Abstract
Background
Osteogenesis imperfecta (OI) is a rare, heritable connective tissue disorder associated with a variety of symptoms, that affect individuals’ quality of life (QoL) and can be associated with increased healthcare resource use. While some aspects of OI are well studied, others remain poorly understood. Therefore, the IMPACT survey aimed to elucidate the humanistic, clinical and economic burden of OI on individuals with OI, their families, caregivers and wider society.
Methods
We developed an international mixed methods online survey in eight languages (fielded July–September 2021), aimed at adults (aged ≥ 18 years) or adolescents (aged ≥ 12–17 years) with OI, caregivers (with or without OI) of individuals with OI and other close relatives. All respondents provided data on themselves; caregivers additionally provided data on individuals in their care by proxy. Data were cleaned, coded, and analysed using the pandas Python software package and Excel.
Results
IMPACT collected 2208 eligible questionnaires (covering 2988 individuals of whom 2312 had OI) including 1290 non-caregiver adults with OI, 92 adolescents with OI, 150 caregiver adults with OI, 560 caregivers for individuals with OI, 116 close relatives and 780 proxy care-recipients with OI. Most individuals with OI (direct or proxy) described their OI as moderate (41–52% across populations) and reported OI type 1 (33–38%). Pain (72–82%) was the most reported clinical condition experienced in the past 12 months and was also most frequently rated as severely or moderately impactful. Further, among adults, 67% reported fatigue, 47% scoliosis, and 46% sleep disturbance; in adolescents, fatigue affected 65%, scoliosis and other bone problems 60%, and mental health problems 46%; in children, fractures were common in 67%, fatigue in 47%, and dental problems in 46%.
Conclusion
IMPACT has generated an extensive dataset on the experience of individuals with OI, their caregivers and relatives. We found that, irrespective of age, individuals with OI experience numerous and evolving symptoms that affect their QoL; however, pain and fatigue are consistently present. Upcoming analyses will provide further insights into the economic impact, healthcare journey and caregiver wellbeing, aiming to contribute to improved treatment and care for the OI community.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13023-024-03126-9.
Keywords: Osteogenesis imperfecta, Patient reported outcomes, Survey, Burden of disease, Children, Adults, Adolescents, Impact, Rare diseases, Mixed methods
Introduction
Osteogenesis imperfecta (OI) is a rare, heritable connective tissue disorder with variable manifestations and numerous symptoms affecting 1–5 in 10,000 individuals [1–3]. Most often the condition is caused by alterations in the type 1 collagen genes (e.g. COL1A1 and COL1A2), but mutations in other genes that are linked to the collagen synthesis are also associated with OI [1]. OI affects multiple systems and organs in the body, resulting in an array of possible symptoms including fractures, skeletal deformities, pain, joint hypermobility and occasionally blue sclerae, hearing loss, dental abnormalities, basilar invagination, cardiovascular and pulmonary abnormalities [1].
Currently there are no curative therapies for OI, and treatment primarily aims to manage and decrease fractures, pain, and bone deformities, and promote mobility and independence. To manage the spectrum of OI symptoms multi-disciplinary care is required [4, 5]. Most therapeutic agents used in OI care were initially developed to target the bone metabolism in conditions such as osteoporosis and are used off-label [4]. Bisphosphonates are most widely used; additionally human monoclonal antibodies (e.g., denosumab) and parathyroid hormone (e.g., teriparatide) are available [4, 5].
Considering the lack of curative treatment and the condition’s effect on multiple systems and organs in the body, living with OI has a significant impact on the physical, social, and emotional wellbeing of individuals as well as their families and caregivers [6–8]. However, due to its rarity and variability, research into OI is challenging, and there are few comprehensive, self-reported patient outcome studies in this field [6, 9].
While some aspects of OI and their impact on health-related quality of life (HRQoL) are well-understood (e.g., mobility challenges and fractures) others, such as women’s health, characteristics of pain, treatment-related adverse events, pulmonological conditions, and gastrointestinal-, sleep-, and skin-related conditions are less well studied [9]. Similarly, the impact on some caregivers of individuals with OI is incompletely understood, particularly fathers and siblings [9]. In addition, as most HRQoL studies are cross-sectional and use small samples, our understanding of the HRQoL of individuals with OI at different life stages is limited [7, 9]
OI may also be associated with a considerable economic burden on individuals and their families, even in socialised healthcare systems [10, 11], and an increased use of healthcare and social service resources [12–17]. However, studies focus on the societal and healthcare resource use associated with OI, while out of pocket spending is rarely described [10, 11].
To better understand the humanistic, clinical and economic impact of OI on individuals with OI, their families, caregivers and wider society we conducted the IMPACT Survey (Living with osteogenesis imperfecta: understanding experiences based on community insight & evidence) aimed at individuals with OI, their caregivers and relatives. Here we present the study’s design, methodology and first findings, including demographics, clinical characteristics and clinical signs, symptoms and events and their impact.
Methods
Development
IMPACT was developed by a steering committee that included independent academic researchers, representatives of the patient advocacy organisation (PAO) Osteogenesis Imperfecta Foundation (OIF; USA), the umbrella PAO Osteogenesis Imperfecta Federation Europe (OIFE) and representatives of Mereo BioPharma.
Questions that could potentially address evidence gaps identified in a scoping literature review [9], that were most relevant to the OI and research community and most suitable to survey-based research, were prioritised. The questionnaire was drafted and reviewed in English and professionally translated into German, Italian, Dutch, French, Russian, Spanish (both South American and European) and Portuguese. The survey was extensively tested by the authors, OI community members and volunteers. Community members from Germany, Norway, the Netherlands, Italy, France, Spain, Mexico, Italy, Russia and the USA tested the survey for local relevance using Microsoft Word copies of the translated survey and advised on regionally relevant question wording and answer options. To this end, individuals were supplied with a Microsoft Word version of the survey as well as a test version of the online survey. Additionally the online version of the survey was tested using respondent profiles developed by the authors to ensure that the survey platform guided respondents as intended and all questions were clear and displayed correctly.
An ethics approval was not sought because exemption was granted by an independent review board (Pearl IRB, Indianapolis, USA).
Population-specific questionnaire design
A basic version of the questionnaire was adapted to cover five main respondent populations. The “non-caregiver adult with OI” questionnaire was designed for individuals with OI ≥ 18 years of age who answered questions about themselves. This population is called “non-caregiver adults with OI” to distinguish from the adults with OI who identified as caregivers of care recipients with OI. The “caregiver adult with OI” questionnaire was designed for individuals with OI ≥ 18 years of age who were caregivers of care recipients with OI who answered questions about themselves, and by proxy, about individuals in their care (children [0–11 years], adolescents [12–17 years] or adults [≥ 18 years] with OI). The “adolescent with OI” questionnaire was designed for adolescents with OI aged 12–17 years who answered questions about themselves. The “caregiver without OI” questionnaire was designed for caregivers of individuals with OI who answered questions about themselves and, by proxy, about their care recipients with OI (children, adolescents or adults with OI). The “relative” questionnaire was designed for other relatives of individuals with OI (Table 1). For the “adolescent with OI” questionnaire, certain topics were removed (e.g., sexual health and financial impact), and the language was adjusted for ease of understanding. Questionnaires were adjusted for each population, to keep the survey size manageable for respondents who provided information on themselves and care recipients. The full questionnaires are provided in Additional file 1.
Table 1.
IMPACT Survey design overview
| Population | |||||
|---|---|---|---|---|---|
| Domain | Non-caregiver adults with OI | Caregiver adults with OIa, b | Caregivers without OIa | Adolescents with OI | Relatives |
| Participation criteria | ≥ 18 years of age |
≥ 18 years of age OI Self-describes as someone who provides care for individuals with OI |
≥ 18 years of age Self-describes as someone who provides care for individuals with OI |
≥ 12–17 years of age OI |
≥ 12 years of age Self-assesses relationship to person with OI as close but does not self-describe as a caregiver |
| N questionsc | 37–84 | 50–111 | 49–94 | 28–69 | 10–12 |
| Clinical characteristics | Demographic data; for each person with OI: height, OI type, OI severity, causative gene, mobility status | Demographics | |||
| Clinical signs, symptoms and events | Signs, symptoms and events in past 12 months and lifetime | NA | |||
| Treatment and care experience | Diagnostic pathway, experience with healthcare providers, access to care | NA | |||
| QoL | Impact of OI on individuals(s) with OI, impact of signs, symptoms and events, worries | NA | |||
| Impact on families | NA | Impact on caregivers and impact on family life | NA | Impact of OI, worries | |
| Healthcare consumption | Use of therapies in past 12 months and lifetime, use of inpatient and outpatient care, consumable use | NA | |||
| Financial sources for treatment | Insurance coverage, out of pocket spending | NA | NA | ||
NA, not applicable; OI, osteogenesis imperfecta; QoL, quality of life
aCaregivers provided information on 1–3 care recipients with OI of any age; bCaregivers with OI only provided information about their OI and their experience of caring for individuals with OI, they did not report about the OI experience of individuals in their care; cThe minimum includes compulsory questions without any follow-up questions that only applied to subgroups, the maximum includes all compulsory and optional questions
Recruitment of participants
Recruitment of participants was undertaken digitally, through self-referral via a website. The website was promoted via PAO social channels, direct emails to organisation members and at meetings. Survey branding, a style guide, key messaging, a promotional animation clip, campaign flyers, proposed email content and social media materials were developed in collaboration with PAO members. A branded survey website was available (www.impactsurveyoi.com) for ongoing referral and information for potential participants.
Before and throughout fielding the project was presented at meetings of OI associations and through social media channels, while no other survey projects were promoted through these channels during that period. The OIFE provided regular updates to member organisations. To mitigate geographic and gender-based disparities in recruitment the steering committee reached out to the OIFE medical advisory board to medical professionals to mention the survey to their patients. This was effective in countries with less active PAOs or countries in which surveys are uncommon.
Fielding
The survey was fielded online 1 July–30 September 2021.
Analysis
Survey data were exported into Excel, translated back into English and compiled into a master database using the pandas Python software package. Free text responses were analysed and used to validate structured responses. Where possible, free text answers were compared with any structured responses in Microsoft Excel to identify mismatch or improve the accuracy of structured responses (e.g. where respondents had used the “Other” option, but the free text response matched one of the answer options). Additionally for all questions recurring themes in free text responses were identified in Microsoft Excel and free text containing recurring themes was quantified. Data were cleaned to exclude any outliers and non-sensical responses. Potential outliers (any values greater than 2 standard deviations from the median of continuous variables) were validated by clinicians. Data-cleaning and analysis were performed in Excel. The main features and characteristics of the data set were summarised with descriptive statistics. Unless otherwise specified “adults with OI” includes both, caregiver and non-caregiver adults with OI.
Results
Overall, 2428 complete questionnaires were submitted. During the data cleaning stage 220 were excluded based on basic consistency checks of the responses leaving 2208 questionnaires for analysis, representing 2312 individuals with OI (1532 of whom answered questions about themselves, and 780 whose answers were provided by proxy) and 676 individuals without OI (560 of whom were caregivers without OI who answered questions about individuals with OI in their care, and 116 of whom were relatives of individuals with OI; Tables 1 and 2).
Table 2.
