ABSTRACT
Objectives
The use of instrument-assisted soft tissue mobilization (IASTM) has been documented to be effective for improving pain and function, but it is unclear whether it helps improve muscle performance in musculoskeletal diseases. This study investigated the effects of IASTM combined with exercise therapy on muscle endurance and pain intensity in patients with chronic neck pain.
Methods
Forty-eight individuals with chronic neck pain were randomly divided into exercise therapy (ET, n = 24) and combined therapy (CT, n = 24) groups. For 4 weeks, each group underwent exercise therapy 3 days a week for a total of 12 sessions. The ET group received exercise therapy only. The CT group received IASTM combined with exercise therapy twice per week for a total of 8 sessions. The muscle endurance of the participants was assessed with the Deep Neck Flexor Muscle Endurance (DNFE) test and pain intensity with Visual Analogue Scale (VAS) at baseline and post-treatment.
Results
While both groups showed significant improvement in pain intensity (p < 0.05), the CT group showed a greater effect size for pain (CT group: Cohen’s d = 3.28; ET group: Cohen’s d = 2.12). The CT group showed significant improvement for muscle endurance (p < 0.05), whereas the ET group did not (p > 0.05).
Conclusion
In the current study, the IASTM intervention combined with ET improved pain and muscular endurance in participants with chronic neck pain compared to exercise therapy alone. As an alternative method, IASTM intervention before exercise seems to increase the short-term recovery effect in chronic neck pain conditions.
KEYWORDS: Chronic neck pain, instrument-assisted soft tissue mobilization, muscle endurance, rehabilitation
Introduction
Chronic neck pain, a musculoskeletal disease, is a common complaint resulting in impaired motor output of the cervical muscles [1]. Impairment of the motor output of the cervical muscles results in decreased strength and endurance and changes in muscle morphology such as atrophy and fat infiltration, resulting in altered cervical muscle behavior [2–4]. Altered muscle behavior is characterized by increased activity in the superficial muscles, the sternocleidomastoid and anterior scalenes, as a response to compensate for decreased deep neck flexor (DNF) muscle activity [5,6]. It has been revealed that there is a decrease in the directional specificity, delayed onset of activation, fatigue of the deep neck flexor muscles during functional tasks, and an increase in the co-contraction of the neck muscles [2,7].
Deep cervical muscles, longus colli and longus capitis, are important in supporting the head’s weight, cervical segments, and cervical curve during functional activities [8]. The endurance capacity of these muscles is crucial for maintaining neck posture and cervical joint stability during activities of daily living that require prolonged low-level deep muscle activation [9,10]. The function of these muscles can be improved by regulating the tone of the superficial muscles and chronic neck pain can be reduced [5,6]. Improving these muscle functions can effectively improve disability and function [6,11].
With the increasing prevalence of pain and disability associated with musculoskeletal disorders, identifying the most effective interventions to maximize the efficiency of treatment sessions, patient outcomes, and reduce the societal burden is very important in today’s healthcare environment where a physiotherapist may have difficulty managing the patient’s deficiencies [12,13].
Among conservative therapeutic interventions for musculoskeletal injuries, soft tissue and mobilization techniques have been frequently used in rehabilitation practice in recent years [14–16]. Many studies suggest that treating musculoskeletal injuries with Instrument-Assisted Soft Tissue Mobilization (IASTM) can reduce pain and improve function [17,18]. It is thought that IASTM therapy stimulates the remodeling of connective tissue through the resorption of excessive fibrosis and induces the repair and regeneration of collagen secondary to fibroblast proliferation. This will cause releasing and breakdown of fascial restrictions, adhesions, and scar tissue [19]. IASTM can provide physiological changes such as increased blood flow, decreased tissue viscosity, myofascial relaxation, and interruption of pain receptors [13,14,20].
IASTM is recommended to improve a range of motions in healthy individuals, reduce pain in patients with musculoskeletal injuries, and improve inpatient-reported functions [12]. However, it is not yet recommended for increasing muscle performance due to limited and conflicting studies [21–23]. Most studies have investigated the acute effects of IASTM on muscle performance. MacDonald et al. [24] found no acute effect difference on muscle performance as measured by vertical jump height, peak power, and peak velocity parameters of the IASTM intervention for the quadriceps compared with the group without IASTM. Similarly, in Stroiney et al. [25] study, one-session IASTM intervention did not increase sprint performance. On the other hand, Sevier and Stegink-Jansen [23] found a greater improvement in grip strength after IASTM combined with exercise therapy with a total of 8 sessions for 4 weeks, compared to exercise therapy alone in patients with chronic lateral elbow tendinopathy. Due to the lack of evidence on the efficacy of IASTM and the heterogeneity of research, there is a literature gap in establishing evidence for clinical applications [19]. Clinical studies should be conducted to establish a consensus on optimal IASTM dosage and IASTM’s effect to improve performance outcomes [19,23,26].
This current randomized clinical trial study is designed to investigate the efficacy of IASTM combined with exercise therapy on pain and muscle endurance in patients with chronic neck pain. The current study hypothesized that IASTM interventions before stretching and strengthening exercises would lead to a greater decrease in pain intensity, increase deep neck flexor muscle endurance compared to exercise therapy alone.
Methods
Study design and participants
This study was a two-armed, single-blinded, single-centered, and randomized controlled trial. According to the Neck Pain Task Force, patients were diagnosed by a physiatrist with nonspecific chronic neck pain at grades 1 and 2 before enrollment in the study. Grade 1 neck pain means there are no signs of severe structural disease, and it does not considerably interfere with activities of daily living (ADL). There are no symptoms of major structural pathology in Grade 2 neck pain, but it significantly affects ADL [27]. Ethical approval was obtained on 9 March 2020 from the Istanbul Medipol University Non-Invasive Research Ethics Committee numbered 10,840,098–604.01.01-E11974. The study was registered in ClinicalTrials.gov (NCT04789265). All participants provided written informed consent before study entry.
