Abstract
Introduction:
A negative relationship between Adverse Childhood Experiences (ACEs) and both physical and mental health in adulthood is well established, as is the positive impact of parenting on child development and future health. However, few studies have investigated unique influences of ACEs and positive parenting together within a large, diverse early childhood sample.
Method:
The study used data on all children ages 0-5 (n=29,997) from the National Survey of Children’s Health (NSCH) 2011/12 to examine effects of positive parenting practices and ACEs on early childhood social-emotional wellbeing and general development. All analyses were performed in 2017 and 2018.
Results:
More than a third of the sample reported experiencing at least one ACE. More than a fourth (26.7%) met study criteria for low social-emotional wellbeing, and 40.1% met criteria for developmental concerns. ACE counts exhibited negative marginal associations with social-emotional and developmental risks, while the count of positive parenting practices showed independent protective effects. Risks associated with an absence of positive parenting were often greater than those of 2+ ACEs, even among no/low adversity families. The population attributable fractions for low wellbeing and developmental risks were 19.1% and 7.8% when adopting all positive parenting practices and 10.0% and 11.5% when eliminating ACEs.
Conclusion:
ACE count was negatively related to both social-emotional wellbeing and development in early childhood; however, positive parenting practices demonstrated robust protective effects independent of the number of ACEs. This evidence further supports promotion of positive parenting practices at home, especially for children exposed to high levels of adversity.
Introduction
Adverse childhood experiences (ACEs) have garnered public attention for their cumulative negative consequences on health in adulthood. 1-4 Many have theorized the accumulation of adversities leads to excessive or prolonged stress, also known as toxic stress. 5 In the absence of sensitive and responsive caregivers, this stress can disrupt brain development which, in turn, causes life-long impairments. Recently, ACEs also have been reported for negative effects among adolescents or young people 4,6,7 and even children.8
However, few studies have examined the isolated effects of ACEs on health or health precursors that occur during very early stages of childhood. Many early childhood programs, practitioners, and researchers have adopted a stance that views child development as a zero-sum game of negative outcomes from toxic stress and positive, adaptive outcomes from “protective factors” that build resilience.9 As Garner and Shonkoff 10 noted “the essence of toxic stress is the absence of buffers [i.e., protective factors] needed to return the physiologic stress response to baseline.” The Centers for Diseases Control and Prevention (CDC) were early supporters of child adversity research and now promote the creation of “Safe, Stable, and Nurturing relationships and environments” for all children.11 Similarly, Strengthening Families™ is a widely implemented program using the protective factors approach for the prevention of childhood adversities.12
One commonly cited, modifiable protective factor is parenting.13 Use of key parenting practices cannot only protect a child from adversity but can also stimulate positive developments that enhance child’s resiliency. Last year, the National Academy of Sciences, Engineering, and Medicine (NAS) released a report entitled Parenting Matters: Supporting Parents of Children Ages 0-8 14 which underscored the perceived importance of quality parenting for child development. Despite popularity of this view, there is limited information available on the combined impact of childhood adversities and parenting practices on development of young children.14 One major reason for a lack of evidence is that most clinical trials obtain selective samples with restricted variability on parenting and/or ACE outcomes. Equipped with a large, nationally representative survey sample, this study aimed 1) to examine the relationship between ACEs and both wellbeing and development during early childhood (0 to 5 years), and 2) to examine effects of positive parenting practices (PPPs), in the presence and absence of adverse experiences, on these same outcomes. Furthermore, in attempts quantify the public health benefits of prevention, several studies have reported population attributable fractions (PAFs) 15 of ACE reductions.16,17 To highlight potential population impact, we aimed 3) to estimate PAFs of ACEs and PPPs on low social-emotional wellbeing or developmental risks among young children.
Method
Data source and Study samples
This study utilized data obtained from the National Survey of Children’s Health (NSCH) 2011/12- a nationally representative, cross-sectional, list-assisted random-digit-dial telephone survey to evaluate children’s health and wellbeing. The detailed design methodology was explained elsewhere.18 Participating parents responded to questions about a single randomly selected child. The current study only included children ages 0-5 to evaluate wellbeing, development, experienced adversities, and parenting practices (n=29,997, 31.4% of the total NSCH sample).
