Abstract
Posterior interosseous nerve syndrome (PINs) is a rare nerve compression syndrome that affects the deep branch of the radial nerve in the supinator muscle region. In this article, we aimed to report a case of a 58-year-old male who had clinical symptoms, electromyographic, ultrasound, and MRI features suggestive of PINs due to compressing the arcade of Frohse. He subsequently underwent surgical correlation at our hospital, and the clinical symptoms were improved significantly.
Keywords: Posterior interosseous nerve syndrome, Nerve compression syndrome, PINs, Arcade of Frohse
Introduction
Posterior interosseous nerve (PINs) syndrome is characterized by the entrapment deep branch of the radial nerve in the supinator muscle region. The clinical findings of PINs include paralysis of finger extension and limitation of extension of the wrist [1]. The cause of the compression may be due to structures such as lipoma, lymph node, synovial cyst, blood vessel, or even trauma or postsurgery [2]. The arcade of Frohse is the most common location of PINs [1].
PINs is an uncommon neuropathy that is characterized by silently progressing symptoms, difficult clinical diagnosis, and can be easily confused with other radial nerve damages. Electromyography has the advantage of localizing the injury and assessing the severity but cannot determine the morphology and the primary cause of the compression [3]. Other imaging studies, including ultrasound and magnetic resonance imaging (MRI), are superior in accurately assessing the location of the main cause of PINs and evaluating surrounding abnormalities such as muscle and blood vessel damage [4]. Our case report points out the typical clinical, electromyographic, ultrasound, and MRI features of PINs, which was confirmed by surgery.
Case presentation
A 58-year-old male had painful episodes in the upper one-third, weakness in his left arm without finger numbness for a year. He was treated with painkillers and acupuncture for a long time, but the symptoms were not improved. Two months recently, the worsening symptoms turned into the inability to stretch his fingers, and difficulty holding which severely affects his daily activities. Physical examination revealed painful abnormalities in the lateral upper one-third of the left forearm, weakness of the wrist and digital extensors, flexion movement in normal range, no numbness in the hand, and the radial and ulnar pulses were clearly detected. The patient was preliminarily diagnosed with left posterior interosseous nerve compression syndrome. Therefore, electromyography and ultrasound of the forearm were prescribed.
Electromyography showed a reduction in the response amplitude of the left radial nerve measured on the index finger extensor muscle, conduction block in the upper 2/3 of the left forearm, and other nerve conductions on the left side were normal. In addition, there were many spontaneous potentials on the extensor muscles of the left fingers, but no exercise contraction potentials were recorded.
On ultrasound (Fig. 1), the radial nerve showed normal size and structure. The posterior interosseous nerve (PIN) increased in size (1.5 mm) just before the arcade of Frohse (Fig. 1b), then flattened at the level of the arcade of Frohse (Fig. 1c), the nerve structure was still normal and continuous, no surrounding infiltrates or masses that compressed the nerve. Adjacent muscles were not edematous.
Fig. 1.
Ultrasound images revealed the transverse axis of PIN at the inlet of the Frohse arch of the supinator muscle (arrow) on the right hand (A) 0,6 mm diameter and on the left hand (B) 1,5 mm diameter. (C) PIN is flattened at the outlet of the supinator muscle (arrow). (D) the longitudinal axis of a PIN segment at the inlet of the Frohse arch of the supinator muscle showed a slight increase in size and slight hypoechogenicity.
The MRI of the left arm showed that the deep supinator muscle bundle, which is dominated by PIN, had atrophy and increased signal intensity on the T2-weighted fatsat sequence(T2W) (Fig. 2), and the superficial supinator muscle bundle showed no abnormalities. On the T1-weighted fatsat sequence(T1W) and T2W sequences, PIN was flattened at the level of the Frohse arcade and increased in size right before entering into this arch, which suggests an edematous lesion (Fig. 3).
Fig. 2.
MRI of axial T2W fatsat sequence through the supinator muscle showed the abnormalities of the deep bundle of the supinator muscle with atrophy and increased signal (arrow).
Fig. 3.
The axial T2W fatsat sequence of the left arm MRI at the level of the arcade of Frohse. (A) PIN increased in size just before entering the arcade of Frohse (arrow). (B) Image of PIN flattened (arrow) right at the position passing through the arcade of Frohse (arrowhead).
