Abstract
The hemagglutinin (HA) of fowl plague virus was lengthened and shortened by site-specific mutagenesis at the cytoplasmic tail, and the effects of these modifications on HA functions were analyzed after expression from a simian virus 40 vector. Elongation of the tail by the addition of one to six histidine (His) residues did not interfere with intracellular transport, glycosylation, proteolytic cleavage, acylation, cell surface expression, and hemadsorption. However, the ability to induce syncytia at a low pH decreased dramatically depending on the number of His residues added. Partial fusion (hemifusion), assayed by fluorescence transfer from octadecylrhodamine-labeled erythrocyte membranes, was also reduced, but even with the mutant carrying six His residues, significant transfer was observed. However, when the formation of fusion pores was examined with hydrophilic fluorescent calcein, transfer from erythrocytes to HA-expressing cells was not observed with the mutant carrying six histidine residues. The addition of different amino acids to the cytoplasmic tail of HA caused an inhibitory effect similar to that caused by the addition of His. On the other hand, a mutant lacking the cytoplasmic tail was still able to fuse at a reduced level. These results demonstrate that elongation of the cytoplasmic tail interferes with the formation and enlargement of fusion pores. Thus, the length of the cytoplasmic tail plays a critical role in the fusion process.
The influenza virus hemagglutinin (HA) is a multifunctional membrane protein responsible for the attachment of virions to the cell surface and for membrane fusion, which allows penetration of the viral genome into the cytoplasm. Several steps in the fusion process can be discriminated. These include the formation of a membrane stalk, partial fusion (hemifusion), pore formation, flickering, and pore enlargement (13, 14). It is generally accepted that the fusion activity of HA is mediated by the hydrophobic fusion peptide at the amino terminus of the HA2 subunit. At a neutral pH, the fusion peptide is located at the bottom of the stem region of the HA spike (36), distant from the membrane of the target cell. It has long been known that fusion occurs only at a low pH (6, 12) and that the pH shift is necessary for a conformational change in the ectodomain of HA (34, 35). Bullough and coworkers (1) have proven this concept by showing in a crystallographic study that, at a low pH, the fusion peptide is exposed at the tip of the spike and thus may interact with the target membrane.
In contrast to understanding of the ectodomain, structure-function relationships are less well understood in the transmembrane domain and in the cytoplasmic tail. In particular, it is not clear how these regions contribute to fusion. The first evidence for their involvement in fusion came from the observation that deletion of the covalently attached fatty acids from the transmembrane and cytoplasmic domains of A/Japan/305/57 HA (subtype H2) abolished fusion activity (18). It was therefore concluded that acylation of these domains was essential for fusion activity. On the other hand, several other studies with H2 and different HA subtypes showed fusion activity after the deletion of all fatty acids (19, 29, 31). Kemble and coworkers (10) replaced the transmembrane and cytoplasmic domains of HA with glycophosphatidylinositol (GPI) and found that the GPI-anchored HA mediated the transfer of lipophilic fluorescent octadecylrhodamine (R18) from R18-labeled erythrocyte membranes to HA-expressing cells but failed to mediate the transfer of hydrophilic fluorescent calcein. The authors concluded from these studies that the ectodomain of HA mediates hemifusion but that the transmembrane and cytoplasmic domains are necessary for pore formation and therefore for complete fusion. However, GPI-anchored HA differed from original HA in oligosaccharide processing, indicating abnormal folding. It is therefore not absolutely clear whether the effect of the GPI anchor on fusion activity is due to the loss of the transmembrane and cytoplasmic domains or to a conformational change in the ectodomain. Jin and coworkers (7) showed that HA lacking the cytoplasmic domain was incorporated into virus particles and that such virus was infectious, indicating that the cytoplasmic domain was not an absolute prerequisite for virus morphogenesis and infectivity. However, such virus was quickly replaced by revertants which possessed the cytoplasmic tail, indicating that this region played some role in virus replication. This finding was also suggested by a study showing that infectious virus particles were not recovered when the acylation of HA was prevented by site-directed mutagenesis (39).
In the present study, we analyzed the effect of modification of the tail length on the fusion activity of HA. We show that tail elongation, while not affecting processing, surface transport, and receptor binding activity, reduces fusion by interfering with the formation and enlargement of fusion pores. The effect depends on the size but not on the sequence of the attached peptide. Deletion of the tail has little effect on fusion. These results indicate that the length of the cytoplasmic tail plays a critical role in the fusion activity of HA.
MATERIALS AND METHODS
Elongation of the cytoplasmic tail of HA.
cDNA of the HA gene derived from fowl plague virus (FPV) strain A/FPV/Rostock/34 (H7N1) was modified by insertion of an oligonucleotide corresponding to six His residues between the end of the coding region and the stop codon by use of an M13mp11 vector as described previously (21). The resulting mutant HA was named +6His. Mutants with shorter His tails were obtained by deleting portions of the +6His mutant. Other amino acids were added to the end of the coding region by essentially the same procedure.
