Abstract
A 52-year-old male patient presented with complaints of abdominal and back pain. CT revealed a deep pelvic abscess extending into the anterior sacral space. Since puncture via the conventional transgluteal approach cannot reach a deep abscess, percutaneous pelvic abscess drainage was performed under CT fluoroscopy using the cranio-caudal puncture technique. The cranio-caudal puncture requires needle insertion perpendicular to the CT cross-section. This method advances the CT gantry deeper than the needle tip and follows the CT cross-section with the needle tip. This series of images and movements continues until the needle reaches the target. The procedure was successful without complications, the abscess was reduced in size, and blood test data improved. The cranio-caudal puncture technique provides an alternative for the drainage of deep pelvic abscesses that avoids the complications associated with gluteal muscle puncture. Percutaneous drainage of pelvic abscesses under CT fluoroscopy-guided cranio-caudal puncture offers a safe option as a puncture route for deep pelvic abscesses.
Keywords: Percutaneous drainage, Pelvic abscess, Cranio-caudal approach, Axial puncture, CT fluoroscopy
Introduction
Pelvic abscesses following gastrointestinal perforation or pelvic surgery are often difficult to control with antibiotic monotherapy and may require additional percutaneous drainage. Deep pelvic abscesses are particularly difficult to treat by open surgery due to the invasiveness of treatment, so minimally invasive image-guided drainage has an important role to play in the management of this pathology [1].
Percutaneous drainage of a pelvic abscess generally uses a puncture route via the gluteal muscles and foramen sciaticum due to the difficulty of achieving successful puncture via the anterior abdomen [2]. Although this is a relatively safe and well-established technique, disadvantages include limited postprocedure movement, spontaneous withdrawal, and the risk of complications such as intramuscular abscess and hematoma due to the route penetrating the muscles [3,4]. In addition, the puncture route is often restricted to avoid damage to the sciatic nerve or gluteal arteries.
Recent developments in imaging modalities have provided various options for approach routes in percutaneous puncture. The cranio-caudal (C-C) puncture technique involves puncture along the body axis under US or X-ray fluoroscopy. Previous reports have described C-C puncture as a useful option for puncturing fluid collection in the lung apex [5,6].
We report herein a case of deep pelvic abscess extending to the anterior sacral space successfully treated by percutaneous drainage of a pelvic abscess via a perineal approach using C-C puncture under CT fluoroscopy.
Case presentation
The patient, a 52-year-old man, presented to our emergency department with chief complaints of left-sided abdominal pain and back pain. Blood testing on admission suggested a marked inflammatory reaction and signs of infection: white blood cell count, 36.0 ×103/μL; C-reactive protein, 30.23 mg/dL; and procalcitonin, 40.4 ng/mL. In addition, creatinine was 17.07 mg/dL and urea nitrogen were 185 mg/dL, indicating severe acute kidney failure. Contrast-enhanced CT revealed a left perirenal and retroperitoneal abscess caused by perforation of a sigmoid colon diverticulum. Both antibiotic therapy and drainage of the left perirenal abscess were started on the day of admission. However, the abscess extended to the anterior sacral space (Fig. 1A). Another percutaneous drainage was requested. The cranial side of the abscess extended to the level of the superior border of the sacrum (Fig. 1B), and placement of a drainage tube in this lesion was required to control the abscess. Since the main abscess was at the level of the superior border of the sacrum, the conventional transgluteal approach was predicted to be ineffective for drainage on the cranial side. We decided to insert a drainage tube in a straight line into the deep abscess in the anterior sacral space from the caudal side by C-C puncture. Fig. 2 shows an example image of the start of the puncture using a phantom. First, non-contrast CT was performed. CT images revealed that the gluteal skin surface, caudal side of the abscess, and cranial side of the deep abscess in the anterior space were in a straight line, in a direction coaxial with the body axis, without any obstructions. A pointer was then placed on this straight line on the monitor (Figs. 3 A-C) and the fluoroscopic cross-section was moved to the intersection with the skin surface to serve as a landmark for the puncture starting point (Fig. 3C; step [i]). Under local anesthesia, puncture was initiated in a direction coaxial with the body axis (i.e., advancing in the direction of the CT gantry). At this time, the puncture point was confirmed by referring to the positioning light of the assumed cross-section on the CT image before puncture (Figs. 2 and 3F; step [ii]). The CT fluoroscopic section was moved deep to the tip of the needle (Fig. 3B; step [iii]), then the needle was advanced until the puncture needle reappeared on the CT fluoroscopic section (Fig. 3E; step [iv]). By repeating this procedure and advancing the needle in a stepwise manner (step [v] and [vi]), the needle was advanced along the originally envisioned trajectory and finally reached the abscess (Fig. 3D). The drainage catheter was advanced from the perineum to the head of the abscess via the C-C puncture route without involving the gluteal muscles (Fig. 4A and B). No complications were noted upon placement of the drainage catheter. The abscess shrank, WBC count improved to 4.8 × 103/μL and CRP fell to 1.90 mg/dL. During drainage, no problems such as poor drainage or tube dislodgement were encountered and the tube was removed after 15 days.