This study was conducted between June 2020 and October 2020 at Istanbul Medipol University Sefaköy Hospital Physical Therapy and Rehabilitation Clinic. They were questioned through a form prepared by the investigators about demographic information such as age, height, weight, educational status, duration of pain, and factors that increase and decrease the pain.
Participants aged 18–70 years with chronic neck pain due to a nonspecific disorder for at least 3 months were included. Participants with a history of cancer (within the last five years), pregnancy, serious skin disorders, previous neck surgery, disc prolapse, spondylolisthesis, vertebral fractures, spinal stenosis, arthritis, osteoporosis, recent neck trauma (within the last 48 hours), postural deformity, chronic trapezitis, severe night pain, symptoms of infection, psychological disorder, and those who received therapy for neck pain in the last 6 months were not included [28].
Randomization, sample size calculation and blind design
Forty-eight eligible participants were randomly divided into two groups through simple randomization at a 1:1 ratio: Group 1- exercise therapy (ET) group (n = 24) and Group 2- combined therapy (CT) group (IASTM combined with exercise therapy) (n = 24) (Figure 1). They were referred to the physiotherapy and rehabilitation clinic and an appointment was made to start their therapy within 1 week. Randomization was conducted using a random number generator (https://www.randomizer.org/). The sample size was calculated using the G*Power 3.1.9.2 analysis program. VAS determined the sample size in line with the standard deviation data obtained from our pilot study for the differences in mean values and primary results between the groups (mean ± SD: combined therapy (n = 10); 2 ± 1.15, exercise therapy (n = 10); 4.5 ± 2.55). The sample size was estimated as 36 patients, 18 for each group, assuming the 95% power and 0.05 alpha level.
Figure 1.
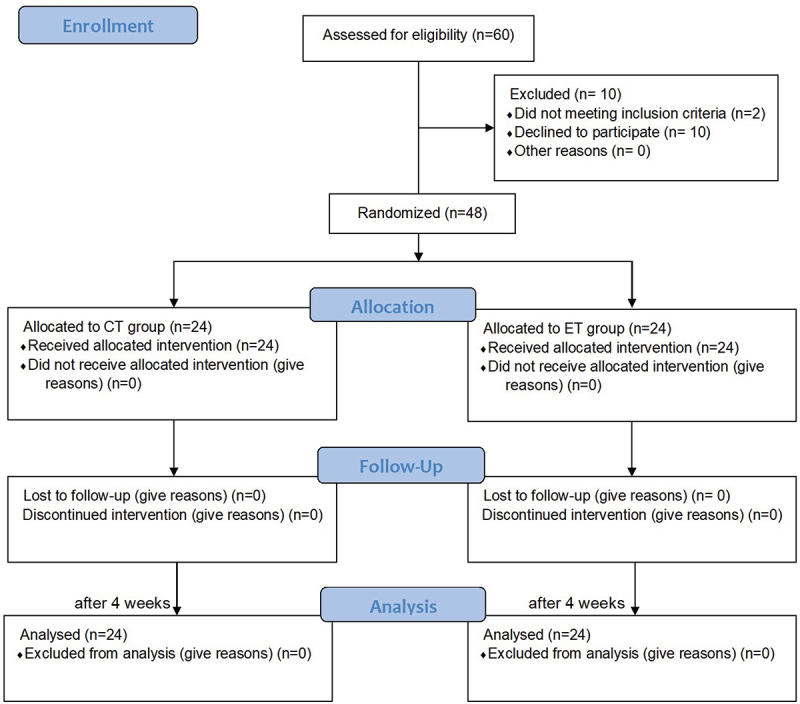
CONSORT flow diagram for current study.
Only the participants were blinded to group allocation. For exercise and combined therapy groups, participants were informed they would receive therapy to improve their pain/symptoms related to nonspecific chronic neck pain. It was impossible for the outcome assessor and the physiotherapist providing the treatment to be blinded due to a lack of investigators. The principal investigator collected all the data and performed all the steps.
Interventions
Participants in the CT and ET groups received exercise therapy for 35 minutes, 3 days a week, for 4 weeks under supervision. Participants in the CT group received a total of 8 sessions IASTM before performing the exercises for 6 minutes a day, 2 days a week, for 4 weeks. They received IASTM before 1. and 3. exercise sessions in a week. All participants received the same exercise therapy protocol. All interventions were performed under the same physiotherapist supervision that was 5-year-experienced and certified for IASTM intervention.
Exercise therapy
The exercise protocol, which consists of stretching and strengthening exercises for the muscles around the neck, shoulders and scapula, was structured by examining previous studies [29–31]. First, a chin-tuck stretching exercise was performed. Participants were instructed to pull their jaws back toward their neck and flex their neck slightly with the head straight and facing forward. Then, the levator scapulae and upper trapezius muscles were stretched. Participants were instructed to contralaterally rotate their head in the direction of the levator scapulae to be stretched and force their head in cervical flexion and lateral flexion using their hand to stretch the levator scapulae. To stretch the upper trapezius, participants tilted their head contralaterally in the direction of the upper trapezius, trying to touch their ears to the shoulder and force their head in lateral flexion using their hand. They repeated each exercise in both directions.
