Since 1986, the Japanese Association for Thoracic Surgery (JATS) has conducted annual thoracic surgery surveys throughout Japan to determine statistics on the number of procedures performed by surgical categories. Herein, we summarize the results of the association’s annual thoracic surgery surveys in 2021.
Adhering to the norm thus far, thoracic surgery had been classified into three categories, including cardiovascular, general thoracic, and esophageal surgeries, with patient data for each group being examined and analyzed. We honor and value all members’ continued professional support and contributions.
Incidence of hospital mortality was included in the survey to determine nationwide status, which has contributed to Japanese surgeons’ understanding of the present status of thoracic surgery in Japan while helping in surgical outcome improvements by enabling comparisons between their work and that of others. This approach has enabled the association to gain a better understanding of present problems and prospects, which is reflected in its activities and member education.
The 30-day mortality (also known as operative mortality) is defined as death within 30 days of surgery, regardless of the patient’s geographic location, including post-discharge from the hospital. Hospital mortality is defined as death within any time interval following surgery among patients yet to be discharged from the hospital.
Transfer to a nursing home or a rehabilitation unit is considered hospital discharge unless the patient subsequently dies of complications from surgery, while hospital-to-hospital transfer during esophageal surgery is not considered a form of discharge. In contrast, hospital-to-hospital transfer 30 days following cardiovascular and general thoracic surgeries are considered discharge given that National Clinical Database (NCD)-related data were used in these categories.
Severe Acute Respiratory Syndrpme Coronavirus-2 (SARS-CoV-2), the causative pathogen for the coronavirus disease 2019 (COVID-19), first emerged in Wuhan, China, in December 2019 and by March 2020, it was declared a pandemic [1]. The pandemic of SARS-CoV-2 resulted in a global healthcare and financial crisis. There was a significant estimated reduction in national case volume of cardiovascular, general thoracic, and esophageal surgeries in Japan during 2020 [2–4]. We have to continue the estimation of the nationwide effect of SARS-CoV-2 pandemic on thoracic surgery in Japan, with surgical volume, outcomes and patient data for each group.
Survey abstract
All data on cardiovascular, general thoracic, and esophageal surgeries were obtained from the NCD. In 2018, the data collection method for general thoracic and esophageal surgeries had been modified from self-reports using questionnaire sheets following each institution belonging to the JATS to an automatic package downloaded from the NCD in Japan.
The data collection related to cardiovascular surgery (initially self-reported using questionnaire sheets in each participating institution up to 2014) changed to downloading an automatic package from the Japanese Cardiovascular Surgery Database (JCVSD), which is a cardiovascular subsection of the NCD in 2015.
Final report: 2021
(A) Cardiovascular surgery
We are extremely pleased with the cooperation of our colleagues (members) in completing the cardiovascular surgery survey, which has undoubtedly improved the quality of this annual report. We are truly grateful for the significant efforts made by all participants within each participating institution in completing the JCVSD/NCD.
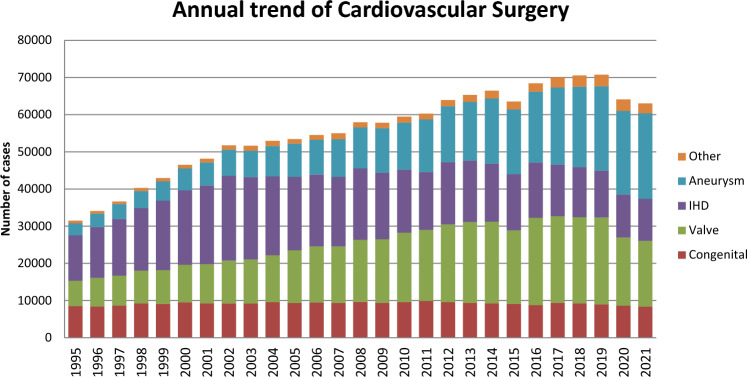
Figure 1 illustrates the development of cardiovascular surgery in Japan over the past 35 years. Aneurysm surgery includes only surgeries for thoracic and thoracoabdominal aortic aneurysms. Extra-anatomic bypass surgery for thoracic aneurysm and pacemaker implantation have been excluded from the survey since 2015. Assist device implantations were not included in the total number of surgical procedures but were included in the survey.
Fig. 1.
Annual trend of cardiovascular surgery
A total of 63,054 cardiovascular surgeries, including 59 heart transplants, had been performed in 2021, with a 1.6% decrease compared to that in 2020 (n = 64,075) [3]. Following on from 2020, a decline in the number of cases has been observed for the second consecutive year. Although the impact of the COVID-19 pandemic is suggested, verification from various perspectives is necessary.
Compared to data for 2020 [3] and 2011 [5], data for 2021 showed 2.9% (8349 vs. 8595) and 15.3% fewer surgeries for congenital heart disease, 3.8% (17,661 vs. 18,366) fewer and 7.8% fewer surgeries for valvular heart disease, 1.4% (11,364 vs. 11,524) and 27.1% fewer surgeries for ischemic heart procedures, and 2.0% (22,982 vs. 22,540) more and 62.7% more surgeries for thoracic aortic aneurysm, respectively. Data for individual categories are summarized in Tables 1, 2, 3, 4, 5, and 6.
Table 1.
Congenital (total; 8349)
(1) CPB ( +) (total; 6510)
| Neonate | Infant | 1 ~ 17 years | ≥ 18 years | Total | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | ||||||
| Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | |||||||||||
| PDA | 6 | 0 | 0 | 0 | 5 | 1 (20.0) | 0 | 1 (20.0) | 3 | 0 | 0 | 0 | 14 | 0 | 0 | 0 | 28 | 1 (3.6) | 0 | 1 (3.6) |
| Coarctation (simple) | 9 | 0 | 0 | 1 (11.1) | 14 | 0 | 0 | 0 | 9 | 0 | 0 | 0 | 12 | 0 | 0 | 0 | 44 | 0 | 0 | 1 (2.3) |
| + VSD | 39 | 0 | 0 | 0 | 46 | 0 | 0 | 0 | 10 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 96 | 0 | 0 | 0 |
| + DORV | 3 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 11 | 0 | 0 | 0 |
| + AVSD | 5 | 0 | 0 | 0 | 5 | 0 | 0 | 1 (20.0) | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 11 | 0 | 0 | 1 (9.1) |
| + TGA | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 |
| + SV | 2 | 0 | 0 | 0 | 9 | 1 (11.1) | 0 | 1 (11.1) | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 14 | 1 (7.1) | 0 | 1 (7.1) |
| + Others | 7 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 5 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 17 | 0 | 0 | 0 |
| Interrupt. of Ao (simple) | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| + VSD | 26 | 1 (3.8) | 0 | 2 (7.7) | 24 | 1 (4.2) | 0 | 2 (8.3) | 14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 64 | 2 (3.1) | 0 | 4 (6.3) |
| + DORV | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 |
| + Truncus | 2 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 | 0 |
| + TGA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| + Others | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 0 | 0 | 0 |
| Vascular ring | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| PS | 6 | 0 | 0 | 0 | 30 | 0 | 0 | 0 | 62 | 0 | 0 | 0 | 17 | 0 | 0 | 0 | 115 | 0 | 0 | 0 |
| PA・IVS or critical PS | 5 | 0 | 0 | 0 | 37 | 0 | 0 | 0 | 57 | 0 | 0 | 0 | 9 | 0 | 0 | 0 | 108 | 0 | 0 | 0 |
| TAPVR | 104 | 4 (3.8) | 0 | 9 (8.7) | 43 | 1 (2.3) | 0 | 2 (4.7) | 11 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 158 | 5 (3.2) | 0 | 11 (7.0) |
| PAPVR ± ASD | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 45 | 0 | 0 | 0 | 12 | 0 | 0 | 0 | 60 | 0 | 0 | 0 |
| ASD | 0 | 0 | 0 | 0 | 48 | 1 (2.1) | 0 | 1 (2.1) | 466 | 0 | 0 | 1 (0.2) | 788 | 7 (0.9) | 0 | 7 (0.9) | 1302 | 8 (0.6) | 0 | 9 (0.7) |
| Cor triatriatum | 3 | 0 | 0 | 0 | 13 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 24 | 0 | 0 | 0 |
| AVSD (partial) | 0 | 0 | 0 | 0 | 7 | 0 | 0 | 0 | 35 | 0 | 0 | 0 | 13 | 0 | 0 | 0 | 55 | 0 | 0 | 0 |
| AVSD (complete) | 1 | 0 | 0 | 0 | 87 | 1 (1.1) | 0 | 2 (2.3) | 104 | 1 (1.0) | 0 | 2 (1.9) | 4 | 0 | 0 | 0 | 196 | 2 (1.0) | 0 | 4 (2.0) |
| + TOF or DORV | 0 | 0 | 0 | 0 | 5 | 0 | 0 | 0 | 10 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 17 | 0 | 0 | 0 |
| + Others | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| VSD (subarterial) | 1 | 0 | 0 | 0 | 77 | 0 | 0 | 0 | 138 | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 224 | 0 | 0 | 0 |
| VSD (perimemb./muscular) | 6 | 0 | 0 | 0 | 645 | 0 | 0 | 0 | 331 | 0 | 0 | 1 (0.3) | 17 | 0 | 0 | 0 | 999 | 0 | 0 | 1 (0.1) |
| VSD (type unknown) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 112 | 2 (1.8) | 0 | 2 (1.8) | 115 | 2 (1.7) | 0 | 2 (1.7) |
| VSD + PS | 1 | 0 | 0 | 0 | 31 | 0 | 0 | 0 | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 42 | 0 | 0 | 0 |
| DCRV ± VSD | 0 | 0 | 0 | 0 | 9 | 0 | 0 | 0 | 10 | 0 | 0 | 0 | 12 | 0 | 0 | 0 | 31 | 0 | 0 | 0 |
| Aneurysm of sinus of Valsalva | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| TOF | 14 | 0 | 0 | 0 | 157 | 0 | 0 | 1 (0.6) | 157 | 0 | 0 | 0 | 57 | 0 | 0 | 1 (1.8) | 385 | 0 | 0 | 2 (0.5) |
| PA + VSD | 7 | 0 | 0 | 1 (14.3) | 85 | 0 | 0 | 0 | 107 | 2 (1.9) | 0 | 3 (2.8) | 10 | 0 | 0 | 0 | 209 | 2 (1.0) | 0 | 4 (1.9) |
| DORV | 13 | 0 | 0 | 2 (15.4) | 117 | 2 (1.7) | 0 | 7 (6.0) | 136 | 1 (0.7) | 0 | 1 (0.7) | 4 | 0 | 0 | 0 | 270 | 3 (1.1) | 0 | 10 (3.7) |
| TGA (simple) | 83 | 1 (1.2) | 0 | 4 (4.8) | 8 | 0 | 0 | 1 (12.5) | 3 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 100 | 1 (1.0) | 0 | 5 (5.0) |
| + VSD | 34 | 1 (2.9) | 0 | 1 (2.9) | 10 | 0 | 0 | 0 | 13 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 58 | 1 (1.7) | 0 | 1 (1.7) |
| VSD + PS | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 |
| Corrected TGA | 1 | 0 | 0 | 0 | 7 | 0 | 0 | 0 | 33 | 0 | 0 | 0 | 10 | 0 | 0 | 0 | 51 | 0 | 0 | 0 |
| Truncus arteriosus | 5 | 0 | 0 | 1 (20.0) | 16 | 0 | 0 | 0 | 27 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 50 | 0 | 0 | 1 (2.0) |
| SV | 16 | 2 (12.5) | 0 | 2 (12.5) | 141 | 2 (1.4) | 0 | 6 (4.3) | 188 | 0 | 0 | 4 (2.1) | 19 | 0 | 0 | 1 (5.3) | 364 | 4 (1.1) | 0 | 13 (3.6) |
| TA | 4 | 0 | 0 | 0 | 33 | 0 | 0 | 0 | 48 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 88 | 0 | 0 | 0 |
| HLHS | 30 | 3 (10.0) | 0 | 7 (23.3) | 101 | 5 (5.0) | 0 | 9 (8.9) | 80 | 0 | 0 | 1 (1.3) | 1 | 0 | 0 | 0 | 212 | 8 (3.8) | 0 | 17 (8.0) |
| Aortic valve lesion | 5 | 0 | 0 | 1 (20.0) | 17 | 2 (11.8) | 0 | 2 (11.8) | 110 | 1 (0.9) | 0 | 1 (0.9) | 43 | 0 | 0 | 0 | 175 | 3 (1.7) | 0 | 4 (2.3) |
| Mitral valve lesion | 0 | 0 | 0 | 0 | 28 | 0 | 0 | 1 (3.6) | 76 | 0 | 0 | 0 | 21 | 0 | 0 | 2 (9.5) | 125 | 0 | 0 | 3 (2.4) |
| Ebstein | 12 | 2 (16.7) | 0 | 2 (16.7) | 10 | 1 (10.0) | 0 | 1 (10.0) | 21 | 0 | 0 | 0 | 15 | 0 | 0 | 0 | 58 | 3 (5.2) | 0 | 3 (5.2) |
| Coronary disease | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 21 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 26 | 0 | 0 | 0 |
| Others | 10 | 1 (10.0) | 0 | 1 (10.0) | 27 | 0 | 0 | 3 (11.1) | 53 | 1 (1.9) | 0 | 1 (1.9) | 237 | 1 (0.4) | 0 | 1 (0.4) | 327 | 3 (0.9) | 0 | 6 (1.8) |
| Conduit failure | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 20 | 0 | 0 | 0 | 9 | 0 | 0 | 0 | 30 | 0 | 0 | 0 |
| Redo (excluding conduit failure) | 1 | 0 | 0 | 0 | 50 | 1 (2.0) | 0 | 2 (4.0) | 106 | 2 (1.9) | 0 | 2 (1.9) | 69 | 0 | 0 | 0 | 226 | 3 (1.3) | 0 | 4 (1.8) |
| Total | 465 | 15 (3.2) | 0 | 34 (7.3) | 1967 | 19 (1.0) | 0 | 43 (2.2) | 2544 | 8 (0.3) | 0 | 17 (0.7) | 1534 | 10 (0.7) | 0 | 14 (0.9) | 6510 | 52 (0.8) | 0 | 108 (1.7) |
| (), % mortality | ||||||||||||||||||||
| CPB cardiopulmonary bypass; PDA patent ductus arteriosus; VSD ventricular septal defect; DORV double outlet right ventricle; AVSD atrioventricular septal defect; TGA transposition of great arteries; SV single ventricle; Interrupt. of Ao. interruption of aorta; PS pulmonary stenosis; PA-IVS pulmonary atresia with intact ventricular septum; TAPVR total anomalous pulmonary venous return; PAPVR partial anomalous pulmonary venous return; ASD atrial septal defect; TOF tetralogy of Fallot; DCRV double-chambered right ventricle; TA tricuspid atresia; HLHS hypoplastic left heart syndrome; RV-PA right ventricle-pulmonary artery | ||||||||||||||||||||
