in the study.
2.3. Sampling strategy
Purposive sampling was used to recruit eligible participants representing a diverse range of perspective in terms of demographics, co-morbidities, and the TB referral and treatment pathway.
2.4. Data collection methods
Enrollment for the qualitative study commenced on August 3rd 2020, approximately five months after the COVID-19 pandemic was declared by WHO. In line with UK government restrictions, and the need for hospital sites to reduce foot traffic and face to face contact, all interviews were conducted remotely via telephone. Interviews were conducted by one researcher (ALC), a behavioural scientist with expertise in understanding perceptions of illness and treatment. Interviews were held in English as the study team did not have access to translators.
Participants were initially approached by a member of their clinical team either via telephone or face-to-face in clinic and were provided with a patient information sheet. Following this initial contact, participants who expressed an interest and provided verbal consent for the transfer of contact details were contacted via telephone by a researcher. For those willing to participate, the researcher took informed consent remotely in the presence of a witness via a 3-way conference call.
2.5. Data collection instruments and technologies
Topic guides (Appendix A) were developed in collaboration with Patient and Public Involvement (PPI) representatives who were affected by TB and informed by the Perceptions and Practicalities Approach (PaPA). Following the first semi-structured patient interview where COVID-19 was a key area of concern for the patient, the topic guide was expanded to explore perceptions around COVID-19 and perceptions of TBI and treatment. This included the addition of the following question: “Did COVID-19 influence your decision to take TBI treatment?”
2.6. Data processing
Data processing and analysis were facilitated by Nvivo 12. Interviews were audio-recorded using an encrypted device, managed on a secure server and professionally transcribed verbatim. Transcripts omitted any identifiable information to ensure anonymity.
2.7. Data analysis
This qualitative study utilized inductive thematic analysis with a phenomenological approach [21] to explore the lived experiences of people with TBI during COVID-19 to gain deeper insights into how TBI care was experienced and interpreted. Thus, research findings would describe the actual experiences of people who engaged with TBI care pathways during COVID-19 where relatively objective representation of the phenomenon could be provided. Accordingly, applying thematic analysis, data were analyzed using a constant comparison approach [22], fitting the need for an iterative process between data collection and analysis, which was required to inform the ongoing formative research for intervention development as part of the RID-TB program.
This approach allowed us to identify key themes inductively, moving between transcripts and making iterative revisions to themes as new insights emerged from the data. As each transcript became available it was checked by several researchers for completeness, read several times, and open coded. Emerging themes related to patient perceptions of COVID-19 and TBI were discussed within the research and clinical team and presented to the patient advisory group to gain contextual insight. Early themes were conceptualized within the Necessity – Concerns Framework [23] and Perceptions and Practicalities Approach [14], validated theories which explain how necessity beliefs (i.e., the degree to which a patient perceives that they need the perceived benefits associated with a treatment), treatment concerns (i.e., perceived negative consequences associated with treatment), and practical barriers are related to adherence behaviours [23]. Those theoretical frameworks were chosen to interpret the rich narratives provided by people with TBI in a structural manner on the engagement with TBI care pathways. Thus, interpretation of their experiences would be easily transformed into the clinical practice. Followingly, an initial coding framework was developed, which was subsequently applied to all transcripts, with themes refined throughout. Transcripts were coded and categorized according to the framework until data saturation was reached.
2.8. Techniques to enhance trustworthiness
Transcripts were open coded by ALC, and themes were cross checked by two independent researchers. Also, purposive sampling was applied to enhance transferability and generalizability of findings.
3. Findings
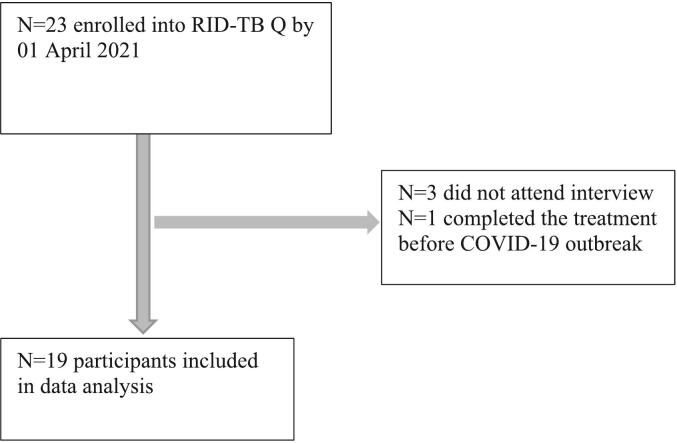
By April 2021, 23 patients were enrolled. Of these 19 were interviewed for the purpose of the present study (Fig. 1). The interviews were conducted between August 2020 and April 2021 and lasted between 17 and 60 min. The participant sample included 13 men and six women, of which four had not yet started TBI treatment, ten were currently on TBI treatment, and five had completed TBI treatment. The majority of participants were from Asian backgrounds (n = 12, 63%), followed by Black (n = 5, 26%) and White (n = 2, 11%) ethnicities, respectively. Participant characteristics are shown in Table 1.
