Abstract
Cognition and behavior could reciprocally impact each other and together determine mental health amid large-scale disasters such as COVID-19. This study reports a six-month cohort study of a population-representative sample of Hong Kong residents (N = 906) from March–August 2021 (T1) to September 2021–February 2022 (T2). Cross-lagged panel analyses reveal that T1 poor behavioral functioning as indicated by high daily routine disruptions is inversely associated with T2 cognitive adaptation as indicated by self-efficacy and meaning-making but not vice versa. T1 routine disruptions but not cognitive adaptation are positively associated with T2 probable depression/anxiety. The positive link between T1 routine disruptions and T2 probable disorders is mediated by poor cognitive adaptation at T2. The present findings suggest that upholding daily behavioral functioning relative to positive states of mind could have a more pivotal role in mental health amid large-scale disasters. Future studies can test interventions that enhance the sustainment of regular daily routines.
Subject terms: Psychiatric disorders, Risk factors, Human behaviour, Epidemiology
Introduction
Cognitive and behavioral aspects of adaptation are considered targets of modification and essential for building strengths and determining mental health1 across different levels of social, behavioral, cognitive, and neurobiological functioning for adaptive adjustment2. These factors do not exhibit their effects in isolation, because changes in some core factors will positively influence other related factors3 and together improve adaptation outcomes. There is a need to investigate and compare protective cognitive and behavioral factors for population mental health assessment and intervention under large-scale disasters.
The Conservation of Resources (COR) theory suggests that resource change dictates mental health in stress adaptation4. Ongoing demands are offset by mobilizing at least three types of resources, namely personal (e.g., personalities and self-concepts that are integral to oneself), social (e.g., social support and relationship quality), and material (e.g., money or tangible belongings that could be utilized) resources.
Cognitive adaptation is the attempt to engage in cognitively adaptive efforts that enable individuals to resume and go beyond pre-existing levels of functioning in response to setbacks and tragedies5,6. Both theoretical and empirical literature suggested that perceived self-efficacy and life meaning as examples of cognitive adaptation predict adaptive behavioral adjustment and better mental health. Self-efficacy denotes confidence in one’s capability to cope with stressors7 and relates to increased levels of physical activity in adaptation to chronic stressors such as medical conditions8 and low socioeconomic status9. Among the general population, individuals with higher self-efficacy were found to report better sleep hygiene and fewer sleep problems10 and perform more oral health care behaviors11. Meaning in life denotes a sense of feeling that one’s life is significant, purposeful, and coherent12. Awareness of meaning in life has been suggested to activate self-regulatory processes that enhance physical and psychological health13. People with cardiovascular disease who had higher levels of meaning in life also reported higher levels of health awareness and positive lifestyle such as smoking cessation and body weight management14.
There is a concurrent body of evidence suggesting the adaptive priority of behavioral processes. The social zeitgeber model proposed that daily activities (e.g., social contact, meal/bedtime, work/studies, leisure) are regularized to form social rhythms that maintain physical and mental health under normal circumstances and reduce the risk of severe mental health problems such as bipolar disorder15. The Drive to Thrive (DTT) theory similarly argued that sustainment of regular daily routines is one of the core processes that contribute to psychological resilience (i.e., non-significant psychological distress or psychiatric symptoms over time) across trauma and chronic stress conditions16.
Data from experience sampling methodology further revealed that more regular daily routines were associated with higher levels of meaning in life, suggesting that everyday activities provide contexts and pathways towards desired goals and a sense of fulfillment in the long run12. Regularities in basic daily activities have also been found to predict higher levels of sleep efficacy, which in turn were associated with lower depressive and anxiety symptoms17. Engagement in leisure activities was inversely associated with depressive symptoms through increased perceptions of predictability, controllability, and meaningfulness18. Regularity per se could be more strongly associated with cognitive and emotional adaptation, for sustainment of regular routines could build an overall well-structured daily life that effectively buffers individuals from the negative mental health impact of stressful events16.
Beyond determining the adaptive priority between cognitive and behavioral processes leading to psychological resilience, theoretical and empirical evidence also points to possible reciprocal facilitation between the two processes. Mental health outcomes can be seen as a product of orchestrated effects of various resilience factors3. These factors exist within an interrelated system where they form positive mutual connections and enhancements critical to adaptive psychological adjustment. The process of resilience is therefore also the process of accumulation and optimization of resilience factors2.
In a similar vein, persons with more resources tend to experience resource gain, while persons with fewer resources are more likely to suffer from resource loss4. Resource caravan passageways refer to contexts that enrich, foster, and conserve coping resources, or reduce, deter, and deplete resources, depending on whether individuals are able to maintain or create the contexts that are conducive to resource gain19. Resource multiplication theory also suggested that the positive association between socioeconomic resources such as education and mental health is stronger for individuals with more resources20. Individuals who are more advantaged, relative to those who are not, are more likely to experience a larger benefit of coping resources on their mental health. Recovery and sustainability have further been suggested to be two parallel aspects of human stress resilience21. Recovery refers to the capacity to recover from negative psychophysiological sequelae brought about by stressful events, whereas sustainability refers to the capacity to maintain or gain positive physical and psychological health over the course of adaptation. The recovery and sustainability pathways interact with each other while developing independently in a stress process22. To our knowledge, most existing cross-sectional and prospective studies on cognitive and/or behavioral processes in stress adaptation were conducted with the assumption of a unidirectional – not bidirectional – sequential pathway between the two processes. A more holistic approach to investigating resilience factors is warranted and will likely generate important insights.
