Abstract
Background and Aims
Diabetes is recognized as a significant factor in both mortality and morbidity worldwide, affecting various demographics regardless of geographic location, age group, or gender. This correspondence aims to express concern and draw the attention of leaders and policymakers worldwide to this critical public health issue.
Methods
A thorough literature search was conducted utilizing various databases, including Google Scholar, PubMed, Science Direct, and the International Diabetes Federation (IDF) website, to collect the required data. Keywords were strategically applied to enhance search results, with preference given to English‐language articles containing pertinent information.
Results
According to the 2021 report by the IDF, approximately 537 million individuals globally were affected with diabetes, constituting roughly 10.5% of the world's populace. This condition incurred healthcare expenditures totaling $966 billion. Projections indicate a surge in diabetes cases to 783 million by 2045, with associated healthcare costs estimated to surpass $1054 billion. However, almost half of all people with diabetes are unaware of their medical condition, with the highest prevalence of undiagnosed diabetes Mellitus (DM) found in low and middle‐income countries (LMICs) of the regions of Africa, the Western Pacific, and Southeast Asia.
Conclusion
Collaborating with the World Health Organization (WHO), LMIC governments should improve healthcare accessibility, including more frequent diabetes screenings for individuals aged ≥ 45 years and younger individuals at elevated risk of having a family history.
Keywords: early diagnosis, global public health concern, International Diabetes Federation (IDF), low and middle‐income countries (LMICs), Type 2 Diabetes Miletus
1. INTRODUCTION
Diabetes mellitus (DM), generally known as diabetes, is a harmful and chronic illness characterized by persistently high blood glucose levels due to inadequate insulin production or when the body fails to utilize the insulin when it is produced. Diabetes affects individuals of all ages, genders, and geographic locations, making it one of the most prevalent global causes of mortality and morbidity. Hereditary and environmental factors contribute to the etiopathogenesis of type 2 diabetes, which makes up over 90% of all instances. 1 The most common types of DM are type 1 and 2; both have recognized diagnostic criteria. The autoimmune death of pancreatic beta cells is the primary cause of type 1 diabetes. 2 Type 2 diabetes has a vital genetic component and is strongly linked to obesity and a sedentary lifestyle. 1 Gestational diabetes increases the risk of complications during pregnancy and delivery for the mother and fetus in pregnant women. 3 According to the 2016 Noncommunicable Disease Risk Factor Collaboration study, less than 1% of women and even fewer males have a chance of meeting worldwide goals for preventing the rise in the incidence of diabetes by 2025. 2 Furthermore, according to the Global Disease Burden 2019, ischemic heart disease and stroke were the primary and second‐leading causes of the worldwide disease burden in 2019. 4 Diabetes is regarded to be a significant precursor for the both disorders.
2. GLOBAL PREVALENCE
Worldwide, it is estimated that 240 million individuals live with undiagnosed diabetes, with nearly half of all adults with diabetes being unaware of their illness. 5 Diabetes imposes a heavy financial strain on healthcare systems worldwide. It is estimated that 537 million (10.5%) individuals (those aged 20–79 years) worldwide are currently managing the disease. 5 , 6 In 2021, the International Diabetes Federation (IDF) approximated that there were 537 million individuals living with diabetes, making up 10.5% of the global population, resulting in global healthcare expenses amounting to $966 billion. 5 This health cost is predicted to rise to more than $1054 billion by 2045. It is alarming that the prevalence of DM is anticipated to increase to 643 million (11.3%) by 2030 and 783 million (12.2%) by 2045 (Figure 1). 4 , 5 Figure 1 also indicates the uprising trend of the number (millions) of people aged 20−79 years who have diabetes worldwide.
Figure 1.