Dependent variable
The NSCH 2011/12 flourishing items 19 were used to evaluate child’s social-emotional wellbeing. The four flourishing questions were developed with an expert panel composed of individuals in the field of survey methodology, children's health, community organizations, and family leaders.19 The items selected for children ages 6 months to 5 years asked parents/guardians to report the past month frequency for the following social-emotional behaviors: (1) [He/She] is affectionate and tender with you, (2) [He/She] bounces back quickly when things don’t go [his/her] way, (3) [He/She] shows interest and curiosity in learning new things, (4) [He/She] smiles and laughs a lot. For purposes of this study, responses were dichotomized into ‘1,’ for “always/usually”, and ‘0,’ for “sometimes/rarely/never.” If there was at least one response of “sometimes/rarely/never” (i.e., sum score < 4), the child was classified as possessing low social-emotional wellbeing.
The developmental risks for children ages 4 months – 5 years old were examined by the Parents’ Evaluation of Developmental Status (PEDS), a screening instrument to assess parent concerns about developmental delay of children under 8 years.20 Responses of “a lot” or “ a little” are typically categorized as concerning, and overall classifications of high, moderate, low, and no developmental delay risks can be constructed as explained elsewhere.19 Using this classification system, we operationalized developmental delay risk as binary indicator of any overall risk (i.e., low, moderate, high) on the PEDS.
Independent variable
Adverse childhood experiences:
The NSCH 2011/12 employed 9 items addressing the following Adverse Childhood Experiences (ACEs): (1) low income, (2) divorce/separation of parent, (3) lived with someone with alcohol/drug problem, (4) community violence, (5) lived with someone who was mentally ill or suicidal family member, (6) witness to intimate partner violence (IPV), (7) parent served time in jail, (8) treated or judged unfairly due to race/ethnicity, (9) death of parent. For items 2 – 9, parents/guardians provided yes/no responses to questions of whether their child had ever experienced the adversity. The exception, item 1, asked: “How often has it been very hard to get by on your family's income, for example, it was hard to cover the basics like food or housing?” Answers to this question were re-categorized into ‘yes,’ for a response of “very/somewhat often,” and ‘no,’ for a response of “not often/never.” We categorized ACE (summed) scores into 4 levels: 0, 1, 2-3, and 4 or more.
Parenting practices:
We utilized questions about parenting practices and family routine care. Responders provided the number of days in the past week where they engaged the child in the following activities: reading stories, storytelling/singing, having meal with all family members, playing with peer children, and going out. Responders also provided the number hours or minutes that the child spent in front of a television. For each activity, a positive parenting practice (PPP) binary indicator was constructed and operationalized as ‘yes’ whenever the frequency of reading, storytelling/singing, family meal, playing with peers, and going out exceeded 3 days and whenever TV watching fell 2 hours and below. All binary indicators were summed to produce a PPPs count variable.
Covariates:
Characteristics of children (sex, age, race/ethnicity) and household (highest education level of household) were included in the statistical models as control variables. Race/ethnicity was categorized as non-Hispanic White, non-Hispanic Black, Hispanic, or other race/multi-race. Education level was coded as more than high school, high school graduate, and less than high school. Family income was initially included in the modeling but latter dropped due to the high degree of overlap with the frequently endorsed low-income ACE item.
Statistical analysis
First, we estimated population proportions for all levels of the demographics, PPP counts, ACE counts, and wellbeing and developmental risk indicators. Second, we estimated proportions of ACE counts among children ages 0-2 and 3-5 years. Third, we conducted a block-hierarchical, multiple logistic regression to examine effects of ACEs, demographic controls, and PPPs on risks for low socio-emotional wellbeing and developmental delay. Finally, we estimated the population attributable fractions (PAFs) 15 of ACEs and PPPs on both outcomes. A PAF represents the predicted proportional reduction in the number of cases (e.g., number at-risk for development delay) when the population proportion of a risk or protective factor is (hypothetically) altered to a new (typically ideal) value. Results are presented for ideal alternatives where either all 6 PPPs are universally adopted or where all ACEs are eliminated. All analyses adjusted for the complex survey design variables (sampling weights, clusters, and strata) using the SVY procedures of STATA.21 R version 3.3.1 was used for producing figures.22 All analyses were performed in 2017 and 2018.
Results
Table 1 provides proportion estimates for the child demographics, the counts of PPPs and ACEs, and wellbeing and developmental risk indicators. More than a third (36.7%) had experienced at least one ACE. Most of the children (89.2%) experienced 3 or more PPPs. Roughly a quarter of the children (26.7%) met study criteria for low social-emotional wellbeing, and two out of every five (40.1%) met PEDS criteria for risks of developmental delay.
Table 1.
