Abstract
Background:
Changes in knee loading have been reported after meniscectomy. Knee loading has previously been assessed during jogging and treadmill running rather than overground running, which could give altered results.
Purpose/Hypothesis:
The purpose of this study was to evaluate knee function during overground running and walking after meniscectomy. It was hypothesized that the affected limb would demonstrate higher external knee adduction moment, lower knee flexion moment (KFM), and lower knee rotation moment (KRM) compared with the contralateral limb and with healthy individuals.
Study Design:
Controlled laboratory study.
Methods:
Kinematic and kinetic data were collected during running and walking in individuals after a meniscectomy and healthy individuals. Total knee joint moments (TKJM) were calculated from the sagittal, frontal, and transverse knee moments. Isometric quadriceps strength, perceived knee function, and kinesiophobia were also assessed. A mixed linear model compared differences between the affected leg, the contralateral leg, and the healthy leg.
Results:
Data were collected on 20 healthy individuals and 30 individuals after a meniscectomy (mean ± SD, 5.7 ± 2.9 months postsurgery), with 12, 16, and 2 individuals who had medial, lateral, and both medial and lateral meniscectomy, respectively. The affected limb demonstrated lower TKJM (P < .001), KFM (P = .004), and KRM (P < .001) during late stance of walking compared with the healthy group. Lower TKJM and KFM were observed during running in the affected limb compared with the contralateral limb and healthy group. No significant differences were observed between contralateral and healthy limbs except for KRM during late stance of walking. Lower quadriceps strength was observed in the affected (P < .001) and contralateral limbs (P = .001) compared with the healthy group. Individuals after a meniscectomy also reported greater kinesiophobia (P = .006) and lower perceived knee function (31.1%; P < .001) compared with the healthy group.
Conclusion:
After meniscectomy, individuals who sustained a traumatic meniscal injury showed lower TKJM in the affected limb compared with the contralateral limb and healthy individuals. This decrease in TKJM can be attributed to altered knee-loading strategies in the sagittal and transverse planes.
Clinical Relevance:
Improving movement strategies, quadriceps strength, and kinesiophobia through rehabilitation approaches will allow individuals to load their knee appropriately when returning to sport.
Registration:
NCT03379415 (ClinicalTrials.gov identifier).
Keywords: meniscal injuries, running, walking, knee kinetics, total knee joint loading
Traumatic injuries to the meniscus are common in sports. 42 Despite clinically relevant improvements after exercise and education, 51 surgical interventions such as meniscal repair and meniscectomies remain common. 1 Meniscectomies are often used to remove the damaged meniscus, particularly when the injury occurs in a location with a low blood supply.1,42 These surgical interventions are used to treat meniscal injuries with the aim of resolving the mechanical issue while at the same time preserving as much of the meniscus as possible.1,42,53,62 However, partial removal of the meniscus reduces its ability to transmit loads and can lead to increased articular cartilage loading and degeneration.4,10,20,37 Long-term consequences of this, such as the development or progression of knee osteoarthritis (OA), are often reported in individuals who have previously had a meniscal injury or meniscectomy.11,16,17,47
External knee adduction moments (KAMs) are often used to estimate medial knee joint loading3,12,43 and are associated with the progression of knee OA.43,57 During walking (1.3-1.4 m/s) and jogging (2.5 m/s), KAM increased at 12 to 24 months postmeniscectomy compared with baseline measures.24,25,55 Greater KAMs were also observed during walking and jogging compared with those in healthy individuals at 3 months after a meniscectomy. 24 However, these studies focused on either surgery as a result of degenerative meniscal injuries or did not differentiate between degenerative or traumatic injuries, which are considered different clinically.6,33 Data exploring knee loading in young individuals who had a meniscectomy as a result of a traumatic meniscal injury are needed.
As knee OA progresses, reduced external knee flexion moment (KFM) during walking associated with pain and quadriceps weakness occurs. 3 After a meniscectomy, individuals also tend to have a lower load at the knee, likely due to altered movement patterns, during walking,24,55 jogging, 25 treadmill running, 61 and bilateral landing. 19 In addition to different etiology before surgery, running speed or mode of running is likely to lead to altered knee kinematics and kinetics.45,46,50 When compared with jogging (2.2-2.6 m/s), faster running speeds (3.3-3.7 m/s) have resulted in increased KFM and a shift to greater ankle moments.45,46 As individuals progress towards returning to sport, they will be required to perform more demanding tasks, including running, and are likely to exceed these speeds. Therefore, evaluating knee loading during overground running after a meniscectomy will improve the understanding of loading strategies in these individuals and support rehabilitation strategies.
Individuals also often present with weaker quadriceps, particularly during the first 12 months postsurgery.22,24,56 Therefore, reduced knee loading may be due to the quadriceps weakness commonly observed after a meniscectomy. Other factors such as pain and kinesiophobia can also contribute to altered knee loading.13,27,38 Individuals who have had a meniscectomy reported higher kinesiophobia postsurgery to values that were comparable with those reported after anterior cruciate ligament (ACL) reconstruction. 58 However, there is limited evidence exploring kinesiophobia and knee loading after a meniscectomy. 30
Often described as the screw-home mechanism, the higher internal rotation moments that occur as the knee extends during late stance are used to support knee joint stability. 2 In knees that have compromised stability, such as ACL-deficient knees, internal rotation moments are lower compared with in healthy control knees. 21 The meniscus also plays a role in knee joint stability,20,44 and after a meniscectomy, stability is often reduced. 44 Although knee rotation moments (KRMs) contribute the least to the overall loading at the knee in individuals with mild knee OA, 3 less is known about KRM during walking or running after a meniscectomy.
The total knee joint moment (TKJM) reflects the contribution from all 3 moment components (frontal, sagittal, and transverse) acting on the knee.3,39 Combining KAM and KFM provides a better predictor of medial contact force than KAM alone.35,40,59 This combination of KAM and KFM has also been shown to be sensitive to treatments in patients with OA. 8 Previous studies have examined longitudinal changes in TKJM in those with medial knee OA 3 and after ACL surgery. 18 In these studies, TKJM did not appear to change over time; however, the contribution of KAM and KFM shifted with time. Reduced KAM and increased KFM contribution were associated with reduced progression of degeneration in the knee. 18 These studies did not compare TKJM with that in healthy controls; therefore, comparing TKJM in knees that have altered loading patterns such as those after a meniscectomy24,55 will give further insight into loading patterns.
Changes in knee loading after a meniscectomy have been reported and are suggested to lead to increased risks of developing knee OA.24,55 However, these studies have either examined individuals who had a degenerative meniscal injury before surgery or have not distinguished between different etiologies (i.e. degenerative or traumatic meniscal injury) before surgery limiting our understanding of knee loading after surgery after a traumatic injury. Studies in young adults after traumatic knee injury have examined KFM only but not explored frontal, transverse, and sagittal loading in the knee. In addition, previous studies have not assessed knee loading during overground running at speeds that individuals are likely to experience after returning to sport. Therefore, examining frontal, sagittal, and transverse knee loading will provide a better understanding of strategies employed in the affected limb compared with the contralateral limb in individuals after a meniscectomy and a comparison with healthy individuals could help inform future rehabilitation approaches.
