Abstract
Climate change is a preeminent threat to health and health systems in The Bahamas. Climate and health resilience depends upon a knowledgeable and coordinated healthcare system and workforce that is highly connected and coordinated with a knowledgeable and empowered community. We present the methodology and results of a novel educational workshop, designed to increase the knowledge and awareness of health care professionals and community members with the goal of empowering them to engage in climate mitigation and adaptation strategies. Following the training, participants demonstrated increased knowledge of the causes of climate change, health exposures, climate-sensitive diseases, and vulnerable populations relevant to The Bahamas. Further, participants reported high levels of willingness and readiness to tackle climate change and its health consequences. Results from this workshop suggest that such a model may serve as a guide for building grass-roots resilience in communities worldwide.
Keywords: Climate change and health, Resilience and capacity building, Health professional training and education
1. Introduction
Climate change is a leading threat to the sustainable national development and health in the 21st century, and threatens to roll back the gains in public health across the world. Climate change has already been associated with morbidity, mortality, and compromised societal capacity to deliver healthcare and support healthy living around the world [1]. The effects of climate change will intensify in coming years. In the Caribbean, acute and chronic threats include forced displacement from sea level rise; direct impacts from extreme weather events including hurricanes; saltwater intrusion of groundwater aquifers; loss of livelihoods; spread of infectious diseases; rising temperatures; and changing precipitation patterns [2]. The Caribbean and Small Island Developing States (SIDS) around the world are highly impacted, despite their collective minor contributions to greenhouse gasses. The Bahamas, has contributed approximately 0.01% of global greenhouse gas emissions but faces impacts from rising sea levels, with approximately 80% of its land mass being less than 1.5 m above sea level. The Bahamas has experienced extreme climate related events such as Hurricane Dorian that devastated coastal communities, tourism, and strained the health sector [3,4]. As a result, The Bahamas has taken the stance to urgently respond to these compounding risks for the sake of protecting human health and preventing further widening of health inequalities. In doing so, The Bahamas must seek to engage a targeted whole-of-society response at individual, community, and national levels to ensure advancement of mitigation and adaptation measures to escalating climate change impacts [5].
It is imperative that The Bahamas focus on building a climate-ready health system with the capacity to anticipate, respond to, cope with, recover from and adapt to climate-related shocks and stresses efficiently and effectively [6]. Furthermore, behavioral approaches must be intersectoral and involve stakeholder engagement from the public and private sectors in the design, implementation, and monitoring of adaptation interventions in order to address vulnerabilities which are intimately interwoven with specific population-based and regional vulnerabilities [7]. While the health sector may serve a leadership role in developing interventions, buy-in and participation from community members is paramount for success of resilience-building efforts,h especially in the face of disasters caused by extreme climate events [8].
For The Bahamas, both COVID-19 pandemic and Hurricane Dorian (2019) revealed the urgent need to build capacity to address climate change and health issues. Capacity deficits were visible in the areas of: 1) climate change and health policy, 2) health workforce readiness, 3) community/civil society engagement, 4) climate resilient health infrastructure, 5) data collection, information & technology, and 6) financing for climate change and health issues. The Bahamas thus sought support from the Pan American Health Organization to access funding from the United Nations CARIFORUM Project and the Green Climate Fund (GCF) to address these health system gaps. The GCF readiness project, “Developing a Climate Resilient Health System,” was designed to build upon and strengthen national bodies, communities, and human resources with new mechanisms for the preparation, coordination and response to climate change and health impacts on The Bahamas' health system, national shelters, and general population, inclusive of vulnerable individuals. Under the GCF Readiness project, The Bahamas Climate Change and Health Project Team, within the Ministry of Health and Wellness (MoHW), engaged Earthmedic/Earthnurse, a Caribbean-based Non-profit Organization, and the Global Consortium on Climate and Health Education, based at Columbia University, to assist in developing a climate change collaborative training curriculum. The primary objective was to increase the knowledge and awareness of health care professionals and community members with the ultimate goal of empowering them to co-create climate mitigation and adaptation strategies [9].
While many educational initiatives and programs exist to train health professionals, there is a dearth of initiatives designed to train and engage community members in concert with health professionals, even though existing literature supports such a collaborative strategy as a mechanism to improve communication and bolster community-level responses to health threats [[10], [11], [12]]. Additionally, such an approach may be prudent in Small Island States, where interdependencies between healthcare and community are substantial. Here we present the results of a pilot workshop designed to build community-level adaptive capacity through the collaboration of health professionals and community stakeholders, with the goal of addressing the multifaceted and complex ways in which climate change threatens to undermine health in The Bahamas. The structure of this training was predicated on the following theory of change:
-
●
Resilience to the health impacts of climate change depends upon a knowledgeable health workforce and coordinated healthcare system that are connected with a knowledgeable and empowered community.
-
●
Training and engaging community stakeholders and healthcare professionals collaboratively will encourage the development of a sustainable and enduring partnership that can evolve over time and respond to a wide variety of climate-related threats to health, thereby improving local and national resilience.
The goals of this training workshop were to (1) Increase community stakeholders' and health professionals' knowledge about climate and health, (2) Equip community stakeholders and health professionals with knowledge and skills that could be readily incorporated into practice, (3) Encourage self-efficacy in individual and collaborative community-level action, (4) Increase communication and collaboration between and among health professionals and the communities they serve and (5) Empower or build confidence within health professionals and community stakeholders to be able to share about climate changes with others in their community of practice or sphere of influence.
2. Methodology
2.1. Program structure
This two-day workshop was administered simultaneously in three locations linked by videoconferencing software within The Bahamas: Marsh Harbour, Abaco; Nassau, New Providence; and Freeport, Grand Bahama. The facilitators at each site consisted of a consultant/faculty member and member(s) of The Bahamian Climate Change and Health Project Team. The didactic content and discussion sessions were shared across the sites via virtual connection, with participants at each site experiencing a mix of in-person and virtual learning and discussion sessions. The participants were also engaged in developing a model climate change community and presenting their reflections based on the various components of the didactic training. The program structure extended beyond technical dimensions of the impacts of climate change on human health and sought to build communication, collaboration and shared goals among stakeholders from the community and the healthcare sector as well initiate discussions of adaptive actions focusing on the role of private and public healthcare partners and communities. The two-day workshop therefore incorporated didactic materials within a structure of interprofessional small group and large group activities and discussion (Supplemental Table 1).