A meta-analysis was conducted on 66 studies (221,970 respondents) and concluded that the pandemic was responsible for a pooled prevalence of 30–40% for common mental health problems such as depression, anxiety, insomnia, and general distress in the acute phase across different populations23. Cognitive adaptation has been associated with lower levels of depressive and anxiety symptoms in COVID-1924. Such personal resources are particularly important to mental health under COVID-19, when social resources are limited by infection control rules such as lockdown and quarantine25. Amid COVID-19, both self-efficacy and meaning in life have been positively related to engagement in health-protective behaviors26,27, suggesting that resources on different levels could collectively influence behavioral outcomes. During lockdown, structured daily routines such as regularized physical activities buffered individuals of depressive, anxiety, and stress symptoms and negative affect28. On the flip side, loss of the original work, exercise, and social schedules was found to compromise coping abilities, which in turn was associated with more emotional symptoms and poorer psychological well-being29.
This study aims to investigate the interrelations between cognitive and behavioral processes and their associations with mental health outcomes in a prospective population-representative cohort in Hong Kong during COVID-19. We hypothesized that cognitive adaptation and daily routine disruptions will be inversely associated with each other both concurrently and prospectively. Cognitive adaptation will be negatively associated whereas routine disruptions will be positively associated with probable psychiatric conditions. We also tested the mediating effects of cognitive adaptation and routine disruptions in the associations of each other with the outcomes.
Methods
Respondents and procedure
This prospective study collected population-representative data at two time points, with a follow-up duration of six months for all respondents (T1 = March–August 2021, T2 = September 2021–February 2022). The methods were performed in accordance with relevant guidelines and regulations and approved by the Ethics Review Committee of The Education University of Hong Kong (2019–2020–0224 and 2020–2021–0277). Telephone surveys were conducted among Hong Kong Chinese aged ≥15 years by interviewers who had received prior formal training. Oral informed consent was obtained from each participant prior to the survey. The sampling procedure of the current study closely followed that of other large-scale local prospective cohort studies. The final sample included 906 individuals. The cooperation (eligible individuals invited) and response (invited individuals complying with acceptable standards) rates at T2 (98.48% and 68.64%) were good30 (Supplementary Notes1–2). All analyses were weighted to account for non-response. All respondents received supermarket coupons with a face value HK$100 (≈US$13) as compensation for participation.
Measures
Cognitive adaptation
Cognitive adaptation consisted of self-efficacy and meaning-making for their relations to adaptive behavioral adjustment and better mental health under large-scale disasters. Self-efficacy was measured using the Chinese version of the 6-item General Self-Efficacy Scale (GSE-6)31. Respondents rated their perceived ability to take control under stressful conditions over the past month on a 4-point Likert scale (1 = strongly disagree, 4 = strongly agree). Meaning-making was measured with the Positive Reinterpretation and Growth subscale on the COPE32 and the Emotional Processing Scale33 based on previous studies34. The Positive Reinterpretation and Growth subscale consisted of four items regarding one’s tendency to approach situations in a positive way, while the Emotional Processing Scale consisted of four items concerning one’s attempts to understand their own emotional reactions to situations. Respondents rated each item on a 4-point Likert scale (1 = not at all, 4 = always) with reference to their experience in the past month. We conducted confirmatory factor analysis (CFA) to evaluate the structural validity of this single composite measure (Supplementary Note 3). Cronbach’s αs were 0.888 and 0.871 at T1 and T2, respectively, suggesting good internal consistency of the items.
Disruptions to primary and secondary routines
Daily routine disruptions were measured with eight items on the Sustainability of Living Inventory (SOLI)35,36, four measuring primary routines (i.e., hygiene, eating, sleep, duties at home) and four measuring secondary routines (i.e., leisure at home, exercising, social activities, work/study involvement). Respondents indicated how much the regularity of each behavior was disrupted over the past two weeks on an 11-point scale (0 = no disruptions, 10 = high level of disruptions). Mean scores were calculated for primary and secondary routines, and then summed to generate a total score, with higher scores indicating higher levels of disruptions. CFA was conducted on the routine items to test the model fit of the single-factor model (Supplemental Note 3). Internal consistency of the items was good over time (T1: α = 0.804; T2: α = 0.811).
Probable depression
Depressive symptoms were assessed using the 9-item Patient Health Questionnaire (PHQ-9)37. Respondents indicated on a 4-point scale (0 = not at all, 1 = on several days, 2 = on more than half of the days, 3 = nearly every day) the frequency of experiencing depressive symptoms over the past two weeks. Higher total scores indicated greater severity of depressive symptoms (range = 0–27). PHQ-9 showed high internal consistency at T1 (α = 0.885) and T2 (α = 0.880) administrations. A cut-off score of 10 was adopted to indicate probable depression and recode the scores into a dichotomized scale (1 = yes, 0 = no)38.
Probable anxiety
Anxiety symptoms were assessed using the 7-item Generalized Anxiety Disorder scale (GAD-7)39. Respondents indicated the frequency they experienced anxiety symptoms over the past two weeks on a 4-point scale (0 = not at all, 1 = on several days, 2 = on more than half of the days, 3 = nearly every day). A total score was calculated, with higher scores indicating greater severity of anxiety symptoms (range = 0–21). The GAD-7 showed high internal consistency at T1 (α = 0.934) and T2 (α = 0.940) administrations. A cut-off score of 10 was used to indicate probable anxiety and recode the scores into a dichotomized scale (1 = yes, 0 = no)40.
Demographics
At T1, gender, age, marital status, education level, employment status, and monthly household income were recorded.
Statistical analysis
All missing data (<1%) were handled with multiple imputation. For cognitive adaptation, scores on self-efficacy and meaning-making were standardized and averaged to indicate cognitive adaptation, whereas for routine disruptions, scores on disrupted primary and secondary routines were summed and standardized to indicate overall daily routine disruptions22. Cognitive adaptation and routine disruptions were then recoded into two groups (1 = high, 0 = low) following median split. At both T1 and T2, correlations between cognitive adaptation and daily routine disruptions were comparable with or lower than those between self-efficacy and meaning-making and between primary and secondary routine disruptions, suggesting empirical divergence between cognitive adaptation and overall routine disruptions.
