Abstract
Purpose
To determine the differences in myopia control efficiency and corneal reshaping between three different brands of orthokeratology (OK) lenses (Lucid, Euclid, and Alpha).
Method
We retrospectively reviewed subjects who started simultaneously using different brands of OK lenses. For each participant, every 6 months in the 19 months of following, the changes in axial length (AL), horizontal and vertical maximum distances of the treatment zone (HMDTZ and VMDTZ), width of the high convex zone (WHCZ), distance of decentration, and horizontal and vertical components of the decentration vector were measured. The average values of the above data, the average value of the decentration vector (ADV), and the average value of decentration calculated algebraically (ADA) were calculated.
Results
All the three pairs (Lucid (n = 46) vs. Euclid (n = 46): groups Lucid-versus-Euclid-Lucid (LE-L) and LE-E), Lucid (n = 50) vs. Alpha (n = 50): groups LA-L and LA-A), and Euclid (n = 17) vs. Alpha (n = 17): groups EA-E and EA-A) showed good comparability. Regarding the change in AL during 19 months, none of the pairs showed significant differences (LE-L:0.27 ± 0.24 mm, LE-E:0.31 ± 0.24 mm (p = 0.68); LA-L:0.36 ± 0.26 mm, LA-A:0.36 ± 0.27 mm (p = 0.85); EA-E:0.34 ± 0.27 mm, EA-A:0.41 ± 0.28 mm (p = 0.63)). Regarding treatment zone, Lucid showed the largest HMDTZ and VMDTZ (both p < 0.05). Regarding the WHCZ, none of the pairs showed significant differences. For the ADV and ADA, Lucid had more ADV and ADA than Euclid (ADV: LE-L:0.73 ± 0.44 mm, LE-E:0.55 ± 0.45 mm, p < 0.05; ADA: LE-L:0.80 ± 0.41 mm, LE-E:0.63 ± 0.44 mm, p < 0.05), and the remaining pairs showed no significant difference. For the overall cohort with 113 eyes, the change in AL was weakly correlated with both ADV and ADA (both p < 0.05). Regarding the ADV/ADA, all pairs showed no significant differences, indicating equal lens position stability.
Conclusion
After OK, there were no significant differences between the different pairs of the three brands in AL growth, WHCZ, or lens position stability, although Lucid had a larger treatment zone than Euclid and Alpha, and Lucid had more decentration than Euclid. A larger lens decentration were weakly related to less AL growth.
Keywords: Myopia, Orthokeratology, Corneal topography, Different brands, Comparison, Decentration
Abbreviations
- Treatment zone centre
TZC
- Horizontal maximum distance of the treatment zone
HMDTZ
- Vertical maximum distance of the treatment zone
VMDTZ
- Distance of decentration
DOD
- Width of the high convex zone
WHCZ
- Horizontal component of the decentration vector
HCD
- Vertical component of the decentration vector
VCD
- Average value of the decentration vector
ADV
- Average value of decentration calculated algebraically
ADA
1. Introduction
Myopia affects approximately 90% of teenagers and young adults in China and 28% of the global population and its incidence has shown a dramatic increase in the past 50 years [1,2]. Holden et al. predicted that without any intervention or control, approximately 50% of the global population will have myopia by 2050 [1]. Some pharmacological and optical methods have been developed to control myopia progression; among these methods, orthokeratology (OK) has proven to be effective [[3], [4], [5]].
Currently, with regards myopia control effects, a few studies have compared the different brands of OK lenses used in clinical practice [[6], [7], [8], [9], [10]], which shown that local brands in China (including joint venture brands) may be relatively ineffective in myopia control [8], and corneal refractive therapy (CRT) lenses may be relatively weak compared with vision shaping treatment (VST) lenses [10], while there may be no significant difference between other brands [[6], [7], [8], [9], [10]].
However, in previous studies, the individual differences are difficult to avoid (E.g. age, baseline axial length, pupil size every moment, daily outdoor sunlight exposure, situation of daily near-work, daily use of OK lenses, actual corneal reshaping, etc.), and the comparison of average corneal reshaping all remains undetermined. Therefore, we performed this retrospective, self-controlled study (the same patient wore two different brands of OK lenses simultaneously; for example, Lucid for the right eye and Euclid for the left eye) to determine whether there was different axial length growth and corneal reshaping among three different brands of OK lenses (Euclid vs. Lucid, Lucid vs. Alpha, and Alpha vs. Euclid) with most individual differences avoided.
2. Methods
2.1. Participants
In this retrospective self-control study, all the sujects who were prescribed OK lenses between January 2015 and January 2020 at our hospital were reviewed. When reviewing cases, the inclusion criteria were as follows: (1) the subjects had to simultaneously wear OK lenses of different brands; (2) the spherical refractive error had to be less than −5.00 D with astigmatism (with-the-rule astigmatism only) of −1.50 D or less, and the best-corrected visual acuity (BCVA) of the logMAR (logarithm of the minimum angle of resolution) had to be 0.0 or better before treatment; (3) all the subjects had to be followed up as scheduled after 6,12 and18 months of OK, and the data had to be complete; and (4) the visual acuity without frame glasses of each eye had to be better than 0.1 (logMAR) after removal of lenses at each follow-up. The exclusion criteria were as follows: (1) subjects with anisometropia (difference in spherical equivalent refractive error between the right and left eyes is more than 1.0D); (2) the included subjects should not have obvious glare, diplopia, or any other corneal complications; (3) subjects with underlying ocular diseases, such as obvious tropia, retinopathy, prematurity, history of genetic disease that might affect refractive development, or other system disorders associated with myopia; (3) decentrations larger than 1.5 mm or inadequate lens fitting were found in at least two consecutive visits; and (4) subjects who underwent other treatments before and afterwards, such as those involving atropine eye drops or red-light-related instruments.
2.2. Clinical pathway of orthokeratology
At the first visit, all subjects underwent comprehensive examinations, including cycloplegic refraction, uncorrected visual acuity, BCVA, corneal light reflection, intraocular pressure, extraocular movements, slit-lamp, fluorescein staining, corneal endothelial cell density, axial length (AL), fundus photography, and corneal topography. Appropriate prescriptions for OK lenses were provided to the subjects by the same group of three experienced doctors. The subjects were asked to wear OK lenses no fewer than 8 h per night and follow-up one week and one month after wearing them (two months after prescription because it usually took approximately a month from the time the prescription was made to the time the lenses were received). Then, they were asked to visit every 3 months thereafter. At each subsequent follow-up, the subjects underwent several ocular examinations, including corneal light reflection tests, slit-lamp evaluations, fluorescein staining, AL examinations, visual acuity tests without frame glasses, and corneal topography. During each follow-up, we recorded the adequacy of lens fitting and lens care and whether the subjects experienced glare, diplopia, or other symptoms. After 1.5 years of wearing OK lenses (the 19th month after fitting), all subjects were required to change lenses. Although a washout period (no OK lens wearing) of one month was suggested, some parents chose to let the doctors formulate the replacement prescriptions directly according to changes in AL to avoid delaying the control of myopia.
