Abstract
Background:
Providers’ unconscious biases reinforce health disparities through negative direct patient care and interactions with colleagues.
Objective:
We created a workshop grounded in Critical Race Theory and the importance of different intersectionalities to improve medical trainees’ self-assessment of their implicit biases in curated facilitated spaces.
Methods:
A total of 44 UCSF first-year clinical anesthesiology residents (CA-1) (95% response rate) and 23 surgery residents in their research year (77% response rate) participated in this workshop over 4 separate sessions in September 2020 and 2021. Quantitative data from a pre-/post-workshop survey was analyzed via a paired t test to evaluate our workshop's effectiveness. Feedback on efficacy was obtained by coding themes from our survey's open-ended questions.
Results:
The workshop was evaluated positively by a total of 65 of 67 participants in the post-workshop survey. On a 5-point Likert scale, participants self-reported they agreed that their unconscious biases affect their clinical interactions from a pre-workshop mean of 3.3 (SD ± 1.32) to a post-workshop mean of 3.9 (SD ± 0.87, P = .008).
Conclusion:
Our findings suggest that this workshop was effective for perioperative residents and can be extrapolated to all residents by tailoring the workshop to their respective work environments.
Keywords: Diversity, equity, inclusion, unconscious bias, implicit bias, learners, perioperative, trainees, interactive, training
Introduction
Implicit bias (unconscious bias) is widespread in health care as providers consciously and unconsciously make stereotype-based assumptions influencing their clinical decisions and patient interactions. Although pattern recognition can supplement clinical judgment, it is important to recognize the harms of implicit bias. Implicit biases too quickly narrow a differential, not necessarily with evidence, and attach potentially irrelevant or harmful qualifiers. We define unconscious or implicit bias as the attitudes or stereotypes affecting our understanding, actions, and decisions, activated involuntarily and without awareness (Table 1).1-10 Providers’ unconscious biases reinforce cross-generational health disparities through direct patient care, negative interactions with colleagues, and negative role modeling for medical students and junior trainees.11,12
Table 1.
Glossary
| Word | Definition |
|---|---|
| Allyship | A term that describes efforts to advance the interests of marginalized groups both in society at large and social contexts, for example in universities or workplaces.1 |
| Critical Race Theory | A theory that posits that challenging and transforming racism-embedded social structures and interactions requires directly addressing race in education, contrasting with the previously used “color-blindness” and “neutral” principles that avoided race.2 |
| Ego-ideal | An inner image of oneself that one unconsciously and consciously desires to become.11 |
| Explicit bias | Where individuals are aware of their deliberate prejudices and attitudes toward certain groups.4 |
| Hidden curriculum | A collection of implicit messages, unwritten rules, unspoken expectations, and unofficial norms of the dominant-culture context in which the teaching and learning is situated.5 |
| Intersectionality | The complex, cumulative way in which effects of multiple forms of discrimination (such as racism, sexism, and classism) combine, overlap, or intersect.6 |
| Marginalized identities | An identity that causes or has historically caused a person with this identity to be disproportionately subject to discrimination, harassment or other negative treatment due to the identity.7 |
| Microaggression | The everyday slights, insults, invalidations, and offensive behaviors that people experience in daily interactions with individuals who may be unaware that they have engaged in demeaning ways.7 |
| Performative allyship | Performing with self-gratification in the center of your action, often done to make yourself feel better, to “prove” you are not a racist or create a perception of yourself for others.8 |
| Real/Effective allyship | Amplifying the voices of people within a marginalized community and what they are saying.8 |
| Stereotype suppression | An attempt to control prejudiced responses by suppressing thoughts about or actions believed to be part of a group's stereotype. Often leads to rebound effect.9 |
| Transformative learning theory | Learning goes beyond just getting new information, as it also leads learners to evaluate and reflect on past ideas and understandings, shifting their worldview.10 |
| Unconscious Bias/Implicit Bias (interchangeable) | The attitudes or stereotypes affecting our understanding, actions, and decisions, activated involuntarily and without an individual's awareness.7 |
Mitigating unconscious bias in health care requires intervention at the individual level by increasing self-awareness of held biases and at the institutional level by widely discouraging reinforcement of biases.11 Despite ample evidence of mistreatment and discrimination in perioperative fields, few interactive unconscious bias curricula for perioperative learners exist.13-15 In light of these findings, the Accreditation Council for Graduate Medical Education released their first diversity accreditation standards in 2019.16 Thus, there is a need for evidence-based Diversity, Equity, and Inclusion (DEI) workshops for trainees targeting unconscious bias to increase awareness and intentionality around the treatment of patients and colleagues. Given this need, the co-authors created an unconscious bias workshop in the summer of 2020 to encourage perioperative trainees to better assess and reduce their own implicit biases.
We created this unconscious bias workshop as the second part of a 4-part synchronous DEI training series that aims to support residents in engaging in difficult dialogues, taking antiracist actions, and supporting people marginalized within health care and society. The series also includes an introductory session describing the purpose and an outline of the series, an allyship workshop, and a microaggressions workshop. Each workshop can be taught as a stand-alone session.
The unconscious bias workshop and overall series is based on the Critical Race Theory's (CRT) tenets, first described by Derrick Bell, and transformative learning theory across various intersectionalities (as coined by Kimberlé Crenshaw).2,17 The CRT model posits that challenging and transforming racism-embedded social structures and interactions requires directly addressing race in education, contrasting with the previously used “color-blindness” and “neutral” principles that avoided race.2 Transformative learning focuses on adult education and aims to empower learners to look differently at society through an ethical lens, thus motivating change within that domain.