Respondent and proxy respondent demographics
| Direct respondents | Proxy respondents | |||||||
|---|---|---|---|---|---|---|---|---|
| Non-caregiver adults with OI n = 1,290 |
Caregiver adults with OI n = 150 |
Adolescents with OI n = 92 |
Caregivers without OI n = 560 |
Relatives n = 116 |
Children with OI (n = 474) | Adolescents with OI (n = 171) | Adults with OI (n = 135) | |
| Age, mean (range)a | 43.4 (18–85) | 42.0 (24–75) | 14.8 (12–17) | 41.9 (18–81) | 43.3 (12–87) | 5.8 (1–11) | 14.0 (12–17) | 25.6 (18–60) |
| Women, n (%)b | 900 (70) | 108 (72) | 51 (55) | 465 (83) | 80 (69) | 214 (45) | 84 (49) | 67 (50) |
| Geography, n (%)c | ||||||||
| Europe | 807 (63) | 104 (69) | 41 (45) | 319 (57) | 102 (88) | 258 (54) | 111 (65) | 92 (68) |
| North America | 327 (25) | 20 (13) | 22 (24) | 103 (18) | 9 (8) | 85 (18) | 26 (15) | 30 (22) |
| South America | 55 (4) | 6 (4) | 8 (9) | 33 (6) | 2 (2) | 32 (7) | 3 (2) | 5 (4) |
| Asia | 62 (5) | 16 (11) | 20 (22) | 87 (16) | 1 (1) | 84 (18) | 21 (12) | 7 (5) |
| Africa | 6 (0.5) | 1 (0.7) | 0 (0) | 5 (1) | 1 (1) | 3 (1) | 2 (1) | 1 (1) |
| Australia/Oceania | 33 (3) | 3 (2) | 1 (1) | 13 (2) | 1 (1) | 12 (3) | 8 (5) | 0 (0) |
Osteogenesis imperfecta, OI
aQuestions 29, 40 and 48 “What is your age?” and “What is your child/children’s age?”; b;Questions 8, 303, 30, 41 and 49 “What is your sex?/What is the sex of your child/children? cQuestions 7, 302 and 370 “What is your country of residence?” It was assumed that proxy respondents reside in the same countries as their caregivers
Individuals reporting their own experience (direct respondents)
Respondent demographics are summarised in Table 2 and Appendix Table 4. There were 1532 respondents with OI who provided information on their own experience including 1290 non-caregiver adults with OI (without care recipients) and 92 adolescents with OI. Additionally, 150 adults with OI who were also caregivers for individuals with OI (“caregivers with OI”) provided information on both their own experience and that of the individuals with OI in their care (see below).
Table 4.
Caregiver and close relative demographics
| Caregiver relation, n (%)b,c | n = 700a |
| Parent | 684 (98) |
| Sibling | 2 (0.3) |
| Grandparent | 7 (1) |
| Legal guardian | 18 (3) |
| Prefer not to say | 0 (0) |
| Other | 2 (0.3) |
| Number of care recipients with OI in household, n (%)d,c | |
| Households with 1 care recipient | 632 (90) |
| Households with 2 care recipients | 56 (8) |
| Households with 3 care recipients | 12 (2) |
| Number of care recipients without OI in household, n (%)d | |
| Households with 0 siblings | 302 (43) |
| Households with 1 sibling | 284 (41) |
| Households with 2 siblings | 91 (13) |
| Households with 3 siblings | 18 (3) |
| Households with 4 siblings | 5 (0.7) |
| Close relative relation, n (%)e | n=116 |
| Partner of a person with OI | 33 (28) |
| Sibling of a person with OI | 23 (20) |
| Friend of a person with OI | 17 (15) |
| Grandparent of a person with OI | 14 (12) |
| Aunt of a person with OI | 8 (7) |
| Child of a person with OI | 4 (3) |
| Friend of a caregiver for a child with OI | 3 (3) |
| Support teacher of a person with OI | 3 (3) |
| Doctor of a person with OI | 2 (2) |
| Grandchild of a person with OI | 2 (2) |
| Great aunt of a person with OI | 2 (2) |
| Brother-in-law of a person with OI | 1 (1) |
| Caregiver of a person with OI | 1 (1) |
| Godmother | 1 (1) |
| Mother of a person with OI | 1 (1) |
| Mother of a deceased child with OI | 1 (1) |
OI, osteogenesis imperfecta
aIncludes caregiver adults with OI and caregivers without OI. Of 710 caregivers 700 provided information on care recipients with OI; b14 respondents indicated > 1 relation to a care recipient; cQuestion 24 “What is your relationship to the child/children with OI in your care?”. Respondents could pick more than one option including: parent, sibling, grandparent, legal guardian, prefer not to say, other and provide free text. dQuestions 22 and 23 included a drop down with numerals from 1 to 3 and 0 to 4 respectively. eQuestion 396 “Please indicate which of the following best describes your relationship to the person with OI”. Answer options included: child of a person with OI, sibling of a person with OI, grandparent of a person with OI, partner of a person with OI, other relationship to a person with OI (please specify below)
Adults with OI (n = 1440, including non-caregiver adults with OI [n = 1290] and caregiver adults with OI [n = 150]) were mostly female, from Europe or North America, with a median age of 42 years (range 18–85). Among 92 adolescents with OI the median age was 15 years (range 12–18) and proportions of male and female respondents were similar. Most adolescents with OI were from Europe (45%).
Respondents without OI, comprising 560 caregivers without OI, and 116 close relatives of individuals with OI, reported on their experience of caring for or being related to a person with OI. Caregivers without OI had a median age of 42 years (range 18–81), were mostly female and from Europe (Table 2).
Of the 710 survey participants identifying as caregivers (560 without OI, 150 with OI), 700 provided valid data on care recipients with OI (proxy data on 10 care recipients with OI were excluded). Most caregivers (90%) provided care to 1 individual with OI to whom they were a parent (98%). Fewer caregivers cared for to 2 (8%) or 3 (2%) individuals with OI or had other relationships to the care recipient (3%, Appendix Table 4).
Close relatives responding to the survey were predominantly female (69%); they self-described as being partners (28%), siblings (20%), or friends (15%) of individuals with OI (Appendix Table 4).
Care recipients with OI for whom caregivers provided survey answers by proxy (proxy respondents)
Of the 780 care recipients with OI who were proxy reported by 700 caregivers (with or without OI), most were children < 12 years (68%; median age 6 years, range 1–11), fewer were adolescents (24%; median age 14 years, range 12–17) or adults (19%; median age 26 years, range 18–60). Approximately half in each age group were female (Table 2).
Clinical characteristics
Direct respondents
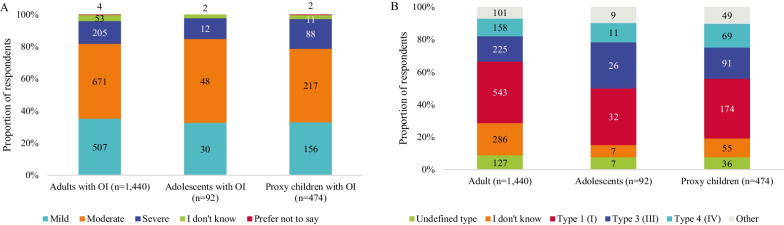
Most adults and adolescents with OI rated their OI as moderate (47% of adults and 52% of adolescents); the smallest proportion of individuals with OI rated their condition as severe (14% of adults and 13% of adolescents; Fig. 1A, Table 3). Similarly, most adults and adolescents with OI reported clinical OI type 1 (38% of adults and 35% of adolescents), 3 (16% of adults and 28% of adolescents) and 4 (11% of adults and 12% of adolescents; Fig. 1B and Table 3). Compared with adolescents, more adults were unaware of their clinical OI type (20% vs. 8% among adults and adolescents, respectively).
Fig. 1.
Respondents’ and proxy-respondents’(A) OI severitya and (B) typeb. OI, osteogenesis imperfecta. aQuestions 18, 32, 46, 54 and 312 “How would you describe the severity of your/your child’s/your children’s OI? Answer options included mild, moderate, severe, prefer not to say, I don’t know. bQuestions 17, 31, 45, 53 and 311.” If you/your child/your children have received an OI type as part of your OI diagnosis or treatment, please indicate your type using the dropdown below.” Answer options included Type 1–Type 15, undefined type, I don’t know, prefer not to say, other type. Participants who responded “other” could provide a free text answer
Table 3.