Two cross-lagged panel models were constructed for probable depression and probable anxiety within Mplus (Version 8.3). In each model, we tested the concurrent and prospective associations between cognitive adaptation, daily routine disruptions, and probable psychiatric conditions at T1 and T2, controlling for sociodemographic covariates. Directional relationships were inferred statistically in the presence of cross-lagged effects, that is, when the coefficient for the parameter linking a variable X1 at T1 with another variable Y2 at T2 was significantly different from zero. The temporal ordering of the three variables was inferred in the presence of simultaneous consideration of potential reciprocal cross-lagged effects (i.e., through comparing the coefficients for parameters for both X1 to Y2 and Y1 to X2) as well as the stability of each variable itself over time within autoregressive pathways (i.e., from X1 to X2).
To establish mediating effects, two additional sets of path analyses were conducted, testing whether T2 routine disruptions (or cognitive adaptation) mediated the prospective associations between T1 cognitive adaptation (or routine disruptions) and T2 probable psychiatric conditions. T1 probable psychiatric condition and sociodemographic covariates were adjusted for. In both cross-lagged panel and path analyses, the weighted least square mean and variance adjusted (WLSMV) estimator were used, whereas model fit was assessed by a combination of residual mean squared error of approximation (RMSEA) (<0.08), standardized root mean square residual (SRMR) (<0.08), comparative fit index (CFI) (>0.90), and Tucker-Lewis index (TLI) (>0.90)41. Sensitivity analyses were conducted adopting continuous variables for all main analyses.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Results
Respondents and Prevalence
Demographics of the respondents (N = 906) are summarized in Table 1. The prevalences of probable depression (i.e., PHQ-9 ≥ 10) and anxiety (i.e., GAD-7 ≥ 10) were 21.41% and 17.11% at T1, and 24.94% and 18.98% at T2.
Table 1.
Descriptive characteristics of the current sample.
| Variable | n | % |
|---|---|---|
| Gender | ||
| Male | 468 | 51.66 |
| Female | 438 | 48.34 |
| Age | ||
| 65 or above | 112 | 12.36 |
| 55–64 | 102 | 11.26 |
| 45–54 | 118 | 13.02 |
| 35–44 | 183 | 20.20 |
| 25–34 | 226 | 24.94 |
| 15–24 | 165 | 18.21 |
| Marital status | ||
| Married | 433 | 47.79 |
| Single/divorced/widowed | 473 | 52.21 |
| Education | ||
| Tertiary or above | 586 | 64.68 |
| Secondary | 284 | 31.35 |
| Primary or below | 36 | 3.97 |
| Employment | ||
| Employed | 630 | 69.54 |
| Unemployed/dependent | 276 | 30.46 |
| Monthly household income | ||
| 80,000 or above | 116 | 12.80 |
| 60,000–79,999 | 102 | 11.26 |
| 40,000–59,999 | 187 | 20.64 |
| 20,000–39,999 | 247 | 27.26 |
| 19,999 or below | 254 | 28.04 |
| T1 Cognitive adaptation | ||
| Low | 432 | 47.68 |
| High | 474 | 52.32 |
| T2 Cognitive adaptation | ||
| Low | 430 | 47.46 |
| High | 476 | 52.54 |
| T1 Routine disruptions | ||
| Low | 453 | 50.00 |
| High | 453 | 50.00 |
| T2 Routine disruptions | ||
| Low | 437 | 48.23 |
| High | 469 | 51.77 |
| T1 Probable depression | ||
| No | 712 | 78.59 |
| Yes | 194 | 21.41 |
| T2 Probable depression | ||
| No | 680 | 75.06 |
| Yes | 226 | 24.94 |
| T1 Probable anxiety | ||
| No | 751 | 82.89 |
| Yes | 155 | 17.11 |
| T2 Probable anxiety | ||
| No | 734 | 81.02 |
| Yes | 172 | 18.98 |
US$1 ≈ HK$7.80. Cognitive adaptation is a composite index constituting self-efficacy and meaning-making; Low vs. high groups were categorized based on median split. Routine disruptions is a composite index constituting disruptions to primary and secondary routines; Low vs. high groups were categorized based on median split. Probable depression was defined by scores of 10 or above on the 9-item Patient Health Questionnaire (PHQ-9). Probable anxiety was defined by scores of 10 or above on the 7-item Generalized Anxiety Disorder scale (GAD-7).
Cross-lagged panel analyses
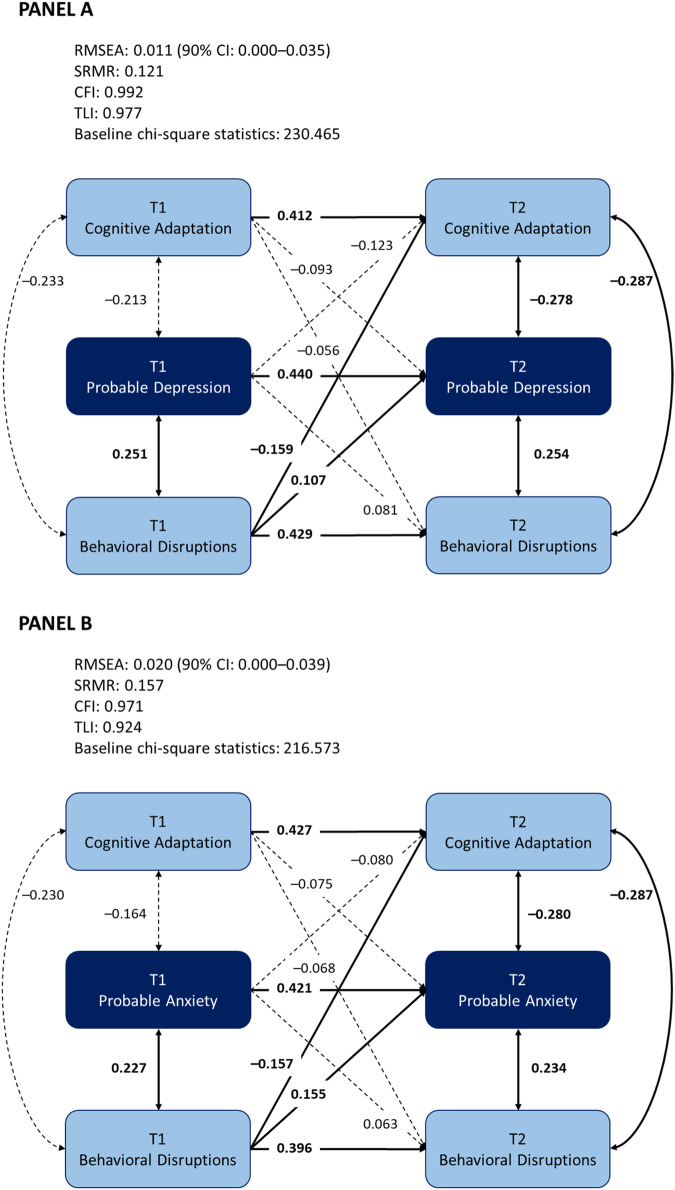
Figure 1 presents the cross-lagged models of cognitive adaptation, routine disruptions, and probable depression and anxiety.