Secondly, the participants performed the following strengthening exercises in sequence. Participants pulled back their chin toward the neck and pressed their forehead lightly with their hands to activate their deep neck flexor muscles. Then, participants performed multi-directional isometric exercises (cervical flexion, extension, rotation, lateral flexion) for strengthening the neck muscles. Ultimately, participants performed the YWT exercises in a sequence to strengthen the rotator cuff muscles [1]; participants raised both arms to the sides at a 120° angle with elbows in extension to form a ‘Y shape’ [2], they created a ‘W shape’ with elbows in flexion at a 90° angle below the level of shoulders [3] they raised both arms to the side horizontally with elbows in extension to form a ‘T shape’. YWT exercises were performed in prone position with palms facing forward and thumbs up. During these movements, participants pulled their arms back and raised their chest, and the shoulder blades converged downwards each other. While they were joining the elbows in front of the chest, the chest bent down slightly, and the shoulder blades were separated from each other. At the end of each exercise, participants were instructed to hold the position for 3–5 seconds and repeat 10 times. The number of repetitions progressed according to participants’ tolerance not to cause an increase in neck pain during the day. All participants were given verbal training for proper posture and the principles required to maintain neck health in daily life.
Instrument-assisted soft tissue mobilization
IASTM is a form of soft tissue mobilization using specially designed stainless steel instruments with beveled edges [32]. This technique has been applied with a stainless steel Arco tool (https://www.omttraining.co.uk/product/arco-tools/). This tool has beveled edges that fit different anatomical positions in the body to treat patients effectively [19]. The clinician can detect trigger and painful points with the thin edge of the tool [33,34]. There is no standard amount of pressure to be applied with IASTM. Still, studies on mice show that increased pressure increases the number of fibroblasts in connective tissue, which can stimulate the healing process [35]. In this study, IASTM pressure was applied at a level that would not cause pain and excessive irritation or reaction (hyperemia, burning, bruising, etc.) according to the tolerance of all participants [36]. The application was performed while the participants were sitting in an upright and comfortable position in the chair, with their arms at their sides and their heads flexed laterally and forward. All participants received IASTM intervention for the identical body region. IASTM was applied to identical standard body regions which were determined as the extensor surface of the neck and bilateral (right/left) upper trapezius, levator scapula, splenius cervicis, splenius capitis muscle fibers in the upper back for each participant. The same Arco tool was used for all muscle groups (Figure 2). Before the treatment, a cream (Vaseline) was applied to the skin in the neck area. For one side, IASTM was applied for a total of 3 minutes, including 1 minute sweeping at a 45° angle, and 2 minutes fan technique with a 30° angle, in parallel directions to muscle fibers with the same method for all muscle groups [33,37]. The same process was repeated for the other side for 3 minutes, and the intervention ended at 6 minutes (Figure 3). After treatment, if any hyperemia or burning reaction occurred, they were asked to put an ice pack on the area. The tool was cleaned with alcohol. Stretching exercises were performed immediately after the IASTM intervention, and exercise therapy was continued with the remaining exercises.
Figure 2.

Arco tool.
Figure 3.

Instrument-assisted soft tissue mobilization sweeping technique for the levator scapulae.
Outcome measures
Deep Neck Flexor muscle Endurance (DNFE)
The DNFE test by Harris et al. [38] was used to assess the endurance of the participants’ deep neck flexors. The DNFE test was performed while the participants were supine with their knees hooked. In this position, the participants were instructed to retract their chin with an isometric contraction. They held this position with their chin pulled toward the chest and raised their head and neck approximately 2.5 cm from the bed. While the participants were in this position, a line was drawn across two approximated skin folds along the participants’ anterior-lateral neck. The assessor slid their left or right hand under the participants’ heads. Then, the participants were asked to relax their necks and place their heads on the assessor’s hand.
Then, participants were instructed to perform the test with verbal commands (‘retract your chin’ and ‘raise your head’) again. During the test, the assessor gently slid their left or right hand under the participants’ heads and provided a tactile cue with fingers to maintain a proper head position for the participant’s heads to gently contact the assessor’s fingers. Participants were asked to hold this position for as long as possible. The duration of holding this position was recorded with a stopwatch when the participants raised their heads. The test was terminated in 4 conditions [1]: when the edges of the drawn lines on the neck of participants no longer came close to each other due to the loss of the chin tuck [2], when the participant raised the head such that there was no longer maintained contact with the assessor’s fingers [3], when the head of the participants touched the hand of the assessor for more than 1 second [4], and when the participants did not want to continue the test. The test was repeated twice with a 5-minute break. During the break, the participants were instructed to rest supine and turn their necks from side to side in a painless range of motion at least 3 times without raising their head off the table. After averaging the 2 test time scores, the results were recorded [38,39].
The DNFE test’s intrarater reliability was good to excellent in patients without neck pain (intraclass correlation coefficient (ICC)[3,1] =.82–.91 and standard error of measurement (SEM) ranged from 8.0 to 11.0. Interrater reliability was moderate to good (ICC)[2,1] =.67–.78) and SEM ranged from 12.6 to 15.3). For subjects with neck pain, interrater reliability was moderate (ICC[2,1] =.67, SEM = 11.5). The DNFE test hold time results were 38.95 ± 26.4 seconds in subjects without neck pain whereas 24.1 ± 12.8 seconds in subjects with neck pain [38]. Additionally, a more recent study demonstrated 64% and 99% power to detect differences between subjects with and without neck pain during the DNF test of 6.91 seconds (SEM) and 19.15 seconds (MDC), respectively [40].
Pain intensity
The current neck pain intensity of the participants was assessed subjectively with the Visual Analogue Scale (VAS). This scale consists of a 10 cm linear line. The line’s starting point is 0, representing no pain; the last point, 10, represents the most severe pain encountered. In this study, participants were asked to rate the number corresponding to their pain. Their correspondence was recorded in cm [41]. In a systematic review of 66 empirical studies (31.254 patients) in the relief of chronic pain, the median absolute minimum clinically important difference (MCID) was 23 mm (interquartile range (IQR) = 12–39) for 50 studies using a mean change approach [42].