OI-related clinical characteristics of individuals with OI
| Adults with OI (n = 1440) | Adolescents with OI (n = 92) | Proxy children with OI (n = 474) | Proxy adolescents with OI (n = 171) | Proxy adults with OI (n = 135) | |
|---|---|---|---|---|---|
| OI severity, n (%)a | |||||
| Mild | 507 (35) | 30 (33) | 157 (33) | 63 (37) | 38 (28) |
| Moderate | 671 (47) | 48 (52) | 216 (46) | 70 (41) | 58 (43) |
| Severe | 205 (14) | 12 (13) | 88 (19) | 33 (19) | 36 (27) |
| I don’t know | 53 (4) | 2 (2) | 11 (2) | 4 (2) | 3 (2) |
| Prefer not to say | 4 (0.3) | 0 (0) | 2 (0.4) | 1 (0.6) | 0 (0) |
| OI type, n (%)b | |||||
| Undefined type | 127 (9) | 7 (8) | 36 (8) | 19 (11) | 7 (5) |
| I don’t know | 286 (20) | 7 (8) | 55 (12) | 24 (14) | 25 (19) |
| Prefer not to say | 2 (0.1) | 0 (0) | 1 (0.2) | 0 (0) | 2 (2) |
| Type 1 (I) | 543 (38) | 32 (35) | 174 (37) | 56 (33) | 44 (33) |
| Type 2 (II) | 23 (2) | 2 (2) | 7 (2) | 3 (2) | 3 (2) |
| Type 3 (III) | 225 (16) | 26 (28) | 91 (19) | 29 (17) | 27 (20) |
| Type 4 (IV) | 158 (11) | 11 (12) | 69 (15) | 27 (16) | 21 (16) |
| Type 5 (V) | 26 (2) | 3 (3) | 16 (3) | 4 (2) | 1 (0.7) |
| Type 6 (VI) | 4 (0.3) | 0 (0) | 8 (2) | 2 (1) | 0 (0) |
| Type 7 (VII) | 2 (0.1) | 0 (0) | 1 (0.2) | 0 (0) | 0 (0) |
| Type 8 (VIII) | 1 (0.1) | 0 (0) | 1 (0.2) | 3 (2) | 0 (0) |
| Type 9 (IX) | 1 (0.1) | 1 (1) | 0 (0) | 0 (0) | 0 (0) |
| Type 11 (XI) | 2 (0.1) | 1 (1) | 0 (0) | 0 (0) | 0 (0) |
| Type 14 (XIV) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1) |
| Type 15 (XV) | 1 (0.1) | 0 (0) | 5 (1) | 0 (0) | 0 (0) |
| Other | 39 (3) | 2 (2) | 10 (2) | 4 (2) | 4 (3) |
| Genetic confirmation, n (%)c | |||||
| Yes | 916 (64) | 73 (79) | 397 (84) | 130 (76) | 95 (70) |
| No | 370 (26) | 12 (13) | 63 (14) | 34 (20) | 34 (25) |
| I don’t know | 153 (11) | 6 (7) | 14 (3) | 7 (4) | 5 (4) |
| Prefer not to say | 1 (0.1) | 1 (1) | 0 (0) | 0 (0) | 1 (0.7) |
| Mobility, n (%)d | |||||
| Walking (inside) | 900 (63) | 56 (61) | 338 (71) | 118 (69) | 82 (61) |
| Walking (outside) | 730 (51) | 49 (53) | 300 (63) | 112 (66) | 80 (59) |
| Cane/walking stick (inside) | 71 (5) | 3 (3) | 6 (1) | 6 (4) | 3 (2) |
| Cane/walking stick (outside) | 163 (11) | 4 (4) | 6 (1) | 7 (4) | 5 (4) |
| Walking frame (inside) | 20 (1) | 6 (7) | 23 (5) | 15 (9) | 1 (0.7) |
| Walking frame (outside) | 16 (1) | 3 (3) | 15 (3) | 6 (4) | 0 (0) |
| Rollator (inside) | 55 (4) | 7 (8) | 23 (5) | 8 (5) | 2 (1) |
| Rollator (outside) | 61 (4) | 2 (2) | 15 (3) | 6 (4) | 4 (3) |
| Crutches (inside) | 96 (7) | 6 (7) | 9 (2) | 6 (4) | 7 (5) |
| Crutches (outside) | 136 (9) | 9 (10) | 3 (0.6) | 4 (2) | 7 (5) |
| Manuel wheelchair (inside) | 300 (21) | 18 (20) | 61 (13) | 38 (22) | 27 (20) |
| Manuel wheelchair (outside) | 370 (26) | 33 (36) | 91 (19) | 61 (36) | 33 (24) |
| Powered wheelchair (inside) | 125 (9) | 5 (5) | 9 (2) | 3 (2) | 12 (9) |
| Powered wheelchair (outside) | 198 (14) | 8 (9) | 16 (3) | 10 (6) | 18 (13) |
| Mobility scooter (inside) | 4 (0.3) | 0 (0) | 6 (1) | 0 (0) | 0 (0) |
| Mobility scooter (outside) | 65 (5) | 0 (0) | 3 (0.6) | 1 (0.6) | 2 (1) |
| Crawling (inside) | 58 (4) | 9 (10) | 115 (24) | 25 (15) | 3 (2) |
| Crawling (outside) | 13 (0.9) | 0 (0) | 46 (10) | 2 (1) | 0 (0) |
| Being carried (inside) | 26 (2) | 8 (9) | 130 (27) | 14 (8) | 5 (4) |
| Being carried (outside) | 32 (2) | 10 (11) | 136 (29) | 17 (10) | 2 (1) |
| Laying in bed or stretcher (inside) | 20 (1) | 7 (8) | 36 (8) | 4 (2) | 3 (2) |
| Laying in bed or stretcher (outside) | 4 (0.3) | 0 (0) | 15 (3) | 3 (2) | 2 (1) |
| Other (inside) | 29 (2) | 5 (5) | 24 (5) | 2 (1) | 0 (0) |
| Other (outside) | 35 (2) | 3 (3) | 28 (6) | 4 (2) | 2 (1) |
| Height, n (%)e | |||||
| < 50 cm | 9 (0.6) | 1 (1) | 7 (1) | 1 (0.6) | 0 (0) |
| ≥ 50–80 cm | 13 (0.9) | 1 (1) | 71 (15) | 2 (1) | 4 (3) |
| > 80–100 cm | 95 (7) | 4 (4) | 126 (27) | 11 (6) | 9 (7) |
| > 100–130 cm | 270 (19) | 23 (25) | 179 (38) | 27 (16) | 21 (16) |
| > 130–160 cm | 702 (49) | 44 (48) | 54 (11) | 86 (50) | 49 (36) |
| > 160 cm | 331 (23) | 13 (14) | 0 (0) | 40 (23) | 48 (36) |
| I don’t know | 18 (1) | 5 (5) | 36 (8) | 4 (2) | 3 (2) |
| Prefer not to say | 2 (0.1) | 1 (1) | 1 (0.2) | 0 (0) | 1 (0.7) |
OI, osteogenesis imperfecta
aQuestions 18, 32, 46, 54 and 312 “How would you describe the severity of your/your child’s/your children’s OI? Answer options included mild, moderate, severe, prefer not to say, I don’t know. bQuestions 17, 31, 45, 53 and 311.” If you/your child/your children have received an OI type as part of your OI diagnosis or treatment, please indicate your type using the dropdown below.” Answer options included Type 1–Type 15, undefined type, I don’t know, prefer not to say, other type. Participants who responded “other” could provide a free text answer. cQuestions 19, 33, 47, 55 “Do you/your child/your children have a genetically confirmed diagnosis of OI”. Answer options included yes, I don’t know, prefer not to say. dQuestions 16, 36, 66, 67, 310 “How do you/your child/your children get around?”. Answer options for both outside and inside your home included Walking unaided, cane/walking stick, walking frame, rollator (wheeled walker), crutches, manual wheelchair, powered wheelchair, mobility scooter, crawling, being carried, laying in bed/stretcher, other (please specify below). Respondents could choose more than one answer in each category. eQuestions 14, 15, 27, 28, 43, 44, 51, 52, 308, 309 “What is your/your child’s height”. Answer options included metric or imperial measurements and “I don’t know”, “Prefer to say”. All values were converted to metric measurements
Most adults and adolescents with OI had a genetic confirmation of their diagnosis. Data on height provided further context to individuals’ OI type—most adults were 130–160 cm tall (49%), fewer were 100–130 cm tall (19%). This distribution was similar among adolescents (Table 3).
Most adults and adolescents reported walking unaided both inside and outside. Manual wheelchair use was the second most common mode of mobility (up to 36% of respondents), power chairs in contrast were used by only up to 14% of respondents (Table 3).
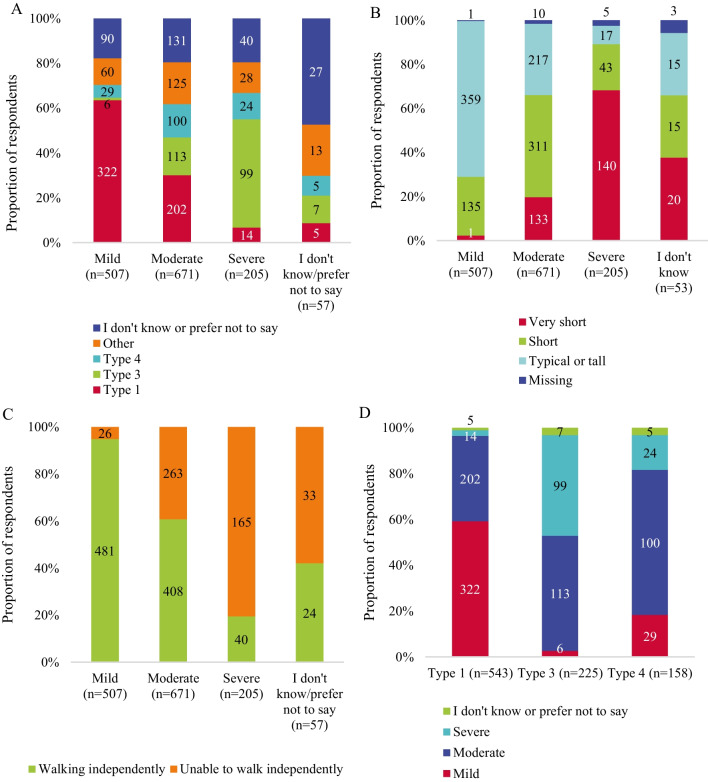
Most adults with mild OI reported OI type 1 (64%), ability to walk independently in- or outside (95%) and typical or tall height (71%; includes women ≥ 150 cm and men ≥ 160 cm). Adults reporting moderate OI were split across clinical OI types: most reported OI type 1 (30%) and similar proportions reported types 3 (17%) and 4 (15%). Adults with moderate OI predominantly reported short height (46%; includes women 120–150 cm and men 130–160 cm) and ability to walk independently (61%). Conversely, adults with severe OI predominantly reported OI type 3 (48%), inability to walk independently (81%) and very short height (68%; women < 120 and men < 130 cm; Fig. 2, Appendix Tables 5, 6, 7, 8).
Fig. 2.
Alignment of OI severity and type (A), severity and height (B)a, and severity and mobility (C)b OI type and severity (D) among adults with OI (n = 1440). OI, osteogenesis imperfecta. aTypical or tall includes women > 150 cm and men > 160 cm height; short includes women 120–150 cm and men 130–160 cm. Women and men < 120 and < 130 cm respectively were grouped in the very short category. Individuals who preferred not to provide their gender were assessed in the female category. bIndividuals who reported to be walking without assistance in- or outside were considered to be walking independetly. All others were considered to be unable to walk independently
Table 5.
Association of OI severity and type among adults with OI (n = 1440)
| n (%) | Type 1 (n = 543) | Type 3 (n = 225) | Type 4 (n = 158) | Other (n = 226) | I don’t know or prefer not to say (n = 288) |
|---|---|---|---|---|---|
| Mild (n = 507) | 322 (64) | 6 (1) | 29 (6) | 60 (12) | 90 (18) |
| Moderate (n = 671) | 202 (30) | 113 (17) | 100 (15) | 125 (19) | 131 (20) |
| Severe (n = 205) | 14 (7) | 99 (48) | 24 (12) | 28 (14) | 40 (20) |
| I don’t know/prefer not to say (n = 57) | 5 (9) | 7 (12) | 5 (9) | 13 (23) | 27 (47) |
Table 6.
Association of OI severity and height among adults with OI (n = 1,440)
| n (%) | Very short (n = 305) | Short (n = 507) | Typical or tall (n = 608) | I don’t know/prefer not to say (n = 20) |
|---|---|---|---|---|
| Mild (n = 507) | 12 (2) | 135 (27) | 359 (71) | 1 (0.2) |
| Moderate (n = 671) | 133 (20) | 311 (46) | 217 (32) | 10 (1) |
| Severe (n = 205) | 140 (68) | 43 (21) | 17 (8) | 5 (2) |
| I don’t know/prefer not to say (n = 57) | 20 (35) | 18 (32) | 15 (26) | 4 (7) |
Table 7.
Association of OI severity and walking status among adults with OI (n = 1440)
| n (%) | Unable to walk independently in-or outside (n = 487) | Walking independently in- or outside (n = 953) |
|---|---|---|
| Mild (n = 507) | 26 (5) | 481 (95) |
| Moderate (n = 671) | 263 (39) | 408 (61) |
| Severe (n = 205) | 165 (80) | 40 (20) |
| I don’t know/prefer not to say (n = 57) | 33 (58) | 24 (42) |
Table 8.
Association of OI type and severity among adults with OI (n = 1440)
| n (%) | Mild | Moderate | Severe | I don’t know or prefer not to say |
|---|---|---|---|---|
| Type 1 (n = 543) | 322 (59) | 202 (37) | 14 (3) | 5 (0.9) |
| Type 3 (n = 225) | 6 (3) | 113 (50) | 99 (44) | 7 (3) |
| Type 4 (n = 158) | 29 (18) | 100 (63) | 24 (15) | 5 (3) |
When considering the relationship between self-reported clinical type and OI severity, adults with OI type 1 commonly reported mild (59%) and moderate (37%) OI severity. Those with OI type 3 were split across moderate (50%) and severe (44%) OI severity. Adults with OI type 4 predominantly reported moderate OI (63%), however mild (18%) and severe OI (15%) were also reported (Fig. 2, Appendix Tables 5, 6, 7, 8).
