Abstract
Adsorption and plaque formation of foot-and-mouth disease virus (FMDV) serotype A12 are inhibited by antibodies to the integrin αvβ3 (A. Berinstein et al., J. Virol. 69:2664–2666, 1995). A human cell line, K562, which does not normally express αvβ3 cannot replicate this serotype unless cells are transfected with cDNAs encoding this integrin (K562-αvβ3 cells). In contrast, we found that a tissue culture-propagated FMDV, type O1BFS, was able to replicate in nontransfected K562 cells, and replication was not inhibited by antibodies to the endogenously expressed integrin α5β1. A recent report indicating that cell surface heparan sulfate (HS) was required for efficient infection of type O1 (T. Jackson et al., J. Virol. 70:5282–5287, 1996) led us to examine the role of HS and αvβ3 in FMDV infection. We transfected normal CHO cells, which express HS but not αvβ3, and two HS-deficient CHO cell lines with cDNAs encoding human αvβ3, producing a panel of cells that expressed one or both receptors. In these cells, type A12 replication was dependent on expression of αvβ3, whereas type O1BFS replicated to high titer in normal CHO cells but could not replicate in HS-deficient cells even when they expressed αvβ3. We have also analyzed two genetically engineered variants of type O1Campos, vCRM4, which has greatly reduced virulence in cattle and can bind to heparin-Sepharose columns, and vCRM8, which is highly virulent in cattle and cannot bind to heparin-Sepharose. vCRM4 replicated in wild-type K562 cells and normal, nontransfected CHO (HS+ αvβ3−) cells, whereas vCRM8 replicated only in K562 and CHO cells transfected with αvβ3 cDNAs. A similar result was also obtained in assays using a vCRM4 virus with an engineered RGD→KGE mutation. These results indicate that virulent FMDV utilizes the αvβ3 integrin as a primary receptor for infection and that adaptation of type O1 virus to cell culture results in the ability of the virus to utilize HS as a receptor and a concomitant loss of virulence.
Many viruses initiate infection by attaching to cell surface molecules which are normal components of the plasma membrane. The molecules which viruses use are diverse, and closely related viruses can use different receptors (74, 88). A well-characterized example of the use of multiple receptors by structurally similar viruses can be found in the Picornaviridae. Within this family, the polioviruses (63) and the major group of human rhinoviruses (40, 80, 82) utilize receptors which are members of the immunoglobulin superfamily, while the minor group of human rhinoviruses utilize the low-density lipoprotein receptor (42). Different variants of encephalomyocarditis virus have been reported to use either the immunoglobulin-like molecule vascular cell adhesion molecule 1 (43) or a 70-kDa cell surface sialoglycoprotein (48) as a receptor, and hepatitis A virus (HAV) has recently been shown to use a unique membrane glycoprotein containing immunoglobulin and mucin domains (3, 49). The coxsackie B viruses have been reported to use either decay-accelerating factor (11, 77), a 100-kDa nucleolin-related membrane protein (33, 52), or a 46-kDa membrane-bound immunoglobulin-like protein (9, 24, 83) either as an initial cell binding protein or in combinations that form functional receptor complexes. Interestingly, this 46-kDa protein has also been shown to be a receptor for two members of the human adenovirus family (9, 83), demonstrating that viruses from different families, which do not share common structural features, can use the same receptor. A coxsackie A virus (type A21) appears to require both decay-accelerating factor and intercellular adhesion molecule 1 (ICAM-1) for productive infection (78).
The picornaviruses echoviruses 1, 8, 9, and 22 (12, 13, 68, 91) and coxsackievirus A9 (CAV9) (73) use cell surface integrins as receptors, although it has been suggested that echovirus 9 and CAV9 can also utilize nonintegrin receptors to infect cells (72, 91). Integrins have also been implicated as receptors for rotaviruses (28) and papillomaviruses (36). They have been shown to play a role in the internalization of some human adenoviruses (4, 86) and in the binding and internalization of a number of other nonviral pathogens (45).
Foot-and-mouth disease virus (FMDV) is a member of the aphthovirus genus of the Picornaviridae. The three-dimensional structure of the virus has revealed a prominant surface protrusion made up of a loop between the βG and βH strands of the capsid protein VP1 (G-H loop [1, 59]). This loop contains major immunodominant epitopes of the virion (22) and a highly conserved sequence, arginine-glycine-aspartic acid (RGD), which has been shown to be essential for virus interactions with its cellular receptor, both by RGD peptide inhibition of virus adsorption (7, 38) and by direct mutation or deletion of the sequences encoding these amino acid residues from infectious cDNA clones of FMDV (55, 61, 62). These data, along with the well-characterized interaction of extracellular matrix proteins containing the RGD sequence with integrin receptors (44), suggested that FMDV could use an integrin to attach to cells.
We have previously shown that FMDV type A12 can compete for cellular receptors with CAV9, which bind to the integrin αvβ3 (73), and also demonstrated that antibodies to αvβ3 inhibited binding and plaque formation of type A12 (14). Recently, Jackson et al. (47) reported that FMDV type O1 utilizes cell surface heparan sulfate (HS), a ubiquitous glycosaminoglycan (GAG), as a coreceptor for viral infection. HS has been shown to mediate attachment of several herpesviruses to susceptible cells (65, 67, 79, 89), although a cofactor may be required for viral entry (66). HS has also been suggested to be an attachment molecule for respiratory syncytial virus (53) and has been used as an unnatural target receptor for engineered adenovirus to increase the efficiency of gene delivery (87). We have suggested, however, that binding of FMDV type O viruses to cell surface HS is a consequence of tissue culture adaptation (75).
In this work, we show that cells which are not normally susceptible to FMDV type A12 can be infected with this serotype if they are transfected with cDNAs encoding human αvβ3. In addition, we show that a tissue culture-adapted type O1 virus which is attenuated for disease in cattle replicates in the presence of cell-surface HS, independent of αvβ3 expression. Finally, we show that a type O1-derived virus which is highly virulent in cattle requires the αvβ3 integrin for infection in cell culture. These data indicate that the integrin, rather than HS, is most likely the receptor involved in viral replication and pathogenesis in the livestock host.
MATERIALS AND METHODS
Viruses.
FMDV type A12, strain 119ab, was derived from the infectious cDNA clone pRMC35 (71). The cDNA was derived from virus which had an unknown high-passage history in bovine kidney and BHK-21 cells, and following recovery from transfected BHK-21 cells, the virus used in these studies was passaged at least five times in this cell line. An antigenic variant of type A12, harboring VP1 sequences present in a bovine tongue tissue-propagated type A12 (vRM-SSP), has also been described (69). This virus was initially derived by transfection of cDNA-transcribed RNA into BHK-21 cells (69) and amplified by passage into CHO cells expressing a chimeric single-chain antibody–ICAM-1 receptor (CHO-11.1 [70]). Two variants derived from infectious cDNAs containing capsid sequences represented in a seed stock of type O1Campos have been described elsewhere (75). These viruses are designated vCRM8, a highly cattle-virulent virus which is unable to bind to heparin-Sepharose, and vCRM4, a cattle-avirulent virus which binds to heparin-Sepharose (75). A derivative of vCRM4 virus, vCRM48 (75), with an RGD→KGE mutation in the G-H loop of VP1 (vCRM48-KGE) was derived by site-directed mutation of the vCRM48 cDNA by using methods similar to those used for the derivation of a type A12 KGE mutant (61). Virus derived from BHK-21 cells, transfected with the cDNA-transcribed RNAs of these three viruses, was used to prepare large stocks of virus used in these studies following three or four passages in BHK-21 cells. A tissue culture-propagated type O1BFS from the Animal Virus Research Institute, Pirbright, United Kingdom, was supplied by Fred Brown (Plum Island Animal Disease Center). Prior to coming to Plum Island, the virus was serially passaged 14 times in BHK-21 cells, plaque purified, and passaged once in BHK-21 cells, followed by a single passage in a swine kidney cell line (IBRS2). After arriving at Plum Island, the virus was plaque purified twice followed by at least five serial passages in BHK-21 cells.