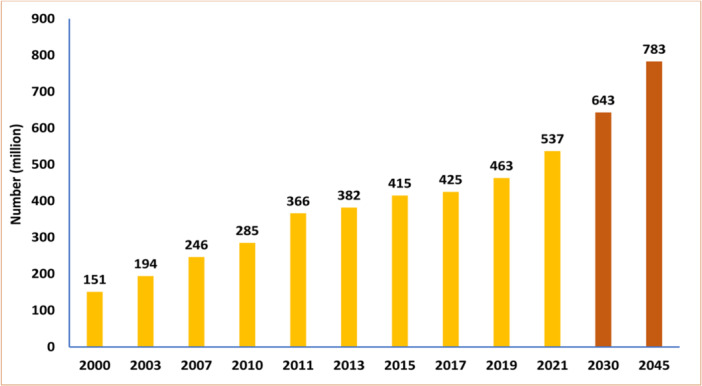
The number (millions) of people aged 20−79 years having diabetes worldwide (projected numbers in case of 2030 and 2045) [The data was retrieved form the 10th edition of IDF atlas; found from: https://diabetesatlas.org].
India, China, the USA, Indonesia, Japan, Pakistan, Russia, Brazil, Italy, and Bangladesh are the top 10 nations with the highest prevalence of diabetes in the world. 5 Consequently, this health problem has grown into a worldwide crisis. In low‐ and middle‐income countries (LMICs), the rate of increase in DM prevalence is much higher than in high‐income countries. 4 It is worth noting that most people with diabetes globally live in LMICs, which account for nearly 80% of the diabetic population. 2 By 2030, the global prevalence of diabetes is projected to reach 643 million, 5 with the majority of this increase due to a 150% increase in emerging economies. 6 In 2021, the global prevalence of DM consecutively outbreaks North Africa and the Middle East (39.4%), where Qatar (76.1%) seems to be the most affected country among all of them. 5 Despite Africa having the lowest prevalence estimate of 4.5% among IDF Regions, it is projected to experience the most substantial increase in the number of individuals affected by diabetes by the year 2045, with a staggering rise of 129%, resulting in approximately 55 million cases. It is noteworthy that Africa also exhibits the highest proportion of undiagnosed diabetes cases, standing at 53.6%. It is worth mentioning that the African Region only dedicated 12.6 billion USD to diabetes‐related expenses, representing just 1.3% of the total global expenditure on diabetes. However, this appropriation does not align with the demographic reality since the African Region hosts about 4.5% of the global population affected by diabetes. 5 Poor nutrition, poverty, and lack of physical activity are some socioeconomic challenges plaguing LMICs. According to a recent report, there is an urgent need for precise, targeted data to drive the development of effective initiatives aimed at addressing these problems. 7 In addition, it was crucial to identify and classify the populations most in risk precisely.
3. ASSOCIATED RISK FACTORS
The prevalence of DM increases in populations whose lifestyles have changed fast from more traditional to more modern forms of living, which are related to an increased risk of developing DM. There is a high correlation between type 2 diabetes and being overweight or obese, as well as growing age, ethnicity, and family history, although the exact causes remain unknown. 8 Polygenic and environmental factors are suspected to contribute to the incidence of type 2 diabetes. 2 The risk of developing DM depends on several factors beyond the simple distribution of genes throughout the population. There is an increasing trend in the worldwide prevalence of type 2 DM. The aging of the population, the rise of the middle class, and the spread of urbanization are all factors that contribute to the rise of obesity. 8 The onset of DM can be delayed by making dietary and lifestyle adjustments. 9 In three of the world's largest groups of countries—North Africa and the Middle East, Latin America and the Caribbean, and Central Europe, Eastern Europe, and Central Asia—high body mass index (BMI) was the leading cause of disability‐adjusted life years caused by type 2 diabetes. 5 Obesity is the leading cause of Type 2 diabetes, accounting for almost 60% of cases. High BMI (52.2%), dietary foods (25.7%), environmental or occupational stress (19.6%), tobacco usage (12.1%), insufficient physical exercise (7.4%), and alcohol use (1.8%) are also significant factors. 10 The long‐term sequelae of diabetes, such as cardiovascular and kidney disease, which appear to be risk factors for death among hospitalized people, may account for some of the increased likelihood of severe consequences associated with diabetes. 5
4. DIABETES AND COVID‐19
The global healthcare system faces a new and unprecedented threat from the coronavirus disease 2019 (COVID‐19) pandemic. In locations where diabetes is common, both the rate of COVID‐19 infection and the rate of death per 100,000 people are higher. 5 , 10 The most significant risks for hospitalized people with diabetes from COVID‐19 were seen in studies conducted in the Western Pacific, Africa, and South and Central America. 4 , 11 Considering additional risks lowered the death rate, although it was still relatively high. In patients with both diabetes and COVID‐19, symptoms and disease progression are extreme. The overall mortality rate is more significant among this group as well. The inflammatory state and increased mortality in the diabetic population have been associated with COVID‐19. Hospitalizations due to COVID‐19 were 3.6 times higher in people with diabetes than those without the condition. 5 , 12