Fig. 1.
Participant flow diagram.
Table 1.
Participant characteristics.
| Participant Characteristics | Participants N = 19 |
|---|---|
| Gender, n (%) | |
| Male | 13 (68%) |
| Female | 6 (32%) |
| Age (years), median IQR | 36 (26–51) |
| Ethnicity (NHS Code), n (%) | |
| Asian or Asian British (Indian/Pakistani/Bangladesh or another other Asian background) | 12 (63%) |
| Black, Black British, Caribbean or African (Caribbean/ African or another black background) | 5 (26%) |
| White (British/Irish or any other white background) | 2 (11%) |
| Region of birth, n (%) | |
| South Asia (India, Pakistan & Afghanistan) | 10 (53%) |
| Sub-Saharan Africa (Ghana, Nigeria & Somalia) | 5 (26%) |
| Europe (UK & Republic of Ireland) | 4 (21%) |
| If migrated, years living in the UK, median IQR | 15 (7–27 years) |
| Indication for TBI treatment, n, (%) | |
| TB Contact | 7 (37%) |
| Patients requiring biological therapies and those who have had a transplant | 5 (26%) |
| National TBI migrant Screening Program | 3 (16%) |
| Symptom investigation (e.g., cough) | 2 (11%) |
| Occupational health screening for health care worker | 2 (11%) |
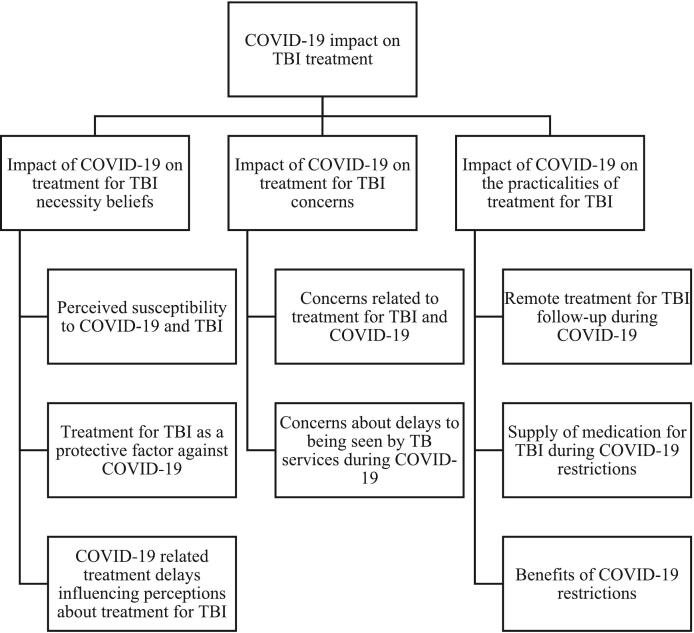
We report findings from the patient's perspective of how COVID-19 influenced their beliefs about TBI and its treatment. Perceptions about TBI treatment are conceptualized within the Necessity - Concerns framework and Perceptions and Practicalities Approach [23]; highlighting the interaction between COVID-19 and beliefs about personal need for TBI treatment, treatment concerns, and any practical barriers to taking TBI treatment [14]. Results generated three interlinked themes and eight sub-themes (Fig. 2).
Fig. 2.
Overview depicting the themes showing how COVID-19 impacted on treatment for TBI and experience of TBI care.
3.1. Theme 1. Impact of COVID-19 on treatment for TBI necessity beliefs
3.1.1. Perceived susceptibility to COVID-19 and TBI
TBI was perceived by most participants as an underlying illness that would increase their vulnerability to contracting COVID-19 and the likelihood of suffering severe disease. Participants described how their perceptions had been influenced by the media, and in the case of one participant their interpretation of medical journals and government reports.
“…if you have something [TBI] already in your system there are high risks of you getting it [COVID-19], high risk of you not getting it, but if you get it that would bring more problems to you, if you have this and COVID so they call this conversion of crisis [being co-infected with COVID-19 and TBI].”
Participant 05, 31 years old male currently on TBI treatment.
“…I was like you know this change in my blood test, do you think it is because I had coronavirus… the doctor said that it is nothing to do with [it], TB and coronavirus, so it's two different things”.
Participant 17, 40 years old male yet to start TBI treatment.
Participants questioned how their body would cope with a co-infection (TBI and COVID-19) and what the consequence of this might be for their health. This concern was heightened among those who were already immunocompromised because of another comorbidity or treatment.