The objectives of the unconscious bias workshop were to increase self-awareness of one's own implicit bias and motivation to help mitigate bias among perioperative trainees. To accomplish these objectives, the workshop delivers interactive tools among trainees within facilitated spaces to promote revealing and acknowledging biases, engaging in difficult dialogues about their biases, and directly addressing and reducing bias in their interactions. Using CRT, we selected interactive activities highlighting marginalized identities to foster conversation around implicit bias. Clinically relevant didactic content was also presented to highlight the correlation of unconscious bias with health care disparities. This workshop's integration into the surgery and anesthesia trainees’ preexisting didactic education underscores its importance, accessibility, and adaptability. Following previous studies’ recommendations, obtaining institutional leadership support was paramount for the implementation of our DEI training series along with the careful selection and training of interdisciplinary facilitators.18 We hypothesized that after our workshop, learners would have increased awareness of their own unconscious biases, assessed through our pre- and post-workshop surveys. In our study, we used a mixed-methods approach to evaluate the completion of these objectives.
Methods
Using Kern's 6-step approach to curriculum development, we describe an innovative curriculum for perioperative learners designed to teach skills to effectively address unconscious bias. Our needs assessment (Appendix A) was a pre-workshop survey administered in 2 ways within 1 month of each other: (1) 4 to 6 weeks before the 2020 curriculum's start via email to second-year clinical anesthesia residents (CA-2), third-year clinical anesthesia residents (CA-3), and surgery residents and (2) at the end of a voluntary 1-hour didactic introductory session for first-year clinical anesthesia residents (CA-1) in 2020 and 2021. This survey captured what perioperative trainees felt was lacking in their DEI training and their prior DEI training experiences.
Informed by the needs assessment, we combined didactics and small group activities to address the learning objectives in each 2-hour workshop (https://anesthesia.ucsf.edu/workshop-materials). Large group didactics introduced important definitions, significant studies on how implicit bias affects physician decision-making behaviors, and data on the extent of health care disparities based on marginalized identities. Small group activities gave participants a space to discover biases and practice relevant skills.
The learning objectives for our workshop included the following:
Explain 2 differences between bias and unconscious bias by providing at least 1 example of each.
Assess one's own unconscious biases in relation to the workshop exercises in a small group discussion.
Describe 2 tools that can be used for reducing bias in clinical spaces.
Identify 3 ways to apply concepts around unconscious bias in the clinical environment.
Model 2 ways to successfully interact with socially dissimilar colleagues and patients.
Pre-Workshop Resources
A week before the workshop, we emailed a learner's guide (Appendix B) to participants that provided recommended reading articles cited in the workshop for background knowledge.
House Rules
At the beginning of the workshop, after introductions, a set of house rules was presented to the group, including but not limited to having videos on throughout the session held over Zoom (Zoom Video Communications Inc.), assuming positive intent, assuring confidentiality, etc. to curate inclusive learning spaces.
Small Group Activities
We included 3 activities during the workshop, allotting 20 to 30 minutes per activity: Whom to Leave Behind, Harvard Implicit Association Test (IAT),19 and How Diverse is Your Universe? Informed by the pre-workshop survey results, these activities were chosen for their ability to engage participants in transformative learning, to encourage the unveiling of implicit biases, and to create easy segues into sharing discussing their personal experiences and memories. Following the CRT's principles, we specifically addressed identities (race, gender, sexual orientation, and other intersectionalities) and encouraged discussion of related biases in each activity.
These activities were conducted in small groups of 5 or fewer learners with 1 or 2 facilitators per group. Participants who identify as underrepresented in medicine were grouped together, but this was imperfect because of uneven numbers of each affinity group. Facilitators were assigned to small groups based on self-described experience and comfort discussing DEI topics; some were paired with a more experienced facilitator if available. Representatives from each small group shared insights anonymously on return to the larger group after permission was granted from small group participants.
Obtaining Institutional Support
Anesthesia and Surgery leadership broadcasted messaging on the importance of DEI, encouraged workshop attendance, agreed to use protected didactic time for the workshop, and assigned departmental educational leaders invested in DEI as collaborators.
Facilitator Selection and Training: “Train the Trainer”
The workshop creators found facilitators of racially and gender-diverse backgrounds in different specialty departments (Table 2) through other institution-wide DEI trainings. All selected facilitators had participated in the UCSF DEI Champion training, which increases clinical teachers’ awareness and skills to effectively address bias and discrimination.20 No clinical time or compensation was offered to facilitators, but facilitators who agreed found the subject matter important and were encouraged to list these facilitations within their CV as promotable academic work.
Table 2.
Facilitator Demographics
| Count Out of 10 (%) | |
|---|---|
| Department | |
| Anesthesiology | 2 (20) |
| Emergency Medicine | 1 (10) |
| General Surgery | 2 (20) |
| Internal Medicine | 1 (10) |
| Ophthalmology | 1 (10) |
| Orthopedic Surgery | 2 (20) |
| Pediatrics | 1 (10) |
| Gender | |
| Male | 4 (40) |
| Female | 6 (60) |
| Race | |
| Black | 3 (30) |
| Indian/South Asian | 1 (10) |
| Latinx | 1 (10) |
| Mixed (White/Black) | 1 (10) |
| White | 4 (40) |
One week before the workshop, a 1-hour preparatory session was taught to facilitators by the curriculum's lead principal investigator (Dr. Odi Ehie) to introduce the exercises and the facilitator guide and discuss ways to address potentially challenging topics that may arise. After each workshop, a facilitator debriefing session took place to highlight any challenging themes that could be added to the facilitator guide for future sessions.
