Abstract
Background
With the growing opioid epidemic across the US, in-hospital utilization of opioids has garnered increasing attention. Using a national cohort, this study sought to characterize trends, outcomes, and factors associated with in-hospital opioid overdose (OD) following major elective operations.
Methods
We identified all adult (≥18 years) hospitalizations entailing select elective procedures in the 2016–2020 National Inpatient Sample. Patients who experienced in-hospital opioid overdose were characterized as OD (others: Non-OD). The primary outcome of interest was in-hospital OD. Multivariable logistic and linear regression models were developed to evaluate the association between in-hospital OD and mortality, length of stay (LOS), hospitalization costs, and non-home discharge.
Results
Of an estimated 11,096,064 hospitalizations meeting study criteria, 5375 (0.05 %) experienced a perioperative OD. Compared to others, OD were older (66 [57–73] vs 64 [54–72] years, p < 0.001), more commonly female (66.3 vs 56.7 %, p < 0.001), and in the lowest income quartile (26.4 vs 23.2 %, p < 0.001). After adjustment, female sex (Adjusted Odds Ratio [AOR] 1.68, 95 % Confidence Interval [CI] 1.47–1.91, p < 0.001), White race (AOR 1.19, CI 1.01–1.42, p = 0.04), and history of substance use disorder (AOR 2.51, CI 1.87–3.37, p < 0.001) were associated with greater likelihood of OD. Finally, OD was associated with increased LOS (β +1.91 days, CI [1.60–2.21], p < 0.001), hospitalization costs (β +$7500, CI [5900–9100], p < 0.001), and greater odds of non-home discharge (AOR 2.00, CI 1.61–2.48, p < 0.001).
Conclusion
Perioperative OD remains a rare but costly complication after elective surgery. While pain control remains a priority postoperatively, protocols and recovery pathways must be re-examined to ensure patient safety.
Keywords: Opioid overdose, Trends, National Inpatient Sample
Introduction
The number of deaths attributable to accidental drug overdose (OD) has increased four-fold in the United States over the past decade, with nearly 3/4 of the 80,000 OD deaths in 2021 involving an opioid [1,2]. While accompanied by significant risks, opioids are commonly prescribed during the perioperative period. Indeed, an estimated 70 % of opioid-naive patients receive narcotics postoperatively following low-risk surgery [3]. However, there is great variation in opioid prescription practices following elective surgery based on patient and hospital factors [4,5].
The prescription of opioids following surgery is a complex decision, as surgeons must weigh acute pain management against the risks of immediate overdose and long-term dependence. This balance is especially difficult in patients with comorbid conditions which may alter opioid tolerance and increased the risk of OD while trying to achieve analgesic targets [[6], [7], [8]]. Although postoperative OD is uncommon, Cauley et al. reported a two-fold increase between 2002 and 2011, with risk exacerbated by patient factors such as substance use disorder [7]. Conversely, Gan et al. observed insufficient pain management with opioids to be associated with a multitude of postoperative complications including delayed recovery and worse quality of life [9]. In the setting of the evolving opioid epidemic, it is essential to optimize perioperative pain management strategies for standardized recovery pathways following elective operations. Thus, contemporary analyses of the burden, risks, and associated impact of perioperative OD on clinical outcomes and healthcare resource utilization are particularly relevant.
In the present study we used a national cohort of patients to characterize trends, outcomes, and factors associated with in-hospital opioid OD following major elective surgery. We hypothesized socioeconomic factors and personal history of substance use disorder to be associated with an increased risk of perioperative OD. Furthermore, we hypothesized OD to be linked to increased length of stay (LOS), hospitalization costs, and odds of non-home discharge.
Methods
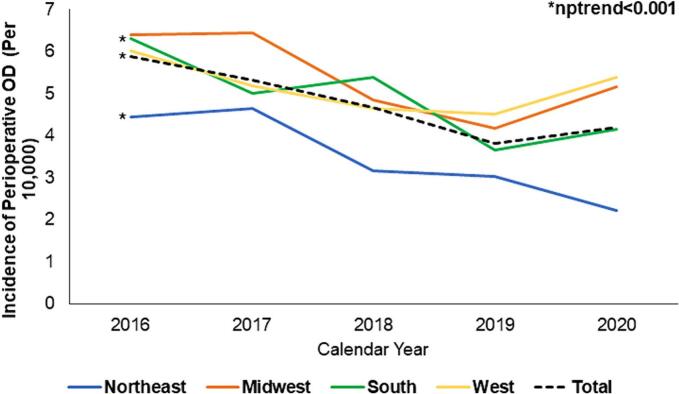
This retrospective study utilized data from the 2016 to 2020 National Inpatient Sample (NIS). Maintained as a part of the Healthcare Cost and Utilization Project (HCUP), NIS is the largest all-payer database providing accurate estimates for ∼97 % of all US hospitalizations [10]. All elective adult admissions (≥18 years of age) for spinal fusion, cardiothoracic (coronary artery bypass, valve operations, esophagectomy, wedge resection, lobectomy, pneumonectomy, thymectomy), general (hernia repair, gastrectomy, bariatric, pancreatectomy, hepatectomy, colorectal, and cholecystectomy), urologic/gynecologic (nephrectomy, cystectomy, prostatectomy, oophorectomy, hysterectomy), orthopedic (hip arthroplasty, knee arthroplasty, hip joint repair), and vascular operations (carotid endarterectomy, aortic repair, revascularization) were tabulated using relevant International Classification of Diseases, Tenth Revision (ICD-10) procedure codes (Supplemental Table 1). These operations were selected to be representative of procedures commonly performed across a wide range of surgical specialties [7,11]. Records were excluded from analysis if the operation was performed after the first day of hospitalization or entailed a primary diagnosis of opioid OD. This was done to minimize outlier effects of patients with a complicated clinical course whose need for opioids could be subject to nuanced decision making not captured within the database. Patients with missing data for age, sex, race, costs, and length of stay (LOS) were additionally excluded (3.8 %; Fig. 1).