In this study, we aimed to compare knee function in the affected limb after a meniscectomy with that in the contralateral limb and healthy individuals. Based on previous research, we hypothesized that the affected limb would demonstrate higher KAM, lower KFM, and lower KRM compared with the contralateral limb and healthy individuals.
Methods
Individuals who had recently undergone a partial meniscectomy were recruited from local National Health Service and private orthopaedic clinics 3 to 12 months after surgery. Healthy individuals were recruited from advertisements placed in fitness centers and sports clubs in the Greater Manchester area. Participants were included if they were aged between 18 and 40 years and competed/participated in sport at least twice a week. For the meniscectomy group, individuals were included in the study if they sustained an isolated meniscal injury during a sporting movement (eg, change of direction, landing, or running) indicating a traumatic meniscal injury. Participants were excluded if they had a concurrent injury with their meniscal injury (ie, ACL injury); a history of lower extremity surgeries (except a meniscectomy); or previous lower limb traumatic injury other than the sustained meniscal injury, inflammatory or infectious pathology in the lower limb, or ligament laxity. Informed consent was obtained from each participant before testing. This study was registered at ClinicalTrials.gov (ID: NCT03379415), and the study protocol received institutional review board approval.
Study Outcomes
Participants completed the Tampa Scale for Kinesiophobia (TSK) 41 and the Knee injury and Osteoarthritis Outcome Score (KOOS) to quantify kinesiophobia and knee function, respectively. 48 Overall KOOS and the 5 subscales (Pain, Symptoms, Activities of Daily Living, Sport and Recreation, and Quality of Life) were assessed for each participant. A lower KOOS indicated higher pain and lower function and quality of life. Activity level preinjury, presurgery, and postsurgery were obtained using a questionnaire developed from the Tegner activity scale and the sports fitness index. 60
A 27-camera Qualisys motion capture system (200 Hz; 27 Qualisys Oqus) and 4 force plates (AMTI force plates, 1000 Hz; Advanced Mechanical Technology Inc) were used to collect kinematic and kinetic data. Participants completed 5 successful self-selected walking and running trials on a 60-m running track. Standardized footwear (Gel Windhawk; Asics) was worn by all participants during data collection. The calibrated anatomical systems technique marker set technique 9 was used to create the 6 degrees of freedom movement for each segment. Retroreflective markers were attached to anatomical landmarks on the lower body and thorax. In addition to anatomical landmarks, rigid clusters that had 4 nonorthogonal markers each were attached to the thigh and shanks to track motion. Before the collection of the walking and running trials, a static calibration trial was collected.
The 6 degrees of freedom model was created using Visual3D (Version 6; C-Motion Inc) software. A fourth-order low-pass Butterworth filter with a matched 15-Hz cutoff frequency was applied to the marker motion data and analog force data. 34 Hip joint centers were estimated using a regression model based on markers placed on the anterior and posterior iliac spine. 7 Midpoints between the malleoli and femoral epicondyles were calculated to identify ankle and knee joint centers. Knee joint kinematics were calculated using X-Y-Z Euler rotation sequence equivalent to the joint coordinate system.23,32 Geometric and inertial segment properties were estimated for each participant.14,26 External knee joint kinetic data were calculated using 3-dimensional inverse dynamics, normalized to body weight multiplied by height, and expressed as a percentage.
TKJMs were calculated throughout stance as the square root of the sum of the squares of KFM, KAM, and KRM. 3 For walking, the peak during early stance was defined as the maximum TKJM from 1% to 50% of stance. Late-stance peak TKJM was defined as the maximum value, 51% to 100%, of stance. During peak running, TKJM was identified as the maximum value during stance. To better understand the contribution to TKJM, sagittal, frontal, and transverse knee kinematic and kinetic outcomes were taken at the point of peak TKJM for both walking and running.
Quadriceps muscle strength was assessed using an isokinetic dynamometer (Biodex System 3 PRO; Biodex Medical Systems). Participants were seated with 85° of hip flexion and 60° of knee flexion with straps placed across the chest and thigh to limit extraneous movement. After 4 submaximum warm-up repetitions for familiarization, participants completed 5 maximum efforts for 5 seconds with 20 seconds of rest between repetitions. Maximum isometric torques were recorded and normalized to body mass.
Statistical Analysis
Linear mixed models were used to compare between limbs, with participants included as random effects and limbs as a fixed effect to account for independent (affected limbs vs healthy limbs) and dependent (affected limb vs contralateral limb) comparisons. Both limbs were included in the analysis for healthy and meniscectomy groups. Post hoc comparisons with 95% CIs were performed using Bonferroni adjustments for multiple comparisons. Effect sizes were determined using the Hedges g bias correction, with values of 0.2, 0.5, and 0.8 determined as small, medium, and large effects, respectively. 29 Statistical analyses were conducted in R (2022; R Core Team, Version 4.2.1) within RStudio (RStudio, Version 2022.7.2.576) using the lme4 and lmerTest packages.5,36,49
Results
Participant Characteristics
A total of 50 participants were recruited for the current study. Data were collected on 20 healthy individuals and 30 patients who had undergone a meniscectomy (Figure 1). A sensitivity analysis was conducted with the desired power of 80%. With the study sample, this study was able to detect effect sizes of 0.83 and above when comparing the meniscectomy and healthy group, and 0.46 when comparing the meniscectomy knee and contralateral knee. Of the individuals who had a meniscectomy, 53.3% had a lateral meniscectomy, 40% had a medial meniscectomy, and 6.7% had a meniscectomy on both the medial and the lateral sides of the knee. Due to missing data in the meniscectomy group, the total number of participants included in the strength data analysis included 27 data sets for the affected limb and 26 for the contralateral limb. No data were missing for the healthy group.
Figure 1.
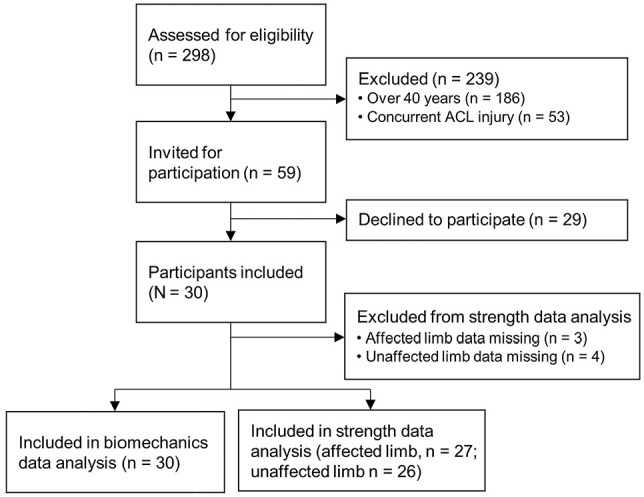
Flowchart of participants with meniscectomy during the study. ACL, anterior cruciate ligament.
