Abstract
Purpose
We report a patient with pseudoxanthoma elasticum (PXE) with angioid streaks near a scleral buckle site.
Observations
A 46-year-old male with PXE presented for evaluation of blurry vision and was found to have classic PXE findings in both eyes and angioid streaks adjacent to the site of a scleral buckle in his left eye. He underwent multimodal imaging, genetic testing, and intravitreal aflibercept in the right eye.
Conclusions and importance
Bruch's membrane is known to be fragile in PXE, and patients are often counseled about the heightened risk of playing contact sports. This report raises the question of whether tension from a scleral buckle in the setting of a calcified and brittle BM may increase the likelihood of angioid streaks near the buckle site. In the setting of retinal detachment, it may be worthwhile to carefully weigh the pros and cons of vitrectomy versus buckle for PXE patients.
Keywords: Angioid streaks, Bruch's membrane, Pseudoxanthoma elasticum, Scleral buckle
1. Introduction
Pseudoxanthoma elasticum (PXE) is an inherited, multisystem disease that is usually caused by autosomal recessive mutations in the ATP binding cassette subfamily C member 6 (ABCC6) gene.1 The hallmark of the disease is progressive mineralization and fragmentation of elastic fibers in the skin, eyes, and cardiovascular systems. The incidence is 1:1,600,000 individuals.2 Ocular manifestations most commonly include angioid streaks in the retina, which involves ectopic calcification of elastic fiber-rich tissues.3 In the setting of a calcified, inelastic Bruch's membrane (BM), it is possible that the mechanical force from placement of a scleral buckle on these eyes may promote the development of angioid streaks in BM.
2. Case report
A 46-year-old male with a history of PXE diagnosed in childhood presented for evaluation of blurry vision in both eyes. He denied prior dermatologic biopsy, cardiac workup, and intravitreal injections. He endorsed seeing constant flashes and floaters in both eyes but denied any pain or discomfort. He had a history of a rhegmatogenous retinal detachment in the left eye with scleral buckle surgery 28 years previously.
Upon evaluation, his visual acuity was 20/400 in the right eye and 20/200 in the left eye with normal intraocular pressures and anterior segment findings in both eyes. Refractive error was +1.375 spherical equivalents in right eye and +1.625 spherical equivalents in the left eye. Skin examination showed small yellow papules on the neck (Fig. 1). Fundus examination of the right eye revealed optic disc drusen, a large fibrovascular scar, diffuse pigment clumping, macular retinal pigment epithelium (RPE) atrophy, and angioid streaks near the optic nerve. Optical coherence tomography (OCT) of the right eye showed intraretinal fluid (Fig. 2). Left eye examination showed extensive macular RPE atrophy with pigmentary changes, optic disc drusen, comet tail lesions, fibrovascular scarring, angioid streaks radiating from the optic disc, evidence of a scleral buckle with adjacent angioid streaks, and cryotherapy scars in the periphery (Fig. 3). OCT of the left eye showed no intra-retinal fluid (Fig. 4). Intravenous fluorescein angiography of the left eye at 56 seconds demonstrated findings similar to the fundus examination, and highlighted hyperfluorescent linear signals corresponding to areas of angioid streaks with no leakage (Fig. 5).
Fig. 1.
Skin examination reveals small yellow patchy papules of the classic “plucked chicken skin” on the neck. This finding is pathognomonic for PXE.
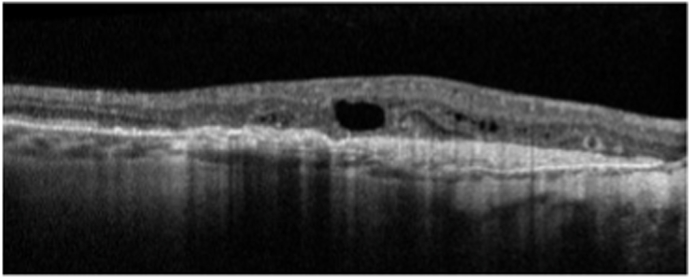
Fig. 2.
OCT of right eye showing fibrotic choroidal neovascularization with overlying intraretinal fluid.
Fig. 3.
Pseudocolor widefield fundus photography of left eye demonstrates a large fibrovascular scar overlying the macula, comet tail lesions, optic nerve head drusen, and cryotherapy scars in the periphery. Blue arrows denote angioid streaks near the ridge of a former scleral buckle placement.
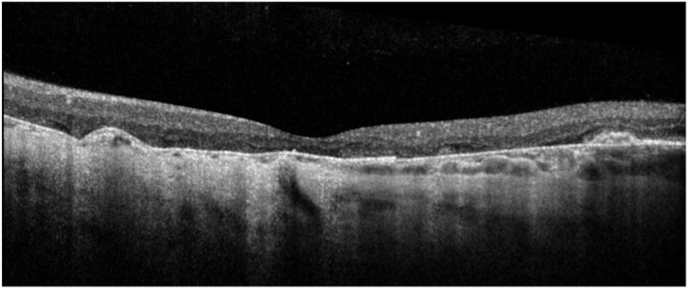
Fig. 4.