Core topics were organized into modules and information was presented for each module in the form of a short lecture followed by a collaborative learning activity. For each module, workshop participants were provided with a glossary of terms as well as links to tools and resources relevant to The Bahamas.
Beginning in the first group work session, participants formed themselves into teams/tables and they were first asked to come up with a name for their group and a name for their fictional community. Then they were provided with climate related cutouts and materials and were asked to collectively design, map or model their own climate resilient community. This exercise considered group dynamics and respected adult education principles of learning by doing. Participants were noted to be adding adaptation or mitigation measures and additional cutouts to their resilient community design as the lecture discussions progressed and new knowledge was gained.
All didactic materials were delivered by experts in climate change and health from the Ministry of Health and Wellness (MoHW), EarthMedic/EarthNurse and the Global Consortium on Climate and Health Education, with two thirds of the facilitators/faculty being from the Caribbean region. The workshop adhered to evidence-based knowledge and skills regarding the health impacts of climate change in The Bahamas.
2.2. Program content
To develop a comprehensive training curriculum, we first performed a gap analysis (Fig. 1). Information and perspectives gathered during stakeholder meetings among Bahamian health professionals and community stakeholders and results from the recent Knowledge Attitude and Practice Survey (KAP) [13] (Box 1) were assimilated and gaps in knowledge and practice among community members and healthcare professionals were identified. (Participants in the KAP survey consisted of 3505 adults who were surveyed using an electronic based convenient sampling. Among respondents, 25 were environmental professionals, 304 were health professionals, 159 were from representatives of civil society organizations, and the remaining 3017 were from the general public.) These gaps were compared to the GCCHE core competencies for health professionals [14], a set of highly-vetted global educational standards which cover climate and health analytic skills and knowledge, communication and collaboration, policy, and public health and clinical practice competencies [15]. Additionally, the adult learning pedagogy of hands-on learning of a situation that has immediate relevancy and problem-solving components for realistic and relevant impact was employed as all participants would have experienced some climate change event. The results of the gap analysis along with the adult learning approach, served to inform the content and structure of the workshop.
Fig. 1.
Process of gap analysis.
Box 1. Findings from Gap Analysis:
-
1.Awareness of Climate Change:
-
a.Awareness of climate change was high, but understanding of the causes of climate change was low, as was awareness of potential solutions or steps that could be taken within the control of environmental officers, community members and health professionals.
-
b.Understanding of the range of climate impacts that can impact health was low.
-
c.Understanding of steps to be taken to protect healthcare infrastructure was low.
-
d.Although most acknowledged that climate change was real, there was low acknowledgement that climate change affects communities, individuals, and national health issues.
-
e.There was mixed recognition of specific subpopulations that are particularly vulnerable to the effects of climate change. Awareness of effects on migrants, first responders, and persons with mental disorders were particularly low.
-
f.Specific mechanisms of health harm resulting from climate change were understood at widely varying rates. Key social factors including increases in unpaid work, losses of paid work, disruptions to health care services and, among the health professionals, loss of housing or physical displacement were less well recognized.
-
g.Awareness of specific medical conditions linked to climate change was low. Aside from vector borne diseases, chronic conditions such as heart disease and mental illness were not reliably connected with climate change.
-
a.
-
2.Personal Responsibility & Combating Climate Change
-
a.Most do not see themselves as contributing substantially to climate change. They ascribed higher levels of responsibility to their community, country, and to other countries.
-
b.Although most agreed that “something needs to be done,” few have taken steps to address causes of or impacts related to climate change on the individual or community level or appreciate the role that they can play in doing something.
-
c.Most do not take actions on an individual basis to reduce their energy use or resource consumption.
-
d.Prevalence of general safety-oriented actions was low, with few reporting taking specific steps to help protect themselves
-
e.Prevalence of safety-oriented actions related to extreme weather events was very low, with few having an evacuation plan, or a first aid kit.
-
a.
-
3.Barriers to action at the institutional level
-
a.Competing health priorities.
-
b.Lack of collective knowledge about mitigation and adaptation options for building a climate resilient health system,
-
c.Lack of a collective action plan across the healthcare system (private & public)
-
d.Lack of adequate external funding due to the ineligibility of The Bahamas at the international level, and
-
e.Lack of internal funding to support climate change work in the healthcare system.
-
a.
Alt-text: Box 1
2.3. Audience
This workshop engaged community members and civil society leaders, physicians, nurses, allied health professionals, national and local health workers, hospital administrators, health system leaders, health educators, teachers, policymakers, environmental health professionals, government officials, journalists, advocates, youth, legal professionals, and others working in areas impacted by climate change. Members of these groups were invited to participate through outreach via email, social media and networking (i.e. word of mouth) as well as through direct engagement by the MoHW.
2.4. Recruitment and enrollment
All participants who registered for the workshop were invited to enroll in the longitudinal study. A pre-workshop survey was sent via email two times prior to the day of the workshop and paper copies were available upon arrival to the workshop. Following the completion of the workshop, all participants were provided with a link to take the follow-up survey and follow up email reminders were sent to workshop participants. Survey period closed 72 h after completion of the workshop. Response data was collected in Qualtrics and was anonymized before being analyzed. The KAP study that was utilized to conduct the gap analysis was approved by the Ministry of Health and Wellness' Stem Cell and Medical Research Oversight Committee. Only those who registered and attended the workshop were included in this study.
2.5. Survey description
The longitudinal survey was structured to assess the effectiveness of this training workshop in increasing climate and health knowledge, personal and professional behavior related to climate and health, and perceived capacity to act individually and in collaboration with a community consisting of health professionals and community members.
The pre-workshop and post-workshop assessment contained questions from the KAP survey which assessed a priori identified common gaps in climate and health knowledge. Additionally, questions assessed perceptions of readiness to engage in climate adaptation and mitigation and perception of individual and collective agency (appendix 2).