| (2) CPB (−) (total; 1839) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neonate | Infant | 1–17 years | ≥ 18 years | Total | ||||||||||||||||
| Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | ||||||
| Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | |||||||||||
| PDA | 230 | 7 (3.0) | 0 | 11 (4.8) | 130 | 1 (0.8) | 0 | 6 (4.6) | 6 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 370 | 8 (2.2) | 0 | 17 (4.6) |
| Coarctation (simple) | 6 | 0 | 0 | 1 (16.7) | 7 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 5 | 0 | 0 | 0 | 19 | 0 | 0 | 1 (5.3) |
| + VSD | 40 | 2 (5.0) | 0 | 2 (5.0) | 12 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 52 | 2 (3.8) | 0 | 2 (3.8) |
| + DORV | 4 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 0 | 0 | 0 |
| + AVSD | 8 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | 0 | 0 | 0 |
| + TGA | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| + SV | 6 | 0 | 0 | 1 (16.7) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 0 | 0 | 1 (16.7) |
| + Others | 3 | 0 | 0 | 1 (33.3) | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 0 | 0 | 1 (11.1) |
| Interrupt. of Ao (simple) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| + VSD | 21 | 0 | 0 | 2 (9.5) | 5 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 27 | 0 | 0 | 2 (7.4) |
| + DORV | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| + Truncus | 6 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 0 | 0 | 0 |
| + TGA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| + Others | 2 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 0 | 0 | 0 |
| Vascular ring | 0 | 0 | 0 | 0 | 20 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 26 | 0 | 0 | 0 |
| PS | 1 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 | 0 |
| PA・IVS or Critical PS | 14 | 0 | 0 | 1 (7.1) | 13 | 1 (7.7) | 0 | 1 (7.7) | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 29 | 1 (3.4) | 0 | 2 (6.9) |
| TAPVR | 8 | 1 (12.5) | 0 | 2 (25.0) | 5 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 14 | 1 (7.1) | 0 | 2 (14.3) |
| PAPVR ± ASD | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| ASD | 1 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 | 0 |
| Cor triatriatum | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| AVSD (partial) | 1 | 0 | 0 | 0 | 1 | 0 | 1 (100.0) | 0 | 6 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 9 | 0 | 1(11.1) | 0 |
| AVSD (complete) | 37 | 0 | 0 | 0 | 70 | 1 (1.4) | 0 | 3 (4.3) | 8 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 117 | 1 (0.9) | 0 | 3 (2.6) |
| + TOF or DORV | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 |
| + Others | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| VSD (subarterial) | 4 | 0 | 0 | 0 | 9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 13 | 0 | 0 | 0 |
| VSD (perimemb./muscular) | 58 | 1 (1.7) | 0 | 4 (6.9) | 143 | 3 (2.1) | 0 | 4 (2.8) | 4 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 207 | 4 (1.9) | 0 | 8 (3.9) |
| VSD (Type Unknown) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| VSD + PS | 1 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 |
| DCRV ± VSD | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Aneurysm of sinus of Valsalva | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| TOF | 9 | 0 | 0 | 0 | 50 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 63 | 0 | 0 | 0 |
| PA + VSD | 22 | 0 | 0 | 1 (4.5) | 35 | 1 (2.9) | 0 | 2 (5.7) | 7 | 1 (14.3) | 0 | 1 (14.3) | 0 | 0 | 0 | 0 | 64 | 2 (3.1) | 0 | 4 (6.3) |
| DORV | 47 | 0 | 0 | 3 (6.4) | 58 | 0 | 0 | 2 (3.4) | 6 | 0 | 0 | 0 | 1 | 1(100.0) | 0 | 1(100.0) | 112 | 1 (0.9) | 0 | 6 (5.4) |
| TGA (simple) | 10 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 16 | 0 | 0 | 0 |
| + VSD | 8 | 1 (12.5) | 0 | 1 (12.5) | 2 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 11 | 1 (9.1) | 0 | 1 (9.1) |
| VSD + PS | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Corrected TGA | 5 | 0 0 | 0 | 0 | 7 | 0 | 0 | 0 | 10 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 28 | 0 | 0 | 0 |
| Truncus arteriosus | 11 | 0 | 1 (9.1) | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 12 | 0 | 0 | 1 (8.3) | |
| SV | 40 | 0 | 0 | 3 (7.5) | 58 | 3 (5.2) | 0 | 6 (10.3) | 8 | 0 | 0 | 0 | 3 | 0 | 0 | 2(66.7) | 109 | 3 (2.8) | 0 | 11 (10.1) |
| TA | 22 | 0 | 0 | 0 | 12 | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 45 | 0 | 0 | 0 |
| HLHS | 66 | 1 (1.5) | 0 | 8 (12.1) | 27 | 1 (3.7) | 1 (3.7) | 1 (3.7) | 11 | 0 | 0 | 1 (9.1) | 1 | 0 | 0 | 0 | 105 | 2 (1.9) | 1(1.0) | 10 (9.5) |
| Aortic valve lesion | 7 | 0 | 0 | 0 | 9 | 1 (11.1) | 0 | 1 (11.1) | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 20 | 1 (5.0) | 0 | 1 (5.0) |
| Mitral valve lesion | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 0 | 0 | 0 |
| Ebstein | 10 | 1 (10.0) | 0 | 1 (10.0) | 3 | 1 (33.3) | 0 | 1 (33.3) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 13 | 2 (15.4) | 0 | 2 (15.4) |
| Coronary disease | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Others | 12 | 1 (8.3) | 0 | 2 (16.7) | 8 | 0 | 0 | 1 (12.5) | 16 | 3 (18.8) | 0 | 5 (31.3) | 1 | 0 | 0 | 0 | 37 | 4 (10.8) | 0 | 8 (21.6) |
| Conduit failure | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Redo (excluding conduit failure) | 14 | 0 | 0 | 0 | 69 | 2 (2.9) | 0 | 3 (4.3) | 120 | 5 (4.2) | 0 | 8 (6.7) | 39 | 1(2.6) | 0 | 2(5.1) | 242 | 8 (3.3) | 0 | 13 (5.4) |
| Total | 739 | 15 (2.0) | 0 | 45 (6.1) | 787 | 15 (1.9) | 2 (0.3) | 31 (3.9) | 244 | 9 (3.7) | 0 | 15 (6.1) | 69 | 2(2.9) | 0 | 5(7.2) | 1839 | 41 (2.2) | 2(0.11) | 96 (5.2) |
| (), % mortality | ||||||||||||||||||||
| CPB cardiopulmonary bypass; PDA patent ductus arteriosus; VSD ventricular septal defect; DORV double outlet right ventricle; AVSD atrioventricular septal defect; TGA transposition of the great arteries; SV single ventricle; Interrupt. of Ao. interruption of aorta; PS pulmonary stenosis; PA-IVS pulmonary atresia with intact ventricular septum; TAPVR total anomalous pulmonary venous return; PAPVR partial anomalous pulmonary venous return; ASD atrial septal defect; TOF tetralogy of Fallot; DCRV double-chambered right ventricle; TA tricuspid atresia; HLHS hypoplastic left heart syndrome; RV-PA right ventricle-pulmonary artery | ||||||||||||||||||||
| (3) Main procedure | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neonate | Infant | 1- 17 years | ≥ 18 years | Total | |||||||||||||||||
| Cases | 30-day mortality | Cases | 30-day mortality | Cases | 30-day mortality | Cases | 30-day mortality | Cases | 30-day mortality | ||||||||||||
| After discharge | Hospital mortality | Hospital | After discharge | Hospital mortality | Hospital | After discharge | Hospital mortality | Hospital | After discharge | Hospital mortality | Hospital | After discharge | Hospital mortality | ||||||||
| 1 | SP Shunt | 100 | 0 | 0 | 3 (3.0) | 267 | 0 | 0 | 6 (2.2) | 37 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 405 | 0 | 0 | 9 (2.2) |
| 2 | PAB | 236 | 1 (0.4) | 0 | 9 (3.8) | 314 | 4 (1.3) | 1 (0.3) | 8 (2.5) | 9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 559 | 5 (0.9) | 1 (0.2) | 17 (3.0) |
| 3 | Bidirectional Glenn or hemi-Fontan ± α | 0 | 0 | 0 | 0 | 217 | 2 (0.9) | 0 | 6 (2.8) | 73 | 0 | 0 | 1 (1.4) | 1 | 0 | 0 | 0 | 291 | 2 (0.7) | 0 | 7 (2.4) |
| 4 | Damus-Kaye-Stansel operation | 0 | 0 | 0 | 0 | 17 | 0 | 0 | 1 (5.9) | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 1 (4.3) |
| 5 | PA reconstruction/repair (including redo) | 13 | 1 (7.7) | 0 | 1 (7.7) | 179 | 2 (1.1) | 0 | 4 (2.2) | 194 | 2 (1.0) | 0 | 4 (2.1) | 23 | 1 (4.3) | 0 | 1 (4.3) | 409 | 6 (1.5) | 0 | 10 (2.4) |
| 6 | RVOT reconstruction/repair | 6 | 1 (16.7) | 0 | 1 (16.7) | 224 | 1 (0.4) | 0 | 3 (1.3) | 267 | 2 (0.7) | 0 | 3 (1.1) | 42 | 0 | 0 | 0 | 539 | 4 (0.7) | 0 | 7 (1.3) |
| 7 | Rastelli procedure | 2 | 0 | 0 | 0 | 43 | 0 | 0 | 0 | 97 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 144 | 0 | 0 | 0 |
| 8 | Arterial switch procedure | 122 | 3 (2.5) | 1 (0.8) | 7 (5.7) | 17 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 141 | 3 (2.1) | 1 (0.7) | 7 (5.0) |
| 9 | Atrial switch procedure | 0 | 0 | 0 | 0 | 4 | 1 (25.0) | 0 | 1 (25.0) | 4 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 10 | 1 (10.0) | 0 | 1 (10.0) |
| 10 | Double switch procedure | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 | 0 |
| 11 | Repair of anomalous origin of CA | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 0 | 0 | 0 |
| 12 | Closure of coronary AV fistula | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| 13 | Fontan / TCPC | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 356 | 0 | 0 | 2 (0.6) | 28 | 0 | 0 | 1 (3.6) | 385 | 0 | 0 | 3 (0.8) |
| 14 | Norwood procedure | 28 | 2 (7.1) | 0 | 5 (17.9) | 76 | 4 (5.3) | 0 | 7 (9.2) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 104 | 6 (5.8) | 0 | 12 (11.5) |
| 15 | Ventricular septation | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 16 | Left side AV valve repair (including Redo) | 0 | 0 | 0 | 0 | 43 | 0 | 0 | 1 (2.3) | 84 | 0 | 0 | 0 | 28 | 0 | 0 | 1 (3.6) | 155 | 0 | 0 | 2 (1.3) |
| 17 | Left side AV valve replace (including Redo) | 0 | 0 | 0 | 0 | 11 | 0 | 0 | 0 | 36 | 0 | 0 | 0 | 20 | 0 | 0 | 1 (5.0) | 67 | 0 | 0 | 1 (1.5) |
| 18 | Right side AV valve repair (including Redo) | 18 | 2 (11.1) | 0 | 2 (11.1) | 71 | 1 (1.4) | 0 | 4 (5.6) | 85 | 0 | 0 | 0 | 64 | 0 | 0 | 0 | 238 | 3 (1.3) | 0 | 6 (2.5) |
| 19 | Right side AV valve replace (including Redo) | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 24 | 0 | 0 | 0 | 33 | 0 | 0 | 0 |
| 20 | Common AV valve repair (including Redo) | 1 | 0 | 0 | 0 | 11 | 0 | 0 | 2 (18.2) | 8 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 21 | 0 | 0 | 2 (9.5) |
| 21 | Common AV valve replace (including Redo) | 0 | 0 | 0 | 0 | 2 | 1 (50.0) | 0 | 1 (50.0) | 14 | 1 (7.1) | 0 | 2 (14.3) | 8 | 0 | 0 | 0 | 24 | 2 (8.3) | 0 | 3 (12.5) |
| 22 | Repair of supra-aortic stenosis | 0 | 0 | 0 | 0 | 9 | 0 | 0 | 1 (11.1) | 23 | 0 | 0 | 1 (4.3) | 0 | 0 | 0 | 0 | 32 | 0 | 0 | 2 (6.3) |
| 23 | Repair of subaortic stenosis (including Redo) | 0 | 0 | 0 | 0 | 7 | 0 | 0 | 0 | 41 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 51 | 0 | 0 | 0 |
| 24 | Aortic valve plasty ± VSD Closure | 2 | 0 | 0 | 0 | 5 | 0 | 0 | 0 | 36 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 49 | 0 | 0 | 0 |
| 25 | Aortic valve replacement | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 28 | 0 | 0 | 0 | 36 | 0 | 0 | 0 | 66 | 0 | 0 | 0 |
| 26 | AVR with annular enlargement | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 14 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 21 | 0 | 0 | 0 |
| 27 | Aortic root Replace (except Ross) | 0 | 0 | 0 | 0 | 1 | 1 (100.0) | 0 | 1 (100.0) | 8 | 1 (12.5) | 0 | 1 (12.5) | 17 | 0 | 0 | 0 | 26 | 2 (7.7) | 0 | 2 (7.7) |
| 28 | Ross procedure | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 19 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | ||||
| 29 | Bilateral pulmonary artery banding | 180 | 9 (5.0) | 0 | 25 (13.9) | 23 | 1 (4.3) | 1 (4.3) | 2 (8.7) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 203 | 10 (4.9) | 1 (0.5) | 27 (13.3) |
| Total | 708 | 19 (2.7) | 1 (0.1) | 53 (7.5) | 1551 | 18 (1.2) | 2 (0.1) | 48 (3.1) | 1462 | 6 (0.4) | 0 | 14 (1.0) | 312 | 1 (0.3) | 0 | 4 (1.3) | 4033 | 44 (1.1) | 3 (0.07) | 119 (3.0) | |
| (), % mortality | |||||||||||||||||||||
| SP systemic-pulmonary; PAB pulmonary artery banding; PA pulmonary artery; RVOT right ventricular outflow tract; CA coronary artery; AV fistula arteriovenous fistula; TCPC total cavopulmonary connection; AV valve atrioventricular valve; VSD ventricular septal defect; AVR aortic valve replacement | |||||||||||||||||||||
Table 2.