Cells.
BHK-21 cells were maintained on minimum essential medium (MEM) containing 10% calf sera and 10% tryptose phosphate broth. The human erythroleukemia cell line K562 transfected with αvβ3 cDNAs (K562-αvβ3) as well as cells transfected with the parental plasmid (K562-pRSV) have been described elsewhere (16, 17). These cells were maintained in RPMI medium containing 10% fetal calf serum (FCS), an additional 2 mM l-glutamine, gentamicin (10 μg/ml), amphotericin B (Fungizone; 12.5 μg/ml), and the neomycin derivative G-418 (1,200 μg/ml; Life Technologies, Gaithersburg, Md.). CHO-K1 cells and the GAG-deficient mutants pgsA-745 (35) and pgsD-677 (57) were cultured in Ham’s F-12 medium supplemented with 10% FCS.
Derivation of CHO cells expressing human αvβ3.
The human αv cDNA subcloned into pcDM8 (Invitrogen, Carlsbad, Calif.) (17) was used as a template for 10 rounds of PCR amplification with specific dUMP-containing human αv primers, and the product was annealed to pAMP1 (Life Technologies). The resulting human αv-encoding cDNA was then subcloned into pcDNA3.1/Zeo(−) (Invitrogen), which contains a Zeocin resistance marker, using the restriction enzymes NotI and EcoRI. The human β3 cDNA cloned into plasmid pIAP58 (58), containing a neomycin resistance marker, has been described elsewhere (17).
CHO-K1 cells and the two GAG-deficient mutant cell lines were cotransfected with αv/pcDNA3.1/Zeo(−) and the β3/pIAP58 clone, using Lipofectin (Life Technologies). Twenty-four hours after transfection, G-418 (600 μg/ml) and Zeocin (500 μg/ml; Invitrogen) were added to the growth medium. Transfected cells expressing human αvβ3 were enriched from the antibiotic-resistant population by a combination of single-cell cloning and fluorescence-activated cell sorting (FACS), using the αvβ3-specific monoclonal antibody (MAb) LM609 (26). Transfectants were sorted based on their fluorescence intensity, and the 10% highest-staining cells were gated, collected under sterile conditions, and expanded in culture. Periodically, cells were reanalyzed by FACS and resorted if the level of cells expressing the integrin had significantly changed.
Viral replication assays.
K-562 cells, at a concentration of 2 × 106 to 3 × 106 cells/ml, were infected with various FMDV serotypes at multiplicities of infection (MOIs) indicated in the figure legends. Virus was allowed to adsorb by rotating the cells at 37°C for 1 h. Cells were then washed with MEM with 1/20 the normal amount of methionine, 25 mM HEPES (pH 7.5), and 0.5% FCS and resuspended to 106 cells/ml in the same medium. One milliliter of cells per well was added to a 12-well tissue culture dish; at various times after infection (as indicated in the figure legends), [35S]methionine (50 to 75 μCi) was added to each well, and the cells were incubated overnight at 37°C. Cells were lysed in 1% Triton X-100, and cell debris was removed by centrifugation in a microcentrifuge for 1 min. Trichloroacetic acid (TCA)-precipitable counts per minute were determined, and radioimmunoprecipitation (RIP) was performed as described previously (5), using a bovine hyperimmune anti-FMDV serum. Equal amounts of TCA-precipitable counts per minute and protein, prepared by the addition of an unlabeled uninfected cell extract, were immunoprecipitated and analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) using a 12% polyacrylamide gel. CHO cells were infected in a similar manner except that they were grown in 24-well tissue culture dishes at a concentration of 1.5 × 105 to 2.0 × 105 cells per well, and viral adsorption was for 2 h.
RESULTS
Replication of FMDV in transfected and nontransfected K562 cells.
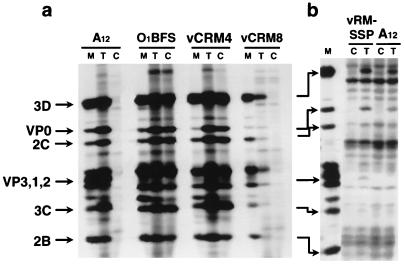
K562-pRSV and K562-αvβ3 cells were infected with A12, O1BFS, vCRM4, and vCRM8 at an MOI of 10 PFU/cell and vRM-SSP at an MOI of 1 PFU/cell. Cells were labeled overnight, and lysates were analyzed by RIP and SDS-PAGE as described in Materials and Methods. The results in Fig. 1a show the presence of viral proteins only in A12- or vCRM8-infected αvβ3-expressing K562 cells, indicating that these two viruses require αvβ3 to initiate infection. In contrast, types O1BFS and vCRM4 were able to infect both K562-pRSV and K562-αvβ3 cells. The results in Fig. 1b show that the vRM-SSP variant, which binds to BHK-21 cells more poorly than the prototype tissue culture-adapted type A12 (69), grew only in cells transfected with αvβ3 cDNAs. These results correlate with those obtained by measuring plaque titer at 24 h after infection of K562 cells by plaque assay in BHK-21 cells (not shown). They also correlate with double-immunofluorescence analysis of infected K562 cells probed with MAb LM609 and a bovine polyclonal anti-FMDV serum (not shown) and confirm our previous findings that antibodies to this integrin inhibit virus adsorption and plaque formation for type A12 (14). In addition, these results indicate that both animal-propagated and tissue culture-adapted type A12 can utilize αvβ3 in cell culture. Furthermore, replication of O1BFS and vCRM4 was not dependent on the presence of this integrin on K562 cells. The only integrin endogenously expressed on the surface of K562 cells is α5β1 (17), which is also dependent on the RGD sequence for ligand binding (44). We were unable to inhibit binding or replication of type O1BFS or vCRM4 in K562 cells with rabbit anti-α5β1 serum (AB1905; 1:10; Chemicon International, Temecula, Calif.), purified rabbit anti-α5 immunoglobulin G (IgG) (AB 1928; 10 μg/ml; Chemicon International), purified anti-β1 MAb P5D2 (20 μg/ml) (17), and purified anti-α5 MAb 16 (20 μg/ml) (17). Taken together, these results suggest that the two tissue culture-adapted type O1 viruses use a nonintegrin receptor to infect K562 cells.
FIG. 1.
Analysis of viral proteins synthesized in FMDV-infected K562 cells transfected with αvβ3 cDNAs. K562-pRSV (C) or K562-αvβ3 (T) cells were infected with type A12, O1BFS, vCRM4, or vCRM8 at an MOI of 10 PFU/cell (a) or type A12 or vRM-SSP at an MOI of 1 PFU/cell (b). Cells were labeled between 3 and 24 h after infection with [35S]methionine, and extracts were analyzed by RIP and SDS-PAGE as described in Materials and Methods. Viral proteins synthesized in infected and labeled BHK-21 cells are included as markers (M), and the positions of major viral proteins are indicated on the left. Type A12 was used as the marker for panel b.
Viral replication in CHO cells transfected with αvβ3 cDNAs and deficient in HS synthesis.
Jackson et al. (47) reported that O1BFS had enhanced binding and infectivity in cells expressing surface HS, by showing that this virus was not able to plaque on mutant CHO cells which were deficient in HS synthesis. We recently showed that O1BFS and vCRM4, but not vCRM8, were able to bind to heparin-Sepharose columns, probably as a result of basic amino acid residues present at the VP2/VP3 interface (75).