Proxy respondents
The OI of most proxy respondents was described as moderate by their caregivers (46% of proxy children, 41% of proxy adolescents and 43% of proxy adults; Table 3). Severe OI was least frequently reported among proxy children (19%) and proxy adolescents (19%). However, mild (28%) and severe OI (27%) were reported in similar proportions in proxy adults. Proportions of OI types 1, 3 and 4 were similar across all proxy-reported age groups (Fig. 1B and Table 3). Awareness of clinical OI type and proportion of genetically confirmed diagnoses decreased slightly with increasing proxy-respondent age.
Most children walked inside (71%) and outside (63%), were carried inside (27%) and outside (29%), or used a manual wheelchair inside (13%) and outside (19%). Proportions of proxy adolescents and adults who walked independently (and used a manual wheelchair were distributed similarly to direct respondents. Most children were 100–130 cm tall (38%); For proxy adolescents a height of 130–160 cm was most commonly reported (50%). Equal proportions of proxy adults were 130–160 cm and over 160 cm tall (both 36%; Table 3).
Signs, symptoms and events in the past 12 months
The survey explored the prevalence of clinical signs, symptoms and events in the past 12 months and throughout an individuals’ lifetime. Here, events reported in the past 12 months are explored.
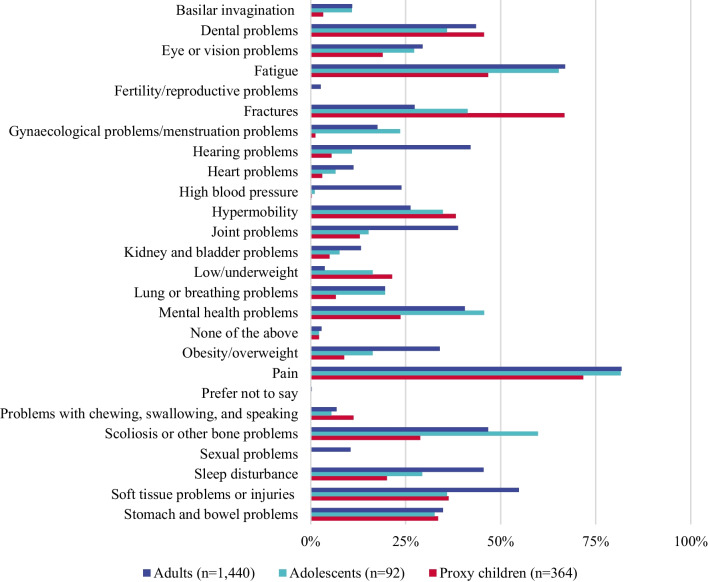
Direct respondents
Pain was the most widely reported condition experienced in the past 12 months in adults (82%) and adolescents (82%); Fig. 3A and Appendix Table 9). Other commonly reported signs, symptoms and events among adults included: fatigue (67%), scoliosis and other bone problems (47%), sleep disturbance (45%), dental problems (43%), hearing problems (42%), mental health problems (41%). In adolescents, in addition to pain, fatigue (65%), scoliosis and other bone problems (60%), mental health problems (46%) and fractures (41%) were common.
Fig. 3.
Prevalence of clinical events, signs and symptoms in participants with OIa. OI, osteogenesis imperfecta. aQuestions 113, 187, 251–253 “Over the past 12 months, have you/your child experienced any of the following signs, symptoms or events? Answer options included 24 options (see above) for adults and 22 options for care recipients and adolescents (excluding sexual health and fertility) and “I don’t know”, “prefer not to say”
Table 9.
Prevalence of clinical signs, symptoms and eventsa
| n, (%) | Adults (n = 1,440) | Adolescents (n = 92) | Proxy children (n = 364) | Proxy adolescents (n = 136) | Proxy adults (n = 95) |
|---|---|---|---|---|---|
| Basilar invagination | 157 (11) | 10 (11) | 12 (3) | 9 (6) | 4 (4) |
| Dental problems | 626 (43) | 33 (36) | 166 (46) | 52 (38) | 35 (37) |
| Eye or vision problems | 424 (29) | 25 (27) | 69 (19) | 21 (15) | 16 (17) |
| Fatigue | 964 (67) | 60 (65) | 170 (47) | 74 (54) | 47 (49) |
| Fertility and reproductive problems | 38 (3) | NA | NA | NA | NA |
| Fractures | 394 (27) | 38 (41) | 243 (67) | 74 (54) | 26 (27) |
| Gynaecological and menstruation problemsb | 174 (17) | 12 (24) | 2 (0.9) | 7 (11) | 7 (17) |
| Hearing problems | 606 (42) | 10 (11) | 20 (5) | 9 (7) | 12 (13) |
| Heart problems | 162 (11) | 6 (7) | 11 (3) | 3 (2) | 1 (1) |
| High blood pressure | 344 (24) | 1 (1) | 1 (0.2) | 0 (0) | 7 (7) |
| Hypermobility | 378 (26) | 32 (35) | 139 (38) | 50 (37) | 21 (22) |
| Joint problems | 558 (39) | 14 (15) | 47 (13) | 31 (23) | 15 (16) |
| Kidney and bladder problems | 190 (13) | 7 (8) | 18 (5) | 6 (4) | 4 (4) |
| Low and underweight | 53 (4) | 15 (16) | 78 (21) | 16 (12) | 8 (8) |
| Lung or breathing problems | 282 (20) | 18 (20) | 24 (7) | 11 (8) | 12 (13) |
| Mental health problems | 584 (41) | 42 (46) | 86 (24) | 37 (27) | 31 (33) |
| Obesity and overweight | 489 (34) | 15 (16) | 32 (9) | 22 (16) | 24 (25) |
| Pain | 1,178 (82) | 75 (82) | 261 (72) | 108 (79) | 72 (76) |
| Problems with chewing, swallowing, and speaking | 98 (7) | 5 (5) | 41 (11) | 4 (3) | 11 (12) |
| Scoliosis or other bone problems | 672 (47) | 55 (60) | 105 (29) | 82 (60) | 38 (40) |
| Sexual problems | 151 (11) | NA | NA | NA | NA |
| Sleep disturbance | 655 (46) | 27 (29) | 73 (20) | 29 (21) | 30 (32) |
| Soft tissue problems or injuries | 789 (55) | 33 (36) | 132 (36) | 71 (52) | 37 (39) |
| Stomach and bowel problems | 501 (35) | 30 (33) | 122 (34) | 34 (25) | 21 (22) |
| None of the above | 41 (3) | 2 (2) | 8 (2) | 3 (2) | 5 (5) |
| Prefer not to say | 4 (0.3) | 0 (0) | 1 (0.2) | 0 (0) | 2 (2) |
aQuestions 113, 187, 251–253 “Over the past 12 months, have you/your child experienced any of the following signs, symptoms or events? Answer options included 24 options (see above) for adults and 22 options for care recipients and adolescents (excluding sexual health and fertility) and “I don’t know”, “prefer not to say” b Calculated as proportion of women and girls responding to the survey
NA, not available
Proxy respondents
In proxy children pain (72%), fractures (67%), fatigue (47%) and dental problems (46%; Fig. 3) were commonly reported. For proxy adolescents such signs, symptoms and events included, pain (79%), scoliosis and other bone problems (60%), fatigue (54%), fractures (54%), and soft tissue injuries (52%; Appendix Table 9); among proxy adults pain (76%) and fatigue (49%) were most common (Appendix Table 9).
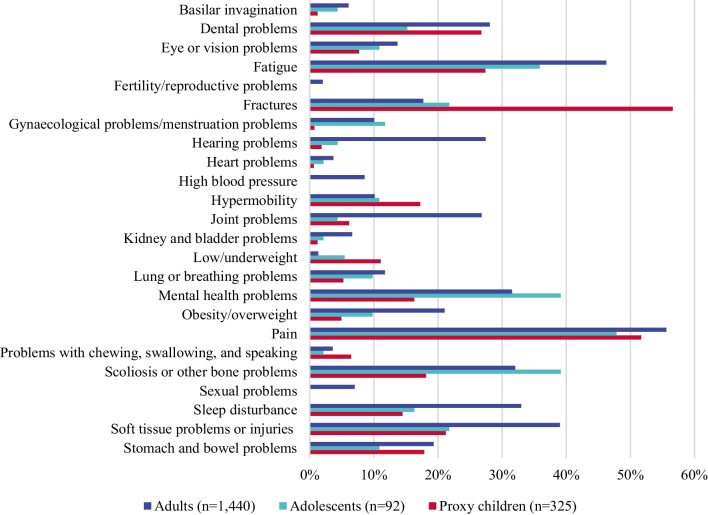
Impact of signs, symptoms and events experienced in the past 12 months
Respondents who reported that they, or individuals with OI in their care, experienced signs, symptoms and events associated with OI were asked follow-up questions on how they were affected by their signs, symptoms and events.
Direct respondents
Pain, fatigue and scoliosis were most commonly reported as moderately-severely impactful by adults and adolescents (56–36% reporting moderate-severe impact; Fig. 4, Appendix Tables 10 and 11). Additionally, adults commonly rated soft tissue (39%) and sleep problems (33%) as moderately-severely impactful, while adolescents most commonly rated mental health problems (39%) and fractures (22%) as moderately-severely impactful signs, symptoms and events.
Fig. 4.
Moderate-severe impact of clinical events, signs and symptoms in adults, adolescents and children with OIa. OI, osteogenesis imperfecta. aQuestions 114, 116, 118–131, 133–142, 188, 191, 193, 194, 195, 197–215, 319, 321, 323, 324, 325, 327–345 “In the past 12 months, how has x impacted your life”, where x is any clinical sign, symptom or event participants reported to have experienced in the past 12 month in questions 113, 187, 251–253. These follow up questions were unavailable for caregivers who provided information on multiple care recipients. Respondents chose a single answer option from a 5-level Likert scale “Not at all impacted–Severely impacted” and I don’t know, prefer not to say. The prevalence of gynaecological problems was calculated within the female subpopulations (n = 1008, n = 51 and n = 137, respectively)
Table 10.
