Abstract
The aim was to evaluate if rehabilitation procedures including occupational health (OH) and workplace participation increase return to work (RTW) rates among patients with subacute and chronic low back pain (LBP). A systematic review of randomized controlled trials was conducted using the PubMed and Cochrane databases. Main outcomes were RTW and days of sick leave. Interventions needed to be multidisciplinary including both OH and active workplace involvement in rehabilitation. Out of 1073 potentially eligible references, 8 met the inclusion criteria. Three studies had OH and 5 case managers involved in rehabilitation. Rehabilitation involving both OH and workplace improved RTW and decreased the number of sick leave days among LBP patients. Having case managers involved had no effect in RTW. In order to improve RTW, workplace visits and work ability meetings (WAMs) between OH and workplace are essential components in the rehabilitation process among patients with chronic LBP. Based on the study results, the authors suggest utilizing these co-operative interventions with workplaces in OH. High quality research investigating only the effect of WAMs in OH setting is needed in future.
Keywords: low back pain, rehabilitation, intervention, workplace, return to work, sick leave
INTRODUCTION
Chronic low back pain (LBP) is a major health problem worldwide and is considered one of the leading disorders causing disability [1,2]. Disability to work has serious consequences for all stakeholders and society. Despite numerous guidelines to improve the quality of care [3], LBP remains a major workability burden needing attention and more effective procedures to be tackled.
Disability to work is a versatile aspect and always comparable to a person's work tasks. Exercise alone or in combination with education is effective for preventing LBP [4]. Exercise therapy can have rehabilitative effects for sub-acute and chronic LBP [5]. It can be assumed that right amount of physical activity in work has a potential in rehabilitating subacute and chronic LBP.
Back schools are educational training programs introduced in 1969 with the aim of treating and preventing LBP. Back schools have been suggested to decrease pain and improve functional status especially in occupational setting [6]. Yet, when it comes to chronic LBP, recent studies have found weak or no evidence on the effectiveness of back school programs [7].
Rehabilitation is a multifaceted person-centred concept in medicine [8] being essentially a multidisciplinary way of acting in health care. Individual needs and factors introduce variability into rehabilitation procedures even within the same program. The rehabilitation process can include various programs such as ergonomic evaluation or individual rehabilitation procedures. For LBP participatory ergonomics [9] and graded activity programs [10] have been introduced. Participatory ergonomics is designed for preventive care but can also be implemented during a sick leave [11]. Graded activity is an individual, gradually increased exercise program with an operant-conditioning behavioural approach based on the results of the tests and the demands of the patient's work. Also, Cochrane review in 2015 concluded that multidisciplinary rehabilitation programs have positive effects on RTW among chronic LBP patients [12].
Occupational health (OH) is typically considered as a medical specialty focusing on disease prevention, protection of occupational diseases and work-related injuries [13]. Other procedures of the OH vary from country to country. Because of the variability, content of the OH ser vices is difficult to generalise. However, global mutual features can be identified. For example, OH has a solid link between the employee and employer. According to international legislation, employers must arrange OH which provides information about the risks and demands related to work and working environment. Occupational health professionals have to be able to carry out the assessment of workability. Therefore, these assets make OH a potentially powerful operator considering LBP rehabilitation.
For occupational back pain, one of the most known rehabilitation programs has been the Sherbrooke model since 1994 [14]. Sherbrooke model is a multidisciplinary 3-step template linking the employee, worksite, and OH into the same program. Sherbrooke model of rehabilitation has been shown to increase return to work (RTW) rate [15,16] and have favourable cost-benefit and cost-effectiveness profile [17].
Rehabilitation is usually carried out in health care services, but it is possible to also include workplaces into this program in the early stage. If chronic disability is already present, multimodal medical rehabilitation needs to be combined with vocational rehabilitation in order to reduce absenteeism and disability pensions [18]. It is essential that workplace is integrated into rehabilitation as soon as possible [18]. The authors assume that early, safe, and long-term RTW especially during the recovery process requires co-operation between the employee, healthcare professionals and the employer.