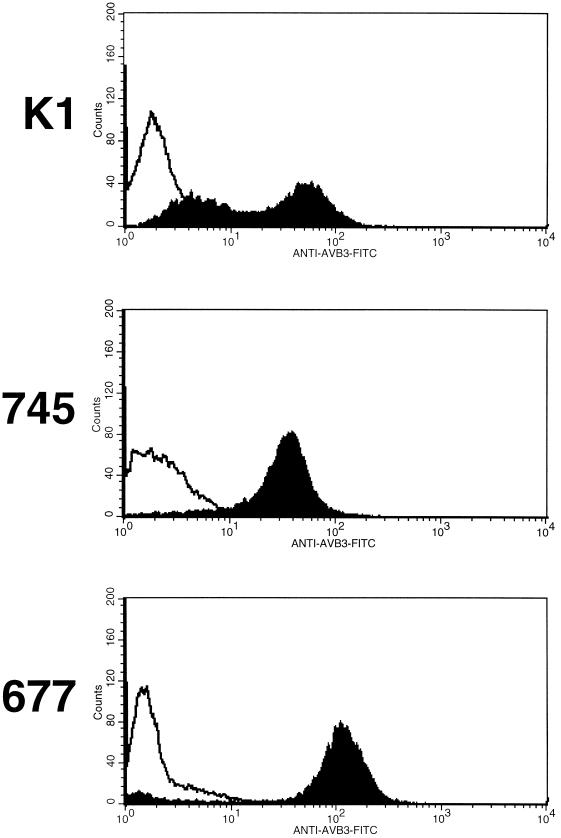
To further examine the relationship between the αvβ3 receptor and cell surface HS, we engineered wild-type and HS-deficient CHO cells to express human αvβ3. The CHO mutant, pgsA-745, synthesizes little, if any, GAG (35), while mutant pgsD-677 is unable to synthesize HS but expresses normal amounts of chondroitin sulfate (57). Figure 2 shows FACS analyses of cells transfected with human αvβ3 cDNAs two to three passages after single-cell cloning and FACS using the αvβ3-specific MAb LM609. These analyses show that after only a few passages, a portion of the wild-type CHO-K1 cells no longer expressed αvβ3, whereas a very high proportion of the transfected pgsA-745 and pgsD-677 cells maintained expression, although the pgsD-677 cells exhibited higher levels of expression than pgsA-745 cells.
FIG. 2.
Analysis of CHO cells transfected with αvβ3 cDNAs. CHO-K1 cells and the two GAG-deficient mutants pgsA-745 and pgsD-677 were transfected with αvβ3 cDNAs and selected as described in Materials and Methods. After two to three passages, transfected and nontransfected cells were incubated with MAb LM609 for 30 min at 4°C in phosphate-buffered saline, washed, and incubated with fluorescein isothiocyanate (FITC)-labeled goat anti-mouse IgG for an additional 30 min at 4°C. After being washed with phosphate-buffered saline, cells were analyzed on a Becton Dickson FACSCaliber analyzer. Nontransfected cells are represented by open curves, and transfected cells are represented by closed curves.
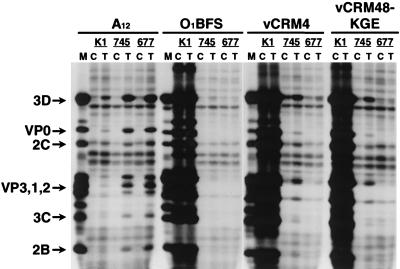
Using this panel of cell lines with defined HS and αvβ3 expression, we tested the abilities of different viruses to utilize these two receptors by analysis of the proteins synthesized in infected cells (Fig. 3). Type A12 was unable to replicate in either wild-type or mutant CHO-K1 cells. When these cells were transfected with αvβ3 cDNAs, however, viral proteins were synthesized, indicating that replication of this virus was dependent on αvβ3 expression. In contrast, both O1BFS and vCRM4 were able to replicate in CHO-K1 cells, regardless of whether they were expressing αvβ3. In both GAG-deficient CHO mutants infected with O1BFS, however, no virus-specific proteins were observed in either control or αvβ3-transfected cells. In the CHO mutants infected with the vCRM4 virus, some viral replication was detected in both control and αvβ3-transfected pgsA-745 cells, although no replication was evident in the pgsD-677 cells (Fig. 3). Since equal amounts of TCA-precipitable counts per minute were used for the immunoprecipitation, comparison of the intensity of the viral proteins in the pgsA-745 cells to the intensity of those present in the CHO-K1 cells indicates that the level of viral replication was low in the mutant cells. FACS analysis of the wild-type and mutant CHO cells with an anti-α5β1 MAb showed that these cells express this integrin to comparable levels on their surface (not shown). To rule out the possibility that vCRM4 used another integrin, we engineered an RGD→KGE mutation in the G-H loop of a derivative virus (vCRM48) [75]). The vCRM48-KGE replicated as well in BHK-21 cells as the virus containing the RGD sequence in the G-H loop (not shown). This contrasted with the inability of a type A12 virus, with similar engineered mutations, to either adsorb to or replicate in BHK-21 cells (61). Infection of CHO cells with vCRM48-KGE resulted in high levels of viral replication in the CHO-K1 control and transfected cells, a much lower level of replication in the pgsA-745 cells, and no replication in the pgsD-677 cells (Fig. 3). These results were indistinguishable from those seen with vCRM4. Treatment of the control and transfected CHO cells with 20 U of heparinase III (47) per ml resulted in an almost total inhibition of viral replication by vCRM4, vCRM48-KGE, and O1BFS, and treatment of vCRM4 with soluble heparin (800 μg/ml) resulted in an almost total inhibition of replication in pgsA-745 cells (not shown). Thus, it appears that the vCRM4 virus and our strain of O1BFS utilize HS, and not an integrin, as their primary receptor. In addition, these results indicate that the pgsA-745 cells may express low levels of HS on their surface, permitting vCRM4 and vCRM48-KGE replication. At this time it is not clear why type O1BFS did not exhibit the low-level replication observed for vCRM4 in the pgsA-745 cells.
FIG. 3.
Analysis of viral proteins synthesized in FMDV-infected CHO cells transfected with αvβ3 cDNAs. Transfected (T) or nontransfected (C) CHO-K1, pgsA-745, or pgsD-677 cells were infected with FMDV type A12, O1BFS, vCRM4, or vCRM48-KGE at an MOI of 10 PFU/cell. Cells were labeled between 3 and 24 h after infection with [35S]methionine, and extracts were analyzed by RIP and SDS-PAGE as described in Materials and Methods. Viral proteins synthesized in infected and labeled BHK-21 cells are included as markers (M), and the positions of major viral proteins are indicated on the left.
When a similar experiment was performed with CHO cells infected with either vCRM8 or vRM-SSP, no viral proteins were observed after 24 h of infection (not shown). Since replication of these viruses in K562 cells was dependent on transfection with αvβ3 cDNAs (Fig. 1), and both viruses grow poorly in BHK-21 cells, we allowed infection of the CHO cell cultures to proceed for another 24 h and labeled the cells between 24 and 48 h after infection. The results in Fig. 4 show that viral proteins were observed only in αvβ3-transfected pgsD-677 cells infected with either virus. The level of viral protein synthesis in the vCRM8-infected pgsD-677-αvβ3 cells was very low, probably reflecting the poor tissue culture adaptation of this virus. With both viruses, however, no replication was evident in either control or transfected CHO-K1 or pgsA-745 cells. This is probably a result of the poor αvβ3 expression in these cells (Fig. 2) coupled with poor viral replication in tissue culture. Interestingly, a similar 24- to 48-h labeling of O1BFS-infected pgsA-745 and pgsD-677 cells failed to show any evidence of viral replication of this virus in the GAG-deficient cells (Fig. 4).
FIG. 4.
Analysis of viral proteins synthesized in FMDV-infected CHO cells transfected with αvβ3 cDNAs. Transfected (T) or nontransfected (C) CHO-K1, pgsA-745, or pgsD-677 cells were infected with FMDV type vCRM8 or O1BFS at an MOI of 10 PFU/cell (a) or vRM-SSP at an MOI of 1 PFU/cell (b). Cells were labeled between 24 and 48 h after infection with [35S]methionine, and extracts were analyzed by RIP and SDS-PAGE as described in Materials and Methods. Viral proteins synthesized in infected and labeled BHK-21 cells are included as markers (M), and the positions of major viral proteins are indicated on the left.
These data from the CHO cell studies confirm those obtained with K562 cells (Fig. 1), showing that both vCRM8 and vRM-SSP utilize αvβ3 as a receptor and can replicate independently of the presence of HS on the cell surface and that replication of O1BFS and vCRM4 is dependent on the presence of HS.