The post-workshop assessment contained the same key questions from the KAP study in addition to questions which aimed to assess the effectiveness of this workshop to prepare participants to communicate about climate change, to apply their knowledge to address community-level risks, to apply climate and health knowledge in their work and to serve as champions of climate and health adaptation and mitigation efforts in the Bahamas (appendix 3). Lastly, they were asked to assess the success of the workshop, in terms of applicability and acceptability to inform future training.
2.6. Analysis
Pre-workshop and post-workshop survey results were analyzed in aggregate, and subgroup analyses were performed for health professionals and community members. Descriptive statistics quantifying the baseline characteristics of the learners (pre-workshop survey) and their perceptions of the effectiveness of the training (post-workshop survey) were computed. For questions replicated in the pre-workshop and post-workshop surveys, respondent-matched data for the subset of respondents who completed both pre- and post-workshop evaluations was analyzed.
For survey responses consisting of Likert scales and other ordinal data, results of the pre and post workshop assessment surveys were compared using a paired Wilcoxon rank sum test. For survey responses consisting of binary answers to questions regarding the causes, mechanisms or impacts of climate change, results of the pre and post workshop assessment surveys were compared using a McNemar test with continuity correction.
For each longitudinal survey question, we calculated the percent change in response for each of the predetermined multiple-choice responses. The number of respondents to each possible answer and total number of respondents was used to calculate response percentages for each question in the pre- and post-surveys. Following these calculations, the pre-workshop survey percentages and participant numbers were subtracted from post-workshop survey percentages and participant numbers for each question. This was listed as the “change” in question and represents the implied impact of the workshop on participants' responses.
Data was collected on both paper and electronic survey formats, the latter via the Qualtrics online survey administration tool. Paper survey results were hand coded into Qualtrics and a comprehensive set of survey results was assembled. Data was organized and analyzed using R version 4.2.2 [16].
3. Results
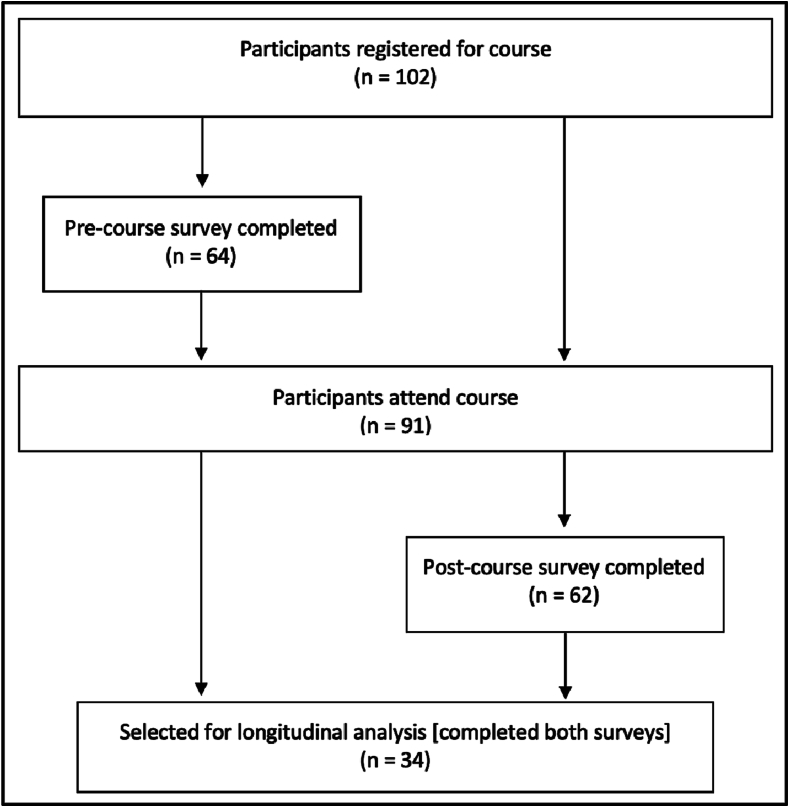
3.1. Demographics and participation
There were 102 individuals who registered for the workshop, of whom 91 participated in the in-person workshops. A total of 41 in New Providence, 28 in Grand Bahama, and 22 participants attended in Abaco. Demographic information regarding general participants can be found in Table 1. A total of 64 participants completed the pre-workshop assessment survey and 62 completed the post-workshop survey, of whom 52 completed the longitudinal questions (Table 1). The majority of health professionals and community survey respondents reported being aged between 30 and 70 years on the pre-workshop survey; 81% of community members and 100% of health professionals identified as female (Table 2).
Table 1.
General Respondent Information.
| a. Distribution of participants by category | ||
|---|---|---|
| Pre (n, (%)) | Post (n, (%)) | |
| Community member | 28 (44%) | 22 (36%) |
| Healthcare professional | 36 (56%) | 40 (65%) |
| All participants | 64 (100%) | 62 (100%)* |
| b. Age distribution of workshop participants by category | ||||||
|---|---|---|---|---|---|---|
| Community member (n (%)) |
Healthcare professional (n (%)) |
All participants (n (%)) |
||||
| Pre (n = 28) | Post (n = 22) | Pre (n = 35)** | Post (n = 40) | Pre (n = 63) | Post (n = 62) | |
| 18–30 | 5 (18%) | 6 (27%) | 4 (11%) | 5 (13%) | 9 (14%) | 11 (18%) |
| 30–50 | 10 (35.7%) | 7 (32%) | 13 (37%) | 17 (43%) | 23 (37%) | 24 (39%) |
| 50–70 | 10 (35.7%) | 8 (36%) | 18 (51%) | 17 (43%) | 28 (44%) | 25 (40%) |
| 70+ | 3 (10.7%) | 1 (4.5%) | 0 (0%) | 1 (3%) | 3 (5%) | 2 (3%) |
| c. Gender distribution of workshop participants by category | ||||||
|---|---|---|---|---|---|---|
| Community member (n (%)) |
Healthcare professional (n (%)) |
All participants (n (%)) |
||||
| Pre (n = 28) | Post (n = 20)** | Pre (n = 32)** | Post (n = 39)** | Pre (n = 60) | Post (n = 59) | |
| Female | 17 (61%) | 14 (70%) | 32 (100%) | 38 (97%) | 49 (82%) | 52 (88%) |
| Male | 11 (39%) | 6 (30%) | 0 (0%) | 1 (3%) | 11 (18%) | 7 (12%) |
*62 participants in total took the post-course survey. However, 10 of those only answered biographical and end-of-course questions (did not complete longitudinal questions)
**This question was skipped over by some respondents. While they are omitted here, their responses are included elsewhere.