Description of child and household
| Unweighted (n= 29,997) | Weighted | ||||
|---|---|---|---|---|---|
| n/ mean (SD) | % | %/ mean (SE) | (95% CI) | ||
| Child's characteristics | |||||
| Age | (Year) | 2.55 (1.7) | 2.53 (0.02) | (2.48, 2.57) | |
| Sex | Male | 15,233 | 50.8% | 49.0% | (47.7, 50.2) |
| Female | 14,742 | 49.1% | 51.0% | (49.8, 52.3) | |
| Race | White, non Hispanic | 18,228 | 62.3% | 50.1% | (48.8, 51.3) |
| Hispanic | 4,609 | 15.8% | 26.4% | (25.2, 27.7) | |
| Black, non Hispanic | 2,698 | 9.2% | 12.2% | (11.4, 13.0) | |
| Other, multi race | 3,734 | 12.8% | 11.4% | (10.6, 12.2) | |
| Household characteristics | |||||
| Highest education in household | More than high school | 22,995 | 78.1% | 67.7% | (66.4, 68.9) |
| High school graduate | 4,584 | 15.6% | 20.5% | (19.4, 21.6) | |
| Less than high school | 1,863 | 6.3% | 11.8% | (10.9, 12.9) | |
| Parenting practices | |||||
| Positive Parenting score | 0 - 2 | 2,420 | 8.1% | 10.8% | (9.9, 11.6) |
| 3 | 3,983 | 13.3% | 15.3% | (14.4, 16.3) | |
| 4 | 7,553 | 25.2% | 25.2% | (24.2, 26.3) | |
| 5 | 10,134 | 33.8% | 31.4% | (30.3, 32.6) | |
| 6 | 5,907 | 19.7% | 17.2% | (16.4, 18.1) | |
| Childhood Adversity experiences | |||||
| ACE score | 0 | 19,810 | 66.8% | 63.3% | (62.1, 64.6) |
| 1 | 6,351 | 21.4% | 24.1% | (23.0, 25.3) | |
| 2 - 3 | 2,676 | 9.0% | 9.9% | (9.2, 10.7) | |
| 4+ | 804 | 2.7% | 2.6% | (2.3, 3.0) | |
| Children's wellbeing and development | |||||
| Socio-emotional wellbeing | High | 21,413 | 77.6% | 73.3% | (72.1, 74.5) |
| Low | 6,199 | 22.5% | 26.7% | (25.5, 27.9) | |
| Developmental concerns (PEDS) | No risk | 17,705 | 62.0% | 59.9% | (58.6, 61.2) |
| Any risks | 10,835 | 38.0% | 40.1% | (38.8, 41.4) | |
Across the nine individual ACEs, low income was the most frequent type among all children (as shown in Table 2). The proportion of low income children in both age strata were comparable (24.5 and 26.1%, respectively), while other types of ACEs were often twice as frequent in the older, relative to younger, age grouping. For younger children, the most frequently endorsed PPPs were limited TV watching (87.9%), family meal (84.4%), and storytelling/singing (83.9%). Family meals was the most popular practice among older children (83.8%), and four other practices- limited TV watching, reading, storytelling/singing, and playing with peers, were also highly prevalent.
Table 2.
Proportions of adverse experiences and positive parenting practices among young children
| 0 - 2 years old | 3 - 5 years old | |||
|---|---|---|---|---|
| Weighted% | (95% CI) | Weighted% | (95% CI) | |
| Childhood Adversity experiences | ||||
| 1. Low income | 24.5% | (22.9, 26.1) | 26.1% | (24.6, 27.8) |
| 2. Divorce/ separation | 5.4% | (4.6, 6.2) | 14.0% | (12.8, 15.4) |
| 3. Drug/alcohol abuse | 3.5% | (3.0, 4.2) | 7.4% | (6.5, 8.4) |
| 4. Community violence | 1.4% | (1.1, 1.9) | 4.0% | (3.4, 4.6) |
| 5. Family mental illness | 3.9% | (3.2, 4.6) | 7.1% | (6.3, 8.0) |
| 6. Intimate partner violence | 2.2% | (1.8, 2.7) | 5.8% | (5.0, 6.8) |
| 7. Parent incarceration | 2.9% | (2.4, 3.6) | 5.9% | (5.2, 6.7) |
| 8. Racial discrimination | 0.6% | (0.3, 1.2) | 1.2% | (0.9, 1.6) |
| 9. Parent died | 0.6% | (0.3, 1.2) | 1.1% | (0.9, 1.5) |
| Positive parenting practices | ||||
| Reading a book (4 + days /week) | 65.7% | (63.9, 67.5) | 77.5% | (75.9, 79.0) |
| Storytelling/ Singing (4 + days /week) | 83.9% | (82.3, 85.3) | 74.9% | (73.3, 76.4) |
| Playing with peer (4 + days /week) | 39.4% | (37.6, 41.2) | 75.1% | (73.5, 76.5) |
| Going out (4 + days /week) | 52.9% | (51.0, 54.7) | 51.7% | (49.9, 53.4) |
| Family meal (4 + days /week) | 84.4% | (83.0, 85.7) | 83.8% | (82.4, 85.1) |
| TV watching (<= 2 hours/day) | 87.9% | (86.7, 89.0) | 76.9% | (75.4, 78.3) |