In Finland, employers are required to take part in the rehabilitation of employees after 90 days of sick leave at the latest. A work-ability meeting (WAM) consisting of the employee, the manager (or supervisor) of the work organisation and an OH physician is arranged by the OH provider and a rehabilitation plan is made [19]. The main topic in the meeting is the employee's work ability. Specific diagnostics are not discussed due to professional confidentiality of personal medical records. The aim of the meeting is to find means to enable RTW. If RTW is not rightly foreseeable, rehabilitation will continue outside the worksite but planned and followed by the OH. If RTW does not seem attainable in the future, vocational rehabilitation or disability pension will be applied after the meeting.
Often employees with ongoing illness can return to work after work accommodation, modification, or vocational rehabilitation. Good praxis includes support from the supervisor and OH as well as follow up.
The aim of the present study is to examine the effectiveness of rehabilitation procedures in which both employer and OH have an active role in RTW and days of sick leave in subacute or chronic LBP.
METHODS
Search strategy
PubMed and Cochrane library databases were searched for relevant studies from January 1, 1990 to December 17, 2022. The authors applied the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [20]. The keywords and the search strategy were (low back pain [Mesh Terms]) AND ((rehabilitation, vocational [Mesh Terms]) OR (rehabilitation) OR (intervention)) AND ((workability) OR (return to work) OR (return NEAR work) OR (sick leave [Mesh Terms]) OR (sickness absence) OR (absenteeism [Mesh Terms]) OR (disability pension)). Total 1015 studies using PubMed search engine was found. Search for trials and systematic reviews was performed separately in the Cochrane library. The keywords and the search strategy for Cochrane trial search were ((chronic low back pain) OR (sub-acute low back pain)) AND (rehabilitation) AND ((occupational health) OR (case manager)). From the Cochrane library 15 trials and 56 systematic reviews were found. After removing duplicates there were 1073 references to potentially eligible studies in total.
Study selection
To be included in the review, primary research studies had to satisfy the following criteria:
-
–
low back pain (≥ 4 weeks),
-
–
at least 1 OH specialist or case manager included in rehabilitation team,
-
–
active workplace involvement in rehabilitation,
-
–
numeric outcome as RTW, sick leave days or disability pension,
-
–
clear control group,
-
–
follow-up time >6 months,
-
–
the full text being available in English.
Studies were excluded in case of:
-
–
articles not fulfilling the above criteria,
-
–
specific low back pain (eq. disc herniation),
-
–
back surgery within 6 months,
-
–
pregnancy,
-
–
occupational therapists not considered as an actor of the OH.
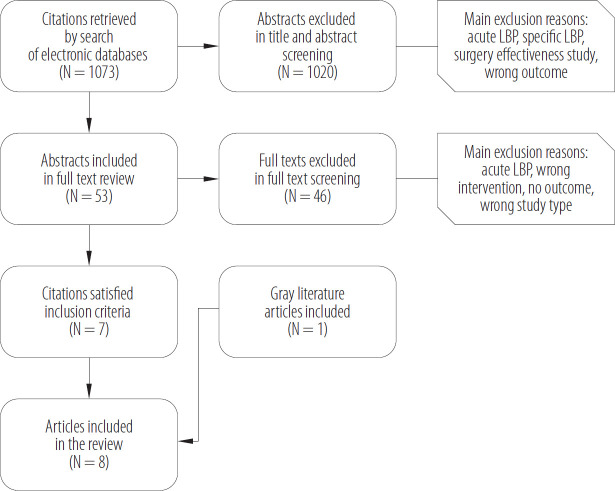
All citations identified by PubMed search were downloaded into the Covidence systematic review management tool. Title and abstract screening were performed by pairs of 2 reviewers. The authors included 53 articles during the title and abstract screening (Figure 1). The abstract was included if 1 reviewer saw a possible inclusion. The identified abstracts were further examined in full text screening. The authors only included randomized controlled trials (RCTs) or trials with a relevant control group. The reference lists of review articles and included studies were examined in order to identify articles which were not found in the database searches. Two reviewers examined each full text article and potential disagreements were discussed among all 3 reviewers and the final decision on the inclusion was based on consensus. The authors identified a total of 5 studies consisting of 8 articles. Seven of the articles were found in the database searches and 1 in grey literature.