There were some significant differences in the characteristics between participant groups, with the meniscectomy group 5 years older (P = .004) and 7.8 kg heavier (P = .044) compared with the healthy group (Table 1). The meniscectomy group reported significantly higher scores on the TSK compared with the healthy group (35.8 ± 6.5 vs 30.9 ± 5.0; P = .006). The meniscectomy group reported significantly lower scores for the overall KOOS and all KOOS subscales, with large effect sizes (P < .001 for all; g = 1.30-2.67). The mean time to assessment postsurgery for individuals in the meniscectomy group was 5.7 ± 2.9 months. Maximum normalized isometric torque was greater in the healthy group (3.27 ± 1.19 N·m/kg) compared with both the affected limb (2.20 ± 0.72 N·m/kg; P < .001; g = 1.45) and the contralateral limb (2.27 ± 0.77 N·m/kg; P = .001; g = 1.33). No significant differences in strength were observed between the contralateral and affected legs. Individuals who had a meniscectomy were more active before their injury compared with the healthy group; however, patients in the meniscectomy group were less active compared with the healthy group after their injury and surgery.
Table 1.
Participant Characteristics According to Study Group a
| Characteristic | Healthy Group (n = 20) | Meniscectomy Group (n = 30) | P | ES b |
|---|---|---|---|---|
| Sex | ||||
| Male | 12 (60) | 20 (66.6) | ||
| Female | 8 (40) | 10 (33.3) | ||
| Age, y | 24.7 ± 5.0 | 29.7 ± 6.6 | .004 | 0.81 |
| Height, cm | 175.1 ± 8.6 | 175.6 ± 9.6 | .877 | 0.04 |
| Mass, kg | 74.5 ± 11.8 | 82.3 ± 13.9 | .044 | 0.59 |
| TSK | 30.9 ± 5.0 | 35.8 ± 6.5 | .006 | 0.82 |
| KOOS | 98.0 ± 2.3 | 67.6 ± 17.1 | <.001 | 2.25 |
| Pain | 99.0 ± 2.1 | 75.3 ± 15.9 | <.001 | 1.88 |
| Symptoms | 94.8 ± 5.2 | 64.9 ± 21.4 | <.001 | 1.74 |
| Activities of Daily Living | 99.9 ± 0.5 | 86.3 ± 13.2 | <.001 | 1.30 |
| Sport and Recreation | 97.8 ± 5.7 | 62.2 ± 23.1 | <.001 | 1.91 |
| Quality of Life | 98.8 ± 3.3 | 49.1 ± 23.4 | <.001 | 2.67 |
| Activity level | ||||
| Preinjury | 6.8 ± 1.7 | 8.0 ± 1.3 | <.001 | 0.80 |
| Postinjury | NA | 3.6 ± 3.0 | .015 c | 1.23 |
| Postsurgery | NA | 5.4 ± 2.3 | <.001 c | 0.66 |
Data are reported as n (%) or mean ± SD. Boldface P values indicate statistically significant difference between groups (P < .05). ES, effect size; KOOS, Knee injury and Osteoarthritis Outcome Score; NA, not applicable; TSK, Tampa Scale for Kinesiophobia.
Hedges g bias correction.
Comparison with preinjury activity level of healthy group.
Walking
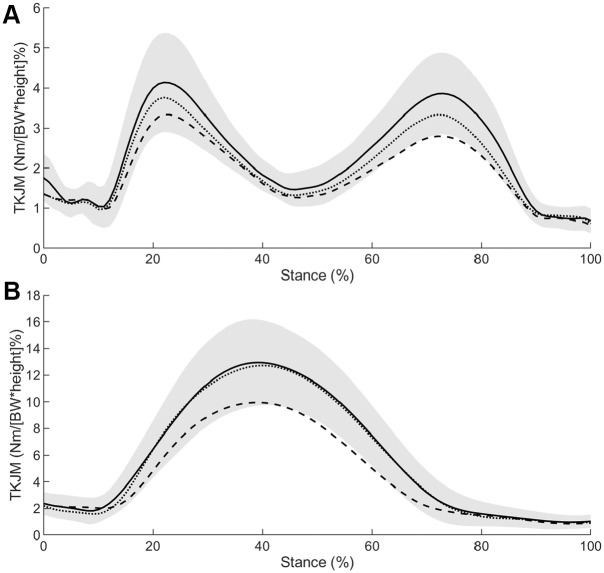
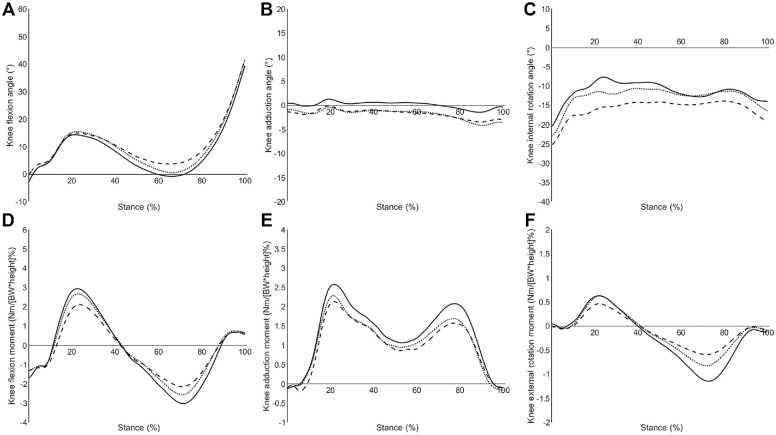
Walking speeds were comparable between the healthy (1.5 ± 0.2 m/s) and meniscectomy (1.5 ± 0.2 m/s; P = .145; g = 0.421) groups. During early stance, the affected limb had lower TKJM compared with the healthy limb (P = .023; g = 0.752), but there were no differences between the affected limb and contralateral limb (P = .081; g = 0.377). Knee flexion angles at initial contact were lower in the affected limb compared with the contralateral limb (P = .003; g = 0.510). Peak TKJM was lower during late stance in the affected limb compared with the healthy limb (P < .001; g = 1.104) and contralateral limb (P = .004; g = 0.599). Peak knee flexion angle during late stance was higher in the affected limb compared with the healthy limb (P = .004; g = 0.918) and contralateral limb (P = .009; g = 0.465). At peak TKJM during late stance, knee extension moment (KEM; P = .004; g = 0.955) and KRM (P < .001; g = 1.09) were lower in the affected limb compared with the healthy limb. No differences were observed between the affected limb and contralateral limb for KEM (P = .127; g = 0.362) and KRM (P = .401; g = 0.355) at peak TKJM. No statistical differences were observed between the healthy and contralateral limbs, except for KRM during late stance. KRM was lower in the contralateral limb compared with the healthy limb (P = .013; g = 0.755) at peak TKJM during late stance (Table 2). Figure 2 shows the ensemble mean TKJM during walking and running. Appendix Figures A1 and A2 show the ensemble mean knee joint angles and knee joint moments for walking (Figure A1) and running (Figure A2).
Table 2.