The same assessor for the groups measured the outcome measures listed above at baseline and post-treatment (4 weeks).
Statistical analysis
All statistical analyzes were performed using the IBM SPSS 22.0 software (Statistical Package for Social Science, Inc., Chicago, IL). Statistical significance was accepted as p < 0.05. Descriptive statistics (frequency, mean, and standard deviations) were calculated to identify the sample. Data were tested for normality using the Shapiro – Wilk test. The between-group differences for the demographic data were analyzed with the independent samples t-test for continuous variables and Chi-square tests for categorical variables. Baseline and post-treatment within-group differences were analyzed with the Wilcoxon signed-rank test for VAS data and paired samples t-test for DNFE test data. The Mann-Whitney U test for VAS data and independent samples t-test for DNFE test data were used to determine the between-group differences. Cohen coefficients (d) were calculated for within-group effect sizes based on the estimated means. Cohen coefficients were interpreted as large (>0.80), medium (0.50–0.79), and small (0.20–0.49) [43].
Results
Sixty participants with chronic neck pain were screened for eligibility, 48 met all the inclusion criteria, were randomized into the CT group (n = 24) and the ET group (n = 24) participated in the study (Figure 1). The mean age of all participants was 44.34 ± 13.38 years, and 66.7% of them were women. It was reported that 66.7% of the participants experienced pain for over a year, more often while lifting heavy things, doing housework, or working. Baseline characteristics of the groups are presented in Table 1. No significant differences were found in age, gender, body mass index, education level, neck pain duration, factors increasing and decreasing pain, smoking history and baseline outcome measures between the CT and ET groups.
Table 1.
Baseline characteristics of the participants.
| Combined therapy group (n = 24) | Exercise therapy group (n = 24) | p value | |
|---|---|---|---|
| Age (years), mean ± SD | 42.96 ± 12.18 | 45.79 ± 14.61 | 0.469 |
| Body mass index (kg\cm2), mean ± SD | 26.58 ± 4.39 | 27.06 ± 3.98 | 0.692 |
| Gender, n (%) | 0.759 | ||
| Female | 17 (70.8) | 15 (62.5) | |
| Male | 7 (29.2) | 9 (37.5) | |
| Education level, n (%) | 0.348 | ||
| 12 years or less | 23 (95.8) | 20 (83.3) | |
| More than 12 years | 1 (4.2) | 4 (16.7) | |
| Neck pain duration, n (%) | 0.133 | ||
| 3–6 months | 2 (8.3) | 6 [25] | |
| 6–12 months | 6 [25] | 2 (8.3) | |
| More than 12 months | 16 (66.7) | 16 (66.7) | |
| Factors increasing the pain, n (%) | 0.764 | ||
| Heavy object lifting | 8 (33.3) | 8 (33.3) | |
| Doing housework/working | 8 (33.3) | 8 (33.3) | |
| Changing position | 2 (8.3) | 2 (8.3) | |
| Stress | 3 (12.5) | 1 (4.2) | |
| Sitting for long time | 3 (12.5) | 5 (20.8) | |
| Factors decreasing the pain, n (%) | 1.000 | ||
| Having a rest | 17 (70.8) | 17 (70.8) | |
| Using drug | 4 (16.7) | 4 (16.7) | |
| Getting exercise and massage | 3 (12.5) | 3 (12.5) | |
| Smoking history, n (%) | 0.516 | ||
| Yes | 5 (20.8) | 8 (33.3) | |
| No | 19 (79.2) | 16 (66.7) | |
| Visual Analog Scale (score), mean ± SD | 9.04 ± 1.04 | 8.67 ± 1.76 | 0.965 |
| Deep Neck Flexor Endurance Test (sec), mean ± SD | 9.02 ± 4.22 | 7.43 ± 7.22 | 0.357 |
Note: SD: Standard deviation.
There was no statistically significant difference in pain intensity at baseline between groups (p = 0.965, Table 1), and post-treatment pain scores were lower than the ET group for participants in the CT group (p = 0.019, Table 2). The post-treatment findings identified that pain levels improved in both groups (p < 0.001). The effect size of the decrease in pain scores for the CT group was larger than the ET group (Cohen’s d: CT group = 3.28, ET group = 2.12). No statistically significant difference was found for DNFE scores between CT and ET groups at baseline (p = 0.357, Table 1) and post-treatment (p = 0.143, Table 2). There was a significant improvement in the DNFE scores of the participants in the CT group after treatment (p = 0.028) with a change of 1.90 ± 3.96 seconds. No significant difference change occurred in DNFE scores post-treatment with a change of 0.95 ± 3.55 seconds for the ET group (p = 0.201).
Table 2.
Comparison of pain intensity and deep neck flexor muscles endurance between and within groups.
| Baseline | Post-treatment | Δ | p value | Effect size (Cohen’s d) | Between-group p value | ||
|---|---|---|---|---|---|---|---|
| VAS (cm) | Combined therapy group | 9.04 ± 1.04 | 2.63 ± 1.71 | −6.41 ± 1.95 | <0.001 | 3.28 | 0.019 |
| Exercise therapy group | 8.67 ± 1.76 | 4.29 ± 2.47 | −4.37 ± 2.06 | <0.001 | 2.12 | ||
| DNFET (sec) | Combined therapy group | 9.02 ± 4.22 | 10.92 ± 5.59 | 1.90 ± 3.96 | 0.028 | 0.40 | 0.143 |
| Exercise therapy group | 7.43 ± 7.22 | 8.39 ± 6.18 | 0.95 ± 3.55 | 0.201 | 0.20 |
Note: Values are mean ± standard deviation; Δ: within-group treatment difference; VAS: Visual Analog Scale; DNFET: Deep Neck Flexor Muscle Endurance Test; Statically significant p-value and subsequent effect size are indicated in bold.