Figure 1.
Flowchart representing selection process of the low back pain (LBP) rehabilitation studies including active workplace involvement and occupational health or case managers in the intervention, published in 1997–2022
Data abstraction
The data was extracted mainly by 1 reviewer and the extraction results were examined in meetings with 2 other reviewers. The focus of the data was on the interventions concerning OH/case managers, active workplace involvement, numeric outcome as RTW or sick leave days. Due to the small number of included studies and the heterogeneity between them in regard to interventions and outcomes, meta-analysis was deemed infeasible.
Interventions
Interventions were required to be multidisciplinary including both OH and active workplace involvement in rehabilitation in the intervention group. Occupational health was considered to be involved if at least 1 OH specialist was mentioned. Case managers were recognized to have similar interconnections with employees and employers as OH have. Occupational therapists separately were not considered as an actor of the OH as they focus on everyday living and are typically independent professionals, unattached from OH. If an occupational therapist were described to be part of the OH team, they would be recognized as OH. There were case managers as occupational therapists in some cases. However, OH and case managers were examined separately. Workplace involvement needed to be active. The employer not attending workplace visits or just paying the health bills were not considered as active involvement of the workplace.
Methodological quality assessment
For quality assessment, Joanna Briggs Institute (JBI) critical appraisal tools for RCT-studies (JBI, Adelaide, Australia) were used (Table 1). The authors evaluated true randomization, concealed randomization, allocation, blinding, follow-up time, randomization, and outcomes.
Table 1.
Joanna Briggs Institute critical appraisal checklist for randomized controlled trials for the included low back pain (LBP) rehabilitation studies having active workplace involvement and occupational health or case managers in the intervention, published in 1997–2022
| Study | True randomization | Allocation to treatment groups concealed | Treatment groups similar at the baseline | Blinded participants to treatment assignment | Patients delivering treatment blind to treatment assignment | Outcomes assessors blind to treatment assignment | Treatment groups treated identically other than the intervention of interest | Complete followup | Participants analysed In the groups where they were randomized | Outcomes measured in the same way for treatment groups | Outcomes measured in a reliable way | Appropriate statistical analysis | Appropriate trial design |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Finland, 2003 [21] | yes | yes | yes | no | no | unclear | yes | yes | yes | yes | yes | yes | yes |
| The Netherlands, 2010 [22] | yes | yes | yes | no | no | no | yes | yes | yes | yes | yes | yes | yes |
| Canada, 1997 [15] | yes | yes | yes | unclear | unclear | ho | yes | yes | yes | yes | yes | yes | yes |
| Denmark, 2011 [23] | yes | no | yes | no | no | no | yes | yes | yes | yes | yes | yes | yes |
| Denmark, 2012 [24] | yes | no | yes | no | no | no | yes | yes | yes | yes | yes | yes | yes |
| Denmark, 2018 [25] | yes | no | yes | no | no | no | yes | yes | yes | yes | yes | yes | yes |
| Denmark, 2021 [26] | yes | no | yes | no | no | no | yes | yes | yes | yes | yes | yes | yes |
| Denmark, 2022 [27] | yes | no | yes | no | no | no | yes | yes | yes | yes | yes | yes | yes |
RESULTS
Study selection
Eight articles were found to satisfy the inclusion criteria [15,21–27]. Several potentially very relevant articles were excluded mostly because of lacking the involvement of OH or workplace or both. Furthermore, studies which did have workplace visits, but the employer was not actively attending to them, were excluded. For such reasons, e.g., graded activity programs were excluded [28]. Also, if RTW or sick leave days were not given, studies were excluded even if interventions were acceptable [29].
Characteristics of the selected studies
Characteristics of the included studies are presented in Table 2. Follow-up time in the trials was at least 12 months. Three of the studies had OH [15,21,22] and 5 had case managers [23–27] as an operator in the rehabilitation. Two of the studies were considered great quality with no holes in the interventions or outcomes [15,22]. Work-place active involvement in rehabilitation did not reach 100% in 6 studies [21–27] for such reasons as termination of employment or lack of motivation of employers. However, active workplace intervention was still >85% in all studies.