“…I do have an underlying health condition [so] it [TBI] did make me worried…because of COVID and my body is already immunosuppressed, if I were to get something it would be harder for me to fight it off… it did make me sort of think twice and maybe be a bit sort of cautious … thinking twice about if I was to get ill or catch an infection, my ability [for]my body sort of fighting it if I had some sort of latent TB”.
Participant 10, 23 years old male completed TBI treatment.
3.1.2. Treatment for TBI as a protective factor against COVID-19
Patient's beliefs about their low personal resilience against COVID-19 appeared to enhance perceived necessity for TBI treatment. Some participants viewed TBI treatment as something that would protect their health in general.
“Yeah, if you are not on treatment, I'm sure you can really get this COVID-19 bad, but if you are I don't think anything will [happen], and you will have that peace of mind … I wouldn't want to leave this world because of COVID and I think drugs will help”.
Participant 02, 30 years old female currently on TBI treatment.
One participant held concerns about their risk of COVID-19 should they stop the treatment, indicating perceived susceptibility to COVID-19 as a potential driver of TBI treatment adherence.
“Yeah, well, this Corona [COVID-19] goes into your lungs mostly. So, what I am treating is the lung. I even was thinking recently, when I stop this medication, will that make me more vulnerable to the corona [COVID-19]. Just something that pops to mind”.
Participant 14, 54 years old male completed TBI treatment.
3.1.3. COVID-19 related treatment delays influencing perceptions about treatment for TBI
One participant in particular felt that service delays could be misinterpreted as TBI not being serious enough to treat.
“…if the people who are dealing with it aren't treating it in a way that is serious like if for me as a patient I don't feel the seriousness from the people who are dealing with my treatment... So when it comes to me being told later ‘oh you have to take the medicines because you don't want to get TB’, I just kind of think oh it's not that serious because my appointment came after two months and nobody even called me to say my test was positive…”.
Participant 06, 26 years old female yet to start TBI treatment.
3.2. Theme 2: Impact of COVID-19 on treatment for TBI concerns
3.2.1. Concerns related to treatment for TBI and COVID-19
While the majority of participants viewed TBI treatment as protective, one participant described concerns about how treatment might affect their immune system, and worried that taking treatment might increase their susceptibility to serious illnesses like COVID-19.
“I'm worried about my immune system would it [TBI treatment] weaken my immune system in anyway? It is just because of the time we're in like COVID-19, it feels like it would put you at more risk, in terms of health”.
Participant 01, 22 years old female yet to start TBI treatment.
3.2.2. Concerns about delays to being seen by TB services during COVID-19
Participants described delays in receiving an TBI diagnosis and starting treatment which they perceived to be a consequence of COVID-19 restrictions. While some participants felt this was to be expected, others felt frustrated with the service, feeling as though TBI treatment delays were putting them at risk of active TB.
“…if I had latent TB and then it became active in that time, and literally I am putting myself at risk during this time [of ongoing COVID-19 pandemic], so what would be the point of them giving me medicine at this time when they have exposed me to risk in that whole time.”
Participant 06, 26 years old female yet to start TBI treatment.
One participant also spoke of her experience of treatment delays for her husband with active TB, describing how this had led to financial hardship for them as a family.
“The [TB] treatment was started very late [for husband]. If the treatment was started on time, you know, we might have treated it already. It might not have affected our normal lives. We might have been back to work … after 3 months of sickness he was admitted to the hospital … we were given appointments [TBI testing] after one and a half months. So that kind of pissed us off.”
Participant 12, 38 years old female currently on TBI treatment.
Frustrations related to service delays were most common among contacts, who described feeling dissatisfied with the level of communication, and felt that reasons for delays were not explained.
“They should have started the treatment earlier. This delay was at least six to five months … they never explained … they did not explain why it was late.”
Participant 12, 38 years old female currently on TBI treatment.
Participants described how the majority of their contact with the TB service has been conducted remotely. Some participants who did attend clinic described concerns about entering a setting which they perceived as a hotspot for COVID-19 exposure. However, in general participants were not deterred from attending, and felt reassured following their clinic visit.
“…when I started my medication the COVID-19 was on the peak … even my friends and my wife all had this concern in the back of our minds … we are going physically to the NHS and this test cannot be done on a virtual thing … I was thinking … what if someone has this [COVID-19] … and what if you get it? So this was always on my mind … I would go to surgery with my mask on and sanitise everything, I was ready, but they were even ultra-ready in the specialty [TB service].
Participant 05, 31 years old male currently on TBI treatment.
3.3. Theme 3. Impact of COVID-19 on the practicalities of TBI treatment
3.3.1. Remote TBI treatment follow up during COVID-19
Remote follow up was a strategy adopted by TB services to reduce footfall in the hospital during the COVID-19 pandemic. The majority of participants felt this was convenient and that they were well supported by nursing staff.