Ethical Approval
All the subjects were treated according to the tenets of the Declaration of Helsinki. This study was approved by the Ethics Committee of the Children's Hospital of Fudan University. The authors confirmed that all methods were performed in accordance with the relevant guidelines and regulations. All brands of OK lenses were equally available and subjects were fitted with different brands of OK lenses only if the first attempted brand did not successfully fit their one eye because of the poor tear circulation, lack of suitable diameter or appropriate toric design, etc. Before prescribing, all parents were well informed about the use of different brands of OK lenses and there was no evidence of different myopia control efficacy between different brands for then [11], but there may be different comfort of different OK lenses. All parents and children were asked to sign informed consent forms.
2.3. Lenses
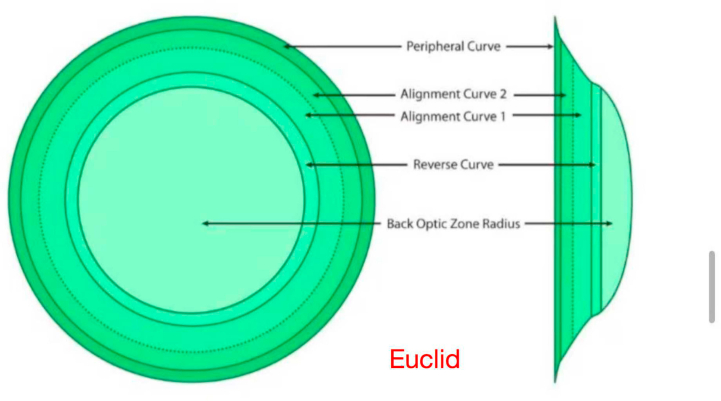
All the subjects were fitted with lenses from among three imported brands of OK lenses (α ORTHO‐K®, ALPHA Corp., Nagoya, Japan, with a nominal oxygen permeability (DK) of 104 × 10−11 (cm2/s) (mL O2/mL·mmHg); LUCID ORTHO‐K®, LUCID Corp., Fenghua County, Korea, with a nominal DK of 100 × 10−11 (cm2/s) (mL O2/mL·mmHg); Euclid ORTHO‐K®, Euclid Systems Corporation, Herndon, USA, with a nominal DK of 104 × 10−11 (cm2/s) (mL O2/mL·mmHg)), according to the manufacturer's fitting instructions. Domestic brands are rarely selected; therefore, they were excluded from this study. The toric OK lenses used in this study were designed to improve stabilisation and central positioning. All brands of OK lenses had a four-zone vision-shaping treatment (VST) design. The optical configurations of the three lens types are listed in Table 1.
Table 1.
The configuration of three orthokeratology (OK) contact lenses (all with a diameter of 10.6 mm).
| Brand of OK lenses | Euclid | Alpha | Lucid |
|---|---|---|---|
| Optic zone diameter | 6.2 mm | 6.0 mm | 6.2 mm |
| Reverse curve width | 0.5 mm | 0.6 mm | 0.9 mm |
| Alignment curve width | 1.2 mm | 1.3 mm | 0.8 mm |
| Peripheral curve width | 0.5 mm | 0.4 mm | 0.5 mm |
| Position for the toric design | Reverse curve Alignment curve |
Alignment curve | Reverse curve Alignment curve Peripheral curve |
| Materials | Boston Equalens II | Boston EM | Boston XO |
2.4. Measurements
Cycloplegic refraction at baseline was measured twice by specialised technicians to ensure accuracy. The K value was measured thrice using an autorefractor keratometer (NIDEK Co., LTD., Japan, Model ARK-1). The AL was measured thrice using an IOL-Master 500 (Carl Zeiss Meditec AG, Jena, Germany). The examinations were performed by the same specialised technician thrice, and the average value was recorded.
Corneal profiles were measured with a Carl Zeiss ATLAS Corneal Topography System 9000 (Carl Zeiss Meditec, Inc., California, USA, Model 9000). Each profile was the best-focus image (accuracy greater than 95%) from four frames captured automatically. The following topographic map measurements were performed by the same experienced technician, who was blinded to the lens brand of the measured object.
Measurement of the treatment zone: According to corneal topography, the treatment zones ranged from the corneal apex to where the keratometry values changed within 1 D and less than two types of colours on the palette scale. The treatment zone centre (TZC) in this study was determined by marking the horizontal and vertical maximum distances of the treatment zone (HMDTZ and VMDTZ) of the corneal topography map through software (Photoshop 6.0); the intersecting point was considered as the centre. The pupillary centre was determined by corneal topography using the Pupil-Finding software. The distance of decentration (DOD) was the length between the TZC and the pupillary centre and was measured precisely using the ruler of the software compared with the grid (one grid represented 1 mm).
Measurement of the width of the high convex zone (WHCZ): The high convex zone was defined as a circular area steeper than the treatment area generated by the reverse curve. The WHCZ was not directly equal to the width of the reverse curve, largely because of the existence of a transition zone. In this study, we artificially measured the four shortest widths of the high-convexity zone, starting at the four frontiers of the HMDTZ and the VMDTZ, and the WHCZ was defined as the average of four values. The measurement method is illustrated in Fig. 1.
Fig. 1.
Measurement diagram of the TZC (treatment zone centre), HMDTZ (horizontal maximum distance of the treatment zone, red line in the topographic map), VMDTZ (vertical maximum distance of the treatment zone, red line in the topographic map), WHCZ (width of the high convex zone, blue line in the topographic map), and the angle of the decentration vector. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Measurement of the direction of decentration: It is generally accepted that decentration is not only a value of distance but also a vector with directional properties, particularly when calculating the average value. We used the following original method to calculate the direction: after drawing the decentration line in Photoshop, we simulated a coordinate system with the origin determined by the pupil centre and then measured its angle (angle α and angle β) between the decentration line and the negative part of the horizontal and vertical axes with the contained protractor tool. All measurements are shown in Fig. 1. The horizontal and vertical components of each decentration vector (HCD and VCD) were finally obtained through the formula HCD = −1 × (DOD × COS α); VCD = −1 × (DOD × COS β). The average value of the decentration vector (ADV) after three measurements was calculated using the Pythagorean theorem, as follows: ADV = . Finally, we matched the horizontal direction to the nasal and temporal sides, depending on whether the tested eye was right or left.