Administration
Because of time constraints in aligning the schedule for anesthesia and surgery residents, the full DEI curriculum and post-workshop surveys (Appendix A) were administered to first-year clinical anesthesia residents and senior general surgery residents (postgraduate year [PGY]-4 and PGY-5) from September 2020 to April 2022 to maximize the number of trainees that could be reached concurrently. The unconscious bias workshop was administered during protected resident education time, which occurred biweekly on Wednesday mornings with half of the class attending in alternating weeks. We integrated the surgery residents into these workshop times, as it was pertinent for our perioperative teams to better their communication, DEI, and teamwork skills. Our workshop was held virtually, because of the COVID-19 pandemic and for ease of access for participants and facilitators. We incorporated a 1:5 facilitator-to-learner ratio to promote vulnerable conversations in Zoom breakout rooms. Although highly encouraged by residency leadership to the 25 first-year anesthesia residents and 15 senior surgery residents both in 2020 and 2021, residents were given an opt-out option to not participate.
Survey Design
Following the Kirkpatrick Model levels, the pre- and post-workshop surveys were used to evaluate the workshop's effects. All surveys were hosted on Qualtrics (Qualtrics, 2020).
Survey items were adapted from a previously published assessment tool with validity evidence. Our survey consisted of 12 items measured on a 5-point Likert scale (1 indicating strong disagreement to a 5 indicating strong agreement) and 4 open-ended items evaluating new insights, likes and dislikes about the workshop, and participants’ planned behavioral changes. We evaluated learners’ satisfaction with the workshop (level 1; reaction) as well as the acquisition of DEI knowledge (level 2; learning). A survey creator assessed each survey question's clarity and coherence by asking open-ended questions, such as “What do you think this question is asking you?” to 2 anesthesia fellows not involved in the intervention's conception and execution. The surveys were then iteratively revised and piloted with 10 second-year and 6 fourth-year medical students, followed by a 30-minute interview with each medical student, to produce our final survey content. The pre- and post-workshop surveys only differ in questions about prior and ideal DEI training in the pre-workshop survey and questions about what they liked and what could have been improved in the post-workshop survey.
Data Analysis
A paired t test analysis of the pre- and post-workshop surveys, using only data collected from participants who completed both surveys, was completed using SPSS (IBM Corp.) to evaluate increases in DEI knowledge. Statistical significance was defined as P < .05. Two data analysts conducted thematic analysis and coding on all open-ended responses, such as feedback about the workshop's most effective portions, from all survey respondents.
Institutional Review Board Statement
The University of California San Francisco Institutional Review Board deemed this study exempt from review (5/14/20). This manuscript adheres to the applicable EQUATOR (Enhancing the Quality and Transparency of Health Research) guidelines.
Results
Participant Characteristics and Demographics
In the pre-workshop survey, 83% (79 of 95) of 2020 respondents (CA-1, CA-2, CA-3, and surgical residents) and 68% (17 of 25) of 2021 respondents (new CA-1 residents) responded that they had not received formal DEI training before. Participants identified that actionable changes and brave and vulnerable group discussions were most important to include in their training.
Eighty-eight percent (n = 44 of 50) of UCSF anesthesiology CA-1 and 77% (n = 23 of 30) of surgery residents in their research year participated in this workshop over 4 separate sessions in September 2020 and 2021. Other participant demographics can be found in Table 3.
Table 3.
Demographic Characteristics of Residents Participating in Workshop
| Characteristics | Overall (n = 65) | Anesthesia (n = 44) | Surgery (n = 21) |
|---|---|---|---|
| Gender Identity | |||
| Male | 28 | 18 | 10 |
| Female | 34 | 24 | 10 |
| Non-Binary | 0 | 0 | 0 |
| Transgender | 0 | 0 | 0 |
| Prefer to Self-Describe | 0 | 0 | 0 |
| Prefer Not to Answer | 3 | 2 | 1 |
| Clinical Postgraduate Year | |||
| PGY-2 | 40 | 40 | 0 |
| PGY-4/Research Year | 11 | 0 | 11 |
| PGY-5 | 5 | 0 | 5 |
| Prefer Not to Answer/Missing | 9 | 4 | 5 |
| Race/Ethnicity (select all that apply) | |||
| White/Caucasian | 30 | 17 | 13 |
| Black/African American | 6 | 4 | 2 |
| American Indian and/or Alaska Native | 0 | 0 | 0 |
| Asian | 22 | 16 | 6 |
| Native Hawaiian and/or other Pacific Islander | 1 | 1 | 0 |
| Latinx | 5 | 3 | 2 |
| Other | 3 | 3 | 0 |
| Prefer Not to Answer | 4 | 1 | 3 |
| Identify as Underrepresented in Medicinea | |||
| Yes | 24 | 19 | 5 |
| No | 37 | 23 | 14 |
| Prefer Not to Answer | 4 | 2 | 2 |
| Identify as a member of the LGBTQIA+ Community | |||
| Yes | 11 | 9 | 2 |
| No | 50 | 32 | 18 |
| Prefer Not to Answer/Missing | 4 | 3 | 1 |
Abbreviation: LGBTQIA+: lesbian, gay, bisexual, transgender, queer, intersex, asexual, and other sexualities not aforementioned.