Discussion
This study aimed to determine the effect of IASTM combined with exercise therapy on pain intensity and deep neck flexor muscle endurance in patients with chronic neck pain. According to the results of our study, there were significant improvements in the pain intensity of the participants who received both exercise therapy alone and IASTM combined with exercise therapy. Although our results indicated statistically significant but low-level improvements on DNFE of CT group, they did not provide sufficient evidence to have a clinically substantial impact.
MacDonald et al. [24] and Stroiney et al. [25] found no immediate improvement in vertical jump performance after applying IASTM to the quadriceps, hamstrings, and triceps surae muscles, respectively, for the 3 intervention groups. They stated that the IASTM was applied to the muscles that were being assessed and while the participants were in the prone or supine positions, which may have caused the physiological and psychological relaxation responses. They also did not find any performance loss after using IASTM [24,25], and our results support this finding. In the current study, IASTM was applied to the muscle groups on the extensor surface (upper trapezius, levator scapulae, multifidi, and splenius cervicis) in the sitting position, and the endurance of deep neck flexor muscles was assessed. A statistically but not clinically significant increase was observed in the deep neck flexor endurance hold time of the participants in the combined therapy group. The wide SEM and MDC might limit the sensitivity of DNFE test [38,40]. Therefore, low-level and clinically unsubstantial time increases may be due to measurement error in the current study. However, the low-level increases may be related to myofascial relaxation of the superficial muscles in the upper back and neck region due to the resolution of fascial restrictions with IASTM. Participants in our study received a total of 8 sessions of IASTM intervention over 4 weeks. The difference between our study and previous similar studies that did not find acute effects of short-term IASTM interventions on performance [24,25] seems to be the duration of the treatment. It is thought that applications exceeding 4 weeks may provide clinical benefits and should be investigated.
Some studies show improvement in muscle performance with IASTM [12,23]. In Sevier and Stegink-Jansen [23] study, the participants’ muscle strength who received IASTM combined with exercise therapy increased more than the exercise therapy alone. They applied the IASTM to a wide area, on the palmar and dorsal surfaces of the affected arm from the wrist retinaculum to the deltoid, including antagonists of the tested muscle similar to the current study. Kivlan et al. [12] found increased isometric squat test maximum force output as the acute effect of IASTM interventions in individuals with a lower extremity injury. The investigators applied the IASTM to the muscles of the anterior and lateral parts of the affected leg, gastrocnemius/soleus muscle complex, quadriceps and hamstring muscle groups, and gluteus maximus and medius muscles in their study [12]. The fact that they found an acute improvement in performance in their results may be related to intervention to a wide region, not a single muscle.
Pain is temporarily reduced or eliminated with soft tissue manipulation when an analgesic effect is provided by applying force to the soft tissue [37]. Reduction in pain can lead to muscle relaxation and reducing muscle guarding can provide significant benefits in movement restoration [24,35]. In this study, because of the pressure applied with IASTM, the inhibition in the superficial muscles with the reduction of pain may have improved the activation of the deep neck flexor muscles.
El Hafez et al. [44] concluded that IASTM applied using an M2T blade for 4 weeks is a useful tool in reducing pain in subjects with upper trapezius spasms and our results are compatible with their study. Elserty and Shokri Morsi Galal [45] also observed in their studies a significant improvement in pain in all individuals after applying active soft tissue techniques in chronic neck pain cases with upper trapezius muscle latent trigger points. In the current study, a greater pain intensity improvement may have occurred for the combined therapy group compared to the exercise group at post-treatment because IASTM triggered tissue microtrauma, causing a regional inflammatory process and increasing fibroblast release. Fibroblast migration increases collagen synthesis and tissue regeneration, accelerating the recovery process [46]. In addition, increased tissue temperature and blood flow due to friction between tool and tissue can improve tissue oxygenation and remove local waste metabolites [33,47]. Instrument use can provide deeper penetration, and increased vibration perception facilitates the clinician’s ability to detect changing tissue characteristics while facilitating the patient’s awareness of differentiated senses in treated tissues [33,34]. It improves the extensibility by decreasing the tissue restrictions and viscosity with the heat generated, and tissue becomes softer [14]. Bulbuli [48] found a decrease in heel pain and an increase in the activity level after IASTM intervention using an M2T blade. The investigators reported that by making rhythmic strokes until the fascia loosens, adhesions and cross-connections on the fascia could be dissolved and used to soften the taut fascia [48]. Naik [49] observed a significant reduction in pain after M2T administration in subjects with shoulder pain.
Our results seem to be consistent with the systematic review of Cheatham et al. [19] who reached ‘nonsignificant results’ that challenge the effectiveness of IASTM as a treatment for common musculoskeletal pathology. To date, four systematic reviews have investigated the efficacy of IASTM as an intervention in patients with musculoskeletal pathology or disorders [13,19,26,50]. While Lambert et al. [13] and Seffrin et al. [26] reported that IASTM was an effective treatment in reducing pain and improving function, two other reviews reported that the existing evidence did not support the efficacy of IASTM based on similar musculoskeletal studies [19,50]. The literature investigating the effects of IASTM is still insufficient [19].