Calculating only the vector may weaken the influence of cases with large differences in the direction of decentration; thus, we also measured the average value of decentration algebraically (ADA, ADA = ).
2.5. Statistical analysis
SPSS Statistics 24.0 (IBM Statistics, Armonk, NY, USA) was used for statistical analysis of ocular biometric parameters. The Shapiro–Wilk test was used to check for normality. The differences in the parameters at baseline, HMDTZ, VMDTZ, WHCZ, HCD, VCD, ADV, and ADA between each pairwise group (Euclid vs. Lucid, Lucid vs. Alpha, and Alpha vs. Euclid) were compared using paired t-tests. Repeated measures analysis of variance (ANOVA) was used to compare the corrected visual acuity after removing OK lens at each visit and the changes in AL over time between each pairwise group. A P value less than 0.05 was considered statistically significant.
3. Results
We totally enrolled 113 children in this study: 46 children wore Lucid and Euclid lens simultaneously; another 50 children simultaneously wore Lucid and Alpha lens; the rest 17 children wore Euclid and Alpha lens simultaneously. There was no intersection between the three groups used for self-control.
3.1. Analysis of three paired groups
3.1.1. Lucid vs. Euclid
There were 46 children (male: 26, female: 20) with an average age of 10.3 (8–14) years were enrolled, and their baseline parameters are shown in Table 2. According to the data, there was very high comparability between the two eye groups.
Table 2.
The baseline parameters of 46 children who simultaneously wore Lucid and Euclid OK lenses.
| Parameter (Mean ± SD) | Eyes with Lucid (n = 46) | Eyes with Euclid (n = 46) | p value |
|---|---|---|---|
| Axial length (mm) | 24.78 ± 0.97 | 24.80 ± 0.93 | 0.65 |
| Spherical refractive error (DS) | −2.88 ± 1.23 | −2.91 ± 1.25 | 0.64 |
| With-the-rule astigmatism (DC) | −0.54 ± 0.51 | −0.58 ± 0.55 | 0.47 |
| J0 | 0.26 ± 0.24 | 0.27 ± 0.26 | 0.57 |
| J45 | −0.03 ± 0.11 | −0.04 ± 0.13 | 0.75 |
| Spherical equivalent refractive error (SE)(D) | −3.15 ± 1.34 | −3.20 ± 1.25 | 0.48 |
| Equivalent e value | 0.61 ± 0.07 | 0.60 ± 0.07 | 0.09 |
| Steep K (D) | 44.39 ± 1.69 | 44.38 ± 1.64 | 0.77 |
| Flat K (D) | 43.26 ± 1.54 | 43.21 ± 1.50 | 0.42 |
| Degree of toric design (D) | −0.55 ± 0.69 | −0.60 ± 0.74 | 0.60 |
| Diameter of the OK lens (mm) | 10.64 ± 0.19 | 10.66 ± 0.16 | 0.21 |
The AL increased by 0.27±0.24mm in the Lucid-versus-Euclid-Lucid group (group LE-L) and 0.31±0.24 in the Euclid group (group LE-E) at 19 months. We found no statistical difference between the paired eyes in the final change of AL by paired t-test (p =0.34) and the changes in AL in both groups are shown in Fig. 2. By repeated-measures analysis of variance, the time course was found to have a significant effect on the change in AL (p< 0.001), whereas the difference in lens brand had no significant effect on the change in AL (p =0.68). In terms of corrected visual acuity at each visit, the time course and the difference in lens brand both had no significant effect (p =0.50 and p= 0.37, respectively). When dividing the subjects into two groups by age, no statistical difference between the paired eyes in the final change of AL was found in both younger group (age 8 to 10, n=24, 0.36± 0.25mm vs. 0.38±0.18mm, p =0.73) and older group (age 11 or older, n=22, 0.18±0.19mm vs. 0.23±0.26 mm, p =0.34). When dividing the subjects into two groups by SE, no statistical difference in the final change of AL between the paired eyes was found in both low-myopia group (0 ≤ SE ≤ −3.00D, n =22, 0.32 ± 0.20 mm vs. 0.35 ± 0.23 mm, p =0.57) and moderate-myopia group (SE<-3.00D, n =24, 0.23 ± 0.27 mm vs. 0.27 ± 0.24 mm, p =0.40).
Fig. 2.
The change in AL in groups LE-L and LE-E, which were both from the 46 children who simultaneously wore Lucid and Euclid OK lenses.
With regards topographic maps, the HMDTZ, VMDTZ, ADV and ADA in the LE-L group were both significantly larger than those in the LE-E group (p<0.001, p=0.01, p = 0.01 and p = 0.02 respectively). There was no significant difference found in the WHCZ, HCD and VCD between the LE-L and LE-E (LE-L:1.02 ± 0.31 mm, LE-E:0.99 ± 0.35 mm, p = 0.37) groups (p = 0.37, 0.06 and 0.99 respectively). The mean corneal reshaping parameters can be seen in Table 3.
Table 3.
The change of AL after 19 months and the mean of three corneal reshaping parameters of 46 children who simultaneously wore Lucid and Euclid OK lenses.
| Parameter (Mean ± SD) | Group LE-L (n = 46) | Group LE-E (n = 46) | p value (paired t-test) |
|---|---|---|---|
| Change of AL (mm) | 0.27 ± 0.24 | 0.31 ± 0.24 | 0.34 |
| HMDTZ (mm) | 3.85 ± 0.52 | 3.45 ± 0.53 | <0.001 |
| VMDTZ (mm) | 3.54 ± 0.60 | 3.26 ± 0.61 | 0.01 |
| WHCZ (mm) | 1.02 ± 0.31 | 0.99 ± 0.35 | 0.37 |
| HCD (mm) | 0.26 ± 0.53 | 0.07 ± 0.46 | 0.06 |
| VCD (mm) | −0.21 ± 0.61 | −0.21 ± 0.47 | 0.99 |
| ADV (mm) | 0.73 ± 0.44 | 0.55 ± 0.45 | 0.01 |
| ADA (mm) | 0.80 ± 0.41 | 0.63 ± 0.44 | 0.02 |
Group LE-L: group Lucid-versus-Euclid-Lucid, Group LE-E: group Lucid-versus-Euclid-Euclid. AL:axial length; HMDTZ: horizontal maximum distance of the treatment zone; VMDTZ: vertical maximum distance of the treatment zone; WHCZ: width of the high convex zone; HCD: horizontal component of the decentration vector; VCD: vertical component of the decentration vector; ADV: average value of the decentration vector; ADA: average value of decentration calculated algebraically.
The distribution of the average position of the TZC in the LE-L and LE-E groups is shown in Fig. 3. Infratemporal decentration was the most commonly observed direction in both the groups.