Heparin neutralization of O1Campos variants.
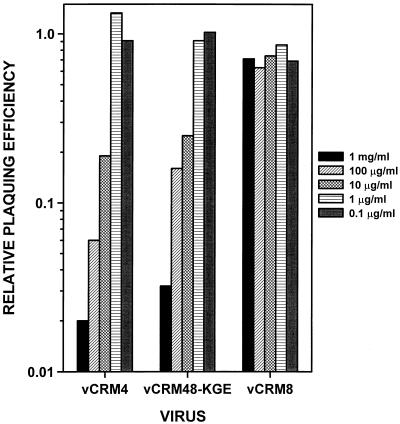
To further delineate the use of HS by vCRM4 and vCRM8, we examined whether soluble heparin was able to neutralize viral infectivity. Decreasing concentrations of heparin were incubated with a fixed number of PFU of either vCRM4, vCRM48-KGE, or vCRM8 and inoculated onto BHK-21 cells. The results in Fig. 5 show that heparin was able to neutralize both vCRM4 and vCRM48-KGE in a dose-dependent manner, indicating that this soluble GAG bound to the viral particles and could prevent viral replication either by direct inhibition of viral adsorption or by viral aggregation. Heparin, however, had no effect on the replication of vCRM8, a result consistent with the ability of this virus to grow on GAG-deficient CHO cells expressing αvβ3.
FIG. 5.
Heparin neutralization of FMDV. Different concentrations of heparin (Sigma) were mixed with 35 to 100 PFU of the indicated viruses in basal medium Eagle with 25 mM HEPES (pH 7.5) and 0.05% bovine serum albumin and incubated for 20 min at room temperature. Aliquots (200 μl) were adsorbed to BHK-21 cells for 1 h at 37°C. The inoculum was aspirated, and the plates overlaid with a mixture of MEM and 0.6% gum tragacanth and incubated at 37°C. Plates were stained with crystal violet-formalin at 48 h (vCRM8) or 72 h (vCRM4 and vCRM48-KGE). Results are expressed as plaque numbers relative to the number of plaques appearing in virus incubated under the same conditions without heparin.
DISCUSSION
Using reciprocal cross-competition binding assays (6, 76), we previously reported that representatives of six serotypes of FMDV use a common, low-copy-number receptor to bind to cells in culture. However these same studies suggested that some serotypes, including type O1, could use alternative receptors which were present in high abundance on cultured cells. Our current experimental approach, using cell types with defined receptors, show that A12 has an absolute requirement for the expression of αvβ3 for the initiation of infection in cell culture, while O1BFS initiates infection following binding to the ubiquitous cell surface molecule HS. These results expand our previous study showing that antibodies to αvβ3 inhibit virus adsorption and plaque formation of type A12 (14) and are consistent with results of a more recent study, suggesting that type O1BFS utilizes HS as a coreceptor (47). However, our studies suggest that tissue culture-propagated O1BFS may be incapable of utilizing the αvβ3 integrin as a receptor to initiate infection and is dependent on HS as its primary receptor in cell culture.
Detailed analysis of cell lines expressing HS in the presence and absence of αvβ3 demonstrated that A12 does not require HS to infect cells and that the use of HS by O1 is exhibited only by viruses that have been propagated extensively in tissue culture. This latter conclusion is based on analyses of two variants of type O1Campos which differ in plaque phenotype, virulence in cattle, and the ability to bind to heparin-Sepharose (75). We have shown that the small-plaque variant (vCRM4), which is avirulent and binds to heparin (75), cannot replicate in HS-deficient cells, even when presented with αvβ3, a result identical to that seen with our tissue culture-propagated strain of O1BFS (Fig. 3). In contrast, the large-plaque variant (vCRM8), which is highly virulent in cattle and cannot bind to heparin (75), replicates only in cells which express αvβ3, independent of the expression of cell-surface HS, a result identical to that seen with type A12 (Fig. 1 and 3). We previously demonstrated that tissue culture growth properties and bovine virulence directly correlated with specific amino acids present at the VP2/VP3 interface of type O1 virus (75). Specifically, we showed that the presence of positively charged residues at positions 134 of VP2 and 56 of VP3 allowed viruses to replicate more efficiently in BHK-21 cells and extended their host range in vitro to CHO cells (75). In contrast, virus present in lesion fluid of infected bovines contained less positively charged residues at either position, could not bind to heparin, and could not infect CHO cells (75). Furthermore, it had also been shown that upon infection of cattle by vCRM4, virus isolated from lesion fluid resembled vCRM8 in plaque phenotype, sequence at the VP2/VP3 interface, and heparin binding (75). The results presented in this report extend the characterization of these variants to their receptor specificities, clearly demonstrating that bovine virulence is inversely related to ability to utilize HS on cells in culture.
To further show that tissue culture adaptation of type O1 results in viruses that do not need to utilize αvβ3 as a receptor, we have engineered a mutation in a vCRM4-related virus. The resulting virus, vCRM48-KGE, adsorbed and replicated as well as the RGD virus in BHK-21 cells (not shown) and replicated in HS-expressing CHO cells (Fig. 3). It was not able to replicate in cells which did not express HS (Fig. 3). This result contrasted with our previous results for mutants within the RGD region of type A12, which were unable to bind or replicate in BHK-21 cells (61) or infect cattle (62). We have also engineered a similar RGD→KGE mutation in the vCRM8 virus, and that mutant was unable to bind or replicate in BHK-21 cells, although an infectious revertant was shown to have a KGD sequence (not shown). The results with the vCRM48-KGE virus are similar to those recently reported for types O1Kaufbeuren (O1K) (55) and type C1 (60). In the case of O1K, an RGD→RGE mutation resulted in the production of infectious virus in BHK-21 cells (55). The cDNA used to engineer the mutation was derived from a virus which underwent at least 10 passages in BHK-21 cells (90), and this virus may have acquired the ability to bind to HS. With type C1, viruses with RGD→RED and RGD→RGG mutations were isolated as MAb escape mutants (60). The virus from which these mutants were isolated, however, was serially passaged 100 times in BHK-21 cells and had acquired three additional mutations to positively charged residues clustered on the surface in VP1 and VP3 that were not related to MAb escape (60). Thus, based on the results presented with our KGE mutant, we believe that the O1K and C1 viruses with RGD mutations use HS as a receptor and bypass the integrin as well.
Taken together, the existing data suggest that type A12 virus adapts to tissue culture by a different mechanism than types O1 and C1. Specifically, type A12 acquires mutations near the RGD sequence, presumably allowing a tighter binding to integrins available on cultured cells (69). We do not know whether the data for type A12 can be extended to other A subtypes, but in preliminary studies, we have not been able to adapt type A24 to use HS as a receptor by serial blind passage in CHO cells (not shown). In the case of type A22, mutations selected during adaptation of virus from monolayer to suspension cultures could alter conformation of the G-H loop. Specifically, the monolayer-adapted virus bound more poorly to tissue culture cells than the suspension-adapted virus (18). In those viruses, there was a single mutation in VP2 lying near the VP1 G-H loop which may alter the favored conformation of the loop (29). Type O1 viruses, however, appear to adapt to cell culture by another mechanism. Structural data comparing a low-passage type O1K virus, a MAb-resistant mutant of this virus, and a high-passage O1BFS isolate showed that the structure of the G-H loop of VP1 was virtually identical for the three viruses and that the main structural differences resided around residue 56 in VP3 (54), which we have previously identified as conferring the vCRM4 and vCRM8 phenotypes (75), including the ability to utilize HS as a receptor. Sequence analysis of the O1BFS virus used in this study also showed that residue 56 in VP3 is an arginine (not shown), as in vCRM4 (75). Assays to measure the adsorption of radioactive O1BFS, vCRM4, and vCRM48-KGE to transfected pgsD-677 cells (8) were unable to detect specific binding due to the low level of adsorption; however, we had shown that unlabeled vCRM4 could inhibit the binding of vCRM8 to BHK-21 cells (75) and that both O1BFS and vCRM4 could inhibit the binding of type A12 to BHK-21 cells (not shown), suggesting that HS-requiring viruses can bind to αvβ3. In addition, it has been recently shown that representatives of six FMDV serotypes, including O1BFS, are able to bind to purified isolated αvβ3 in vitro (46).
