Abstract
Background
Mass casualty incident (MCI) triage simulation is an increasingly useful tool for teaching triage systems to medical students, trainees, and hospital staff. MCI simulation in the prehospital setting has not yet been studied in this population.
Objectives/Aims
We aimed to assess the effectiveness of a prehospital MCI simulation in medical students, residents, and fellows. Our primary outcome was knowledge of the components of the triage algorithms used in MCI response. Our secondary outcome was each participant's confidence level if required to assist with or lead a MCI response.
Methods
This was an observational study with pre–post surveys. We recruited 30 medical students, 14 emergency medicine (EM) residents, and four pediatric EM fellows to fill out a survey before and after a 3‐h simulation session practicing the START and JumpSTART algorithms on two prehospital MCI scenarios.
Results
Overall, all groups demonstrated significant improvement in knowledge of triage colors, information needed to assign a triage color, pediatric airway management during a MCI, and indications for breaths‐first CPR. They also demonstrated significant increase in confidence both in assisting with and in leading a MCI response.
Conclusions
Simulated practice triaging patients in prehospital MCI scenarios improves knowledge of triage algorithms and increases confidence in assisting with or leading a MCI response in medical trainees.
Keywords: curriculum development, instruction/teaching strategies, learning environment, simulation, teamwork
INTRODUCTION/BACKGROUND
Mass casualty incident (MCI) triage simulation has been utilized for years to prepare hospital staff to respond to disaster‐level events, most often in emergency medicine (EM) training programs and within a hospital setting. 1 These simulations focus on hospital‐based interventions and resuscitation capabilities and may use institution‐specific triage algorithms. 2 This style of simulated triage and resuscitation, with consideration of available resources, has even developed into a competitive interprofessional event called SimWars. 3
Prehospital MCI simulation, in contrast, has historically been reserved for prehospital providers and nursing training programs 4 without inclusion in graduate medical education (GME). As GME providers are rarely deployed to the scene of an MCI, it follows that their educational focus is on the in‐hospital response rather than prehospital management unless in certain circumstances such as an emergency medical services rotation. In recent years prehospital MCI simulation has seen increased inclusion in medical student curricula, 5 , 6 typically utilizing the simple triage and rapid treatment (START) triage algorithm 7 in quiz format, whereby all patients are triaged by a single person. In a real‐life prehospital scenario, there may be multiple individuals participating in the triage process.
Additionally, MCIs in certain wilderness settings require additional triage considerations. Lightning strikes resulting in multiple casualties follow a reverse triage process 8 that is not typically included in triage algorithms. Wilderness incidents that may result in a primary respiratory arrest (lightning strike, avalanche burial, submersion) also warrant expeditious airway protection and emphasis on breaths‐first cardiopulmonary resuscitation (CPR). 9
The START and JumpSTART 10 algorithms utilize colored tags to label the severity of adult and pediatric patients, respectively, in a MCI. In a comparative analysis between triage systems, START has shown an 85% sensitivity for detecting critical injury in trauma patients. 11 JumpSTART has shown to be faster than the pediatric Sort, Assess, Lifesaving Interventions, and Treatment/Transport (SALT) algorithm, saving paramedics 8 s per patient in assigning a color designation. 12
To date, to our knowledge, there is no study comparing the efficacy of a prehospital simulation session on both knowledge and confidence with MCI triage or in learners of different levels (medical students, residents, and fellows). Our study aimed to introduce the START and JumpSTART algorithms to a mixed group of students, residents, and fellows at various training levels and assess their recall on the elements of the triage algorithms as well as their confidence in responding to an out‐of‐hospital MCI.
MATERIALS AND METHODS
Recruitment
Participants were invited to attend an event titled Outdoor SIM Day scheduled during the weekly conference for the EM residency program; this was also when graduating medical students had returned to campus for their residency preparation courses. EM residents, graduating fourth‐year medical students (MS4s), and pediatric EM (PEM) fellows were all invited to participate. This study was deemed exempt by the University of California San Diego Institutional Review Board.