To evaluate the potential for confounding of ACE and PPP effects, we next examined the relationships between the count variables for each construct. Somewhat surprisingly, while there is a significant correlation between the counts (r = −0.07 and −0.08 for younger and older strata, p’s < 0.001), the effect was small and would not typically indicate severe levels of confounding. [See also Figure 1 of supplemental material.] Table 3 shows the effects of the number of ACEs and PPPs on wellbeing and general development. ACEs displayed a significant negative gradient with low social-emotional wellbeing and risk for developmental delay (model 1). All odds ratios involving the lowest ACE score group remained significant after adjusting for the demographic covariates in model 2, and after adding PPPs in model 3. The odds ratios [OR] of model 3 increased from 1.30 (95% C.I. 1.11-1.52) for 1 ACE up to 1.59 for 4+ ACEs (1.18-2.14) for low socio-emotional wellbeing and 1.50 (1.31-1.72) to 3.42 (2.50-4.69) for risks of developmental delay. The ordered gradation of ACEs effects was altered somewhat in the covariate-adjusted models (2 and 3) of the social-emotional, but not general development, outcome and was characterized by virtually indistinguishable risks for the middle two ACE categories (scores of 1 vs 2-3). Altered ACEs effect ordering was also present in social-emotional (but not general development) models for each age subgroup (results not shown). PPPs showed significant protective effects for both outcomes after controlling effects of ACEs. Providing all PPPs resulted in approximately half the odds of meeting criteria for social-emotional (OR, 95%C.I.: 0.46, 0.35-0.61) and general developmental (0.55, 0.44-0.70) risks. These protective effects were similar in the separate age-group analyses. Finally, inclusion of interaction terms between ACEs and parenting indicators for both outcome models resulted in, at best, weak evidence for effect modification (see Figure 2 of the supplemental material).
Table 3.
Effects of ACEs and number of parenting practices on wellbeing and development of children
| 1. Low socio-emotional wellbeing | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 2b | Model 3 | ||||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | ||
| ACE score | |||||||||
| (ref: 0) | 1 | 1.52 | (1.31-1.77) | 1.33 | (1.14-1.55) | 1.30 | (1.11-1.52) | ||
| 2-3 | 1.60 | (1.32-1.94) | 1.33 | (1.08-1.63) | 1.29 | (1.05-1.58) | |||
| 4+ | 1.82 | (1.37-2.42) | 1.60 | (1.19-2.16) | 1.59 | (1.18-2.14) | |||
| Covariates | |||||||||
| Age | (year) | 1.06 | (1.02-1.10) | 1.08 | (1.04-1.13) | 1.07 | (1.03-1.12) | ||
| Sex (ref: female) | Male | 1.24 | (1.09-1.41) | 1.25 | (1.10-1.42) | 1.24 | (1.09-1.41) | ||
| Race (ref: White, non Hispanic) | Hispanic | 1.19 | (0.99-1.43) | 1.08 | (0.90-1.30) | 1.08 | (0.90-1.31) | ||
| Black, non Hispanic | 2.00 | (1.68-2.39) | 1.88 | (1.57-2.25) | 1.84 | (1.54-2.21) | |||
| Other, Multiracial | 1.63 | (1.34-1.98) | 1.51 | (1.24-1.84) | 1.53 | (1.25-1.86) | |||
| Parental education (ref: >high school) | High school graduate | 1.69 | (1.44-1.99) | 1.62 | (1.38-1.91) | 1.56 | (1.32-1.84) | ||
| Less than high school | 2.35 | (1.87-2.96) | 2.13 | (1.68-2.70) | 2.05 | (1.62-2.60) | |||
| Number of parenting practices | |||||||||
| (ref: 0-2) | 3 | 0.73 | (0.56-0.95) | 0.73 | (0.56-0.96) | ||||
| 4 | 0.68 | (0.53-0.87) | 0.68 | (0.53-0.87) | |||||
| 5 | 0.49 | (0.39-0.63) | 0.50 | (0.39-0.64) | |||||
| 6 | 0.45 | (0.34-0.60) | 0.46 | (0.35-0.61) | |||||
| 2. General developmental risks | |||||||||
| Model 1 | Model 2 | Model 2b | Model 3 | ||||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | ||
| ACE score | |||||||||
| (ref: 0) | 1 | 1.71 | (1.50-1.94) | 1.53 | (1.34-1.75) | 1.50 | (1.31-1.72) | ||
| 2-3 | 2.30 | (1.92-2.75) | 1.91 | (1.57-2.32) | 1.86 | (1.54-2.26) | |||