Our findings that viruses which have acquired the ability to utilize HS as a receptor are attenuated in bovines suggest that ability to utilize an integrin as a receptor in vivo is critical for production of this disease. With echovirus 9, an insertion in VP1 containing the RGD sequence appears to be critical for virulence of this virus in mice (91). Furthermore, additional positively charged amino acid residues in the envelope glycoprotein of tissue culture-adapted strains of the alphavirus Sindbis virus resulted in a virus which bound to HS and had an attenuated phenotype in mice (51).
It has been previously suggested that the integrin α5β1 might be a receptor for FMDV (2, 25, 85). K562 cells (17) and CHO-K1, pgsA-745, and pgsD-677 cells (not shown) express α5β1 endogenously. Since type A12 viruses expressing bovine-derived and tissue culture-propagated RGD-containing loops, and the bovine-virulent type O1Campos (vCRM8), cannot replicate in these four cell lines in the absence of transfected αvβ3 cDNAs (Fig. 1, 3, and 4), it appears that they cannot utilize α5β1 as a receptor. Although antibodies to α5β1 failed to inhibit replication by O1BFS and vCRM4 (not shown), we cannot rule out that this integrin may be involved in HS-dependent replication of these two viruses. Recently, both subunits of the α5β1 integrin have been shown to contain covalently linked sulfate groups which are part of both HS and chondroitin sulfate, leading to the suggestion that this integrin may be a hybrid proteoglycan (84). It had also been shown that interaction of both the αvβ3 and α5β1 integrins to the core protein of the membrane proteoglycan, perlecan, is partially mediated by the RGD sequence of the protein and modulated by HS (41).
Based on the data showing that αvβ3 is required for tissue culture growth of cattle-virulent viruses, it is interesting to examine the distribution of this integrin in relation to the pathogenesis of foot-and-mouth disease. A number of studies have suggested that lung and pharanyngeal areas are sites of initial viral replication (20, 23, 81), with rapid dissemination of the virus to oral and pedal epithelial areas, possibly mediated by cells of monocyte/macrophage origin (20). Recently, a study was performed with bovines experimentally infected with the prototype tissue culture-adapted type A12 via aerosol (21). By using in situ hybridization, it was shown that within the first 24 h, virus was present in respiratory bronchiolar epithelium, subepithelium, and interstitial areas of the lung. By 72 h, signal was detected in epithelial cells of the tongue, soft palate, feet, tonsils, and tracheobronchial lymph nodes. While, to our knowledge, there are no studies reporting the distribution of αvβ3 within the bovine respiratory tract, this integrin is generally found expressed on vascular endothelium and on smooth muscle cells (19, 37, 56). In the human lung, αvβ3 appears to be restricted to large-vessel endothelium (30) and was not detected in bronchial epithelial cells (64). The integrin is present, however, in multiple salivary gland cells from a number of different species (32). We have performed a preliminary survey for the presence of αvβ3 mRNA by reverse transcription-PCR in tissues susceptible to FMDV removed from bovines at necropsy. These studies showed that mRNA was present in these tissues (not shown), but we have not yet demonstrated protein expression in the relevant cell types. FMDV has been reported to replicate in vitro in bovine keratinocytes (31). We have also detected virus in keratinocytes within lesions in the tongue of infected bovines by electron microscopy (not shown). Human keratinocytes express low levels of αvβ3 along with much higher levels of another related integrin, αvβ5 (50). This latter integrin also appears to be expressed in undifferentiated epithelia derived from the human airway (39). We previously reported that antibodies to the αvβ5 integrin did not inhibit the binding or replication of type A12 (14), and a preliminary experiment suggests that our prototype tissue culture-propagated type A12, vRM-SSP, and vCRM8 cannot replicate in K562 cells transfected with cDNAs of this integrin (not shown).
This study presents another example of how selective pressures applied to an RNA virus quasispecies (34) can select viruses with different receptor specificities for replication in either the natural host or tissue culture. This type of receptor variation in clinical versus laboratory prototype strains has also been shown to occur for the coxsackie B viruses (10). In the case of human immunodeficiency virus type 1, phenotype has been related to differences in the chemokine coreceptors used for virus envelope fusion to target cells (15). It has also been possible to isolate poliovirus mutants which are able to use a mutated poliovirus receptor, and have expanded host range, simply by growing wild-type poliovirus on mutant receptor-expressing cells (27). Thus, in determining the proper types of antiviral intervention, be it either vaccines or non-immune system-based interference, the ability of some viruses to escape by changing the receptors they use for infection should be considered.
ACKNOWLEDGMENTS
We thank Fran Nargi, PIADC, for performing the FACS analysis and sorting of the various transfected CHO cells, and we thank Jeffrey Esko, University of California at San Diego, for providing the wild-type CHO cells and the two HS-deficient mutants used in this study. We also thank Mike LaRocco for excellent technical assistance.
REFERENCES
- 1.Acharya R, Fry E, Stuart D, Fox G, Rowlands D, Brown F. The three-dimensional structure of foot-and-mouth disease virus at 2.9 Å resolution. Nature. 1989;337:709–716. doi: 10.1038/337709a0. [DOI] [PubMed] [Google Scholar]
- 2.Amadori M, Berneri C, Archetti I L. Immunogenicity of foot-and-mouth disease virus grown in BHK-21 suspension cells. Correlation with cell ploidy alterations and abnormal expression of the α5β1 integrin. Vaccine. 1994;12:159–166. doi: 10.1016/0264-410x(94)90055-8. [DOI] [PubMed] [Google Scholar]
- 3.Ashida M, Hamada C. Molecular cloning of the hepatitis A virus receptor from a simian cell line. J Gen Virol. 1997;78:1565–1569. doi: 10.1099/0022-1317-78-7-1565. [DOI] [PubMed] [Google Scholar]
- 4.Bai M, Harfe B, Freimuth P. Mutations that alter an Arg-Gly-Asp (RGD) sequence in the adenovirus type 2 penton base protein abolish its cell-rounding activity and delay virus reproduction in flat cells. J Virol. 1993;67:5198–5205. doi: 10.1128/jvi.67.9.5198-5205.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baxt B. Effect of lysosomotropic compounds on early events in foot-and-mouth disease virus replication. Virus Res. 1987;7:257–271. doi: 10.1016/0168-1702(87)90032-3. [DOI] [PubMed] [Google Scholar]
- 6.Baxt B, Bachrach H L. Early interaction of foot-and-mouth disease virus with cultured cells. Virology. 1980;104:42–55. doi: 10.1016/0042-6822(80)90364-5. [DOI] [PubMed] [Google Scholar]
- 7.Baxt B, Becker Y. The effect of peptides containing the arginine-glycine-aspartic acid sequence on the adsorption of foot-and-mouth disease virus to tissue culture cells. Virus Genes. 1990;4:73–83. doi: 10.1007/BF00308567. [DOI] [PubMed] [Google Scholar]