Fig. 1. Cross-lagged panel model for cognitive adaptation, routine disruptions, and psychopathology.
A Probable depression. B Probable anxiety. Cognitive adaptation included self-efficacy and meaning-making; routine disruptions included primary and secondary routine disruptions. Demographics covariates were adjusted for in the cross-lagged panel model. The full figure including demographics covariates is available from the corresponding author.
The model for probable depression demonstrated good data-model fit (RMSEA = 0.011, 90% CI [0.000, 0.035], SRMR = 0.121, CFI = 0.992, TLI = 0.977). All autoregressive paths were statistically significant (ps ≤ 0.024). The cross-lagged paths were significant between T1 routine disruptions and T2 cognitive adaptation (β = –0.159, 95% CI [–0.312, –0.006], p = 0.042) and between T1 routine disruptions and T2 probable depression (β = 0.107, 95% CI [0.010, 0.204], p = 0.030). The cross-lagged paths were not significant between T1 cognitive adaptation and T2 routine disruptions (β = –0.056, 95% CI [–0.152, 0.040], p = 0.256) or T2 probable depression (β = –0.093, 95% CI [–0.213, 0.027], p = 0.128), or between T1 probable depression and T2 cognitive adaptation (β = –0.123, 95% CI [–0.272, 0.025], p = 0.103) or routine disruptions (β = 0.081, 95% CI [–0.014, 0.176], p = 0.093). Detailed statistical results are summarized in Table 2. Results of the sensitivity analysis based on continuous variables are presented in Supplementary Table 1.
Table 2.
Cross-lagged analyses examining the autoregressive and cross-lagged effects of cognitive adaptation, routine disruptions, and probable depression.
| Effect | Variables | β [95% CI] |
|---|---|---|
| Autoregressive | T1 Cognitive adaptation → T2 Cognitive adaptation | 0.412 [0.054, 0.771]* |
| T1 Routine disruptions → T2 Routine disruptions | 0.429 [0.254, 0.604]*** | |
| T1 Probable depression → T2 Probable depression | 0.440 [0.352, 0.528]*** | |
| Cross-lagged | T1 Cognitive adaptation → T2 Routine disruptions | –0.056 [–0.152, 0.040] |
| T1 Routine disruptions → T2 Cognitive adaptation | –0.159 [–0.312, –0.006]* | |
| T1 Cognitive adaptation → T2 Probable depression | –0.093 [–0.213, 0.027] | |
| T1 Routine disruptions → T2 Probable depression | 0.107 [0.010, 0.204]* | |
| T1 Probable depression → T2 Cognitive adaptation | –0.123 [–0.272, 0.025] | |
| T1 Probable depression → T2 Routine disruptions | 0.081 [–0.014, 0.176] |
*p < 0.050, *** p < 0.001.
Probable depression was defined by scores of 10 or above on the 9-item Patient Health Questionnaire (PHQ-9); Cognitive adaptation and routine disruptions were binary variables (based on median split). Results of the sensitivity analysis based on continuous variables are presented in Supplementary Table 1.
Similarly, the model for probable anxiety demonstrated good data-model fit (RMSEA = 0.020, 90% CI [0.000, 0.039], SRMR = 0.157, CFI = 0.971, TLI = 0.924). All autoregressive paths were statistically significant (ps ≤ 0.011). The cross-lagged paths were significant between T1 routine disruptions and T2 cognitive adaptation (β = –0.157, 95% CI [–0.296, –0.018], p = 0.027), and between T1 routine disruptions and T2 probable anxiety (β = 0.155, 95% CI [0.058, 0.252], p = 0.002). The cross-lagged paths were not significant between T1 cognitive adaptation and T2 routine disruptions (β = –0.068, 95% CI [–0.165, 0.030], p = 0.173) or T2 probable anxiety (β = –0.075, 95% CI [–0.176, 0.026], p = 0.146), or between T1 probable anxiety and T2 cognitive adaptation (β = –0.080, 95% CI [–0.196, 0.037] p = 0.180) or routine disruptions (β = 0.063, 95% CI [–0.029, 0.154], p = 0.180). The detailed statistics are summarized in Table 3. Results of the sensitivity analysis based on continuous variables are presented in Supplementary Table 2.
Table 3.