Fig. 1.
Flow diagram of study cohort of patients undergoing elective surgery. OD; opioid overdose, LOS; length of stay.
As reported previously, perioperative OD was defined using ICD-10 diagnosis codes for overt opioid overdose or as a composite of a pulmonary complications (acute respiratory distress syndrome, respiratory failure, apnea, dyspnea, and periodic breathing) along with a major adverse event from an opioid (Supplemental Table 2) [7]. Patients who experienced a perioperative opioid overdose comprised the OD cohort, with the others classified as Non-OD.
The HCUP data dictionary was further used to define patient and hospital characteristics including age, sex, race, income quartile, primary payer, hospital region, hospital teaching status, and bed size [10]. Comorbid conditions, including substance use disorder, were defined using previously published ICD-10 diagnosis codes. The van Walraven modification of the Elixhauser Comorbidity Index was utilized to include the burden of comorbid disease into our analysis [12,13]. Hospitalization costs were computed using institution-specific cost-to-charge ratios, with subsequent inflation adjustment to the 2020 Personal Health Index [14].
The primary outcome of interest was perioperative OD. Secondary outcomes included in-hospital mortality, patient and hospital characteristics associated with OD, hospitalization costs, LOS, and non-home discharge. Non-home discharge was defined as disposition to a short-term hospital, skilled nursing facility, or home health care. Categorical data are reported as group proportions (%) and continuous data as means with standard deviation (SD) if normally distributed, or median with interquartile range (IQR) if otherwise. The adjusted Wald and Pearson's χ2 tests were used to determine the significance of intergroup differences for continuous and categorical variables, respectively. Cuzick's non-parametric rank-based test was utilized to evaluate the significance of temporal trends (nptrend) [15]. Prior to regression, the Least Absolute Shrinkage Selection Operator (LASSO) guided selection of covariates for regression analyses. This regularization method reduces collinearity among covariates while enhancing out-of-sample reliability of prediction models [16]. A multivariable logistic regression model was used to examine patient and hospital factors associated with perioperative OD. Similarly, multivariable linear and logistic regressions were further utilized to examine the association between OD and outcomes of interest. All models were optimized using Bayesian information criteria and receiver operating characteristics (C-statistic) [17]. Regression outputs are reported as adjusted odds ratio (AOR) or beta-coefficients (β) with 95 % confidence intervals (CI). An α <0.05 was set for significance.
Stata 16.1 was used for all analyses (StataCorp, College Station, TX). This study was deemed exempt from full review by the Institutional Review Board at the University of California, Los Angeles.
Results
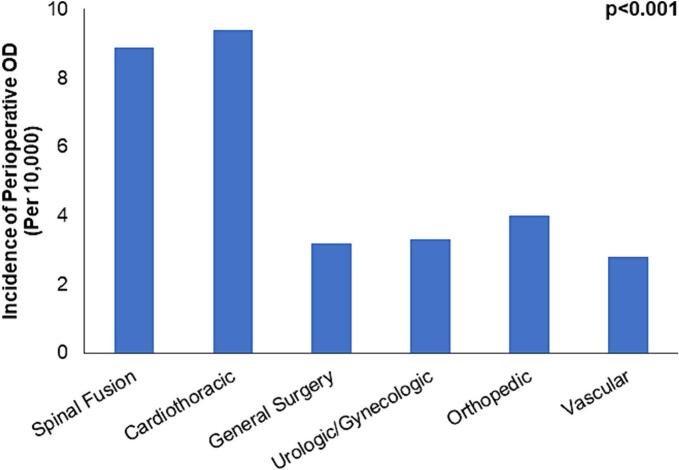
Of an estimated 11,096,064 hospitalizations for elective surgery meeting study criteria, 5375 (0.05 %) experienced a perioperative OD. The overall incidence of OD decreased from 6 to 4.1 per 10,000 cases between 2016 and 2020 (nptrend <0.001). As shown in Fig. 2, the Northeast and South were the only regions that demonstrated a significant decline in the incidence of OD (both nptrend <0.001). Compared to Non-OD, OD were older (66 [58–73] vs 64 [54–72] years, p < 0.001), more commonly female (66.4 vs 56.7 %, p < 0.001), and had a higher burden of comorbid disease (3 [2–4] vs 2 [1–3], p < 0.001). Additionally, OD were more commonly White (80.4 vs 77.8 %, p < 0.001) and in the lowest income quartile (26.4 vs 23.2 %, p = 0.001), but less frequently treated in the Northeast region of the United States (15.3 vs 20.4 %, p < 0.001). Finally, OD had a higher incidence of substance use disorder (4.9 vs 1.4 %, p < 0.001) and chronic lung disease (29.2 vs 17.3 %, p < 0.001; Table 1).