Table 2.
General Longitudinal Respondents Information.
| a. Distribution of participants by category | |
|---|---|
| Community member (n (%)) | 16 (47%) |
| Healthcare professional (n (%)) | 18 (53%) |
| All participants (n (%)) | 34 (100%) |
| b. Age distribution of workshop participants by category | |||
|---|---|---|---|
| Community member (n (%)) | Healthcare professional (n (%)) | All participants (n (%)) | |
| 18–30 | 1 (6%) | 3 (17%) | 4 (12%) |
| 30–50 | 5 (31%) | 5 (28%) | 10 (29%) |
| 50–70 | 9 (56%) | 10 (56%) | 19 (56%) |
| 70+ | 1 (6%) | 0 | 1 (3%) |
| c. Gender distribution of workshop participants by category | |||
|---|---|---|---|
| Community member (n (%)) | Healthcare professional (n (%)) | All participants (n (%)) | |
| Female | 13 (81%) | 18 (100%) | 31 (91%) |
| Male | 3 (19%) | 0 | 3 (9%) |
A total of 34 individuals completed both pre and post workshop surveys, allowing for matched analysis comparing responses before and after the training intervention (Fig. 2). See appendix 1 for comparison of participant demographics based on survey participation. The 34 individuals that completed both pre and post assessment surveys consisted of 18 health care workers and 16 community members. The group was 91% female; 56% were 50–70 years of age.
Fig. 2.
Workshop and survey participation.
3.2. Longitudinal survey results
3.2.1. General climate change awareness
Baseline knowledge and attitudes regarding climate change were notable for a recognition of climate change but a lack of understanding around its causes and impacts as shown in Table 3.
Table 3.
General climate change awareness.
| a. Do you believe climate change is real? | ||||
|---|---|---|---|---|
| Pre | Post | Change | P-value | |
| Yes | 34 (100%) | 34 (100%) | 0% | No statistically significant change |
| No | 0 (0%) | 0 (0%) | 0% | |
| Don't know | 0 (0%) | 0 (0%) | 0% | |
| b. If you believe climate change is real, when do you think it will happen?⁎ | ||||
|---|---|---|---|---|
| Pre | Post | Change | P-value | |
| Happening now | 34 (100%) | 33 (100%) | 0% | No statistically significant change |
| In the future | 0 (0%) | 0 (0%) | 0% | |
| Don't know | 0 (0%) | 0 (0%) | 0% | |
| c. Assuming climate change is real, what is causing it? | ||||
|---|---|---|---|---|
| Pre | Post | Change | P-value | |
| Entirely by human activities | 6 (18%) | 6 (18%) | 0% | No statistically significant change |
| Mostly by human activities | 6 (18%) | 9 (27%) | 9% | |
| Equally by human activities and natural environmental changes | 21 (62%) | 19 (56%) | −6% | |
| Mostly environmental changes | 1 (3%) | 0 (0%) | −3% | |
| Entirely natural environmental changes | 0 (0%) | 0 (0%) | 0% | |
| None of the above because climate change isn't happening | 0 (0%) | 0 (0%) | 0% | |
| d. How much do you think that climate change affects….? | |||||
|---|---|---|---|---|---|
| Affected Group | Response | Pre | Post | Change | P-value |
| You personally? | A great deal | 21 (62%) | 31 (91%) | 29% | 0.0015 (McNemar) |
| Moderately | 11 (32%) | 3 (9%) | −24% | ||
| Slightly | 2 (6%) | 0 (0%) | −6% | ||
| Not at all | 0 (0%) | 0 (0%) | 0% | ||
| Don't know | 0 (0%) | 0 (0%) | 0% | ||
| People in your community? | A great deal | 25 (74%) | 31 (91%) | 17% | |
| Moderately | 8 (24%) | 3 (9%) | −15% | 0.0263 (McNemar) | |
| Slightly | 1 (3%) | 0 (0%) | −3% | ||
| Not at all | 0 (0%) | 0 (0%) | 0% | ||
| Don't know | 0 (0%) | 0 (0%) | 0% | ||
| People in your country?⁎ | A great deal | 23 (68%) | 29 (91%) | 23% | 0.0147 (McNemar) |
| Moderately | 10 (29%) | 3 (9%) | −20% | ||
| Slightly | 1 (3%) | 0 (0%) | −3% | ||
| Not at all | 0 (0%) | 0 (0%) | 0% | ||
| Don't know | 0 (0%) | 0 (0%) | 0% | ||
| “People in other countries?”⁎ | A great deal | 25 (78%) | 29 (91%) | 13% | No statistically significant change |
| Moderately | 7 (22%) | 3 (9%) | −13% | ||
| Slightly | 0 (0%) | 0 (0%) | 0% | ||
| Not at all | 0 (0%) | 0 (0%) | 0% | ||
| Don't know | 0 (0%) | 0 (0%) | 0% | ||
| “Future generations?”⁎ | A great deal | 30 (88%) | 30 (91%) | 3% | No statistically significant change |
| Moderately | 4 (12%) | 3 (9%) | −3% | ||
| Slightly | 0 (0%) | 0 (0%) | 0% | ||
| Not at all | 0 (0%) | 0 (0%) | 0% | ||
| Don't know | 0 (0%) | 0 (0%) | 0% | ||
Indicates a respondent or multiple respondents did not respond to this question.
All survey analysis respondents stated they both believed climate change was real and that it is “happening now”, with no change across longitudinal surveys.
Regarding the causes of climate change, the majority of participants (62%) originally stated that climate change is caused “equally by human activities and natural environmental changes,” while 35% stated it was either “mostly” or “entirely” due to human activities. Following the workshop there was a slight increase in the number of respondents who believed climate change was “mostly” due to human activities (Table 3).