Fig. 3.
The distribution of the vectorized average position of the TZC (treatment zone centre) in the LE-L and LE-E groups. For Lucid there was one eye located at the origin of the axis, while for Euclid there were 8 eyes located at the origin of the axis where they overlapped each other.
3.2. Lucid vs. alpha
Another 50 children (male: 16, female: 34) with an average age of 9.4 (8–14) years were enrolled, and their baseline parameters are shown in Table 4. Significant differences were found only in the degree of toric design between the two groups (previously, we did not have lenses with a toric design for alpha lenses).
Table 4.
The baseline parameters of 50 children who simultaneously wore Lucid and Alpha OK lenses.
| Parameter (Mean ± SD) | Eyes with Lucid (n = 50) | Eyes with Alpha (n = 50) | p value |
|---|---|---|---|
| Axial length (mm) | 24.32 ± 0.58 | 24.32 ± 0.62 | 0.94 |
| Spherical refractive error (DS) | −2.15 ± 0.87 | −2.24 ± 0.99 | 0.13 |
| With-the-rule astigmatism (DC) | −0.47 ± 0.43 | −0.43 ± 0.45 | 0.41 |
| J0 | 0.22 ± 0.21 | 0.20 ± 0.21 | 0.35 |
| J45 | −0.03 ± 0.08 | −0.04 ± 0.09 | 0.47 |
| Spherical equivalent refractive error (SE)(D) | −2.38 ± 0.99 | −2.45 ± 1.08 | 0.26 |
| Equivalent e value | 0.63 ± 0.09 | 0.64 ± 0.09 | 0.16 |
| Steep K (D) | 44.28 ± 1.23 | 44.28 ± 1.17 | 0.94 |
| Flat K (D) | 43.13 ± 1.13 | 43.17 ± 1.13 | 0.39 |
| Degree of toric design (D) | −0.28 ± 0.50 | 0.00 ± 0.00 | <0.001 |
| Diameter of the OK lens (mm) | 10.54 ± 0.19 | 10.58 ± 0.11 | 0.05 |
The AL increased by 0.36± 0.26mm in the Lucid group (group LA-L) and 0.36 ±0.27 mm in the Alpha group (group LA-A) at 19 months. We found no statistical difference between the paired eyes in the final change of AL by paired t-test (p =0.96). By repeated-measures analysis of variance, the time course was found to have a significant effect on the change in AL (p <0.001), whereas the difference in lens brand had no significant effect on the change in AL (p =0.85). The changes in AL in both groups are shown in Fig. 4. In terms of corrected visual acuity at each visit, the time course and the difference in lens brand both had no significant effect (p =0.15 and p =0.58, respectively). When dividing the subjects into two groups by age, no statistical difference between the paired eyes in the final change of AL was found in both younger group (age 8 to 9, n =34, 0.43 ±0.27 mm vs. 0.45 ±0.25 mm, p =0.50) and older group (age 10 or older, n =16, 0.21 ±0.15 mm vs. 0.17 ±0.22 mm, p =0.25). When dividing the subjects into two groups by SE, no statistical difference between the paired eyes in the final change of AL was found in both low-myopia group (0 ≤ SE ≤ −2.50D, n =31, 0.46 ±0.25 mm vs. 0.46 ±0.25 mm, p =0.82) and moderate-myopia group (SE<-2.50D, n = 19, 0.19 ±0.15 mm vs. 0.27 ±0.24 mm, p =0.81).
Fig. 4.
The change in AL in the LA-L and LA-L groups, which were both from the 50 children who simultaneously wore Lucid and Alpha OK lenses.
With regards topographic maps, the HMDTZ and VMDTZ in the LA-L group were both significantly larger than those in the LA-A group (both p <0.001). But there was no significant difference found in the WHCZ, HCD, VCD, ADV and ADA (p =0.97, 0.83, 0.31, 0.68 and 0.97, respectively). The mean corneal reshaping parameters can be seen in Table 5.
Table 5.
The change of AL after 19 months and the mean of three corneal reshaping parameters of 50 children who simultaneously wore Lucid and Alpha OK lenses.
| Parameter (Mean ± SD) | Group LA-L (n = 50) | Group LA-L (n = 50) | p value (paired t-test) |
|---|---|---|---|
| Change of AL (mm) | 0.36 ± 0.26 | 0.36 ± 0.27 | 0.96 |
| HMDTZ (mm) | 3.93 ± 0.60 | 3.67 ± 0.56 | <0.001 |
| VMDTZ (mm) | 3.58 ± 0.50 | 3.23 ± 0.48 | <0.001 |
| WHCZ (mm) | 0.87 ± 0.26 | 0.87 ± 0.24 | 0.97 |
| HCD (mm) | 0.32 ± 0.42 | 0.33 ± 0.41 | 0.83 |
| VCD (mm) | −0.23 ± 0.44 | −0.29 ± 0.44 | 0.31 |
| ADV (mm) | 0.60 ± 0.41 | 0.62 ± 0.40 | 0.68 |
| ADA (mm) | 0.65 ± 0.41 | 0.67 ± 0.42 | 0.67 |
Group LE-L: group Lucid-versus-Euclid-Lucid, Group LE-E: group Lucid-versus-Euclid-Euclid. AL:axial length; HMDTZ: horizontal maximum distance of the treatment zone; VMDTZ: vertical maximum distance of the treatment zone; WHCZ: width of the high convex zone; HCD: horizontal component of the decentration vector; VCD: vertical component of the decentration vector; ADV: average value of the decentration vector; ADA: average value of decentration calculated algebraically.
The distribution of every average position of the TZC in the LA-L and LA-A groups is illustrated in Fig. 5, and we found that the infratemporal decentration was the most commonly observed direction in the two groups.
Fig. 5.
The distribution of the vectorized average position of the TZC in the LA-L and LA-A groups. For Lucid there were 9 eyes located at the origin of the axis where they overlapped each other, while for Alpha there were 8 eyes.
3.3. Euclid vs. alpha
The rest 17 children (male: 6, female: 11) with an average age of 9.4 (8–15) years were enrolled; their baseline parameters are summarized in Table 6, indicating high baseline comparability (see Table 7).
Table 6.