Impact of signs, symptoms and events in adults with OI (n = 1,440)a
| n, (%) | n affectedb | Severely impacted | Moderately impacted | Mildly impacted | Very mildly impacted | Not impacted | I don’t know | Prefer not to say | Missing |
|---|---|---|---|---|---|---|---|---|---|
| Basilar invagination | 157 | 27 (2) | 60 (4) | 48 (3) | 16 (1) | 3 (0.2) | 2 (0.1) | 0 (0) | 1 (0.1) |
| Dental problems | 626 | 166 (12) | 238 (17) | 151 (11) | 51 (4) | 15 (1) | 1 (0.1) | 1 (0.1) | 3 (0.2) |
| Eye or vision problems | 424 | 55 (4) | 142 (10) | 155 (11) | 58 (4) | 9 (0.6) | 2 (0.1) | 0 (0) | 3 (0.2) |
| Fatigue | 964 | 255 (18) | 411 (29) | 216 (15) | 69 (5) | 6 (0.4) | 3 (0.2) | 1 (0.1) | 3 (0.2) |
| Fertility and reproductive problems | 38 | 18 (1) | 11 (0.8) | 2 (0.1) | 2 (0.1) | 5 (0.3) | 0 (0) | 0 (0) | 0 (0) |
| Fractures | 394 | 103 (7) | 152 (11) | 86 (6) | 36 (3) | 11 (0.8) | 3 (0.2) | 1 (0.1) | 2 (0.1) |
| Gynaecological and menstruation problem | 174 | 33 (3) | 68 (7) | 49 (5) | 16 (2) | 5 (0.5) | 1 (0.1) | 2 (0.2) | 0 (0) |
| Hearing problems | 606 | 163 (11) | 232 (16) | 143 (10) | 52 (4) | 12 (0.8) | 1 (0.1) | 0 (0) | 3 (0.2) |
| Heart problems | 162 | 16 (1) | 37 (3) | 45 (3) | 34 (2) | 26 (2) | 4 (0.3) | 0 (0) | 0 (0) |
| High blood pressure | 344 | 27 (2) | 96 (7) | 118 (8) | 61 (4) | 39 (3) | 0 (0) | 1 (0.1) | 2 (0.1) |
| Hypermobility | 378 | 37 (3) | 109 (8) | 104 (7) | 69 (5) | 54 (4) | 5 (0.3) | 0 (0) | 0 (0) |
| Joint problems | 558 | 150 (10) | 236 (16) | 103 (7) | 47 (3) | 16 (1) | 4 (0.3) | 0 (0) | 2 (0.1) |
| Kidney and bladder problems | 190 | 24 (2) | 71 (5) | 57 (4) | 27 (2) | 8 (0.6) | 1 (0.1) | 0 (0) | 2 (0.1) |
| Low/underweight | 53 | 7 (0.5) | 12 (0.8) | 16 (1) | 11 (0.8) | 5 (0.4) | 2 (0.1) | 0 (0) | 0 (0) |
| Lung or breathing problems | 282 | 56 (4) | 113 (8) | 77 (5) | 30 (2) | 5 (0.3) | 0 (0) | 0 (0) | 1 (0.1) |
| Mental health problems | 584 | 187 (13) | 267 (19) | 110 (8) | 19 (1) | 0 (0) | 1 (0.1) | 0 (0) | 0 (0) |
| Obesity/overweight | 489 | 112 (8) | 191 (13) | 120 (8) | 48 (3) | 17 (1) | 1 (0.1) | 0 (0) | 0 (0) |
| Pain | 1,178 | 280 (19) | 521 (36) | 265 (18) | 97 (7) | 7 (0.5) | 1 (0.1) | 2 (0.1) | 5 (0.3) |
| Problems with chewing, swallowing, and speaking | 98 | 22 (2) | 30 (2) | 28 (2) | 16 (1) | 1 (0.1) | 0 (0) | 0 (0) | 1 (0.1) |
| Scoliosis or other bone problems | 672 | 158 (11) | 303 (21) | 147 (10) | 46 (3) | 10 (0.7) | 6 (0.4) | 0 (0) | 2 (0.1) |
| Sexual problems | 151 | 48 (3) | 53 (4) | 34 (2) | 9 (0.6) | 1 (0.1) | 3 (0.2) | 3 (0.2) | 0 (0) |
| Sleep disturbance | 655 | 174 (12) | 301 (21) | 143 (10) | 29 (2) | 4 (0.3) | 1 (0.1) | 1 (0.1) | 2 (0.1) |
| Soft tissue problems or injuries | 789 | 181 (13) | 381 (27) | 154 (11) | 56 (4) | 12 (0.8) | 2 (0.1) | 0 (0) | 3 (0.2) |
| Stomach and bowel problems | 501 | 81 (6) | 197 (14) | 150 (10) | 59 (4) | 11 (0.8) | 0 (0) | 1 (0.1) | 2 (0.1) |
OI, osteogenesis imperfecta
aQuestions 114, 116, 118–131 and 133–142 “In the past 12 months, how has x impacted your life”, where x is any clinical sign, symptom or event participants reported to have experienced in the past 12 month in questions 113. Respondents chose a single answer option from a 5-level Likert scale “Not at all impacted–Severely impacted” and I don’t know, prefer not to say. bBased on responses to question 113. Percentages of affected individuals were calculated for the overall population of 1,440 adults for all but gynaecological problems, where percentages were calculated based on the number of women (n = 1,008) in the survey
Table 11.
Impact of signs, symptoms and events in adolescents (n = 92)a
| n, (%) | n affectedb | Severely impacted | Moderately impacted | Mildly impacted | Very mildly impacted | Not impacted | I don’t know | Prefer not to say | Missing |
|---|---|---|---|---|---|---|---|---|---|
| Basilar invagination | 10 | 0 (0) | 4 (4) | 2 (2) | 4 (4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Dental problems | 33 | 3 (3) | 11 (12) | 12 (13) | 4 (4) | 2 (2) | 0 (0) | 0 (0) | 1 (1) |
| Eye or vision problems | 25 | 2 (2) | 8 (9) | 8 (9) | 5 (5) | 1 (1) | 0 (0) | 0 (0) | 1 (1) |
| Fatigue | 60 | 9 (10) | 24 (26) | 18 (20) | 6 (7) | 1 (1) | 1 (1) | 0 (0) | 1 (1) |
| Fractures | 38 | 6 (7) | 14 (15) | 13 (14) | 3 (3) | 0 (0) | 1 (1) | 0 (0) | 1 (1) |
| Gynaecological and menstruation problems | 12 | 1 (2) | 5 (10) | 3 (6) | 1 (2) | 2 (4) | 0 (0) | 0 (0) | 0 (0) |
| Hearing problems | 10 | 0 (0) | 4 (4) | 2 (2) | 2 (2) | 1 (1) | 0 (0) | 0 (0) | 1 (1) |
| Heart problems | 6 | 0 (0) | 2 (2) | 3 (3) | 0 (0) | 1 (1) | 0 (0) | 0 (0) | 0 (0) |
| High blood pressure | 1 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 0 (0) | 0 (0) | 0 (0) |
| Hypermobility | 32 | 0 (0) | 10 (11) | 12 (13) | 6 (7) | 4 (4) | 0 (0) | 0 (0) | 0 (0) |
| Joint problems | 14 | 1 (1) | 3 (3) | 7 (8) | 1 (1) | 2 (2) | 0 (0) | 0 (0) | 0 (0) |
| Kidney and bladder problems | 7 | 1 (1) | 1 (1) | 1 (1) | 2 (2) | 2 (2) | 0 (0) | 0 (0) | 0 (0) |
| Low and underweight | 15 | 3 (3) | 2 (2) | 1 (1) | 4 (4) | 5 (5) | 0 (0) | 0 (0) | 0 (0) |
| Lung or breathing problems | 18 | 3 (3) | 6 (7) | 6 (7) | 3 (3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Mental health problems | 42 | 18 (20) | 18 (20) | 4 (4) | 2 (2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Obesity and overweight | 15 | 6 (7) | 3 (3) | 6 (6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Pain | 75 | 10 (11) | 34 (37) | 21 (23) | 8 (9) | 1 (1) | 0 (0) | 0 (0) | 1 (1) |
| Problems with chewing, swallowing, and speaking | 5 | 0 (0) | 2 (2) | 2 (2) | 0 (0) | 1 (1) | 0 (0) | 0 (0) | 0 (0) |
| Scoliosis or other bone problems | 55 | 13 (14) | 23 (25) | 9 (10) | 4 (4) | 5 (5) | 0 (0) | 0 (0) | 1 (1) |
| Sleep disturbance | 27 | 6 (7) | 9 (10) | 6 (7) | 3 (3) | 2 (2) | 0 (0) | 0 (0) | 1 (1) |
| Soft tissue problems or injuries | 33 | 6 (7) | 14 (15) | 11 (12) | 2 (2) | 1 (1) | 0 (0) | 0 (0) | 0 (0) |
| Stomach and bowel problems | 30 | 3 (3) | 7 (8) | 10 (11) | 8 (9) | 1 (1) | 0 (0) | 0 (0) | 1 (1) |
OI, osteogenesis imperfecta
aQuestions 319, 321, 323, 324, 325, 327–345 “In the past 12 months, how has x impacted your life”, where x is any clinical sign, symptom or event participants reported to have experienced in the past 12 month in questions 318. Respondents chose a single answer option from a 5-level Likert scale “Not at all impacted–Severely impacted” and I don’t know, prefer not to say. b Based on responses to question 318. Percentages of affected individuals were calculated for the overall population of 92 adolescents for all but gynaecological problems, where percentages were calculated based on the number of girls (n = 51) in the survey
Proxy respondents
Pain (52%), fractures (57%), dental problems (27%), fatigue (27%) and soft tissue problems (21%) were most commonly rated as moderately-severely impactful in children (Fig. 4, Appendix Table 12). Among proxy adolescents such signs, symptoms and events included pain (79%), scoliosis and other bone problems (60%), fractures (54%), fatigue (54%) and soft tissue problems (52%; Appendix Table 13). For proxy adults, most commonly moderately-severely impactful signs, symptoms and events included pain (76%), fatigue (49%), scoliosis and other bone problems (40%), dental problems (37%), sleep disturbance (32%) and mental health problems (33%; Appendix Table 14).
Table 12.
Impact of signs, symptoms and events in proxy children (n = 325)a
| n, (%) | n affectedb | Severely impacted | Moderately impacted | Mildly impacted | Very mildly impacted | Not impacted | I don’t know | Prefer not to say | Missing |
|---|---|---|---|---|---|---|---|---|---|
| Basilar invagination | 12 | 0 (0) | 4 (1) | 1 (0.3) | 2 (0.6) | 3 (0.9) | 1 (0.3) | 0 (0) | 1 (0.3) |
| Dental problems | 166 | 24 (7) | 63 (19) | 44 (14) | 13 (4) | 3 (0.9) | 1 (0.3) | 1 (0.3) | 18 (6) |
| Eye or vision problems | 69 | 6 (2) | 19 (6) | 20 (6) | 11 (3) | 4 (1) | 2 (0.6) | 2 (0.6) | 7 (2) |
| Fatigue | 170 | 26 (8) | 63 (19) | 46 (14) | 13 (4) | 2 (0.6) | 2 (0.6) | 0 (0) | 18 (6) |
| Fractures | 243 | 97 (30) | 87 (27) | 29 (9) | 5 (2) | 1 (0.3) | 1 (0.3) | 1 (0.3) | 23 (7) |
| Gynaecological and menstruation problems | 2 | 0 (0) | 1 (0.7) | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Hearing problems | 20 | 3 (0.9) | 3 (0.9) | 5 (2) | 2 (0.6) | 4 (1) | 0 (0) | 0 (0) | 3 (0.9) |
| Heart problems | 11 | 1 (0.3) | 1 (0.3) | 4 (1) | 1 (0.3) | 4 (1) | 0 (0) | 0 (0) | 0 (0) |
| High blood pressure | 1 | 0 (0) | 0 (0) | 1 (0.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Hypermobility | 139 | 9 (3) | 47 (14) | 26 (8) | 15 (5) | 16 (5) | 5 (2) | 0 (0) | 21 (6) |
| Joint problems | 47 | 8 (2) | 12 (4) | 10 (3) | 9 (3) | 1 (0.3) | 1 (0.3) | 1 (0.3) | 5 (2) |
| Kidney and bladder problems | 18 | 0 (0) | 4 (1) | 10 (3) | 3 (0.9) | 0 (0) | 0 (0) | 0 (0) | 1 (0.3) |
| Low and underweight | 78 | 17 (5) | 19 (6) | 15 (5) | 9 (3) | 9 (3) | 0 (0) | 0 (0) | 9 (3) |
| Lung or breathing problems | 24 | 7 (2) | 10 (3) | 5 (1) | 1 (0.3) | 0 (0) | 1 (0.3) | 0 (0) | 0 (0) |
| Mental health problems | 86 | 20 (6) | 33 (10) | 14 (4) | 5 (2) | 0 (0) | 0 (0) | 0 (0) | 14 (4) |
| Obesity and overweight | 32 | 5 (2) | 11 (3) | 10 (3) | 1 (0.3) | 1 (0.3) | 0 (0) | 0 (0) | 4 (1) |
| Pain | 261 | 60 (18) | 108 (33) | 48 (15) | 12 (4) | 3 (0.9) | 2 (0.6) | 0 (0) | 28 (9) |
| Problems with chewing, swallowing, and speaking | 41 | 10 (3) | 11 (4) | 11 (4) | 5 (2) | 1 (0.3) | 0 (0) | 0 (0) | 3 (0.9) |
| Scoliosis or other bone problems | 105 | 27 (8) | 32 (10) | 21 (6) | 7 (2) | 5 (2) | 3 (0.9) | 0 (0) | 10 (3) |
| Sleep disturbance | 73 | 20 (6) | 27 (8) | 12 (4) | 4 (1) | 0 (0) | 0 (0) | 0 (0) | 10 (3) |
| Soft tissue problems or injuries | 132 | 16 (5) | 53 (16) | 33 (10) | 9 (3) | 1 (0.3) | 5 (2) | 0 (0) | 15 (5) |
| Stomach and bowel problems | 122 | 15 (5) | 43 (13) | 34 (10) | 11 (3) | 5 (2) | 1 (0.3) | 0 (0) | 13 (4) |
OI, osteogenesis imperfecta
aQuestions 188, 191, 193, 194, 195, 197–215 “In the past 12 months, how has x impacted your child’s life”, where x is any clinical sign, symptom or event participants reported to have experienced in the past 12 month in questions 187. Respondents chose a single answer option from a 5-level Likert scale “Not at all impacted–Severely impacted” and I don’t know, prefer not to say. bBased on responses to question 187. Percentages of affected individuals were calculated for the overall population of 325 children for all but gynaecological problems, where percentages were calculated based on the number of girls (n = 137) in the survey
Table 13.