Expression of HA genes.
cDNAs of wild-type (WT) and mutant HAs were inserted in the BamHI site of the simian virus 40 (SV40) late promoter-regulated region of the pA11SVL3 vector. Cells were transfected together with helper DNA as described previously (20). CV-1 cells were grown in Dulbecco’s modified minimum essential medium (DMEM) supplemented with 5% fetal calf serum (FCS). Recombinant virus was harvested by freezing and thawing the transfected cells twice, and the cell homogenate was used as a virus source. WT and mutant HAs were expressed in the presence of 10 mM ammonium chloride to prevent inactivation in the acidic milieu of the trans-Golgi network (20, 30). Hemadsorption, fusion testing, and analysis of expressed protein were done 2 days after infection with recombinant virus.
Hemadsorption test.
Two days after infection, HA-expressing cell monolayers were washed once with FCS-free medium and incubated with 50 mU of Vibrio cholerae neuraminidase (VCNA; test neuraminidase; Behringwerke, Marburg, Germany) in 2 ml of medium at 37°C for 1 h, since FPV HA requires VCNA pretreatment for hemadsorption activity (21). After VCNA treatment, the cells were washed three times with phosphate-buffered saline (PBS) containing Mg and Ca ions and then overlaid with a suspension of freshly prepared guinea pig erythrocytes. After a 15-min adsorption period, unbound erythrocytes were removed with the overlay fluid and by rinsing of the culture with an excess of PBS.
Fusion test.
HA-expressing CV-1 cells were treated with acidic RPMI 1640 medium (pH 5.0) for 5 min at 37°C. The medium was exchanged for neutral DMEM containing 5% FCS. After 4 h of incubation in neutral DMEM, cells were fixed with ethanol and stained with Giemsa solution. The number of cells fused was determined by counting nuclei in syncytia, and the number of HA-expressing cells was estimated by counting hemadsorption-positive cells after VCNA treatment. The specific fusion activity of each HA mutant was expressed as the fusion index, which is the total number of nuclei in syncytia per microscopic field divided by the number of hemadsorption-positive cells per field.
PAGE of expressed HA protein.
HA-expressing CV-1 cells were labeled with [35S]methionine for 3 h, chased for 1 h, and then lysed in radioimmunoprecipitation buffer as described previously (21). After immunoprecipitation with anti-FPV rabbit serum and protein A-Sepharose 4B (Sigma), HA proteins were analyzed under denaturing conditions by sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis (PAGE). Fatty acid bound covalently to HA was labeled for 16 h with [3H]palmitic acid and then analyzed by SDS-PAGE in the absence of a reducing agent as described previously (31).
Endo H digestion of expressed HA protein.
HA protein was labeled with [35S]methionine and recovered by immunoprecipitation as described above. The complex of HA, anti-FPV rabbit immunoglobulin G (IgG), and protein A-Sepharose 4B was suspended in 10 μl of 0.1 M phosphate buffer (pH 7.5) containing 0.1% SDS and 0.5% 2-mercaptoethanol and heated at 95°C for 3 min. Excess SDS was blocked with Triton X-100 at a final concentration of 1%. HA was digested with endoglycosidase H (endo H) (Boehringer GmbH, Mannheim, Germany) at a concentration of 1 mU/10 μl overnight at 37°C and analyzed by PAGE as described previously (21).
Immunofluorescence staining of HA-expressing cells.
HA-expressing CV-1 cell monolayers were washed once with PBS, incubated with anti-FPV rabbit antiserum at 37°C for 1 to 30 min, washed twice, and fixed with a chilled solution of 1% paraformaldehyde in PBS. After extensive washing with saline, the fixed cells were incubated with anti-rabbit IgG biotinylated donkey serum at 37°C for 1 h, and then the antigen-antibody complex was visualized with streptavidin fluorescein (Amersham Co., Amersham, United Kingdom).
Flow cytometric analysis of immunostained HA-expressing cells.
For detection of HA on cell surfaces, CV-1 cells infected with recombinant SV40-HA were detached from culture dishes by EDTA and trypsin treatment 48 h postinfection and fixed with 2% paraformaldehyde for 15 min at room temperature. Cells were washed once with 2% glycine in PBS and incubated with a mouse monoclonal antibody (2A11-H7) recognizing the neutral HA and the low-pH form for 1 h at 37°C, followed by staining with a fluorescein isothiocyanate-conjugated goat anti-mouse immunoglobulin (4). Cells were resuspended in 1 ml of PBS and subjected to fluorescence-activated cell sorter (Becton Dickinson) analysis. Data were evaluated with Becton Dickinson FACScan research software, version 2.1. Inoculi of recombinant SV40-HA stocks were adjusted for infection of CV-1 cells to yield a maximum number of infected cells with similar surface HA expression levels. However, to ensure that HA-expressing CV-1 cells were surrounded by a sufficient number of noninfected cells for quantification of fusion, CV-1 cells were infected with 10% the input virus required for maximum expression of recombinant HA.
Labeling of erythrocyte membranes with R18.