Knee Kinematic and Kinetic Outcomes During Walking in the Healthy and Meniscectomy Groups a
| Knee Joint Movement | Healthy Group | Meniscectomy Group | Mean Difference (95% CI) b | |||
|---|---|---|---|---|---|---|
| Affected Leg | Contralateral Leg | Affected Leg vs Healthy Group | Affected Leg vs Contralateral Leg | Healthy Group vs Contralateral Leg | ||
| Knee joint kinematics, deg | ||||||
| KFA at initial contact | −2.8 ± 3.4 | −0.4 ± 4.7 | −2.8 ± 5.1 | 2.5 (−0.4 to 5.36) | 2.5 (0.7 to 4.2) | 0.0 (−2.9 to 2.9) |
| KFA at early TKJM | 13.9 ± 4.3 | 14.8 ± 7.0 | 14.6 ± 7.4 | 0.9 (−3.2 to 5.1) | 0.2 (−2.3 to 2.8) | −0.7 (−4.8 to 3.4) |
| KAA at early TKJM | 1.0 ± 3.3 | −0.6 ± 4.4 | −0.5 ± 3.7 | −1.6 (−4.0 to 0.8) | −0.1 (−1.9 to 1.7) | 1.5 (−1.0 to 3.9) |
| KRA at early TKJM | −7.7 ± 9.7 | −16.0 ± 9.8 | −11.8 ± 9.2 | −8.3 (−14.5 to −2.2) | −4.3 (−9.0 to 0.5) | 4.1 (−2.1 to 10.2) |
| KFA at late TKJM | 0.5 ± 3.4 | 5.3 ± 6.1 | 2.4 ± 6.4 | 4.8 (1.3 to 8.3) | 2.9 (0.6 to 5.2) | −1.9 (−5.4 to 1.6) |
| KAA at late TKJM | −0.1 ± 3.4 | −2.1 ± 4.3 | −2.0 ± 3.1 | −2.0 (−4.5 to 0.4) | −0.2 (−1.6 to 1.3) | 1.9 (−0.5 to 4.3) |
| KRA at late TKJM | −12.3 ± 8.8 | −14.3 ± 9.8 | −12.0 ± 10.7 | −2.0 (−8.2 to 4.2) | −2.2 (−7.2 to 2.7) | −0.3 (−6.4 to 5.9) |
| Knee joint kinetics, % c | ||||||
| Peak early stance TKJM | 4.3 ± 1.2 | 3.5 ± 1.0 | 3.9 ± 1.0 | −0.8 (−1.5 to −0.1) | −0.4 (−0.8 to 0.0) | 0.4 (−0.3 to 1.1) |
| KFM at early TKJM | 2.9 ± 1.7 | 2.1 ± 1.7 | 2.5 ± 1.5 | −0.8 (−1.9 to 0.3) | −0.4 (−1.1 to 0.3) | 0.4 (−0.6 to 1.5) |
| KAM at early TKJM | 2.5 ± 0.8 | 2.1 ± 1.1 | 2.2 ± 0.9 | −0.4 (−1.0 to 0.2) | −0.1 (−0.7 to 0.4) | 0.3 (−0.3 to 0.9) |
| KERM at early TKJM | 0.6 ± 0.3 | 0.4 ± 0.7 | 0.6 ± 0.5 | −0.2 (−0.5 to 0.1) | −0.2 (−0.4 to 0.1) | 0.0 (−0.3 to 0.3) |
| Peak late stance TKJM | 4.0 ± 1.0 | 3.0 ± 0.8 | 3.4 ± 0.7 | −1.0 (−1.6 to −0.4) | −0.5 (−0.8 to −0.1) | 0.5 (−0.1 to 1.1) |
| KEM at late TKJM | −3.0 ± 1.1 | −2.1 ± 0.9 | −2.4 ± 1.1 | 0.9 (0.2 to 1.6) | 0.4 (−0.1 to 0.8) | −0.6 (−1.2 to 0.1) |
| KAM at late TKJM | 2.1 ± 1.0 | 1.5 ± 1.0 | 1.6 ± 1.1 | −0.5 (−1.2 to 0.2) | 0.0 (−0.5 to 0.4) | 0.5 (−0.2 to 1.2) |
| KIRM at late TKJM | −1.2 ± 0.4 | −0.6 ± 0.6 | −0.8 ± 0.6 | 0.6 (0.3 to 0.9) | 0.2 (−0.1 to 0.6) | −0.4 (−0.7 to −0.1) |
| Knee adduction angular impulse | 0.9 ± 0.3 | 0.7 ± 0.3 | 0.8 ± 0.3 | −0.2 (−0.4 to 0.1) | 0.0 (−0.2 to 0.1) | 0.1 (−0.1 to 0.3) |
Data are reported as mean ± SD unless otherwise indicated. Boldface values indicate statistically significant difference between groups compared (P < .05). KAA, knee adduction angle; KAM, knee adduction moment; KEM, knee extension moment; KERM, knee external rotation moment; KFA, knee flexion angle; KFM, knee flexion moment, KIRM, knee internal rotation moment; KRA, knee rotation angle; TKJM, total knee joint moment.
CI, Confidence Interval
All kinetic data were normalized to body weight × height and are reported as percentages.
Figure 2.
Ensemble mean total knee joint moments (TKJMs), normalized to body weight (BW) and height, during (A) walking and (B) running for the healthy group (solid) and affected leg (dashed) and contralateral leg (dotted) for the meniscectomy group.
Running
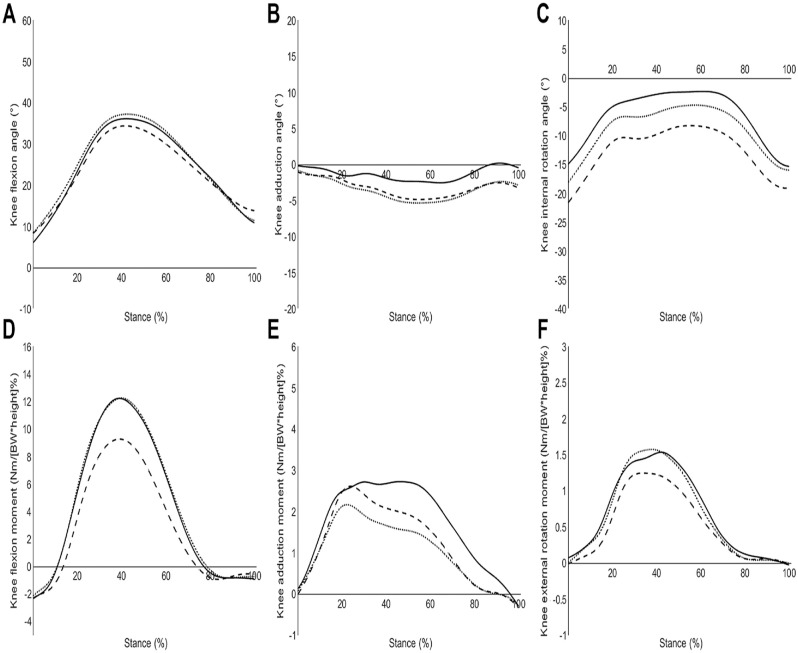
Running speeds did not differ between healthy (3.7 ± 0.6 m/s) and meniscectomy (3.6 ± 0.7 m/s; P = .693; g = 0.113) groups. Peak TKJM was lower for the affected limb compared with the healthy limb (P < .001; g = 1.01) and contralateral limb (P < .001; g = 0.986). Knee flexion angle at peak TKJM was lower in the affected limb compared with the contralateral limb (P = .004; g = 0.632). No differences in knee flexion angles at peak TKJM were observed between the affected limb and healthy limb (P = .471; g = 0.344). The affected limb had higher external knee rotation angles at peak TKJM compared with the healthy limb (P = .004; g = 0.845) and contralateral limb (P = .044; g = 0.503). At peak TKJM, KFM was lower in the affected limb compared with the healthy (P = .002; g = 0.834) and contralateral limbs (P < .001; g = 1.02). No statistical differences were observed between the healthy and contralateral limbs (Table 3).