The patient was diagnosed with nerve and muscle damage in posterior interosseous nerve syndrome regarding these aforementioned clinical features, ultrasound, electromyography, and MRI images.
He underwent surgery for decompressing PIN from the arcade of Frohse targeting to reduce pain and weakness symptoms. During surgery, the PIN significantly increased in size at the level of the arcade of Frohse (Fig. 4).
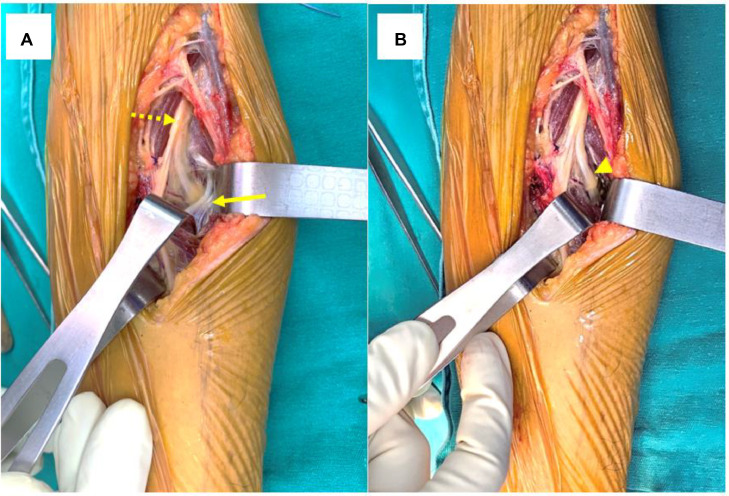
Fig. 4.
The intraoperative images. (A) Exposing the radial nerve (dashed arrow) and the PIN passing through the arch of Frohse (arrow) into the supinator muscle. (B) PIN image after resection of the arcade of Frohse (arrowhead).
One month after surgery, the patient no longer had pain in the upper 1/3 of the forearm, and the muscle strength of the finger extensors had partially improved.
Combining clinical symptoms, ultrasound images, MRI, and functional response after surgery, the definitive diagnosis of this case was PINs due to entrapment of the arcade of Frohse.
Discussion
The posterior interosseous nerve (PIN) is the deep motor branch of the radial nerve. After passing anterior to the lateral epicondyle of the humerus, the radial nerve divides into a superficial sensory branch and the PIN at the level of the proximal radioulnar joint. After passing through the arcade of Frohse (also known as the supinator arch), the PIN runs between the superficial and deep parts of the supinator muscle. This structure subsequently branches and innervates the extensor compartment muscles of the forearm [5,6].
Nerve entrapment syndrome is a neurological disease due to structural abnormalities caused by external compression, displacement, or traction of the nerve as a result of a mass, cyst, fibrous band, or deformation of the bone. It may also be caused by intrinsic abnormalities of the nerve itself, such as neurogenic tumors [1,7]. PINs is a rare condition compared to other compressive neuropathies such as carpal tunnel syndrome and cubital tunnel syndrome, with an annual incidence of PINs of 0,003%, and it accounts for less than 0,7% of all upper extremity peripheral nerve syndromes [8].
Five common sites of PIN compression have been identified. The most proximal site is at the level of the fibrous band of the radial head, next to the proximal margin of the supinator muscle. The second site, at the level of the radial neck, is where the branch of the radial recurrent artery (the leash of Henry) crosses. The next site is the tendinous edge of the extensor carpi radialis brevis. The fourth site is at the level of Frohse's arcade. The last and most distal point is the distal edge of the supinator muscle [2,9]. Frohse's arcade is the most common site of PIN compression, it is the proximal margin of the superficial part of the supinator muscle, composed of fascia, tendons, or membranes, the tendinous type is considered a significant risk factor for PINs, with an occurrence rate ranging from 64% to 87% in different studies [9]. Tendinous thickening is caused by overuseand repetition of pronation and supination [10].
Regarding clinical symptoms, PINs lead to paralysis of muscles innervated by this entity. Patients may present radial deviation of the wrist during extension due to impaired function of the extensor carpi ulnaris and extensor carpi radialis brevis, reducing the ability to extend the fingers at the metacarpophalangeal joints (also called the “finger drop” sign, distinguishing it from the “dropping hand” sign in radial nerve palsy), decreased ability to extend and abduct the thumb [2]. Our patient had symptoms consistent with PIN compression.