Fig. 2.
National trends in perioperative Opioid Overdose (OD) by United States Region, 2016–2020. Temporal trends overall, and in the Northeast and South were significant.
Table 1.
Demographic and hospital characteristics of patients who experienced a perioperative Opioid Overdose (OD) and those who did not (Non-OD) from 2016 to 2020; IQR, interquartile range.
| Non-OD (n = 11,090,689) |
OD (n = 5375) |
p-Value | |
|---|---|---|---|
| Patient characteristics | |||
| Age (years [IQR]) | 64 [54–72] | 66 [58–73] | <0.001 |
| Female (%) | 56.7 | 66.4 | <0.001 |
| Elixhauser Comorbidity Index [IQR] | 2 [1–3] | 3 [2–4] | <0.001 |
| Race (%) | <0.001 | ||
| White | 77.8 | 80.4 | |
| Black | 10.3 | 7.6 | |
| Hispanic | 7.3 | 7.1 | |
| Asian/Pacific Islander | 1.5 | 1.8 | |
| Other | 3.4 | 2.9 | |
| Income quartile (%) | 0.07 | ||
| >75 % | 24.5 | 22.2 | |
| 51–75 % | 26.2 | 26.9 | |
| 26–50 % | 26.1 | 24.5 | |
| 0–25 % | 23.2 | 26.4 | |
| Insurance coverage (%) | 0.02 | ||
| Private | 39.6 | 28.4 | |
| Medicare | 47.8 | 58.7 | |
| Medicaid | 7.8 | 8.8 | |
| Other payer | 3.6 | 3.2 | |
| Uninsured | 1.3 | 1.0 | |
| Comorbidities (%) | |||
| Cancer, non-metastatic | 12.1 | 13.5 | 0.19 |
| Cancer, metastatic | 2.6 | 4.2 | 0.001 |
| Cardiac arrhythmia | 13.1 | 26.0 | <0.001 |
| Chronic liver disease | 2.9 | 3.3 | 0.50 |
| Chronic lung disease | 17.3 | 29.2 | <0.001 |
| Coagulopathy | 3.7 | 10.8 | <0.001 |
| Congestive heart failure | 5.7 | 12.2 | <0.001 |
| Diabetes | 21.6 | 29.7 | <0.001 |
| End-stage renal disease | 0.9 | 2.0 | 0.001 |
| Hypertension | 60.4 | 71.0 | <0.001 |
| Neurologic disorder | 2.7 | 9.0 | <0.001 |
| Peripheral vascular disease | 7.4 | 8.9 | 0.07 |
| Pulmonary circulatory disease | 1.4 | 3.8 | <0.001 |
| Rheumatologic disorder | 3.7 | 5.2 | 0.005 |
| Psychiatric | 13.7 | 23.3 | <0.001 |
| Substance use disorder | 1.4 | 4.9 | <0.001 |
| Alcohol use disorder | 1.3 | 2.0 | 0.07 |
| Surgical specialty (%) | <0.001 | ||
| Spinal fusion | 15.0 | 27.2 | |
| Cardiothoracic | 7.3 | 14.3 | |
| General surgery | 19.3 | 12.7 | |
| Urologic/gynecologic | 11.5 | 8 | |
| Orthopedic | 40.7 | 33.7 | |
| Vascular | 6.3 | 3.6 | |
| Hospital characteristics | |||
| Teaching status (%) | 0.33 | ||
| Urban teaching | 72.7 | 69.5 | |
| Urban non-teaching | 21.2 | 24.1 | |
| Rural | 6.1 | 6.4 | |
| Hospital region (%) | 0.001 | ||