The baseline parameters of 17 children who simultaneously wore Euclid and Alpha OK lenses.
| Parameter (Mean ± SD) | Eyes with Euclid (n = 17) | Eyes with Alpha (n = 17) | p value |
|---|---|---|---|
| Axial length (mm) | 24.51 ± 0.74 | 24.53 ± 0.83 | 0.92 |
| Spherical refractive error (DS) | −1.97 ± 0.95 | −2.13 ± 1.00 | 0.63 |
| With-the-rule astigmatism (DC) | −0.33 ± 0.41 | −0.37 ± 0.42 | 0.80 |
| J0 | 0.15 ± 0.20 | 0.15 ± 0.20 | 0.97 |
| J45 | −0.02 ± 0.05 | −0.02 ± 0.08 | 0.96 |
| Spherical equivalent refractive error (SE)(D) | −2.13 ± 1.05 | −2.30 ± 1.12 | 0.65 |
| Equivalent e value | 0.62 ± 0.07 | 0.63 ± 0.07 | 0.57 |
| Steep K (D) | 43.46 ± 0.91 | 43.38 ± 0.82 | 0.81 |
| Flat K (D) | 42.46 ± 0.96 | 42.44 ± 0.93 | 0.96 |
| Degree of toric design (D) | −0.26 ± 0.59 | 0.00 ± 0.00 | 0.07 |
| Diameter of the OK lens (mm) | 10.62 ± 0.14 | 10.60 ± 0.19 | 0.68 |
Table 7.
The change of AL after 19 months and the mean of three corneal reshaping parameters of 17 children who simultaneously wore Euclid and Alpha OK lenses.
| Parameter (Mean ± SD) | Group EA-E (n = 17) | Group EA-A (n = 17) | p value (paired t-test) |
|---|---|---|---|
| Change of AL (mm) | 0.34 ± 0.27 | 0.41 ± 0.28 | 0.06 |
| HMDTZ (mm) | 3.21 ± 0.77 | 3.33 ± 0.73 | 0.38 |
| VMDTZ (mm) | 3.04 ± 0.55 | 3.08 ± 0.47 | 0.68 |
| WHCZ (mm) | 0.70 ± 0.19 | 0.66 ± 0.19 | 0.26 |
| HCD (mm) | 0.15 ± 0.20 | 0.20 ± 0.24 | 0.51 |
| VCD (mm) | −0.09 ± 0.184 | −0.11 ± 0.24 | 0.64 |
| ADV (mm) | 0.23 ± 0.22 | 0.31 ± 0.28 | 0.34 |
| ADA (mm) | 0.25 ± 0.25 | 0.32 ± 0.31 | 0.42 |
Group LE-L: group Lucid-versus-Euclid-Lucid, Group LE-E: group Lucid-versus-Euclid-Euclid. AL:axial length; HMDTZ: horizontal maximum distance of the treatment zone; VMDTZ: vertical maximum distance of the treatment zone; WHCZ: width of the high convex zone; HCD: horizontal component of the decentration vector; VCD: vertical component of the decentration vector; ADV: average value of the decentration vector; ADA: average value of decentration calculated algebraically.
The AL increased by 0.34 ± 0.27 mm in the Euclid group (group EA-E) and 0.41 ± 0.28 mm in the Alpha group (group EA-A) at 19 months. We found no statistical difference between the paired eyes in the final change of AL by paired t-test (p = 0.06). By repeated-measures analysis of variance, the time course was found to have a significant effect on the change in AL (p < 0.001), whereas the difference in lens brand had no significant effect on the change in AL (p = 0.63). The changes in AL in both groups are shown in Fig. 6. In terms of corrected visual acuity at each visit, the time course and the difference in lens brand both had no significant effect (p = 0.56 and p = 0.82 respectively) (see Fig. 7).
Fig. 6.
The change in AL in the EA-E and EA-A groups was observed in 17 children who simultaneously wore both Euclid and Alpha OK lenses.
Fig. 7.
The distribution of the vectorized average position of the TZC in the EA-E and EA-A groups. Points at the same position in the figure covered each other, mainly the position of the origin.
With regards topographic maps, the HMDTZ, VMDTZ, WHCZ, HCD, VCD, ADV and ADA all showed no difference between the EA-E and EA-A groups (p = 0.38, 0.68, 0.26, 0.51, 0.64, 0.34 and 0.42 respectively).
Due to the small sample size, stratified analysis was abandoned in the Euclid-Alpha paired group.
3.4. Stability of lens position
According to the theorem that the synthesis of vectors in different directions is always smaller than their algebraic sum, the value of the ADV of the same eye does not exceed the ADA. Therefore, the result of ADV/ADA can be used to determine the percentage of vectors lost in different directions during synthesis (if ADV = ADA = 0, then the result of ADV/ADA is defined as 1). Therefore, the closer the result of ADV/ADA is to 1, the more stable is the lens position, and the closer it is to 0, the more unstable is the position. In this study, the results of the ADV/ADA were 0.91 ± 0.18 for Lucid (n = 96), 0.90 ± 0.19 for Euclid (n = 63) and 0.95 ± 0.11 for Alpha (n = 67). Although the result of Alpha was the closest to 1, the independent sample t-test showed that there was no significant difference between each pair (Lucid vs. Euclid: p = 0.80, Lucid vs. Alpha: p = 0.12, Euclid vs. Alpha: p = 0.10).
3.5. Analysis of pooled data
For the further analysis, we pooled all the subjects together (113 eyes from 113 subjects). Due to the subsequent statistical analysis requiring independence between samples, only the data of right eyes were used in the subsequent statistical analyses.
Effect of individual differences on axial elongation: for the overall cohort with 113 eyes, after dividing participants into three groups according to lens brand (group Lucid: n = 43; group Euclid: n = 36; and group Alpha: n = 34), We find statistical differences in baseline age (p = 0.01, only significant difference between group Euclid and group Alpha (p = 0.01)) and no difference in final change of AL, baseline AL and baseline SE among three groups by ANOVAs after homogeneity of variance test as well as post hoc analysis of Bonferroni correction (p = 0.55, 0.12, and 0.42, respectively). In this regard, individual differences seem did not affect the results of AL elongation meaningfully and it will draw similar conclusions if we did not use the self-controlled method. But as far as we know, the statistical efficiency of paired t-test is better than independent t-test and more better than ANOVAs, and the baseline comparability of paired groups are better, so the authors believe that conclusions based on the self-controlled method will be more solid.
Correlation analysis: For the overall cohort with 113 eyes, we performed Pearson correlation analysis on the change in AL with WHCZ, HMDTZ, VMDTZ, ADV, and ADA, and Spearman correlation analysis on the brands of lenses. We found that the change in AL was significantly correlated with the ADV and ADA, and the correlation coefficients were −0.38 (p < 0.001) and −0.37 (p < 0.001) respectively. No obvious correlation was found between the changes in AL and the WHCZ, HMDTZ, VMDTZ, or brand (p = 0.15, 0.52, 0.74, and 0.58, respectively).