Freshly prepared guinea pig erythrocytes (0.5 ml) were suspended in 10 ml of PBS. The suspension was vigorously mixed with 20 μl of R18 (Molecular Probes, Eugene, Oreg.) solution (2 mM in ethanol), and the mixture was incubated at 37°C for 15 min as described previously (16). The erythrocytes again pelleted, resuspended in 10 ml of PBS containing 0.4% bovine serum albumin, and incubated for 15 min at 37°C. R18-labeled erythrocytes were washed by centrifugation until the supernatant became clear and then were used for hemadsorption and fusion testing.
Labeling of erythrocytes with calcein.
Calcein AM (10 mM; 5 μl; Molecular Probes) in dimethyl sulfoxide was added to 10 ml of a guinea pig erythrocyte suspension. The mixture was vortexed and incubated for 30 min at 37°C as described previously (11). After the removal of excess calcein by centrifugation, the erythrocytes were incubated in 10 ml of PBS containing 0.4% bovine serum albumin for 15 min at 37°C. Calcein-filled erythrocytes were washed twice and used for further experiments.
RESULTS
Effect of His addition on the fusion activity of HA.
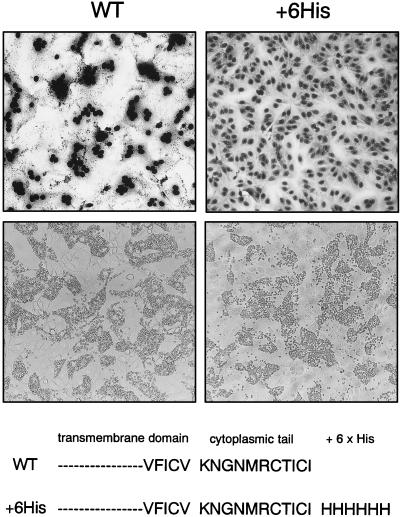
When six His residues were added to the end of the cytoplasmic domain of FPV HA by site-specific mutagenesis (+6His; Fig. 1), HA lost fusion activity, although the mutant showed hemadsorption activity as high as that of the WT. Cell fusion was induced by exposing the HA-expressing cells to pH 5.0 as described previously (20). Hemadsorption was induced by treatment of the HA-expressing cells with VCNA, since neuraminidase is essential for FPV HA to show hemadsorption activity (21). The results indicated that the His residues added to the cytoplasmic tail of HA interfered with cell fusion activity.
FIG. 1.
Hemadsorption (bottom panels) and cell fusion (top panels) of CV-1 cells expressing WT HA and +6His HA. Cells were infected with recombinant SV40-HA stocks and incubated for 2 days. HA was expressed in the presence of 10 mM ammonium chloride for protection against acid degradation during transport (20). Before hemadsorption, HA-expressing cells were treated with VCNA to remove sialic acid interfering with the binding of erythrocytes (21). Cell fusion was induced by acid treatment (pH 5.0). Amino acid sequences of the cytoplasmic tail of the WT and the +6His mutant are also shown.
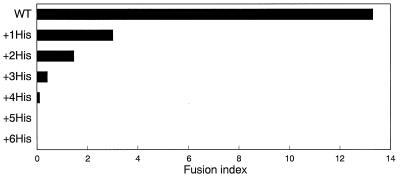
To examine how many His residues are necessary to interfere with cell fusion, we deleted His residues one by one from mutant +6His. When mutants carrying one to five His residues at the cytoplasmic tail (mutants +1His to +5His, respectively) were expressed in CV-1 cells by the SV40 expression vector, all mutants showed high hemadsorption activity after VCNA treatment (data not shown). Specific fusion activities of each mutant and the WT were evaluated as fusion indices. As shown in Fig. 2, the addition of as little as one His residue affected fusion activity considerably, and the addition of five His residues abolished fusion activity completely.
FIG. 2.
Specific fusion activity of the WT and +His mutants. HA expression and fusion tests were done as described in the legend to Fig. 1. The fusion index is the total number of nuclei in syncytia per field divided by the number of hemadsorption-positive cells per field before fusion induction.
Intracellular transport.
We then examined the effects of His addition on the intracellular transport, glycosylation, and acylation of HA. As FPV HA is cleaved by a cellular proprotein convertase in the trans-Golgi network, the cleavage of HA is a marker for transport through the exocytic pathway. HA-expressing cells were labeled with [35S]methionine, and HA proteins were analyzed by PAGE after quantitative immunoprecipitation. As shown in Fig. 3A, mutants with additional His residues were cleaved by cellular protease as well as the WT was. Cleavage rates were slightly lower with +5His and +6His mutants than with other HA mutants. However, the cleavage of +5His and +6His mutants was enhanced by trypsin treatment, but this treatment did not restore fusion activity (data not shown), indicating that the slight differences in cleavage rates could not explain the loss of cell fusion activity in these mutants. The intracellular transport of HA was also monitored by the acquisition of resistance against endo H digestion. It is known that the HA1 subunit of FPV HA has five complex oligosaccharides in the mature virion (9). The results shown in Fig. 3A and B indicate that all oligosaccharides of the HA1 subunit were endo H resistant, indicating that they were all of the complex type and therefore well processed. The HA2 subunit of FPV has two oligosaccharides, one of which is a high-mannose type and the other of which is partly a high-mannose type and partly a complex type (9). The results shown in Fig. 3A and B indicate that HA2 was a mixture of molecules containing two endo H-sensitive oligosaccharides and molecules containing one sensitive oligosaccharide and one resistant oligosaccharide. These results indicate that there was no significant difference in processing between the WT and the mutants.