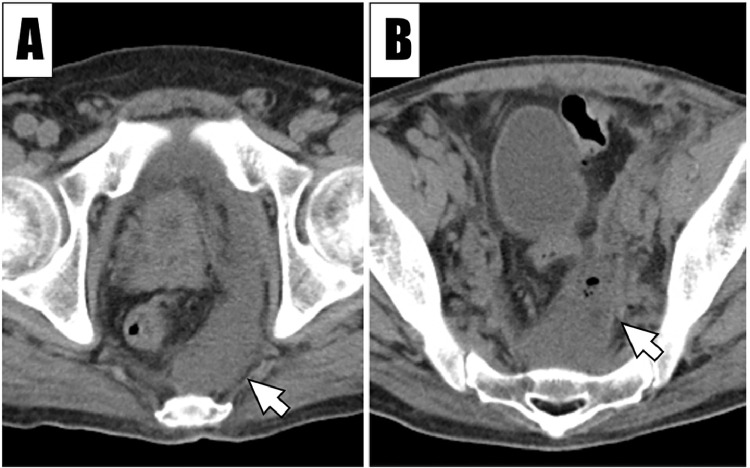
Fig. 1.
Preoperative CT of the pelvic abscess. Preoperative CT shows an abscess in the presacral space (A, arrow), with the upper edge extending to the level of the sacral superior border (B, arrow). This area is surrounded by pelvic bones (B), making a transgluteal approach difficult.
Fig. 2.
A representation of the start of the puncture using a phantom. The puncture is started at the point where the skin surface intersects the puncture line assumed from CT performed before the puncture. The positioning light helps confirm the starting point for the puncture.
Fig. 3.
Procedures for C-C punctures. The methods proceeds chronologically from ⅰ) to ⅵ). i) Place the cursor in the abscess cavity on the CT monitor during the positioning phase of (A-C). Scroll down the slice to the surface of caudal skin plane with the arrow-shaped cursor in place. Ensure that there are no structures to be avoided in the area through which the arrow-shaped cursor passes. ii) Start the puncture using the arrow-shaped cursor position in (C) as a landmark. The high-density point drawn at the intersection of the 2 white dashed lines in (F) is the puncture needle. The image in (F) is a cross-section at the same level as in (C). iii) Shift the fluoroscopic slice in the head direction (B) and check again that there is no obstruction. iv) Advance the needle until the puncture needle appears on the fluoroscopic plane. The puncture needle is the dense dot drawn at the intersection of the 2 white dashed lines in (E). The image in (B) is a cross-section at the same level as (E). Similarly, by repeatedly rechecking the slightly cephalic section (v) and inserting the needle, the needle finally reaches the abscess cavity (vi).
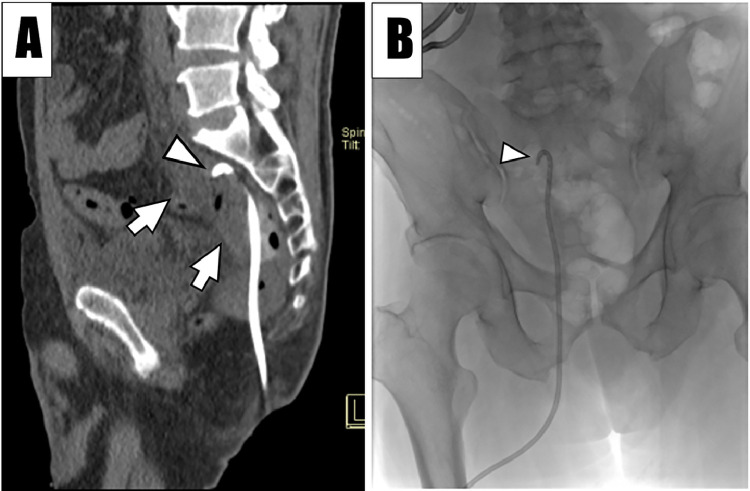
Fig. 4.
CT and radiographic images after placement of the drainage tube. A drainage tube is placed via a caudal approach using C-C puncture. The tip (A, arrowhead; B arrowhead) is successfully inserted near the upper border of the sacrum within the abscess (A, arrows).
Discussion
We have reported a case of successful percutaneous pelvic abscess drainage under CT-fluoroscopy-guided C-C puncture. We consider this technique as a useful alternative for the drainage of deep pelvic abscesses.