Rates of Axial elongation: According to Lu's research [10], after 19 months, no progression is defined as AL elongation ≤0.15 mm, slow progression is defined as AL elongation 0.15–0.4 mm, fast progression is defined as AL elongation >0.4 mm. After Pearson's chi-square test for multiple sample rates with the Bonferroni method of correction for multiple comparisons,no statistical differences in rates of Axial elongation between group Lucid (no progression, slow progression, fast progression: n = 14 (32.6%), n = 12 (27.9%), n = 17 (39.5%)), group Euclid (n = 10 (27.8%), n = 17 (47.2%), n = 9 (25%)) and group Alpha (n = 6 (17.6%), n = 13 (38.2%), n = 15 (44.1%)) was found (p = 0.24).
4. Discussion
4.1. Differences in myopia control effects of different OK lenses
With the growing popularity of OK lenses, increasing attention has been paid to the efficacy of OK lenses in controlling myopia. Furthermore, an increasing number of OK lenses with varying lens designs and materials are available. This led to a discussion on whether these different brands and designs lead to differences in the clinical efficacy of myopia control. With regards the comparison of different brands of lenses, we found that a final conclusion could not be reached based on previous study because of the small amount of research and large individual differences. Related studies have shown that local brands in China (including joint venture brands) may be relatively ineffective in myopia control [8], and corneal refractive therapy (CRT) lenses may be relatively weak compared with VST lenses [10] (the possible reason are as follow: CRT lens had a lower compression factor (0.5 D) than the VST lenses (0.75 D), CRT lens have less curves than VST lens, the center thickness was thinner in the CRT lens which may lead to less mechanical action on the cornea and the different material may also be a possible
influencing factor [10]), while there may be no significant difference between other brands [[6], [7], [8], [9], [10]]. A brief description of all relevant studies is provided in Table 8.
Table 8.
Differences in myopia control effects of different OK lenses (different brands or designs).
| Study | Difference in the design of OK lenses | Study time | Country or area | Number of eyes | Criteria | Efficacy of myopia control |
|---|---|---|---|---|---|---|
| Mj Zhu, Hy Feng and Xm Qu [6] | Different brand (hidden) | One year | China | Brand 1: 102 Brand 2: 50 Brand 3: 102 |
Change in AL | Brand 1 = Brand 2 Brand 2 = Brand 3 Brand 3>Brand 1 |
| Pauline Kang and Helen Swarbrick [7] | BE, Australia Paragon CRT, USA Contex, USA |
Two weeks | Australia | BE: 38 CRT: 19 Contex: 19 |
Relative peripheral refraction changes | Differed minimally among the three OK lens |
| Ruru Chen, Colm McAlinden et al. [8] | Essence, USA Euclid, USA Lucid, Korea Moldway, China |
Two years | China | Essence: 51x2 Euclid: 51x2 Lucid: 46x2 Moldway: 53x2 |
Change in AL | Essence > Moldway Other intergroups: Equal |
| Nakamura Y, Kinoshita S. et al. [9] | Menicon, Japan Alpha, Japan Emerald, America |
Two years | Japan | Menicon: 24x2 Alpha: 28x2 Emerald: 27x2 |
Change in AL and refractive error | Menicon = Alpha = Emerald |
| Lu W, Jin W. et al. [10] | CRT vs. VST (Euclid, America Alpha, Japan Hiline, China) |
1.5 years | China | CRT: 263 Euclid: 277 Alpha: 236 Hiline: 225 |
Change in AL | Euclid, Alpha, Hiline > CRT Euclid = Alpha Alpha = Hiline Euclid > Hiline |
| Pauné J, Queirós A. et al. [12] | Different back optical zone diameters | One year | Spain | Larger diameter (>5 mm): 36 Smaller diameter (≤5 mm): 35 |
Change in AL | Smaller diameter > Larger diameter |
| Guo B. Cho P. et al. [13] | Different back optic zone diameters | One year | China | 6 mm: 34 5 mm: 36 |
Change in AL | Lens with 5 mm diameter > Lens with 6 mm diameter |
| Loertscher M, Phillips JR. et al. [14] | New multifocal orthokeratology vs. Conventional orthokeratology | 1.5 years | New Zealand | 30 (Paired-eye study) | Change in AL | New multifocal > Conventional |
| Wan K, Cho P. et al. [15] | Different compression factors (0.75 D vs. 1.75 D) | Two years | China | 0.75 D: 29 1.75 D: 35 |
Change in AL | Increased compression factors (1.75 D) > Conventional compression factors (0.75 D) |
With regards the AL growth rate, no significant difference was found between each pair in our study (LE-L:0.27 ± 0.24 mm, LE-E:0.31 ± 0.24 mm, p = 0.68; LA-L:0.36 ± 0.26 mm, LA-A:0.36 ± 0.27 mm, p = 0.85; EA-E:0.34 ± 0.27 mm, EA-A:0.41 ± 0.28 mm, p = 0.63), which is consistent with the results of studies by Chen and Lu [8,10]. The lenses in this study were all designed for VST; therefore, the differences between CRT and VST could not be examined.
4.2. Corneal reshaping of different OK lenses
According to existing research, the effect of OK lenses on myopia control differs among subjects owing to patient-related factors. In general, smaller increases in AL are associated with factors such as older age, greater baseline spherical equivalent myopic refractive error, larger pupil diameter, more outdoor lighting [[16], [17], [18], [19], [20]]. On the other hand, there are lens-related factors. For example, based on current research, smaller increases in AL are associated with a smaller back-optic zone of lenses, increased compression factors, and a new multifocal design (details can be seen in Table 8) [[12], [13], [14], [15]]. In addition, smaller increases in AL may be related to lens decentration [[21], [22], [23], [24]].Therefore, this study not only used self-controlled methods but also compared the corneal reshaping of children who wore different brands of OK lenses through corneal topography to improve the credibility of our study.
Currently, there are few studies on the differences in corneal reshaping based on corneal topography after wearing different brands of OK lenses. According to a study by Marcotte-Collard, Paragon CRT lenses have a larger treatment zone and equal width of the high convex zone compared to that of the Dreamlens [25]. According to this study, the average diameter of the treatment zone of Lucid lenses was significantly larger than that of Euclid and Alpha lenses, while there was no significant difference between the Euclid and Alpha lenses. Besides, no obvious difference in the width of the high convex zone was found between each paired group. So, it can be seen that there is some contradiction between the differences in the parameters of the three lenses and the few difference in corneal reshaping in this study. For example, Lucid had the same optic zone diameter as the Euclid but a larger HMDTZ and VMDTZ; moreover, Lucid had the design with larger reverse curve width, but the same WHCZ as the other brands. According to the authors’ conjecture, this may be because the parameters of the transition zone between each curve of the different lenses were dissimilar and not publicly available. In addition, corneal shaping is not completely consistent with the back surface of the lens in clinics. According to previous studies, improved myopia control efficiency is related to a smaller treatment zone [12,13], which may be due to a greater peripheral defocus. However, in this study, although Euclid and Alpha had smaller treatment zones, better efficiency was not observed. The explanation for this could be that the difference in the size of the treatment zone found in this experiment was less than 0.5 mm, which is obviously smaller than the 1.0 mm used in other studies [12,13]. In this study, we also found that WHCZ has no significant correlation with axial growth for the overall cohort with 113 eyes, which has not been mentioned in previous studies. In authors' consideration, this may be because the definition of WHCZ in this study included a portion of the transition zone. About this result, further studies are required to verify.