- 8.Baxt B, Morgan D O, Robertson B H, Timpone C H. Epitopes on foot-and-mouth disease virus outer capsid protein VP1 involved in neutralization and cell attachment. J Virol. 1984;51:298–305. doi: 10.1128/jvi.51.2.298-305.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bergelson J M, Cunningham J A, Droguett G, Kurt-Jones E A, Krithivas A, Hong J S, Horwitz M S, Crowell R L, Finberg R W. Isolation of a common receptor for coxsackie B viruses and adenoviruses 2 and 5. Science. 1997;275:1320–1323. doi: 10.1126/science.275.5304.1320. [DOI] [PubMed] [Google Scholar]
- 10.Bergelson J M, Modlin J F, Wieland-Alter W, Cunningham J A, Crowell R L, Finberg R W. Clinical coxsackievirus B isolates differ from laboratory strains in their interaction with two cell surface receptors. J Infect Dis. 1997;175:697–700. doi: 10.1093/infdis/175.3.697. [DOI] [PubMed] [Google Scholar]
- 11.Bergelson J M, Mohanty J G, Crowell R L, St. John N F, Lublin D M, Finberg R W. Coxsackievirus B3 adapted to growth in RD cells binds to decay-accelerating factor (CD55) J Virol. 1995;69:1903–1906. doi: 10.1128/jvi.69.3.1903-1906.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bergelson J M, Shepley M P, Chan B M C, Hemler M E, Finberg R W. Identification of the integrin VLA-2 as a receptor for echovirus 1. Science. 1992;255:1718–1720. doi: 10.1126/science.1553561. [DOI] [PubMed] [Google Scholar]
- 13.Bergelson J M, St. John N, Kawaguchi S, Chan B M C, Stubdal H, Modlin J, Finberg R W. Infection by echoviruses 1 and 8 depends on the α2 subunit of human VLA-2. J Virol. 1993;67:6847–6852. doi: 10.1128/jvi.67.11.6847-6852.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berinstein A, Roivainen M, Hovi T, Mason P W, Baxt B. Antibodies to the vitronectin receptor (integrin αvβ3) inhibit binding and infection of foot-and-mouth disease virus to cultured cells. J Virol. 1995;69:2664–2666. doi: 10.1128/jvi.69.4.2664-2666.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Björndal Å, Deng H, Jansson M, Fiore J, Colognesi C, Karlsson A, Albert J, Scarlatti G, Littman D R, Fenyö E M. Coreceptor usage of primary human immunodeficiency virus type 1 isolates varies according to biological phenotype. J Virol. 1997;71:7478–7487. doi: 10.1128/jvi.71.10.7478-7487.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blystone S D, Graham I L, Lindberg F P, Brown E J. Integrin αvβ3 differentially regulates adhesive and phagocytic functions of the fibronectin receptor α5β1. J Cell Biol. 1994;127:1129–1137. doi: 10.1083/jcb.127.4.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blystone S D, Lindberg F P, LaFlamme S E, Brown E J. Integrin β3 cytoplasmic tail is necessary and sufficient for regulation of α5β1 phagocytosis by αvβ3 and integrin-associated protein. J Cell Biol. 1995;130:745–754. doi: 10.1083/jcb.130.3.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bolwell C, Brown A L, Barnett P V, Campbell R O, Clarke B E, Parry N R, Ouldridge E J, Brown F, Rowlands D J. Host cell selection of antigenic variants of foot-and-mouth disease virus. J Gen Virol. 1989;70:45–57. doi: 10.1099/0022-1317-70-1-45. [DOI] [PubMed] [Google Scholar]
- 19.Brooks P C, Clark R A F, Cherish D A. Requirement of vascular integrin αvβ3 for angiogenesis. Science. 1994;264:569–571. doi: 10.1126/science.7512751. [DOI] [PubMed] [Google Scholar]
- 20.Brown C C, Meyer R F, Olander H J, House C, Mebus C A. A pathogenesis study of foot-and-mouth disease in cattle using in situ hybridization. Can J Vet Res. 1992;56:189–193. [PMC free article] [PubMed] [Google Scholar]
- 21.Brown C C, Piccone M E, Mason P W, McKenna T S-C, Grubman M J. Pathogenesis of wild-type and leaderless foot-and-mouth disease virus in cattle. J Virol. 1997;70:5638–5641. doi: 10.1128/jvi.70.8.5638-5641.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown F. Antibody recognition and neutralization of foot-and-mouth disease virus. Semin Virol. 1995;6:243–248. [Google Scholar]
- 23.Burrows R, Mann J A, Garland J M, Greig A, Goodridge D. The pathogenesis of natural and simulated natural foot-and-mouth disease infection cattle. J Comp Pathol. 1981;91:599–609. doi: 10.1016/0021-9975(81)90089-x. [DOI] [PubMed] [Google Scholar]
- 24.Carson S D, Chapman N N, Tracy S M. Purification of the putative coxsackievirus B receptor from HeLa cells. Biochem Biophys Res Commun. 1997;233:325–328. doi: 10.1006/bbrc.1997.6449. [DOI] [PubMed] [Google Scholar]
- 25.Chambers M, Dougan G, Newman J, Brown F, Crowther J, Mould A P, Humphries M J, Francis M J, Clarke B, Brown A L, Rowlands D. Chimeric hepatitis B virus core particles as probes for studying peptide-integrin interactions. J Virol. 1996;70:4045–4052. doi: 10.1128/jvi.70.6.4045-4052.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheresh D. Human endothelial cells synthesize and express an arg-gly-asp-directed adhesion receptor involved in attachment to fibrinogen and von Willebrand factor. Proc Natl Acad Sci USA. 1987;84:6471–6475. doi: 10.1073/pnas.84.18.6471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colston E M, Racaniello V R. Poliovirus variants selected on mutant receptor-expressing cells identify capsid residues that expand receptor recognition. J Virol. 1995;69:4823–4829. doi: 10.1128/jvi.69.8.4823-4829.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coulson B, Londrigan S L, Lee D J. Rotavirus contains integrin ligand sequences and a disintegrin-like domain that are implicated in virus entry into cells. Proc Natl Acad Sci USA. 1997;94:5389–5394. doi: 10.1073/pnas.94.10.5389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Curry S, Fry E, Blakemore W, Abu-Ghazaleh R, Jackson T, King A, Lea S, Newman J, Rowlands D, Stuart D. Perturbations in the surface structure of A22 Iraq foot-and-mouth disease virus accompanying coupled changes in host cell specificity and antigenicity. Structure. 1996;4:135–145. doi: 10.1016/s0969-2126(96)00017-2. [DOI] [PubMed] [Google Scholar]
- 30.Damjanovich L, Albelda S M, Mette S A, Buck C A. Distribution of integrin cell adhesion receptors in normal and malignant lung tissue. Am J Respir Cell Mol Biol. 1992;6:197–206. doi: 10.1165/ajrcmb/6.2.197. [DOI] [PubMed] [Google Scholar]
- 31.David D, Stram Y, Yadin H, Trainin Z, Becker Y. Foot-and-mouth disease virus replication in bovine skin langerhans cells under in vitro conditions detected by RT-PCR. Virus Genes. 1995;10:5–13. doi: 10.1007/BF01724292. [DOI] [PubMed] [Google Scholar]
- 32.Delporte C, Redman R S, Baum B J. Relationship between the cellular distribution of the αvβ3/5 integrins and adenoviral infection in salivary glands. Lab Invest. 1997;77:167–173. [PubMed] [Google Scholar]
- 33.De Verdugo U R, Selinka H-C, Huber M, Kramer B, Kellerman J, Hofschneider P H, Kandolf R. Characterization of a 100-kilodalton binding protein for the six serotypes of coxsackie B viruses. J Virol. 1995;69:6751–6757. doi: 10.1128/jvi.69.11.6751-6757.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Domingo E, Mateu M G, Escarmis C, Martinez-Salas E, Andreu D, Giralt E, Verdaguer N, Fita I. Molecular evolution of aphthoviruses. Virus Genes. 1996;11:197–207. doi: 10.1007/BF01728659. [DOI] [PubMed] [Google Scholar]