Exercise therapy is highly promising among the different conservative approaches used in treating individuals with neck pain [51]. Previous research supports that exercise therapy can alter the impaired recruitment pattern in neck muscles and that repetition of a particular task can lead to adaptive changes in weak muscles [52]. Exercise effectively improves pain and function in patients with both acute and chronic neck pain [53]. A review reported that although the role of exercise is important in neck pain rehabilitation, studies have generally investigated the effect of one-dimensional exercises. The same review suggested that a rehabilitation protocol should include more than one training mode focusing on strengthening, flexibility, or motor control training specific to all impaired physiological functions [3]. The reduction in pain of all groups in the current study may be related to the content of multimodal exercise protocol, which includes both flexibility and strengthening exercises. Our findings showed that although the participants in the CT group’s DNFE test hold time scores statistically increased, the fact that the change values were at a low level did not seem to be clinically meaningful. These current findings suggest that measurement error may have an impact on the improvements and IASTM is not directly responsible.
Limitations
The current study has some limitations. First, the small sample size may have affected the results. A randomized controlled trial with larger sample size is needed to determine the effects of IASTM combined with exercise therapy on outcomes in patients with chronic neck pain. Moreover, improvements in the daily life activities of the participants were not assessed in our study, the use of standardized and patient-reported outcome measures in future studies may reveal the results more effectively. Additionally, wide SEM and MDC of the DNFE test may increase measurement errors, research on the use of instruments that can measure structural muscle changes can reveal the improvements more clearly. Another limitation of this study is the possibility that detection bias may affect the results due to the fact that the outcome assessor was not blinded. Lastly, the outcome measures were not followed-up. Assessment of long-term therapy outcomes can determine the effectiveness and persistence of the treatment more accurately.
Conclusions
In summary, our findings demonstrated statistically significant but low-level improvements in DNFE in the CT group, but they did not offer sufficient evidence for clinically beneficial outcomes. The subjects’ levels of pain significantly decreased after receiving both exercise therapy alone and exercise therapy combined with IASTM. More research is needed to determine whether exercise therapy with IASTM is clinically beneficial in patients with chronic neck pain.
Acknowledgements
We would like to thank Dr. Kıvanç Katmerlikaya, Dr. Şen Bezirgan, and Sefaköy Hospital Physiotherapy and Rehabilitation Clinic for their clinical assistance. Particular thanks to Prof. Dr. Özlem Ülger who proof-read the final version of this manuscript.
Biographies
Pınar Kaya graduated with a bachelor's degree in 2009 Hacettepe University School of Physical Therapy and Rehabilitation in Turkey. She graduated from her master's university with her master's in 2013 and her PhD in the six years of rehabilitation in 2018. After various clinics in a physiotherapy her career as lecturer at Istanbul Medipol University's Faculty of Health Sciences, Department of Physiotherapy and Rehabilitation after gaining master degree. She started to work as an assistant professor at Istanbul Medipol University after gaining her PhD, and she is now working as an associate professor at the same university. She also continues in research on projects and conduct research domains in the chronic pain and rehabilitation rehabilitation, and she also in undergraduate and master students in these subjects. She keeps working on technology solutions for rehabilitation in collaboration with engineers from several universities. Moreover, she continues to work to raise the standard of physiotherapy education in Turkey.
Ayşegül BOSTAN graduated with a bachelor's degree in 2011 Istanbul Medipol University School of Physical Therapy and Rehabilitation in Turkey. She graduated from the same university with her master's in 2021. She continues her PhD's program in physical therapy and rehabilitation at Hacettepe University. After spending three years treating patients with various diseases in a physiotherapy clinic, she started her career as a research assistant in 2020. She is now a research assistant at Bahçeşehir University, Faculty of Health Sciences, Department of Physiotherapy and Rehabilitation. She continues to work on projects and research in the fields of chronic pain, low back and neck health, orthopedic rehabilitation and neuroscience. In her doctoral thesis, she is developing a project investigating brain activities with EEG in individuals with chronic neck pain.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].Blanpied PR, Gross AR, Elliott JM, et al. Clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American physical therapy association. J Orthop Sports Phys Ther. 2017;47(7):1–183. [DOI] [PubMed] [Google Scholar]
- [2].Blomgren J, Strandell E, Jull G, et al. Effects of deep cervical flexor training on impaired physiological functions associated with chronic neck pain: a systematic review. BMC Musculoskelet Disord. 2018;19(1):415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].De Pauw R, Coppieters I, Kregel J, et al. Does muscle morphology change in chronic neck pain patients? - a systematic review. Manual Ther. 2016;22:42–49. [DOI] [PubMed] [Google Scholar]