Ultrasound is the first-line diagnostic tool in the assessment of PIN, helping to evaluate the morphology, structure, continuity of the nerve, and adjacent structures over the entire length of the PIN from its origin to its division into branches in the supinator muscle [11,12]. Many studies revealed nerve deformity due to compression or increase in size due to nerve edema in the group of patients with PIN compression of the arcade of Frohse. According to research by Youdong Kim [7] in 2017 of 10 patients with PINs, including 4 patients with PIN lesions due to compression of Frohse's arcade, sonography showed that the PIN was compressed, hypoechoic, and loss of the normal structure of the nerve bundle, the average anteroposterior diameter of the PIN is 179 ± 043 mm in the affected side and 102 ± 022 mm in the contralateral normal side, the difference in size is statistically significant (P = 0.003).In another study by Djurdjevic et al [13], the anteroposterior diameter of the PIN nerve measured near the arcade of Frohse in the pathological group was 2mm (16-33 mm). In the control group, it was 11 mm (01-15 mm), the difference is statistically significant (P < 0.05). In our cases, the diameter of PIN just before Frohse's arcade in the affected forearm is 1.5 mm, and the contralateral side is 0.6 mm.
Another useful tool besides ultrasonography for diagnosing neuropathy is electromyography, which helps localize the lesion and rule out brachial plexus injury [3]. The manifestation of PINs on electromyography is a reduced or blockage of motor nerve conduction at the injured site, a decrease in the response amplitude of the extensor digitorum muscle, and in addition, spontaneous potentials may appear in the extensor digitorum muscle; sensory conduction is still preserved [3,14]. In cases of PINs, anatomical variations that cause nerve compression are often difficult to visualize by MRI, however, MRI is sensitive in detecting muscle edema, muscle atrophy, and fatty infiltration [4]. In addition, MRI can help to identify other causes of compression including tumors, lymph nodes, synovitis, fractures... [4,15]. Study by B. Ferdinand [16] of 25 patients with PINs on MRI showed that 52% of patients had degeneration and atrophy of the supinator or extensor muscles in the forearm, 28% of patients had extrinsic compression lesions such as Henry's leash, schwannoma, synovial cyst..., 4 patients had normal MRI findings.
Non-operative management is usually used as the initial treatment of PINs, including splints, NSAIDs, and physical therapy [15,17]. Surgical treatment is indicated for cases refractory to conservative treatment for at least 3 months. Decompression surgery depends on the cause of the syndrome (such as cutting off Frohse's arcade, or ligation and cutting of Henry's leash...) [18]. Our patient had pain that lasted for 1 year and had complications of supination muscle injury on MRI. Hence, he was indicated for surgery to release Frohse's arcade.
Conclusion
PINs is a rare nerve compression syndrome of the deep branch of the radial nerve in the supinator muscle region, with the most common cause due to the compression of the arcade of Frohse. Diagnosis of PINs requires a combination of clinical, electromyographic, and imaging features. Ultrasonography is the first tool to help evaluate the structure, continuity, and morphology of PIN, especially at the level of Frohse's arcade. MRI helps evaluate muscle injury and figure out causes of compression other than Frohse's arcade. Surgical treatment is necessary for patients with compressive entity causes or patients who do not respond to conservative treatment.
Author's contributions
Ho XT and Nguyen MD: Case file retrieval and case summary preparation. Ho XT and Nguyen MD: preparation of manuscript and editing. All authors read and approved the final manuscript.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Our institution does not require ethical approval for reporting individual cases or case series. Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
Consent for publication
Not applicable.
Patient consent
Informed consent for patient information to be published in this article was obtained.
Footnotes
Acknowledgments: Nil.