Intervention
We hosted a 3‐h simulation session with pre‐ and postsession surveys assessing components of the START and JumpSTART algorithms as well as everyone's confidence in assisting with and leading a MCI response. During the session, participants were given a 15‐min introduction to the use of the triage systems following either a checklist listed on a commercial triage tag or a printed algorithm sourced from the U.S. Department of Health and Human Services website. Both formats were provided as there were insufficient triage tags for every participant. They were then divided into two groups to complete the first of two simulated scenarios (school bus crash and a boat collision). Each scenario lasted 15–20 min, followed by a 30‐min debrief reviewing the triage tags assigned and care provided during the scenario. Participants had a 10‐min break while switching to the next scenario.
Within each group, all participants were randomly assigned to be either a victim or a rescuer. Scenarios were designed to have 12–16 victims and a minimum of six rescuers with no maximum. Some participants were assigned to start out as a rescuer and then become a victim during the scenario, unbeknownst to the other rescuers. Participants were encouraged to switch roles in the following scenario to get experience as both a victim and a rescuer, although this was not enforced. Participants given a more passive role in the first scenario (i.e., black tag) were prioritized to receive a more active role in the following scenario if not switching into a rescuer role.
Each victim was given a card listing the victim's approximate age, complaint(s), physical examination finding(s) they had to act out, and the color triage tag they were to ultimately be assigned. If a rescuer had to perform an action (i.e., repositioning the airway) or assessment (i.e., ability to walk) to determine the triage category, this was also listed on the card for the victim to either act out or verbalize when performed or assessed (Figure 1). Rescuers were not allowed to see the victims' cards. Rescuers were allowed 5 min to prepare a strategy while victims were given moulage and props to help act out their assigned role. No leadership roles were preassigned, as the rescuers were instructed to formulate their plan of approach prior to starting and adapt it over the course of the scenario.
FIGURE 1.
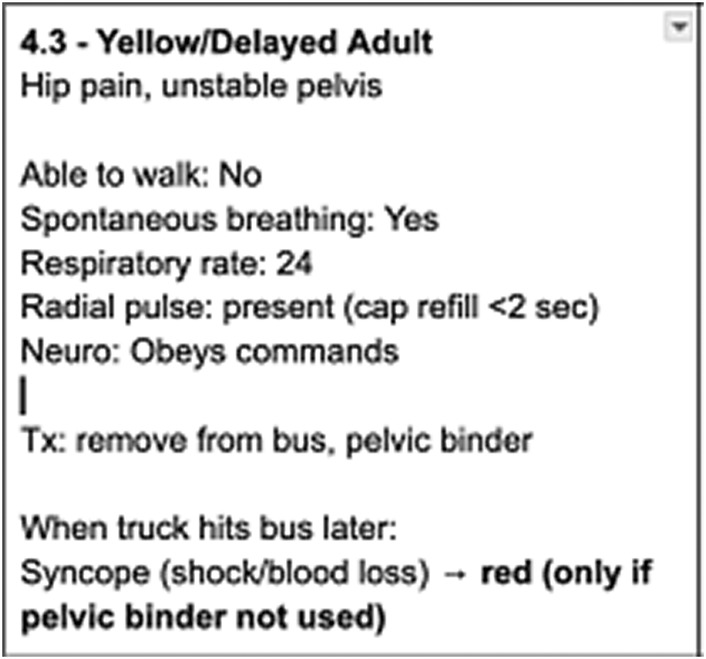
Sample card for victim assignment.
EM attending faculty with either pediatric or wilderness subspecialty training served as facilitators. Facilitators read each scenario from a script as well as standard instructions for rescuers on how to request examination finding that victims were unable to act out as well as how victims should respond (Appendix S1). One facilitator was assigned to time the scenario, as a major event occurs at the 10‐min mark. One facilitator played the role of dispatch and emergency medical personnel when they arrive on scene. One facilitator supervised any CPR interventions performed on mannequins. While CPR is generally discouraged during MCI triage and response, we wanted to provide mannequins as an option for any rescuer that felt compelled to initiate CPR on a victim. Any additional life‐ or limb‐saving interventions needed to be improvised from a small bag of medical supplies provided or anything the rescuers were actively wearing during the simulation. The medical supply bag included one emergency blanket, one moldable aluminum splint, one elastic bandage wrap, one Velcro tourniquet with a built‐in windlass, and three pieces of extra clothing including shirts and pants to be used for improvised splinting material or bleeding control.