Underrepresented in Medicine/Underrepresented Minority is as defined by the UCSF School of Medicine: someone whose racial or ethnic makeup is from one of the following: African American/Black, Filipino, Hmong, Vietnamese, Hispanic/Latinx, Native American/Alaskan Native, Native Hawaiian/Other Pacific Islander, 2 or more races, when 1 or more are from the preceding racial and ethnic categories in this list.
Workshop and Facilitator Satisfaction
Ninety-seven percent (65 of 67) of the workshop participants completed the post-workshop survey. All 65 survey respondents evaluated the workshop positively. On a 5-point Likert scale, participants rated this workshop's importance, relevance, likelihood for being recommended to peers, and ability to reveal previously unknown implicit biases with a mean of 4.68 (SD ± 0.50), 4.71 (SD ± 0.49), 4.62 (SD ± 0.58), and 4.09 (SD ± 0.86), respectively. Participants rated the workshop facilitators’ preparation, ability to create an inclusive environment, and communication effectiveness a mean of 4.82 (SD ± 0.43), 4.92 (SD ± 0.32), and 4.85 (SD±0.40), respectively. In addition, 77% of participants agreed that the Unconscious Bias workshop gave them insight on biases they did not know they had (Table 4).
Table 4.
Post-Workshop Student Evaluations of Unconscious Bias Workshop and Facilitators (N = 65)
| Statement | Strongly Disagree, % | Somewhat Disagree, % | Neutral, % | Somewhat Agree, % | Strongly Agree, % | Mean (± SD) |
|---|---|---|---|---|---|---|
| This unconscious bias workshop is important to my training. | 0 | 0 | 2 | 29 | 69 | 4.7 (± 0.5) |
| I believe this unconscious bias workshop is relevant to my workplace. | 0 | 0 | 2 | 26 | 72 | 4.7 (± 0.5) |
| I would recommend this unconscious bias workshop to my peers. | 0 | 0 | 5 | 29 | 66 | 4.6 (± 0.6) |
| This unconscious bias workshop has given me insight on biases I didn't know I had. | 0 | 5 | 18 | 40 | 37 | 4.8 (± 0.4) |
| The facilitators were well prepared. | 0 | 0 | 2 | 15 | 83 | 4.9 (± 0.3) |
| The facilitators created a welcoming and inclusive environment for discussions. | 0 | 0 | 2 | 5 | 94 | 4.8 (± 0.4) |
| The facilitators effectively communicated this information. | 0 | 0 | 2 | 12 | 86 | 4.7 (± 0.5) |
Paired t Test Results
We matched 27 anesthesia participants (15 participants from the 2020 workshop and 12 participants from 2021) of the 44 who completed both the pre-workshop survey and post-workshop surveys for a paired t test analysis. These participants self-reported more strongly agreeing that they know how to define “unconscious bias,” that they have unconscious biases, and that these biases affect their interactions around clinical practice from a pre-workshop mean of 4.1 (SD ± 0.53) to a post-workshop mean of 4.8 (SD ± 0.42, P < .00002), 4.4 (SD ± 0.64) to 4.8 (SD ± 0.40, P = .001), and 3.3 (SD ± 1.32) to 3.9 (SD ± 0.87, P = .008), respectively (Figure 1). Unfortunately, most of the surgery residents did not complete the pre-workshop survey emailed to them, so we could not pair their responses.
Figure 1.
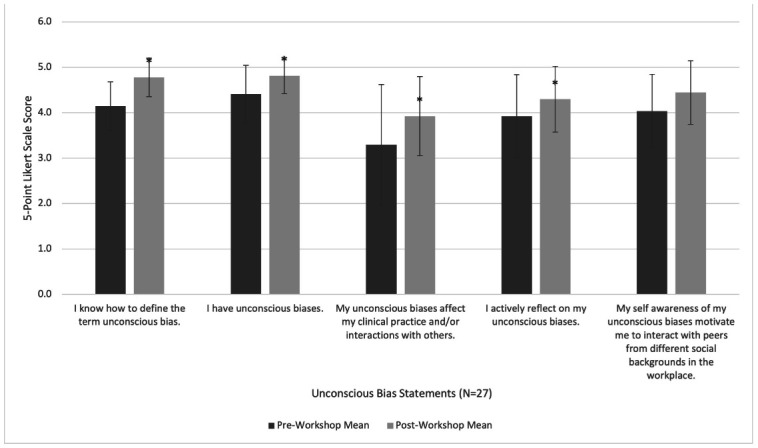
Post-workshop increases in mean agreement (±1 SD) with unconscious bias statements. Paired analysis showed that participants self-reported more strongly agreeing that they know how to define “unconscious bias,” that they have unconscious biases, and that these biases affect their interactions around clinical practice after the workshop. This was revealed using the successfully paired 27 anesthesia residents’ pre- versus post-workshop survey results. The “*” symbol indicates statistical significance with a P < .5.