Table 2.
Characteristics of the low back pain (LBP) rehabilitation studies (published in 1997–2022 in Finland, the Netherlands, Canada and Denmark) including active workplace involvement and occupational health (OH) or case managers in the intervention
| Study | Study population and design | Total sample/subgroup sample number | Randomization/allocation | Intervention | Control group | Outcome and follow-up | Potential confounders* |
|---|---|---|---|---|---|---|---|
| Finland, 2003 [21] | patients were recruited from 36 primary health care centres in the Helsinki metropolitan area (RCT) | total N = 164 subgroups:
|
|
Worksite visit group consisted of mini-intervention and worksite visit. The FIOH physiotherapist visited the patient's worksite. The patient's work supervisor and OH of the company joined the session (86% of cases employers attended). The aim of the visit was to ensure practical instructions of appropriate ergonomics at work with the cooperation of OH and employer. In mini-intervention, patient had appointments with physiatrist and physiotherapist and continued with graded activity and light mobilisation program. | Usual care group: patients in the usual care group were not examined but did receive an informative leaflet about back pain (as did all other study patients). They were treated by their GPs in public primary health care, including specialist consultations and physiotherapy, if assessed necessary by the GP. Patients could also have visited private doctors if they paid the costs of the visits themselves. | sick leaves resulting from back pain (1 year) | LBP for >4 weeks but <3 months age (M (range)):
gender: females
blue-collar workers:
losses during follow-up: 1 in usual care group (total <1%) |
| The Netherlands, 2010 [22] | outpatient clinic patients of the participating hospitals in Amsterdam (RCT) | total N = 134 subgroups:
|
|
The integrated care consisted of a workplace intervention based on participatory ergonomics and a graded activity programme. The intervention was provided by a team consisting of a care manager, clinical occupational physician, GP, a medical specialist, an occupational therapist, and a graded activity therapist. Care coordinators were occupational physicians trained for the task. Every patient had an appointment with care coordinator at the start. In the workplace intervention OT visited a workplace and discussed between patient and supervisor finding feasible solutions for RTW. | Usual care was passive observation of the health care usage. Healthcare use of all the patients was monitored during the 12 months of follow-up. In most cases usual care consisted of treatment by a physiotherapist (N = 42) or manual therapist (N = 20). Only a few patients visited their occupational physician (N = 16) or general practitioner (N = 10). Compared to the integrated care, patients in the usual care group received more diagnostic tests, used more analgesics and had more consultations for manual therapy, Cesar therapy, medical specialist, and psychological care. |
|
LBP lasting >12 weeks and patients being on sick leave (also partial sick leave) age (M±SD ):
gender: females
radiculopathy: not evaluated physical work:
losses during follow-up:
|
| Canada, 1997 [15] | patients were recruited from workplaces (which had >175 employees) in the Sherbrooke are (Canada, Quebec) (RCT) | total N = 104 subgroups:
|
|
Sherbrooke model is a 3-step rehabilitation program combining occupational intervention and clinical intervention. Occupational arm included only the occupational intervention. In the first step on sixth week of absence occupational doctor examines the worker and physiotherapist visits the worksite. Afterwards the meeting was held with the worker and the employer to find sustainable solutions for return to work. Second step was clinical intervention which included back pain specialist appointment after 8 weeks of absence from work. If needed, third step began after 12 weeks consisting of multidisciplinary intervention with functional restoration and cognitive-behavioural therapy. | At the start of the study, every study group (including standard care group) got an educational video of back pain and employers got a questionnaire. The physicians in standard care group had no limitations compared with their usual work. The physicians did not get advice about return to work as other groups had. | HR (1 year) | LBP and absence from regular work for >4 weeks age (M±SD) years:
gender: females
|
| Denmark, 2011 [23], 2012 [24], 2018 [25] | patients from 9 municipalities in Denmark Region were referred to The Spine Centre by their GP (RCT) | [23, 24] total N = 351 subgroups:
[25]: total N = 464 second study population (N = 120) was included to the previous subgroups:
|
all studies:
|