At the end of each scenario, all victims, rescuers, and facilitators within the scenario huddled together for a group debrief (Appendix S2). Each victim was asked to explain what injury or problem they had; what actions, assessments, or treatments were performed on them; and what color triage tag they were assigned. As a group, the triage algorithm was reviewed and determined whether each victim was correctly assessed and triaged. If there was any discrepancy in what the victim received, this was reviewed and discussed as a group. The results of each of these were not recorded in the survey, as not all rescuers attended to all victims, and we anticipated that some victims would be triaged multiple times by different rescuers while others may not get triaged at all during the scenario. This was intentional to reflect the chaos and possibility of duplicate work and/or missed patients in a real‐life prehospital setting. Any field interventions applied were also reviewed as a group, and discussion on ways to improvise devices such as tourniquets, cervical collars, pelvic binders, and splints was reviewed.
After all the victims presented, the rescuers were asked to debrief the challenges they faced in their scenario, what they thought went well during the scenario, and how they felt working together as a team of mostly strangers. Each group then switched into the next scenario and repeated the process. After everyone had finished debriefing from the second scenario, participants were invited to fill out the postsession survey.
Data collection
Participants were invited to fill out an online survey using a QR code that assessed them on the components of the START and JumpSTART algorithms, indications for reverse triage in wilderness and austere environments, and their confidence assisting with and leading an MCI response. The same survey was distributed before and after the simulation session to assess changes in knowledge and confidence. Facilitators were excluded from the survey.
Data analysis
A sample size of 43 was calculated based on previous test score improvement in the McMains study with a goal improvement of 50% on the tests after our session with an alpha level of 0.05 and power size of 0.8. Paired t‐tests using an effect size of 0.5 and alpha of 0.05 were used to determine the mean change in each knowledge area and confidence levels. Questions that only had one correct answer were graded 0 for a wrong answer and 1 for a correct answer. Questions that had multiple correct answers were graded 1 point for each correct answer. Confidence scoring was assigned 0–4 points based on their selection of five different confidence levels.
RESULTS
Participants
Forty‐eight participants completed both the pre and post surveys before and after the session. This included 30 MS4s, 14 EM residents varying in postgraduate year (PGY) training (four PGY‐1, three PGY‐2, three PGY‐3, four PGY‐4), and four PEM fellows. Seven (two students, three residents, and two fellows) had previously participated in a MCI drill; four (one student, two residents, one fellow) of those drills were in a wilderness setting. Two (one student, one fellow) had previously participated in an actual MCI in a hospital.
Knowledge areas
Participants were asked to answer the following questions:
What is the definition of a MCI? (scored 0 or 1)
What are the colors used in MCI triage? (scored 0 or 1)
What information do you need to triage a patient in a MCI? (scored 0–6)
What is reverse triage? (scored 0 or 1)
What airway maneuver should you perform in pediatric patients with a pulse but without spontaneous breathing before assigning a triage color? (scored 0 or 1)
Under what circumstances should you perform CPR with breaths first? (scored 0–3)
These questions were based on the learning outcomes from the course plan of the MCI exercise included in our institution's wilderness medicine elective.