| 4+ | 4.07 | (3.04-5.45) | 3.43 | (2.51-4.66) | 3.42 | (2.50-4.69) | |||
| Covariates | |||||||||
| Age | (year) | 1.20 | (1.16-1.24) | 1.23 | (1.19-1.28) | 1.21 | (1.17-1.25) | ||
| Sex (ref: female) | Male | 1.43 | (1.27-1.60) | 1.43 | (1.28-1.60) | 1.43 | (1.28-1.60) | ||
| Race (ref: White, non Hispanic) | Hispanic | 1.41 | (1.20-1.65) | 1.30 | (1.11-1.53) | 1.30 | (1.11-1.53) | ||
| Black, non Hispanic | 1.34 | (1.14-1.58) | 1.31 | (1.11-1.55) | 1.25 | (1.05-1.47) | |||
| Other, Multiracial | 1.42 | (1.19-1.69) | 1.32 | (1.11-1.58) | 1.34 | (1.12-1.60) | |||
| Parental education (ref: >high school) | High school graduate | 1.31 | (1.13-1.52) | 1.33 | (1.15-1.54) | 1.22 | (1.06-1.42) | ||
| Less than high school | 1.57 | (1.26-1.95) | 1.48 | (1.19-1.85) | 1.38 | (1.11-1.73) | |||
| Number of parenting practices | |||||||||
| (ref: 0-2) | 3 | 0.84 | (0.66-1.08) | 0.85 | (0.66-1.09) | ||||
| 4 | 0.68 | (0.55-0.85) | 0.68 | (0.55-0.86) | |||||
| 5 | 0.54 | (0.44-0.68) | 0.56 | (0.45-0.69) | |||||
| 6 | 0.53 | (0.42-0.68) | 0.55 | (0.44-0.70) | |||||
Colored values were significant (p<0.05).
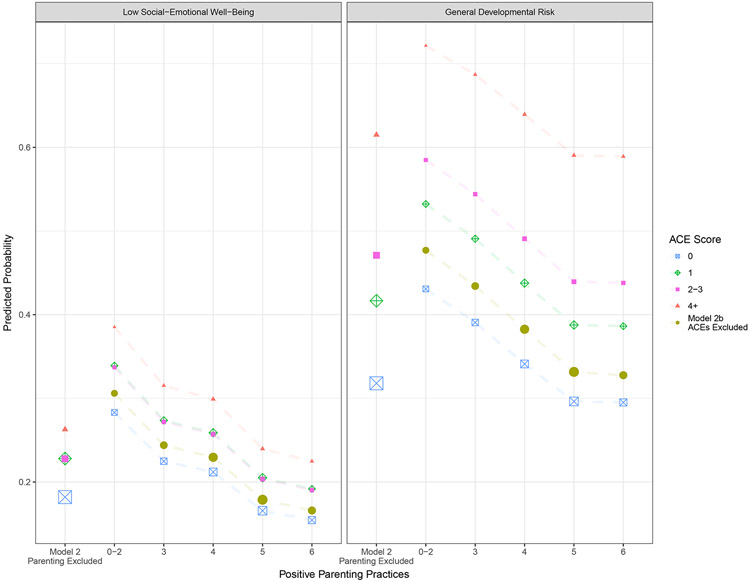
Given the goals of our analysis, it is worth comparing the ACEs effects of model 2 (ACEs and covariates) and model 3 (ACEs, PPPs, and covariates) to evaluate the impact of a parenting confounder. Likewise, comparing parenting main effects from an alternate version of model 2, where PPPs replace ACEs (see model 2b of Table 3), to those of model 3 would be prudent. Unfortunately, direct comparison of the adjusted odds ratios is not appropriate for this task, since this measure of association suffers from noncollapsibility.23,24 So, we provide, instead, a plot of predicted probabilities from these models (including 2b) in Figure 1. The ACE and PPP absolute risk differences did not change much in model 3 compared to models 2 and 2b, which suggests little confounding of either effect was evident in the data. It is worth stressing this empirical finding need not have been true hypothetically. Control for the parenting variables could have effectively eliminated the relationship between ACEs and our outcomes; or vice versa, control for ACEs could have eliminated the parenting main effects. As shown in Figure 1, both main effects remain intact in our model 3. Notably, when comparing 0-2 PPP and 6 PPP families who also reported zero ACEs, we observed a model-predicted 12.9% and 13.6% reduction in low social-emotional and developmental risks. This same comparison among families with 4+ ACEs revealed risk reductions of 16.1% and 13.2%, respectively. Flipping the scenario and comparing 0 ACE and 4+ ACE families with 6 reported PPPs, we observed risk reductions of 7.0% and 29.4% for these two outcomes. This same ACE effect among 0-2 PPP families resulted in 10.2% and 29.1% risk reductions. Contrasting these simple effects across outcomes, one notices the absolute risk reductions were greatest for the PPP factor in our social-emotional model, while the oppositie was true, extreme ACE differences produced greatest risk reduction, for our developmental risk outcome. In terms of population impacts, under the condition that all families provide all 6 PPPs, the estimated population attributable fractions (PAFs) for low wellbeing and developmental risks were 19.1% and 10.0%, which were equilavent to reductions of 5.1% and 4.0% in prevalence. This equates to an outcome reversal/benefit (i.e., moving from “at-risk” to “not at-risk”) for 1.2+ million children at risk for low socio-emotional wellbeing and more than 950,000+ children at risk for general developmental concerns nationwide under the age of 6. [See also Table 1 and 2 of supplemental material.] Likewise, under the condition that all families have zero ACEs, PAFs for low wellbeing and developmental risks were 7.8% and 11.5%, which were equilavent to reductions of 2.1% and 4.6% in prevalence. Among U.S. children under age 6, this equates to a social-emotional reversal/benefit for 500,000+ children and a general developmental reversal/benefit for 1.1+ million.