| Northeast | 20.4 | 15.3 | |
| Midwest | 23.4 | 26.3 | |
| South | 36.8 | 38.0 | |
| West | 19.4 | 20.4 | |
| Bed size (%) | 0.03 | ||
| Large | 49.3 | 54.3 | |
| Medium | 27.5 | 25.9 | |
| Small | 23.2 | 19.8 | |
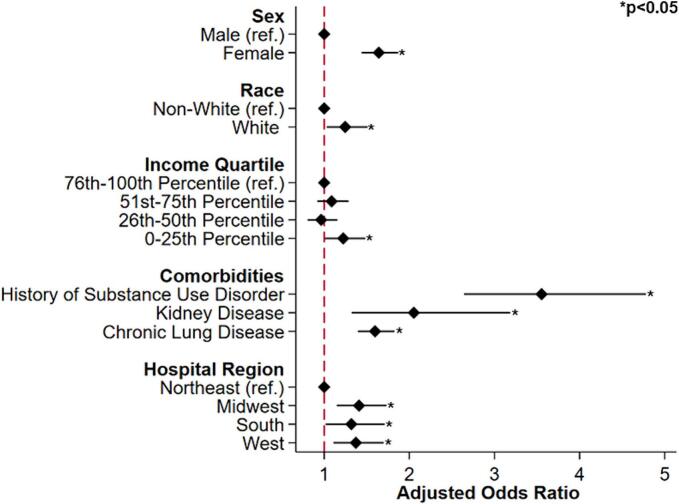
The most common operations were orthopedic (40.6 %), while vascular was the least common (6.3 %). Despite only comprising 15 % of the total cohort, spinal fusions accounted for nearly 28 % of all OD's. Similarly, cardiothoracic operations were responsible for 14 % of observed OD's, while only making up 7 % of the study population. Incident rates of OD by surgical specialty are shown in Fig. 3.
Fig. 3.
Incidence of Opioid Overdoses (OD) by surgical specialty.
On unadjusted analysis, the incidence of in-hospital mortality was similar between OD and others (0.25 vs 0.42 %, p = 0.22). Patients who experienced a perioperative OD stayed in the hospital longer (4 [3–7] vs 2 [1–3] days, p < 0.001), accrued higher costs ($26,100 [$17,500–$42,800] vs $16,500 [$12,000–$24,900], p < 0.001), and had higher rates of non-home discharge (30.4 vs 11.5 %, p < 0.001).
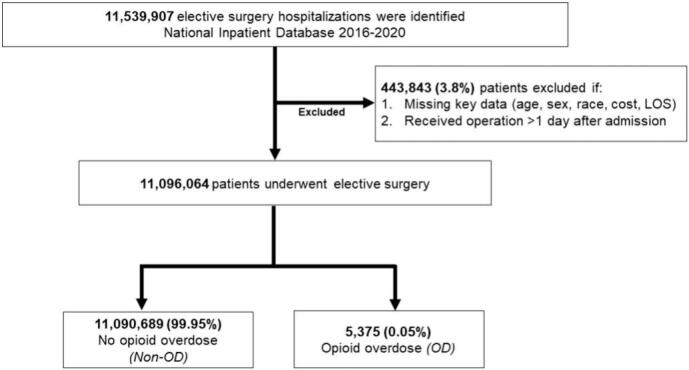
After risk adjustment, female sex (AOR 1.68, CI 1.47–1.92, p < 0.001), White race (AOR 1.19, CI 1.01–1.42, p = 0.04), and lowest income quartile (AOR 1.22, CI 1.02–1.45, p = 0.02) were associated with a greater likelihood of experiencing OD. History of substance use disorder (AOR 2.51, CI 1.87–3.37, p < 0.001), comorbid kidney disease (AOR 1.68, CI 1.07–2.65, p = 0.03), chronic lung disease (AOR 1.26, CI 1.09–1.46), and geographical region were also linked with OD (Fig. 4). Additionally, spinal fusion and cardiothoracic operations were associated with the greatest odds of experiencing a postoperative OD, compared to others. There was no significant difference in odds of mortality between those who experienced and OD and others (AOR 1.12, CI 0.42–2.99, p = 0.82). Finally, the OD cohort demonstrated incremental increases in LOS (β +1.84 days, CI 1.54–2.15, p < 0.001) and hospitalization expenditures (β + $7000, CI [$5400–$8500], p < 0.001), as well as greater odds of non-home discharge (AOR 2.56, CI 2.16–3.03; Table 2).
Fig. 4.
Association of patient and hospital factors with the development of opioid overdose (OD) following elective procedures. Ref; Reference Group.
Table 2.