Research into glycemic control has been extensive because of the potential risk it poses for severe diseases associated with COVID‐19. Poorer COVID‐19 outcomes, including hospitalization, intensive care unit admission, and mortality, were related to higher HbA1c levels, even after adjusting for age, sex, and other risk variables. The poor prognosis of COVID‐19 diabetic individuals is due to a combination of factors. Some of these complications include hyperglycemia, insulin resistance, diminished pancreatic function, and the development of ages. 11 , 12 COVID‐19 and DM have bidirectional effects on one another, where each condiction can worsen other, creating a vicious circle or interplay. It is reported that up to 50% of individuals who have succumbed to COVID‐19 were afflicted with vascular and metabolic disorders, including DM. 13 After introducing severe acute respiratory syndrome coronavirus 2, patients with pre‐existing conditions such as diabetes were more likely to be hospitalized and die. 10 Increases in prediabetes‐to‐diabetes transition, newly diagnosed cases of diabetes, and diabetes caused by corticosteroid use are all linked to the COVID‐19 pandemic. 5
5. TACKLING STRATEGIES
Type 2 DM can be prevented or delayed by adopting several non‐pharmaceutical strategies, including managing a normal weight, practicing regular physical activity, altering a sedentary lifestyle, and quitting smoking. Another critical factor in limiting the incidence of DM is weight loss. Each kilogram of weight loss results in a 16% relative risk reduction and strongly correlates with a decreased progression to Type 2 diabetes. 14 According to a clinical investigation carried out in Da Qing, China, diet or exercise or a combination of diet and exercise was significantly linked to reductions in the probability of acquiring diabetes by 31%, 46%, and 42%, respectively. 15 People with a higher likelihood of developing diabetes should undergo more frequent screenings. The elevated risk can be assessed through various factors, such as personal attributes (advanced age, belonging to a minority racial or ethnic group, having a family history of diabetes), medical indicators (being overweight, having high blood pressure, experiencing abnormal cholesterol levels), and past instances of abnormal glucose levels (gestational diabetes, impaired fasting glucose and tolerance). 16
6. EARLY DETECTION AND ITS CONSEQUENTIAL IMPLICATIONS
A recent report demonstrated that almost half of all people with diabetes (44.7%; 239.7 million) were unconscious of their medical condition in 2021. 5 The prevalence of undiagnosed DM is most enunciated in the regions of Africa, Western Pacific, and Southeast Asia, with respective proportions of 53.6%, 52.8%, and 51.3%. Conversely, the incidence of undiagnosed DM is notably lower in North America and the Caribbean, where it stands at 24.2%. 17 The discrepancy between high and low to moderate‐income regions as well as the frequency of undiagnosed diabetes remains significant. During the pre‐diagnostic phase of Type 2 diabetes, a latent period ensues wherein the disease remains undetected. Throughout this interval, there exists a notable elevation in the risk factors associated with both microvascular and macrovascular complications of diabetes, particularly evident among individuals with suboptimal glycemic regulation, concurrent with the progressive development of diabetic complications. The evidence obtained from numerous studies unequivocally suggests that DM undergoes substantial progression in severity before its clinical diagnosis. This progression signifies the emergence of pervasive structural abnormalities associated with diabetes during its asymptomatic preclinical stage. 16 The advancement of Type 2 DM stemming from impaired fasting glucose (IFG) is conventionally characterized by a gradual trajectory, wherein its symptomatic manifestations often elude detection over protracted periods. Significantly, delays in the detection and diagnosis of T2DM represent pivotal factors contributing to suboptimal disease management and an escalated predisposition to complications. 18