Acquired (total, (1) + (2) + (4) + (5) + (6) + (7) + isolated operations for arrhythmia in (3); 31,479
| (1) Valvelar heart disease (total; 17,661) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Valve | Cases | Operation | 30-Day mortality | Hospital mortality | Redo | ||||||||||||
| Mechanical | Bioprosthesis | Repair | Unknown | With CABG | Hospital | After discharge | Cases | 30-Day mortality | Hospital mortality | ||||||||
| Replace | Repair | Replace | Repair | Replace | Repair | Hospital | After discharge | ||||||||||
| Isolated | A | 8206 | 879 | 7142 | 113 | 72 | 2020 | 118 (1.5) | 0 | 4 (0.05) | 1 (0.9) | 202 (2.5) | 2 (1.8) | 625 | 23 (3.7) | 0 | 33 (5.3) |
| M | 4415 | 384 | 847 | 3155 | 29 | 557 | 63 (5.1) | 21 (0.7) | 0 | 2 (0.06) | 97 (7.9) | 39 (1.2) | 527 | 18 (3.3) | 1 (0.2) | 34 (6.5) | |
| T | 221 | 7 | 44 | 167 | 3 | 37 | 0 | 7 (4.2) | 0 | 0 | 3 (5.9) | 11 (6.6) | 57 | 1 (1.8) | 0 | 3 (5.3) | |
| P | 20 | 0 | 17 | 0 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 16 | 0 | 0 | 0 | |
| A + M | 971 | 152 | 42 (4.3) | 1 (0.1) | 74 (7.6) | 143 | 11 (7.7) | 0 | 17 (11.9) | ||||||||
| A | 171 | 777 | 22 | 1 | |||||||||||||
| M | 134 | 308 | 520 | 9 | |||||||||||||
| A + T | 366 | 50 | 6 (1.6) | 0 | 16 (4.4) | 55 | 2 (3.6) | 0 | 4 (7.3) | ||||||||
| A | 38 | 323 | 5 | 0 | |||||||||||||
| T | 0 | 0 | 358 | 8 | |||||||||||||
| M + T | 2663 | 274 | 44 (1.7) | 1 (0.04) | 81 (3.0) | 317 | 7 (2.2) | 0 | 13 (4.1) | ||||||||
| M | 255 | 750 | 1631 | 27 | |||||||||||||
| T | 6 | 17 | 2622 | 18 | |||||||||||||
| A + M + T | 738 | 89 | 29 (3.9) | 0 | 49 (6.6) | 99 | 5 (5.1) | 0 | 6 (6.1) | ||||||||
| A | 100 | 624 | 12 | 2 | |||||||||||||
| M | 96 | 278 | 356 | 8 | |||||||||||||
| T | 3 | 6 | 728 | 1 | |||||||||||||
| others | 61 | 3 | 1 (1.6) | 0 | 3 (4.9) | 23 | 1 (4.3) | 0 | 1 (4.3) | ||||||||
| Total | 17,661 | 3183 | 303 (1.7) | 6 (0.03) | 525 (3.0) | 1862 | 68 (3.7) | 1 (0.05) | 111 (6.0) | ||||||||
| Cases | 30-day mortality | |
|---|---|---|
| TAVR | 12,202 | 140 (1.1) |
| (2) Ischemic heart disease (total, (A) + (B); 11,364) | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (A) Isolated CABG (total; (a) + (b); 10,184) | |||||||||||||||||||||
| (a-1) On-pump arrest CABG (total; 2374) | |||||||||||||||||||||
| Primary, elective | Primary, emergent | Redo, elective | redo, emergent | Artery only | Artery + SVG | SVG only | others | Unclear | |||||||||||||
| Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | ||||||||||
| Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | ||||||||||||||
| 1VD | 46 | 0 (0.0) | 0 | 0 (0.0) | 11 | 3 (27.3) | 0 | 3 (27.3) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 16 | 24 | 15 | 2 | 0 |
| 2VD | 296 | 1 (0.3) | 0 | 4 (1.4) | 27 | 3 (11.1) | 0 | 3 (11.1) | 0 | 0 | 0 | 0 | 1 | 0 (0.0) | 0 | 0 (0.0) | 38 | 263 | 22 | 1 | 0 |
| 3VD | 877 | 12 (1.4) | 0 | 17 (1.9) | 111 | 8 (7.2) | 0 | 10 (9.0) | 3 | 0 (0.0) | 0 | 0 (0.0) | 0 | 0 | 0 | 0 | 45 | 916 | 22 | 8 | 0 |
| LMT | 796 | 8 (1.0) | 0 | 11 (1.4) | 168 | 6 (3.6) | 0 | 13 (7.7) | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 69 | 851 | 43 | 6 | 1 |
| No info | 21 | 1 | 0 | 1 (4.8) | 8 | 1 (12.5) | 0 | 4 (50.0) | 1 | 0 (0.0) | 0 | 1 (100.0) | 2 | 1 (50.0) | 0 | 1 (50.0) | 3 | 15 | 11 | 1 | 2 |
| Total | 2036 | 22 (1.1) | 0 | 33 (1.6) | 325 | 21 (6.5) | 0 | 33 (10.2) | 10 | 0 (0.0) | 0 | 1 (10.0) | 3 | 1 (33.3) | 0 | 1 (33.3) | 171 | 2069 | 113 | 18 | 3 |
| Kawasaki | 4 | 1 (25.0) | 0 | 0 (0.0) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 |
| on dialysis | 250 | 10 (4.0) | 0 | 14 (5.6) | 36 | 4 | 0 | 6 (16.7) | 3 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 20 | 252 | 16 | 1 | 0 |
| (), % mortality | |||||||||||||||||||||
| CABG coronary artery bypass grafting; 1VD one-vessel disease; 2VD two-vessel disease; 3VD three-vessel disease; LMT left main trunk; SVG saphenous vein graft | |||||||||||||||||||||
| LMT includes LMT alone or LMT with other branch diseases | |||||||||||||||||||||
| (a-2) On-pump beating CABG (total; 2003) | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary, elective | Primary, emergent | Redo, elective | Redo, emergent | Artery only | Artery + SVG | SVG only | Others | Unclear | |||||||||||||
| Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | ||||||||||
| Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | ||||||||||||||
| 1VD | 38 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 11 | 1 (9.1) | 0 | 2 (18.2) | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 23 | 17 | 10 | 0 | 0 |
| 2VD | 206 | 1 (0.5) | 2 (1.0) | 3 (1.5) | 38 | 1 (2.6) | 0 | 3 (7.9) | 5 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 52 | 174 | 22 | 2 | 0 |
| 3VD | 662 | 11 (1.7) | 0 (0.0) | 18 (2.7) | 110 | 13 (11.8) | 0 | 19 (17.3) | 4 | 0 | 0 | 0 (0.0) | 3 | 1 (33.3) | 0 | 1 (33.3) | 81 | 668 | 28 | 2 | 0 |
| LMT | 643 | 17 (2.6) | 1 (0.2) | 27 (4.2) | 228 | 19 (8.3) | 0 | 26 (11.4) | 11 | 1 (9.1) | 0 | 2 (18.2) | 3 | 0 | 0 | 1 (33.3) | 116 | 731 | 32 | 5 | 1 |
| no info | 27 | 0 (0.0) | 0 (0.0) | 1 (3.7) | 9 | 1 (11.1) | 0 | 1 (11.1) | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 1 (33.3) | 14 | 18 | 7 | 0 | 0 |
| Total | 1576 | 29 (1.8) | 3 (0.2) | 49 (3.1) | 396 | 35 (8.8) | 0 (0.0) | 51 (12.9) | 20 | 1 (5.0) | 0 | 2 (10.0) | 11 | 1 (9.1) | 0 | 3 (27.3) | 286 | 1608 | 99 | 9 | 1 |
| Kawasaki | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 2 | 1 | 0 | 0 |
| on dialysis | 255 | 11 (4.3) | 1 | 21 (8.2) | 59 | 9 (15.3) | 0 (0.0) | 11 (18.6) | 6 | 1 (16.7) | 0 | 2 (33.3) | 1 | 1 (100.0) | 0 | 1 (100.0) | 23 | 278 | 19 | 1 | 0 |
| (), % mortality | |||||||||||||||||||||
| CABG, coronary artery bypass grafting; 1VD, one-vessel disease; 2VD two-vessel disease; 3VD, three-vessel disease; LMT, left main trunk; SVG, saphenous vein graft | |||||||||||||||||||||
| LMT includes LMT alone or LMT with other branch diseases | |||||||||||||||||||||
| (b) Off-pump CABG (total; 5807) | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Including cases of planned off-pump CABG in which, during surgery, the change is made to an on-pump CABG or on-pump beating-heart procedure) | |||||||||||||||||||||
| Primary, elective | Primary, emergent | Redo, elective | Redo, emergent | Artery only | Artery + SVG | SVG only | Others | Unclear | |||||||||||||
| Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | ||||||||||
| Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | ||||||||||||||
| 1VD | 307 | 0 (0.0) | 0 | 5 (1.6) | 36 | 3 (8.3) | 0 | 6 (16.7) | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 244 | 72 | 32 | 0 | 2 |
| 2VD | 786 | 6 (0.8) | 0 | 9 (1.1) | 63 | 1 (1.6) | 0 | 4 (6.3) | 8 | 0 | 0 | 1 (12.5) | 0 | 0 | 0 | 0 | 299 | 533 | 20 | 4 | 1 |
| 3VD | 2093 | 21 (1.0) | 1 (0.0) | 35 (1.7) | 186 | 5 (2.7) | 0 | 11 (5.9) | 14 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 462 | 1780 | 36 | 15 | 1 |
| LMT | 1873 | 14 (0.7) | 1 (0.1) | 26 (1.4) | 331 | 10 (3.0) | 1 (0.3) | 18 (5.4) | 13 | 0 | 0 | 1 (7.7) | 2 | 0 | 0 | 0 | 603 | 1562 | 44 | 10 | 0 |
| no info | 67 | 1 (1.5) | 0 (0.0) | 1 (1.5) | 15 | 1 | 0 | 1 (6.7) | 4 | 0 | 0 | 0 | 1 | 1 (100.0) | 0 | 1 (100.0) | 34 | 45 | 7 | 1 | 0 |
| Total | 5126 | 42 (0.8) | 2 (0.0) | 76 (1.5) | 631 | 20 (3.2) | 1 (0.2) | 40 (6.3) | 46 | 0 | 0 | 2 (4.3) | 4 | 1 (25.0) | 0 | 1 (25.0) | 1642 | 3992 | 139 | 30 | 4 |
| Kawasaki | 15 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 9 | 0 | 0 | 1 |
| On dialysis | 566 | 12 (2.1) | 1 (0.2) | 26 (4.6) | 55 | 6 (10.9) | 0 | 10 (18.2) | 13 | 0 | 0 | 2 (15.4) | 1 | 0 | 0 | 0 | 154 | 458 | 18 | 5 | 0 |
| (), % mortality | |||||||||||||||||||||
| CABG coronary artery bypass grafting; 1VD one-vessel disease; 2VD two-vessel disease; 3VD three-vessel disease; LMT left main trunk; SVG saphenous vein graft | |||||||||||||||||||||
| LMT includes LMT alone or LMT with other branch diseases | |||||||||||||||||||||
| (c) Cases of conversion, during surgery, from off-pump CABG to on-pump CABG or on- pump beating-heart CABG (these cases are also included in category (b)) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary, elective | Primary, emergent | Redo, elective | Redo, emergent | |||||||||||||
| Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | Cases | 30 day mortality | Hospital mortality | |||||
| Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | |||||||||
| Converted to arrest | 24 | 2 (8.3) | 0 | 2 (8.3) | 8 | 0 (0.0) | 0 | 1 (12.5) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Converted to beating | 107 | 5 (4.7) | 0 | 6 (5.6) | 17 | 3 (17.6) | 0 | 6 (35.3) | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 131 | 7 (5.3) | 0 | 8 (6.1) | 25 | 3 (12.0) | 0 | 7 (28.0) | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| On dialysis | 28 | 5 (17.9) | 0 | 5 (17.9) | 3 | 1 (33.3) | 0 | 1 (33.3) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (), % mortality | ||||||||||||||||
| CABG coronary artery bypass grafting | ||||||||||||||||
| (B) Operation for complications of MI (total; 1180) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chronic | Acute | Concomitant operation | |||||||||
| Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | ||||||
| Hospital | After discharge | Hospital | After discharge | CABG | MVP | MVR | |||||
| Infarctectomy or Aneurysmectomy | 90 | 6 (6.7) | 0 | 8 (8.9) | 36 | 10 (27.8) | 1 (2.8) | 15 (41.7) | 56 | 14 | 6 |
| VSP closure | 86 | 12 (14.0) | 0 | 21 (24.4) | 244 | 60 (24.6) | 0 | 77 (31.6) | 85 | 9 | 0 |
| Cardiac rupture | 50 | 7 (14.0) | 0 | 10 (20.0) | 231 | 64 (27.7) | 0 | 78 (33.8) | 38 | 3 | 4 |
| Mitral regurgitation | |||||||||||
| (1) Papillary muscle rupture | 23 | 2 (8.7) | 0 | 2 (8.7) | 70 | 14 (20.0) | 0 | 20 (28.6) | 35 | 15 | 78 |
| (2) Ischemic | 142 | 9 (6.3) | 0 | 11 (7.7) | 39 | 6 (15.4) | 0 | 9 (23.1) | 134 | 111 | 70 |
| Others | 90 | 1 (1.1) | 0 | 2 (2.2) | 79 | 20 (25.3) | 0 | 25 (31.6) | 59 | 10 | 4 |
| Total | 481 | 37 (7.7) | 0 | 54 (11.2) | 699 | 174 (24.9) | 1 (0.1) | 224 (32.0) | 407 | 162 | 162 |
| (), % mortality | |||||||||||
| MI myocardial infarction; CABG coronary artery bypass grafting; MVP mitral valve repair; MVR mitral valve replacement; VSP ventricular septal perforation | |||||||||||
| Acute, within 2 weeks from the onset of myocardial infarction | |||||||||||
| (3) Operation for arrhythmia (total; 6720) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | 30-day mortality | Hospital mortality | Concomitant operation | ||||||||
| Isolated | Congenital | Valve | IHD | Others | Multiple combination | ||||||
| Hospital | After discharge | 2 categories | 3 categories | ||||||||
| Maze | 3442 | 53 (1.5) | 0 | 98 (2.8) | 155 | 172 | 2918 | 572 | 319 | 660 | 36 |
| For WPW | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 |
| For ventricular tachyarrhythmia | 23 | 0 | 0 | 1 (4.3) | 1 | 1 | 4 | 10 | 5 | 3 | 0 |
| Others | 3254 | 74 (2.3) | 2 (0.06) | 127 (3.9) | 80 | 153 | 2680 | 635 | 382 | 654 | 38 |
| Total | 6720 | 127 (1.9) | 2 (0.03) | 226 (3.4) | 236 | 326 | 5603 | 1218 | 706 | 1318 | 74 |
| (), % mortality | |||||||||||
| WPW Wolff–Parkinson-White syndrome; IHD ischemic heart disease | |||||||||||
| Except for 170 isolated cases, all remaining 5164 cases are doubly allocated, one for this subgroup and the other for the subgroup corresponding to the concomitant operations | |||||||||||
| (4) Operation for constrictive pericarditis (total; 190) | ||||||||
|---|---|---|---|---|---|---|---|---|
| CPB ( +) | CPB ( −) | |||||||
| Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | |||
| Hospital | After discharge | Hospital | After discharge | |||||
| Total | 102 | 6 (5.9) | 0 | 12 (11.8) | 88 | 4 (4.5) | 2 (2.3) | 7 (8.0) |
| (), % mortality | ||||||||
| CPB cardiopulmonary bypass | ||||||||
| (5) Cardiac tumor (total; 618) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Cases | 30-day mortality | Hospital mortality | Concomitant operation | |||||
| Hospital | After discharge | AVR | MVR | CABG | Others | |||
| Benign tumor | 550 | 6 (1.1) | 0 | 8 (1.5) | 24 | 15 | 40 | 120 |
| (Cardiac myxoma) | 392 | 2 (0.5) | 0 | 3 (0.8) | 7 | 3 | 22 | 73 |
| Malignant tumor | 68 | 8 (11.8) | 0 | 8 (11.8) | 0 | 2 | 7 | 13 |
| (Primary) | 38 | 3 (7.9) | 0 | 3 (7.9) | 0 | 1 | 4 | 8 |
| (), % mortality | ||||||||
| AVR aortic valve replacement; MVR mitral valve replacement; CABG coronary artery bypass grafting | ||||||||
| (6) HOCM and DCM (total; 226) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Cases | 30-day mortality | Hospital mortality | Concomitant operation | |||||
| Hospital | After discharge | AVR | MVR | MVP | CABG | |||
| Myectomy | 116 | 4 (3.4) | 0 | 5 (4.3) | 41 | 16 | 14 | 6 |
| Myotomy | 4 | 0 | 0 | 0 | 1 | 1 | 0 | 0 |
| No-resection | 100 | 7 (7.0) | 0 | 13 (13.0) | 20 | 51 | 49 | 4 |
| Volume reduction surgery of the left ventricle | 6 | 0 | 0 | 1 (16.7) | 1 | 0 | 4 | 1 |
| Total | 226 | 11 (4.9) | 0 | 19 (8.4) | 63 | 68 | 67 | 11 |
| (), % mortality | ||||||||
| HOCM hypertrophic obstructive cardiomyopathy; DCM dilated cardiomyopathy; AVR aortic valve replacement; MVR mitral valve replacement; MVP mitral valve repair, CABG coronary artery bypass grafting | ||||||||
| (7) Other open-heart operation (total; 1184) | ||||
|---|---|---|---|---|
| Cases | 30-day mortality | Hospital mortality | ||
| Hospital | After discharge | |||
| Open-heart operation | 491 | 57 (11.6) | 0 | 82 (16.7) |
| Non-open-heart operation | 693 | 81 (11.7) | 0 | 115 (16.6) |
| Total | 1184 | 138 (11.7) | 0 | 197 (16.6) |
| (), % mortality | ||||
Table 3.