Figure 1.
Predicted Probability Comparisons Across Models
Dots are proportion to population size. Gold dots reflect (model 2b) predicted probabilities WITHOUT adjustment for ACEs. Disconnected dots reflect (model 2) predicted probabilities WITHOUT adjustment for positive parenting. Predictions produced with covariates fixed to modal (male, white not Hispanic, household educated beyond high school) or mean (2.53 years old) values.
Surprisingly, our full social emotional model predicted higher probability of risk for families reporting poor parenting practices (0-2 PPPs) and no adversities (ACE 0) than for families reporting all 6 PPPs and 4+ ACEs (28.3% vs 22.5%). Similarly, model 3 for general development predicted roughly equivalent risks for poor parenting families with zero ACEs and for 2-3 ACE families reporting all 6 PPPs (43.1% vs 43.8%). Ergo, in some instances, absence of positive parenting among the lowest ACE families could be viewed as roughly equivalent to the impact of 2 or more ACEs.
Discussion
This study found that accumulated adversities had already negatively affected wellbeing and development of young children. However, PPPs had protective effects even after controlling for ACEs. Over one third of children under age six had already experienced at least one of nine NSCH adversities, which might partly be explained by relatively high child poverty,25 divorce,26 and incarceration 27 rates in the U.S. Given the ACE prevalence and its estimated long-term economic burden,28 the increased attention and importance placed on how children are affected by adversities seems well justified.
The most important finding herein is that positive parenting practices (PPPs) can mitigate negative effects of adversities among young children. The recent Parenting Matters… NAS report 14 noted that “High-quality ‘serve and return’ parenting skills do not always develop spontaneously,”especially for among families living with adversities. While changes in parenting practices may be more challenging for those facing adversities, encouraging and facilitating adoption of positive parenting techniques remains the primary, front-line intervention for promoting healthy development among young children.10
Moreover, the absence of PPPs could be viewed, itself, as an adversity which at the extremes is equivalent to the addition of 2 or more ACE score units. This finding, coupled with the lack of evidence for effect modification (see supplemental materials), seems promising for prevention professionals. To promote PPPs, policies that strengthen and fund evidence-based parenting training (e.g., home visiting) and parent resource (e.g., Reach Out and Read) programs ought to remain at the forefront of early childhood prevention efforts. The population impacts of PPPs are particularly worth emphasizing since promotion of PPPs can be a simple, feasible, and universal intervention. If the studied relationships are (directly or indirectly) causal, adoption of all PPPs could reduce developmental risks for nearly 1 million children under age six nationwide. Thus, practitioners and policy makers would be wise to pay equitable attention to both ACEs and to the absence of positive parenting during early childhood. Promotion of PPPs, not only as a buffer for adversity, but as a generally effective intervention for lowering risks of social-emotional and developmental disabilities seems to be a worthy public health message that ought to be spread within all early childhood service settings (clinics, childcare and education centers, etc.).