“…it was easier [appointments] to be done on the phone. I did not feel that I was any less treated or maltreated because it mostly was on the phone”.
Participant 11, 42 years old male completed TBI treatment.
3.3.2. Supply of TBI medication during COVID-19 restrictions
Participants also described how the TB service supported their ability to take treatment during COVID-19 by posting medications and ensuring they had a full supply to avoid additional visits.
“…they [TB service] made sure I had plenty of medication, it wasn't something that I had to chase”.
Participant 09, 49 years old male completed TBI treatment.
3.3.3. Benefits of COVID-19 restrictions
Some participants felt that government restrictions for COVID-19 had positively impacted on their experience of taking TBI treatment, with isolation and lockdown making it easier to conceal their diagnosis and more convenient to take treatment, as well as reducing any perceived risk of spreading TB.
“I guess for me, it was just because I was at home, it was in lockdown, it was just convenient for me to do it [take treatment]”.
Participant 10, 23 years old male completed TBI treatment.
“I feel like if it wasn't [for] COVID-19 then you kind of have to tell certain people especially if you are exposing yourself to them before and during if you are contagious”.
Participant 06, 26 years old female yet to start TBI treatment.
4. Discussion
This is the first study to explore the impact of the COVID-19 pandemic on TBI services in the UK, from the perspective of people eligible for TBI treatment. Our study included a representative sample of people with different demographics and at different stages of treatment for TBI, increasing the generalizability of our findings. We found that COVID-19 may have influenced perceptions and practicalities around starting and continuing with treatment for TBI, with potential implications beyond the context of COVID-19. Interviews highlighted that COVID-19 communications, possibility of co-infection (TBI and COVID-19) and similarities in acquisition for both conditions increased awareness towards TBI, where completing TBI treatment being reviewed as a protective factor against the COVID-19. Thus, viewing TBI treatment as beneficial for general health may enhance perceptions of personal need for TBI treatment. Meanwhile, TB service disruptions due to COVID-19, such as delays to being seen by TB clinics, were interpreted by some people as a sign that the disease was not important enough to be prioritized, which may lead to decreased perceived need for TBI treatment and increased concerns once the treatment is offered. In the post COVID-19 context, people may still hold those negative perceptions and may be less likely to involve in TB clinics. Further, the adaptation of remote consultations during the COVID-19 and the increased convenience of accessing TBI medication, such as having it mailed to the patient, may offer alternative and convenient solutions for TBI care post COVID-19. Accordingly, this work highlights the importance of delivering person-centered care and understanding and addressing unique perceptual and practical barriers to TBI treatment adherence.
We found there to be considerable interaction between participant's perceptions of COVID-19 and TBI. To understand the relationship between perceptions of health and illness with treatment adherence, we can look to the Common Sense Model [24] and Necessity ∼ Concerns Framework [23] which describe how people form representations around illness (or health threats) and their treatment. These models suggest that adherence behavior is related to a patients' common-sense representations of the illness and treatment. For example, patients in this study who perceive that their TBI may have put them at increased risk for severe COVID-19 may believe more strongly in the importance of their TBI treatment, as they see this as a way of reducing the risk of COVID-19, as well as TBI. These people may be more likely to adhere to their TBI treatment. However, treatment adherence may be lower among those who hold concerns or misperceptions about the safety of TBI treatment. For example, one patient saw their TBI treatment as something that could damage the immune system and impair the body's ability to fight infection, therefore putting them at increased risk of COVID-19. These perceptions could lead to lower levels of TBI treatment acceptance and completion. This has been observed in other conditions, with higher recorded levels of voluntary suspension of medicines (e.g., psoriatic patients) following COVID-19 announcements [25]. Our findings highlight the importance of considering how patients' beliefs about other health threats may influence their perceptions about TBI treatment, and the need to ensure that tailored information (with education) is available for people starting treatment.
COVID-19 disrupted TB service provisions in the UK [26], resulting in delayed appointments, diagnosis, and treatment, which negatively impacted patient experience. This study highlights the risk of patients internalizing service delays, and misinterpreting this to view TBI less seriously as their care is postponed, leading to some participants questioning their personal need for treatment. Treatment delays of greater than one month following the communication of a positive diagnosis were previously shown to predict poorer treatment acceptance rates in the evaluation of the National latent tuberculosis infection testing and treatment programme [27]. In the event of future TB service delays, increased efforts should be taken to communicate the importance of treatment for TBI and explain the reasons for delays. This can be achieved by providing timely contact with the patient (e.g., phone call by nurse) to address any concerns of the patient may have about care and treatment delays, updating the patients about when they were likely to be treated, and providing information leaflets in multiple languages. In contrast, other service changes (e.g., remote follow-up and home postal delivery of TBI treatment) reduced practical barriers to adherence and were deemed acceptable and convenient in comparison to face-to-face care. This is promising for the future and may present a suitable alternative treatment model. However, remote care may not be suitable for all participants, especially the vulnerable and underserved where limited access to IT technologies, language barriers, and cultural interpretations of disease and health could limit engagement with healthcare services [28,29].