Open-ended Results
Furthermore, when asked what participants liked most and what they want improved about the workshop, 48% of open-ended responses (n = 19 of 40) indicated they liked small group discussions and 32% (n = 10 of 31) of responses desired more time for small group discussions. Sixty-one percent (n = 11 of 18) identified unconscious biases they did not know they had. When asked what they would do differently post-workshop, 46% (n = 19 of 41) of participants reported they would make more efforts in recognizing their own biases, 32% (n = 13 of 41) said they would increase intentionality with patient care, and 34% (n = 14 of 41) said they would be more mindful and slower in their interactions with peers and patients to reduce bias. Other thematic analysis results can be found in Table 5.
Table 5.
Themes Derived From Unconscious Bias Workshop Participants’ Responses Regarding Their Experience in the Workshop and the Impact the Workshop Made
| Question Asked | Main Themes (count/responses to question)a |
|---|---|
| What did you like most about this workshop? | Small Group/Break Out Sessions (48%; 19/40) |
| Interactive and Engaging Exercises (25%; 10/40) | |
| Different Viewpoints and Departments (15%; 6/40) | |
| Open and Safe Spaces for Discussion (13%; 5/40) | |
| Effective Facilitators and Moderators (13%; 5/40) | |
| What could be improved in this workshop? | More Time for Small Group Discussions (32%; 10/31) |
| Nothing (16%; 5/31) | |
| Virtual Versus In-Person Preferences (13%; 4/31) | |
| Preparation Work Emailed Earlier in Advance (10%; 3/31) | |
| More Breaks in Workshop (10%; 3/31) | |
| What will you do differently moving forward? | More Effort in Recognizing Own Biases (46%; 19/41) |
| More Intentionality With Patient Care (32%; 13/41) | |
| Increased Mindfulness and Slowing Down in Patient/Peer Interactions (34%; 14/41) | |
| Creating a More Inclusive and Diverse Environment (15%; 6/41) | |
| Self-Education (15%; 6/41) | |
| Speaking Up and Out in Addressing Racism (12%; 5/41) | |
| What did you learn about yourself? | I Have Unconscious Biases (61%; 11/18) |
| Implicit Biases are a Worthwhile Challenge to Work On (33%; 6/18) | |
| Contemplation of Impact on Patient Interactions (11%; 2/18) |
The “(count)” number in parentheses describes the number of responses that included the respective theme. We drew these responses from 65 of the 67 workshop participants who responded to the post-workshop survey. However, it is important to note that not all 65 respondents wrote in a response to the open-ended questions, and some responses contained multiple themes.
Discussion
Our results indicate that our workshop objectives, of using transformative learning to increase (1) self-awareness of one's own implicit bias and (2) motivation to help mitigate that bias among perioperative trainees, were fulfilled. Our hypothesis that after attending our workshop, learners will have increased awareness of their own unconscious biases was also confirmed (Table 4 and Figure 1). As seen in Figure 1, there is a statistically significant increase in participants agreeing that they know how to define the term unconscious bias post-workshop, that they have unconscious biases, that these biases affect their clinical practice and/or interactions with others, and that they actively reflect on these biases. In addition, most participants agreed that the unconscious bias workshop gave them insight on biases they did not know they had (Tables 4 and 5). Building on this new awareness of their biases, participants seemed to have also learned ways to mitigate these biases, as evidenced by those self-reporting that they would make more efforts in recognizing their own biases, bring more intention and mindfulness into patient care, and slow down after the workshop.
Another unique finding from the workshop delivery was the positive assessment received for the facilitated small group discussions. Participants praised the intimate dialogue and desired more time in these groups, which were increased to 30 minutes per activity in the 2021 workshops from 20 minutes in the 2020 workshops. We believe the small groups created vulnerable settings that allowed participants to confront their true actions and challenge their ego-ideals, the inner image that one unconsciously and consciously desires to become. Recognizing one's distance from their ego-ideal can cause discomfort, especially regarding socially stigmatized topics like racism, making these spaces and competent facilitation critical to allowing participants to engage with their biases. High participant satisfaction suggests that the facilitated spaces created within the workshop were effective, possibly related to the facilitator selection and training. The large percentage of participants agreeing that the workshop was important (98%, 55 of 56 participants), relevant to their training (98%, 55 of 56 participants), and gave them insight on new biases (77%, 43 of 56 participants) suggests endorsement of the need for DEI education in perioperative residencies.
Several limitations of our study should be noted. Although we found many significant post-workshop changes, an incomplete number of paired surveys reduced the number of results available for analysis, decreasing power to detect post-workshop effects. The incomplete pairs were due to incomplete pre- or post-workshop survey responses and other learners forgetting their anonymous identification. Many 2020 surgery residents most likely did not complete the pre-workshop survey because of the anonymity of receiving a survey through email versus as an activity in the live introductory session for the anesthesia residents. Surgery residents in 2021 were accidentally not sent the pre-workshop survey. We hope to include future surgery residents in introductory sessions with better scheduling but also believe that other currently unknown barriers to participation should be studied. We also have improved the identification generator for future iterations of our survey. Another limitation comes from this intervention being done at a single institution with great diversity (race/ethnicity, gender, sexual orientation) in our faculty and trainees, providing us diverse facilitators. However, we believe our intervention is still adaptable to other institutions with different, or less diverse, populations. It is not necessary to have diverse facilitators, but it is important that recruited facilitators have prior DEI training, which is available through multiple platforms. Our facilitator's guide can be found in Appendix C. A recording of our facilitator training, which should be reviewed in addition to other DEI training before workshop facilitation, is available on request to Dr. Odi Ehie. Furthermore, one could recruit additional assets and allies across campus by attending institution-wide or interdisciplinary DEI trainings.