Participants were asked how much climate change affects them personally, people in their community, people in their country, people in other countries and future generations. While prior to the workshop the majority of participants did recognize that climate change would affect them personally (61.8%), their community (61.8%), or their country (67.6%) – a greater number of participants believed climate change would affect people in other countries (78.1%) and future generations (88.2%). Following the workshop, the overwhelming majority of participants demonstrated understanding that climate change would affect all five categories of people (Supplemental Table 2).
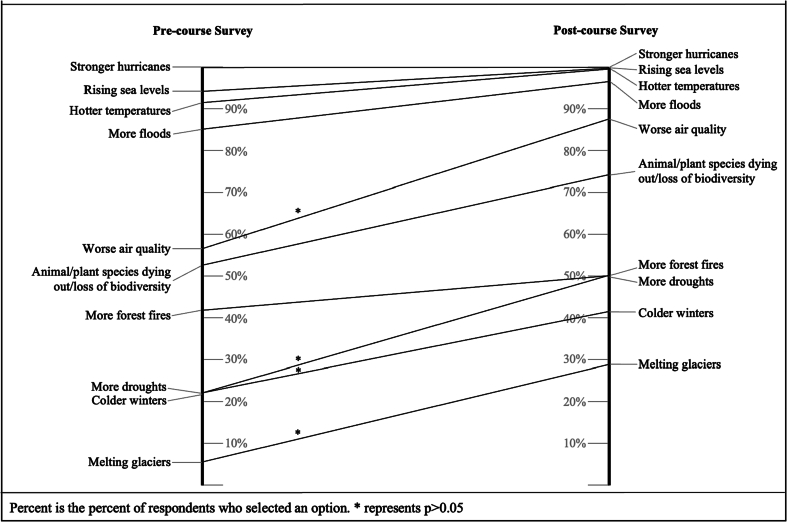
3.2.2. Awareness of climate and health impacts in the Bahamas
Pre-workshop, the majority of participants recognized stronger hurricanes (100%), rising sea levels (94%), hotter temperatures (91%) and more floods (85%) as relevant impacts of climate change in the Bahamas. In the post workshop assessment, the acknowledgement of these risks increased among participants (rising sea levels (100%), hotter temperatures (100%) and more floods (97%), while the majority of participants were also able to recognize degraded air quality (88%), loss of biodiversity (73%), drought (50%), colder winters (41%) and melting glaciers (29%) as relevant risks in The Bahamas. Statistically significant improvements in hazard recognition were seen for climate-related exposures due to degraded air quality, more droughts, colder winters, and melting glaciers (Fig. 3).
Fig. 3.
Longitudinal change in response to the question, “What impacts of climate change are relevant in The Bahamas?”
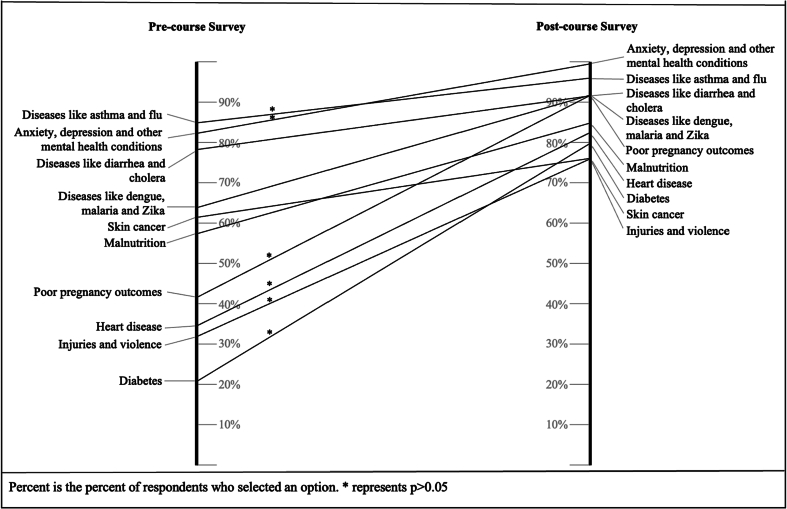
In the pre-workshop assessment, participants identified respiratory diseases, (85.3%), anxiety, depression, and other mental health conditions (82.4%), and gastrointestinal diseases (79.4%) as conditions which can be affected due to climate change. Fewer respondents identified diabetes (20.6%), injuries and violence (32.4%), heart disease (35.3%), and poor pregnancy outcomes (41.2%) (Fig. 4). The post-workshop survey showed improvement among all categories with statistically significant increases seen in awareness of respiratory diseases, mental health conditions, pregnancy outcomes, heart disease, injuries and violence and diabetes as being climate-sensitive. Overall understanding of health implications in the group was higher among healthcare workers than community members (See appendix 4).
Fig. 4.
Longitudinal change in response to the question, “Which of these conditions can affect people because of climate change?”
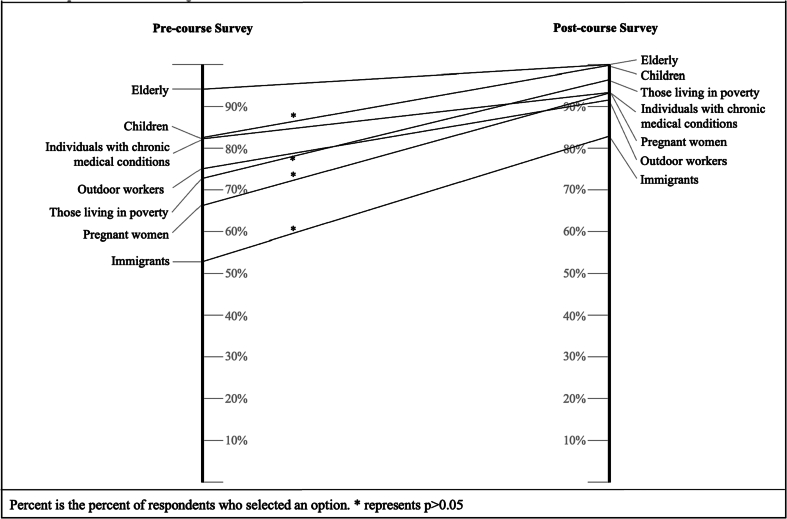
Regarding population-level vulnerability to climate and health impacts in The Bahamas, over 80% of participants initially recognized the elderly, children and individuals with chronic medical conditions. Following the workshop, there was a significant increase in awareness of additional vulnerable populations including immigrants, pregnant individuals and those in poverty (Fig. 5). Vulnerable group identification was generally the same among community members and healthcare professionals (See Appendix 3).