Risk-adjusted outcomes for patients who experienced a perioperative Opioid Overdose (OD) relative to those who did not. Outcomes reported as adjusted odds ratio or beta coefficient (reference group: Non-OD). AOR, adjusted odds ratio; β, beta coefficient; CI, confidence interval; LOS, length of stay.
| Estimate | 95 % CI | p-Value | |
|---|---|---|---|
| Complications | |||
| In-hospital mortality (AOR) | 1.12 | [0.42–2.99] | 0.82 |
| Resource utilization | |||
| Hospitalization cost (β; USD $1000) | 7.0 | [+5.4 − +8.5] | <0.001 |
| LOS (β; days) | 1.84 | [1.54–2.15] | <0.001 |
| Non-home discharge (AOR) | 2.56 | [2.16–3.03] | <0.001 |
Discussion
Opioid overdose is a rare but potentially costly perioperative complication that can occur following elective surgery. In this nationwide retrospective study, we observed a decreasing trend in perioperative opioid overdose following elective surgery over a 4-year period. However, there was geographic variation in this trend with the Northeast experiencing the greatest decline in the rates of OD. Factors associated with perioperative OD included female sex, White race, lowest income quartile, hospital region, and operation. Additionally, comorbid chronic kidney and lung disease, as well as a history of substance use disorder were linked with higher odds of OD. Interestingly, OD was not associated with in-hospital mortality. Finally, OD was associated with longer LOS, increased hospitalization costs, and higher odds of non-home discharge. With relevance to the current opioid epidemic, several of these findings warrant further discussion.
We observed a modest decrease in the incidence of in-hospital opioid overdose from 6.0 to 4.1 per 10,000 cases between 2016 and 2020. A prior national analysis demonstrated a two-fold increase in the incidence of perioperative OD from 2002 to 2012, reaching an estimated peak of 10 per 10,000 in 2012 [7]. However, the opioid epidemic has greatly evolved in the decade since this study likely resulting in the evolution of in patient opioid prescription practices. Interestingly, the Northeast was associated with the steepest decrease in observed rates and the lowest odds of perioperative OD throughout the study period. In a study conducted by Unick and colleagues, the Northeast was found to have lower rates of prescription opioid-related hospitalizations relative to other geographical regions, but the highest rates of heroin related overdose [18]. Notably, as of 2016, Vermont, New Hampshire and Massachusetts were among the top 10 states in the US for synthetic opioid overdose death rates, with a large surge in incidence between 2013 and 2015 [19]. The trend observed in the present analysis could point toward conservative systematic prescription practices that were adopted in response to the striking increase observed [20]. Indeed, in a large meta-analysis performed by Nataraj et al., hospitals in the Northeast U.S. had lower prescription opioid volume relative to other regions [21]. Future research is needed to further characterize the regional variations in policies surrounding opioid prescriptions and perioperative pain management to minimize the risk of harm both in-patient and after discharge.
We observed several patient and clinical factors to be associated with increased odds of OD. Female sex, in particular, was linked to a nearly 70 % increase in the odds of perioperative OD. Prior literature has suggested that compared to age-matched men, women have poorer health status and less physiologic reserve [22]. Indeed, studies using the frailty index (FI) consistently demonstrate that women have higher FI scores, but paradoxically tolerate the frailty better as evidence by their longer life expectancy [22]. Sex differences in pain and responses to analgesic agents, coupled with increased frailty and smaller body habitus further complicate the delicate balance between appropriate analgesia and risk of OD [23]. We additionally observed White race to be associated with greater odds of OD. Considerable literature has described the effects of systemic racism and implicit bias on adequate pain management for non-White patients. Al-Hashimi et al. demonstrated medical professionals to be more likely to attribute reports of pain among White patients to medical conditions, and thus treat with strong painkillers, including opioids [[24], [25], [26]]. Conversely, non-White patients are less likely to be believed and treated for equivalent pain in both the acute and chronic setting. Furthermore, White adults continue to experience the highest rates of prescription opioid overdose, which may leave them more vulnerable to OD due to increased tolerance [27,28]. Opioid use disorder and tolerance was strongly associated with risk of perioperative OD and could explain this observed association. Preexisting chronic lung and kidney disease further increased the risk of experiencing perioperative OD. Opioids are known to have an increased risk of respiratory depression for those with decreased baseline pulmonary reserve [29]. Additionally, opioids are renally excreted, and underlying renal disease can narrow the delicate therapeutic index [30]. Individual patient characteristics must be considered when managing perioperative pain to mitigate the risk of opioid overdose.
The risk of perioperative OD was not equivalent across all operations, with spinal fusion and cardiothoracic procedures accounting for the greatest proportion of OD patients in the cohort. Deyo et al. reported back pain is one of the most common reasons for seeking medical care in the U.S. and opioids are now the most frequently prescribed drug class within this patient population [31]. As such, it is likely many of these patients have been managed outpatient with an opioid prior to fusion. Furthermore, pain is generally in proportion to factors which influence the nociceptive threshold, such as the location of the surgery, as well as the degree of skin and tissue involvement [32]. Midline sternotomy and extracorporeal circulation are commonly required in cardiothoracic operations and are associated with a high pain index [32]. However, enhanced recovery after thoracic surgery protocols have demonstrated success in reducing the burden of opioid use postoperatively without negatively affecting outcomes [33]. While there are unmodifiable factors associated with pain following surgery, implementing standardized care pathways reduces bias and opioid utilization, which has important implications for patient safety.