Despite these limitations, the overall positive feedback indicates that this session could be applicable to a wider group of trainees. Specifically, the 95%, or 53 of 56 participants, agreeing that they would recommend the workshop to peers supports this generalizability. This 2-hour workshop could even be shortened to a 90-minute session to accommodate scheduling restrictions, as our lead principal investigator has by removing the third small group activity for a version taught to faculty. This workshop has also been taught to medical students, but no data on its efficacy for faculty or medical students were collected. The largest barrier is finding protected didactic time to deliver this curriculum to a large body of learners synchronously, so that the facilitated time can be more cost-effective for faculty. This protected didactic time is necessary to better engage the trainees and enhance their experience with others’ perspectives. We have gathered data about lasting changes in participant approaches to unconscious bias by reevaluating participants 1 year after the DEI curriculum's end but have not yet sufficiently analyzed these data to be presented. We also repeat an unconscious bias workshop a year later to ensure retention of the knowledge gained from the workshop.
This unconscious bias workshop fills an important DEI education gap in our institution's graduate medical curricula by spurring self-reflection critical for tackling one's biases and discussing tools for mitigating these biases. This study adds to a growing body of work trying to better understand and approach implicit bias as a health care issue. We recommend that this workshop be further developed, tested, and disseminated to residents nationwide, as reducing the impact of implicit biases on long-marginalized communities is paramount to equity.
Acknowledgments
We give special thanks to Ms. Gillian Earnest for her support with statistical analysis.
Appendix A. Pre- and Post-Workshop Survey Questions
| Survey Question | Question Included in Pre-workshop Survey, Post-workshop Survey, or Both? |
|---|---|
| 1. Have you received formal Diversity, Equity, and Inclusion (DEI) training before? | Pre-workshop |
| 2. What was most effective in that DEI training? | Pre-workshop |
| 3. What does an ideal DEI training look like for you? | Pre-workshop |
| 4. Anything else you'd like to share? | Pre-workshop |
| 5. How strongly do you agree with the following? | Both |
| • I know how to define the term unconscious bias. | Both |
| • I have unconscious biases. | Both |
| • My unconscious biases affect my clinical practice and/or interactions with others. | Both |
| • I actively reflect on my unconscious biases. | Both |
| • My self-awareness of my unconscious biases motivates me to interact with peers from different social backgrounds in the workplace. | Both |
| 6. The following True/False questions are meant to evaluate your general understanding of the terms, and not what you would do personally | Both |
| • Unconscious bias is defined as a strong inclination of the mind or a preconceived opinion about someone or something. | Both |
| • Stereotype suppression is the active suppression of stereotypical thoughts about an individual of a different social background that usually results in increased social encounters. | Both |
| 7. Please answer the following 4 questions in the context of life in general, and not just in work settings. Choose the response that is most applicable to you up to this point: | Both |
|
Both |
|
Both |
|
Both |
|
Both |
| 8. What department are you in? | Both |
| 9. Which year of anesthesia/surgery postgraduate training are you? | Both |
| 10. Race/ethnicity: (Choose all that apply) | Both |
| 11. Do you identify as Underrepresented In Medicine as defined by UCSF School of Medicine? Includes African American/Black, Asian (Filipino, Hmong, or Vietnamese only), Hispanic/Latinx, Native American/Alaskan Native, Native Hawaiian/Other Pacific Islander, or 2 or more races (when 1 or more are from the preceding racial and ethnic categories in this list) | Both |
| 12. Gender identity: Choose all that apply. | Both |
| 13. Do you identify as a member of the LGBTQIA+ community? | Both |
| 14. Do you plan to apply what you've learned in this unconscious bias workshop within your workplace? | Post-Workshop |
| 15. If yes, how will you apply what you've learned in this unconscious bias workshop within your workplace? | Post-Workshop |
| 16. What did you like the most about this unconscious bias workshop? | Post-Workshop |
| 17. What could be improved in this unconscious bias workshop? | Post-Workshop |
| 18. Anything else you'd like to share about your experience in this workshop? | Post-Workshop |
Appendix B. UCSF Department of Anesthesia Unconscious Bias Workshop
Learner's Guide
Session Authors: Odinakachukwu Ehie, LaMisha Hill, Rebecca Chen, and Janette Tang
Session Dates:
Session Duration: 2 hours
Faculty: Small group facilitators
Format: 2-hour group session with small breakout groups
Session Overview
In this 2-hour session, learners will be presented current data on unconscious bias seen within residency programs and perform self-reflective small group exercises.
Curriculum Objectives
By the end of these sessions, learners will be able to
Explain 2 key differences between bias and unconscious bias by providing at least 1 example of each.
Assess one's own unconscious biases in relation to the workshop exercises in a small group discussion.
Describe 2 tools that can be used for reducing bias in clinical spaces.
Identify 3 ways to apply concepts around unconscious bias to be intentional in the clinical environment.
Model 2 ways to successfully interact with socially dissimilar colleagues and patients.
Pre-Session Preparation
Required reading prior to workshop
Morin, Rich. 2015. Exploring Racial Bias Among Biracial and Single-Race Adults: The IAT. Pew Research Center, Washington, DC: August 19, 2015.