4.3. Decentration of different OK lenses
In orthokeratology lens fitting, clinicians should basically try to locate the OK-lens centered on the corneal center. However, in fact, the situation of decentration still happens frequently. At present, there is no unified measurement method for decentration, and it is mainly divided into two types: one is indirectly measurement by difference maps of corneal topography after removing lens and the other is directly assessment through corneal topography with the lens on. About the myopia control, there is no clear conclusion regarding whether decentration affects the control efficiency, although studies indicate that it may be beneficial for efficiency [[21], [22], [23], [24],26]. The authors presumed that the possible reason could be more peripheral defocus and larger higher-order aberrations brought by decentration [27,28]. Herein, we observed significant differences in decentration between the LE-L and LE-E groups in both vector and algebraic values. Although the correlation analysis for the overall cohort with 113 eyes showed a weak correlation between greater decentration and less AL growth, there was still no significant difference in axial length growth between the LE-L and LE-E groups and that could be because the difference in decentration between the two groups (vector value:0.73 ± 0.44 mm vs. 0.55 ± 0.45 mm; algebraic value: 0.80 ± 0.41 mm vs. 0.63 ± 0.44 mm) was too small to cause a difference in myopia control efficiency. To the best of our knowledge, this is the first time that vectorial and algebraic calculation methods have been used for average decentration assessment, where the direction can only be calculated after vectorisation. Therefore, the relevant results of this study are not comparable to those of previous related studies. In this study, there was a significant difference between the ADV and ADA in all 113 pairs of eyes (0.57 ± 0.42 mm vs. 0.63 ± 0.43 mm P < 0.05) by paired t-test, and whether the vector method or algebraic method should be used to calculate the average value of decentration remains undetermined, but the authors still suggest that after the vector is considered, the calculation of decentration will be more comprehensive. Considering the results of the ADV/ADA, we believe that it can reflect the stability of the lens position or the degree of dispersion for each eye. The standard deviation of the ADV or ADA reflects the dispersion of lens decentration for all participants but not for each individual. In the authors' opinion, the result of the ADV/ADA is more accurate when measuring the stability of each lens' position. In this study, there was no statistical difference in ADV/ADA values among the three brands of OK lenses, meaning they had the same lens position stability. We also found that infratemporal decentration was the most common direction of decentration, which was similar to most other studies. In addition, this study provides a reference scheme for a computer program to calculate the average degree and direction of decentration, and the stability of the lens position after OK.
5. Advantages and limitations
Compared to previous studies, this study largely avoided most individual differences, such as age, baseline AL and SE, pupil size every moment, daily outdoor sunlight exposure, situation of daily near-work, daily use of OK lenses, etc. In addition, this study added detailed analysis of actual corneal reshaping, which was lack in other studies. Besides, this was the first study to present a method for vector measurement of mean decentration and the stability of the lens position. However, this study only focused on the comparison of the axial length growth and corneal reshaping among different brands of OK lenses and has the following limitations. First, there was a lack of analysis on the spherical equivalent and visual quality (e.g. high order aberrations). Second, it was difficult to rule out subtle effects between the paired eyes (impact on accommodation, variable parameters, etc). Third, considering that lenses were worn in both eyes, a washout period was not implemented to increase the number of cases. Fourth, the sample size for the Euclid vs. Alpha group was relatively small, and it could affect the difference in axial elongation and corneal reshaping detected in this study. Finally, peripheral defocus and the degree of the high convex zone was not detected because of the past inadequate testing conditions; therefore, we could not fully explain the results.
6. Conclusion
In general, after OK according to this self-control study (children with myopia simultaneously wear OK lenses of different brands), there was no significant difference between each pair of the three brands in terms of axial length growth, although Lucid had a larger treatment zone both than Euclid and Alpha, and Lucid had more decentration than Euclid. The average value and direction of decentration could be assessed more comprehensively through vectorisation. The ADV/ADA results can be used to measure the stability of the lens position, and there was no significant difference among the three brands in this study. A larger lens decentration was weakly related to better myopia control efficiency.
Data availability statement
Data associated with this study was not deposited into a publicly available repository, but the myopia data and corneal topography measurement results for all subjects at every visit can be found in a supplementary material named "raw data". Please correspond to the corresponding authors regarding the further information regarding the subjects.
Funding
This study was supported by the Shanghai Hospital Development Center with Project: SHDC2020CR1043B-002.
Ethical approval
This study was approved by the Ethics Committee of the Children's Hospital of Fudan University (No. [2021]468) as routine data for the clinical purpose. We confirmed that all methods were performed in accordance with the relevant guidelines and regulations.
CRediT authorship contribution statement
Anken Wang: Writing – review & editing, Writing – original draft, Methodology, Data curation, Conceptualization. Wansheng Zang: Software, Methodology, Data curation. Li Shen: Methodology, Data curation. Lu Gao: Writing – review & editing, Writing – original draft, Methodology, Data curation. Chenhao Yang: Writing – review & editing, Supervision, Methodology, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e27562.
Contributor Information
Lu Gao, Email: gaolu-dr@hotmail.com.
Chenhao Yang, Email: ychben@hotmail.com.
Appendix A. Supplementary data
The following are the Supplementary data to this article.
figs1.
figs2.
figs3.