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Miller TT, Reinus WR. Nerve entrapment syndromes of the elbow, forearm, and wrist. AJR Am J Roentgenol. 2010;195(3):585–594. doi: 10.2214/AJR.10.4817. [DOI] [PubMed] [Google Scholar]
- 2.Portilla Molina AE, Bour C, Oberlin C, Nzeusseu A, Vanwijck R. The posterior interosseous nerve and the radial tunnel syndrome: an anatomical study. Int Orthop. 1998;22(2):102–106. doi: 10.1007/s002640050218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bevelaqua AC, Hayter CL, Feinberg JH, Rodeo SA. Posterior interosseous neuropathy: electrodiagnostic evaluation. HSS Journal. 2012;8(2):184. doi: 10.1007/s11420-011-9238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spinner M. The arcade of Frohse and its relationship to posterior interosseous nerve paralysis. J Bone Joint Surg Br. 1968;50(4):809–812. [PubMed] [Google Scholar]
- 5.Martinoli C, Bianchi S, Pugliese F, Bacigalupo L, Gauglio C, Valle M, Derchi LE. Sonography of entrapment neuropathies in the upper limb (wrist excluded) J Clin Ultrasound. 2004;32(9):438–450. doi: 10.1002/jcu.20067. [DOI] [PubMed] [Google Scholar]
- 6.PIN Compression Syndrome - Hand - Orthobullets. Accessed December 8, 2023. https://www.orthobullets.com/hand/6023/pin-compression-syndrome.
- 7.Kim Y, Ha DH, Lee SM. Ultrasonographic findings of posterior interosseous nerve syndrome. Ultrasonography. 2017;36(4):363–369. doi: 10.14366/usg.17007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hazani R, Engineer NJ, Mowlavi A, Neumeister M, Lee WPA, Wilhelmi BJ. Anatomic landmarks for the radial tunnel. Eplasty. 2008;8:e37. [PMC free article] [PubMed] [Google Scholar]
- 9.Konjengbam M, Elangbam J. Radial nerve in the radial tunnel: anatomic sites of entrapment neuropathy. Clin Anat. 2004;17(1):21–25. doi: 10.1002/ca.10194. [DOI] [PubMed] [Google Scholar]
- 10.Clavert P, Lutz JC, Adam P, Wolfram-Gabel R, Liverneaux P, Kahn JL. Frohse's arcade is not the exclusive compression site of the radial nerve in its tunnel. Orthop Traumatol Surg Res. 2009;95(2):114–118. doi: 10.1016/j.otsr.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Chien AJ, Jamadar DA, Jacobson JA, Hayes CW, Louis DS. Sonography and MR imaging of posterior interosseous nerve syndrome with surgical correlation. Am J Roentgenol. 2003;181(1):219–221. doi: 10.2214/ajr.181.1.1810219. [DOI] [PubMed] [Google Scholar]
- 12.Silvestri E, Martinoli C, Derchi LE, Bertolotto M, Chiaramondia M, Rosenberg I. Echotexture of peripheral nerves: correlation between US and histologic findings and criteria to differentiate tendons. Radiology. 1995;197(1):291–296. doi: 10.1148/radiology.197.1.7568840. [DOI] [PubMed] [Google Scholar]
- 13.Djurdjevic T, Loizides A, Löscher W, Gruber H, Plaikner M, Peer S. High resolution ultrasound in posterior interosseous nerve syndrome. Muscle Nerve. 2014;49(1):35–39. doi: 10.1002/mus.23867. [DOI] [PubMed] [Google Scholar]
- 14.Park D, Kim DY, Eom YS, Lee SE, SB Chae. Posterior interosseous nerve syndrome caused by a ganglion cyst and its surgical release with intraoperative neurophysiological monitoring: a case report. Medicine (Baltimore) 2021;100(8):e24702. doi: 10.1097/MD.0000000000024702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lubahn JD, Cermak MB. Uncommon nerve compression syndromes of the upper extremity. J Am Acad Orthop Surg. 1998;6(6):378–386. doi: 10.5435/00124635-199811000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Ferdinand BD, Rosenberg ZS, Schweitzer ME, Stuchin SA, Jazrawi LM, Lenzo SR, Meislin RJ, Kiprovski K. MR imaging features of radial tunnel syndrome: initial experience. Radiology. 2006;240(1):161–168. doi: 10.1148/radiol.2401050028. [DOI] [PubMed] [Google Scholar]
- 17.Wheeler R, DeCastro A. Posterior interosseous nerve syndrome. StatPearls. StatPearls Publishing; Treasure Island (FL);2023. Accessed December 8, 2023 http://www.ncbi.nlm.nih.gov/books/NBK541046/. [PubMed]
- 18.Kim DH, Murovic JA, Kim YY, Kline DG. Surgical treatment and outcomes in 45 cases of posterior interosseous nerve entrapments and injuries. J Neurosurg. 2006;104(5):766–777. doi: 10.3171/jns.2006.104.5.766. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.