In addition to the BI described next, RTW plan was performed by a case manager and the treatment continued with the same rheumatologist and physiotherapist, along with a specialist in clinical social medicine and a social worker. The first visit for the case manager was taken place few days after the allocation to treatment groups. Follow-up visits were scheduled if needed. The multidisciplinary team had regular meetings. The case manager and a participant made a rehabilitation plan together. If suitable, the case manager assisted at a meeting at the workplace or contacted the employer by phone. Later, if RTW was deemed unrealistic, a plan for vocational rehabilitation was made (e.g., in some cases participants started other jobs supported by the social system). | Before allocation to treatment groups, all study patients had a similar clinical examination in the beginning, which was carried out by a rheumatologist and a physiotherapist (double blinded before the allocation). Relevant examinations and imaging were scheduled. In the visits patients with nonspecific LBP were informed about exercise being the best treatment. Patients with sciatica were informed about the good spontaneous prognosis and beneficial exercises for the pain. All study participants had a second visit to the physiotherapist after 2 weeks. The BI group participants were informed to book appointments with their GP, if they needed continuation for sick leave or needed advice for RTW. | HR (RTW to regular work) (1, 2 years)
employment status “cumulative weeks at work” (1, 2, 3, 4 and 5 years) |
[23, 24]: LBP and sick listed 3–16 weeks
age (M±SD):
gender: females
physical work: not evaluated radiculopathy:
losses during follow-up:
[25]: gender: females 58.3% age (M±SD):
radiculopathy: not evaluated losses during follow-up: 0 |
| Denmark, 2021 [26], 2022 [27] | patients from 9 municipalities in Denmark Region were referred to The Spine Centre by their GP (RCT) | total N = 476 new study group subgroups:
|
all studies:
|
Multidisciplinary intervention was similar as in the previous Danish study. As in the earlier study the case manager arranged a meeting in workplace with an employer or called the employer by phone. Both interventions happened only if they were approved by the participant. | Brief intervention was similar as in the previous Danish study. Rheumatologist does all the relevant tests and imaging for the diagnosis. Similar fear avoidance advises were given for all participants. | HR (RTW) in weak and strong job relation groups (1, 2 years) | LBP and partial or full sick leave for 4–12 weeks
age (M±SD):
gender, females:
physical work: not evaluated radiculopathy:
losses during follow-up: 0 (RTW was analysed for every participant) |
Bl - brief intervention; f IOH - Finnish Institute of Occupational Health; GP - general practitioner; HR - hazard ratio per protocol; IBP - low back pain; MOI - multidisciplinary intervention; OH - occupational health; OT - occupational therapist; RCT - randomized controlled trial; RTW - return to work.
Low back pain, age, gender, sciatica, losses during follow-up.
The included Finnish study [21] had a governmental OH operator guiding the rehabilitation. The intervention consisted of workplace visits by a governmental OH physiotherapist. During the visit, patients could already have returned to work. Therefore, outcome was selected as days of sick leave during the 12 months resulting from back pain. Occupational health services (OHS) attended the workplace visits in 82% of the cases. Employer attendance was 86% of the visits. The focus of the visits was finding adapted work techniques. Yet, the employer had the authority to fulfil them or not.
The study from the Netherlands [22] had workplace multidisciplinary rehabilitation intervention based on participatory ergonomics and a graded activity programme. Occupational health physician was coordinating the rehabilitation. Supervisor, patient, and all health care team members were evaluating obstacles on RTW. During the program patient, supervisor, and occupational therapist discussed in the meeting possible solutions for the obstacles of the RTW. The aim of the workplace intervention was to achieve consensus between patient and supervisor regarding solutions for RTW. Work adaptations were executed if needed and deemed executable. The Canadian study [15] had Sherbrooke model rehabilitation in the intervention group. The study had a total of 4 groups (Sherbrooke, occupational, clinical arms, and standard care) and examined the combined and separate effectiveness of the occupational groups (Sherbrooke and occupational arm) for RTW. The authors' focus was on all the results as both occupational groups fulfilled their inclusion criteria. In both occupational groups, the meeting was held with the employee and the employer to find sustainable solutions for RTW.