FIG. 3.
Posttranslational processing of WT HA and mutant HA. (A) Proteolytic cleavage of HA. Expressed HA was labeled with [35S]methionine, recovered by immunoprecipitation, and then analyzed by PAGE. (B) Endo H digestion of HA. Labeled HA was recovered as described above and digested with endo H. (C) Acylation of HA. Expressed HA was labeled with [3H]palmitic acid for 16 h and analyzed by PAGE without 2-mercaptoethanol.
Acylation, which occurs before HA enters the Golgi apparatus, was examined by labeling with [3H]palmitic acid and PAGE analysis in the absence of a reducing agent. As shown in Fig. 3C, there was no difference in acylation between the WT and the mutants. A faint band corresponding to the HA2 subunit was also detected in each lane in spite of the absence of a reducing agent. This band appeared to result from the shedding of HA1 during the long labeling period. The data shown in Fig. 3C, as well as those shown in Fig. 3A and B, demonstrate that the number of His residues attached affected the electrophoretic mobility of HA2. From these observations it is clear that there are no significant differences in expression and processing rates between WT HA and the His mutants.
Surface exposure.
To determine the amount of HA exposed at the cell surface, CV-1 cells were analyzed by flow cytometry 48 h after infection with SV40 recombinants. As shown in Table 1, the mean fluorescence intensity and the percentage of cells expressing HA were similar in the WT and all the His mutants, indicating that tail elongation had little effect on the surface density of HA. We then compared the distribution of WT HA and +6His HA on the cell surface by immunostaining. HA-expressing cells were incubated with anti-FPV rabbit antiserum (final dilution, 1:250 in PBS) at 37°C for 1 to 30 min and fixed with 1% paraformaldehyde. After being washed with PBS, the fixed cells were incubated with anti-rabbit IgG biotinylated donkey serum at 37°C for 1 h, and the antigen-antibody complex was visualized with streptavidin-fluorescein. Antigen-antibody complexes formed many small clusters on the cell surface. The clusters became slightly larger with increasing incubation periods before fixation. However, no significant difference in the distribution or size of the clusters was observed between the WT and mutant +6His (data not shown). Thus, the distribution of +6His HA in the cell membrane resembles that of WT HA.
TABLE 1.
Fluorescence-activated cell sorter analysis of CV-1 cells expressing WT FPV HA and tail elongation mutants of FPV HAa
| HA | % of cells expressing HA | Mean fluorescence intensityb |
|---|---|---|
| WT | 69 ± 5 | 776 ± 46 |
| +1His | 72 ± 8 | 764 ± 25 |
| +2His | 69 ± 5 | 705 ± 58 |
| +3His | 67 ± 9 | 734 ± 45 |
| +4His | 65 ± 6 | 727 ± 31 |
| +5His | 61 ± 9 | 712 ± 25 |
| +6His | 81 ± 8 | 723 ± 33 |
Values are averages from four experiments.
Arbitrary units.
Effect of other amino acids added to the C terminus on fusion activity.
To examine whether the fusion-inhibiting effect is specific for His, we made three mutants with different elongation sequences (Table 2). These mutants were also expressed efficiently by the SV40 vector, and their cleavage, glycosylation, and hemadsorption activities were essentially the same as those of WT and the other mutants (data not shown). The fusion indices showed that all three mutants had extremely low fusion activity, demonstrating that not only His but also other amino acids interfere with cell fusion activity when added to the end of the cytoplasmic tail (Table 2). We also examined the fusion activity of a mutant from which the entire cytoplasmic domain had been deleted (mutant Nocyt). As shown in Table 2, mutant Nocyt had fusion activity, although at a reduced level compared to the WT.
TABLE 2.
Cell fusion activity of mutants with different cytoplasmic tails
| Mutant | Cytoplasmic domain | Amino acids added | Fusion index |
|---|---|---|---|
| —(WT) | KNGNMRCTICI | 12.80 | |
| Alagly | KNGNMRCTICI | AGAGA | 0.05 |
| Thrser | KNGNMRCTICI | TSTST | 0.04 |
| Arglys | KNGNMRCTICI | RKSRS | 0.02 |
| Nocyt | Deleted | 2.50 |
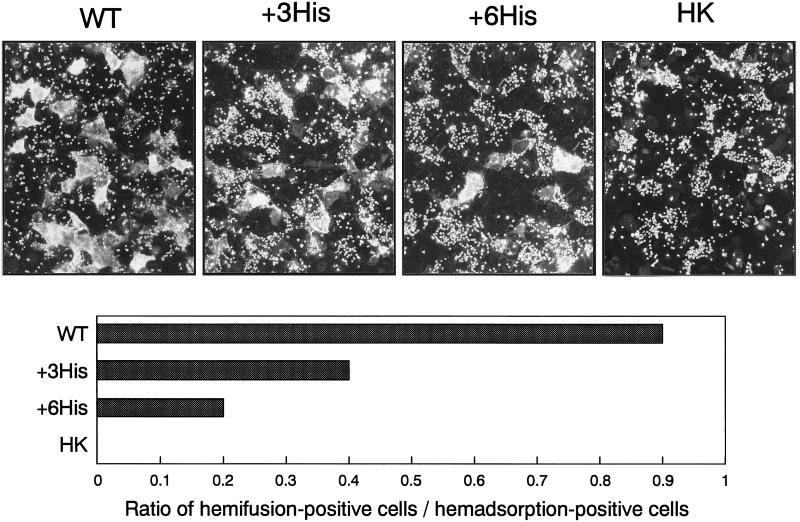
Effect of tail elongation on different stages of the fusion process.