The mean (±SD) survey score on the definition of an MCI was 0.6 (±0.5) before the session and 0.7 (±0.4) after the session, with a mean change of 0.1 (16%; t(47) = 1.7, p = 0.090, 95% CI −0.32 to 0.02). The mean (±SD) survey score on the four triage colors was 0.3 (±0.5) before the session and 0.9 (±0.3) after the session, with a mean change of 0.6 (200%; t(47) = 7.8, p < 0.001, 95% CI −0.71 to −0.42). The mean (±SD) survey score on the information needed to assign a triage color was 3.7 (±1.3) before the session and 4.9 (±1.2) after the session, with a mean change of 1.2 (32%; t(47) = 5.8, p < 0.001, 95% CI −1.54 to −0.75). The mean (±SD) survey score for the definition of reverse triage was 0.5 (±0.5) before the session and 0.6 (±0.5) after the session, with a mean change of 0.1 (20%; t(47) = 0.8, p = 0.42, 95% CI −0.29 to 0.12). The mean (±SD) survey score on the management of a pediatric airway during an MCI was 0.2 (±0.4) before the session and 0.9 (±0.3) after the session, with a mean change of 0.7 (350%; t(47) = 9, p < 0.001, 95% CI −0.87 to −0.55). The mean (±SD) survey score on indications for breaths‐first CPR was 1.0 (±0.7) before the session and 2.2 (±1) after the session, with a mean change of 1.1 (120%; t(47) = 8.4, p < 0.001, 95% CI −1.52 to −0.93). Mean differences pre‐ and postsession for each subgroup (medical students, residents, and fellows) are summarized in Table 1.
TABLE 1.
Change in knowledge by training level.
| Medical students | Residents | Fellows | |
|---|---|---|---|
| Definition of a MCI | |||
| Pre | 0.4 ± 0.5 | 0.9 ± 0.4 | No change |
| Post | 0.7 ± 0.5 | 0.7 ± 0.5 | |
| Change |
Δ = 0.3 b , 75% t(29) = 2.8 p = 0.010 95% CI 0.52 to −0.08 |
Δ = −0.2, −22% t(13) = 1.0 p = 0.336 95% CI −0.17 to 0.45 |
|
| Triage colors | |||
| Pre a | 0.1 ± 0.3 | 0.6 ± 0.5 | No change |
| Post a | 0.8 ± 0.4 | 1.0 ± 0 | |
| Change |
Δ = 0.7 b , 700% t(29) = 8.9 p < 0.001 95% CI −0.90 to −0.57 |
Δ = 0.4 b , 40% t(13) = 2.7 p = 0.019 95% CI −0.64 to −0.07 |
|
| Information to triage | |||
| Pre a | 3.6 ± 1.4 | 3.6 ± 1.2 | 4.8 ± 1.5 |
| Post a | 5.0 ± 1.2 | 4.6 ± 1.1 | 4.5 ± 1.3 |
| Change |
Δ = 1.4 b , 39% t(29) = 5.8 p < 0.001 95% CI −1.90 to −0.90 |
Δ = 1 b , 28% t(13) = 2.6 p = 0.020 95% CI −1.82 to −0.18 |
Δ = −0.3, −6% t(3) = 1.0 p = 0.391 95% CI −0.55 to 1.05 |
| Reverse triage definition | |||
| Pre a | 0.6 ± 0.5 | 0.4 ± 0.5 | 0.5 ± 0.6 |
| Post a | 0.5 ± 0.5 | 0.7 ± 0.5 | 0.8 ± 0.5 |
| Change |
Δ = −0.1, −17% t(29) = 0.2 p = 0.813 95% CI −0.25 to 0.32 |
Δ = 0.3, 75% t(13) = 1.7 p = 0.104 95% CI −0.64 to 0.07 |
Δ = 0.3, 60% t(3) = 1 p = 0.391 95% CI −1.05 to 0.55 |
| Pediatric airway maneuver | |||
| Pre a | 0.1 ± 0.4 | 0.3 ± 0.5 | 0.5, SD =0.6 |
| Post a | 0.9 ± 0.3 | 0.9 ± 0.3 | 1.0 ± 0 |
| Change |
Δ = 0.8 b , 800% t(29) = 7.4 p < 0.001 95% CI −0.98 to −0.55 |
Δ = 0.6 b , 200% t(13) = 4.8 p < 0.001 95% CI −0.93 to −0.36 |
Δ = 0.5, 100% t(3) = 1.7 p = 0.182 95% CI −1.42 to 0.42 |
| Indication for breaths‐first CPR | |||
| Pre a | 0.9 ± 0.7 | 1.1 ± 0.8 | 0.8 ± 0.5 |
| Post a | 2.1 ± 1.1 | 2.5 ± 0.8 | 2.3 ± 1.0 |
| Change |
Δ = 1.2 b , 133% t(29) = 5.5 p < 0.001 95% CI −1.56 to −0.71 |
Δ = 1.4 b , 127% t(13) = 8.0 p < 0.001 95% CI −1.72 to −0.99 |
Δ = 1.5, 188% t(3)=2.3 p = 0.103 95% CI −3.55 to 0.55 |
Abbreviation: MCI, mass casualty incident.