Impact of signs, symptoms and events in proxy adolescents (n = 118)a
| n, (%) | n affectedb | Severely impacted | Moderately impacted | Mildly impacted | Very mildly impacted | Not impacted | I don’t know | Prefer not to say | Missing |
|---|---|---|---|---|---|---|---|---|---|
| Basilar invagination | 9 | 0 (0) | 4 (3) | 2 (2) | 0 (0) | 1 (0.9) | 0 (0) | 0 (0) | 2 (2) |
| Dental problems | 52 | 6 (5) | 21 (18) | 14 (12) | 3 (3) | 1 (0.9) | 0 (0) | 0 (0) | 7 (6) |
| Eye or vision problems | 21 | 3 (3) | 5 (4) | 7 (6) | 3 (3) | 1 (0.9) | 0 (0) | 0 (0) | 2 (2) |
| Fatigue | 74 | 13 (11) | 25 (21) | 16 (14) | 7 (6) | 1 (0.9) | 0 (0) | 0 (0) | 12 (10) |
| Fractures | 74 | 22 (19) | 23 (19) | 18 (15) | 1 (0.9) | 0 (0) | 0 (0) | 0 (0) | 10 (8) |
| Gynaecological and menstruation problems | 7 | 1 (2) | 6 (11) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Hearing problems | 9 | 2 (2) | 3 (3) | 1 (0.9) | 3 (3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Heart problems | 3 | 0 (0) | 1 (0.9) | 1 (0.9) | 1 (0.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| High blood pressure | 0 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Hypermobility | 50 | 6 (5) | 11 (9) | 10 (8) | 8 (7) | 7 (6) | 1 (0.9) | 0 (0) | 7 (6) |
| Joint problems | 31 | 5 (4) | 13 (11) | 5 (4) | 2 (2) | 1 (0.9) | 0 (0) | 0 (0) | 5 (4) |
| Kidney and bladder problems | 6 | 0 (0) | 6 (5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Low and underweight | 16 | 2 (2) | 4 (3) | 7 (6) | 1 (0.9) | 0 (0) | 0 (0) | 0 (0) | 2 (2) |
| Lung or breathing problems | 11 | 3 (3) | 4 (3) | 3 (3) | 1 (0.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Mental health problems | 37 | 7 (6) | 17 (14) | 5 (4) | 2 (2) | 0 (0) | 0 (0) | 0 (0) | 6 (5) |
| Obesity and overweight | 22 | 5 (4) | 8 (7) | 3 (3) | 0 (0) | 3 (3) | 0 (0) | 0 (0) | 3 (3) |
| Pain | 108 | 22 (19) | 42 (36) | 19 (16) | 8 (7) | 1 (0.9) | 0 (0) | 0 (0) | 16 (14) |
| Problems with chewing, swallowing, and speaking | 4 | 3 (3) | 0 (0) | 1 (0.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Scoliosis or other bone problems | 82 | 25 (21) | 24 (20) | 15 (13) | 5 (4) | 2 (2) | 1 (0.9) | 0 (0) | 10 (8) |
| Sleep disturbance | 29 | 8 (7) | 14 (12) | 3 (3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 4 (3) |
| Soft tissue problems or injuries | 71 | 4 (3) | 29 (25) | 18 (15) | 7 (6) | 5 (4) | 0 (0) | 0 (0) | 7 (6) |
| Stomach and bowel problems | 34 | 5 (4) | 12 (10) | 10 (8) | 3 (3) | 1 (0.9) | 0 (0) | 0 (0) | 3 (3) |
OI, osteogenesis imperfecta
aQuestions 319, 321, 323, 324, 325, 327–345 “In the past 12 months, how has x impacted your life”, where x is any clinical sign, symptom or event participants reported to have experienced in the past 12 month in questions 318. Respondents chose a single answer option from a 5-level Likert scale “Not at all impacted–Severely impacted” and I don’t know, prefer not to say. bBased on responses to question 318. Percentages of affected individuals were calculated for the overall population of 118 adolescents for all but gynaecological problems, where percentages were calculated based on the number of girls (n = 57) in the survey
Table 14.
Impact of signs, symptoms and events in proxy adults (n = 85)a
| n, (%) | n affectedb | Severely impacted | Moderately impacted | Mildly impacted | Very mildly impacted | Not impacted | I don’t know | Prefer not to say | Missing |
|---|---|---|---|---|---|---|---|---|---|
| Basilar invagination | 4 | 1 (1) | 0 (0) | 1 (1) | 0 (0) | 0 (0) | 2 (2) | 0 (0) | 0 (0) |
| Dental problems | 35 | 9 (11) | 16 (19) | 8 (9) | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 1 (1) |
| Eye or vision problems | 16 | 0 (0) | 5 (6) | 8 (9) | 3 (4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Fatigue | 47 | 8 (9) | 21 (25) | 12 (14) | 2 (2) | 0 (0) | 0 (0) | 0 (0) | 4 (5) |
| Fractures | 26 | 4 (5) | 14 (16) | 2 (2) | 1 (1) | 1 (1) | 1 (1) | 0 (0) | 3 (4) |
| Gynaecological and menstruation problems | 7 | 1 (3) | 5 (13) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (3) |
| Hearing problems | 12 | 1 (1) | 6 (7) | 0 (0) | 3 (4) | 1 (1) | 0 (0) | 0 (0) | 1 (1) |
| Heart problems | 1 | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| High blood pressure | 7 | 0 (0) | 4 (5) | 1 (1) | 2 (2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Hypermobility | 21 | 0 (0) | 6 (7) | 9 (11) | 3 (4) | 1 (1) | 0 (0) | 0 (0) | 2 (2) |
| Joint problems | 15 | 2 (2) | 7 (8) | 4 (5) | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 1 (1) |
| Kidney and bladder problems | 4 | 1 (1) | 2 (2) | 0 (0) | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Low and underweight | 8 | 3 (4) | 0 (0) | 1 (1) | 0 (0) | 3 (4) | 0 (0) | 0 (0) | 1 (1) |
| Lung or breathing problems | 12 | 5 (6) | 4 (5) | 3 (4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Mental health problems | 31 | 12 (14) | 11 (13) | 5 (6) | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 2 (2) |
| Obesity and overweight | 24 | 7 (8) | 9 (11) | 6 (7) | 2 (2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Pain | 72 | 17 (20) | 30 (35) | 11 (13) | 6 (7) | 0 (0) | 1 (1) | 0 (0) | 7 (8) |
| Problems with chewing, swallowing, and speaking | 11 | 4 (5) | 4 (5) | 0 (0) | 2 (2) | 1 (1) | 0 (0) | 0 (0) | 0 (0) |
| Scoliosis or other bone problems | 38 | 17 (20) | 10 (12) | 6 (7) | 2 (2) | 1 (1) | 0 (0) | 0 (0) | 2 (2) |
| Sleep disturbance | 30 | 5 (6) | 18 (21) | 5 (6) | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 1 (1) |
| Soft tissue problems or injuries | 37 | 3 (4) | 16 (19) | 9 (11) | 2 (2) | 1 (1) | 2 (2) | 0 (0) | 4 (5) |
| Stomach and bowel problems | 21 | 4 (5) | 9 (11) | 4 (5) | 2 (2) | 0 (0) | 0 (0) | 0 (0) | 2 (2) |
OI, osteogenesis imperfecta
aQuestions 319, 321, 323, 324, 325, 327–345 “In the past 12 months, how has x impacted your life”, where x is any clinical sign, symptom or event participants reported to have experienced in the past 12 month in questions 318. Respondents chose a single answer option from a 5-level Likert scale “Not at all impacted–Severely impacted” and I don’t know, prefer not to say. bBased on responses to question 318. Percentages of affected individuals were calculated for the overall population of 85 adults for all but gynaecological problems, where percentages were calculated based on the number of women (n = 39) in the survey
Discussion
The IMPACT Survey has compiled the largest known patient-reported dataset on the experience of individuals with OI (n = 2312 individuals across self- and proxy reports), and their caregivers (n = 560) to date. This was achieved through an ambitious and self-driven collaboration between the clinical and OI communities, aided by third-party funding from a pharmaceutical manufacturer. Past research on the impact of OI on individuals and their caregivers has been limited by small sample sizes and did not cover the breadth of topics included in IMPACT [6, 7, 9, 18, 19]. Therefore, IMPACT was designed as an online survey to maximise accessibility across geographies and included questions covering a breadth of topics exploring the clinical, humanistic, and economic impact of OI that may be insufficiently documented in the existing literature.
While in this survey sample self-reported OI severity correlated well with other characteristics like height, mobility and clinical OI type, OI types were split across multiple OI severities. This finding mirrors previous research and suggests that “severity” is a holistic, patient-centric view of individuals’ health, that is not entirely captured by the clinical OI type which is determined based on clinical and molecular patient characteristics [20, 21]. Additionally, while general predictions about the clinical OI type can be made based on the causative gene, mutation type and location, genetic variation alone does not account for all phenotypic variation [22–24].