We used two methods to analyze different stages of the fusion reaction, i.e., hemifusion and fusion pore building (11). Hemifusion was analyzed with R18-labeled erythrocytes. When hemifusion occurs, R18 is transferred in this assay from the outer layer of erythrocyte membranes to the outer layer of HA-expressing cell membranes, without an exchange of cytoplasmic contents (10, 15). Fusion pore building can be monitored by the transfer of hydrophilic fluorescent calcein from calcein-filled erythrocytes to HA-expressing cells. Freshly prepared guinea pig erythrocytes were labeled with R18 or calcein, and WT and mutant HA-expressing cells were pretreated with VCNA for hemadsorption tests as described in Materials and Methods. Fluorescence-labeled erythrocytes were added to the VCNA-pretreated cell monolayers and allowed to stand for 15 min at room temperature for hemadsorption. Excess erythrocytes were washed away, and the cell monolayers were treated with acidic fusion medium (pH 5.0) at 37°C for 5 min. Transfer of R18 and calcein was monitored immediately under a fluorescence microscope. As shown in Fig. 4, transfer of fluorescence from R18-labeled erythrocytes to HA-expressing cells was clearly observed with cells expressing WT FPV HA. On the other hand, there was no transfer when uncleaved Hong Kong type HA was expressed as a control (HK in Fig. 4). With +3His HA-expressing cells, many fluorescence-positive cells were observed, although the transfer efficiency seemed lower than that with the WT (+3His in Fig. 4). With +6His HA-expressing cells, the transfer rate was further reduced, but fluorescence-positive cells were still detected (+6His in Fig. 4). Hemifusion-positive cells and hemadsorption-positive cells were counted under a fluorescence microscope, and the ratios of hemifusion-positive cells to hemadsorption-positive cells are also shown in Fig. 4. It is clear that the +6His mutant retained hemifusion activity, although at a reduced level.
FIG. 4.
Fluorescence transfer from R18-labeled erythrocyte membranes to HA-expressing cells. After adsorption of R18-labeled erythrocytes, HA-expressing cells were treated at pH 5.0 for 5 min, and then the transfer of fluorescence was immediately examined under a fluorescence microscope. Photographs were taken 10 min after fusion induction. HK, Hong Kong type HA used as a control.
As shown in Fig. 5, calcein was readily transferred from erythrocytes to cells expressing WT HA, whereas transfer to +6His HA-expressing cells was hardly or not detected in most microscopic fields analyzed. Due to concentration-dependent quenching effects, calcein-filled intact erythrocytes are only faintly recognized under the fluorescence microscope. When calcein is released from the erythrocytes into HA-expressing cells, the quenching effect disappears, resulting in strong fluorescence in erythrocytes and cells. Figure 5 also shows that calcein was transferred not only to WT HA-expressing cells, i.e., hemadsorption-positive cells, but also to neighboring hemadsorption-negative cells, probably again through fusion pores.
FIG. 5.
Fluorescence transfer from calcein-filled erythrocytes to HA-expressing cells. Hemadsorption and fusion tests were done as described in the legend to Fig. 1. Photographs were taken 10 min after fusion induction.
Taken together, these results demonstrate that elongation of the cytoplasmic tail of HA abolishes the formation of fusion pores almost completely while reducing hemifusion only moderately.
DISCUSSION
The high conservation among the many HA subtypes emphasizes the structural and functional significance of the cytoplasmic tail, and it is generally assumed that by interacting with the matrix protein, the tail plays an important role in virus assembly. We describe here another function of this domain. We have found that elongation of the cytoplasmic tail of FPV HA interferes with fusion while not affecting transport, processing, surface density, and receptor binding activity. The observations made with the His mutants demonstrated that the inhibitory effect dramatically increased with the number of amino acid residues added. Loss of fusion activity was also observed when other amino acids were used for tail elongation, indicating that the effect neither required sequence specificity nor depended on charge or other apparent structural peculiarities. On the other hand, removal of the cytoplasmic tail, which did not interfere with surface exposure and receptor binding activity, could reduce but did not abolish fusion activity. This conclusion is indicated by the observations made here with the Nocyt mutant and by several other studies with similar results (8, 14, 26). Taken together, these observations indicate that the cytoplasmic tail is not an absolute requirement for fusion but that it plays an important modulating role in this process.