The 5 Danish studies [23–27] had case managers making the rehabilitation plan for RTW. The authors noticed the control groups of brief intervention (BI) had almost the same clinical specialists (except case managers) in the beginning of the trial. Therefore they were good studies to evaluate the effect of the case managers for RTW as fewer confounding factors were present. The multidisciplinary intervention (MDI) groups included rehabilitation physician, a physiotherapist, a specialist in clinical social medicine, a social worker, and an occupational therapist. In each case, 1 of the last mentioned 3 professionals was assigned as case manager. Case manager kept in contact with the participant and was a part of the multidisciplinary team. The problems were discussed at regular team conferences where the participant was not present. If accepted by the participant, the case manager assisted at a meeting at the workplace or contacted the employer by phone. It can be assumed the participant was not present when the employer was contacted by phone. Appointments with other members of the team and meetings at the workplace or at the social service centre were regularly arranged. Two study groups in the 5 articles were identified. In 3 trials [23–25], LBP patients were recruited when sick listed 3–16 weeks. The trials were designed to have LBP patients sick listed from work 4–12 weeks but difficulties in scheduling first appointments in Spine Centre made LBP range wider. The study aim was to find studies minimum of 4 weeks of LBP. It can be assumed that in most cases LBP symptoms started few days prior to sick leave. Also median of the cases is clearly in the inclusion limits. The small number of intervention studies fulfilling all the inclusion criteria in the review study made the authors include the 3 Danish studies which are determined as high-quality studies. The 2 latest Danish studies [26,27] with the same intervention had LBP patients on partial or full sick leave for 4–12 weeks.
Workplace interventions with OH
The results of the included studies are presented in Table 3. In 3 trials, the intervention consisted of OH and an active workplace involvement in the rehabilitation process. In 2 of them [15,21], workplace intervention was carried out by a workplace visit and a concurrent meeting which employer attended. The remaining trial [22] had meeting(s) outside the worksite with OH, employee and employer. The employer had the final say to execute suggested work adaptations or not. In 2 studies intervention groups returned to work significantly faster than control groups [15,21]. In the Dutch study, the integrated care group returned to work faster than the usual care group with clear statistically significant results (RR = 1.83, 95% CI: 1.24–2.93). In the Canadian Sherbrooke model study, occupational groups (Sherbrooke and occupational arm together) returned to work faster than groups that not included occupational intervention (RR = 1.91, 95% CI: 1.18–3.1). The Sherbrooke model group returned to work even faster compared with the usual care group (RR = 2.23, 95% CI: 1.19–4.89). In the Finnish study, the group having workplace visits by the governmental OH institute had fewer sick leave days than the usual care group, but the result was not statistically significant.
Table 3.
Comparing effectiveness of the low back pain (LBP) rehabilitation studies including active workplace involvement and occupational health or case managers to the control groups for return to work (RTW) and sick leave days, published in 1997–2022
| Study | Outcome | Follow-up | Results | 95% CI | p |
|---|---|---|---|---|---|
| Finland, 2003 [21] | sick leaves resulting from back pain | 1 year |
|
0.071 | |
| The Netherlands, 2010 [22] | HR (RTW hazard ratio per protocol) | 1 year |
|
1.24–2.93 | 0.007 |
| RTW (days until) |
|
0.003 | |||
| sick leave days (including recurrences) |
|
0.003 | |||
| Canada, 1997 [15] | HR (RTW) | 1 year |
|
1.19–4.89 | 0.01 |
|
1.18–3.1 | <0.01 0.26 | |||
| Denmark, 2011 [23] | HR (RTW) | 1 year | MDI returned to work 0.84 times faster than BI | 0.65–1.08 | 0.18 |
| 2012 [24] | 2 years | MDI vs. BI 0.86 | 0.68–1.09 | ||
| 2018 [25] | employment status at work “cumulative weeks at work” | 5 years | MDI 140.5 weeks vs. BI 151.4, difference 10.8 weeks | −6.7–28.4 | |
| Denmark, 2021 [26] | HR (RTW) in weak and strong job relation groups | 1 year |
|
0.55–0.96 | <0.05 |
|
0.77–1.49 | ||||
| 2022 [27] | 2 years |
|
0.57–0.96 | ||
|
0.73–1.34 |
BI – brief intervention; HR – hazard ratio; IQR – interquartile range; MDI – multidisciplinary intervention.