There were also some positive consequences of the COVID-19 pandemic response on TBI. Government restrictions in response to COVID-19 (e.g., isolating, working from home or attending remote consultations) made it easier for patients to self-manage their treatment and medication side effects by being at home and not needing to disclose their TBI diagnosis to others [30]. Some patients felt less pressure to disclose their diagnosis in their communities due to them isolating or working from home which meant they were not interacting with others in their communities. Previous research has shown that concealment of TBI diagnosis and treatment is a behavior enacted by patients wanting to avoid anticipated stigma [31]. TB stigma is known to be linked to diagnostic delays, decreased treatment adherence, continued transmission of TB within the community, and increased morbidity and mortality [32]. Thus, integrating remote consultation appointments into routine care may be advantageous within the post-COVID-19 context, which can provide an alternative strategy to decrease the burden of anticipated stigma. However, the COVID-19 response and the unknowns around COVID-19 have also given rise to an increase in stigma and discrimination around COVID-19 [33], which could also act as an additional barrier to TBI patients seeking care. It is also important to note that being managed remotely by clinical services increased the potential risk of side effects undetected as patients were not accessing face-to-face clinical care.
While there is no evidence to suggest that TBI is an independent risk factor for increased vulnerability to experiencing severe COVID-19 [34], this study highlights that patients perceive the two conditions to be inter-related. This raises issues related to communication and information giving during a public health emergency. Participants in the current study held misperceptions about their own personal susceptibility and vulnerability based on messages about increased risks for people with underlying conditions. Furthermore, some participants had concerns about taking treatment for TBI, believing that it might negatively impact on their immune function, and so increasing their risk of severe COVID-19. Furthermore, participants perceived a lack of communication regarding service delays, which also led to the misinterpretation that TBI is not serious, and as such treatment is not a priority, impacting future treatment decisions. This shows how ‘blanket’ public health information can be misinterpreted by individuals, and how communication which does not address beliefs about TBI or its treatment can lead to doubts in treatment necessity, and unaddressed treatment concerns.
4.1. Limitations
COVID-19 was an unanticipated theme in our qualitative study, and as such our topic guide was not designed to explore other potential areas of interest such as how perceptions of TBI might influence willingness to have the COVID-19 vaccine. While the aim of qualitative research is not to generalize, it should be noted that some of the participants in this study may have been more at risk of developing TB or severe COVID-19, than others with TBI. This is a consequence of the time during which participants were recruited, whereby TB services in the UK were mandated to only treat TBI in individuals at high risk of progression to active TB (e.g., contact of a smear-positive index case, or patients awaiting to commence biological therapies for another severe condition such as connective-tissue disease). Our findings may only be generalizable to high-income countries where COVID-19 service practices were similar to the UK. Also, non-English speaking people, one of the main target groups for TBI screening in the UK, and those without IT infrastructure and skills could not be included in the interviews, limiting our findings' relevance to more vulnerable people with TBI. Even though the appearance of the repeated themes through the interviews suggests that saturation is reached, the imbalance in participants' gender and ethnicity could make saturation an issue. Further, considering the distressful nature of the pandemic timeline and being at different stages of treatment for TBI, participants might experience recall bias regarding their interaction with TB services. However, despite these limitations, we believe that this study offers novel insights from the patient's perspective on the impact of COVID-19 on TBI care and furthers our understanding of people with TB infection's unmet needs.
5. Conclusion
This study has shown that the impact of COVID-19 on UK TB services may have influenced patients' perceptions of TBI and its treatment, especially where changes in TB services (e.g., delays to TBI diagnosis and treatment initiation) may result in decreased personal need of treatment and increased concerns. Those changes in one's perceptions during COVID-19 may have long lasting effects on TB prevention and how public health interventions are being perceived by decreasing one's motivation and ability to start and continue TBI treatment in the post COVID-19 context. Results also highlight how perceptions of TB care can be influenced by perceptions around other relevant long-term conditions or health threats. Therefore, it is important to consider patients' beliefs about TB and treatment, and how these might be affected by factors like adaptations and disruptions to care or competing illness priorities. Participants viewed remote care during the pandemic as an acceptable alternative to face-to-face care, with some participants finding it more convenient, providing insights for future strategies to improve patient experience of treatment follow-up, such as providing hybrid care (e.g., electronic reminder Dossett boxes). Delays to TBI diagnosis and treatment initiation, resulting from service disruption, could negatively impact on perceived TBI treatment need. Strategies are required to support TBI patients in terms of engagement with the TB service and treatment, beyond the COVID-19 pandemic.