The observation that elongation of the cytoplasmic tail of HA interferes with fusion is reminiscent of previous studies with simian immunodeficiency virus (SIV) and human immunodeficiency virus (HIV) reporting that the cytoplasmic tails of the envelope proteins of these viruses could affect their fusion activity, since truncation at the C-terminal end resulted in increased syncytium-forming ability (17, 25, 27, 38). In other retroviruses, including murine leukemia virus (MuLV), Mason-Pfizer monkey virus, and equine infectious anemia virus, the envelope protein cytoplasmic tails are further processed by the viral protease during virus maturation (2, 5, 24, 27, 28). Furthermore, it has been shown that processing results in removal of the C-terminal R peptide and that this removal is important to activate fusion activity (22, 23). Finally, a study with SIV-MuLV chimeric envelope proteins, in which the entire cytoplasmic tail of the SIV envelope protein was replaced by either the full-length MuLV cytoplasmic tail or a truncated MuLV cytoplasmic tail with the R peptide deleted or in which the MuLV R peptide was added to the cytoplasmic tail of the SIV envelope protein, confirmed the concept that the highly hydrophilic MuLV R peptide has profound inhibitory effects on virus-induced cell fusion (37).
Insight into the mechanism of how the cytoplasmic tail modulates fusion comes from recent X-ray crystallographic studies performed on the fusion-active conformation of HA2 (1) and on the transmembrane subunits of the envelope glycoproteins of Moloney MuLV (3) and HIV type 1 (32) and suggesting a common mechanism for fusion initiation. According to these studies, the core of the proteins is an extended, triple-stranded α-helical coiled coil with the amino terminus at its tip. A carboxy-terminal α helix packs in the reverse direction against the outside of the coiled coil. This conformation places the amino-terminal fusion peptides and the carboxy-terminal membrane anchors near each other at one end of the rod-shaped molecule. Electron microscopy and antibody labeling of membrane-associated HA2 provide further support for such a structure (33). With the membrane anchor embedded in the viral envelope and the fusion peptide immersed in the target membrane, this structure forces both membranes into close apposition. Flexible links between the central rod on one side and the fusion peptide and the membrane anchor on the other side allow oscillation of both hydrophobic domains in the adjacent membranes, which causes perturbation and mixing of the lipid bilayers and eventually results in fusion (32). It is an intrinsic feature of this model that the fusion peptide and the membrane anchor have very similar functions in fusion, and the observation that the process only proceeds to hemifusion when the anchor peptide is replaced by lipid (10) indicates that both hydrophobic peptide domains are equally important for complete fusion. On the other hand, the data presented here support the view that the mobility of the membrane anchor is limited by the cytoplasmic tail and that this constraint interferes with fusion when the tail is elongated beyond its natural size. Restriction of anchor mobility by an elongated tail should therefore have the same effect as replacement of the transmembrane peptide by a lipid anchor; i.e., it should interfere with the formation and enlargement of fusion pores rather than with hemifusion, exactly as was observed in the present study. Studies with acylation mutants of FPV HA indicate that the loss of tail fatty acids reduces fusion activity in a manner similar to that of tail elongation (unpublished data). Thus, it appears that the size and hydrophobicity of the tail are important determinants for anchor mobility. The observation that removal of the tail has little effect on fusion conforms with this concept. Our data are also compatible with other models (10, 13) which, although differing in several important details, agree with the model proposed by Weissenhorn and coworkers (32) in postulating an active role of the membrane anchor in the fusion process.
ACKNOWLEDGMENTS
We thank Sachiyo Omori, Kawasaki Medical School, for illustrations.
This work was supported by the Deutsche Forschungsgemeinschaft (SFB 286); the Fonds der Chemischen Industrie; the Japanese Ministry of Education, Science, and Culture (science research grants C 08670350 and C 09670321); and Kawasaki Medical School (project research grants IV 8-401 and V 9-507).