Fig. 5.
Longitudinal change in response to the question, “What populations in the Bahamas do you believe are vulnerable to the health impacts of climate change?”
3.2.3. Climate change and health action
Following the workshop, participants nearly unanimously stated that action by the government (100%), the community (100%), health professionals (100%), international organizations (100%), and individuals (91%) was needed to respond to the health impacts of climate change (Table 4), representing an upward trend in acknowledgement of the multisectoral nature from pre-post workshop.
Table 4.
Attitudes and beliefs regarding action on the causes and impacts of climate change on health.
| a. To combat the health impacts of climate change, who do you think should respond? (Multiple choice. If counted, responded “Yes”) | ||||
|---|---|---|---|---|
| Pre | Post | Change | P-value | |
| The government | 30 (88%) | 34 (100%) | 12% | No statistically significant change in any group |
| The community | 30 (88%) | 34 (100%) | 12% | |
| Healthcare professionals | 29 (85%) | 34 (100%) | 15% | |
| International organizations | 31 (91%) | 34 (100%) | 9% | |
| Individual action | 29 (85%) | 31 (91%) | 6% | |
| b. To combat the causes of climate change... | |||||
|---|---|---|---|---|---|
| Response | Pre | Post | Change | P-value | |
| Do you think you can do something?⁎ | Yes | 29 (96%) | 34 (100%) | 4% | No statistically significant change |
| No | 1 (4%) | 0 (0%) | −4% | ||
| Don't know | 0 (0%) | 0 (0%) | 0% | ||
| Do you want to do something?⁎ | Yes | 34 (100%) | 33 (100%) | 0% | No statistically significant change |
| No | 0 (0%) | 0 (0%) | 0% | ||
| Don't know | 0 (0%) | 0 (0%) | 0% | ||
| c. To combat the health impacts of climate change... | |||||
|---|---|---|---|---|---|
| Do you think you can do something?⁎ | Yes | 31 (100%) | 33 (100%) | 0% | No statistically significant change |
| No | 0 (0%) | 0 (0%) | 0% | ||
| Don't know | 0 (0%) | 0 (0%) | 0% | ||
| Do you want to do something?⁎ | Yes | 33 (100%) | 33 (100%) | 0% | No statistically significant change |
| No | 0 (0%) | 0 (0%) | 0% | ||
| Don't know | 0 (0%) | 0 (0%) | 0% | ||
Indicates a respondent or multiple respondents did not respond to this question.
Pre and post workshop attitudes regarding climate action were high. In both pre- and post-workshop assessments, nearly all respondents stated they believed they could do something to combat the causes and health impacts of climate change (100%) and wanted to do something (100%)(Supplemental Table 3).
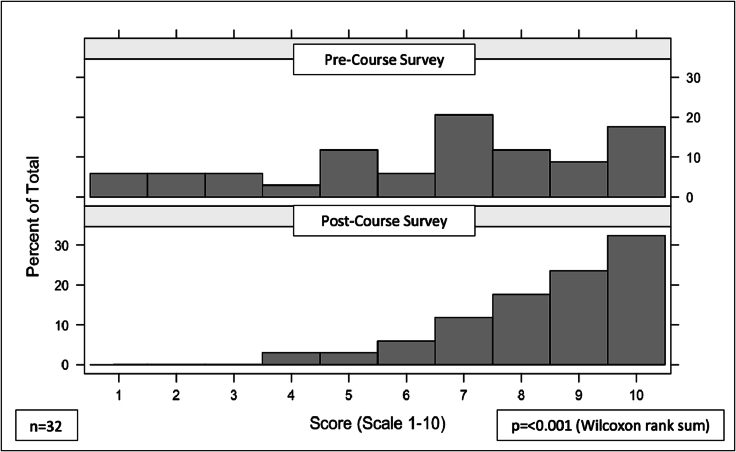
Pre-workshop, participants reported mixed feelings when asked to rate how prepared they felt to work on addressing the health impacts of climate change on a scale of 1–10 with 1 being “not ready at all”. A longitudinal analysis showed an increase in the self-reported preparedness participants felt to address the health impacts of climate change (p < 0.001 via paired Wilcoxon Rank-Sum) (Fig. 6.)
Fig. 6.
Response to question: On a scale of 1–10 how ready do you feel to work on addressing the health impacts of climate change?
3.3. Post-workshop assessment
Following the workshop, 73% of health professionals and 73% community members reported that they felt very prepared to collaborate with each other to address root causes and health impacts from climate change (Supplemental Fig. 1).
Roughly equal numbers of community members (68%) and health professionals (70%) reported that the workshop had prepared them “very well” to speak with patients/community members about climate change and their health. The remainder felt prepared to have conversations with patients and community members, but in limited scenarios (Supplemental Fig. 2).
Regarding how knowledge gained during the workshop would change their community/professional/business and individual efforts and activities, 80% of healthcare professionals and 68% of community members reported that the new knowledge and skills they had obtained would change their efforts and activities to a large degree while the remainder reported that it would change some aspects of their efforts and activities (Supplemental Fig. 3).
A similar proportion of healthcare professionals (78%) and community members (77%) reported that the knowledge and skills they gained from the workshop would change their personal behavior to a large degree while the remainder reported that it would change some aspects of their behavior (Supplemental Fig. 4).
When asked whether the workshop prepared them to serve as leaders in climate and health initiatives within their communities or workplaces, 50% of community members and 43% of healthcare professionals reported feeling confident, while the remainder reported that they felt they needed more knowledge or experience to serve as a leader (Supplemental Fig. 5).