Cross-lagged analyses examining the autoregressive and cross-lagged effects of cognitive adaptation, routine disruptions, and probable anxiety.
| Effect | Variables | β [95% CI] |
|---|---|---|
| Autoregressive | T1 Cognitive adaptation → T2 Cognitive adaptation | 0.427 [0.096, 0.758]* |
| T1 Routine disruptions → T2 Routine disruptions | 0.396 [0.258, 0.534]*** | |
| T1 Probable anxiety → T2 Probable anxiety | 0.421 [0.321, 0.520]*** | |
| Cross-lagged | T1 Cognitive adaptation → T2 Routine disruptions | –0.068 [–0.165, 0.030] |
| T1 Routine disruptions → T2 Cognitive adaptation | –0.157 [–0.296, –0.018]* | |
| T1 Cognitive adaptation → T2 Probable anxiety | –0.075 [–0.176, 0.026] | |
| T1 Routine disruptions → T2 Probable anxiety | 0.155 [0.058, 0.252]** | |
| T1 Probable anxiety → T2 Cognitive adaptation | –0.080 [–0.196, 0.037] | |
| T1 Probable anxiety → T2 Routine disruptions | 0.063 [–0.029, 0.154] |
Probable anxiety was defined by scores of 10 or above on the 7-item Generalized Anxiety Disorder scale (GAD-7); Cognitive adaptation and routine disruptions were binary variables (based on median split). Results of the sensitivity analysis based on continuous variables are presented in Supplementary Table 2.
*p < 0.050, **p < 0.010, ***p < 0.001.
Path analyses
Path models were constructed to test the mediating effect of T2 daily routine disruptions on the associations between T1 cognitive adaptation and T2 probable psychiatric conditions and the mediating effect of T2 cognitive adaptation on the associations between T1 daily routine disruptions and T2 probable psychiatric conditions (Supplementary Fig. 1). Both the models for probable depression (RMSEA = 0.044, 90% CI [0.020, 0.070], SRMR = 0.040, CFI = 0.977, TLI = 0.918) and probable anxiety (RMSEA = 0.040, 90% CI [0.005, 0.072], SRMR = 0.026, CFI = 0.988, TLI = 0.946) demonstrated good data-model fit. The effect of T1 routine disruptions on T2 probable depression/anxiety was fully mediated by T2 cognitive adaptation (β = 0.032, 95% CI [0.006, 0.058], p = 0.017; β = 0.036, 95% CI [0.006, 0.066], p = 0.018). Meanwhile, T1 cognitive adaptation demonstrated neither a direct nor an indirect effect on T2 probable depression/anxiety. The results of the direct and indirect effects are summarized in Table 4. Results of the sensitivity analysis based on continuous variables are presented in Supplementary Table 3.
Table 4.
Path analyses examining the mutual mediating mechanisms of cognitive adaptation and routine disruptions on probable depression/anxiety.
| Outcome | Direct/Indirect effects | Direct/Indirect effect β [95% CI] |
|---|---|---|
| T2 Probable depression | T1 Cognitive adaptation | 0.021 [–0.078, 0.120] |
| T1 Cognitive adaptation → T2 Routine disruptions | –0.009 [–0.025, 0.007] | |
| T1 Routine disruptions | –0.042 [–0.149, 0.065] | |
| T1 Routine disruptions → T2 Cognitive adaptation | 0.032 [0.006, 0.058]* | |
| T2 Probable anxiety | T1 Cognitive adaptation | 0.060 [–0.049, 0.170] |
| T1 Cognitive adaptation → T2 Routine disruptions | –0.011 [–0.027, 0.006] | |
| T1 Routine disruptions | 0.024 [–0.097, 0.145] | |
| T1 Routine disruptions → T2 Cognitive adaptation | 0.036 [0.006, 0.066]* |
Probable depression was defined by scores of 10 or above on the 9-item Patient Health Questionnaire (PHQ-9); Probable anxiety was defined by scores of 10 or above on the 7-item Generalized Anxiety Disorder scale (GAD-7); Cognitive adaptation and routine disruptions were binary variables (based on median split). Results of the sensitivity analysis based on continuous variables are presented in Supplementary Table 3.
*p < 0.050.
Discussion
This two-wave cross-lagged panel analysis aims to investigate the reciprocal associations between cognitive and behavioral adjustment and the mediating effect of each on the other’s associations with prospective probable psychiatric conditions amid the COVID-19 pandemic. Our findings were largely comparable between probable depression and probable anxiety. Partially consistent with our expectations, only daily routine disruptions (at T1) displayed cross-lagged effects on both cognitive adaptation and probable depression/anxiety (at T2), meaning that daily routine disruptions could predict lower cognitive adaptation and higher odds of probable depression/anxiety but not the other way round. Further path analyses only identified a significant mediating effect of T2 cognitive adaptation on the association between T1 daily routine disruptions and T2 probable depression/anxiety. The COVID-19 pandemic disrupted perceptions of the self and the world as well as obstructed daily lives. The current study demonstrated elements that could be rebuilt to aid adaptive adjustment.
Our findings suggested a fundamental role of behavioral processes preceding emotional and cognitive adjustments in face of chronic stressors. Under COVID-19 when the maintenance of regular activities was seriously challenged, daily routine disruptions were positively associated with depressive or anxiety symptoms29, whereas successful maintenance of daily routines served as one of the protective factors against mental ill health28. Theoretically, the current results provided further prospective empirical evidence supporting the conceptual and clinical utility of the social zeitgeber model and the Drive to Thrive (DTT) theory15,16, with both proposing that regularity in daily routines could be seen as a necessary condition for emotional adjustment under chronic stress and trauma.
Conversely, we did not find significant prospective positive associations of probable depression/anxiety with subsequent daily routine disruptions. Our findings showed that daily routine disruptions are conceptually different from behavioral symptoms (e.g., changes in eating, sleep, or physical activity) that have long been considered as consequential to mood disorders42. Daily routine disruptions are the antecedent, not secondary behavioral manifestation, of probable depression/anxiety.