REFERENCES
- 1.Bullough P A, Hughson F M, Skehel J J, Wiley D C. Structure of influenza haemagglutinin at the pH of membrane fusion. Nature. 1994;371:37–43. doi: 10.1038/371037a0. [DOI] [PubMed] [Google Scholar]
- 2.Crawford S, Goff S P. A deletion mutation in the 5′ part of the pol gene of Moloney murine leukemia virus blocks proteolytic processing of the Gag and Pol polyproteins. J Virol. 1985;53:899–907. doi: 10.1128/jvi.53.3.899-907.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fass D, Harrison S C, Kim P S. Retrovirus envelope domain at 1.7 angstrom resolution. Nat Struct Biol. 1996;3:465–469. doi: 10.1038/nsb0596-465. [DOI] [PubMed] [Google Scholar]
- 4.Garten W, Will C, Buckard K, Kuroda K, Ortmann D, Munk K, Scholtissek C, Schnittler H, Drenckhahn D, Klenk H-D. Structure and assembly of hemagglutinin mutants of fowl plague virus with impaired surface transport. J Virol. 1992;66:1495–1505. doi: 10.1128/jvi.66.3.1495-1505.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Green N, Shinnick T M, Witte O, Ponticelli A, Sutcliffe J G, Lerner R A. Sequence-specific antibodies show that maturation of Moloney leukemia virus envelope polyprotein involves removal of a COOH-terminal peptide. Proc Natl Acad Sci USA. 1981;78:6023–6027. doi: 10.1073/pnas.78.10.6023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang R T, Rott R, Klenk H-D. Influenza viruses cause hemolysis and fusion of cells. Virology. 1981;110:243–247. doi: 10.1016/0042-6822(81)90030-1. [DOI] [PubMed] [Google Scholar]
- 7.Jin H, Leser G P, Lamb R A. The influenza virus hemagglutinin cytoplasmic tail is not essential for virus assembly or infectivity. EMBO J. 1994;13:5504–5515. doi: 10.1002/j.1460-2075.1994.tb06885.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jin H, Subbarao K, Bagai S, Leser G P, Murphy B R, Lamb R A. Palmitylation of the influenza virus hemagglutinin (H3) is not essential for virus assembly or infectivity. J Virol. 1996;70:1406–1414. doi: 10.1128/jvi.70.3.1406-1414.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keil W, Geyer R, Dabrowski J, Dabrowski U, Niemann H, Stirm S, Klenk H-D. Carbohydrates of influenza virus. Structural elucidation of the individual glycans of the FPV hemagglutinin by two-dimensional 1H n.m.r. and methylation analysis. EMBO J. 1985;4:2711–2720. doi: 10.1002/j.1460-2075.1985.tb03991.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kemble G W, Danieli T, White J M. Lipid-anchored influenza hemagglutinin promotes hemifusion, not complete fusion. Cell. 1994;76:383–391. doi: 10.1016/0092-8674(94)90344-1. [DOI] [PubMed] [Google Scholar]
- 11.Kemble G W, Henis Y I, White J M. GPI- and transmembrane-anchored influenza hemagglutinin differ in structure and receptor binding activity. J Cell Biol. 1993;122:1253–1265. doi: 10.1083/jcb.122.6.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maeda T, Ohnishi S. Activation of influenza virus by acidic media causes hemolysis and fusion of erythrocytes. FEBS Lett. 1980;122:283–287. doi: 10.1016/0014-5793(80)80457-1. [DOI] [PubMed] [Google Scholar]
- 13.Melikyan G B, Chernomordik L V. Membrane rearrangements in fusion mediated by viral proteins. Trends Microbiol. 1997;5:349–355. doi: 10.1016/S0966-842X(97)01107-4. [DOI] [PubMed] [Google Scholar]
- 14.Melikyan G B, Jin H, Lamb R A, Cohen F S. The role of the cytoplasmic tail region of influenza virus hemagglutinin in formation and growth of fusion pores. Virology. 1997;235:118–128. doi: 10.1006/viro.1997.8686. [DOI] [PubMed] [Google Scholar]
- 15.Melikyan G B, White J M, Cohen F S. GPI-anchored influenza hemagglutinin induces hemifusion to both red blood cell and planar bilayer membranes. J Cell Biol. 1995;131:679–691. doi: 10.1083/jcb.131.3.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morris S J, Sarkar D P, White J M, Blumenthal R. Kinetics of pH-dependent fusion between 3T3 fibroblasts expressing influenza hemagglutinin and red blood cells. J Biol Chem. 1989;264:3972–3978. [PubMed] [Google Scholar]
- 17.Mulligan M J, Yamshchikov G V, Ritter G D, Jr, Gao F, Jin M J, Nail C D, Spies C P, Hahn B H, Compans R W. Cytoplasmic domain truncation enhances fusion activity by the exterior glycoprotein complex of human immunodeficiency virus type 2 in selected cell types. J Virol. 1992;66:3971–3975. doi: 10.1128/jvi.66.6.3971-3975.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Naeve C W, Williams D. Fatty acids on the A/Japan/305/57 influenza virus hemagglutinin have a role in membrane fusion. EMBO J. 1990;9:3857–3866. doi: 10.1002/j.1460-2075.1990.tb07604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naim H Y, Amarneh B, Ktistakis N T, Roth M G. Effects of altering palmitylation sites on biosynthesis and function of the influenza virus hemagglutinin. J Virol. 1992;66:7585–7588. doi: 10.1128/jvi.66.12.7585-7588.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ohuchi M, Cramer A, Vey M, Ohuchi R, Garten W, Klenk H-D. Rescue of vector-expressed fowl plague virus hemagglutinin in biologically active form by acidotropic agents and coexpressed M2 protein. J Virol. 1994;68:920–926. doi: 10.1128/jvi.68.2.920-926.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ohuchi M, Feldmann A, Ohuchi R, Klenk H-D. Neuraminidase is essential for fowl plague virus hemagglutinin to show hemagglutinating activity. Virology. 1995;212:77–83. doi: 10.1006/viro.1995.1455. [DOI] [PubMed] [Google Scholar]