Thoracic aortic aneurysm (total; 22,982)
(1) Dissection (total; 11,247)
| Stanford type | Acute | Chronic | Concomitant operation | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | A | B | ||||||||||||||||||||
| Replaced site | Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | AVP | AVR | MVP | MVR | CABG | Others | |||||
| Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | Hospital | After discharge | ||||||||||||||||
| Ascending Ao | 1934 | 129 (6.7) | 2 (0.10) | 175 (9.0) | 4 | 1 (25.0) | 0 | 1 (25.0) | 222 | 6 (2.7) | 0 | 7 (3.2) | 3 | 0 | 0 | 0 | 56 | 130 | 18 | 11 | 84 | 35 | |
| Aortic Root | 188 | 22 (11.7) | 0 | 25 (13.3) | 0 | 0 | 0 | 0 | 94 | 3 (3.2) | 1 (1.1) | 5 (5.3) | 5 | 0 | 0 | 0 | 29 | 194 | 2 | 1 | 66 | 6 | |
| Arch | 2092 | 143 (6.8) | 1 (0.05) | 190 (9.1) | 21 | 0 | 0 | 0 | 393 | 5 (1.3) | 0 | 11 (2.8) | 176 | 9 (5.1) | 0 | 13 (7.4) | 66 | 133 | 11 | 11 | 124 | 32 | |
| Aortic root + asc. Ao. + Arch | 170 | 20 (11.8) | 0 | 27 (15.9) | 1 | 0 | 0 | 0 | 60 | 2 (3.3) | 0 | 3 (5.0) | 7 | 1 (14.3) | 0 | 1 (14.3) | 31 | 151 | 2 | 0 | 56 | 0 | |
| Descending Ao | 20 | 0 | 0 | 1 (5.0) | 33 | 4 (12.1) | 0 | 5 (15.2) | 73 | 1 (1.4) | 0 | 3 (4.1) | 201 | 3 (1.5) | 0 | 9 (4.5) | 2 | 2 | 0 | 0 | 2 | 0 | |
| Thoracoabdominal | 2 | 0 | 0 | 0 | 19 | 2 (10.5) | 0 | 4 (21.1) | 55 | 4 (7.3) | 0 | 6 (10.9) | 163 | 12 (7.4) | 0 | 18 (11.0) | 0 | 0 | 0 | 0 | 0 | 0 | |
| Simple TEVAR | 105 | 9 (8.6) | 0 | 12 (11.4) | 450 | 37 (8.2) | 1 (0.2) | 43 (9.6) | 251 | 2 (0.8) | 1 (0.4) | 4 (1.6) | 1186 | 14 (1.2) | 1 (0.1) | 22 (1.9) | 0 | 1 | 0 | 0 | 0 | 1 | |
| Open SG with BR | 1350 | 112 (8.3) | 2 (0.15) | 135 (10.0) | 59 | 3 (5.1) | 0 | 6 (10.2) | 193 | 4 (2.1) | 1 (0.5) | 8 (4.1) | 229 | 8 (3.5) | 0 | 11 (4.8) | 48 | 132 | 7 | 3 | 103 | 13 | |
| Open SG without BR | 526 | 50 (9.5) | 0 | 62 (11.8) | 21 | 2 (9.5) | 0 | 2 (9.5) | 74 | 1 (1.4) | 0 | 3 (4.1) | 85 | 3 (3.5) | 0 | 4 (4.7) | 17 | 47 | 3 | 1 | 34 | 2 | |
| Arch TEVAR with BR | 20 | 0 | 0 | 0 | 146 | 11 (7.5) | 0 | 13 (8.9) | 67 | 1 (1.5) | 0 | 2 (3.0) | 431 | 5 (1.2) | 0 | 7 (1.6) | 0 | 0 | 0 | 0 | 0 | 0 | |
| Thoracoabdominal TEVAR with BR | 3 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 23 | 2 (8.7) | 0 | 3 (13.0) | 0 | 0 | 0 | 0 | 0 | 0 | |
| Other | 6 | 2 (33.3) | 0 | 2 (33.3) | 21 | 4 (19.0) | 0 | 6 (28.6) | 19 | 1 (5.3) | 0 | 1 (5.3) | 35 | 0 | 0 | 1 (2.9) | 0 | 0 | 0 | 0 | 0 | 0 | |
| Total | 6416 | 323 (5.0) | 5 (0.08) | 629 (9.8) | 778 | 64 (8.2) | 1 (0.1) | 80 (10.3) | 1509 | 30 (2.0) | 3 (0.2) | 53 (3.5) | 2544 | 57 (2.2) | 1 (0.0) | 89 (3.5) | 249 | 790 | 43 | 27 | 469 | 89 | |
| (), % mortality | |||||||||||||||||||||||
| Ao aorta; AVP aortic valve repair; AVR aortic valve replacement; MVP mitral valve repair; MVR mitral valve replacement; CABG coronary artery bypass grafting; TEVAR thoracic endovascular aortic (aneurysm) repair | |||||||||||||||||||||||
| Acute, within 2 weeks from the onset | |||||||||||||||||||||||
| (2) Non-dissection (total; 11,735) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Replaced site | Unruptured | Ruptured | Concomitant operation | |||||||||||
| Cases | 30-day mortality | Hospital mortality | Cases | 30-day mortality | Hospital mortality | AVP | AVR | MVP | MVR | CABG | Others | |||
| Hospital | After discharge | Hospital | After discharge | |||||||||||
| Ascending Ao | 1334 | 20 (1.5) | 3 (0.22) | 38 (2.8) | 53 | 3 (5.7) | 0 | 9 (17.0) | 37 | 929 | 69 | 40 | 154 | 88 |
| Aortic Root | 1114 | 27 (2.4) | 0 | 42 (3.8) | 50 | 10 (20.0) | 0 | 14 (28.0) | 285 | 790 | 67 | 34 | 148 | 63 |
| Arch | 2041 | 35 (1.7) | 1 (0.05) | 71 (3.5) | 98 | 10 (10.2) | 0 | 15 (15.3) | 34 | 571 | 47 | 17 | 260 | 83 |
| Aortic root + asc. Ao. + Arch | 259 | 9 (3.5) | 0 | 15 (5.8) | 16 | 5 (31.3) | 0 | 5 (31.3) | 49 | 190 | 9 | 4 | 39 | 11 |
| Descending Ao | 276 | 10 (3.6) | 0 | 22 (8.0) | 36 | 4 (11.1) | 0 | 6 (16.7) | 1 | 3 | 1 | 0 | 10 | 3 |
| Thoracoabdominal | 322 | 12 (3.7) | 0 | 21 (6.5) | 35 | 7 (20.0) | 0 | 8 (22.9) | 0 | 0 | 0 | 0 | 0 | 0 |
| Simple TEVAR | 2417 | 36 (1.5) | 5 (0.21) | 65 (2.7) | 349 | 49 (14.0) | 2 (0.57) | 64 (18.3) | 0 | 0 | 0 | 0 | 1 | 6 |
| Open SG with BR | 1200 | 36 (3.0) | 0 | 70 (5.8) | 81 | 11 (13.6) | 0 | 17 (21.0) | 21 | 134 | 13 | 6 | 185 | 24 |
| Open SG without BR | 464 | 7 (1.5) | 0 | 21 (4.5) | 38 | 4 (10.5) | 0 | 7 (18.4) | 6 | 79 | 6 | 4 | 49 | 19 |
| Arch TEVAR with BR | 1190 | 19 (1.6) | 3 | 44 (3.7) | 75 | 9 (12.0) | 0 | 13 (17.3) | 0 | 3 | 0 | 0 | 5 | 4 |
| Thoracoabdominal TEVAR with BR | 98 | 4 (4.1) | 1 (1.02) | 10 (10.2) | 14 | 1 (7.1) | 0 | 2 (14.3) | 0 | 0 | 0 | 0 | 0 | 0 |
| Other | 153 | 6 (3.9) | 1 (0.65) | 9 (5.9) | 22 | 4 (18.2) | 0 | 5 (22.7) | 0 | 13 | 0 | 1 | 5 | 5 |
| Total | 10,868 | 221 (2.0) | 14 (0.13) | 428 (3.9) | 867 | 117 (13.5) | 2 (0.23) | 165 (19.0) | 433 | 2712 | 212 | 106 | 856 | 306 |
| (), % mortality | ||||||||||||||
| Ao aorta; AVP aortic valve repair; AVR aortic valve replacement; MVP mitral valve repair; MVR mitral valve replacement; CABG coronary artery bypass grafting; TEVAR thoracic endovascular aortic (aneurysm) repair | ||||||||||||||
Table 4.
Pulmonary thromboembolism (total; 185)
| Cases | 30-day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| Acute | 125 | 12 (9.6) | 1 (0.8) | 15 (12.0) |
| Chronic | 60 | 0 | 0 | |
| Total | 185 | 12 (6.5) | 1 (0.5) | 15 (8.1) |
(), % mortality
Table 5.
Implantation of VAD (total; 144)
| Cases | 30-day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| Implantation of VAD | 144 | 1 (0.7) | 0 | 9 (6.3) |
(), % mortality
VAD ventricular assist devise
Table 6.
Heart transplantation (total; 59)
| Cases | Hospital mortality | |
|---|---|---|
| Heart transplantation | 59 | 0 |
| Heart and lung transplantation | 0 | 0 |
| Total | 59 | 0 (0.0) |
(), % mortality
Among the 8349 procedures for congenital heart disease conducted in 2021, 6510 were open-heart surgeries, with an overall hospital mortality rate of 1.7% (Table 1). The number of surgeries for neonates and infants in 2021 significantly decreased compared to that in 2011 (3958 vs 5048); on the other hands, hospital mortality did not significantly differ compared to those in 2011 (7.1% vs 6.6% for neonates and 2.4–2.7% for infants) despite the increasing ratio of surgeries for severe cases. In 2021, atrial septal defect (1302 cases) and ventricular septal defect (1338 cases) were the most common diseases as previously reported, with patients aged ≥ 18 years accounting for 59% of atrial septal defect and ventricular septal defect surgeries.
Hospital mortality of open heart surgeriews for complex congenital heart disease within the past 10 years was as follows (2011 [5], 2016 [6], and 2021): complete atrioventricular septal defect (2.6%, 2.4%, and 2.0%); tetralogy of Fallot (0.7%, 1.6%, and 0.5%); transposition of the great arteries with the intact septum (2.5%, 4.4%, and 5.0%), ventricular septal defect (3.6%, 8.3%, and 1.7%), single ventricle (4.4%, 5.1%, and 3.6%); and hypoplastic left heart syndrome (14.3%, 7.5%, and 8.0%). Currently, right heart bypass surgery has been commonly performed (291 bidirectional Glenn procedures, excluding 23 Damus–Kaye–Stansel procedures, and 385 Fontan type procedures, including total cavopulmonary connection) with acceptable hospital mortality rates (2.4% and 0.8%). The Norwood type I procedure was performed in 104 cases, with a relatively low hospital mortality rate (11.5%) (Table 1).
Valvular heart disease procedures, excluding transcatheter procedures, were performed less than that in the previous year. Isolated aortic valve replacement/repair with/without coronary artery bypass grafting (CABG) (n = 8206) was 4.5% fewer than that in the previous year (n = 8592) and 13.4% fewer than that 5 years ago (n = 9472 in 2016), as opposed to the rapid increase of transcatheter aortic valve replacement (n = 9774 and 12,202 in 2020 and 2021). Isolated mitral valve replacement/repairs with/without CABG (n = 4415) was not differ compared that in the previous year (n = 4471) and 3.5% fewer than that 5 years ago (n = 4576 in 2016). Aortic and mitral valve replacement with bioprosthesis were performed in 8866 and 2183 cases, respectively. The rate at which bioprosthesis was used had dramatically increased from 30% in the early 2000s [7, 8] to 88.2% and 71.5% in 2021 for aortic and mitral positions, respectively. Additionally, CABG was performed concurrently in 18.0% of all valvular procedures (17.5% in 2011 [5] and 18.4% in 2016 [6]). Valve repair was common in mitral and tricuspid valve positions (5662 and 3875 cases, respectively) but less common in aortic valve positions (152 patients, only 1.5% of all aortic valve procedures). Mitral valve repair accounted for 64.4% of all mitral valve procedures. Hospital mortality rates for isolated valve replacement for aortic and mitral positions were 2.5% and 7.9%, respectively, but only 1.2% for mitral valve repair. Moreover, hospital mortality rates for redo isolated valve surgery for the aortic and mitral positions were 5.3% and 6.5%, respectively. Finally, overall hospital mortality rates did not significantly improve over the past 10 years (3.4% in 2011 [5], 3.4% in 2016 [6], and 3.0% in 2021) (Table 2).
Isolated CABG had been performed in 10,184 cases, accounting for only 71.4% of the procedures performed 10 years ago (n = 14,256 in 2011) [5]. Of the aforementioned cases, 5807 (57.0%) underwent off-pump CABG, with a success rate of 97.3%. The percentage of planned off-pump CABG in 2021 was similar to that in 2020. Hospital mortality associated with primary elective CABG procedures among 8738 cases accounted for 1.8%, which is slightly higher than that in 2011 (1.1%) [5]. Hospital mortality for primary emergency CABG among 1352 cases remained high (9.2%). The percentage of conversion from off-pump to on-pump CABG or on-pump beating-heart CABG was 2.6% among the primary elective CABG cases, with a hospital mortality rate of 5.6%. Patients with end-stage renal failure on dialysis had higher hospital mortality rates than overall mortality, regardless of surgical procedure (on-pump arrest, on-pump beating, and off-pump). This study excluded concomitant CABGs alongside other major procedures under the ischemic heart disease category but rather under other categories, such as valvular heart disease and thoracic aortic aneurysm. Accordingly, the overall number of CABGs in 2020, including concomitant CABG with other major procedures, was 15,158 (Table 2).
Arrhythmia management was primarily performed as concomitant procedures in 6720 cases, with a hospital mortality rate of 3.4%. Pacemaker and implantable cardioverter-defibrillator implantation were not included in this category (Table 2).