Based on the current significant association between T1 daily routine disruptions and T2 cognitive adaptation, behavioral processes could be considered as a fundamental process that precedes cognitive adaptation. There is a growing body of prospective evidence suggesting a close positive link of regularity in daily routines with self-efficacy43 or meaning in life12. Performance of routine behaviors have been found to relate to more feelings of comfort, safety, and confidence across real-life and laboratory settings44. For families with children suffering physical45 or mental46 health issues, routines were perceived as the bedrock on which family members supported one another, and children perceived themselves as able to accomplish tasks and achieve normal functioning levels, despite their health challenges. Daily routines function not only as a mere collection of activity schedules but also as an externalized form of coping under life difficulties.
The Conservation of Resources (COR) theory suggests that resource gain begets further resource gain, putting an individual within a positive cycle of resource accumulation4. Considering the unidirectional cross-lagged effect of daily routine disruptions on cognitive adaptation in conjunction with their significant cross-sectional associations among different factors, our results serve as a concrete illustration of how various resilience factors dynamically interact with one another through orchestrated effects to form a knitted network of resources2,3. Different types of daily routines and disruptions could demonstrate differential associations with cognitive adaptation, which could both be targets of intervention for positive adaptation3.
In the family routines literature, for example, it is suggested that household routines likely provide a context for children to experience belonging, acquire values/norms, improve self-regulation, and perceive predictability47. Our current findings similarly suggested that regularity of daily routines could form a behavioral context conducive to resilience outcomes through their positive associations with cognitive adaptation16,35. Broadly speaking, our results resonated theoretical perspectives on the priority to establish a resourceful environment over the pure cultivation of internal characteristics48, because securing the right context could foster the development of positive inner qualities, forming, in turn, a positive loop for psychological resilience.
On the other hand, we did not identify a significant association between T1 cognitive adaptation (i.e., combined self-efficacy and meaning-making) and T2 daily routine disruptions. Previous evidence has nevertheless suggested the health-promoting behavioral benefits of self-efficacy8,10 and meaning in life13,14. Taken together, this discrepancy might suggest that the regularity of daily routines should be assessed and intervened separably from individual activities amid large-scale disasters or in the post-disaster period. For example, public health intervention could sequentially enhance regularity of daily routines or restore disrupted routines, which form a solid behavioral foundation for facilitating positive cognitive adaptation such as self-efficacy and meaning-making and then health behaviors.
Several limitations warranted cautions. First, the mediators (i.e., self-efficacy, meaning-making, daily routine disruptions) and the outcome variables (i.e., probable depression and anxiety) in the path analyses were assessed cross-sectionally. Therefore, we cannot fully rule out possible bidirectional associations, although there were a wealth of theoretical and empirical evidence7,14,15 supporting a directional relationship between the mediators and the outcome variables. Relatedly, there could be unmeasured confounding variables that dilute an absolute causal conclusion. Second, the small effect sizes of certain significant paths and the wide confidence intervals of certain non-significant paths, although comparable with previous similar studies in COVID-19, could have limited the validity of the current findings. Third, probable psychiatric conditions were self-reported. Although we used validated measures that have been tested reliable across contexts and populations38,40, the current evidence could be cross-validated with clinical diagnoses or structured interviews. Fourth, cognitive adaptation could also be manifested in mental processes other than efficacious and meaningful thinking, such as self-esteem, perceived predictability, and optimism5, which await future investigations. Fifth, routine subgroups were summarized into single items, whereas different activities belonging to each subgroup could be specifically analyzed within future studies. Finally, the interval between the two assessments was short, i.e., six months, and our results should be interpreted within the timeframe of one-year post-COVID-outbreak. As COVID-19 transformed from an acute stressor to a chronic stressor49, the respective roles of cognitive and behavioral factors in adaptive functioning might also differ.
Notwithstanding the limitations, this study has largely benefited from the cross-lagged analyses based on a population-representative prospective dataset, which have provided methodological and statistical rigor to the inferences of directionality between cognitive and behavioral adaptation. Overall consistency in patterns of probable depression and anxiety further supported the reliability of our conclusions. On a broader sense, the current study contributed preliminary insights to the interrelating cognitive and behavioral processes in psychological adjustment. Specifically, adjustment could warrant better mental health outcomes by beginning with regularizing daily routine behaviors followed by sustaining or gaining cognitive adaptation such as efficacious and meaningful thinking in order to achieve resilience under chronic stress and trauma. Moving forward, an in-depth understanding of the cognitive and behavioral processes, as well as their interactions, should be achieved with the investigation of additional cognitive and behavioral elements other than those (self-efficacy, meaning-making, and routine disruptions) included in the current study, such as self-esteem5, health behaviors50, and the ability to concentrate on individual work51. Experimental studies and clinical trials will further inform the clinical knowledge base for the cognitive-behavioral stream in psychotherapies. A more comprehensive consideration of additional diagnostic outcomes is necessary to determine whether these processes are truly shared across psychiatric conditions.
Supplementary information
Acknowledgements
The authors would like to thank all the respondents who participated in this study and all individuals who made significant contributions to the data collection. This work was supported by the Research Grants Council, University Grants Committee, Hong Kong SAR, China [grant number 18600320 (W.K.H.)]. The funding source had no role in any process of our study.
Author contributions
TJT: Conceptualization, Methodology, Formal Analysis, Data Curation, Writing—Original Draft, Writing—Review & Editing; TWL: Conceptualization, Methodology, Data Curation, Writing—Review & Editing; LL: Methodology, Formal Analysis, Writing—Review & Editing; HL: Conceptualization, Writing—Review & Editing; WKH: Conceptualization, Methodology, Formal Analysis, Data Curation, Writing—Original Draft, Writing—Review & Editing, Supervision, Project Administration, Funding Acquisition.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon request.
Code availability
The codes for analyses are available from the corresponding author upon request. All codes are written within Mplus (Version 8.3) for the present study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s44184-023-00037-8.