- [4].Elliott JM, Courtney M, Rademaker A, et al. The rapid and progressive degeneration of the cervical multifidus in whiplash: an MRI study of fatty infiltration. Spine. 2015;40(12):694–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Jull G, Falla D.. Does increased superficial neck flexor activity in the craniocervical flexion test reflect reduced deep flexor activity in people with neck pain? Manual Ther. 2016;25:43–47. [DOI] [PubMed] [Google Scholar]
- [6].Falla D, Jull G, Edwards S, et al. Neuromuscular efficiency of the sternocleidomastoid and anterior scalene muscles in patients with chronic neck pain. Disabilit Rehabilitat. 2004;26(12):712–717. [DOI] [PubMed] [Google Scholar]
- [7].Javanshir K, Rezasoltani A, Mohseni-Bandpei MA, et al. Ultrasound assessment of bilateral longus colli muscles in subjects with chronic bilateral neck pain. Am J Phys Med Rehabil. 2011;90(4):293–301. [DOI] [PubMed] [Google Scholar]
- [8].Panjabi MM, Cholewicki J, Nibu K, et al. Critical load of the human cervical spine: an in vitro experimental study. Clin Biomech. 1998;13(1):11–17. [DOI] [PubMed] [Google Scholar]
- [9].Boyd-Clark LC, Briggs CA, Galea MP. Muscle spindle distribution, morphology, and density in longus colli and multifidus muscles of the cervical spine. Spine. 2002;27(7):694–701. [DOI] [PubMed] [Google Scholar]
- [10].Ghamkhar L, Kahlaee AH. Are ultrasonographic measures of cervical flexor muscles correlated with flexion endurance in chronic neck pain and asymptomatic participants? Am J Phys Med Rehabil. 2017;96(12):874–880. [DOI] [PubMed] [Google Scholar]
- [11].Ylinen J, Takala EP, Nykänen M, et al. Active neck muscle training in the treatment of chronic neck pain in women: a randomized controlled trial. JAMA. 2003;289(19):2509–2516. [DOI] [PubMed] [Google Scholar]
- [12].Kivlan BR, Carcia CR, Clemente FR, et al. The effect of Astym® Therapy on muscle strength: a blinded, randomized, clinically controlled trial Rehabilitation, physical therapy and occupational health. BMC Musculoskelet Disord. 2015;16(1):325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Lambert M, Hitchcock R, Lavallee K, et al. The effects of instrument-assisted soft tissue mobilization compared to other interventions on pain and function: a systematic review. Phys Ther Rev. 2017;22(1–2):76–85. [Google Scholar]
- [14].Markovic G. Acute effects of instrument assisted soft tissue mobilization vs. foam rolling on knee and hip range of motion in soccer players. J Bodyw Mov Ther. 2015;19(4):690–696. [DOI] [PubMed] [Google Scholar]
- [15].Noten S, Meeus M, Stassijns G, et al. Efficacy of different types of mobilization techniques in patients with primary adhesive capsulitis of the shoulder: a systematic review. Arch Phys Med Rehabil. 2016;97(5):815–825. [DOI] [PubMed] [Google Scholar]
- [16].Rodríguez-Fuentes I, De Toro FJ, Rodríguez-Fuentes G, et al. Myofascial release therapy in the treatment of occupational mechanical neck pain: a randomized parallel group study. Am J Phys Med Rehabil. 2016;95(7):507–515. [DOI] [PubMed] [Google Scholar]
- [17].Laudner K, Compton BD, McLoda TA, et al. Walters, Acute effects of instrument assisted soft tissue mobilization for improving posterior shoulder range of motion in collegiate baseball players. Int J Sports Phys Ther. 2014;9(1):1–7. [PMC free article] [PubMed] [Google Scholar]
- [18].Kim J, Sung DJ, Lee J. Therapeutic effectiveness of instrument-assisted soft tissue mobilization for soft tissue injury: mechanisms and practical application. J Exerc Rehabil. 2017;13(1):12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Cheatham SW, Lee M, Cain M, et al. The efficacy of instrument assisted soft tissue mobilization: a systematic review. J Can Chiropr Assoc. 2016;60(3):200–211. [PMC free article] [PubMed] [Google Scholar]
- [20].Lauche R, Wübbeling K, Lüdtke R, et al. Randomized controlled pilot study: pain intensity and pressure pain thresholds in patients with neck and low back pain before and after traditional east asian ‘gua Sha’ therapy. American J Chinese Med. 2012;40(05):905–917. [DOI] [PubMed] [Google Scholar]
- [21].Blanchette MA, Normand MC. Augmented soft tissue mobilization vs natural history in the treatment of lateral epicondylitis: a pilot study. J Manipulative Physiol Ther. 2011;34(2):123–130. [DOI] [PubMed] [Google Scholar]
- [22].Burke J, Buchberger DJ, Carey-Loghmani MT, et al. A pilot study comparing two manual therapy interventions for carpal tunnel syndrome. J Manipulative Physiol Ther. 2007;30(1):50–61. [DOI] [PubMed] [Google Scholar]
- [23].Sevier TL, Stegink-Jansen CW. Astym treatment vs. eccentric exercise for lateral elbow tendinopathy: a randomized controlled clinical trial. Peer J. 2015;3:967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].MacDonald N, Baker R, Cheatham SW. The effects of instrument assisted soft tissue mobilization on lower extremity muscle performance: a randomized controlled trial. Int J Sports Phys Ther. 2016;11(7):1040–1047. [PMC free article] [PubMed] [Google Scholar]
- [25].Stroiney DA, Mokris RL, Hanna GR, et al. Examination of self-myofascial release vs. instrument-assisted soft-tissue mobilization techniques on vertical and horizontal power in recreational athletes. J Strength Cond Res. 2020;34(1):79–88. [DOI] [PubMed] [Google Scholar]
- [26].Seffrin CB, Cattano NM, Reed MA, et al. Instrument-assisted soft tissue mobilization: a systematic review and effect-size analysis. J Athl Train. 2019;54:808–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Haldeman S, Carroll L, Cassidy JD, et al. The bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Eur Spine J. 2008;17(S1):5–7. [Google Scholar]