Some characteristics of this sample reflect the nature of the study. While OI is equally prevalent in men and women, most direct respondents to the survey were female. This is in line with past patient-reported outcomes research in OI, where an increased participation of women with OI and female caregivers is common [9]. Most direct respondents were from Europe and European respondents made up > 50% of participants. This strong representation of European individuals is unsurprising as survey languages and recruitment efforts focussed on this region, although the survey was open to participants from any geography. OI type 1, which is commonly associated with mild OI, was the most commonly reported type across direct and proxy respondents. This is a somewhat lower prevalence of type 1 than reported in past population-based studies, but in line with other large surveys among individuals with OI [1, 20, 25]. Past research has shown that in samples selected primarily based on individuals’ availability and willingness to participate, more engaged individuals (e.g., those who participate more in a computer game or are more involved with an organisation) who may also be more severely affected by a given health concern are overrepresented [26, 27]. Moreso, past patient-reported outcomes research similarly underrepresented individuals with OI type 1 [9, 28].
The survey includes adults (both self- and proxy reported), adolescents (self- and proxy reported), caregivers (with and without OI) of individuals with OI, children (proxy-reported), and relatives of individuals with OI. Caregivers also provided information on the OI-related QoL of any siblings to individuals with OI in their care. For some of these populations few data are available elsewhere: comparatively few studies, which commonly have small samples, provide information on the wellbeing of caregivers and siblings [29, 30] and few studies include self-reporting adolescents [9].
This study found that, irrespective of age, individuals with OI experience numerous signs, symptoms and events that affect their HRQoL. Pain was highly prevalent and impactful on the HRQoL of individuals with OI, as reported in past research [20, 31–33]. Notably, fatigue, which has rarely been explored in children, was prevalent in children in this sample, but much less so than adults or adolescents. Past research also found that fatigue was prevalent in adults but not children [20, 34]. Furthermore, our data suggest that fatigue may be underreported in caregiver-based studies: in our dataset, fatigue was reported by much higher proportions of self-reporting compared with proxy-reported individuals. This discrepancy has also been detected for numerous other clinical events, signs and symptoms including, in adolescents compared with proxy adolescents, gynaecological and menstruation problems, mental health problems, sleep disturbance and stomach and bowel problems. Similarly, differences were also common among reports of adults compared with proxy adults, for example in the proportion of individuals experiencing hearing problems, fatigue, sleep disturbance, stomach and bowel problems and mental health problems. While the survey does not include self-reported paediatric data, this suggests that differences in self- and proxy report may be an issue in the paediatric population as well. Past literature largely reports that parents underreport pain and some other not directly observable health conditions, however some reports found relatively high agreement between self- and proxy report [35–42]. Nonetheless, underreporting may contribute to suboptimal health outcomes due to lack of attention focused on understanding a health issue; while there are few reports on bowel problems in the OI population, past research lists diseases of the digestive system as a common cause of death [43, 44]. Among adults and adolescents, our survey has found a high prevalence of bowel and stomach issues.
Our survey has also detected a high prevalence of mental health problems in adults, adolescents and, to a lesser extent, children. Past literature on the mental health impact of OI is conflicting: while some reports found higher prevalence of mental health issues in adults and children, others have reported that the mental health of individuals with OI is preserved which in part may be due to the adaptation process experienced by individuals with chronic conditions [8, 19, 20, 31, 34, 45–47]. More detailed exploration of the mental health impact of OI and affected areas of life will be the subject of additional analyses of the IMPACT dataset.
A mental health impact of OI may be aligned with participants’ responses on the effect of signs, symptoms and events on their life. Pain and fatigue were commonly perceived as negatively impactful across survey populations and these conditions have indeed been associated with a negative impact on mental health in past reports [48–50]. Additionally, the negative impact of OI may increase with age: larger proportions of adults described signs, symptoms and events they experienced as moderately-severely impactful compared with adolescents. This may be due to an overall increasing burden of health events and/or a progressively decreasing resilience to health events.
Similarly sleep disturbance was commonly reported among all age groups. This finding is aligned with past literature [20, 34, 51, 52] and may be correlated with the findings of a high prevalence of mental health issues and fatigue in the OI population [53–55]
It remains to be explored whether the changes in prevalence and impact of clinical symptoms are caused by underlying differences in respondent demographics, differences in awareness and perception of symptoms by individuals with OI and their caregivers, or changes in symptom intensity or resilience.
Further analysis of the survey responses may fill current data gaps in our understanding of the lived experience of the OI community, to improve treatment and care, and to evaluate potential differences across diverse geographical or cultural settings.
Strengths and limitations
The IMPACT survey was developed in collaboration with researchers and OI community members to ensure that the survey design is relevant and inclusive. To this end, questions were adjusted to fit multiple demographics, including individuals who are underrepresented in existing research. The design was also adapted to cover a wide range of geographies, include relevant and culturally appropriate answer options, and was translated into 8 languages to include as many members of the community as possible. However, though IMPACT did not include any validated patient-reported outcome tools, questions were validated by members of the OI community and academic researchers. Our study does not include a control population which limits the generalisability of our findings; comparison with past population-based research can provide insights into the significance of our findings but may not be able to fully mitigate this shortcoming. Questions about ethnicity were omitted due to the breadth of potential fielding geographies and the resulting multitude of possible responses and respondent attitudes on questions about this topic.
During its 3-month fielding period the survey generated a large sample that includes a wide range of community members including demographics for which few data are available, e.g., adolescents and caregivers (with or without OI) of multiple individuals with OI. Despite our best efforts to recruit men, most survey respondents were female. As the survey includes a convenience sample of individuals recruited by patient organisations, the survey population includes those who were able to respond to a survey online and are engaged with PAOs.
Lastly, any self-reported data are limited by the respondents’ accuracy and recall bias. As the survey was fielded in 2021 under the extraordinary circumstances of the Coronavirus Disease Pandemic 2019 (COVID-19) pandemic in 2021 this bias may be exacerbated, and the generalisability of some survey outcomes may be affected. To mitigate this limitation and contextualise survey findings, the survey included questions about behavioural changes among individuals with OI and caregivers due to the COVID-19 pandemic.
Conclusion
IMPACT has generated an extensive dataset on the experience of individuals with OI, their caregivers and relatives. Upcoming analyses of the IMPACT data will further our understanding of the humanistic, economic and clinical burden of OI and contribute to improved treatment and care for the OI community.
Supplementary Information
Additional file 1. IMPACT Survey Questionnaire.
Acknowledgements
The authors thank members of the OIF and OIFE for their participation in the development and dissemination of the IMPACT survey. We are also grateful for every respondent taking the time to participate and provide information for this research. Authors further thank Ruby Dadzie and Alysia Battersby, of Wickenstones, who helped to analyse data presented here.
Appendix
Author contributions
IW, TH, TvW, LLW, OS, CR, MBB, MR, SP and FR contributed to the planning of this research. SP and MR drafted and implemented survey questions. IW, TH, TvW, LLW, OS, CR, MBB and FR reviewed proposed survey content. MR analysed data and drafted the manuscript. IW, TH, TvW, LLW, OS, CR, MBB, SP and FR contributed to the planning of the manuscript, reviewed the work, provided revisions and final approval for the publication of this version of the manuscript. All authors read and approved by the final manuscript.
Funding
Funding for this research was provided by Mereo BioPharma Group, London, United Kingdom.
Availability of data and materials
The data that support the findings of this study are not openly available due to reasons of sensitivity. They are managed by a data management committee and are available upon reasonable request to the authors.
Declarations
Ethics approval and consent to participate
An ethics approval exemption was granted by Pearl IRB, Indianapolis, IN, USA.
Consent for publication
Not applicable.
Competing interests
SP and MR are employees of Wickenstones Ltd, Abingdon, United Kingdom. Wickenstones. MB and CR have received payments for their contributions to the present manuscript. MB has received grants and from Ultragenyx Pharmaceuticals Inc, Novato, USA. and the Osteogenesis Imperfecta Foundation. TH serves as the Chief Executive Officer of the Osteogenesis Imperfecta Foundation and has received unrestricted educational grants from Mereo BioPharma Group London, United Kingdom and Ultragenyx Pharmaceuticals Inc, Novato, USA. OS has participated in a national advisory board for Mereo BioPharma Group London, United Kingdom. FR has received study contracts for experimental preclinical studies with Precithera Inc, Quebec, Canada, Mesentech Inc, Vancouver, Canada and Catabasis Pharmaceuticals Inc, Cambridge, USA. He has participated in advisory boards for Ultragenyx Pharmaceuticals Inc, Novato, USA, Sanofi S.A. Paris, France, Novartis International AG, Basel, Switzerland and Mereo BioPharma Group, London, United Kingdom. FR has received a speaker fee from Ultragenyx Pharmaceuticals Inc, Novato, USA for a lecture and received a donation of experimental drugs for a preclinical study from Acceleron Pharma Inc, Cambridge, USA. CR received an institutional grant from and has been a speaker for BioMarin Pharmaceuticals Inc, Novato, California, has participated in advisory boards for Ultragenyx Pharmaceuticals Inc, Novato, USA. She has received an institutional grant from and is a consultant for Nextcure, Beltville, MD, USA. CR sits on the board of directors of the Osteogenesis Imperfecta Foundation. CR has also participated in an advisory board for Mereo BioPharma Group, London, United Kingdom. TW and IW hold leadership positions in the Osteogenesis Imperfecta Federation Europe, which has received grants from Mereo BioPharma Group, London, United Kingdom (unrestricted), Ultragenyx Pharmaceuticals Inc, Novato, USA (restricted grant for a conference), Quince Therapeutics Inc, San Francisco, CA, USA (donation for a conference), UCB (restricted grant to conference), Angitia Biopharmaceuticals Inc., Woodland Hills, CA, USA (donation to conference), Azafaros BV, Naarden, the Netherlands (donation to conference), Alexion Inc. Boston, MA, USA, (sponsorship of conference); Pega Medical Inc, Laval, Quebec, Canada (donation), Sanofi S.A. Paris, France (payment to IW for engagement in steering committee; donated to OIFE). IW has also received payment as a panellist from Takeda, Tokyo, Japan.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Marini JC, et al. Osteogenesis imperfecta. Nat Rev Dis Primers. 2017;3:17052. doi: 10.1038/nrdp.2017.52. [DOI] [PubMed] [Google Scholar]
- 2.Folkestad L. Mortality and morbidity in patients with osteogenesis imperfecta in Denmark. Dan Med J. 2018; 65(4). [PubMed]
- 3.Bishop N. Osteogenesis Imperfecta. In: Orphanet encyclopedia. 2021.
- 4.Marom R, Rabenhorst BM, Morello R. Osteogenesis imperfecta: an update on clinical features and therapies. Eur J Endocrinol. 2020;183(4):R95–r106. doi: 10.1530/EJE-20-0299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rossi V, Lee B, Marom R. Osteogenesis imperfecta: advancements in genetics and treatment. Curr Opin Pediatr. 2019;31(6):708–715. doi: 10.1097/MOP.0000000000000813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hill M, et al. Exploring the impact of Osteogenesis Imperfecta on families: a mixed-methods systematic review. Disabil Health J. 2019;12(3):340–349. doi: 10.1016/j.dhjo.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Mc Donald D, et al. Systematic review of health related-quality of life in adults with osteogenesis imperfecta. Orphanet J Rare Dis. 2023;18(1):36. doi: 10.1186/s13023-023-02643-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dogba MJ, et al. The impact of severe osteogenesis imperfecta on the lives of young patients and their parents—a qualitative analysis. BMC Pediatr. 2013;13:153. doi: 10.1186/1471-2431-13-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rapoport M, et al. The patient clinical journey and socioeconomic impact of osteogenesis imperfecta: a systematic scoping review. Orphanet J Rare Dis. 2023;18(1):34. doi: 10.1186/s13023-023-02627-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murphy A, Howard A, Sochett E. Financial burden in families of children with osteogenesis imperfecta (OI). 8th International. 2017.