In 2021, 22,982 procedures for thoracic and thoracoabdominal aortae diseases were performed, among which aortic dissection and non-dissection accounted for 11,247 and 11,735, respectively. The number of surgeries for aortic dissection this year was 3.6% higher than that in the preceding year (n = 10,855 in 2020). Hospital mortality rates for the 6416 Stanford type A acute aortic dissections remained high (9.8%). The number of procedures for non-dissected aneurysms increased by 0.4%, with a hospital mortality rate of 5.1% for all aneurysms and 3.9% and 19.0% for unruptured and ruptured aneurysms, respectively. Thoracic endovascular aortic repair (TEVAR) has been performed for aortic diseases at an increasing rate. Stent graft placement was performed in 5230 patients with aortic dissection, including 2693 TEVARs and 2537 open stent graftings. Moreover, 1640 and 314 cases underwent TEVAR and open stent grafting for type B chronic aortic dissection, accounting for 60.9% and 12.4% of the total number of cases, respectively. Hospital mortality rates associated with simple TEVAR for type B aortic dissection were 9.6% and 1.9% for acute and chronic cases, respectively. Stent graft placement was performed in 5926 patients with non-dissected aortic aneurysms, among which 4143 were TEVARs (an 1.3% increase compared to that in 2020, n = 4090) and 1783 were open stent graftings (a 10.6% increase compared to that in 2020, n = 1612). Hospital mortality rates were 3.2% and 18.0% for TEVARs and 5.5% and 20.2% for open stenting in unruptured and ruptured aneurysms, respectively (Table 3).
(B) General thoracic surgery
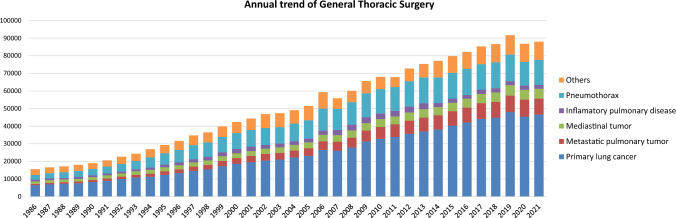
The 2021 survey of general thoracic surgeries comprised 699 surgical units, with bulk data submitted via a web-based collection system established by the NCD [3]. General thoracic surgery departments reported 88,027 procedures in 2021 (Table 7), which is 2.1 times more than that in 2000 and 5834 more procedures than that in 2016 [6] (Fig. 2). It increased compared to that in 2020 (the first year of COVID-19 pandemic: 86,813) [3] by 1.4%. However it still decreased by 3.9% compared to that of 2019 (before COVID-19 pandemic: 91,626) [2], mostly because of the protraction of COVID-19 pandemic, despite the steadily increase up to 2019.
Table 7.
Total cases of general thoracic surgery during 2021
| Cases | % | |
|---|---|---|
| Benign pulmonary tumor | 2418 | 2.7 |
| Primary lung cancer | 46,624 | 53.0 |
| Other primary malignant pulmonary tumor | 405 | 0.5 |
| Metastatic pulmonary tumor | 9047 | 10.3 |
| Tracheal tumor | 90 | 0.1 |
| Pleural tumor including mesothelioma | 524 | 0.6 |
| Chest wall tumor | 716 | 0.8 |
| Mediastinal tumor | 5590 | 6.4 |
| Thymectomy for MG without thymoma | 139 | 0.2 |
| Inflammatory pulmonary disease | 2117 | 2.4 |
| Empyema | 3123 | 3.5 |
| Bullous disease excluding pneumothorax | 273 | 0.3 |
| Pneumothorax | 14,266 | 16.2 |
| Chest wall deformity | 282 | 0.3 |
| Diaphragmatic hernia including traumatic | 37 | 0.0 |
| Chest trauma excluding diaphragmatic hernia | 461 | 0.5 |
| Lung transplantation | 93 | 0.1 |
| Others | 1822 | 2.1 |
| Total | 88,027 | 100.0 |
Fig. 2.
Annual trend of general thoracic surgery
In 2021, 46,624 procedures for primary lung cancer had been performed which increased by 2.6% compared to that of 2020 (45,436) [3], but still decreased by 3.0% compared to that of 2019 (48,052) [2], similarly to the total number of surgeries in general thoracic surgery. The number of procedures in 2021 was 2.5 times higher than that in 2000, with lung cancer procedures accounting for 53% of all general thoracic surgeries.
Information about the number of video-assisted thoracoscopic surgery (VATS), which is defined as surgical procedures using a skin incision less than 8 cm including a mini-thoracotomy (hybrid) approach, have been available since the 2015 annual report. Tables 8, 9, 11, 14, 15, 16, 18, 19, 20, 21, 22, 24, 25, and 26 present the number of VATS procedures for benign pulmonary tumors, primary lung cancer, metastatic pulmonary tumor, chest wall tumor, mediastinal tumor, thymectomy for myasthenia gravis, inflammatory pulmonary disease, empyema, descending necrotizing mediastinitis, bullous diseases, pneumothorax, diaphragmatic hernia, chest trauma and other respiratory surgeries in 2021, respectively.
Table 8.
Benign pulmonary tumor
| Cases | 30-day mortality | Hospital mortality | By VATS | ||
|---|---|---|---|---|---|
| Hospital | After discharge | ||||
| 1. Benign pulmonary tumor | |||||
| Hamartoma | 457 | 0 | 0 | 1 (0.2) | 435 |
| Sclerosing hemangioma | 107 | 0 | 0 | 0 | 99 |
| Papilloma | 21 | 0 | 0 | 0 | 18 |
| Mucous gland adenoma bronchial | 19 | 0 | 0 | 0 | 19 |
| Fibroma | 118 | 0 | 0 | 0 | 112 |
| Lipoma | 9 | 0 | 0 | 0 | 9 |
| Neurogenic tumor | 16 | 0 | 0 | 0 | 13 |
| Clear cell tumor | 1 | 0 | 0 | 0 | 1 |
| Leiomyoma | 16 | 0 | 0 | 0 | 15 |
| Chondroma | 4 | 0 | 0 | 0 | 4 |
| Inflammatory myofibroblastic tumor | 1 | 0 | 0 | 0 | 1 |
| Pseudolymphoma | 18 | 0 | 0 | 0 | 15 |
| Histiocytosis | 17 | 0 | 0 | 0 | 17 |
| Teratoma | 7 | 0 | 0 | 0 | 4 |
| Others | 1607 | 0 | 0 | 3 (0.2) | 1491 |
| Total | 2418 | 0 | 0 | 4 (0.17) | 2253 |
(), Mortality %
Table 9.
Primary malignant pulmonary tumor
| Cases | 30-Day mortality | Hospital mortality | VATS | Robotic surgery | ||
|---|---|---|---|---|---|---|
| Hospital | After discharge | |||||
| 2. Primary malignant pulmonary tumor | 47,029 | 119 (0.3) | 52 (0.1) | 218 (0.5) | 34,458 | 4253 |
| Lung cancer | 46,624 | 119 (0.3) | 52 (0.1) | 216 (0.5) | 34,458 | 4253 |
| Histological classification | ||||||
| Adenocarcinoma | 32,784 | 46 (0.1) | 28 (0.09) | 75 (0.2) | ||
| Squamous cell carcinoma | 8048 | 50 (0.6) | 17 (0.2) | 97 (1.2) | ||
| Large cell carcinoma | 323 | 0 | 2 (0.6) | 3 (0.9) | ||
| LCNEC | 549 | 2 (0.4) | 2 (0.4) | 3 (0.5) | ||
| Small cell carcinoma | 901 | 3 (0.3) | 2 (0.2) | 6 (0.7) | ||
| Adenosquamous carcinoma | 541 | 2 (0.4) | 0 | 5 (0.9) | ||
| Carcinoma with pleomorphic, sarcomatoid or sarcomatous elements | 520 | 8 (1.5) | 0 | 14 (2.7) | ||
| Carcinoid | 226 | 0 | 0 | 0 | ||
| Carcinomas of salivary-gland type | 46 | 0 | 0 | 0 | ||
| Unclassified | 36 | 0 | 0 | 0 | ||
| Multiple lung cancer | 2257 | 5 (0.2) | 1 (0.0) | 9 (0.4) | ||
| Others | 358 | 3 (0.8) | 0 | 4 (1.1) | ||
| Operative procedure | ||||||
| Wedge resection | 8683 | 14 (0.2) | 8 (0.1) | 22 (0.3) | 7982 | 18 |
| Segmental excision | 6781 | 8 (0.1) | 4 (0.06) | 17 (0.3) | 5438 | 619 |
| (Sleeve segmental excision) | 14 | 0 | 0 | 0 | 11 | 0 |
| Lobectomy | 30,682 | 89 (0.3) | 39 (0.13) | 160 (0.5) | 20,852 | 3609 |
| (Sleeve lobectomy) | 351 | 2 (0.6) | 1 (0.3) | 8 (2.3) | 46 | 8 |
| Pneumonectomy | 205 | 5 (2.4) | 0 | 12 (5.9) | 22 | 2 |
| (Sleeve pneumonectomy) | 6 | 0 | 0 | 0 | 0 | 0 |
| Other bronchoplasty | 30 | 1 (3.3) | 0 | 2 (6.7) | 1 | 0 |
| Pleuropneumonectomy | 2 | 0 | 0 | 0 | 1 | 0 |
| Others | 206 | 2 (1.0) | 1 (0.5) | 3 (1.5) | 133 | 4 |
| Multiple incision for multiple lung cancer | 35 | 0 | 0 | 1 (2.9) | 29 | 1 |
| Sarcoma | 54 | 0 | 0 | 1 (1.9) | ||
| AAH | 103 | 0 | 0 | 0 | ||
| Lymphoma | 197 | 0 | 0 | 1 (0.5) | ||
| Others | 51 | 0 | 0 | 0 | ||
(), Mortality %
Table 11.
Metastatic pulmonary tumor
| Cases | 30-Day mortality | Hospital mortality | VATS | Robotic surgery | ||
|---|---|---|---|---|---|---|
| Hospital | After discharge | |||||
| 3. Metastatic pulmonary tumor | 9047 | 5 (0.1) | 9 (0.10) | 10 (0.1) | 8331 | 298 |
| Colorectal | 4307 | 2 (0.05) | 2 (0.05) | 3 (0.1) | 4000 | 157 |
| Hepatobiliary/Pancreatic | 503 | 0 | 0 | 0 | 474 | 16 |
| Uterine | 530 | 0 | 0 | 0 | 483 | 21 |
| Mammary | 552 | 0 | 0 | 0 | 530 | 16 |
| Ovarian | 91 | 0 | 0 | 0 | 82 | 2 |
| Testicular | 50 | 0 | 0 | 0 | 45 | 0 |
| Renal | 733 | 0 | 0 | 0 | 687 | 22 |
| Skeletal | 89 | 0 | 0 | 0 | 72 | 5 |
| Soft tissue | 236 | 0 | 0 | 0 | 207 | 2 |
| Otorhinolaryngological | 469 | 0 | 2 (0.4) | 1 (0.2) | 434 | 16 |
| Pulmonary | 443 | 1 (0.2) | 1 (0.2) | 2 (0.5) | 362 | 4 |
| Others | 1044 | 2 (0.2) | 4 (0.4) | 4 (0.4) | 955 | 37 |
(), Mortality %
Table 14.
Chest wall tumor
| Cases | 30-Day mortality | Hospital mortality | VATS | ||
|---|---|---|---|---|---|
| Hospital | After discharge | ||||
| 6. Chest wall tumor | |||||
| Primary malignant tumor | 137 | 0 | 0 | 0 | 37 |
| Metastatic malignant tumor | 188 | 0 | 2(1.1) | 2(1.1) | 61 |
| Benign tumor | 391 | 1(0.3) | 0 | 1(0.3) | 297 |
| Total | 716 | 1(0.1) | 2(0.3) | 3(0.4) | 395 |
(), Mortality %
Table 15.
Mediastinal tumor
| Cases | 30-Day mortality | Hospital mortality | By VATS | Robotic surgery | ||
|---|---|---|---|---|---|---|
| Hospital | After discharge | |||||
| 7. Mediastinal tumor | 5590 | 7 (0.13) | 1 (0.02) | 10 (0.2) | 4373 | 1261 |
| Thymoma* | 2174 | 3 (0.1) | 1 (0.0) | 3 (0.1) | 1557 | 517 |
| Thymic cancer | 380 | 1 (0.3) | 0 | 1 (0.3) | 228 | 57 |
| Thymus carcinoid | 49 | 0 | 0 | 0 | 27 | 13 |
| Germ cell tumor | 105 | 1 (1.0) | 0 | 1 (1.0) | 70 | 19 |
| Benign | 81 | 1 (1.2) | 0 | 1 (1.2) | 61 | 17 |
| Malignant | 24 | 0 | 0 | 0 | 9 | 2 |
| Neurogenic tumor | 479 | 0 | 0 | 0 | 448 | 102 |
| Congenital cyst | 1188 | 0 | 0 | 1 (0.1) | 1124 | 319 |
| Goiter | 86 | 0 | 0 | 0 | 42 | 7 |
| Lymphatic tumor | 164 | 1 (0.6) | 0 | 1 (0.6) | 130 | 28 |
| Excision of pleural recurrence of thymoma | 34 | 0 | 0 | 0 | 24 | 2 |
| Thymolipoma | 14 | 0 | 0 | 0 | 14 | 1 |
| Others | 917 | 1 (0.1) | 0 | 3 (0.3) | 709 | 196 |
(), Mortality %
Table 16.
Thymectomy for myasthenia gravis
| Cases | 30-Day mortality | Hospital mortality | By VATS | Robotic surgery | ||
|---|---|---|---|---|---|---|
| Hospital | After discharge | |||||
| 8. Thymectomy for myasthenia gravis | 505 | 0 | 0 | 0 | 352 | 38 |
| With thymoma | 366 | 0 | 0 | 0 | 249 | 5 |
(), Mortality %
Table 18.
A. Inflammatory pulmonary disease
| Cases | 30-Day mortality | Hospital mortality | VATS | ||
|---|---|---|---|---|---|
| Hospital | After discharge | ||||
| A. Inflammatory pulmonary disease | 2117 | 8 (0.4) | 3 (0.1) | 14 (0.7) | 1794 |
| Tuberculous infection | 29 | 0 | 0 | 0 | 21 |
| Mycobacterial infection | 428 | 2 (0.5) | 1 (0.2) | 2 (0.5) | 374 |
| Fungal infection | 270 | 0 | 0 | 3 (1.1) | 193 |
| Bronchiectasis | 41 | 0 | 0 | 0 | 29 |
| Tuberculous nodule | 58 | 0 | 0 | 0 | 50 |
| Inflammatory pseudotumor | 930 | 2 (0.2) | 0 | 2 (0.2) | 847 |
| Interpulmonary lymph node | 37 | 0 | 0 | 0 | 36 |
| Others | 324 | 4 (1.2) | 2 (0.6) | 7 (2.2) | 244 |
(), Mortality %
Table 19.
B. Empyema
| Cases | 30-Day mortality | Hospital mortality | By VATS | ||
|---|---|---|---|---|---|
| Hospital | After discharge | ||||
| Acute empyema | 2508 | 60 (2.4) | 5 (0.2) | 127 (5.1) | 2038 |
| With fistula | 483 | 32 (6.6) | 2 (0.4) | 64 (13.3) | 235 |
| Without fistula | 2000 | 25 (1.3) | 3 (0.2) | 60 (3.0) | 1780 |
| Unknown | 25 | 3 (12.0) | 0 | 3 (12.0) | 23 |
| Chronic empyema | 615 | 13 (2.1) | 4 (0.7) | 55 (8.9) | 315 |
| With fistula | 277 | 5 (1.8) | 2 (0.7) | 33 (11.9) | 81 |
| Without fistula | 299 | 6 (2.0) | 2 (0.7) | 18 (6.0) | 202 |
| Unknown | 39 | 2 (5.1) | 0 | 4 (10.3) | 32 |
| Total | 3123 | 73 (2.3) | 9 (0.3) | 182 (5.8) | 2353 |
(), Mortality %
Table 20.