Mean ± SD.
Statistically significant change.
Confidence
Participants were given the following five categories to choose when selecting their confidence level in assisting with or leading a MCI response:
NO for “I would run the other way.” (score = 0)
UNSURE for “I would need someone to tell me what to do.” (score = 1)
MAYBE for “I could probably help with some guidance.” (score = 2)
YES for “I know what to do in most situations.” (score = 3)
DEFINITELY for “I can confidently handle any scenario.” (score = 4)
The mean (±SD) confidence score when asked to assist with a MCI was 1.5 (±0.9) before the session and 2.7 (±0.6) after the session, with a mean change of 1.2 (80%; t(47) = 8.9, p < 0.001, 95% CI −1.43 to −0.90). The mean (±SD) confidence score when asked to lead a MCI was 0.9 (±0.9) before the session and 2.2 (±0.8) after the session, with a mean change of 1.3 (144%), t(47) = 8.7, p < 0.001, 95% CI −1.67 to −1.04). The changes in confidence scores by subgroup analysis of training level are summarized in Table 2. The pre‐ and postsession confidence levels are summarized in Figure 2.
TABLE 2.
Change in confidence by training level.
| Medical students | Residents | Fellows | |
|---|---|---|---|
| Assisting with a MCI response | |||
| Pre a | 1.2 ± 0.8 | 2 ± 1 | 2.3 ± 0.5 |
| Post a | 2.6 ± 0.6 | 2.9 ± 0.5 | 2.8 ± 0.5 |
| Change |
Δ = 1.4 b , 117% t(29) = 9.3 p < 0.001 95% CI −1.67 to −1.06 |
Δ = 0.9 b , 45% t(13) = 3.2 p = 0.006 95% CI −1.55 to −0.31 |
Δ = 0.5, 22% t(3) = 1.7 p = 0.182 95% CI −1.42 to 0.42 |
| Leading a MCI response | |||
| Pre a | 0.6 ± 0.7 | 1.2 ± 1.3 | 1.5 ± 0.6 |
| Post a | 2.0 ± 0.7 | 2.5 ± 0.9 | 2.8 ± 0.5 |
| Change |
Δ = 1.4 b , 233% t(29) = 7.6 p < 0.001 95% CI −1.77 to −1.03 |
Δ = 1.3 b , 108% t(13) = 3.5 p = 0.004 95% CI −2.08 to −0.49 |
Δ = 1.3 b , 87% t(3) = 5 p = 0.015 95% CI −2.05 to −0.45 |
Abbreviation: MCI, mass casualty incident.
Mean ± SD.
Statistically significant change.
FIGURE 2.