Early identification of high‐risk individuals could aid in implementing preventative and therapeutic measures to lower the risk of DM and its associated complications. 19 Further advancements in diabetes surveillance systems, as well as the implementation of strategies and tactics to detect undiagnosed diabetes at the population level, are required, especially among LMICs. Therefore, it is prudent to advocate early screening protocols for individuals identified as having an augmented susceptibility to diabetes. This heightened predisposition may be discerned through various avenues, encompassing demographic parameters such as advanced age, belonging to minority racial or ethnic groups, or possessing a familial history of diabetes. Additionally, clinical indicators, including but not limited to obesity, hypertension, and dyslipidemia, as well as antecedent instances of aberrant glucose levels (e.g., gestational diabetes, impaired fasting glucose, impaired glucose tolerance), serve as significant determinants of elevated risk. The American Diabetes Association has provided guidelines defining routine screening for adults aged 45 years or above while delineating specific high‐risk cohorts that necessitate screening among younger demographics. Furthermore, individuals presenting with fasting plasma glucose exceeding 126 mg/dL warrant confirmatory testing, mandating repetition of the assessment to establish a definitive diagnosis, particularly in asymptomatic patients. 16
The African region confronts specific challenges in effectively managing diabetes and its complications. These challenges include insufficient funding allocations, a shortage of specialized healthcare professionals focused on noncommunicable diseases prevention and control, inadequate availability of requisite medications, disparities in healthcare delivery, limited accessibility to healthcare facilities, and insufficient community sensitization efforts. Cumulatively, these issues contribute to Africa bearing a disproportionate burden of diabetes relative to the global population. 20 In addition, urbanization trends and nutritional influences, notably the adoption of high‐calorie “Westernized” dietary patterns leading to obesity, are significant reasons in Sub‐Saharan Africa. Concurrently, lifestyle modifications characterized by sedentary behaviors contribute significantly to this epidemiological challenge. 21 Therefore, the implementation of early screening initiatives in Africa may prove to be a strategically advantageous approach, considering the economic implications associated with the management of diabetes.
7. CONCLUSION
The epidemic of DM threatens human health on a global scale. The best way to prevent DM is to lead a healthy lifestyle by ensuring a health‐promoting habit that includes regular physical activity and a well‐balanced diet, maintaining a healthy weight, and cutting back on harmful practices. Long‐term consequences of DM can be avoided via intensive lifestyle adjustments and therapies to regulate blood glucose levels. The deceleration of diabetes proliferation necessitates implementing a cohesive health strategy, augmenting the framework provided by the World Health Organization (WHO). Undiagnosed DM presents a dual hazard, manifesting as both a financial burden and a source of complications for individuals, communities, and healthcare systems alike. As most diabetes‐related challenges arise from its associated complications, implementing a preventative initiative grounded in family history assessment and other tailored early screening modalities emerges as a viable strategy for effectively managing DM within LMICs. In collaboration with WHO, governments of LMICs should enhance the availability of healthcare initiatives, including more frequent diabetes screenings for specifically individuals aged 45 years and above and for younger individuals at higher risk.
AUTHOR CONTRIBUTIONS
Md. Jamal Hossain: Conceptualization; methodology; software; data curation; investigation; validation; formal analysis; supervision; funding acquisition; writing—original draft; visualization; writing—review and editing; project administration; resources. Md. Al‐Mamun: Investigation; validation; formal analysis; writing—original draft; visualization; data curation; supervision; resources. Md. Rabiul Islam: Writing—review and editing; validation; visualization; supervision; resources; formal analysis; data curation.