- 35.Esko J D, Stewart T E, Taylor W H. Animal cell mutants defective in glycosaminoglycan biosynthesis. Proc Natl Acad Sci USA. 1985;82:3197–3201. doi: 10.1073/pnas.82.10.3197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Evander M, Frazer I H, Payne E, Qi Y M, Hengst K, McMillan N A. Identification of the α6 integrin as a candidate receptor for papillomaviruses. J Virol. 1997;71:2449–2456. doi: 10.1128/jvi.71.3.2449-2456.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Felding-Haberman B, Cheresh D A. Vitronectin and its receptors. Curr Opin Cell Biol. 1993;5:864–868. doi: 10.1016/0955-0674(93)90036-p. [DOI] [PubMed] [Google Scholar]
- 38.Fox G, Parry N R, Barnett P V, McGinn B, Rowlands D, Brown F. The cell attachment site on foot-and-mouth disease virus includes the amino acid sequence RGD (arginine-glycine-aspartic acid) J Gen Virol. 1989;70:625–637. doi: 10.1099/0022-1317-70-3-625. [DOI] [PubMed] [Google Scholar]
- 39.Goldman M J, Wilson J M. Expression of αvβ5 integrin is necessary for efficient adenovirus-mediated gene transfer in the human airway. J Virol. 1995;69:5951–5958. doi: 10.1128/jvi.69.10.5951-5958.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Greve J M, Davis G, Meyer A M, Forte C P, Yost S C, Marlor C W, Kamarck M E, McClelland A. The major human rhinovirus receptor is ICAM-1. Cell. 1989;56:839–847. doi: 10.1016/0092-8674(89)90688-0. [DOI] [PubMed] [Google Scholar]
- 41.Hayashi K, Madri J A, Yurchenco P D. Endothelial cells interact with the core protein of basement membrane perlecan through β1 and β3 integrins: an adhesion modulated by glycosaminoglycans. J Cell Biol. 1992;119:945–959. doi: 10.1083/jcb.119.4.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hoefer F, Gruenberger M, Kowalski H, Marchat H, Heuttinger M, Kuechler E, Blass D. Members of the low density lipoprotein receptor family mediate cell entry of amino-group common cold virus. Proc Natl Acad Sci USA. 1994;91:1839–1842. doi: 10.1073/pnas.91.5.1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huber S A. VCAM-1 is a receptor for encephalomyocarditis virus on murine vascular endothelial cells. J Virol. 1994;68:3453–3458. doi: 10.1128/jvi.68.6.3453-3458.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hynes R O. Integrins: versatility, modulation, and signaling in cell adhesion. Cell. 1992;69:11–25. doi: 10.1016/0092-8674(92)90115-s. [DOI] [PubMed] [Google Scholar]
- 45.Isberg R R, Nhieu G T V. Binding and internalization of microorganisms by integrin receptors. Trends Microbiol. 1994;2:10–19. doi: 10.1016/0966-842x(94)90338-7. [DOI] [PubMed] [Google Scholar]
- 46.Jackson T, Sharma A, Abu Ghazaleh R, Blakemore W E, Ellard F M, Simmons D L, Newman J W I, Stuart D I, King A M Q. Arginine-glycine-aspartic acid-specific binding by foot-and-mouth disease viruses to the purified integrin αvβ3in vitro. J Virol. 1997;71:8357–8361. doi: 10.1128/jvi.71.11.8357-8361.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jackson T, Ellard F M, Abu Ghazaleh R, Brooks S M, Blakemore W E, Corteyn A H, Stuart D I, Newman J W I, King A M Q. Efficient infection of cells in culture by type O foot-and-mouth disease virus requires binding to cell surface heparan sulfate. J Virol. 1996;70:5282–5287. doi: 10.1128/jvi.70.8.5282-5287.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jin Y-M, Pardoe I U, Burness A T H, Michalak T I. Identification and characterization of the cell surface 70-kilodalton sialoglycoprotein(s) as a candidate receptor for encephalomyocarditis virus on human nucleated cells. J Virol. 1994;68:7308–7319. doi: 10.1128/jvi.68.11.7308-7319.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kaplan G, Totsuck A, Thompson P, Akatsuda T, Moritsugu Y, Feinstone S M. Identification of a surface glycoprotein on African green monkey kidney cells as a receptor for hepatitis A virus. EMBO J. 1996;15:4282–4296. [PMC free article] [PubMed] [Google Scholar]
- 50.Kim J P, Zhang K, Chen J D, Kramer R H, Woodley D T. Vitronectin-driven human keratinocyte locomotion is mediated by the αvβ5 integrin receptor. J Biol Chem. 1994;269:26926–26932. [PubMed] [Google Scholar]
- 51.Klimstra, W., and R. Johnston. Personal communication.
- 52.Kramer B, Huber M, Kern C, Klingel K, Kandolf R, Selinka H-C. Chinese hamster ovary cells are non-permissive towards infection with coxsackievirus B3 despite functional virus-receptor interactions. Virus Res. 1997;48:149–156. doi: 10.1016/s0168-1702(96)01438-4. [DOI] [PubMed] [Google Scholar]
- 53.Krusat T, Streckert H-J. Heparin-dependent attachment of respiratory syncytial virus (RSV) to host cells. Arch Virol. 1997;142:1247–1254. doi: 10.1007/s007050050156. [DOI] [PubMed] [Google Scholar]
- 54.Lea S, Abu-Ghazaleh R, Blakemore W, Curry S, Fry E, Jackson T, King A, Logan D, Newman J, Stuart D. Structural comparison of two strains of foot-and-mouth disease virus subtype O1 and a laboratory antigenic variant, G67. Structure. 1995;3:571–580. doi: 10.1016/s0969-2126(01)00191-5. [DOI] [PubMed] [Google Scholar]
- 55.Leippert M, Beck E, Weiland F, Pfaff E. Point mutations within the βG-βH loop of foot-and-mouth disease virus O1K affect virus attachment to target cells. J Virol. 1997;71:1046–1051. doi: 10.1128/jvi.71.2.1046-1051.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liaw L, Skinner M P, Raines E W, Ross R, Cherish D A, Schwartz S M, Giachelli C M. The adhesive and migratory effects of osteopontin are mediated via distinct cell surface integrins. Role of αvβ3 in smooth muscle cell migration to osteopontin in vitro. J Clin Invest. 1995;95:713–724. doi: 10.1172/JCI117718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lidholt K, Weinke J L, Kiser C S, Lugemwa F L, Bame K J, Cheifetz S, Massagué J, Lindahl U, Esko J D. A single mutation affects both N-acetylglucosaminyltransferase and glucuronosyltransferase activities in a Chinese hamster ovary cell mutant defective in heparan sulfate biosynthesis. Proc Natl Acad Sci USA. 1992;89:2267–2271. doi: 10.1073/pnas.89.6.2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lindberg F P, Gresham H D, Schwarz E, Brown E J. Molecular cloning of integrin-associated protein: an immunoglobulin family member with multiple membrane-spanning domains implicated in αvβ3-dependent ligand binding. J Cell Biol. 1993;123:485–496. doi: 10.1083/jcb.123.2.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Logan D, Abu-Ghazaleh R, Blakemore W, Curry S, Jackson T, King A, Lea S, Lewis R, Newman J, Parry N, Rowlands D, Stuart D, Fry E. Structure of a major immunogenic site on foot-and-mouth disease virus. Nature. 1993;362:566–568. doi: 10.1038/362566a0. [DOI] [PubMed] [Google Scholar]
- 60.Martínez M, Verdaguer N, Mateu M G, Domingo E. Evolution subverting essentiality: dispensability of the cell attachment arg-gly-asp motif in multiply passaged foot-and-mouth disease virus. Proc Natl Acad Sci USA. 1997;94:6798–6802. doi: 10.1073/pnas.94.13.6798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mason P W, Rieder E, Baxt B. RGD sequence of foot-and-mouth disease virus is essential for infecting cells via the natural receptor but can be bypassed by an antibody-dependent enhancement mechanism. Proc Natl Acad Sci USA. 1994;91:1932–1936. doi: 10.1073/pnas.91.5.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McKenna T St C, Lubroth J, Rieder E, Baxt B, Mason P W. Receptor binding site-deleted foot-and-mouth disease (FMD) virus protects cattle from FMD. J Virol. 1995;69:5787–5790. doi: 10.1128/jvi.69.9.5787-5790.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mendelsohn C L, Wimmer E, Racaniello V. Cellular receptor for poliovirus: molecular cloning, nucleotide sequence, and expression of a new member of the immunoglobulin superfamily. Cell. 1989;56:855–865. doi: 10.1016/0092-8674(89)90690-9. [DOI] [PubMed] [Google Scholar]