Table 3.
Knee Kinematic and Kinetic Outcomes During Running in the Healthy and Meniscectomy Groups a
| Knee Joint Movement | Healthy Group | Meniscectomy Group | Mean Difference (95% CI) b | |||
|---|---|---|---|---|---|---|
| Affected Leg | Contralateral Leg | Affected Leg vs Healthy Group | Affected Leg vs Contralateral Leg | Healthy Group vs Contralateral Leg | ||
| Knee joint kinematics, deg | ||||||
| KFA at initial contact | 6.0 ± 4.3 | 8.4 ± 4.2 | 8.5 ± 5.4 | 2.3 (−0.7 to 5.4) | −0.1 (−2.2 to 2.0) | −2.4 (−5.5 to 0.6) |
| KFA at peak TKJM | 35.7 ± 5.7 | 33.4 ± 6.9 | 37.2 ± 4.9 | −2.2 (−6.1 to 1.6) | −3.8 (−6.6 to −1.0) | −1.6 (−5.4 to 2.3) |
| KAA at peak TKJM | −1.5 ± 5.2 | −3.4 ± 6.3 | −4.2 ± 5.1 | −1.8 (−5.4 to 1.7) | 0.9 (−1.9 to 3.6) | 2.7 (−0.8 to 6.2) |
| KRA at peak TKJM | −2.7 ± 9.2 | −10.7 ± 9.6 | −6.1 ± 8.3 | −8.0 (−13.9 to −2.1) | −4.5 (−9.0 to −0.1) | 3.5 (−2.4 to 9.3) |
| Knee joint kinetics, % c | ||||||
| Peak TKJM | 13.3 ± 3.0 | 10.4 ± 2.8 | 13.0 ± 2.5 | −2.9 (−4.8 to −1.1) | −2.6 (−3.9 to −1.4) | 0.3 (−1.6 to 2.1) |
| KFM at peak TKJM | 12.1 ± 3.2 | 9.2 ± 3.6 | 12.5 ± 2.6 | −2.9 (−5.0 to −0.9) | −3.3 (−4.9 to −1.6) | −0.3 (−2.4 to 1.7) |
| KAM at peak TKJM | 2.6 ± 3.2 | 2.4 ± 2.6 | 1.9 ± 2.4 | −0.2 (−2.0 to 1.6) | 0.6 (−0.9 to 2.1) | 0.8 (−1.0 to 2.6) |
| KERM at peak TKJM | 1.4 ± 1.0 | 1.3 ± 1.2 | 1.5 ± 1.3 | −0.1 (−0.8 to 0.6) | −0.3 (−1.0 to 0.5) | −0.2 (−0.9 to 0.5) |
| Knee adduction angular impulse | 0.4 ± 0.4 | 0.3 ± 0.2 | 0.2 ± 0.3 | −0.1 (−0.3 to 0.1) | 0.0 (−0.1 to 0.2) | 0.1 (−0.1 to 0.3) |
Data are reported as mean ± SD unless otherwise indicated. Boldface values indicate statistically significant difference between groups compared (P < .05). KAA, knee adduction angle; KAM, knee adduction moment; KERM, knee external rotation moment; KFA, knee flexion angle; KFM, knee flexion moment; KRA, knee rotation angle; TKJM, total knee joint moment.
CI, Confidence Interval
All kinetic data were normalized to body weight × height and are reported as percentages.
Discussion
In the current study, lower TKJM was observed in the affected limb compared with the healthy group during walking and running. However, differences in TKJM between the affected limb and the contralateral limb were only apparent during running and the late stance phase of walking. Lower TKJM in the affected limb is likely to be a result of altered knee loading strategies in the sagittal and transverse planes. These differences could be associated with a number of factors including greater kinesiophobia and lower quadriceps strength; however, further research is needed to confirm this.
This is the first study to examine TKJM during walking and running in individuals who had a meniscectomy as a result of a traumatic meniscal injury compared with the contralateral limb and healthy individuals. In those with medial knee OA, TKJM remained constant over 5 years with the dominant component that contributed to TKJM shifting from KFM to KAM. 3 Greater KAM and lower KFM were also observed in studies that have examined walking postmeniscectomy after a degenerative meniscal injury.24,55 In this study, when compared with the contralateral knee and healthy knees, the meniscectomy (affected) knee demonstrated lower TKJM, which was due to lower KFM and KRM during running and walking, respectively. These findings could provide insight into early rehabilitation approaches after surgery. However, further research is needed to examine whether TKJM changes over time and how the individual moment components contribute to the TKJM.
Lower peak KFM has previously been reported in individuals after a meniscectomy during walking,24,55 jogging, 25 treadmill running, 61 and bilateral landing. 19 The lower KFM (early stance) and KEM (late stance) observed in this study suggests the affected limb was employing a quadriceps avoidance strategy to reduce anterior knee loading associated with contraction of the quadriceps.19,21 In asymptomatic individuals with evidence of knee degeneration, lower KEM and higher knee flexion angles during late stance were also demonstrated, suggesting compensatory changes before individuals were clinically diagnosed. 15 During walking, the affected limb also demonstrated higher knee flexion angle during late stance. Higher knee flexion angles during late stance are suggested to be a result of greater activity of the hamstrings and are often employed in ACL-deficient knees as a strategy to offset quadriceps activity during propulsion and improve knee stability. 28 Greater hamstring activity has been previously reported in those who had a meniscectomy compared with healthy controls. 54 This approach is often reported in individuals who are ACL-deficient and individuals with medial knee OA in a response to weaker quadriceps, poorer stability, and pain. 3
The running speed of participants in this study (3.6 m/s) was faster than that in previous studies exploring knee biomechanics in jogging (2.5 m/s) 25 and treadmill running (3.3 m/s). 61 During the midstance of running, where TKJMs are greatest, KFM and knee flexion angles were found to be lower in the affected limb compared with the contralateral limb. Lower KFM despite a more extended knee could be a result of other coping strategies to reduce the moment arm such as greater forward lean or altered ankle motion. These findings were similar to those reported in individuals after a meniscectomy during jogging. 25 Lower KFM observed during dynamic tasks such as jogging, treadmill running, and landing is suggested to be a strategy to offload the knee and is attributed to the observed quadriceps muscle weakness.19,25,61 Similar to previous reports, the affected limb demonstrated quadriceps weakness when compared with the healthy group during the first year postsurgery22,24,55 and was therefore likely to contribute to the lower KFM observed in the affected limb. Unlike previous reports,22,56 the contralateral limb also demonstrated lower quadriceps strength compared with the healthy group, possibly as a result of decreased sport activity postsurgery. Despite weaker quadriceps in the contralateral limb compared with healthy individuals, no differences in TKJM and KFM were observed between the contralateral and healthy groups. These findings suggest that the strategy employed by the affected limb is not solely a response to weaker quadriceps; thus, psychological aspects may play a part.