OCT of left eye showing absence of intraretinal fluid.
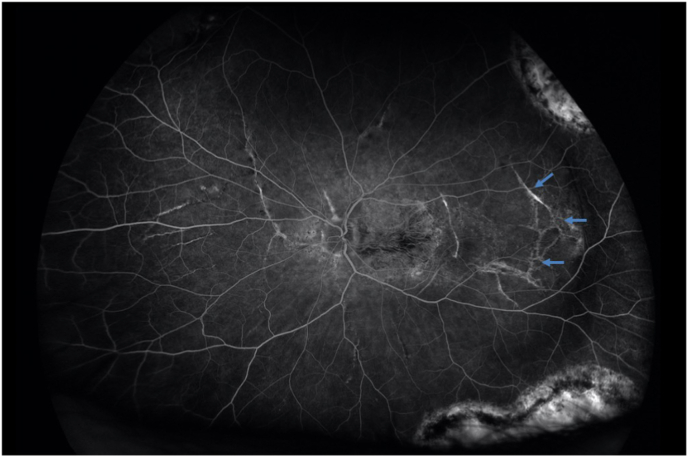
Fig. 5.
IVFA of left eye at 56 seconds. Arrows demonstrate hyperfluorescent signal correlating to angioid streaks overlying the optic nerve and tracking out from site of former scleral buckle placement.
The patient was treated with intravitreal aflibercept in his right eye for intraretinal fluid. Genetic testing at time of presentation revealed the homozygous pathogenic variants c.3490C > T p.(Arg 1164*) in ABCC6. Results were reported in standard fashion and thus likely obtained through next generation sequencing. Evaluation with cardiology and gastroenterology were recommended to rule out systemic involvement of PXE.
3. Discussion
In this report, we present a 46-year-old male with PXE and angioid streaks near the site of a previously placed scleral buckle of the left eye. Breaks in BM in PXE manifest as angioid streaks, usually around the optic disc, which are associated with choroidal neovascularization. Other hallmark ocular manifestations include retinal comet tail lesions and optic nerve head drusen.4,5 Our patient exhibited many of these classic findings. Though we suspect that the patient's the angioid streaks were caused by buckling, it is also possible that unrecognized prior trauma could have precipitated the streaks. However, it is most common for angioid streaks to develop in the posterior pole. This case raises the question of whether tension from a scleral buckle in the setting of a calcified and brittle PXE BM increases the likelihood of angioid streaks near the buckle site. This report may provide the impetus to study the outcomes of scleral buckles in patients with PXE and prompts the careful determination of the pros and cons of vitrectomy versus buckles for these patients.
Because of the poor prognosis in both eyes, it was felt that an attempt to treat the right eye with intravitreal aflibercept in the presence of intraretinal fluid might be worthwhile. In the absence of a marked change in vision, treatment was stopped after three injections. Follow-up OCT-A after injections showed minimal flow, therefore OCT findings are not included.
PXE is also associated with numerous systemic disorders, including involvement of the skin, cardiovascular system, and gastrointestinal tract.6 Although our patient exhibited classic “plucked chicken skin” on his neck, he had never undergone a dermatology evaluation. He was subsequently referred to a dermatologist as well as a cardiologist and gastroenterologist for further evaluations.
4. Conclusions
Pseudoxanthoma elasticum is a hereditary disease that causes ophthalmic findings including angioid streaks in the retina, optic disc drusen, and choroidal neovascularization. In this report, we present a case of angioid streaks near a scleral buckle site.
Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Funding
No funding or grant support
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship".
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Supported in part by an unrestricted grant from the J. Arch McNamara, Research fund of the Wills Eye Hospital and Mid Atlantic Retina.
References
- 1.Germain D.P. Pseudoxanthoma elasticum. Orphanet J Rare Dis. 2017;12(1):85. doi: 10.1186/s13023-017-0639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.D'Marco L., Lima-Martínez M., Karohl C., et al. Pseudoxanthoma elasticum: an interesting model to evaluate chronic kidney disease-like vascular damage without renal disease. Kidney Dis. 2020;6:92–97. doi: 10.1159/000505026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mandura R.A., Radi R.E. Angioid streaks in pseudoxanthoma elasticum. Cureus. 2021;13(6) doi: 10.7759/cureus.15720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gliem M., Müller P.L., Birtel J., et al. Frequency, phenotypic characteristics and progression of atrophy associated with a diseased Bruch's membrane in pseudoxanthoma elasticum. Invest Ophthalmol Vis Sci. 2016;57(7):3323–3330. doi: 10.1167/iovs.16-19388. [DOI] [PubMed] [Google Scholar]
- 5.Gliem M., De Zaeytijd J., Finger R.P., et al. An update on the ocular phenotype in patients with pseudoxanthoma elasticum. Front Genet. 2013;4:14. doi: 10.3389/fgene.2013.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lefthériotis G., Omarjee L., Le Saux O., et al. The vascular phenotype in Pseudoxanthoma elasticum and related disorders: contribution of a genetic disease to the understanding of vascular calcification. Front Genet. 2013;4:4. doi: 10.3389/fgene.2013.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]