Idiopathic macular telangiectasia type 1 (MacTel type 1) was first noticed in 1982 by Gass and Oyakawa and described as a disease characterized by capillary ectasia and dilatation in the juxtafoveal region.[1] It is a retinal vascular disease mainly affecting men unilaterally and consists of vascular leakage, cystoid macular edema, and yellowish exudation resulting in vision impairment.[2]
Among therapeutic modalities for MacTel type 1, laser photocoagulation has been considered the standard treatment. On the other hand, anti-vascular endothelial growth factor (anti-VEGF) agents have been shown to be effective, providing visual acuity improvement and central retinal thickness decrease.[3,4]
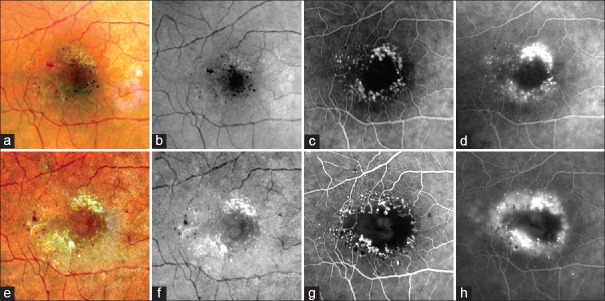
A 67-year-old male with no past medical history presented vision loss in his right eye (OD) for several months, progressively. At the initial examination, his best-corrected visual acuity (BCVA) was 20/40 in the OD and 20/20 in the left eye. Anterior segment examination was unremarkable, and dilated ophthalmoscopy followed by fundus photography revealed parafoveal aneurysms in OD [Figure 1a and b]. Fluorescein angiography demonstrated early hyperfluorescence in areas corresponding to the dilated capillaries and an increased foveal avascular zone [Figure 1c and d]. Once there were no signs of disease activity such as subretinal fluid or exudation, a conservative follow-up was decided along with the patient. He presented for clinical follow-up annually.
Figure 1.
Initial presentation (a-d) versus visual impairment 10 years after the first examination (e-h). a and e: Color fundus photography; b and f: Red-free fundus photography; c and g: Early-phase fluorescein angiography (FA); d and h: Late-phase FA
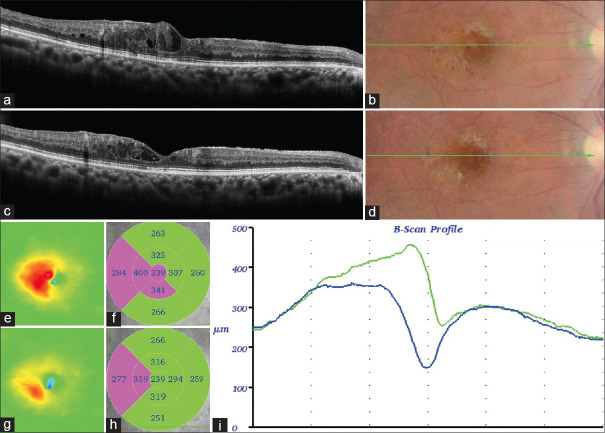
Ten years after the initial visit, he presented with visual impairment, and his BCVA decreased to 20/80 in the OD. Fundus examination revealed parafoveal exudation and worsening of angiographic findings [Figure 1e-h], and spectral-domain optical coherence tomography (SD-OCT) showed disorganization of the retinal layers and intraretinal fluid [Figure 2a, b and e, f, i].
Figure 2.
Spectral-domain optical coherence tomography showing findings at the moment before treatment (a, b and e, f) and after 3-monthly loading dose of anti-vascular endothelial growth factor treatment (c, d and g, h). a and c: B-scan profile (horizontal); b and d: Color fundus photography; e and g: Color thickness map; f and h: ETDRS subfields; i: B-scan thickness before (green line) and after (blue line) treatment
After obtaining written informed consent, the patient underwent treatment with intravitreal anti-VEGF, following a 3-monthly loading dose. Thirty days after the third intravitreal anti-VEGF, SD-OCT already revealed regression of the macular edema, and BCVA was improved to 20/60 [Figure 2c, d and g, h].
In the case herein presented, we described a patient with MacTel Type 1 who remained with visual acuity stability for 10 years with no treatment after diagnosis, which later presented intraretinal fluid and a decrease in vision. We decided on this case to treat with intravitreal anti-VEGF, and we demonstrated its beneficial anatomical and functional effects in our patient, who showed an excellent response to therapy, resulting in edema resolution and visual improvement.
MacTel Type 1 is a rare disease, and there is no consensus regarding treatment schemes. Chatziralli et al.[4] showed that laser photocoagulation remains the standard treatment, as it has been proven to resolve exudation and improve and stabilize visual acuity successfully. Although laser photocoagulation can be performed and considered the first treatment choice, intravitreal anti-VEGF therapy has also been assessed to reduce macular edema and improve vision.[5]
This case reveals macular edema resolution and both anatomical and functional improvements after intravitreal anti-VEGF in a patient with MacTel type 1 who remained asymptomatic for 10 years. The results obtained here are encouraging and are in agreement with the data provided by the literature. Good guidance from both physician and patient is critical for early treatment and consequently better outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Gass JD, Oyakawa RT. Idiopathic juxtafoveolar retinal telangiectasis. Arch Ophthalmol. 1982;100:769–80. doi: 10.1001/archopht.1982.01030030773010. [DOI] [PubMed] [Google Scholar]
- 2.Yannuzzi LA, Bardal AM, Freund KB, Chen KJ, Eandi CM, Blodi B. Idiopathic macular telangiectasia. Arch Ophthalmol. 2006;124:450–60. doi: 10.1001/archopht.124.4.450. [DOI] [PubMed] [Google Scholar]
- 3.Nowilaty SR, Al-Shamsi HN, Al-Khars W. Idiopathic juxtafoveolar retinal telangiectasis: A current review. Middle East Afr J Ophthalmol. 2010;17:224–41. doi: 10.4103/0974-9233.65501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chatziralli IP, Sharma PK, Sivaprasad S. Treatment modalities for idiopathic macular telangiectasia: An evidence-based systematic review of the literature. Semin Ophthalmol. 2017;32:384–94. doi: 10.3109/08820538.2015.1096399. [DOI] [PubMed] [Google Scholar]
- 5.Kowalczuk L, Matet A, Dirani A, Daruich A, Ambresin A, Mantel I, et al. Efficacy of intravitreal aflibercept in macular telangiectasia type 1 is linked to the ocular angiogenic profile. Retina. 2017;37:2226–37. doi: 10.1097/IAE.0000000000001424. [DOI] [PMC free article] [PubMed] [Google Scholar]