Similar to previous studies,55,61 the meniscectomy group reported lower perceived knee function compared with the healthy group. In particular, for the KOOS Pain subscale, the meniscectomy group reported 23.7 points lower compared with the healthy group. These findings were similar to Thorlund et al 55 and although the meniscectomy patients in the current study were 5.7 months postsurgery and had returned to sport, these patients still perceived poorer knee-related function and higher knee-related pain. In addition to perceived pain, individuals after a meniscectomy demonstrated higher (5 point change) kinesiophobia compared with the healthy group. Higher kinesiophobia is also common after ACL reconstruction 58 and is often reported in individuals who have developed patellofemoral pain 13 and knee OA. 38 Heightened kinesiophobia can delay recovery and return to sport and influence movement strategies and muscle activity.13,27,38 In female patients with patellofemoral pain, altered knee biomechanics during stair descent were associated with kinesiophobia rather than quadriceps strength. 13 Given that quadriceps strength was similar between the affected and contralateral limbs, the lower KFM and subsequent TKJM observed in the affected leg compared with the contralateral leg was likely influenced by higher kinesiophobia, perceived pain, and poorer perceived knee function. Addressing kinesiophobia and fear-avoidance movements is likely to facilitate recovery after a meniscectomy. 21 However, further exploration of kinesiophobia on recovery after a meniscectomy is needed.
During walking, the affected limb demonstrated lower internal rotation moments during late stance compared with the healthy group. These findings are similar to those reported in ACL-deficient patients during walking and have been termed the pivot-shift avoidance strategy. 21 During late stance of walking when the knee is extended or partially flexed, internal rotation moments are normally produced to allow for a stable knee joint. 2 However, when stability is compromised, such as in ACL-deficient knees, there is a tendency to avoid high internal rotation moments. 21 The meniscus also plays a role in stabilizing the knee; in particular, the lateral meniscus acts as a secondary restraint for axial and rotatory loads.20,44 Partial removal of the meniscus will compromise the ability of the meniscus to stabilize the knee 44 and could lead to altered movement strategies. This is the first study to provide evidence to suggest a pivot-shift avoidance strategy in individuals after a meniscectomy. Rehabilitation approaches that address the strategies used to offload the knee, possibly due to muscle weakness and greater kinesiophobia, could improve recovery after a meniscectomy.
Previously, greater KAM values have been reported in the affected meniscectomy limb compared with the contralateral limb and healthy group during walking and jogging.24,25,55 However, our findings do not reflect these previous reports where KAM did not differ between limbs or groups in this study. KAM has been used to indicate loading on the medial aspect of the knee and has been associated with degenerative changes in the medial compartment of the knee in individuals with knee OA.12,43 As knee OA progresses, KAM has been shown to increase and become the dominant contributor to TKJM. 3 In this study, we examined individuals between 3 and 12 months after a meniscectomy; therefore, KAM changes may not be apparent until after this period. Hall et al24,25 reported increases in the affected limb at 2 years after surgery when compared with 3 months postsurgery.
Limitations
Several limitations to this study should be acknowledged. First, due to the retrospective design, it is unclear whether the individuals evaluated in the meniscectomy group showed similar muscle weaknesses and loading strategies before their injury or whether this was a consequence of surgery. However, our findings reflect those of previous studies exploring frontal and sagittal knee loading.24,25,55,61 Our sample size was restricted due to resource constraints. The sensitivity analysis revealed that with the study sample, this study was able to detect effect sizes ≥0.83 when comparing the meniscectomy and healthy groups and 0.46 when comparing the meniscectomy knee and contralateral knee. Our findings explored linear movements such as walking and running; however, it is important to note that when individuals progress towards returning to sport, they are likely to be required to perform multidimensional movements such as changes of direction and landing-based movements. These types of movements place greater demand on the individuals and their knees; therefore, future studies should explore sport-specific movements to improve ecological validity and generalizability.
Our sample consisted of individuals who underwent either a medial or a lateral meniscectomy. Although this has introduced heterogeneity into our data, our ancillary analysis did not observe statistical differences between medial and lateral meniscectomies during this first year after surgery. 52 Participants included in this study were recruited between 3 and 12 months postsurgery with a mean time of assessment of 5.7 ± 2.9 months postsurgery. Although participants were required to compete or participate in sport to be eligible for this study, they were likely to be at different stages of recovery, which could increase the variability of the results. Future studies should explore knee loading throughout the rehabilitation postsurgery for those who sustained traumatic meniscal injury. Rehabilitation strategies and the length of structured rehabilitation programs are important in reducing kinesiophobia and improving strength and movement patterns before return to sport.31,58 However, we did not collect information regarding rehabilitation after surgery. Future research should consider exploring rehabilitation approaches on kinesiophobia and knee loading after a meniscectomy.
Conclusion
In the first year after a meniscectomy, individuals who sustained a traumatic meniscal injury had lower TKJM in the affected limb during walking and running. Lower TKJM is likely to be a result of altered knee-loading strategies in the sagittal and transverse planes. Factors such as lower perceived knee function, higher perceived pain, greater kinesiophobia, and lower quadriceps strength may explain the differences in TKJM; however, further research is needed to confirm this. Lower KFM and knee flexion angles suggest individuals offload their knee in the first year after a meniscectomy. Rehabilitation strategies are needed to improve knee function in the affected knee after a meniscectomy.
Acknowledgments
The authors thank the Manchester Institute of Health and Performance for their support and use of facilities for this study.
Appendix
Appendix Figure A1.
Ensemble mean of sagittal, frontal, and transverse (A-C) knee joint angles in degrees and (D-F) knee joint moments normalized to body weight (BW) and height during walking for each group: the healthy group (solid) and affected leg (dashed) and contralateral leg (dotted) for the meniscectomy group.
Appendix Figure A2.
Ensemble mean of sagittal, frontal, and transverse (A-C) knee joint angles in degrees and (D-F) knee joint moments normalized to body weight and height during running for each group: the healthy group (solid) and affected leg (dashed) and contralateral leg (dotted) for the meniscectomy group.
Footnotes
Final revision submitted June 5, 2023; accepted June 19, 2023
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from University of Salford (reference No. 18/EE/0015).