Burgess et al. Reducing racial bias among health care providers: lessons from social-cognitive psychology. Society of General Internal Medicine. 2007;22:882-887.
Green et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. Journal of General Internal Medicine. 2007;22(9):1231-1238.
Appendix C. UCSF Department of Anesthesia Unconscious Bias Workshop
Faculty Facilitator's Guide
Session Authors: Odinakachukwu Ehie, MD, LaMisha Hill, PhD, Rebecca Chen, BS, and Janette Tang, BS, MS
Session Dates:
Session Time: 2 hours
Faculty: Small group facilitators from
Format: 2-hour group session with small breakout groups
Session Overview
In this 2-hour session, learners will be presented current data on unconscious bias seen within residency programs and perform self-reflective small group exercises.
Curriculum Objectives
By the end of these sessions, learners will be able to
Explain 2 key differences between bias and unconscious bias by providing at least 1 example of each.
Assess one's own unconscious biases in relation to the workshop exercises in a small group discussion.
Explain 2 reasons for reducing bias in a safe and nonthreatening space.
Identify 3 ways to apply concepts around unconscious bias to be more intentional in the clinical environment.
Model 2 ways to successfully interact with socially dissimilar colleagues and patients.
Session Outline
| Duration | Topic | Who |
|---|---|---|
| 10 min | Introduction of Large Group/Goals and Objectives | Facilitator and Learners |
| 10 min | Introduction Within Small Group: Name one thing you are hoping to get from this workshop | Small Group of 5 Learners + 1 Facilitator |
| 20 min | Whom To Leave Behind Exercise | Small Group of 5 Learners + 1 Facilitator |
| 2 min | Large Group Debrief | Facilitator and Learners |
| 10 min | Implicit Bias Test | Learners |
| 13 min | Small Group Debrief | Small Group of 5 Learners + 1 Facilitator |
| 2 min | Large Group Debrief | Facilitator and Learners |
| 8 min | Break | |
| 10 min | Bias vs. Unconscious Bias Lecture (Data) | Facilitator and Learners |
| 15 min | How Diverse Is Your Universe? Exercise | Small Group of 5 Learners + 1 Facilitator |
| 2 min | Large Group Debrief | Facilitator and Learners |
| 7 min | Stereotype Lecture | Facilitator and Learners |
| 5 min | Online Post-curriculum Survey | Learners |
| 5 min | Wrap Up: Share Ideas for Diversity Curriculum | Facilitator and Leaners |
Pre-Session Preparation
Recommended reading before workshop:
Morin, Rich. 2015. Exploring Racial Bias Among Biracial and Single-Race Adults: The IAT. Pew Research Center, Washington, DC: August 19, 2015.
Burgess et al. Reducing racial bias among health care providers: lessons from social-cognitive psychology. Society of General Internal Medicine. 2007;22:882-887.
Green et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. Journal of General Internal Medicine. 2007;22(9):1231-1238. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2219763/#
Before this session facilitators should
Review the Whom To Leave Behind Exercise: https://ucsf.app.box.com/file/711995408991
Take the Implicit Association Test: https://implicit.harvard.edu/implicit/takeatest.html
Unconscious Bias Session
Intro in a large group setting (10 minutes)
Review goals and objectives and house rules as a large group
-
Intro in a small group setting (10 minutes)
-
»
Name one thing you are hoping to get from this workshop
-
»
Name
-
»
Pronoun
-
»
Department that you are from
-
»
-
Whom To Leave Behind Exercise (20 minutes)
-
»
Small Group Instructions
-
›
As a small group facilitator, instruct the learners that they have 10 minutes to deliberate and unanimously agree on which 8 people to save after reading the instructions by ranking each individual.
-
›
By no later than 8:30 am, please start debriefing as a small group.
-
›
Possible debrief questions:
-
–
Who assumed the accountant was male?
-
–
Who assumed the militant African American student was male?
-
–
Who assumed the famous novelist was male?
-
–
Who assumed the racist armed police officer was male?
-
–
Who assumed the 60-year-old Jewish university administrator was male?
-
–
-
›
Large Group Debrief (2 minutes)
-
›
-
»
Harvard Implicit Bias Test (https://implicit.harvard.edu/implicit/takeatest.html)
-
›
Learners to complete this test in 10 minutes; for the sake of time please focus on the questions below, not IAT validity or structure
-
›
Small Group Debrief Questions (13 minutes)
-
–
What surprised you about your results?
-
–
What feelings did you notice bubbling up?
-
–
How does unconscious bias manifest in your educational training? In your workplace?
-
–
How does structural racism manifest in your educational training? In your workplace?
-
–
-
›
Large Group Debrief (2 minutes)
-
›
-
»
Bias Versus Unconscious Bias lecture by large group facilitator (10 minutes)
-
»
Exercise on How Diverse Is Your Universe? (10 minutes)
-
›
Note: This section uses a weblink to Poll EV. The host will post the link in the group chat during the presentation (https://pollev.com/odinakachukw765)
-
›
As a large group, the following poll questions will be asked toward the group.
-
–
Who was the last guest invited to your house for dinner?
-
–
Who was the last person you went out with socially?
-
–
Who makes up the majority of residents in your entire program?
-
–
Who is your closest friend?
-
–
Who made up the majority of people in your childhood community?