References
- 1.Padesky CA, Mooney KA. Strengths‐based cognitive-behavioural therapy: a four‐step model to build resilience. Clin. Psychol. Psychother. 2012;19:283–290. doi: 10.1002/cpp.1795. [DOI] [PubMed] [Google Scholar]
- 2.Kalisch R, et al. The resilience framework as a strategy to combat stress-related disorders. Nat. Hum. Behav. 2017;1:784–790. doi: 10.1038/s41562-017-0200-8. [DOI] [PubMed] [Google Scholar]
- 3.Fritz J, Fried EI, Goodyer IM, Wilkinson PO, Van Harmelen AL. A network model of resilience factors for adolescents with and without exposure to childhood adversity. Sci. Rep. 2018;8:15774. doi: 10.1038/s41598-018-34130-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hobfoll, S. E. Stress, Culture, and Community: The Psychology and Philosophy of Stress (Plenum, 1998).
- 5.Taylor SE. Adjustment to threatening events: a theory of cognitive adaptation. Am. Psychol. 1983;38:1161–1173. doi: 10.1037/0003-066X.38.11.1161. [DOI] [Google Scholar]
- 6.Aspinwall LG, Taylor SE. Modeling cognitive adaptation: a longitudinal investigation of the impact of individual differences and coping on college adjustment and performance. J. Pers. Soc. Psychol. 1992;63:989–1003. doi: 10.1037/0022-3514.63.6.989. [DOI] [PubMed] [Google Scholar]
- 7.Bandura A. Health promotion from the perspective of social cognitive theory. Psychol. Health. 1998;13:623–649. doi: 10.1080/08870449808407422. [DOI] [Google Scholar]
- 8.Suorsa KI, et al. Adolescents and young adults with asthma and allergies: physical activity, self-efficacy, social support, and subsequent psychosocial outcomes. Child. Health. Care. 2016;45:414–427. doi: 10.1080/02739615.2015.1065741. [DOI] [Google Scholar]
- 9.Cleland V, et al. Individual, social and environmental correlates of physical activity among women living in socioeconomically disadvantaged neighbourhoods. Soc. Sci. Med. 2010;70:2011–2018. doi: 10.1016/j.socscimed.2010.02.028. [DOI] [PubMed] [Google Scholar]
- 10.Przepiórka A, Błachnio A, Siu NYF. The relationships between self-efficacy, self-control, chronotype, procrastination and sleep problems in young adults. Chronobiol. Int. 2019;36:1025–1035. doi: 10.1080/07420528.2019.1607370. [DOI] [PubMed] [Google Scholar]
- 11.Khamrin P, Boonyathee S, Bootsikeaw S, Ong-Artborirak P, Seangpraw K. Factors associated with health literacy, self-efficacy, social support, and oral health care behaviors among elderly in northern border community Thailand. Clin. Interv. Aging. 2021;16:1427–1437. doi: 10.2147/CIA.S320900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heintzelman SJ, King LA. (The feeling of) meaning-as-information. Pers. Soc. Psychol. Rev. 2014;18:153–167. doi: 10.1177/1088868313518487. [DOI] [PubMed] [Google Scholar]
- 13.Hooker SA, Masters KS, Park CL. A meaningful life is a healthy life: a conceptual model linking meaning and meaning salience to health. Rev. Gen. Psychol. 2018;22:11–24. doi: 10.1037/gpr0000115. [DOI] [Google Scholar]
- 14.Vos J. Cardiovascular disease and meaning in life: a systematic literature review and conceptual model. Palliat. Support. Care. 2021;19:367–376. doi: 10.1017/S1478951520001261. [DOI] [PubMed] [Google Scholar]
- 15.Ehlers CL, Frank E, Kupfer DJ. Social zeitgebers and biological rhythms: a unified approach to understanding the etiology of depression. Arch. Gen. Psychiatry. 1988;45:948–952. doi: 10.1001/archpsyc.1988.01800340076012. [DOI] [PubMed] [Google Scholar]
- 16.Hou, W. K., Hall, B. J. & Hobfoll, S. E. Drive to thrive: a theory of resilience following loss. In: Mental Health of Refugee and Conflict-Affected Populations: Theory, Research and Clinical Practice, (eds Morina, N. & Nickerson, A.) 111–133 (Springer, 2018).
- 17.Sabet SM, Dautovich ND, Dzierzewski JM. The rhythm is gonna get you: social rhythms, sleep, depressive, and anxiety symptoms. J. Affect. Disord. 2021;286:197–203. doi: 10.1016/j.jad.2021.02.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nagata S, McCormick B, Piatt J. Leisure behavior and sense of coherence in the context of depression. J. Community. Psychol. 2020;48:283–301. doi: 10.1002/jcop.22250. [DOI] [PubMed] [Google Scholar]
- 19.Hobfoll SE, Halbesleben J, Neveu JP, Westman M. Conservation of resources in the organizational context: the reality of resources and their consequences. Ann. Rev. Organ. Psychol. Organ. Behav. 2018;5:103–128. doi: 10.1146/annurev-orgpsych-032117-104640. [DOI] [Google Scholar]
- 20.Ross CE, Mirowsky J. Sex differences in the effect of education on depression: resource multiplication or resource substitution? Soc. Sci. Med. 2006;63:1400–1413. doi: 10.1016/j.socscimed.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 21.Zautra, A. J., Hall, J. S. & Murray, K. E. Resilience: a new definition of health for people and communities. In: Handbook of Adult Resilience, (eds Reich, J. W., Zautra, A. J. & Hall, J. S.) 3–29 (Guilford Publications, 2010).