References
- 1. Abram SGF, Price AJ, Judge A, Beard DJ. Anterior cruciate ligament (ACL) reconstruction and meniscal repair rates have both increased in the past 20 years in England: hospital statistics from 1997 to 2017. Br J Sports Med. 2020;54(5):286-291. [DOI] [PubMed] [Google Scholar]
- 2. Andriacchi TP, Dyrby CO. Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J Biomech. 2005;38(2):293-298. [DOI] [PubMed] [Google Scholar]
- 3. Asay JL, Erhart-Hledik JC, Andriacchi TP. Changes in the total knee joint moment in patients with medial compartment knee osteoarthritis over 5 years. J Orthop Res. 2018;36(9):2373-2379. [DOI] [PubMed] [Google Scholar]
- 4. Badlani JT, Borrero C, Golla S, Harner CD, Irrgang JJ. The effects of meniscus injury on the development of knee osteoarthritis: data from the osteoarthritis initiative. Am J Sports Med. 2013;41(6):1238-1244. [DOI] [PubMed] [Google Scholar]
- 5. Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1-48. [Google Scholar]
- 6. Beaufils P, Becker R, Kopf S, et al. Surgical management of degenerative meniscus lesions: the 2016 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):335-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bell AL, Brand RA, Pedersen DR. Prediction of hip joint centre location from external landmarks. Hum Mov Sci. 1989;8(1):3-16. [Google Scholar]
- 8. Boyer KA, Angst MS, Asay J, Giori NJ, Andriacchi TP. Sensitivity of gait parameters to the effects of anti-inflammatory and opioid treatments in knee osteoarthritis patients. J Orthop Res. 2012;30(7):1118-1124. [DOI] [PubMed] [Google Scholar]
- 9. Cappozzo A, Catani F, Della Croce U, Leardini A. Position and orientation in space of bones during movement. Clin Biomech (Bristol, Avon). 1995;10(4):171-178. [DOI] [PubMed] [Google Scholar]
- 10. Chahla J, Cinque ME, Godin JA, et al. Meniscectomy and resultant articular cartilage lesions of the knee among prospective national football league players: an imaging and performance analysis. Am J Sports Med. 2018;46(1):200-207. [DOI] [PubMed] [Google Scholar]
- 11. Chatain F, Adeleine P, Chambat P, Neyret P. A comparative study of medial versus lateral arthroscopic partial meniscectomy on stable knees: 10-year minimum follow-up. Arthroscopy. 2003;19(8):842-849. [DOI] [PubMed] [Google Scholar]
- 12. Chehab EF, Favre J, Erhart-Hledik JC, Andriacchi TP. Baseline knee adduction and flexion moments during walking are both associated with 5 year cartilage changes in patients with medial knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(11):1833-1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. de Oliveira Silva D, Barton CJ, Briani RV, et al. Kinesiophobia, but not strength is associated with altered movement in women with patellofemoral pain. Gait Posture. 2019;68:1-5. [DOI] [PubMed] [Google Scholar]
- 14. Dempster WT. Space Requirements of the Seated Operator: Geometrical, Kinematic, and Mechanical Aspects of the Body, With Special Reference to the Limbs. WADC technical report 55-159. Wright Air Development Center; 1955. [Google Scholar]
- 15. Edd SN, Favre J, Blazek K, Omoumi P, Asay JL, Andriacchi TP. Altered gait mechanics and elevated serum pro-inflammatory cytokines in asymptomatic patients with MRI evidence of knee cartilage loss. Osteoarthritis Cartilage. 2017;25(6):899-906. [DOI] [PubMed] [Google Scholar]
- 16. Edd SN, Giori NJ, Andriacchi TP. The role of inflammation in the initiation of osteoarthritis after meniscal damage. J Biomech. 2015;48(8):1420-1426. [DOI] [PubMed] [Google Scholar]
- 17. Englund M. Degenerative meniscus lesions, cartilage degeneration, and osteoarthritis of the knee. In: Hulet C, Pereira H, Peretti G, Denti M, eds. Surgery of the Meniscus. Springer Berlin Heidelberg; 2016:79-91. [Google Scholar]
- 18. Erhart-Hledik JC, Chu CR, Asay JL, Favre J, Andriacchi TP. Longitudinal changes in the total knee joint moment after anterior cruciate ligament reconstruction correlate with cartilage thickness changes. J Orthop Res. 2019;37(7):1546-1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ford KR, Minning SJ, Myer GD, Mangine RE, Colosimo AJ, Hewett TE. Landing adaptations following isolated lateral meniscectomy in athletes. Knee Surg Sports Traumatol Arthrosc. 2011;19(10):1716-1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fox AJSS, Wanivenhaus F, Burge AJ, Warren RF, Rodeo SA. The human meniscus: a review of anatomy, function, injury, and advances in treatment. Clin Anat. 2015;28(2):269-287. [DOI] [PubMed] [Google Scholar]
- 21. Fuentes A, Hagemeister N, Ranger P, Heron T, De Guise JA. Gait adaptation in chronic anterior cruciate ligament-deficient patients: pivot-shift avoidance gait. Clin Biomech (Bristol, Avon). 2011;26(2):181-187. [DOI] [PubMed] [Google Scholar]
- 22. Ganderup T, Jensen C, Larsen AH. Recovery of lower extremity muscle strength and functional performance in middle-aged patients undergoing arthroscopic partial meniscectomy. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):347-354. [DOI] [PubMed] [Google Scholar]
- 23. Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136. [DOI] [PubMed] [Google Scholar]
- 24. Hall M, Wrigley TV, Metcalf BR, et al. A longitudinal study of strength and gait after arthroscopic partial meniscectomy. Med Sci Sports Exerc. 2013;45(11):2036-2043. [DOI] [PubMed] [Google Scholar]
- 25. Hall M, Wrigley TV, Metcalf BR, et al. Knee biomechanics during jogging after arthroscopic partial meniscectomy: a longitudinal study. Am J Sports Med. 2017;45(8):1872-1880. [DOI] [PubMed] [Google Scholar]
- 26. Hanavan EP. A Mathematical Model for the Human Body. Technical report AMRL-TDR-64-102. Aerospace Medical Research Laboratories; 1964. [PubMed] [Google Scholar]
- 27. Hart HF, Collins NJ, Ackland DC, Crossley KM. Is impaired knee confidence related to worse kinesiophobia, symptoms, and physical function in people with knee osteoarthritis after anterior cruciate ligament reconstruction? J Sci Med Sport. 2015;18(5):512-517. [DOI] [PubMed] [Google Scholar]
- 28. Hart JM, Ko JWK, Konold T, Pietrosimone B. Sagittal plane knee joint moments following anterior cruciate ligament injury and reconstruction: a systematic review. Clin Biomech (Bristol, Avon). 2010;25(4):277-283. [DOI] [PubMed] [Google Scholar]
- 29. Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. J Educ Behav Stat. 1981;6(2):107-128. [Google Scholar]