CRediT authorship contribution statement
Ayşenur Kılıç: Formal analysis, Writing – original draft, Writing – review & editing. Amy L. Clarke: Conceptualization, Data curation, Formal analysis, Writing – original draft. Zoe Moon: Formal analysis, Writing – original draft, Writing – review & editing. Yohhei Hamada: Data curation, Writing – original draft, Writing – review & editing. Amy Hai Yan Chan: Conceptualization, Data curation, Formal analysis, Writing – review & editing. Ananna Rahman: Data curation, Writing – review & editing. Charlotte Layton: Data curation, Project administration, Writing – review & editing. Chris J. Griffiths: Conceptualization, Writing – review & editing. Dominik Zenner: Conceptualization, Writing – review & editing. Ellen Powell: Project administration, Writing – review & editing. Heinke Kunst: Data curation, Writing – review & editing. Marc Lipman: Conceptualization, Data curation, Writing – review & editing. Mike Mandelbaum: Formal analysis, Writing – review & editing. Padmasayee Papineni: Data curation, Writing – review & editing. Tessa Tattersall: Project administration, Writing – review & editing. Trinh Duong: Data curation, Writing – review & editing. Ibrahim Abubakar: Conceptualization, Funding acquisition, Writing – review & editing. Molebogeng X. Rangaka: Conceptualization, Funding acquisition, Writing – review & editing. Robert Horne: Conceptualization, Formal analysis, Funding acquisition, Supervision, Writing – review & editing.
Declaration of Competing Interest
None.
Acknowledgement
The funding body of this study (NIHR RID-TB Program [RP-PG-0217-20009]) have no involvement in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
AK has been supported for her independent research by the Türkiye Ministry of National Education. Please note that the supporter has no involvement in the project.
Appendix A. RID-TB-Q Semi-structured interview topic guide
A.1. Introduction
Firstly, I/We would like to welcome you to the interview and thank you for agreeing to speak to us.
We are doing this because we want a better understanding of how latent TB affects people, and about their experience of testing and treatment. This will help us improve care and services for the future.
Just to remind you, this interview is confidential and anonymous. It will not be shared with your doctors, nurses or anyone involved in your care. We would like to record the conversation if that is ok with you? This means we can focus on listening to you, rather than having to take notes.
Do you have any questions before we start?
A.2. Introductions
-
-
Please can you tell me a little bit about yourself or how you have come to be here today? Prompts: perceptions of current health, length of time in country, family and living situation)
A.3. Testing
-
-
What does latent TB mean to you?
-
-
Prompt: cause, consequence, timeline, control, coherence, differs from active TB
-
-
How familiar are you with latent TB?
-
-
Prompt: previous knowledge, family members tested or diagnosed
-
-
How did you come to get tested?
Prompt: decision making easy/hard
-
-
What do you feel about your test result?
Prompt: clear picture/ understanding what it means to you, surprise/ not surprised, concerns around the test or diagnosis, how was it waiting for the results?
-
-
Has anything changed in your life as a result of your latent TB diagnosis?
Prompt: what's different now?
Let's move on to talk about the treatment…
What does the treatment mean to you?
Prompt questions:
-
-
How do you feel about it?
-
-
How important do you think treatment is for latent TB?
-
-
Were you aware that you might need medicines? (Where did this information come from?)
-
-
Do you have any concerns about your treatment?
-
-
Have you spoken to anyone about your treatment?
-
-
How easy do you think it will be to take it?
-
-
Do you foresee any problems taking it?
-
-
Have you considered not starting your medication?
If you have started treatment…
-How did you decide that taking medicines was right for you?
Prompt: importance of prescription, how you have been feeling on treatment, how easy/difficult treatment has been and if this differs to expectations.
-Have there been particular times where it has been difficult to take it?
Prompt: what happened, what could have been done, what the consequences were e.g. missing a dose, thoughts about stopping, what happened next.
A.4. Service
-
-
Has anything helped you to take your medicines?
Prompt: who explained your medicines and how, what could have been done better, how might we improve things for future people?
-
-
Can you tell me a little bit about how you take your medicines now?
Prompt reflection: it seems like you are able to take them regularly, what do you think has helped you to do this OR it sounds like you are have experienced some difficulties, can you think of anything that could be done to help?
A.5. Intervention development
We would like to develop a programme to help people with latent TB to get the most out of their medicines.
-
-
Where do you find/look for information about latent TB infection?
Prompt: presentation of information, further questions, anything else that you would like to have known about testing or treatment.
-
-
You mentioned earlier that (insert barrier or perceived barrier from above) made it difficult/ might make it difficult to take medicines. Can you think of anything that might help?