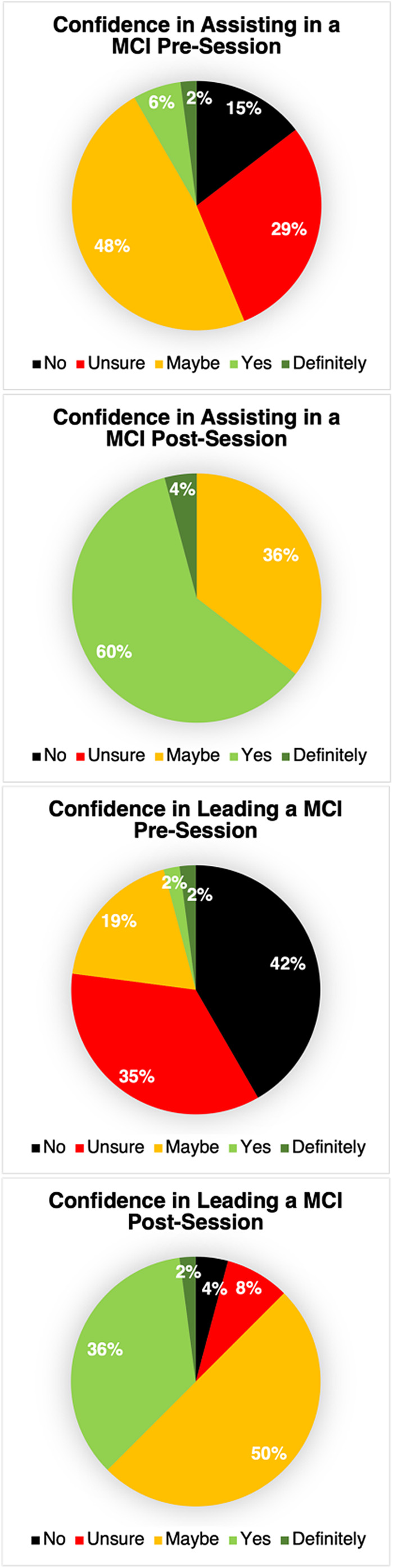
Aggregate confidence levels pre‐ and postsession. MCI, mass casualty incident.
DISCUSSION
After a 3‐h simulation session introducing the START and JumpSTART algorithms, MS4s, EM residents, and PEM fellows demonstrated a significant increase in knowledge of the triage colors, information needed to assign a triage color, pediatric airway maneuvers to employ during triage, and indications for breaths‐first CPR. The areas of the greatest increase were the triage colors (200%) and pediatric airway maneuver during JumpSTART triage (350%); these are core components of the algorithms that are clearly printed on commercial triage tags. There was a modest (32%) increase in recall of the information needed to assign a triage color. However, it likely was difficult to remember all the components of the algorithm without the aid of a tag or printout available, thereby highlighting the importance of having those resources readily available in the event of an incident.
There was a trend toward increased knowledge on the definition of a MCI and the definition of reverse triage that did not reach statistical significance. These were the two categories that were not practiced during the scenarios compared to the other knowledge areas; they were only reviewed in the introduction to the session and are not on the triage tags or in the printed algorithm.
On subgroup analysis, medical students showed statistically significant improvement in all knowledge areas except for the definition of reverse triage. They were also the only subgroup that showed a significant increase in the definition of a MCI. This is likely because EM trainees are exposed to this terminology during their residency, but MCI response is not a part of standard medical school curriculum. Only 10% of medical students and 21% of residents had any previous MCI practice. The percentage improvement in the residents' knowledge was less than the medical students' in all categories, suggesting that elements of MCI triage are taught over the progression of medical training even in the absence of drills. Fellows showed no change in their knowledge of the definition of a MCI or the triage colors and no statistically significant change in any other knowledge categories. This was likely due to the small sample size. Additionally, three (75%) of them had previously either participated in a MCI drill or actual MCI response.
Residents and fellows showed the most improvement in pediatric airway maneuver and indications for breaths‐first CPR. This could be because they were exposed to adult triage algorithms in the past but not pediatric algorithms. Additionally, they may not have had prior experience in prehospital MCI where the environmental factors of drowning, avalanche burial, or lightning strike were relevant for breaths‐first CPR.
This study also shows that an out‐of‐hospital in situ simulation with no previously established leadership roles results in a statistically significant increase in confidence in both assisting with and leading a MCI response. On subgroup analysis, medical students and residents demonstrate increased confidence in both circumstances while fellows only demonstrated a statistically significant increase in confidence with leading a MCI response. This could again be due to the small sample size of fellows or because most of them had previous experience with MCI response.