- [28].Bernal-Utrera C, Gonzalez-Gerez JJ, Anarte-Lazo E, et al. Manual therapy versus therapeutic exercise in non-specific chronic neck pain: a randomized controlled trial. Trials. 2020;21(1). doi: 10.1186/s13063-020-04610-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Pico-Espinosa OJ, Aboagye E, Côté P, et al. Deep tissue massage, strengthening and stretching exercises, and a combination of both compared with advice to stay active for subacute or persistent non-specific neck pain: a cost-effectiveness analysis of the Stockholm Neck trial (STONE). Musculoskeletal Sci Pract. 2020;46:102109. [DOI] [PubMed] [Google Scholar]
- [30].Park SH, Lee MM.. Effects of lower trapezius strengthening exercises on pain, dysfunction, posture alignment, muscle thickness and contraction rate in patients with neck pain; randomized controlled trial. Med Sci Monit. 2020;26: 920208–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Dusunceli Y, Ozturk C, Atamaz F, et al. Efficacy of neck stabilization exercises for neck pain: a randomized controlled study. J Rehabil Med. 2009;41(8):626–631. [DOI] [PubMed] [Google Scholar]
- [32].Crane P, Ladden J, Monica D. Treatment of axillary web syndrome using instrument assisted soft tissue mobilization and thoracic manipulation for associated thoracic rotation dysfunction. Physiother Theory Pract. 2017;34(1):74–78. [DOI] [PubMed] [Google Scholar]
- [33].Baker RT, Nasypany A, Seegmiller JG. Instrument-assisted soft tissue mobilization treatment for tissue extensibility dysfunction. Int J Athl Train. 2013;18(5):16–21. [Google Scholar]
- [34].Lee JH, Lee DK, Oh JS. The effect of Graston technique on the pain and range of motion in patients with chronic low back pain. J Phys Ther Sci. 2016;28(6):1852–1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Loghmani MT, Whitted M. Soft tissue manipulation: a powerful form of mechanotherapy. J Physiother Rehabil. 2016;1(04):1–6. [Google Scholar]
- [36].McMurray J, Landis S, Lininger K, et al. A comparison and review of indirect myofascial release therapy, instrument-assisted soft tissue mobilization, and active release techniques to inform clinical decision making. Int J Athl Train. 2015;20(5):29–34. [Google Scholar]
- [37].Gulick DT. Influence of instrument assisted soft tissue treatment techniques on myofascial trigger points. J Bodyw Mov Ther. 2014;18(4):602–607. [DOI] [PubMed] [Google Scholar]
- [38].Harris KD, Heer DM, Roy TC, et al. Reliability of a measurement of neck flexor muscle endurance. Phys Ther. 2005;85(12):1349–1355. [PubMed] [Google Scholar]
- [39].Domenech MA, Sizer PS, Dedrick GS, et al. The deep neck flexor endurance test: normative data scores in healthy adults. PMR. 2011;3(2):105–110. [DOI] [PubMed] [Google Scholar]
- [40].Lourenço AS, Lameiras C, Silva AG. Neck flexor and extensor muscle endurance in subclinical neck pain: intrarater reliability, standard error of measurement, minimal detectable change, and comparison with asymptomatic participants in a university student population. J Manip Physiol Ther. 2016;39(6):427–433. [DOI] [PubMed] [Google Scholar]
- [41].Simon CB, Stryker SE, George SZ. Assessing the influence of treating therapist and patient prognostic factors on recovery from axial pain. J Man Manip Therapy. 2013;21(4):187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Olsen MF, Bjerre E, Hansen MD, et al. Minimum clinically important differences in chronic pain vary considerably by baseline pain and methodological factors: systematic review of empirical studies. J Clin Epidemiol. 2018;101:87–106. [DOI] [PubMed] [Google Scholar]
- [43].Cohen J. A power primer. Psychol Bull. 1992;112(1):155–159. [DOI] [PubMed] [Google Scholar]
- [44].El-Hafez HM, Hamdy HA, Takla MK, et al. Instrument-assisted soft tissue mobilisation versus stripping massage for upper trapezius myofascial trigger points. J Taibah Univ Med Sci. 2020;15:87–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Elserty N, Morsi Galal DO S. Withdrawn: influence of instrument assisted soft tissue techniques versus active soft tissue therapies on latent trigger point of upper trapezius muscle: randomized clinical study. Physiotherapy Res Int. 2020. 10.1002/pri.1859 [DOI] [PubMed] [Google Scholar]
- [46].Imai K, Ikoma K, Chen Q, et al. Biomechanical and histological effects of augmented soft tissue mobilization therapy on achilles tendinopathy in a rabbit model. J Manip Physiol Ther. 2015;38(2):112–118. [DOI] [PubMed] [Google Scholar]
- [47].Portillo-Soto A, Eberman LE, Demchak TJ, et al. Comparison of blood flow changes with soft tissue mobilization and massage therapy. J Altern Complementary Med. 2014;20(12):932–935. [DOI] [PubMed] [Google Scholar]
- [48].Bulbuli DA. Effect of IASTM using M2T blade on acute heel pain: a pilot study. J Med Sci Clin Res. 2017;5(04):20631–20636. [Google Scholar]
- [49].Naik NV. Immediate effects of M2T blade on pain and range of motion inrecreational badminton shoulder pain subjects: a pilot study. J Med Sci Clin Res. 2016;4:12965–12968. [Google Scholar]
- [50].Nazari G, Bobos P, MacDermid JC, et al. The effectiveness of instrument-assisted soft tissue mobilization in athletes, participants without extremity or spinal conditions, and individuals with upper extremity, lower extremity, and spinal conditions: a systematic review. Arch Phys Med Rehabil. 2019;100(9):1726–1751. [DOI] [PubMed] [Google Scholar]
- [51].Amiri Arimi S, Mohseni Bandpei MA, Javanshir K, et al. The effect of different exercise programs on size and function of deep cervical flexor muscles in patients with chronic nonspecific neck pain. Am J Phys Med Rehabil. 2017;96(8):582–588. [DOI] [PubMed] [Google Scholar]
- [52].O’Leary S, Jull G, Kim M, et al. Training mode–Dependent changes in motor performance in neck pain. Arch Phys Med Rehabil. 2012;93(7):1225–1233. [DOI] [PubMed] [Google Scholar]
- [53].Gross A, Kay TM, Paquin JP, et al. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2015;2015(1). [DOI] [PMC free article] [PubMed] [Google Scholar]