-
–
-
›
As a small group, the following debriefing questions will be asked by the assigned facilitator.
-
–
Did you ever stop to think how often you communicate with people outside of your group?
-
–
Did you consider yourself to be someone who often interacted with others? Do you still?
-
–
What did your visual representation show you?
-
–
If you have little to no interaction with people outside of your group, how does that affect your ability to deliver care to a diverse group of patients?
-
–
If you have little to no exposures to others, do you think you should make an effort to be more involved? If so how?
-
–
What are 3 ways to successfully interact with socially dissimilar colleagues and patients?
-
–
Any other questions or comments?
-
–
-
›
Large group debrief (5 minutes)
-
›
-
»
Stereotype Lecture by large group facilitator (7 minutes)
Post-curriculum Survey (5 minutes)
Wrap Up: In one word, how would you describe this workshop? https://PollEv.com/free_text_polls/GoxSaH834LAeEoNxq35um/respond
Footnotes
Conflicts of interest: None
Financial disclosures: Odinakachukwu A. Ehie received research funding from the Research in Education Grant-Foundation of Anesthesia Education and Research (FAER) as the principal investigator of the Diversity, Equity, and Inclusion Curriculum for Anesthesia and Surgery Residents. Rebecca P. Chen and Janette Tang received research funding from the UCSF School of Medicine Summer Explore Research Fellowship.
References
- 1.Allyship: What it means to be an ally in social work. [Accessed July 10, 2023]. https://socialwork.tulane.edu/blog/allyship/
- 2.Delgado R, Stefancic J. Critical Race Theory (Third Edition): An Introduction. New York, NY: NYU Press; 2017. [Google Scholar]
- 3.Akhtar S. Comprehensive Dictionary of Psychoanalysis. London Karnac Books; 2009. [Google Scholar]
- 4.Bias, Module 3-1 Georgetown University Center for Child and Human Development National Center for Cultural Competence: Bias. [Accessed July 10, 2023]. https://nccc.georgetown.edu/bias/module-3/1.php
- 5.Jackson PW. Life in Classrooms. New York: Teachers College Press; 1968. [Google Scholar]
- 6.Crenshaw K. On Intersectionality: Essential Writings. Faculty Books. [Published online March 1, 2017]. [Accessed July 10, 2023]. https://scholarship.law.columbia.edu/books/255
- 7.DEI Glossary | Working at Cornell [Accessed July 10, 2023]. https://hr.cornell.edu/culture/inclusion-belonging/learning-and-development/dei-glossary
- 8.Fosberg A, Bynum A, Tripp H. How do you distinguish effective allyship from performative allyship? Penn State Law | University Park, PA. [Published February 26, 2021]. [Accessed July 10, 2023]. https://pennstatelaw.psu.edu/news/effective-allyship-part-one
- 9.Monteith MJ, Sherman JW, Devine PG. Suppression as a stereotype control strategy. Pers Soc Psychol Rev. 1998;2(1):63–82. doi: 10.1207/s15327957pspr0201_4. [DOI] [PubMed] [Google Scholar]
- 10.Mezirow J. Transformative learning: theory to practice. New Directions for Adult and Continuing Education. 1997;1997(74):5–12. [Google Scholar]
- 11.van Ryn M, Hardeman R, Phelan SM, et al. Medical school experiences associated with change in implicit racial bias among 3547 students: a medical student CHANGES study report. J Gen Intern Med. 2015;30(12):1748–56. doi: 10.1007/s11606-015-3447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94(8):666–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Peel JK, Flexman AM, Cygler J, Kirkham KR, Lorello GR. Standing out or fitting in: a latent projective content analysis of discrimination of women and 2SLGBTQ+ anesthesiologists and providers. J Clin Anesth. 2022;80:110884. doi: 10.1016/j.jclinane.2022.110884. [DOI] [PubMed] [Google Scholar]
- 14.Miller J, Katz D. Gender differences in perception of workplace experience among anesthesiology residents. J Educ Perioper Med. 2018;20(1):E618. [PMC free article] [PubMed] [Google Scholar]
- 15.Hu YY, Ellis RJ, Hewitt DB, et al. Discrimination, abuse, harassment, and burnout in surgical residency training. N Engl J Med. 2019;381(18):1741–52. doi: 10.1056/NEJMsa1903759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Accreditation Council for Graduate Medical Education ACGME Common Program Requirements (Residency) [Published online July 1, 2019]. [Accessed February 26, 2021]. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRResidency2019.pdf
- 17.Crenshaw K. Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics. The University of Chicago Legal Forum. 1989;140:139–67. [Google Scholar]
- 18.Gonzalez CM, Garba RJ, Liguori A, et al. How to make or break implicit bias instruction: implications for curriculum development. Academic Medicine: Journal of the Association of American Medical Colleges. 2018;93:S74–S81. doi: 10.1097/ACM.0000000000002386. 11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 57th Annual Research in Medical Education Sessions. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moon T. Project implicit: implicit association test. [Accessed September 15, 2023]. https://implicit.harvard.edu/implicit/takeatest.html Published 2011.
- 20.Diversity, Equity, and Inclusion Champion Training (Postponed as of December 2022) | UCSF Medical Education. [Accessed July 8, 2023]. https://meded.ucsf.edu/faculty-educators/faculty-development-all/diversity-equity-and-inclusion-champion-training-postponed-december-2022