C. Descending necrotizing mediastinitis
| Cases | 30-Day mortality | Hospital mortality | VATS | ||
|---|---|---|---|---|---|
| Hospital | After discharge | ||||
| C. Descending necrotizing mediastinitis | 94 | 4 (4.3) | 0 | 10 (10.6) | 59 |
(), Mortality %
Table 21.
D. Bullous diseases
| Cases | 30-Day mortality | Hospital mortality | VATS | ||
|---|---|---|---|---|---|
| Hospital | After discharge | ||||
| D. Bullous diseases | 273 | 3 (1.1) | 0 | 3 (1.1) | 241 |
| Emphysematous bulla | 198 | 2 (1.0) | 0 | 2 (1.0) | 183 |
| Bronchogenic cyst | 7 | 0 | 0 | 0 | 6 |
| Emphysema with LVRS | 14 | 1 (7.1) | 0 | 1 (7.1) | 11 |
| Others | 54 | 0 | 0 | 0 | 41 |
(), Mortality %
LVRS lung volume reduction surgery
Table 22.
E. Pneumothorax
| Cases | 30-Day mortality | Hospital mortality | VATS | |
|---|---|---|---|---|
| Hospital | After discharge | |||
| 14,266 | 94 (0.7) | 29 (0.2) | 159 (1.1) | 13,880 |
| Spontaneous pneumothorax | |||||
|---|---|---|---|---|---|
| Operative procedure | Cases | 30-Day mortality | Hospital mortality | VATS | |
| Hospital | After discharge | ||||
| Bullectomy | 2465 | 4 (0.2) | 1 (0.0) | 7 (0.3) | 2424 |
| Bullectomy with additional procedure | 7217 | 9 (0.1) | 2 (0.03) | 14 (0.2) | 7123 |
| Coverage with artificial material | 7011 | 8 (0.1) | 2 (0.03) | 12 (0.2) | 6924 |
| Parietal pleurectomy | 40 | 0 | 0 | 1 (2.5) | 39 |
| Coverage and parietal pleurectomy | 63 | 0 | 0 | 0 | 61 |
| Others | 103 | 1 (1.0) | 0 | 1 (1.0) | 99 |
| Others | 636 | 7 (1.1) | 1 (0.2) | 8 (1.3) | 584 |
| Unknown | 11 | 0 | 1 (9.1) | 0 | 9 |
| Total | 10,329 | 20 (0.2) | 5 (0.0) | 29 (0.3) | 10,140 |
| Secondary pneumothorax | |||||
|---|---|---|---|---|---|
| Associated disease | Cases | 30-Day mortality | Hospital mortality | VATS | |
| Hospital | After discharge | ||||
| COPD | 2745 | 39 (1.4) | 10 (0.4) | 66 (2.4) | 2625 |
| Tumorous disease | 156 | 11 (7.1) | 4 (2.6) | 16 (10.3) | 147 |
| Catamenial | 200 | 0 | 0 | 0 | 199 |
| LAM | 39 | 0 | 0 | 0 | 39 |
| Others (excluding pneumothorax by trauma) | 797 | 24 (3.0) | 8 (1.0) | 48 (6.0) | 730 |
| Unknown | 0 | 0 | 0 | 0 | 0 |
| Operative procedure | Cases | 30 Day mortality | Hospital mortality | VATS | |
|---|---|---|---|---|---|
| Hospital | After discharge | ||||
| Bullectomy | 693 | 10 (1.4) | 5 (0.7) | 19 (2.7) | 673 |
| Bullectomy with additional procedure | 2359 | 25 (1.1) | 9 (0.4) | 44 (1.9) | 2285 |
| coverage with artificial material | 2265 | 25 (1.1) | 9 (0.4) | 41 (1.8) | 2197 |
| parietal pleurectomy | 7 | 0 | 0 | 0 | 7 |
| coverage and parietal pleurectomy | 31 | 0 | 0 | 0 | 29 |
| others | 56 | 0 | 0 | 3 (5.4) | 52 |
| Others | 882 | 39 (4.4) | 8 (0.9) | 67 (7.6) | 776 |
| Unknown | 3 | 0 | 0 | 0 | 3 |
| Total | 3937 | 74 (1.9) | 22 (0.6) | 130 (3.3) | 3737 |
(), Mortality %
Table 24.
G. Diaphragmatic hernia
| Cases | 30-Day mortality | Hospital mortality | VATS | ||
|---|---|---|---|---|---|
| Hospital | After discharge | ||||
| G. Diaphragmatic hernia | 37 | 0 | 0 | 0 | 11 |
| Congenital | 8 | 0 | 0 | 0 | 1 |
| Traumatic | 12 | 0 | 0 | 0 | 3 |
| Others | 17 | 0 | 0 | 0 | 7 |
(), Mortality %
Table 25.
H. Chest trauma
| Cases | 30-Day mortality | Hospital mortality | VATS | ||
|---|---|---|---|---|---|
| Hospital | After discharge | ||||
| H. Chest trauma | 461 | 32 (6.9) | 2 (0.4) | 35 (7.6) | 257 |
(), Mortality %
Table 26.
I. Other respiratory surgery
| Cases | 30-Day mortality | Hospital mortality | VATS | ||
|---|---|---|---|---|---|
| Hospital | After discharge | ||||
| I. Other respiratory surgery | 1728 | 38 (2.2) | 3 (0.2) | 75 (4.3) | 1267 |
| Arteriovenous malformation* | 98 | 0 | 0 | 0 | 93 |
| Pulmonary sequestration | 87 | 0 | 0 | 0 | 71 |
| Postoperative bleeding ・air leakage | 553 | 14 (2.5) | 2 (0.4) | 38 (6.9) | 344 |
| Chylothorax | 55 | 0 | 0 | 0 | 45 |
| Others | 935 | 24 (2.6) | 1 (0.1) | 37 (4.0) | 714 |
(), Mortality %
A total of 2418 procedures for benign pulmonary tumors had been conducted in 2021 (Table 8). Hamartomas were the most frequent benign pulmonary tumors diagnosed, with 2253 patients (93%) undergoing VATS.
Tables 9 and 10 show additional information on primary malignant pulmonary tumors. Accordingly, the most frequently diagnosed lung cancer subtype was adenocarcinoma (71% of all lung cancers), followed by squamous cell carcinoma (17%). Sublobar resection was performed in 15,464 lung cancer cases (33% of all cases) and lobectomy in 30,682 cases (66% of all cases). Sleeve lobectomy was performed in 351 cases (0.8% of all cases), while pneumonectomy was required in 205 cases (0.4% of all cases). VATS lobectomy was performed in 20,852 cases of lung cancer (68% of all lobectomy cases). RATS lobectomy was performed in 3609 cases of lung cancer (12% of all lobectomy cases). Patients aged ≥ 80 years who underwent lung cancer surgery accounted for 6912 (15%). Among those who died within 30 days postoperatively, 119 and 52 died before and after hospital discharge, respectively. Overall, 171 patients died within 30 days postoperatively (30-day mortality rate, 0.4%), while 119 died before discharge (hospital mortality rate, 0.3%). Moreover, 30-day mortality rates according to the procedure were 0.1%, 0.4%, and 2.4% for segmentectomy, lobectomy, and pneumonectomy, respectively. Interstitial pneumonia had been the leading cause of death after lung cancer surgery, followed by pneumonia, cardiovascular events and respiratory failure.
Table 10.
Details of lung cancer operations
| TNM | |
|---|---|
| c-Stage | Cases |
| 0 | 2126 |
| IA1 | 8867 |
| IA2 | 13,972 |
| IA3 | 7991 |
| IB | 4994 |
| IIA | 1582 |
| IIB | 3570 |
| IIIA | 2422 |
| IIIB | 451 |
| IIIC | 18 |
| IVA | 400 |
| IVB | 95 |
| NA | 102 |
| Total | 46,590 |
| Sex | Cases |
|---|---|
| Male | 28,363 |
| Female | 18,226 |
| NA | 0 |
| Total | 46,589 |
| Cause of death | Cases |
|---|---|
| Cardiovascular | 37 |
| Pneumonia | 73 |
| Pyothorax | 2 |
| Bronchopleural fistula | 15 |
| Respiratory failure | 22 |
| Pulmonary embolism | 7 |
| Interstitial pneumonia | 109 |
| Brain infarction or bleeding | 18 |
| Others | 136 |
| Unknown | 35 |
| Total | 454 |
| p-Stage | Cases |
|---|---|
| 0(pCR) | 3308 |
| IA1 | 9431 |
| IA2 | 10,842 |
| IA3 | 5229 |
| IB | 6560 |
| IIA | 1310 |
| IIB | 4363 |
| IIIA | 3541 |
| IIIB | 732 |
| IIIC | 11 |
| IVA | 886 |
| IVB | 90 |
| NA | 286 |
| Total | 46,589 |
| Age (y) | Cases |
|---|---|
| < 20 | 20 |
| 20–29 | 65 |
| 30–39 | 235 |
| 40–49 | 1226 |
| 50–59 | 3828 |
| 60–69 | 11,020 |
| 70–79 | 23,283 |
| 80–89 | 6779 |
| ≥ 90 | 133 |
| NA | 0 |
| Total | 46,589 |
The procedures for metastatic pulmonary tumors performed in 2021 decreased 6.3% to 9047 cases compared to that in 2020 (9654) [3], which showed contrastive trend to primary lung cancer (Table 11). Among such procedures, the most frequent primary tumor was colorectal cancer (48% of all cases).
A total of 90 procedures for tracheal tumors, including 37, 25, and 28 cases of primary malignant, metastatic, and benign tracheal tumors, respectively, were performed in 2021. Further, 16 patients underwent sleeve resection and reconstruction (Table 12).
Table 12.
Tracheal tumor
| Cases | 30-Day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| 4. Tracheal tumor | 90 | 6 (6.7) | 1 (1.1) | 8 (8.9) |
| A. Primary malignant tumor | ||||
| Histological classification | ||||
| Squamous cell carcinoma | 6 | 0 | 0 | 0 |
| Adenoid cystic carcinoma | 22 | 0 | 0 | 0 |
| Mucoepidermoid carcinoma | 1 | 0 | 0 | 0 |
| Others | 8 | 0 | 0 | 0 |
| Total | 37 | 0 | 0 | 0 |
| B. Metastatic/invasive malignant tumor e.g. invasion of thyroid cancer | ||||
| 25 | 4 (16.0) | 1 (4.0) | 6 (24.0) | |
| C. Benign tracheal tumor | ||||
| Papilloma | 5 | 0 | 0 | 0 |
| Adenoma | 0 | 0 | 0 | 0 |
| Neurofibroma | 1 | 0 | 0 | 0 |
| Chondroma | 0 | 0 | 0 | 0 |
| Leiomyoma | 4 | 0 | 0 | 0 |
| Others | 18 | 2(11.1) | 0 | 2(11.1) |
| Histology unknown | 0 | 0 | 0 | 0 |
| Total | 28 | 2(7.1) | 0 | 2(7.1) |
| Operative procedure | ||||
| Sleeve resection with reconstruction | 16 | 0 | 0 | 0 |
| Wedge with simple closure | 2 | 0 | 0 | 0 |
| Wedge with patch closure | 0 | 0 | 0 | 0 |
| Total laryngectomy with tracheostomy | 0 | 0 | 0 | 0 |
| Others | 0 | 0 | 0 | 0 |
| Unknown | 0 | 0 | 0 | 0 |
| Total | 18 | 0 | 0 | 0 |
(), Mortality %
Overall, 524 pleural tumors had been diagnosed in 2021 (Table 13), with diffuse malignant pleural mesothelioma as the most frequent histologic diagnosis. Total pleurectomy was performed in 123 cases and extrapleural pneumonectomy in 26 cases. The 30-day mortality rate was 0% and 4% after total pleurectomy and extrapleural pneumonectomy, respectively.
Table 13.
Tumor of pleural origin
| Histological classification | Cases | 30-Day mortality | Hospital mortality | |
|---|---|---|---|---|
| Hospital | After discharge | |||
| Solitary fibrous tumor | 101 | 0 | 0 | 0 |
| Diffuse malignant pleural mesothelioma | 203 | 3 (1.5) | 0 | 4 (2.0) |
| Localized malignant pleural mesothelioma | 26 | 0 | 0 | 0 |
| Others | 194 | 5 (2.6) | 0 | 6 (3.1) |
| Total | 524 | 8 (1.5) | 0 | 10 (1.9) |
| Operative procedure | Cases | 30-Day mortality | Hospital mortality | |
|---|---|---|---|---|
| Hospital | After discharge | |||
| Extrapleural pneumonectomy | 26 | 1 (3.8) | 0 | 1 (3.8) |
| Total pleurectomy | 123 | 0 | 0 | 0 |
| Others | 54 | 2 (3.7) | 0 | 3 (5.6) |
| Total | 203 | 3 (1.5) | 0 | 4 (2.0) |
(), Mortality %
Overall, 716 chest wall tumor resections had been performed in 2021, including 137, 188, and 391 cases of primary malignant, metastatic, and benign tumors, respectively (Table 14).
In 2021, 5590 mediastinal tumors were resected, which was similar to that in 2020 (5573) (Table 15) [3]. Thymic epithelial tumors, including 2174 thymomas, 380 thymic carcinomas, and 49 thymic carcinoids, were the most frequently diagnosed mediastinal tumor subtype in 2021.
A total of 505 patients underwent thymectomy for myasthenia gravis (Table 16), among which 366 procedures were associated with thymoma in 2021.
Overall, 22,381 patients underwent procedures for non-neoplastic disease. Accordingly, 2117 patients underwent lung resection for inflammatory lung diseases (Table 17, 18), among which 428 and 270 patients were associated with mycobacterial and fungal infections, respectively. Procedures for inflammatory pseudotumor were performed in 930 cases (44%).
Table 17.
Operations for non-neoplastic diseases: A + B + C + D + E + F + G + H + I
| Cases | 30-Day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| 9. Operations for non-neoplastic diseases | 22,381 | 252 (1.1) | 46 (0.2) | 479 (2.1) |
A total of 3123 procedures were performed for empyema (Table 19), among which 2508 (80%) were acute and 615 (20%) were chronic. Further, pleural fistulas developed in 483 and 277 patients with acute and chronic empyema, respectively. The hospital mortality rate was 13% among patients with acute empyema with fistula.
Further, 94 operations were performed for descending necrotizing mediastinitis (Table 20), with a hospital mortality rate of 11%.
A total of 273 procedures were conducted for bullous diseases (Table 21), while only 14 patients underwent lung volume reduction surgery.
A total of 14,266 procedures were performed for pneumothorax (Table 22). Among the 10,329 procedures for spontaneous pneumothorax, 2465 (24%) were bullectomies alone, while 7217 (70%) required additional procedures, such as coverage with artificial material, as well as parietal pleurectomy. A total of 3937 procedures for secondary pneumothorax were performed, with chronic obstructive pulmonary disease (COPD) being the most prevalent associated disease (2745 cases, 70%). The hospital mortality rate for secondary pneumothorax associated with COPD was 2.4%.
The 2021 survey reported 282 procedures for chest wall deformity (Table 23). However, this may have been underestimated because the Nuss procedure for pectus excavatum was more likely performed in pediatric surgery centers not associated with the Japanese Association for Thoracic Surgery.
Table 23.
F. Chest wall deformity
| Cases | 30-Day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| F. Chest wall deformity | 282 | 0 | 0 | 0 |
| Funnel chest | 268 | 0 | 0 | 0 |
| Others | 14 | 0 | 0 | 1 (7.1) |
(), Mortality %
Surgical treatment for diaphragmatic hernia was performed in 37 patients (Table 24). This may have been underestimated because procedures may have been classified as gastrointestinal surgery.