When asked if this workshop was effective in equipping them with actionable solutions for their communities, 55% of community members and 60% of healthcare professionals reported they felt knowledgeable and equipped to enact solutions, while the remainder reported that they felt somewhat equipped but needed more training (Supplemental Fig. 6).
4. Discussion
Community members and healthcare professionals stand on the front lines of the climate crisis, yet many barriers exist which prevent meaningful engagement and action [14]. The MoHW of The Bahamas, in collaboration with EarthMedic/EarthNurse and the Global Consortium on Climate and Health Education, delivered a 2-day workshop designed to build knowledge, skills, collaboration, and ultimately adaptive capacity of the Bahamian healthcare workforce and community members. In total, 91 individuals from the islands of Abaco, Grand Bahama and New Providence, representing youth and many sectors of civil society and the healthcare professions, participated simultaneously in this workshop linked realtime by technology across the three sites. This tri-island hybrid training helped foster a sense of individual island spirit, collaborative inter island camaraderie and a cross-country awareness of the impact of climate change within The Bahamas. The goals of this training workshop were to (1) Increase community stakeholder and health professional knowledge about climate and health, (2) Equip community stakeholders and health professionals with knowledge and skills that could be readily incorporated into practice, (3) Encourage self-efficacy in individual and collaborative community-level action, (4) Increase communication and collaboration between health professionals and community stakeholders with each other and the public and (5) Empower or build confidence within health professionals and community stakeholders to be able to share about climate changes with others in their community of practice or sphere of influence.
This training curriculum appears to have successfully increased community members' and healthcare professionals' knowledge about climate change and its implications for health. Following the workshop, participants reported increased understanding of the causes of climate change, who would be affected, and to what degree. Furthermore, we observed an increased understanding of climate-related exposures relevant to The Bahamas, including rising sea levels, hotter temperatures, more floods, degraded air quality, loss of biodiversity, and floods. Additionally, participants increased their ability to recognize climate-sensitive diseases and health outcomes of relevance to The Bahamas, including respiratory diseases, mental health conditions, pregnancy outcomes, heart disease, injuries and violence and diabetes. Importantly, participants were better able to identify climate-vulnerable populations, including immigrants, pregnant individuals and those in poverty.
Based on results from the post-workshop assessment, many community members and health professionals felt they gained some knowledge and skills that could be readily incorporated into practice, but opportunities to further empower these cohorts remain. While the majority of participants reported that the knowledge they gained would change their community/professional/business and/or individual efforts and activities and their personal behavior, only half of participants reported feeling confident serving as leaders of initiatives in their communities and just over half reported that they felt equipped with actionable solutions. Many reported that they felt they needed additional training to lead climate actions in their communities and professional practices.
Longitudinal and post-workshop questions were used to assess whether this workshop encouraged self-efficacy in individual and collaborative action. While personal willingness to act on the causes of climate change and its health impacts was already high going into the workshop, we saw a dramatic increase in participants' feeling of readiness to tackle climate change and its health consequences (Fig. 6). Furthermore, in longitudinal analysis, there was a trend towards participants recognizing multiple stakeholders including health professionals, the government, and community members as being responsible for taking action (Table 4).
The majority of participants reported that the workshop prepared them to collaborate with each other to address root causes and health impacts from climate change. A smaller majority reported that the workshop equipped them to speak with patients and community members, but many acknowledged limitations to their ability to hold such conversations (Fig. 8). The results appear promising for this type of capacity building.
The specific knowledge gains and shift in attitudes of readiness to address the climate and health crisis are promising, however, to be fully effective, participants would need further support through a supportive local and national environment, additional skills building as ambassadors, educators, and incentives and financial investment to implement climate action in their communities.
There is a paucity of literature comparing outcomes from similar workshops, courses or trainings from which we can draw comparisons. There were no available published outcomes for any existing courses that focused particularly on the education of community members and health workers as a group. Feedback for similar training programs (i.e. short courses on climate and health targeting medical students) were often very brief, or comprehensive analysis of feedback was not published [17].
4.1. Strengths and limitations
The strengths of this workshop included strong leadership from the MoHW of The Bahamas, that had previously undertaken a KAP study which informed the gap analysis; a Climate Change and Health Project Team in the MoHW that supported the tri-island planning for the workshops; support from international, regional and local experts that insured the curriculum was culturally-attuned with relevant climate experiences and relatable climate case studies; wide geographic representation among health professionals and a large diversity of community stakeholders; deep engagement of experts from within the MoHW and the region to serve as workshop faculty; ample opportunities throughout the workshop for group work and bi-directional engagement among workshop faculty and participants; an evidence-based approach which adhered to global competencies for responding to the health impacts of the climate crisis and finally the undergirding of financial support from the GCF Readiness Proposal funding and the Government of The Bahamas for inter-island travel, accommodation, transport, supplies and the streaming technology. The simultaneous workshops across three islands linked by technology was a cost effective innovation and facilitated inclusion of the Family islands.
An important limitation to recognize is the self-selection of participants into the workshop and into the longitudinal study cohort. Though the workshop was widely promoted, it was organized on a short timeline, and thus existing relationships between the MoHW and civil society and healthcare professional organizations were leveraged to recruit participants. There was limited representation by several key vulnerable populations i.e. migrant population, persons with disabilities, pregnant women, and outdoor workers. Additionally, data collection required participants to engage in two optional surveys, which may have biased selection of respondents toward those who were particularly engaged with the workshop, with strong pre-existing interest in climate change, or those who had strong computer skills and/or internet access. The majority of participants were women and thus the perspective of the male gender was missed.