CONFLICT OF INTERESTS STATEMENT
The author declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Md. Jamal Hossain affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Hossain MJ, Al‐Mamun M, Islam MR. Diabetes mellitus, the fastest growing global public health concern: early detection should be focused. Health Sci Rep. 2024;7:e2004. 10.1002/hsr2.2004
DATA AVAILABILITY STATEMENT
The manuscript includes all the required data to support the findings. All authors have read and approved the final version of the manuscript. The corresponding author had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1. The Lancet . Diabetes: a defining disease of the 21st century. The Lancet. 2023;401(10394):2087. [DOI] [PubMed] [Google Scholar]
- 2. Ahmad E, Lim S, Lamptey R, Webb DR, Davies MJ. Type 2 diabetes. The Lancet. 2022;400(10365):1803‐1820. [DOI] [PubMed] [Google Scholar]
- 3. Sun H, Saeedi P, Karuranga S, et al. IDF diabetes Atlas: global, regional and country‐level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ong KL, Stafford LK, McLaughlin SA, et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the global burden of disease study 2021. Lancet. 2023;402:203‐234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Magliano D, Boyko EJ. IDF diabetes atlas. 10th edition. International Diabetes Federation; 2021. https://diabetesatlas.org/atlas/tenth-edition/ [PubMed] [Google Scholar]
- 6. Laraeni Y, Danuyanti IGAN, Resnhaleksmana E, Pauzi I, Mataram IKA, Agustini NP. High antioxidant level in cajanus sajan reduces blood glucose level and improves blood lipid profile of rats as diabetes mellitus models. Int J Health Sci. 2021;5(1):29‐37. [Google Scholar]
- 7. Dunachie S, Chamnan P. The double burden of diabetes and global infection in low and middle‐income countries. Trans R Soc Trop Med Hyg. 2019;113(2):56‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lovic D, Piperidou A, Zografou I, Grassos H, Pittaras A, Manolis A. The growing epidemic of diabetes mellitus. Curr Vasc Pharmacol. 2020;18(2):104‐109. [DOI] [PubMed] [Google Scholar]
- 9. Rajput R, YogeshYadav M, Rajput M, Nanda S. Utility of HbA1c for diagnosis of gestational diabetes mellitus. Diabetes Res Clin Pract. 2012;98(1):104‐107. [DOI] [PubMed] [Google Scholar]
- 10. Khunti K, Valabhji J, Misra S. Diabetes and the COVID‐19 pandemic. Diabetologia. 2023;Feb 66(2):255‐266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gangadaran P, Padinjarathil H, Rajendran SHS, et al. COVID‐19 and diabetes: what do we know so far? Exp Biol Med. 2022;247(15):1330‐1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nassar M, Daoud A, Nso N, et al. Diabetes mellitus and COVID‐19: review article. Diabetes & metabolic syndrome. 2021;15(6):102268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Steenblock C, Schwarz PEH, Ludwig B. COVID‐19 and metabolic disease: mechanisms and clinical management. The Lancet Diabetes & Endocrinology. 2021;9(11):786‐798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sarker A, Das R, Ether S, Saif‐Ur‐Rahman KM. Non‐pharmacological interventions for the prevention of type 2 diabetes mellitus in low and middle‐income countries: protocol for a systematic review and meta‐analysis of randomized controlled trials. Syst Rev. 2020;9(1):288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and diabetes study. Diabetes Care. 1997;20(4):537‐544. [DOI] [PubMed] [Google Scholar]
- 16. Harris MI, Eastman RC. Early detection of undiagnosed diabetes mellitus: a US perspective. Diabetes Metab Res Rev. 2000;16(4):230‐236. [DOI] [PubMed] [Google Scholar]
- 17. Ogurtsova K, Guariguata L, Barengo NC, et al. IDF diabetes Atlas: global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res Clin Pract. 2022;183:109118. [DOI] [PubMed] [Google Scholar]
- 18. Kopitar L, Kocbek P, Cilar L, Sheikh A, Stiglic G. Early detection of type 2 diabetes mellitus using machine learning‐based prediction models. Sci Rep. 2020;10(1):11981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Juan J, Yang H. Prevalence, prevention, and lifestyle intervention of gestational diabetes mellitus in China. Int J Environ Res Public Health. 2020;17(24):9517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mukamusoni D, Ndabarora E. Systematic review of diabetes mellitus prevalence and determinants of early detection in Africa. Kibogora Polytech Scient J. 2018;1(1):1‐5. [Google Scholar]
- 21. Glezeva N, Chisale M, McDonald K, Ledwidge M, Gallagher J, Watson CJ. Diabetes and complications of the heart in Sub‐Saharan Africa: an urgent need for improved awareness, diagnostics and management. Diabetes Res Clin Pract. 2018;137:10‐19. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The manuscript includes all the required data to support the findings. All authors have read and approved the final version of the manuscript. The corresponding author had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.