- 30. Hsu CJ, George SZ, Chmielewski TL. Association of quadriceps strength and psychosocial factors with single-leg hop performance in patients with meniscectomy. Orthop J Sports Med. 2016;4(12):2325967116676078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jahan A, Dmitrievna M, Ismayilova M. Development and preliminary validation of a new protocol for postoperative rehabilitation of partial meniscectomy. J Hum Sport Exerc. 2018;13(3):577-600. [Google Scholar]
- 32. Jones RK, Nester CJ, Richards JD, et al. A comparison of the biomechanical effects of valgus knee braces and lateral wedged insoles in patients with knee osteoarthritis. Gait Posture. 2013;37(3):368-372. [DOI] [PubMed] [Google Scholar]
- 33. Kopf S, Beaufils P, Hirschmann MT, et al. Management of traumatic meniscus tears: the 2019 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1177-1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kristianslund E, Krosshaug T, Van den Bogert AJ. Effect of low pass filtering on joint moments from inverse dynamics: implications for injury prevention. J Biomech. 2012;45(4):666-671. [DOI] [PubMed] [Google Scholar]
- 35. Kumar D, Manal KT, Rudolph KS. Knee joint loading during gait in healthy controls and individuals with knee osteoarthritis. Osteoarthritis Cartilage. 2013;21(2):298-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kuznetsova A, Brockhoff PB, Christensen RHB. LmerTest package: tests in linear mixed effects models. J Stat Softw. 2017;82:1-26. [Google Scholar]
- 37. Lee JH, Heo JW, Lee DH. Comparative postural stability in patients with lateral meniscus versus medial meniscus tears. Knee. 2018;25(2):256-261. [DOI] [PubMed] [Google Scholar]
- 38. Leeuw M, Goossens MEJB, Linton SJ, Crombez G, Boersma K, Vlaeyen JWS. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30(1):77-94. [DOI] [PubMed] [Google Scholar]
- 39. Lewinson RT, Maag CP, Lun VMY, Wiley JP, Patel C, Stefanyshyn DJ. A three dimensional approach for quantifying resultant loading at the knee. Knee. 2017;24(1):31-39. [DOI] [PubMed] [Google Scholar]
- 40. Meireles S, De Groote F, Reeves ND, et al. Knee contact forces are not altered in early knee osteoarthritis. Gait Posture. 2016;45:115-120. [DOI] [PubMed] [Google Scholar]
- 41. Miller RP, Kori SH, Todd DD. No he Tampa Scale: a measure of kinesiophobia. Clin J Pain. 1991;7(1):51. [Google Scholar]
- 42. Mitchell J, Graham W, Best TM, et al. Epidemiology of meniscal injuries in US high school athletes between 2007 and 2013. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):715-722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38(8):1591-1597. [DOI] [PubMed] [Google Scholar]
- 45. Orendurff MS, Kobayashi T, Tulchin-Francis K, et al. A little bit faster: lower extremity joint kinematics and kinetics as recreational runners achieve faster speeds. J Biomech. 2018;71:167-175. [DOI] [PubMed] [Google Scholar]
- 46. Petersen J, Sørensen H, Nielsen RØ. Cumulative loads increase at the knee joint with slow-speed running compared to faster running: a biomechanical study. J Orthop Sports Phys Ther. 2015;45(4):316-322. [DOI] [PubMed] [Google Scholar]
- 47. Roemer FW, Kwoh CK, Hannon MJ, et al. Partial meniscectomy is associated with increased risk of incident radiographic osteoarthritis and worsening cartilage damage in the following year. Eur Radiol. 2017;27(1):404-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88-96. [DOI] [PubMed] [Google Scholar]
- 49. Searle SR, Speed FM, Milliken GA. Population marginal means in the linear model: an alternative to least squares means. Am Stat. 1980;34(4):216-221. [Google Scholar]
- 50. Sinclair J, Richards J, Taylor PJ, Edmundson CJ, Brooks D, Hobbs SJ. Three-dimensional kinematic comparison of treadmill and overground running. Sports Biomech. 2013;12(3):272-282. [DOI] [PubMed] [Google Scholar]
- 51. Skou ST, Hölmich P, Lind M, et al. Early surgery or exercise and education for meniscal tears in young adults. NEJM Evidence. 2022;1(2):1-12. doi: 10.1056/EVIDoa2100038 [DOI] [PubMed] [Google Scholar]
- 52. Starbuck C, Walters V, Herrington L, Barkatali B, Jones R. No differences in knee joint loading between individuals who had a medial or lateral meniscectomy: an ancillary study. Knee. 2023;42:304-311. [DOI] [PubMed] [Google Scholar]
- 53. Stein T, Mehling AP, Welsch F, Von Eisenhart-Rothe R, Jäger A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38(8):1542-1548. [DOI] [PubMed] [Google Scholar]
- 54. Sturnieks DL, Besier TF, Lloyd DG. Muscle activations to stabilize the knee following arthroscopic partial meniscectomy. Clin Biomech (Bristol, Avon). 2011;26(3):292-297. [DOI] [PubMed] [Google Scholar]
- 55. Thorlund JB, Holsgaard-Larsen A, Creaby MW, et al. Changes in knee joint load indices from before to 12 months after arthroscopic partial meniscectomy: a prospective cohort study. Osteoarthritis Cartilage. 2016;24(7):1153-1159. [DOI] [PubMed] [Google Scholar]
- 56. Thorlund JB, Østengaard L, Cardy N, Wilson F, Jørgensen C, Juhl CB. Trajectory of self-reported pain and function and knee extensor muscle strength in young patients undergoing arthroscopic surgery for meniscal tears: a systematic review and meta-analysis. J Sci Med Sport. 2017;20(8):712-717. [DOI] [PubMed] [Google Scholar]
- 57. Thorp LE, Sumner DR, Wimmer MA, Block JA. Relationship between pain and medial knee joint loading in mild radiographic knee osteoarthritis. Arthritis Care Res. 2007;57(7):1254-1260. [DOI] [PubMed] [Google Scholar]
- 58. Tichonova A, Rimdeikienė I, Petruševičienė D, Lendraitienė E. The relationship between pain catastrophizing, kinesiophobia and subjective knee function during rehabilitation following anterior cruciate ligament reconstruction and meniscectomy: a pilot study. Medicina (Kaunas). 2016;52(4):229-237. [DOI] [PubMed] [Google Scholar]
- 59. Walter JP, Korkmaz N, Fregly BJ, Pandy MG. Contribution of tibiofemoral joint contact to net loads at the knee in gait. J Orthop Res. 2015;33(7):1054-1060. [DOI] [PubMed] [Google Scholar]
- 60. Wilkerson GB, Colston MA, Baker CS. A sport fitness index for assessment of sport-related injury risk. Clin J Sport Med. 2016;26(5):423-428. [DOI] [PubMed] [Google Scholar]
- 61. Willy RW, Bigelow MA, Kolesar A, Willson JD, Thomas JS. Knee contact forces and lower extremity support moments during running in young individuals post-partial meniscectomy. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):115-122. [DOI] [PubMed] [Google Scholar]
- 62. Xu C, Zhao J. A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. 2013;23(1):164-170. [DOI] [PubMed] [Google Scholar]