Perioperative OD was associated with increased LOS, hospitalization costs, and higher odds of non-home discharge. Immediate intervention following in-hospital OD may prevent sequelae of prolonged respiratory depression, including death [34]. While monitoring of respiratory status and vital signs following an OD is undoubtedly necessary, prolonged hospitalization is not without risk of additional clinical complications and greater financial burden [35]. Costs aside, prolonged hospitalization is associated with greater risk of thromboembolic events, infection, and overall deconditioning [36,37]. While individual clinical outcomes were not examined in the present analysis due to the heterogeneity in procedures examined, non-home discharge is a proxy often used to evaluate clinical status upon discharge [38]. Prior literature has suggested that each day in a hospital is associated with a ∼5 % reduction in muscle strength from baseline and may necessitate prolonged rehabilitation [39]. While perioperative OD poses an immediate risk to patient safety, it is also important to consider the potential long-term impact of experiencing a perioperative OD on patients' health, including the risk of substance use disorder. Prior research has demonstrated a large majority of patients who develop opioid use disorder were first exposed to opioids in a healthcare setting [40]. In a study of 7651 patients undergoing major operations across 3 major medical centers, Thiels and colleagues identified significant hospital variation in opioid prescription practices independent of patient factors [41]. Furthermore, Hill et al. observed that, on average, 200 % of the opioid dose need to reach analgesia was prescribed to patients following general surgery [5]. Surgeons play a critical role in perioperative pain management, and a significant proportion of prescriptions for people who die from prescription overdose are provided by surgeons [42]. While the analgesic benefit of postoperative opioids should not be diminished, it is important to balance the potential long-term risks of such medications. Contemporary pain management strategies have emphasized nerve blocks, and alternative pharmacologic interventions for post-operative pain to combat the iatrogenic influence on the opioid epidemic [43]. Our findings underscore the relevance of such opioid-sparing strategies in the management of postoperative pain. Future work is needed to develop appropriate pain management alternatives which minimize exposure to medications carrying high risk of dependence.
The present analysis has several limitations inherent to its retrospective design and the administrative structure of the data. The NIS does not include data regarding specific imaging findings or laboratory results that may guide clinical decision-making regarding pain management or the provide insight into the use of opioid sparing analgesic strategies. We also lack information about the exact timing and location of the in-hospital OD, as well as the exact analgesic regimen used. We are further unable to examine the impact of individual procedures and complications on overall length of stay and costs reported. Furthermore, we were unable to account for patient-reported outcomes including pain level and prior experience with opioid medications that may further influence their course of care. Our reliance on conservative ICD-10 codes for the classification of overdose may only captured the most severe cases of perioperative OD, and therefore probably underestimates the true incidence. Additionally, given the retrospective design, we are unable to make causal associations between OD and the outcomes of interest. Nevertheless, the present analysis utilized the largest all-payer database and robust statistical analysis to decrease bias and enhance the generalizability of our findings.
Conclusion
Our findings suggest that perioperative opioid overdose is a rare complication following elective surgery that impacts clinical outcomes and overall resource utilization. Several patient factors including age, female sex, race, burden of comorbid disease, income quartile, as well as a history of substance use disorder were associated with experiencing a perioperative OD. Additionally, the type of operation and hospital region independently influenced the risk of OD. Finally, OD was associated with incremental increases in LOS and hospitalization costs, and higher odds of non-home discharge. Given the opioid epidemic, examination of in-hospital use of opioids remains important to ensure safe, standardized, and adequate pain management strategies in the perioperative setting.
Ethics approval
This study was deemed exempt from full review by the Institutional Review Board at the University of California, Los Angeles.
Funding/financial support
No external financial support was received from any source.
CRediT authorship contribution statement
Joanna Curry: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft. Troy Coaston: Conceptualization, Methodology, Writing – review & editing. Amulya Vadlakonda: Writing – review & editing. Sara Sakowitz: Conceptualization, Methodology. Saad Mallick: Writing – review & editing. Nikhil Chervu: Conceptualization, Methodology. Baran Khoraminejad: Resources. Peyman Benharash: Conceptualization, Methodology, Supervision, Writing – review & editing.
Declaration of competing interest
The authors of this manuscript have no related conflicts of interest to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sopen.2024.03.002.