3. Limitations
The current study has several limitations. First, we utilized a cross-sectional study that could not eliminate the possibility of reverse or reciprocal causation. Further longitudinal research is needed to examine the mechanism of how ACEs affect PPPs and young children’s outcomes. Second, for sake of interpretive clarity, we dichotomized items and constructed simple summed scores for key independent and dependent variables in our models, which could lose or distort variable relationships. We did perform additional analyses without these coarsened scoring approaches, and the results largely replicated our general findings. Last, the NSCH ACE items do differ from those included in the original ACE study.2 Because parents are reporting on their child’s ACEs, NSCH avoided including conventional items of child maltreatment. NSCH 2011/12 alternatively includes additional adversity items for life-course stressors.19 Still, the NSCH ACE scale is limited in scope. Finkelhor et al.29 proposed a revised inventory of ACEs including peer victimization, peer isolation/rejection, community violence, and low socioeconomic status. Recently, McLaughlin et al.30 proposed a conceptual framework of “deprivation” and “threat” to understand differential impact of childhood adversities. Most adversities in our study would fall under deprivation, e.g., poverty, limited/no exposure to one parent, etc., rather than under threats like physical abuse. Further research should evaluate these differential effects of deprivation and threats along with broader adversities. These same limitations exist for our parenting measure which only incorporated the 6 NSCH practices, and for interpretive simplicity, treated each as equally impactful. Similarly, reliance on frequency of parenting behaviors ignores the importance of engagement/interaction quality. While our findings cannot speak to value or need for parent training on the intracacies of “serve and return” skills, mastery of these interactive skills are likely to lead to higher quality parenting and even greater reductions in developmental risk. The small correlation and minimal cross-variable confounding observed for our ACE and parenting predictors might, at least partially, be an artifact of these construct measurement scope limitations. To be fair, these same limitations apply to most or all self-report measures of adversity, including the conventional ACE items, and to nearly all secondary uses of archived data.
Conclusion
Adverse childhood experiences have noteworthy negative effects on wellbeing and development in early childhood; however, positive parenting practices (PPPs) exhibited independent and in some situations (social-emotional wellbeing outcomes), larger protective effects. These data further support and champion sustaining and furthering interventions that promote PPPs at home for all children, but especially for those within families experiencing high levels of adversity.
Supplementary Material
Acknowledgement
Dr. Yamaoka is financially supported by the Nippon Foundation International Fellowship program. Dr. Bard’s support of this work was partly funded by the Maternal, Infant, and Early Childhood Home Visiting Grant Program by the Health Resources and Services Administration (HRSA; Grant Numbers: D89MC28275 and X10MC29496).
Footnotes
Conflict of Interest Statement: The authors have indicated they have no potential conflicts of interest to disclose.
Financial Disclosure Statement: Aside from the funding sources above, the authors have indicated no other financial relationships relevant to this article to disclose.
Reference
- 1.Brown DW, Anda RF, Tiemeier H, et al. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med. 2009;37(5):389–396. [DOI] [PubMed] [Google Scholar]
- 2.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. [DOI] [PubMed] [Google Scholar]
- 3.Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111(3):564–572. [DOI] [PubMed] [Google Scholar]
- 4.Björkenstam E, Hjern A, Vinnerljung B. Adverse childhood experiences and disability pension in early midlife: results from a Swedish National Cohort Study. Eur J Public Health. 2016. [DOI] [PubMed] [Google Scholar]
- 5.National Scientific Council on the Developing Child. Excessive Stress Disrupts the Architecture of the Developing Brain: Working Paper No. 3. Updated Edition. 2005/2014; http://www.developingchild.harvard.edu. Accessed 05/03, 2017.
- 6.Lynch BA, Agunwamba A, Wilson PM, et al. Adverse family experiences and obesity in children and adolescents in the United States. Prev Med. 2016;90:148–154. [DOI] [PubMed] [Google Scholar]
- 7.Mersky JP, Topitzes J, Reynolds AJ. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the U.S. Child Abuse Negl. 2013;37(11):917–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bright MA, Knapp C, Hinojosa MS, Alford S, Bonner B. The Comorbidity of Physical, Mental, and Developmental Conditions Associated with Childhood Adversity: A Population Based Study. Matern Child Health J. 2016;20(4):843–853. [DOI] [PubMed] [Google Scholar]
- 9.National Scientific Council on the Developing Child. Supportive Relationships and Active Skill-Building Strengthen the Foundations of Resilience: Working Paper 13. 2015; http://www.developingchild.harvard.edu. Accessed 05/03, 2017.