-
-
Prompt: information, diary, and support emotional and practical
A.6. Summary questions
-
-
What do you think is the most important barrier to people taking latent TB medicines?
-
-
What do you think is the most important reason for people to get tested for latent TB?
-
-
What would you consider an important reason for taking latent TB medicines?
-
-
What could be a key factor in making this experience better for you or others in a similar position? (i.e. something we could do to help)
-
-
Anything else you would like to say/ any questions?
-
-
Is there anything you feel we have missed out or thought we would cover that you would like to discuss?
References
- 1.World Health Organization (WHO) WHO; Geneva: 2022. Global Tuberculosis Report 2022 [Internet] [cited 2023 Oct 20]. Available from: https://iris.who.int/bitstream/handle/10665/363752/9789240061729-eng.pdf?sequence=1. [Google Scholar]
- 2.Houben R.M., Dodd P.J. The global burden of latent tuberculosis infection: a re-estimation using mathematical modelling. PLoS Med. 2016 Oct 25;13(10) doi: 10.1371/journal.pmed.1002152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matteelli A., Rendon A., Tiberi S., Al-Abri S., Voniatis C., Carvalho A.C.C., et al. Tuberculosis elimination: where are we now? Eur Respir Rev. 2018 Jun 30;27(148) doi: 10.1183/16000617.0035-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeong Y., Min J. Impact of COVID-19 pandemic on tuberculosis preventive services and their post-pandemic recovery strategies: A rapid review of literature. J Korean Med Sci. 2023 Feb 6;38(5) doi: 10.3346/jkms.2023.38.e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dara M., Kuchukhidze G., Yedilbayev A., Perehinets I., Schmidt T., Van Grinsven W.L., et al. Early COVID-19 pandemic’s toll on tuberculosis services, WHO European Region, January to June 2020. Eurosurveillance. 2021 Jun 17;26(24):2100231. doi: 10.2807/1560-7917.ES.2021.26.24.2100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barrett J., Painter H., Rajgopal A., Keane D., John L., Papineni P., et al. Increase in disseminated TB during the COVID-19 pandemic. Int J Tuberc Lung Dis. 2021 Feb 1;25(2):160–166. doi: 10.5588/ijtld.20.0846. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO) 2020 May. Information Note Tuberculosis and COVID-19 [Internet] [cited 2021 Aug 4]. Available from: https://www.who.int/docs/default-source/documents/tuberculosis/infonote-tb-covid-19.pdf. [Google Scholar]
- 8.Loutet M.G., Burman M., Jayasekera N., Trathen D., Dart S., Kunst H., et al. National roll-out of latent tuberculosis testing and treatment for new migrants in England: a retrospective evaluation in a high-incidence area. Eur Respir J. 2018;51(1):1701226. doi: 10.1183/13993003.01226-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.NHS England . 2020. NHS England COVID-19: Provision of tuberculosis services update [Internet] [cited 2021 Jun 4]. Available from: https://www.england.nhs.uk/publication/covid-19-provision-of-tuberculosis-services-update/ [Google Scholar]
- 10.UK Health Security Agency . 2023. TB incidence and epidemiology in England, 2021 [Internet] [cited 2023 Jul 26]. Available from: https://www.gov.uk/government/publications/tuberculosis-in-england-2022-report-data-up-to-end-of-2021/tb-incidence-and-epidemiology-in-england-2021#about-this-report. [Google Scholar]
- 11.UK Health Security Agency [Internet] 2021. Press release, Learning from pandemic will be vital in UK’s fight to eliminate TB after temporary 2020 drop in cases [cited 2023 Jul 26] Available from: https://www.gov.uk/government/news/learning-from-pandemic-will-be-vital-in-uk-s-fight-to-eliminate-tb-after-temporary-2020-drop-in-cases. [Google Scholar]
- 12.Migliori G.B., Thong P.M., Akkerman O., Alffenaar J.-W., Álvarez-Navascués F., Assao-Neino M.M., et al. Worldwide effects of coronavirus disease pandemic on tuberculosis services, January-April 2020. Emerg Infect Dis. 2020 Nov;26(11):2709–2712. doi: 10.3201/eid2611.203163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moynihan R., Sanders S., Michaleff Z.A., Scott A.M., Clark J., To E.J., et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021 Mar 16;11(3) doi: 10.1136/bmjopen-2020-045343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horne R., Cooper V., Wileman V., Chan A. Supporting adherence to medicines for long-term conditions. Eur Psychol. 2019 Jan;24(1):82–96. [Google Scholar]
- 15.The National Institute for Health and Care Excellence (NICE) 2009 Jan. Medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence. [PubMed] [Google Scholar]