- 22.Hou WK, Lam JHM. Resilience in the year after cancer diagnosis: a cross-lagged panel analysis of the reciprocity between psychological distress and well-being. J. Behav. Med. 2014;37:391–401. doi: 10.1007/s10865-013-9497-6. [DOI] [PubMed] [Google Scholar]
- 23.Wu T, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bendau A, et al. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID‐19 pandemic in Germany. Brain. Behav. 2021;11:e01964. doi: 10.1002/brb3.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Werner A, Kater MJ, Schlarb AA, Lohaus A. Sleep and stress in times of the COVID-19 pandemic: the role of personal resources. Appl. Psychol. Health. Well-Being. 2021;13:935–951. doi: 10.1111/aphw.12281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kang Y, et al. Purpose in life, loneliness, and protective health behaviors during the COVID-19 pandemic. Gerontol. 2021;61:878–887. doi: 10.1093/geront/gnab081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maykrantz SA, Langlinais LA, Houghton JD, Neck CP. Self-leadership and psychological capital as key cognitive resources for shaping health-protective behaviors during the COVID-19 pandemic. Adm. Sci. 2021;11:41. doi: 10.3390/admsci11020041. [DOI] [Google Scholar]
- 28.Kornilaki EN. The psychological effect of COVID‐19 quarantine on Greek young adults: risk factors and the protective role of daily routine and altruism. Int. J. Psychol. 2022;57:33–42. doi: 10.1002/ijop.12767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lau BHP, Cheung MKT, Chan LTH, Chan CLW, Leung PPY. Resilience in the storm: impacts of changed daily lifestyles on mental health in persons with chronic illnesses under the COVID-19 pandemic. Int. J. Environ. Res. Public. Health. 2021;18:5875. doi: 10.3390/ijerph18115875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fincham JE. Response rates and responsiveness for surveys, standards, and the Journal. Am. J. Pharm. Edu. 2008;72:43. doi: 10.5688/aj720243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Romppel M, et al. A short form of the General Self-Efficacy Scale (GSE-6): development, psychometric properties and validity in an intercultural non-clinical sample and a sample of patients at risk for heart failure. GMS. Psycho-Soc-Med. 2013;10:Doc01. doi: 10.3205/psm000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carver CS, Scheier MF, Weintraub KJ. Assessing coping strategies: a theoretically based approach. J. Pers. Soc. Psychol. 1989;56:267–283. doi: 10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 33.Stanton AL, Danoff-burg S, Huggins ME. The first year after breast cancer diagnosis: hope and coping strategies as predictors of adjustment. Psychooncology. 2002;11:93–102. doi: 10.1002/pon.574. [DOI] [PubMed] [Google Scholar]
- 34.Park CL, George LS. Assessing meaning and meaning making in the context of stressful life events: measurement tools and approaches. J. Posit. Psychol. 2013;8:483–504. doi: 10.1080/17439760.2013.830762. [DOI] [Google Scholar]
- 35.Hou WK, Lai FTT, Hougen C, Hall BJ, Hobfoll SE. Measuring everyday processes and mechanisms of stress resilience: development and initial validation of the Sustainability of Living Inventory (SOLI) Psychol. Assess. 2019;31:715–729. doi: 10.1037/pas0000692. [DOI] [PubMed] [Google Scholar]
- 36.Hou WK, et al. Psychiatric symptoms and behavioral adjustment during the COVID-19 pandemic: evidence from two population-representative cohorts. Transl. Psychiatry. 2021;11:174. doi: 10.1038/s41398-021-01279-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yeung A, et al. Validation of the Patient Health Questionnaire-9 for depression screening among Chinese Americans. Compr. Psychiatry. 2008;49:211–217. doi: 10.1016/j.comppsych.2006.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Levis B, Benedetti A, Thombs BD. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. 2019;365:11476. doi: 10.1136/bmj.l1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spitzer RL, Kroenke K, Wiliams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 40.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 41.Hooper D, Coughlan J, Mullen M. Structural equation modelling: guidelines for determining model fit. Electron. J. Bus. Res. Methods. 2008;6:53–60. [Google Scholar]
- 42.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) (American Psychiatric Association, 2013).
- 43.Huang Q, Wang X, Ge Y, Cai D. Relationship between self-efficacy, social rhythm, and mental health among college students: a 3-year longitudinal study. Curr. Psychol. 2023;42:9053–9062. doi: 10.1007/s12144-021-02160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Avni‐Babad D. Routine and feelings of safety, confidence, and well‐being. Br. J. Psychol. 2011;102:223–244. doi: 10.1348/000712610X513617. [DOI] [PubMed] [Google Scholar]
- 45.Frare M, Axia G, Battistella PA. Quality of life, coping strategies, and family routines in children with headache. Headache. 2002;42:953–962. doi: 10.1046/j.1526-4610.2002.02224.x. [DOI] [PubMed] [Google Scholar]
- 46.Koome F, Hocking C, Sutton D. Why routines matter: the nature and meaning of family routines in the context of adolescent mental illness. J. Occup. Sci. 2012;19:312–325. doi: 10.1080/14427591.2012.718245. [DOI] [Google Scholar]
- 47.Höltge J, Ungar M, Theron L. The differential interplay of home routines and comforting beliefs on adolescent mental health in situations of severe parental conflict. Advers. Resil. Sci. 2021;2:5–17. doi: 10.1007/s42844-021-00029-7. [DOI] [Google Scholar]
- 48.Panter-Brick, C. & Eggerman, M. Understanding culture, resilience, and mental health: the production of hope. In:The Social Ecology of Resilience: A Handbook of Theory and Practice, (ed. Ungar, M.), 369–386 (Springer, 2012).
- 49.Norrholm SD, et al. Does COVID‐19 count?: defining Criterion A trauma for diagnosing PTSD during a global crisis. Depress. Anxiety. 2021;38:882–885. doi: 10.1002/da.23209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Naslund JA, et al. Health behavior models for informing digital technology interventions for individuals with mental illness. Psychiatr. Rehabil. J. 2017;40:325–335. doi: 10.1037/prj0000246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wiese BS, et al. Staying focused on work and satisfied with the job in times of pandemic: the power of everyday routines. Int. J. Stress. Manag. 2022;29:166–170. doi: 10.1037/str0000241. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon request.
The codes for analyses are available from the corresponding author upon request. All codes are written within Mplus (Version 8.3) for the present study.