Appendix A. Supplementary data
Supplementary tables
References
- 1.Opioids. CDC; August 8, 2023. Understanding the opioid overdose epidemic.https://www.cdc.gov/opioids/basics/epidemic.html [Google Scholar]
- 2.Abuse NI on D. Drug Overdose Death Rates National Institute on Drug Abuse (NIDA) June 30, 2023. https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates
- 3.Wunsch H., Wijeysundera D.N., Passarella M.A., Neuman M.D. Opioids prescribed after low-risk surgical procedures in the United States, 2004–2012. JAMA. 2016;315(15):1654–1657. doi: 10.1001/jama.2016.0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cron D.C., Lee J.S., Dupree J.M., et al. Provider characteristics associated with outpatient opioid prescribing after surgery. Ann Surg. 2020;271(4):680–685. doi: 10.1097/SLA.0000000000003013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill M.V., McMahon M.L., Stucke R.S., Barth R.J. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265(4):709–714. doi: 10.1097/SLA.0000000000001993. [DOI] [PubMed] [Google Scholar]
- 6.Hah J.M., Bateman B.T., Ratliff J., Curtin C., Sun E. Chronic opioid use after surgery: implications for perioperative management in the face of the opioid epidemic. Anesth Analg. 2017;125(5):1733–1740. doi: 10.1213/ANE.0000000000002458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cauley C.E., Anderson G., Haynes A.B., Menendez M., Bateman B.T., Ladha K. Predictors of in-hospital postoperative opioid overdose after major elective operations: a nationally representative cohort study. Ann Surg. 2017;265(4):702–708. doi: 10.1097/SLA.0000000000001945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ward E.N., Quaye A.N.A., Wilens T.E. Opioid use disorders: perioperative management of a special population. Anesth Analg. 2018;127(2):539–547. doi: 10.1213/ANE.0000000000003477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gan T.J. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287–2298. doi: 10.2147/JPR.S144066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.HCUP-US NIS overview. https://hcup-us.ahrq.gov/nisoverview.jsp
- 11.Sahni N.R., Dalton M., Cutler D.M., Birkmeyer J.D., Chandra A. Surgeon specialization and operative mortality in United States: retrospective analysis. BMJ. 2016;354 doi: 10.1136/bmj.i3571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Walraven C., Austin P.C., Jennings A., Quan H., Forster A.J. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626–633. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 13.Elixhauser A., Steiner C., Harris D.R., Coffey R.M. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Using appropriate price indices for expenditure comparisons. https://meps.ahrq.gov/about_meps/Price_Index.shtml
- 15.Cuzick J. A Wilcoxon-type test for trend. Stat Med. 1985;4(1):87–90. doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- 16.H T., Tibshirani Robert, Wainwright Martin. Chapman and Hall/CRC; 2015. Statistical learning with sparsity: the Lasso and generalizations. [DOI] [Google Scholar]
- 17.Tilford J.M., Roberson P.K., Fiser D.H. Using lfit and lroc to evaluate mortality prediction models. Stata Tech Bull. 1996;5(28) https://ideas.repec.org//a/tsj/stbull/y1996v5i28sbe12.html [Google Scholar]
- 18.Unick G.J., Ciccarone D. US regional and demographic differences in prescription opioid and heroin-related overdose hospitalizations. Int J Drug Policy. 2017;46:112–119. doi: 10.1016/j.drugpo.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stopka T.J., Jacque E., Kelso P., et al. The opioid epidemic in rural northern New England: an approach to epidemiologic, policy, and legal surveillance. Prev Med. 2019;128 doi: 10.1016/j.ypmed.2019.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zajacova A., Grol-Prokopczyk H., Limani M., Schwarz C., Gilron I. Prevalence and correlates of prescription opioid use among US adults, 2019–2020. PLoS One. 2023;18(3) doi: 10.1371/journal.pone.0282536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nataraj N., Zhang K., Guy G.P., Losby J.L. Identifying opioid prescribing patterns for high-volume prescribers via cluster analysis. Drug Alcohol Depend. 2019;197:250–254. doi: 10.1016/j.drugalcdep.2019.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gordon E.H., Peel N.M., Samanta M., Theou O., Howlett S.E., Hubbard R.E. Sex differences in frailty: a systematic review and meta-analysis. Exp Gerontol. 2017;89:30–40. doi: 10.1016/j.exger.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 23.Thurston K.L., Zhang S.J., Wilbanks B.A., Billings R., Aroke E.N. A systematic review of race, sex, and socioeconomic status differences in postoperative pain and pain management. J Perianesth Nurs. 2023;38(3):504–515. doi: 10.1016/j.jopan.2022.09.004. [DOI] [PubMed] [Google Scholar]