- 64.Mette S A, Pilewski J, Buck C A, Albelda S M. Distribution of integrin cell adhesion receptors on normal bronchial epithelial cells and lung cancer cells in vitro and in vivo. Am J Respir Cell Mol Biol. 1993;8:562–572. doi: 10.1165/ajrcmb/8.5.562. [DOI] [PubMed] [Google Scholar]
- 65.Mettenleiter T C, Zsak L, Zuckermann F, Sugg N, Kern H, Ben-Porat T. Interaction of glycoprotein gIII with a cellular heparinlike substance mediates adsorption of pseudorabies virus. J Virol. 1990;64:278–286. doi: 10.1128/jvi.64.1.278-286.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Montgomery R I, Warner M S, Lum B J, Spear P G. Herpes simplex virus-1 entry into cells mediated by a novel member of the TNF/NGF receptor family. Cell. 1996;87:427–436. doi: 10.1016/s0092-8674(00)81363-x. [DOI] [PubMed] [Google Scholar]
- 67.Okazaki K, Mitsuzaki T, Sugahara Y, Okada J, Hasebe M, Iwamura Y, Ohnishi M, Kanno T, Shimizu M, Honda E, Kono Y. BHV-1 adsorption is mediated by the interaction of glycoprotein gIII with heparin-like moiety on the cell surface. Virology. 1991;181:666–670. doi: 10.1016/0042-6822(91)90900-v. [DOI] [PubMed] [Google Scholar]
- 68.Pulli T, Koivunen E, Hyypiä T. Cell-surface interaction of echovirus 22. J Biol Chem. 1997;272:21176–21180. doi: 10.1074/jbc.272.34.21176. [DOI] [PubMed] [Google Scholar]
- 69.Rieder E, Baxt B, Mason P W. Animal derived antigenic variants of foot-and-mouth disease virus type A12 have low affinity for cells in culture. J Virol. 1994;68:5296–5299. doi: 10.1128/jvi.68.8.5296-5299.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rieder E, Berinstein A, Baxt B, Kang A, Mason P W. Propagation of an attenuated virus by design: engineering a novel receptor for a noninfectious foot-and-mouth disease virus. Proc Natl Acad Sci USA. 1996;93:10428–10433. doi: 10.1073/pnas.93.19.10428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rieder E, Bunch T, Brown F, Mason P W. Genetically engineered foot-and-mouth disease viruses with poly(C) tracts of two nucleotides are virulent in mice. J Virol. 1993;67:5139–5145. doi: 10.1128/jvi.67.9.5139-5145.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Roivainen M, Piiraninen L, Hovi T. Efficient RGD-independent entry process of coxsackievirus A9. Arch Virol. 1996;141:1909–1919. doi: 10.1007/BF01718203. [DOI] [PubMed] [Google Scholar]
- 73.Roivainen M, Piirainen L, Hovi T, Virtanen I, Riikonen T, Heino J, Hyypiä T. Entry of coxsackievirus A9 into host cells: specific interaction with αvβ3 integrin, the vitronectin receptor. Virology. 1994;203:357–365. doi: 10.1006/viro.1994.1494. [DOI] [PubMed] [Google Scholar]
- 74.Rossmann M G. Viral cell recognition and entry. Protein Sci. 1994;3:1712–1725. doi: 10.1002/pro.5560031010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sa-Carvalho D, Rieder E, Baxt B, Rodarte R, Tanuri A, Mason P W. Tissue culture adaptation of foot-and-mouth disease virus selects viruses that bind to heparin and are attenuated in cattle. J Virol. 1997;71:5115–5123. doi: 10.1128/jvi.71.7.5115-5123.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sekiguchi K, Franke A J, Baxt B. Competition for cellular receptor sites among selected aphthoviruses. Arch Virol. 1982;74:53–64. doi: 10.1007/BF01320782. [DOI] [PubMed] [Google Scholar]
- 77.Shafren D R, Bates R C, Agrez M V, Herd R L, Burns G F, Barry R D. Coxsackieviruses B1, B3, and B5 use decay-accelerating factor as a receptor for cell attachment. J Virol. 1995;69:3873–3877. doi: 10.1128/jvi.69.6.3873-3877.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shafren D R, Dorahy D J, Ingham R A, Burns G F, Barry R D. Coxsackievirus A21 binds to decay-accelerating factor but requires intercellular adhesion molecule 1 for cell entry. J Virol. 1997;71:4736–4743. doi: 10.1128/jvi.71.6.4736-4743.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shieh M-T, WuDunn D, Montgomery R I, Esko J D, Spear P. Cell surface receptors for herpes simplex virus are heparan sulfate proteoglycans. J Cell Biol. 1992;116:1273–1281. doi: 10.1083/jcb.116.5.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Staunton D E, Merluzzi V J, Rothlein R, Barton R, Marlin S D, Springer T A. A cell adhesion molecule, ICAM-1, is the major surface receptor for rhinoviruses. Cell. 1989;56:849–853. doi: 10.1016/0092-8674(89)90689-2. [DOI] [PubMed] [Google Scholar]
- 81.Sutmoller P, McVicar J. Pathogenesis of foot-and-mouth disease: the lung as an additional portal of entry of the virus. J Hyg (Cambridge) 1976;77:235–243. doi: 10.1017/s0022172400024669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tomassini J E, Graham D, DeWitt C M, Lineberger D W, Rodkey J A, Colonno R J. cDNA cloning reveals that the major group rhinovirus receptor on HeLa cells is intercellular adhesion molecule 1. Proc Natl Acad Sci USA. 1989;86:4907–4911. doi: 10.1073/pnas.86.13.4907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tomko R P, Xu R, Philipson L. HCAR and MCAR: the human and mouse cellular receptors for subgroup C adenoviruses and group B coxsackieviruses. Proc Natl Acad Sci USA. 1997;94:3352–3356. doi: 10.1073/pnas.94.7.3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Veiga S S, Carolina M, Elias Q B, Gremski W, Porcionatto M A, da Silva R, Nader H B, Brentani R R. Post-translational modifications of the α5β1 integrin by glycosaminoglycan chains. The α5β1 integrin as a facultative proteoglycan. J Biol Chem. 1997;272:12529–12535. doi: 10.1074/jbc.272.19.12529. [DOI] [PubMed] [Google Scholar]
- 85.Villaverde A, Feliu J X, Harbottle R P, Benito A, Coutelle C. A recombinant arginine-glycine-aspartic acid (RGD) motif from foot-and-mouth disease virus binds mammalian cells through vitronectin and to a lower extent, fibronectin receptors. Gene. 1996;180:101–106. doi: 10.1016/s0378-1119(96)00413-1. [DOI] [PubMed] [Google Scholar]
- 86.Wickham T J, Mathias P, Cheresh D A, Nemerow G R. Integrins αvβ3 and αvβ5 promote adenovirus internalization but not virus attachment. Cell. 1993;73:309–319. doi: 10.1016/0092-8674(93)90231-e. [DOI] [PubMed] [Google Scholar]
- 87.Wickham T J, Roelvink P W, Brough D E, Kovesdi I. Adenovirus targeted to heparan-containing receptors increases its gene delivery efficiency to multiple cell types. Nat Biotechnol. 1996;14:1570–1573. doi: 10.1038/nbt1196-1570. [DOI] [PubMed] [Google Scholar]
- 88.Wimmer E. Introduction. In: Wimmer E, editor. Cellular receptors for animal viruses. Plainview, N.Y: Cold Spring Harbor Laboratory Press; 1994. pp. 1–13. [Google Scholar]
- 89.WuDunn D, Spear P G. Initial interaction of herpes simplex virus with cells is binding to heparan sulfate. J Virol. 1989;63:52–58. doi: 10.1128/jvi.63.1.52-58.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zibert A, Maas G, Strebel K, Falk M, Beck E. Infectious foot-and-mouth disease virus derived from a cloned full-length cDNA. J Virol. 1990;64:2467–2473. doi: 10.1128/jvi.64.6.2467-2473.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zimmerman H, Eggers H J, Nelsen-Salz B. Cell attachment and mouse virulence of echovirus 9 correlate with an RGD motif in the capsid protein VP1. Virology. 1997;233:149–156. doi: 10.1006/viro.1997.8601. [DOI] [PubMed] [Google Scholar]