- 10.Garner AS, Shonkoff JP. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012;129(1):e224–231. [DOI] [PubMed] [Google Scholar]
- 11.CDC. Essentials for Childhood: Steps to create safe, stable, nurturing relationships and environments for all children. 2014; https://www.cdc.gov/violenceprevention/childmaltreatment/essentials.html. Accessed 08/01, 2017.
- 12.Browne HC. The Strengthening Families Approach and Protective Factors Framework: Branching out and reaching deeper. 2014. https://www.cssp.org/young-children-their-families/strengtheningfamilies/about. Accessed 08/01, 2017. [Google Scholar]
- 13.Traub F, Boynton-Jarrett R. Modifiable Resilience Factors to Childhood Adversity for Clinical Pediatric Practice. Pediatrics. 2017;139(5). [DOI] [PubMed] [Google Scholar]
- 14.National Academies of Sciences Engineering, and Medicine. Parenting Matters: Supporting Parents of Children Ages 0-8. 2016. [PubMed]
- 15.Greenland S, Drescher K. Maximum likelihood estimation of the attributable fraction from logistic models. Biometrics. 1993;49(3):865–872. [PubMed] [Google Scholar]
- 16.Afifi TO, Enns MW, Cox BJ, Asmundson GJ, Stein MB, Sareen J. Population attributable fractions of psychiatric disorders and suicide ideation and attempts associated with adverse childhood experiences. Am J Public Health. 2008;98(5):946–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roos LE, Mota N, Afifi TO, Katz LY, Distasio J, Sareen J. Relationship between adverse childhood experiences and homelessness and the impact of axis I and II disorders. Am J Public Health. 2013;103 Suppl 2:S275–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention., National Center for Health Statistics., State and Local Area Integrated Telephone Survey. 2011-2012 National Survey of Children’s Health Frequently Asked Questions. 2013; http://www.cdc.gov/nchs/slaits/nsch.htm. Accessed 12/10, 2017.
- 19.2011/12 National Survey of Children’s Health. Child and Adolescent Health Measurement Initiative (CAHMI), “2011-2012 NSCH: Child Health Indicator and Subgroups SAS Codebook, Version 1.0”. 2013; http://www.childhealthdata.org. Accessed 05/04, 2017.
- 20.Woolfenden S, Eapen V, Williams K, Hayen A, Spencer N, Kemp L. A systematic review of the prevalence of parental concerns measured by the Parents' Evaluation of Developmental Status (PEDS) indicating developmental risk. BMC Pediatr. 2014;14:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.StataCorp L. STATA SURVEY DATA REFERENCE MANUAL, RELEASE 14. 2015. Accessed 11/08, 2017
- 22.R Core Team. R: A language and environment for statistical computing. 2017; https://www.R-project.org/.
- 23.Greenland S, Robins JM, Pearl J. Confounding and Collapsibility in Causal Inference. Statistical Science. 1999;14(1):29–46. [Google Scholar]
- 24.Greenland S. Interpretation and choice of effect measures in epidemiologic analyses. Am J Epidemiol. 1987;125(5):761–768. [DOI] [PubMed] [Google Scholar]
- 25.Sachs JD. High US Child Poverty: Explanations and Solutions. Acad Pediatr. 2016;16(3 Suppl):S8–S12. [DOI] [PubMed] [Google Scholar]
- 26.OECD. OECD Family Database, SF3.1 Marriage and divorce rate. Updated: 25-08-16; http://www.oecd.org/els/family/database.htm. Accessed 10/10, 2017.
- 27.Weiss D, MacKenzie D. A Global Perspective on Incarceration: How an International Focus Can Help the United States Reconsider Its Incarceration Rates. Victims & Offenders. 2010;5(3):268–282. [Google Scholar]
- 28.Caspi A, Houts RM, Belsky DW, et al. Childhood forecasting of a small segment of the population with large economic burden. Nat Hum Behav. 2016;1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Finkelhor D, Shattuck A, Turner H, Hamby S. A revised inventory of Adverse Childhood Experiences. Child Abuse Negl. 2015;48:13–21. [DOI] [PubMed] [Google Scholar]
- 30.McLaughlin KA, Sheridan MA, Lambert HK. Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev. 2014;47:578–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.