Pelvic abscesses sometimes respond poorly to medical treatment with antibiotic monotherapy and are potentially life-threatening [1]. Drainage of pelvic abscesses through the gluteal muscles has been reported to provide good results as a treatment that avoids surgical salvage treatment [2,3]. Minimally invasive percutaneous drainage is a relatively safe and well-established technique [1,2]. However, puncture via the gluteal muscles has been reported to cause pseudoaneurysm of a small branch of the inferior gluteal artery and sciatic nerve injury [3]. Puncture via the pisiform muscle has been associated with a particularly high frequency of sciatic nerve injury [7]. A previous case series showed that drainage tube placement via the gluteal muscles risked the spread of abscesses or the formation of hematomas within the gluteal muscles [4].
Drainage by puncture coaxial to the body axis was first reported by Takizawa et al. as the “axial puncture approach” for the treatment of fluid collections in the pulmonary apex [5]. In that report, the puncture route was also confirmed by scrolling through image slices using the cursor on the CT monitor as a landmark. On the other hand, puncture was performed under X-ray fluoroscopic guidance. A retrospective cohort study of the same technique was later reported as the “craniocaudal approach” [6]. That second report used US and X-ray fluoroscopy for drainage and biopsy cases. In our case, we applied this technique to percutaneous pelvic abscess drainage under CT fluoroscopic guidance. This CT fluoroscopic technique was considered safe and reliable for puncturing lesions.
In our case, CT fluoroscopic-guided C-C puncture approached the deep pelvic abscess in a straight line and prevented complications from puncture of the gluteal muscles. Another advantage of this technique is that it can be performed by operators inexperienced in CT fluoroscopy-guided procedures, regardless of their level of ability, because the puncture is performed in a straight line along a predetermined route, eliminating the need for adjusting the direction of puncture. Occasionally, cases are encountered in which a straight puncture route coaxial to the body axis cannot be applied or in which a slightly oblique puncture is required. Even in such cases, this technique might be applicable by placing the patient at a slight angle to the gantry direction or in a head-up or head-down position.
Conclusion
Percutaneous drainage of pelvic abscesses with CT fluoroscopic-guided C-C puncture can be performed safely and appears to represent a helpful option, particularly when selecting a puncture route for deep pelvic abscesses.
Patient consent
Written informed consent for publication of this case was obtained from the patient.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Duszak RL, Levy JM, Akins EW, Bakal CW, Denny DD, Martin LG, et al. Percutaneous catheter drainage of infected intra-abdominal fluid collections. American College of Radiology. ACR Appropriateness Criteria. Radiology. 2000;215:1067–1075. [PubMed] [Google Scholar]
- 2.Harisinghani MG, Gervais DA, Hahn PF, Cho CH, Jhaveri K, Varghese J, et al. CT-guided transgluteal drainage of deep pelvic abscesses: indications, technique, procedure-related complications, and clinical outcome. Radiographics. 2002;22(6):1353–1367. doi: 10.1148/rg.226025039. [DOI] [PubMed] [Google Scholar]
- 3.Harisinghani MG, Gervais DA, Maher MM, Cho CH, Hahn PF, Varghese J, et al. Transgluteal approach for percutaneous drainage of deep pelvic abscesses: 154 cases. Radiology. 2003;228(3):701–705. doi: 10.1148/radiol.2283020924. [DOI] [PubMed] [Google Scholar]
- 4.van Doesburg IA, Boerma D, Bollen TL, van Ramshorst B, Wiezer MJ. Large gluteal abscesses as a complication of transgluteal drainage of pelvic abscesses: analysis of three cases and a search of the literature. Dig Surg. 2009;26(4):329–332. doi: 10.1159/000235821. [DOI] [PubMed] [Google Scholar]
- 5.Takizawa K, Nakajima Y, Ogawa Y, Hmaguchi S, Yoshimatsu M, Fujikawa A, et al. A new method of an axial puncture approach for draining loculated pleural effusions. Cardiovasc Intervent Radiol. 2011;34(6):1303–1307. doi: 10.1007/s00270-011-0138-6. [DOI] [PubMed] [Google Scholar]
- 6.Koretsune Y, Sone M, Arai Y, Sugawara S, Itou C, Kimura S, et al. Feasibility and safety of the craniocaudal approach for superior sulcus lesions of the thorax. Cardiovasc Intervent Radiol. 2021;44(9):1456–1461. doi: 10.1007/s00270-021-02844-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robert B, Chivot C, Rebibo L, Sabbagh C, Regimbeau JM, Yzet T. Percutaneous transgluteal drainage of pelvic abscesses in interventional radiology: a safe alternative to surgery. J Visc Surg. 2016;153(1):3–7. doi: 10.1016/j.jviscsurg.2015.10.006. [DOI] [PubMed] [Google Scholar]