- 22.Ragheb J A, Anderson W F. pH-independent murine leukemia virus ecotropic envelope-mediated cell fusion: implications for the role of the R peptide and p12E TM in viral entry. J Virol. 1994;68:3220–3231. doi: 10.1128/jvi.68.5.3220-3231.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rein A, Mirro J, Haynes J G, Ernst S M, Nagashima K. Function of the cytoplasmic domain of a retroviral transmembrane protein: p15E-p2E cleavage activates the membrane fusion capability of the murine leukemia virus Env protein. J Virol. 1994;68:1773–1781. doi: 10.1128/jvi.68.3.1773-1781.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rice N R, Henderson L E, Sowder R C, Copeland T D, Oroszlan S, Edwards J F. Synthesis and processing of the transmembrane envelope protein of equine infectious anemia virus. J Virol. 1990;64:3770–3778. doi: 10.1128/jvi.64.8.3770-3778.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ritter G D, Jr, Mulligan M J, Jydy S L, Compans R W. Cell fusion activity of the simian immunodeficiency virus envelope protein is modulated by the intracytoplasmic domain. Virology. 1993;197:255–264. doi: 10.1006/viro.1993.1586. [DOI] [PubMed] [Google Scholar]
- 26.Simpson D A, Lamb R A. Alterations to influenza virus hemagglutinin cytoplasmic tail modulate virus infectivity. J Virol. 1992;66:790–803. doi: 10.1128/jvi.66.2.790-803.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sodroski J, Goh W C, Rosen C, Campbell K, Haseltine W A. Role of the HTLV-III/LAV envelope in syncytium formation and cytopathicity. Nature. 1986;322:470–474. doi: 10.1038/322470a0. [DOI] [PubMed] [Google Scholar]
- 28.Sommerfelt M A, Petteway S R, Jr, Dreyer G B, Hunter E. Effect of retroviral proteinase inhibitors on Mason-Pfizer monkey virus maturation and transmembrane glycoprotein cleavage. J Virol. 1992;66:4220–4227. doi: 10.1128/jvi.66.7.4220-4227.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steinhauer D A, Wharton S A, Wiley D C, Skehel J J. Deacylation of the hemagglutinin of influenza A/Aichi/2/68 has no effect on membrane fusion properties. Virology. 1991;184:445–448. doi: 10.1016/0042-6822(91)90867-b. [DOI] [PubMed] [Google Scholar]
- 30.Takeuchi K, Lamb R A. Influenza virus M2 protein ion channel activity stabilizes the native form of fowl plague virus hemagglutinin during intracellular transport. J Virol. 1994;68:911–919. doi: 10.1128/jvi.68.2.911-919.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Veit M, Kretzschmar E, Kuroda K, Garten W, Schmidt M F G, Klenk H-D, Rott R. Site-specific mutagenesis identifies three cysteine residues in the cytoplasmic tail as acylation sites of influenza virus hemagglutinin. J Virol. 1991;65:2491–2500. doi: 10.1128/jvi.65.5.2491-2500.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weissenhorn W, Dessen A, Harrison S C, Skehel J J, Wiley D C. Atomic structure of the ectodomain from HIV-1 gp41. Nature. 1997;387:426–430. doi: 10.1038/387426a0. [DOI] [PubMed] [Google Scholar]
- 33.Wharton S A, Calder L J, Ruigrok R W, Skehel J J, Steinhauer D A, Wiley D C. Electron microscopy of antibody complexes of influenza virus haemagglutinin in the fusion pH conformation. EMBO J. 1995;14:240–246. doi: 10.1002/j.1460-2075.1995.tb06997.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.White J M, Wilson I A. Anti-peptide antibodies detect steps in a protein conformational change: low pH activation of influenza virus hemagglutinin. J Cell Biol. 1987;105:2887–2896. doi: 10.1083/jcb.105.6.2887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wiley D C, Skehel J J. The structure and function of the hemagglutinin membrane glycoprotein of influenza virus. Annu Rev Biochem. 1987;56:365–395. doi: 10.1146/annurev.bi.56.070187.002053. [DOI] [PubMed] [Google Scholar]
- 36.Wilson I A, Skehel J J, Wiley D C. Structure of the haemagglutinin membrane glycoprotein of influenza virus at 3 A resolution. Nature. 1981;182:366–373. doi: 10.1038/289366a0. [DOI] [PubMed] [Google Scholar]
- 37.Yang C, Compans R W. Analysis of the cell fusion activities of chimeric simian immunodeficiency virus-murine leukemia virus envelope proteins: inhibitory effects of the R peptide. J Virol. 1996;70:248–254. doi: 10.1128/jvi.70.1.248-254.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zingler K, Littman D R. Truncation of the cytoplasmic domain of the simian immunodeficiency virus envelope glycoprotein increases Env incorporation into particles and fusogenicity and infectivity. J Virol. 1993;67:2824–2831. doi: 10.1128/jvi.67.5.2824-2831.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zürcher T, Luo G, Palese P. Mutations at palmitylation sites of the influenza virus hemagglutinin affect virus formation. J Virol. 1994;68:5748–5754. doi: 10.1128/jvi.68.9.5748-5754.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]