LIMITATIONS/FUTURE AVENUES
The participants in this study were recruited on a voluntary basis and may have self‐selected due to intrigue from the title of the educational event for the day. Knowledge base and confidence findings observed may have been different if it was a required session or included a larger number of participants. Participants were composed primarily of MS4s and EM residents, with only four PEM fellows participating. This limits our evaluation of fellows or residents from other specialties. In future studies, we could consider recruiting fellows from other EM subspecialties and/or residents from other specialties. Additionally, we could include a lightning strike scenario to have participants practice reverse triage.
The participants were surveyed only immediately before and after the session to assess their knowledge and confidence. While prior studies have included follow‐up surveys at various intervals, this was not part of our study. Therefore, we cannot assess the retention of the knowledge or confidence in the weeks or months following our simulation session.
CONCLUSIONS
Prehospital mass casualty incident triage is not commonly taught to medical students or trainees, who typically only get triage practice within a hospital setting. This study proves that prehospital simulation practicing the START and JumpSTART algorithms is effective in improving knowledge of the components of the algorithms but does not place enough emphasis on definitions of mass casualty incident or reverse triage. Additionally, confidence in assisting with or leading a mass casualty incident response can be significantly improved after a simulation session, thereby proving its value in medical education.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Supporting information
Appendix S1.
Appendix S2.
Yu E, Coffey C. Prehospital mass casualty incident triage simulation builds knowledge and confidence in medical trainees. AEM Educ Train. 2024;8:e10962. doi: 10.1002/aet2.10962
Supervising Editor: Daniel P Runde
REFERENCES
- 1. Walker A, Elahi N, Tassone M, Littell J, Ganti L. Residency exposure to emergency medical services concepts through immersion, interprofessional collaboration and assembly line education. Cureus. 2021;13(12):e20470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Musisca NJ, Rybasack‐Smith H, Musits A, et al. Multiple hospital in‐situ mass casualty incident training simulation for emergency medicine residents: a sarin bomb scenario. R I Med J. 2023;106(9):36‐40. [PubMed] [Google Scholar]
- 3. Bentley S, Iavicoli L, Boehm L, et al. A simulated mass casualty incident triage exercise: SimWars. MedEdPORTAL. 2019;15:10823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McCrea DL, Coghlan RC, Champagne‐Langabeer T, Cron S. Collaborative interprofessional health science student led realistic mass casualty incident simulation. Healthcare. 2023;11(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McMains JC, Larkins MC, Doherty AM, et al. Knowledge retention from emergency medicine simulation‐based learning curriculum for pre‐clinical medical students. Cureus. 2023;15(6):e41216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gable BD, Misra A, Doos DM, Hughes PG, Clayton LM, Ahmed RA. Disaster day: a simulation‐based disaster medicine curriculum for novice learners. J Med Educ Curric Dev. 2021;8:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Benson M, Koenig KL, Schultz CH. Disaster triage: START, then SAVE—a new method of dynamic triage for victims of a catastrophic earthquake. Prehosp Disaster Med. 1996;11(2):117‐124. [DOI] [PubMed] [Google Scholar]
- 8. Davis C, Engeln A, Johnson EL, et al. Wilderness Medical Society practice guidelines for the prevention and treatment of lightning injuries: 2014 update. Wilderness Environ Med. 2014;25(4 Suppl):S86‐S95. [DOI] [PubMed] [Google Scholar]
- 9. Vanden Hoek TL, Morrison LJ, Shuster M, et al. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S829‐S861. [DOI] [PubMed] [Google Scholar]
- 10. Romig LE. Pediatric triage. A system to JumpSTART your triage of young patients at MCIs. JEMS. 2002;27(7):52‐58, 60–63. [PubMed] [Google Scholar]
- 11. Garner A, Lee A, Harrison K, Schultz CH. Comparative analysis of multiple‐casualty incident triage algorithms. Ann Emerg Med. 2001;38(5):541‐548. [DOI] [PubMed] [Google Scholar]
- 12. Jones N, White ML, Tofil N, et al. Randomized trial comparing two mass casualty triage systems (JumpSTART versus SALT) in a pediatric simulated mass casualty event. Prehosp Emerg Care. 2014;18(3):417‐423. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1.
Appendix S2.