- 11.Tsimicalis A et al. Use of Netnography to Understand GoFundMe(®) crowdfunding profiles posted for individuals and families of children with osteogenesis imperfecta. Healthcare. 2022; 10(8). [DOI] [PMC free article] [PubMed]
- 12.Dye DE, et al. The impact of single gene and chromosomal disorders on hospital admissions of children and adolescents: a population-based study. Public Health Genomics. 2011;14(3):153–161. doi: 10.1159/000321767. [DOI] [PubMed] [Google Scholar]
- 13.Ruiter-Ligeti J, et al. Pregnancy outcomes in women with osteogenesis imperfecta: a retrospective cohort study. J Perinatol. 2016;36(10):828–831. doi: 10.1038/jp.2016.111. [DOI] [PubMed] [Google Scholar]
- 14.Darbà J, Marsà A. Hospital incidence, management and direct cost of osteogenesis imperfecta in Spain: a retrospective database analysis. J Med Econ, 2020; 1–6. [DOI] [PubMed]
- 15.Belyea CM, Knox JB. Spinal fusion in children with osteogenesis imperfecta: a nationwide retrospective comparative cohort study over a 12-year period. Current Orthopaedic Practice. 2020;31(1):72–75. doi: 10.1097/BCO.0000000000000805. [DOI] [Google Scholar]
- 16.Kolovos S, Javaid MK. Hospital admissions of patients with osteogenesis imperfecta in the English NHS. Osteoporosis 2020; ora.ox.ac.uk. [DOI] [PMC free article] [PubMed]
- 17.Vitale MG, et al. Osteogenesis imperfecta: determining the demographics and the predictors of death from an inpatient population. J Pediatr Orthop. 2007;27(2):228–232. doi: 10.1097/BPO.0b013e31803179e2. [DOI] [PubMed] [Google Scholar]
- 18.Dahan-Oliel N, et al. Quality of life in osteogenesis imperfecta: a mixed-methods systematic review. Am J Med Genet A. 2016;170a(1):62–76. doi: 10.1002/ajmg.a.37377. [DOI] [PubMed] [Google Scholar]
- 19.Hill CL, Baird WO, Walters SJ. Quality of life in children and adolescents with Osteogenesis Imperfecta: a qualitative interview based study. Health Qual Life Outcomes. 2014;12:54. doi: 10.1186/1477-7525-12-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tosi LL, et al. Initial report of the osteogenesis imperfecta adult natural history initiative. Orphanet J Rare Dis. 2015;10:146. doi: 10.1186/s13023-015-0362-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Dijk FS, Sillence DO. Osteogenesis imperfecta: clinical diagnosis, nomenclature and severity assessment. Am J Med Genet A, 2014; 164a(6): 1470–81. [DOI] [PMC free article] [PubMed]
- 22.Storoni S, et al. From genetics to clinical implications: a study of 675 Dutch Osteogenesis imperfecta patients. Biomolecules. 2023 doi: 10.3390/biom13020281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhytnik L, et al. Inter-and intrafamilial phenotypic variability in individuals with collagen-related osteogenesis imperfecta. Clin Transl Sci. 2020;13(5):960–971. doi: 10.1111/cts.12783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sillence DO, Rimoin DL, Danks DM. Clinical variability in osteogenesis imperfecta-variable expressivity or genetic heterogeneity. Birth Defects Orig Artic Ser. 1979;15(5B):113–129. [PubMed] [Google Scholar]
- 25.Kuurila K, et al. Hearing loss in Finnish adults with osteogenesis imperfecta: a nationwide survey. Ann Otol Rhinol Laryngol. 2002;111(10):939–946. doi: 10.1177/000348940211101014. [DOI] [PubMed] [Google Scholar]
- 26.Maclennan B, et al. Non-response bias in a community survey of drinking, alcohol-related experiences and public opinion on alcohol policy. Drug Alcohol Depend. 2012;126(1–2):189–194. doi: 10.1016/j.drugalcdep.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 27.Khazaal Y, et al. Does self-selection affect samples’ representativeness in online surveys? An investigation in online video game research. J Med Internet Res. 2014;16(7):e164. doi: 10.2196/jmir.2759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gooijer K et al. A baseline measurement of quality of life in 322 adults with osteogenesis imperfecta. JBMR Plus, 2020. [DOI] [PMC free article] [PubMed]
- 29.Wiggins S, Kreikemeier R, Struwe L. Parents’ perceptions of health-related quality of life of children diagnosed with osteogenesis imperfecta. J Pediatr Nurs. 2020;55:75–82. doi: 10.1016/j.pedn.2020.06.009. [DOI] [PubMed] [Google Scholar]
- 30.Santos MCD, et al. Family experience with osteogenesis imperfecta type 1: the most distressing situations. Disabil Rehabil. 2018;40(19):2281–2287. doi: 10.1080/09638288.2017.1334236. [DOI] [PubMed] [Google Scholar]
- 31.Orlando G et al. Physical function in UK adults with osteogenesis imperfecta: a cross-sectional analysis of the RUDY study. Osteoporos Int. 2020. [DOI] [PubMed]
- 32.Zack P, et al. Fracture and non-fracture pain in children with osteogenesis imperfecta. Acta Paediatr. 2005;94(9):1238–1242. doi: 10.1111/j.1651-2227.2005.tb02082.x. [DOI] [PubMed] [Google Scholar]
- 33.Provenzano AH, Åström E, Löwing K. Exploring pain interference and self-perceived health status in children with osteogenesis imperfecta - a cross-sectional study. BMC Musculoskelet Disord. 2022;23(1):876. doi: 10.1186/s12891-022-05825-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tosi LL, et al. Assessing disease experience across the life span for individuals with osteogenesis imperfecta: challenges and opportunities for patient-reported outcomes (PROs) measurement: a pilot study. Orphanet J Rare Dis. 2019;14(1):23. doi: 10.1186/s13023-019-1004-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou H, Roberts P, Horgan L. Association between self-report pain ratings of child and parent, child and nurse and parent and nurse dyads: meta-analysis. J Adv Nurs. 2008;63(4):334–342. doi: 10.1111/j.1365-2648.2008.04694.x. [DOI] [PubMed] [Google Scholar]
- 36.Cohen LL, Vowles KE, Eccleston C. Adolescent chronic pain-related functioning: concordance and discordance of mother-proxy and self-report ratings. Eur J Pain. 2010;14(8):882–886. doi: 10.1016/j.ejpain.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 37.Waters E, Stewart-Brown S, Fitzpatrick R. Agreement between adolescent self-report and parent reports of health and well-being: results of an epidemiological study. Child Care, Health Develop, 2003; 29(6): 501–9. [DOI] [PubMed]
- 38.Sundblad GMB, Saartok T, Engström LMT. Child—parent agreement on reports of disease, injury and pain. BMC Public Health. 2006;6(1):276. doi: 10.1186/1471-2458-6-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kröner-Herwig B et al. Agreement of parents and children on characteristics of pediatric headache, other pains, somatic symptoms, and depressive symptoms in an epidemiologic study. Clin J Pain, 2009; 25(1). [DOI] [PubMed]
- 40.Vetter TR, et al. Patient versus parental perceptions about pain and disability in children and adolescents with a variety of chronic pain conditions. Pain Res Manag. 2014;19(1):7–14. doi: 10.1155/2014/736053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kamper SJ, Dissing KB, Hestbaek L. Whose pain is it anyway? Comparability of pain reports from children and their parents. Chiropractic Manual Ther. 2016;24(1):24. doi: 10.1186/s12998-016-0104-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Montgomery KE, et al. Comparison of child self-report and parent proxy-report of symptoms: results from a longitudinal symptom assessment study of children with advanced cancer. J Spec Pediatr Nurs. 2021;26(3):e12316. doi: 10.1111/jspn.12316. [DOI] [PubMed] [Google Scholar]
- 43.Folkestad L, et al. Mortality and causes of death in patients with osteogenesis imperfecta: a register-based nationwide cohort study. J Bone Miner Res. 2016;31(12):2159–2166. doi: 10.1002/jbmr.2895. [DOI] [PubMed] [Google Scholar]
- 44.Martins G, et al. Bladder and bowel symptoms experienced by children with osteogenesis imperfecta. J Pediatr (Rio J) 2020;96(4):472–478. doi: 10.1016/j.jped.2018.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Balkefors V, et al. Functioning and quality of life in adults with mild-to-moderate osteogenesis imperfecta. Physiother Res Int. 2013;18(4):203–211. doi: 10.1002/pri.1546. [DOI] [PubMed] [Google Scholar]
- 46.Forestier-Zhang L, et al. Health-related quality of life and a cost-utility simulation of adults in the UK with osteogenesis imperfecta, X-linked hypophosphatemia and fibrous dysplasia. Orphanet J Rare Dis. 2016;11(1):160. doi: 10.1186/s13023-016-0538-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Graf A, et al. Gait characteristics and functional assessment of children with type I osteogenesis imperfecta. J Orthop Res. 2009;27(9):1182–1190. doi: 10.1002/jor.20871. [DOI] [PubMed] [Google Scholar]
- 48.Vanz AP, et al. Health-related quality of life of children and adolescents with osteogenesis imperfecta: a cross-sectional study using PedsQL™. BMC Pediatr. 2018;18(1):95. doi: 10.1186/s12887-018-1077-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kroenke K, et al. Chronic fatigue in primary care. Prevalence, patient characteristics, and outcome. Jama. 1988;260(7):929–34. doi: 10.1001/jama.1988.03410070057028. [DOI] [PubMed] [Google Scholar]
- 50.Skapinakis P, Lewis G, Meltzer H. Clarifying the relationship between unexplained chronic fatigue and psychiatric morbidity: results from a community survey in Great Britain. Am J Psychiatry. 2000;157(9):1492–1498. doi: 10.1176/appi.ajp.157.9.1492. [DOI] [PubMed] [Google Scholar]
- 51.Arponen H, et al. Is sleep apnea underdiagnosed in adult patients with osteogenesis imperfecta? -a single-center cross-sectional study. Orphanet J Rare Dis. 2018;13(1):231. doi: 10.1186/s13023-018-0971-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hill C et al. Sleep-related problems in children with osteogenesis imperfecta. 2019: bmjopenrespres.bmj.com.
- 53.McCallum SM, et al. Associations of fatigue and sleep disturbance with nine common mental disorders. J Psychosom Res. 2019;123:109727. doi: 10.1016/j.jpsychores.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 54.Batterham PJ, Glozier N, Christensen H. Sleep disturbance, personality and the onset of depression and anxiety: prospective cohort study. Aust N Z J Psychiatry. 2012;46(11):1089–1098. doi: 10.1177/0004867412457997. [DOI] [PubMed] [Google Scholar]
- 55.Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059–1068. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. IMPACT Survey Questionnaire.
Data Availability Statement
The data that support the findings of this study are not openly available due to reasons of sensitivity. They are managed by a data management committee and are available upon reasonable request to the authors.