- 16.Nunes V., Neilson J., O’flynn N., et al. Vol. 364. National Collaborating Centre for Primary Care and Royal College of General Practitioners; London: 2009. Clinical Guidelines and Evidence Review for Medicines Adherence: involving patients in decisions about prescribed medicines and supporting adherence. [PubMed] [Google Scholar]
- 17.Horne R., Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999 Dec;47(6):555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 18.Mwamba C., Kerkhoff A.D., Kagujje M., Lungu P., Muyoyeta M., Sharma A. Diagnosed with TB in the era of COVID-19: patient perspectives in Zambia. Public Health Action. 2020 Dec 21;10(4):141–146. doi: 10.5588/pha.20.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mc Sharry J., Bishop F.L., Moss-Morris R., Kendrick T. ‘The chicken and egg thing’: Cognitive representations and self-management of multimorbidity in people with diabetes and depression. Psychol Health. 2013;28(1):103–119. doi: 10.1080/08870446.2012.716438. [DOI] [PubMed] [Google Scholar]
- 20.O’Brien B.C., Harris I.B., Beckman T.J., Reed D.A., Cook D.A. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014 Sep;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 21.Sundler A.J., Lindberg E., Nilsson C., Palmér L. Qualitative thematic analysis based on descriptive phenomenology. Nurs Open. 2019 Jul;6(3):733–739. doi: 10.1002/nop2.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glaser B.G. The constant comparative method of qualitative analysis. Soc Probl. 1965 Apr;12(4):436–445. [Google Scholar]
- 23.Horne R., Chapman S.C., Parham R., Freemantle N., Forbes A., Cooper V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the Necessity-Concerns Framework. PloS One. 2013 Dec 2;8(12) doi: 10.1371/journal.pone.0080633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leventhal H., Diefenbach M., Leventhal E.A. Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cognitive Therapy Res. 1992;16(2):143–163. [Google Scholar]
- 25.Bernardini N., Skroza N., Spagnoli A., Marchesiello A., Balduzzi V., Tolino E., et al. How lockdown measures, during COVID-19 pandemic, matter on psoriatic patient’s perception: Study on 600 patients on biologic therapy. J Infect Public Health. 2021 Jul;14(7):878–882. doi: 10.1016/j.jiph.2021.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morrison H., Perrin F., Dedicoat M., Ahmed R., Brown J., Loughenbury M., et al. Impact of COVID-19 on NHS tuberculosis services: Results of a UK-wide survey. J Infect. 2023 Jul 1;87(1):59–61. doi: 10.1016/j.jinf.2023.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.NHS England and NHS Improvement . Mar 26, 2021. COVID-19: Provision of tuberculosis services [Internet] Available from: https://www.gmmh.nhs.uk/download.cfm?doc=docm93jijm4n7153.pdf&ver=9691. [Google Scholar]
- 28.Kaihlanen A.M., Virtanen L., Buchert U., Safarov N., Valkonen P., Hietapakka L., et al. Towards digital health equity-a qualitative study of the challenges experienced by vulnerable groups in using digital health services in the COVID-19 era. BMC Health Serv Res. 2022 Feb 12;22(1):188. doi: 10.1186/s12913-022-07584-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burns R., Stevenson K., Miller A., Hargreaves S. Migrant-inclusive healthcare delivery in the UK: Lessons learned from the COVID-19 Pandemic. Lancet Reg Health–Europe. 2022 Oct 1:21. doi: 10.1016/j.lanepe.2022.100505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bao Y., Wang C., Xu H., Lai Y., Yan Y., Ma Y., et al. Effects of an mHealth intervention for pulmonary tuberculosis self-management based on the integrated theory of health behavior change: randomized controlled trial. JMIR Public Health Surveill. 2022 Jul 14;8(7) doi: 10.2196/34277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spruijt I., Haile D.T., van den Hof S., Fiekert K., Jansen N., Jerene D., et al. Knowledge, attitudes, beliefs, and stigma related to latent tuberculosis infection: a qualitative study among Eritreans in the Netherlands. BMC Public Health. 2020;20(1):1602. doi: 10.1186/s12889-020-09697-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Courtwright A., Turner A.N. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. 2010;125 Suppl 4(Suppl. 4):34–42. doi: 10.1177/00333549101250S407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sattler S., Maskileyson D., Racine E., Davidov E., Escande A. Stigmatization in the context of the COVID-19 pandemic: a survey experiment using attribution theory and the familiarity hypothesis. BMC Public Health. 2023 Mar 18;23(1):521. doi: 10.1186/s12889-023-15234-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Madan M., Baldwa B., Raja A., Tyagi R., Dwivedi T., Mohan A., et al. Impact of latent tuberculosis on severity and outcomes in admitted COVID-19 patients. Cureus. 2021;13(11) doi: 10.7759/cureus.19882. [DOI] [PMC free article] [PubMed] [Google Scholar]