The survey reported 461 procedures for chest trauma, excluding iatrogenic injuries (Table 25), with a hospital mortality rate of 7.6%.
Table 26 summarizes the procedures for other diseases, including 98 and 87 cases of arteriovenous malformation and pulmonary sequestration, respectively.
A total of 93 lung transplantations were performed in 2021 (Table 27), among which 74 and 19 were from brain-dead and living-related donors, respectively. 30-day mortality for total lung transplantation was 1.1% (1/93).
Table 27.
Lung transplantation
| Cases | 30-Day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| Single lung transplantation from brain-dead donor | 44 | 0 | 0 | 0 |
| Bilateral lung transplantation from brain-dead donor | 30 | 1 (3.3) | 0 | 3 (10.0) |
| Lung transplantation from living donor | 19 | 0 | 0 | 1 (5.3) |
| Total lung transplantation | 93 | 1 (1.1) | 0 | 4 (4.3) |
| Donor of living donor lung transplantation | 37 | 0 | 0 | 0 |
(), Mortality %
In 2021, the number of VATS procedures increased by 1.4% from 76,073 to 77,152 compared to that of 2020 [3]with the increase of all procedures in general thoracic surgery (1.4%). The population of VATS procedures in all procedures 88% in 2021 was similar as that in 2020 (88%) (Table 28).
Table 28.
Video-assisted thoracic surgery
| Cases | 30-Day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| 11. Video-assisted thoracic surgery | 77,152 | 256 (0.3) | 86 (0.1) | 434 (0.6) |
(), Mortality % (including thoracic sympathectomy 330)
A total of 590 tracheobronchoplasty procedures were performed in 2021, including 352 sleeve lobectomies, 10 carinal reconstructions and 9 sleeve pneumonectomies (Table 29). 30-day mortality for sleeve lobectomy, carinal reconstruction and sleeve lobectomy were 10, 0 and 2% respectively.
Table 29.
Tracheobronchoplasty
| Cases | 30-Day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| 12. Tracheobronchoplasty | 590 | 11 (1.9) | 2 (0.3) | 23 (3.9) |
| Trachea | 30 | 0 | 0 | 0 |
| Sleeve resection with reconstruction | 19 | 0 | 0 | 0 |
| Wedge with simple closure | 3 | 0 | 0 | 0 |
| Wedge with patch closure | 0 | 0 | 0 | 0 |
| Total laryngectomy with tracheostomy | 0 | 0 | 0 | 0 |
| Others | 8 | 0 | 0 | 0 |
| Carinal reconstruction | 10 | 0 | 0 | 1 (10.0) |
| Sleeve pneumonectomy | 9 | 0 | 0 | 0 |
| Sleeve lobectomy | 352 | 1 (0.3) | 7 (2.0) | |
| Sleeve segmental excision | 15 | 0 | 0 | |
| Bronchoplasty without lung resection | 16 | 0 | 1 (6.3) | |
| Others | 158 | 8 (5.1) | 1 (0.6) | 14 (8.9) |
(), Mortality %
Tables 30, 31, and 32 present the details regarding pediatric surgery and combined resection of neighboring organs.
Table 30.
Pediatric surgery
| Cases | 30-Day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| 13. Pediatric surgery | 355 | 5 (1.4) | 0 | 5 (1.4) |
(), Mortality %
Table 31.
Combined resection of neighboring organ(s)
| Cases | 30-Day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| 14. Combined resection of neighboring organ(s) | 1229 | 11 (0.9) | 1 (0.1) | 21 (1.7) |
| Organ resected | Cases | 30-Day mortality | Hospital mortality | |
|---|---|---|---|---|
| Hospital | After discharge | |||
| A. Primary lung cancer | ||||
| Aorta | 7 | 0 | 0 | 0 |
| Superior vena cava | 22 | 1 (4.5) | 0 | 4 (18.2) |
| Brachiocephalic vein | 7 | 0 | 0 | 0 |
| Pericardium | 65 | 0 | 0 | 2 (3.1) |
| Pulmonary artery | 105 | 2 (1.9) | 1 (1.0) | 4 (3.8) |
| Left atrium | 9 | 0 | 0 | 1 (11.1) |
| Diaphragm | 52 | 0 | 0 | 0 |
| Chest wall (including ribs) | 279 | 5 (1.8) | 0 | 8 (2.9) |
| Vertebra | 9 | 0 | 0 | 0 |
| Esophagus | 3 | 0 | 0 | 0 |
| Total | 558 | 8 (1.4) | 1 (0.2) | 19 (3.4) |
| B. Mediastinal tumor | ||||
| Aorta | 4 | 0 | 0 | 0 |
| Superior vena cava | 58 | 1 (1.7) | 0 | 1 (1.7) |
| Brachiocephalic vein | 111 | 0 | 0 | 0 |
| Pericardium | 357 | 2 (0.6) | 0 | 2 (0.6) |
| Pulmonary artery | 5 | 0 | 0 | 0 |
| Left atrium | 1 | 0 | 0 | 0 |
| Diaphragm | 40 | 0 | 0 | 0 |
| Chest wall (including ribs) | 17 | 0 | 0 | 0 |
| Vertebra | 4 | 0 | 0 | 0 |
| Esophagus | 4 | 0 | 0 | 0 |
| Lung | 457 | 1 (0.2) | 0 | 1 (0.2) |
| Total | 1058 | 4 (0.4) | 0 | 4 (0.4) |
(), Mortality %
Table 32.
Operation of lung cancer invading the chest wall of the apex
| Cases | 30-Day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| 15. Operation of lung cancer invading the chest wall of the apex | 588 | 6 (1.0) | 1 (0.2) | 11 (1.9) |
(), Mortality %. Includes tumors invading the anterior apical chest wall and posterior apical chest wall (superior sulcus tumor, so called Pancoast type)
(C) Esophageal surgery
In 2018, the data collection method for esophageal surgery had been modified from self-reports using questionnaire sheets following each institution belonging to the Japanese Association for Thoracic Surgery to an automatic package downloaded from the NCD in Japan. Consequently, the registry excluded data for non-surgical cases with esophageal diseases. Furthermore, data regarding the histological classification of malignant tumors, multiple primary cancers, and mortality rates for cases with combined resection of other organs could not be registered because they were not included in the NCD. Instead, detailed data regarding postoperative surgical and non-surgical complications were collected from the NCD. Moreover, data regarding surgeries for corrosive esophageal strictures and salvage surgeries for esophageal cancer had been exceptionally registered by participating institutions (Table 33).
Table 33.
Diagnostic procedures
| Cases | 30-Day mortality | Hospital mortality | ||
|---|---|---|---|---|
| Hospital | After discharge | |||
| Mediastinoscopic biopsy | 258 | 0 | 1 (0.4) | 1 (0.4) |
| Lung biopsy for diffuse parenchymal lung disease | 634 | 3 (0.5) | 2 (0.3) | 5 (0.8) |
| Biopsy for lymph node, tumor and pleura | 2926 | 27 (0.9) | 20 (0.7) | 48 (1.6) |
| Others | 1494 | 68 (4.6) | 12 (0.8) | 114 (7.6) |
(), Mortality %
Throughout 2021, 5755 patients underwent surgery for esophageal diseases (752 and 4993 for benign and malignant esophageal diseases, respectively) from institutions across Japan. Compared to 2019, there was a total decrease of 1480 cases (20.5%) observed, and a decrease of 154 cases (2.6%) compared to 2020 with a decrease of 98 cases (11.4%) in benign diseases and a decrease of 56 cases (1.1%) in malignant diseases. These significant declines which were largely influenced by the COVID-19 pandemic that began in 2020, continued even in 2021, with factors such as surgical restrictions, reduced medical visits, and postponed screenings being considered as contributing factors (Fig. 3).
Fig. 3.
Annual trend of in-patients with esophageal diseases
Concerning benign esophageal diseases (Table 34), thoracoscopic and/or laparoscopic surgeries were performed in 89.3% (42/47), 85.8% (363/423), 97.8% (44/45), and 43.5% (54/124) of patients with esophagitis (including esophageal ulcer), hiatal hernia, benign tumors, and achalasia, respectively. Conversely, 100% (93/93) of patients with spontaneous rupture of the esophagus underwent open surgery. Hospital mortality rates within 30 postoperative days were 0.9% (4/423), 1.1% (1/93) for hiatal hernia and spontaneous rupture of the esophagus, respectively.
Table 34.
Benign esophageal diseases
| Operation ( +) | T/L*3 | |||||||
|---|---|---|---|---|---|---|---|---|
| Cases | Hospital mortality | Cases | Hospital mortality | |||||
| ~ 30 days | 31–90 days | Total (including after 91days mortality) | ~ 30days | 31–90days | Total (including after 91days mortality) | |||
| 1. Achalasia | 124 | 0 | 0 | 0 | 54 | 0 | 0 | 0 |
| 2. Benign tumor | 45 | 0 | 0 | 0 | 44 | 0 | 0 | 0 |
| 3. Diverticulum | 25 | 0 | 0 | 0 | 5 | 0 | 0 | 0 |
| 4. Hiatal hernia | 423 | 4 (0.9) | 1 (0.2) | 5 (1.2) | 363 | 2 (0.6) | 1 (0.3) | 3 (0.8) |
| 5. Spontaneous rupture of the esophagus | 93 | 1 (1.1) | 0 | 1 (1.1) | 0 | 0 | 0 | 0 |
| 6. Esophago-tracheal fistula | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 7. Esophagitis, esophageal ulcer | 47 | 0 | 0 | 0 | 42 | 0 | 0 | 0 |
| Total | 762 | 5 (0.7) | 1 (0.1) | 6 (0.8) | 508 | 2 (0.4) | 1 (0.2) | 3 (0.6) |
(), Mortality %
T/L thoracoscopic and/or laparoscopic
The most common tumor location for malignant esophageal diseases was the thoracic esophagus (Table 35). Among the cases with esophageal malignancies, esophagectomy for superficial and advanced cancers was performed in 1847 (40.0%) and 3146 (60.0%), respectively. Hospital mortality rates within 30 days after esophagectomy were 0.5% and 0.8% for patients with superficial and advanced cancer, respectively.
Table 35.
Malignant Esophageal disease
| Operation ( +) | Thoracoscopic and/or laparscopic procedure | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Cases | Hospital mortality | Cases | Conversion to thoracotomy | Hospital mortality | |||||
| ~ 30days | 31–90days | Total (including after 91days mortality) | ~ 30days | 31–90days | Total (including after 91days mortality) | ||||
| Location | |||||||||
| (1) Cervical esophagus | 118 | 2 (1.7) | 0 | 2 (1.7) | 51 | 1 (2.0) | 1 (2.0) | 0 | 1 (2.0) |
| (2) Thoracic esophagus | 4181 | 27 (0.6) | 18 (0.4) | 45 (1.1) | 3788 | 19 (0.5) | 23 (0.6) | 15 (0.4) | 38 (1.0) |
| (3) Abdominal esophagus | 436 | 4 (0.9) | 2 (0.5) | 6 (1.4) | 361 | 2 (0.6) | 3 (0.8) | 2 (0.6) | 5 (1.4) |
| Total | 4735 | 33 (0.7) | 20 (0.4) | 53 (1.1) | 4200 | 22 (0.5) | 27 (0.6) | 17 (0.4) | 44 (1.0) |
| Tumor depth | |||||||||
| (A) Superficial cancer(T1) | |||||||||
| (1) Transhiatal esophagectomy | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (2) Mediastinoscopic esophagectomy and reconstruction | 103 | 0 | 1 (1.0) | 1 (1.0) | 103 | 0 | 0 | 1 | 1 (1.0) |
| (3) Transthoracic (rt.) esophagectomy and reconstruction | 1124 | 6 (0.5) | 5 (0.4) | 11 (1.0) | 1043 | 4 (0.4) | 6 (0.6) | 5 (0.5) | 11 (1.1) |
| (4) Transthoracic (lt.) esophagectomy and reconstruction | 31 | 0 | 0 | 0 | 26 | 0 | 0 | 0 | 0 |
| (5) Cervical esophageal resection and reconstruction | 25 | 2 (8.0) | 0 | 2 (8.0) | 0 | 0 | 0 | 0 | 0 |
| (6) Robot-assisted esophagectomy and reconstruction | 424 | 1 (0.2) | 0 | 1 (0.2) | 423 | 0 | 1 (0.2) | 0 | 1 (0.2) |
| (7) Others | 17 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (8) Esophagectomy without reconstruction | 119 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| subtotal | 1847 | 9 (0.5) | 6 (0.3) | 15 (0.8) | 1595 | 4 (0.3) | 7 (0.4) | 6 (0.4) | 13 (0.8) |
| (B)Advanced cancer(T2-T4) | |||||||||
| (1) Transhiatal esophagectomy | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (2) Mediastinoscopic esophagectomy and reconstruction | 129 | 0 | 1 (0.8) | 1 (0.8) | 129 | 0 | 0 | 1 (0.8) | 1 (0.8) |
| (3) Transthoracic (rt.) esophagectomy and reconstruction | 2099 | 17 (0.8) | 10 (0.5) | 27 (1.3) | 1791 | 18 (1.0) | 14 (0.8) | 7 (0.4) | 21 (1.2) |
| (4) Transthoracic (lt.) esophagectomy and reconstruction | 58 | 1 (1.7) | 0 | 1 (1.7) | 33 | 0 | 0 | 0 | 0 |
| (5) Cervical esophageal resection and reconstruction | 52 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (6) Robot-assisted esophagectomy and reconstruction | 644 | 6 (0.9) | 3 (0.5) | 9 (1.4) | 643 | 0 | 6 (0.9) | 3 (0.5) | 3 (0.5) |
| (7) Others | 18 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (8) Esophagectomy without reconstruction | 139 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Subtotal | 3146 | 24 (0.8) | 14 (0.4) | 38 (1.2) | 2596 | 18 (0.7) | 20 (0.8) | 11 (0.4) | 25 (1.0) |
| Total | 4993 | 33 (0.7) | 20 (0.4) | 53 (1.1) | 4191 | 22 (0.5) | 27 (0.6) | 17 (0.4) | 38 (0.9) |
| Cases | Overall morbidity | Morbidity ≥ CD III | Surgical complications | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Surgical site infection | Anastomotic leakage | Recurrent nerve palsy | Wound dehiscence | ||||||
| Superficial incision | Deep incision | Organ space | |||||||
| Location | |||||||||
| (1) Cervical esophagus | 118 | 61 (51.7) | 29 (24.6) | 10 (8.5) | 5 (4.2) | 11 (9.3) | 15 (12.7) | 17 (14.4) | 3 (2.5) |
| (2) Thoracic esophagus | 4181 | 2340 (56.0) | 968 (23.2) | 272 (6.5) | 143 (3.4) | 316 (7.6) | 532 (12.7) | 594 (14.2) | 45 (1.1) |
| (3) Abdominal esophagus | 436 | 215 (49.3) | 96 (22.0) | 24 (5.5) | 13 (3.0) | 41 (9.4) | 57 (13.1) | 45 (10.3) | 3 (0.7) |
| Total | 4735 | 2616 (55.2) | 1093 (23.1) | 306 (6.5) | 161 (3.4) | 368 (7.8) | 604 (12.8) | 656 (13.9) | 51 (1.1) |
| Tumor depth | |||||||||
| (A)Superficial cancer(T1) | |||||||||
| (1) Transhiatal esophagectomy | 4 | 1 (25.0) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (2) Mediastinoscopic esophagectomy and reconstruction | 103 | 64 (62.1) | 31 (30.1) | 7 (6.8) | 3 (2.9) | 13 (12.6) | 23 (22.3) | 28 (27.2) | 0 |