4.2. Next steps and future directions
In initiatives to educate and empower, it is important to keep up momentum. The second day of the workshop engaged the same group of participants to brainstorm the vision for a Terms of Reference and an annual work plan for a Climate and Health Advocacy Network (CHAN) for The Bahamas. A draft structure of this network has been established and teams, lead by community members and health professionals facilitated by the MoHW, EarthMedic/EarthNurse, and supported by GCCHE, have begun work on three islands, each having identified their most pressing climate and health challenges. Furthermore, the CHAN has begun planning a train the trainer style workshop, as this was identified by CHAN island leaders, as well as in the survey, as a necessary next step to scale-up and ensure ownership of the implementation of effective climate action in The Bahamas. Additionally, the MoHW and EarthMedic/EarthNurse, supported by GCCHE have plans to review the curriculum with the input from the workshop participants regarding how to streamline and augment to meet the areas that were identified by participants as needing more education - communicating about climate change, leading climate and health initiatives and implementing climate action/actionable solutions. To ensure that all community members have equal access and opportunity consideration should be given for language translation as well as the visual and hearing impaired. It will also be necessary to seek further governmental and international climate financing to ensure this work is not only scaled up but has sustainable support to ensure measurable climate action takes place in healthcare settings, workplaces and communities within The Bahamas. Further, to create a more climate-educated health workforce, it is recommended that climate and health sensitization and community engagement training be rolled out across The Bahamas, as well as integrated into curricula of health training institutions. Other Caribbean countries may wish to consider similar training and capacity building initiatives.
5. Conclusion
Climate change is a reality in The Bahamas that will have increasingly significant impacts on human health and healthcare. Community members and health professionals are on the front lines of this crisis. Health protection in a changing climate depends upon a knowledgeable and empowered workforce and community working in a connected and coordinated healthcare system. Our experience with this workshop suggests that training and engaging community stakeholders and healthcare professionals collaboratively can be an effective model to advance shared understanding of climate impacts and solutions. Such approaches may have a role to play in the development of sustainable and enduring partnerships that can evolve over time and respond to a wide variety of climate-related threats to health, thereby improving local and national resilience in Small Island Developing States and across the world.
The following are the supplementary data related to this article.
Supplemental Figure 1. Response to the question: “Do you think that this workshop has prepared you to speak with patients/community members about climate change and their health?”
Supplementary material
Declaration of Competing Interest
No authors of this manuscript have conflicts of interest to declare.
Acknowledgements
The UNFCCC, GCF Readiness Proposal Funding, The Climate Change Advisory Unit in The Office of The Prime Minister, The Department of Environmental Planning and Protection, the National Designated Authority (NDA), Mr. Darrell Audinette and the Caribbean Community Climate Change Center (5C's) Implementing agency,The Climate Change and Health Project Team for the support in preparation of the Training, Ministry of Health and Wellness, Mrs. Shavon Peet, Training Unit, Mrs. Glathonya Sands-Higgs, Epidemiologist Assistant and Dr. Monique Mitchell (Supervisor), Ms. Khandi Gibson and Mrs. Ginnette Horton- Community Engagement Officers, Abaco, Grand Bahama and New Providence NGO's
References
- 1.Romanello M., McGushin A., Di Napoli C., Drummond P., Hughes N., Jamart L., et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet. 2021;398(10311):1619–1662. doi: 10.1016/S0140-6736(21)01787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Intergovernmental Panel on Climate Change Climate Change 2022 Impacts, Adaptation and Vulnerability Summary for Policy Makers Available at: https://reportipccch/ar6wg2/pdf/IPCC_AR6_WGII_SummaryForPolicymakerspdf Accessed 18 March 2022.
- 3.WHO Health and climate change: country profile 2021: the Bahamas [Internet] 2023 Jan 29. https://www.who.int/publications-detail-redirect/WHO-HEP-ECH-CCH-21.01.03 Available from:
- 4.The facts: Hurricane Dorian's devastating effect on The Bahamas - Bahamas | ReliefWeb [Internet]. 2020 [cited 2023 Jan 29]. Available from: https://reliefweb.int/report/bahamas/facts-hurricane-dorian-s-devastating-effect-bahamas.
- 5.Hill A.C. Oxford University Press; 2021. The Fight for Climate After COVID-19. [Google Scholar]
- 6.WHO . 2015. Operational framework for building climate resilient health systems. Available at: https://www.who.int/publications/i/item/9789241565073. [Google Scholar]
- 7.WHO . 2019. Caribbean Action Plan on Health and Climate Change. Available at: https://www.who.int/publications/i/item/PAHO-CDE-19-007. [Google Scholar]
- 8.UNDP. Disaster Resilince Measurements. Available at: https://www.unisdr.org/files/37916_disasterresiliencemeasurementsundpt.pdf.
- 9.The Bahamas GCF Readiness Project Proposal. 2021. https://www.greenclimate.fund/document/developing-climate-resilient-health-system-bahamas Available at:
- 10.Barna S., Maric F., Simons J., Kumar S., Blankestijn P.J. Education for the Anthropocene: Planetary health, sustainable health care, and the health workforce. Med Teach. 2020;42(10):1091–1096. doi: 10.1080/0142159X.2020.1798914. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan J.K., Lowe K.E., Gordon I.O., Colbert C.Y., Salas R.N., Bernstein A., et al. Climate change and medical education: an integrative model. Acad Med. 2022;97(2):188–192. doi: 10.1097/ACM.0000000000004376. [DOI] [PubMed] [Google Scholar]
- 12.Harris O.O., Bialous S.A., Muench U., Chapman S., Dawson-Rose C. Climate change, public health, health policy, and nurses training. Am J Public Health. 2022;112(S3) doi: 10.2105/AJPH.2022.306826. S321-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Knowledge Attitude and Practice (KAP) Survey - Ministry of Health - Government [Internet]. [cited 2023 Jan 31].
- 14.Global Consortium on Climate and Health Education. Core Climate and Health Competencies for Health Professionals. Available at:https://www.publichealth.columbia. edu/research/global-consortium-climate-and-health-education/core-competencies-0 (accessed on January 23, 2022).
- 15.Shaman J., Knowlton K. American Public Health Association; 2018. The need for climate and health education. p. S66-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2022. R: A language and environment for statistical computing.https://www.R-project.org/ [Google Scholar]
- 17.Aasheim E.T., Bhopal A.S., O’Brien K., Lie A.K., Nakstad E.R., Andersen L.F., et al. Climate change and health: a 2-week course for medical students to inspire change. Lancet Planet Health. 2023;7(1) doi: 10.1016/S2542-5196(22)00304-7. e12-e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Response to the question: “Do you think that this workshop has prepared you to speak with patients/community members about climate change and their health?”
Supplementary material