- 24.Al-Hashimi M., Scott S., Griffin-Teall N., Thompson J. Influence of ethnicity on the perception and treatment of early post-operative pain. Br J Pain. 2015;9(3):167–172. doi: 10.1177/2049463714559254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mossey J.M. Defining racial and ethnic disparities in pain management. Clin Orthop Relat Res. 2011;469(7):1859. doi: 10.1007/s11999-011-1770-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Herb J.N., Williams B.M., Chen K.A., et al. The impact of standard postoperative opioid prescribing guidelines on racial differences in opioid prescribing: a retrospective review. Surgery. 2021;170(1):180–185. doi: 10.1016/j.surg.2020.12.034. [DOI] [PubMed] [Google Scholar]
- 27.Hoopsick R.A., Homish G.G., Leonard K.E. Differences in opioid overdose mortality rates among middle-aged adults by race/ethnicity and sex, 1999–2018. Public Health Rep. 2021;136(2):192–200. doi: 10.1177/0033354920968806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Larochelle M.R., Slavova S., Root E.D., et al. Disparities in opioid overdose death trends by race/ethnicity, 2018–2019, from the HEALing communities study. Am J Public Health. 2021;111(10):1851–1854. doi: 10.2105/AJPH.2021.306431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gupta K., Nagappa M., Prasad A., et al. Risk factors for opioid-induced respiratory depression in surgical patients: a systematic review and meta-analyses. BMJ Open. 2018;8(12) doi: 10.1136/bmjopen-2018-024086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Owsiany M.T., Hawley C.E., Triantafylidis L.K., Paik J.M. Opioid management in older adults with chronic kidney disease: a review. Am J Med. 2019;132(12):1386–1393. doi: 10.1016/j.amjmed.2019.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deyo R.A., Korff M.V., Duhrkoop D. Opioids for low back pain. BMJ. 2015;350 doi: 10.1136/bmj.g6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Full article: assessment and pathophysiology of pain in cardiac surgery. https://www.tandfonline.com/doi/full/10.2147/JPR.S162067 [DOI] [PMC free article] [PubMed]
- 33.Razi S.S., Stephens-McDonnough J.A., Haq S., et al. Significant reduction of postoperative pain and opioid analgesics requirement with an Enhanced Recovery After Thoracic Surgery protocol. J Thorac Cardiovasc Surg. 2021;161(5):1689–1701. doi: 10.1016/j.jtcvs.2019.12.137. [DOI] [PubMed] [Google Scholar]
- 34.Danovitch I., Vanle B., Van Groningen N., Ishak W., Nuckols T. Opioid overdose in the hospital setting: a systematic review. J Addict Med. 2020;14(1):39. doi: 10.1097/ADM.0000000000000536. [DOI] [PubMed] [Google Scholar]
- 35.Marmor M., Liu S., Long J., Chertow G.M., Rogers A.J. Prolonged hospitalization following acute respiratory failure. Chest. 2021;159(5):1867–1874. doi: 10.1016/j.chest.2020.11.023. [DOI] [PubMed] [Google Scholar]
- 36.Smith T.O., Sreekanta A., Walkeden S., Penhale B., Hanson S. Interventions for reducing hospital-associated deconditioning: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2020;90 doi: 10.1016/j.archger.2020.104176. [DOI] [PubMed] [Google Scholar]
- 37.Anderson M.E., Glasheen J.J., Anoff D., Pierce R., Capp R., Jones C.D. Understanding predictors of prolonged hospitalizations among general medicine patients: a guide and preliminary analysis. J Hosp Med. 2015;10(9):623–626. doi: 10.1002/jhm.2414. [DOI] [PubMed] [Google Scholar]
- 38.Arya S., Long C.A., Brahmbhatt R., et al. Preoperative frailty increases risk of nonhome discharge after elective vascular surgery in home-dwelling patients. Ann Vasc Surg. 2016;35:19–29. doi: 10.1016/j.avsg.2016.01.052. [DOI] [PubMed] [Google Scholar]
- 39.Hashem M.D., Parker A.M., Needham D.M. Early mobilization and rehabilitation of patients who are critically ill. Chest. 2016;150(3):722–731. doi: 10.1016/j.chest.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Edlund M.J., Martin B.C., Russo J.E., DeVries A., Braden J.B., Sullivan M.D. The role of opioid prescription in incident opioid abuse and dependence among individuals with chronic noncancer pain: the role of opioid prescription. Clin J Pain. 2014;30(7):557. doi: 10.1097/AJP.0000000000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thiels C.A., Anderson S.S., Ubl D.S., et al. Wide variation and overprescription of opioids after elective surgery. Ann Surg. 2017;266(4):564. doi: 10.1097/SLA.0000000000002365. [DOI] [PubMed] [Google Scholar]
- 42.Bicket M.C., Brat G.A., Hutfless S., Wu C.L., Nesbit S.A., Alexander G.C. Optimizing opioid prescribing and pain treatment for surgery: review and conceptual framework. Am J Health-Syst Pharm. 2019;76(18):1403–1412. doi: 10.1093/ajhp/zxz146. [DOI] [PubMed] [Google Scholar]
- 43.Gabriel R.A., Swisher M.W., Sztain J.F., Furnish T.J., Ilfeld B.M., Said E.T. State of the art opioid-sparing strategies for post-operative pain in adult surgical patients. Expert Opin Pharmacother. 2019;20(8):949–961. doi: 10.1080/14656566.2019.1583743. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary tables