References
- 1.Holden B.A., Fricke T.R., Wilson D.A., Jong M., Naidoo K.S., Sankaridurg P., Wong T.Y., Naduvilath T.J., Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Dolgin E. The myopia boom. Nature. 2015;519:276–278. doi: 10.1038/519276a. [DOI] [PubMed] [Google Scholar]
- 3.Kakita T., Hiraoka T., Oshika T. Influence of overnight Orthokeratology on axial elongation in childhood myopia. Invest. Ophthalmol. Vis. Sci. 2011;52:2170–2174. doi: 10.1167/iovs.10-5485. [DOI] [PubMed] [Google Scholar]
- 4.Tarutta E.P., Verzhanskaya T.Y. Stabilizing effect of orthokeratology lenses (ten-year follow-up results) Vestn. Oftalmol. 2017;133:49–54. doi: 10.17116/oftalma2017133149-54. [DOI] [PubMed] [Google Scholar]
- 5.Li X., Friedman I.B., Medow N.B., Zhang C. Update on orthokeratology in Managing progressive myopia in children: efficacy. J. Pediatr. Ophthalmol. Strabismus. 2017;54:142–148. doi: 10.3928/01913913-20170106-01. [DOI] [PubMed] [Google Scholar]
- 6.Zhu Mj, Feng Hy, Qu Xm. The effect of different optical designs for orthokeratology in controling the development of myopia in pre-adolescents. Chinese Journal of ophthalmic optics and Visual Science. 2012;14(2):82–89. [Google Scholar]
- 7.Kang Pauline, Swarbrick Helen. The influence of different OK lens designs on peripheral refraction. Optom. Vis. Sci. 2016;93(9):1112–1119. doi: 10.1097/OPX.0000000000000889. [DOI] [PubMed] [Google Scholar]
- 8.Chen Ruru, Yu Jinjin, Lipson Michael, Cheema Abdullah A., Chen Yan, Lian Hengli, Huang Jinhai, McAlinden Colm. Comparison of four different orthokeratology lenses in controlling myopia progression. Contact Lens Anterior Eye. 2020;43:78–83. doi: 10.1016/j.clae.2019.11.012. [DOI] [PubMed] [Google Scholar]
- 9.Nakamura Y., Hieda O., Yokota I., Teramukai S., Sotozono C., Kinoshita S. Comparison of myopia progression between children wearing three types of orthokeratology lenses and children wearing single-vision spectacles. Jpn. J. Ophthalmol. 2021 Sep;65(5):632–643. doi: 10.1007/s10384-021-00854-4. [DOI] [PubMed] [Google Scholar]
- 10.Lu W., Ning R., Diao K., Ding Y., Chen R., Zhou L., Lian Y., McAlinden C., Sanders F.W.B., Xia F., Huang J., Jin W. Comparison of two Main orthokeratology lens designs in efficacy and Safety for myopia control. Front. Med. 2022 Apr 1;9 doi: 10.3389/fmed.2022.798314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wen D., Huang J., Chen H., et al. Efficacy and Acceptability of orthokeratology for slowing myopic progression in children: a Systematic review and Meta-analysis. J Ophthalmol. 2015 doi: 10.1155/2015/360806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pauné J., Fonts S., Rodríguez L., Queirós A. The Role of back optic zone diameter in myopia control with orthokeratology lenses. J. Clin. Med. 2021 Jan 18;10(2):336. doi: 10.3390/jcm10020336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guo B., Cheung S.W., Kojima R., Cho P. One-year results of the Variation of orthokeratology lens treatment zone (VOLTZ) study: a prospective randomised clinical trial. Ophthalmic Physiol. Opt. 2021 Jul;41(4):702–714. doi: 10.1111/opo.12834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loertscher M., Backhouse S., Phillips J.R. Multifocal orthokeratology versus Conventional orthokeratology for myopia control: a paired-eye study. J. Clin. Med. 2021 Jan 24;10(3):447. doi: 10.3390/jcm10030447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lau J.K., Wan K., Cho P. Orthokeratology lenses with increased compression factor (OKIC): a 2-year longitudinal clinical trial for myopia control. Cont Lens Anterior Eye. 2022 Aug 19 doi: 10.1016/j.clae.2022.101745. [DOI] [PubMed] [Google Scholar]
- 16.Wang B., Naidu R.K., Qu X. Factors related to axial length elongation and myopia progression in orthokeratology practice. PLoS One. 2017;12(4) doi: 10.1371/journal.pone.0175913. Published 2017 Apr 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qi Y., Liu L., Li Y., Zhang F. Factors associated with faster axial elongation after orthokeratology treatment. BMC Ophthalmol. 2022;22(1):62. doi: 10.1186/s12886-022-02294-1. Published 2022 Feb 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fu A.C., Chen X.L., Lv Y., et al. Higher spherical equivalent refractive errors is associated with slower axial elongation wearing orthokeratology. Cont Lens Anterior Eye. 2016;39(1):62–66. doi: 10.1016/j.clae.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Chen Z., Niu L., Xue F., et al. Impact of pupil diameter on axial growth in orthokeratology. Optom. Vis. Sci. 2012;89(11):1636–1640. doi: 10.1097/OPX.0b013e31826c1831. [DOI] [PubMed] [Google Scholar]
- 20.Wu P.C., Chen C.T., Lin K.K., et al. Myopia Prevention and outdoor light Intensity in a School-based Cluster Randomized trial. Ophthalmology. 2018;125(8):1239–1250. doi: 10.1016/j.ophtha.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 21.Wang A., Yang C. Influence of overnight orthokeratology lens treatment zone decentration on myopia progression. J Ophthalmol. 2019;2019 doi: 10.1155/2019/2596953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang S., Zhang H., Li L., Yang X., Li S., Li X. Effect of treatment zone decentration on axial length growth after orthokeratology. Front. Neurosci. 2022;16 doi: 10.3389/fnins.2022.986364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen R., Chen Y., Lipson M., et al. The effect of treatment zone decentration on myopic progression during or-thokeratology. Curr. Eye Res. 2020;45(5):645–651. doi: 10.1080/02713683.2019.1673438. [DOI] [PubMed] [Google Scholar]
- 24.Lin W., Gu T., Bi H., Du B., Zhang B., Wei R. The treatment zone decentration and corneal refractive profile changes in children undergoing orthokeratology treatment. BMC Ophthalmol. 2022;22(1):177. doi: 10.1186/s12886-022-02396-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marcotte-Collard R., Simard P., Michaud L. Analysis of two orthokeratology lens designs and comparison of their optical effects on the cornea. Eye Contact Lens. 2018;44(5):322–329. doi: 10.1097/ICL.0000000000000495. [DOI] [PubMed] [Google Scholar]
- 26.Sun L., Li Z.X., Chen Y., He Z.Q., Song H.X. The effect of orthokeratology treatment zone decentration on myopia progression. BMC Ophthalmol. 2022;22(1):76. doi: 10.1186/s12886-022-02310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vincent S.J., Cho P., Chan K.Y., et al. Clear - orthokeratology. Cont Lens Anterior Eye. 2021;44(2):240–269. doi: 10.1016/j.clae.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 28.Nti A.N., Berntsen D.A. Optical changes and visual performance with orthokeratology. Clin. Exp. Optom. 2020;103(1):44–54. doi: 10.1111/cxo.12947. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data associated with this study was not deposited into a publicly available repository, but the myopia data and corneal topography measurement results for all subjects at every visit can be found in a supplementary material named "raw data". Please correspond to the corresponding authors regarding the further information regarding the subjects.