| (3) Transthoracic (rt.) esophagectomy and reconstruction | 1124 | 619 (55.1) | 217 (19.3) | 63 (5.6) | 34 (3.0) | 80 (7.1) | 161 (14.3) | 153 (13.6) | 10 (0.9) |
| (4) Transthoracic (lt.) esophagectomy and reconstruction | 31 | 12 (38.7) | 7 (22.6) | 4 (12.9) | 1 (3.2) | 1 (3.2) | 2 (6.5) | 3 (9.7) | 0 |
| (5) Cervical esophageal resection and reconstruction | 25 | 12 (48.0) | 7 (28.0) | 3 (12.0) | 0 | 1 (4.0) | 1 (4.0) | 4 (16.0) | 0 |
| (6) Robot-assisted esophagectomy and reconstruction | 424 | 200 (47.2) | 85 (20.0) | 20 (4.7) | 11 (2.6) | 27 (6.4) | 53 (12.5) | 53 (12.5) | 2 (0.5) |
| (7) Others | 17 | 4 (23.5) | 2 (11.8) | 1 (5.9) | 1 (5.9) | 3 (17.6) | 4 (23.5) | 4 (23.5) | 0 |
| (8) Esophagectomy without reconstruction | 119 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Subtotal | 1847 | 912 (49.4) | 349 (18.9) | 98 (5.3) | 50 (2.7) | 125 (6.8) | 244 (13.2) | 245 (13.3) | 12 (0.6) |
| (B) Advanced cancer (T2–T4) | |||||||||
| (1) Transhiatal esophagectomy | 7 | 4 (57.1) | 1 (14.3) | 1 (14.3) | 0 | 0 | 0 | 0 | 0 |
| (2) Mediastinoscopic esophagectomy and reconstruction | 129 | 76 (58.9) | 28 (21.7) | 14 (10.9) | 2 (1.6) | 4 (3.1) | 15 (11.6) | 26 (20.2) | 0 |
| (3) Transthoracic (rt.) esophagectomy and reconstruction | 2099 | 1213 (57.8) | 529 (25.2) | 144 (6.9) | 84 (4.0) | 173 (8.2) | 263 (12.5) | 271 (12.9) | 35 (1.7) |
| (4) Transthoracic (lt.) esophagectomy and reconstruction | 58 | 24 (41.4) | 7 (12.1) | 2 (3.4) | 2 (3.4) | 4 (6.9) | 3 (5.2) | 4 (6.9) | 0 |
| (5) Cervical esophageal resection and reconstruction | 52 | 33 (63.5) | 13 (25.0) | 5 (9.6) | 4 (7.7) | 5 (9.6) | 8 (15.4) | 12 (23.1) | 2 (3.8) |
| (6) Robot-assisted esophagectomy and reconstruction | 644 | 345 (53.6) | 160 (24.8) | 41 (6.4) | 19 (3.0) | 53 (8.2) | 66 (10.2) | 102 (15.8) | 2 (0.3) |
| (7) Others | 18 | 9 (50.0) | 6 (33.3) | 1 (5.6) | 0 | 4 (22.2) | 5 (27.8) | 0 | 0 |
| (8) Esophagectomy without reconstruction | 139 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| subtotal | 3146 | 1704 (54.2) | 744 (23.6) | 208 (6.6) | 111 (3.5) | 243 (7.7) | 360 (11.4) | 415 (13.2) | 39 (1.2) |
| Total | 4993 | 2616 (52.4) | 1093 (21.9) | 306 (6.1) | 161 (3.2) | 368 (7.4) | 604 (12.1) | 660 (13.2) | 51 (1.0) |
| Cases | Nonsurgical complications | Readmission within 30d | Reoperation within 30d | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pneumonia | Unplanned intubation | Prolonged ventilation > 48 h | Pulmonary embolism | Atelectasis | Renal failure | CNS events | Cardiac events | Septic shock | ||||
| Location | ||||||||||||
| (1) Cervical esophagus | 118 | 14 (11.9) | 7 (5.9) | 13 (11.0) | 1 (0.8) | 3 (2.5) | 1 (0.8) | 2 (1.7) | 0 | 1 (0.8) | 15 (12.7) | |
| (2) Thoracic esophagus | 4181 | 670 (16.0) | 162 (3.9) | 166 (4.0) | 39 (0.9) | 187 (4.5) | 16 (0.4) | 16 (0.4) | 18 (0.4) | 29 (0.7) | 104 (2.5) | 246 (5.9) |
| (3) Abdominal esophagus | 436 | 50 (11.5) | 10 (2.3) | 18 (4.1) | 6 (1.4) | 27 (6.2) | 3 (0.7) | 2 (0.5) | 1 (0.2) | 4 (0.9) | 5 (1.1) | 25 (5.7) |
| Total | 4735 | 734 (15.5) | 179 (3.8) | 197 (4.2) | 46 (1.0) | 217 (4.6) | 19 (0.4) | 19 (0.4) | 21 (0.4) | 33 (0.7) | 110 (2.3) | 286 (6.0) |
| Tumor depth | ||||||||||||
| (A) Superficial cancer (T1) | ||||||||||||
| (1) Transhiatal esophagectomy | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (2) Mediastinoscopic esophagectomy and reconstruction | 103 | 13 (12.6) | 3 (2.9) | 4 (3.9) | 1 (1.0) | 4 (3.9) | 0 | 0 | 2 (1.9) | 1 (1.0) | 3 (2.9) | 5 (4.9) |
| (3) Transthoracic (rt.) esophagectomy and reconstruction | 1124 | 163 (14.5) | 42 (3.7) | 37 (3.3) | 5 (0.4) | 51 (4.5) | 2 (0.2) | 7 (0.6) | 4 (0.4) | 8 (0.7) | 23 (2.0) | 68 (6.0) |
| (4) Transthoracic (lt.) esophagectomy and reconstruction | 31 | 4 (12.9) | 1 (3.2) | 1 (3.2) | 0 | 3 (9.7) | 1 (3.2) | 0 | 0 | 0 | 1 (3.2) | 2 (6.5) |
| (5) Cervical esophageal resection and reconstruction | 25 | 5 (20.0) | 2 (8.0) | 2 (8.0) | 0 | 1 (4.0) | 0 | 0 | 0 | 1 (4.0) | 0 | 3 (12.0) |
| (6) Robot-assisted esophagectomy and reconstruction | 424 | 57 (13.4) | 10 (2.4) | 12 (2.8) | 6 (1.4) | 13 (3.1) | 0 | 1 (0.2) | 1 (0.2) | 1 (0.2) | 11 (2.6) | 31 (7.3) |
| (7) Others | 17 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 (5.9) | 2 (11.8) |
| (8) Esophagectomy without reconstruction | 119 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| subtotal | 1847 | 242 (13.1) | 58 (3.1) | 56 (3.0) | 12 (0.6) | 72 (3.9) | 3 (0.2) | 8 (0.4) | 7 (0.4) | 11 (0.6) | 39 (2.1) | 111 (6.0) |
| (B)Advanced cancer (T2–T4) | ||||||||||||
| (1) Transhiatal esophagectomy | 7 | 2 (28.6) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| (2) Mediastinoscopic esophagectomy and reconstruction | 129 | 25 (19.4) | 2 (1.6) | 3 (2.3) | 1 (0.8) | 8 (6.2) | 0 | 0 | 1 (0.8) | 0 | 4 (3.1) | 3 (2.3) |
| (3) Transthoracic (rt.) esophagectomy and reconstruction | 2099 | 354 (16.9) | 91 (4.3) | 106 (5.1) | 23 (1.1) | 101 (4.8) | 11 (0.5) | 9 (0.4) | 10 (0.5) | 14 (0.7) | 50 (2.4) | 130 (6.2) |
| (4) Transthoracic (lt.) esophagectomy and reconstruction | 58 | 8 (13.8) | 3 (5.2) | 3 (5.2) | 0 | 2 (3.4) | 1 (1.7) | 0 | 0 | 1 (1.7) | 1 (1.7) | 2 (3.4) |
| (5) Cervical esophageal resection and reconstruction | 52 | 5 (9.6) | 4 (7.7) | 5 (9.6) | 1 (1.9) | 0 | 0 | 0 | 0 | 0 | 0 | 5 (9.6) |
| (6) Robot-assisted esophagectomy and reconstruction | 644 | 96 (14.9) | 21 (3.3) | 24 (3.7) | 9 (1.4) | 33 (5.1) | 4 (0.6) | 2 (0.3) | 1 (0.2) | 7 (1.1) | 17 (2.6) | 35 (5.4) |
| (7) Others | 18 | 2 (11.1) | 0 | 0 | 0 | 1 (5.6) | 0 | 0 | 2 (11.1) | 0 | 0 | 0 |
| (8) Esophagectomy without reconstruction | 139 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Subtotal | 3146 | 492 (15.6) | 121 (3.8) | 141 (4.5) | 34 (1.1) | 145 (4.6) | 16 (0.5) | 11(0.3) | 22 (0.7) | 72 (2.3) | 175 (5.6) | |
| Total | 4993 | 734 (14.7) | 179 (3.6) | 197 (3.9) | 46 (0.9) | 217 (4.3) | 19 (0.4) | 19 (0.4) | 21 (0.4) | 33 (0.7) | 111 (2.2) | 286 (5.7) |
Among esophagectomy procedures, transthoracic esophagectomy via right thoracotomy or right thoracoscopy was most commonly adopted for patients with superficial (1124/1847, 60.9%) and advanced cancer (2099/3146, 66.7%) (Table 35). Transhiatal esophagectomy, which is commonly performed in Western countries, was adopted in only 4 (0.2%) and 7 (0.2%) patients with superficial and advanced cancer who underwent esophagectomy in Japan, respectively. Minimally invasive esophagectomy (MIE) including thoracoscopic and/or laparoscopic esophagectomy, robot-assisted esophagectomy and mediastinoscopic esophagectomy was utilized in 1595 (86.3%) and 2596 (82.5%) patients with superficial and advanced cancer, respectively. Incidence of MIE for superficial or advanced cancer have been increasing, whereas that of open surgery, especially for advanced cancer, has been decreasing annually (Fig. 4). Although mediastinoscopic esophagectomy was performed only for 103 (5.6%) and 129 (4.1%) patients with superficial and advanced esophageal cancer, respectively. Robot-assisted esophagectomy has been remarkably increased since 2018 when the insurance approval was obtained in Japan, and performed for 424 (23.0%) and 624 (20.5%) patients with superficial and advanced esophageal cancer, respectively in 2021. Patients who underwent robot-assisted surgery are increasing for both superficial and advancer esophageal cancers (18.8% and 34.4% increases compared to that in 2020, respectively). Hospital mortality rates within 30 days after MIE were 0.4% and 0.8% for patients with superficial and advanced cancer, respectively (Table 35).
Fig. 4.
Annual trend of esophagectomy
Detailed data collection regarding postoperative surgical and non-surgical complications was initiated in 2018. Overall, 1093 (21.9%) of 4993 patients developed grade III or higher complications based on the Clavien–Dindo classification in 2021 (Table 35). The incidence of grade III or higher complications was relatively higher in cervical esophageal cancer compared to thoracic or abdominal esophageal cancer. Among surgical complications in patients with advanced esophageal cancer, anastomotic leakage and recurrent nerve palsy occurred in 12.5% and 12.9% of the patients who underwent right transthoracic esophagectomy, in 10.2% and 15.8% of those who underwent robot-assisted esophagectomy, and in 11.6% and 20.2% of those who underwent mediastinoscopic esophagectomy, respectively. Among non-surgical postoperative complications, pneumonia occurred in 14.7% of the patients, 3.6% of whom underwent unplanned intubation. Postoperative pulmonary embolism occurred in 0.9% of the patients. These complication rates, including the others, were similar to those in 2020.
We aim to continue our efforts in collecting comprehensive survey data through more active collaboration with the Japan Esophageal Society and other related institutions, with caution due to the impact of COVID-19 pandemic.
Acknowledgements
On behalf of the Japanese Association for Thoracic Surgery, the authors thank the Heads of the Affiliate and Satellite Institutes of Thoracic Surgery for their cooperation and the Councilors of the Japan Esophageal Society. We also appreciate Mr. Hiroaki Miyata for his contribution as one of the founders of the JCVSD.
Data availability
Based on the data use policy of JATS, data access is approved through assessment by the JATS: Committee for Scientific Affairs. Those interested in using the data should contact the JATS: Committee for Scientific Affairs(survey@jpats.org) to submit a proposal. The use of the data is granted for the approved study proposals.
Declarations
Conflict of interest
Hiroyuki Yamamoto and Hiraku Kumamaru are affiliated with the Department of Healthcare Quality Assessment at the University of Tokyo. The department is a social collaboration department supported by grants from the National Clinical Database, Johnson & Johnson K.K., Nipro Corporation and Intuitive Surgical Sàrl.
Footnotes
Annual report by the Japanese Association for Thoracic Surgery: Committee for Scientific Affairs.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Naoki Yoshimura, Yukio Sato, and Hiroya Takeuchi contributed equally to this work.
References
- 1.Lotfi M, Hamblin MR, Rezaei N. COVID-19: transmission, prevention, and potential atherapeutic opportunities. Clin Chim Acta. 2020;508:254–266. doi: 10.1016/j.cca.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Minatoya K, Sato Y, Toh Y, et al. Thoracic and cardiovascular surgery in Japan during 2019—annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2023;71:595–628. doi: 10.1007/s11748-023-01945-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsumiya G, Sato Y, Takeuchi H, et al. Thoracic and cardiovascular surgery in Japan during 2020—annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2024;72:61–94. doi: 10.1007/s11748-023-01979-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sato Y, Yamamoto H, Ikeda N, et al. The impact of COVID-19 on thoracic surgical procedures in Japan: analysis of data from the national clinical database. Lung Cancer. 2022;172:127–135. doi: 10.1016/j.lungcan.2022.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amano J, Kuwano H, Yokomise H. Thoracic and cardiovascular surgery in Japan during 2011—annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2013;61:578–607. doi: 10.1007/s11748-013-0289-2. [DOI] [PubMed] [Google Scholar]
- 6.Shimizu H, Endo S, Natsugoe S, et al. Thoracic and cardiovascular surgery in Japan during 2016—annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2019;67:377–411. doi: 10.1007/s11748-019-01068-9. [DOI] [PubMed] [Google Scholar]
- 7.Kazui T, Wada H, Fujita H, Japanese Association for Thoracic Surgery Committee of Science Thoracic and cardiovascular surgery in Japan during 2003—annual report by the Japanese Association for Thoracic Surgery. Jpn J Thorac Cardiovasc Surg. 2005;53:517–536. doi: 10.1007/s11748-005-0100-0. [DOI] [PubMed] [Google Scholar]
- 8.Kazui T, Osada H, Fujita H, Japanese Association for Thoracic Surgery Committee of Science Thoracic and cardiovascular surgery in Japan during 2004—annual report by the Japanese Association for Thoracic Surgery. Jpn J Thorac Cardiovasc Surg. 2006;54:363–385. doi: 10.1007/s11748-006-0008-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Based on the data use policy of JATS, data access is approved through assessment by the JATS: Committee for Scientific Affairs. Those interested in using the data should contact the JATS: Committee for Scientific Affairs(survey@jpats.org) to submit a proposal. The use of the data is granted for the approved study proposals.