Workplace interventions with case managers
Case managers were used instead of OH in 5 trials with a follow-up time of 1–5 years [23–27]. In 2 trials, the MDI groups had returned to work less often than the BI control groups at 1, 2 and 5 years but the results were not statistically significant [23–25] (Table 3). In addition, patients with strong job relation in the MDI intervention group returned to work less often than those in the control groups (RR 0.73, 95% CI: 0.55–0.96) [26]. The same results concerning strong job relation were seen also in the 2-year-follow-up study [27]. Therefore it seems that patients who have strong influence on their job, do not benefit from multidisciplinary programs with workplace intervention due to the fact that they can modify their job themselves.
Ideas and prospective research
In this systematic review, the authors examined if rehabilitation in OH is more beneficial with the active involvement of the workplace in the rehabilitation process compared to processes without it. Their findings suggest that the co-operation of the OH and worksite increase RTW among sub-acute and chronic LBP patients. The effective co-operation is achieved by collective meetings or work-place visits by employee, manager, and OH specialist. The meetings can be arranged at the workplace or at OHS. Based on the study results, these co-operative interventions with workplace in OH have a big effect and utilizing them in rehabilitation of LBP patients is recommended. However, introducing the interventions in OH may be challenging. OHS vary globally and the contents of the services are difficult to generalize [30]. Other specialities such as orthopaedics and physiatry have more similarities with each other from country to country. In some countries, OH covers only preventive work like risk assessment which affects the applicability of the results in other countries. However, OH commonality worldwide being the link to the employer has a huge potential in improving the rehabilitation results in chronic LBP.
For example, employers in Finland are legally obliged to have occupational health care for all employees [31]. Thus, OHS has a unique opportunity to provide services to support the work ability of all employees.
Case managers are widely used in some countries such as Denmark. Their professional background may be very heterogenous whereas OH professionals have education in health care. For example, in the Danish studies included in this review, the case managers were either specialists in social medicine, social employees, or occupational therapists.
If an employee has more or less permanent LBP symptoms or disability, work modifications are usually needed in order to succeed in RTW. Sometimes even minor modifications can make significant effect. As exercise is proved beneficial for LBP, it can be assumed that adapted work has a potential as a rehabilitative step. Also, a work-place visit or meeting itself can make an impact without the need for work modifications in cases with lack of information or fear-avoidance. The objective of the meetings is to discuss about the employee's work ability and its prognosis in order to build a feasible RTW plan.
The authors defined active workplace involvement as meetings or workplace visits that employer actively attended. Concerning sub-acute and chronic LBP patients, recovery often happens gradually and mild symptoms can alternate and continue for weeks or months. Procedures of getting employees RTW before they are fully recovered benefit of the cooperation of the health care and workplace. Russo et al. [32] found in their systematic review that workplace interventions improve clinical outcomes such as RTW in a worker population affected by LBP. These findings are similar to the authors' study results suggesting that sessions with all the parties concerned are a good platform for tackling the obstacles for RTW especially in OH.
Lappalainen et al. [33] found in a survey to supervisors concerning WAMs that collaboration with OHS is an important option for supervisors to enhance work modifications and the work participation of employees with work disability. Collaboration with OH can advance work modifications and lead to medical procedures to improve work performance. Supervisor training, companies' explicit disability management policy, and collaboration with OHS all advance employee's work participation. Four key elements were identified by the supervisors as major success factors in the negotiations [34]. It was crucial that the supervisors learned about the employee's health restrictions and understood the issues relating to their work disability and the parties aim for common solutions and conclusions through collaboration. Active participation of all negotiation parties is important. Supervisors gave a high rating to OHS taking their views seriously and appreciated collaboration in a constructive atmosphere [33].
Employer's and employee's motivation to RTW plays a big role. The employer has the authority to fulfil the recommended modifications for LBP employees returning to work. Work accommodation, vocational rehabilitation, and partial work is not possible if supervisor and work-place are not involved in RTW process. If the employee is valuable for the company, the motivation to rehabilitate the person sooner is self-evident. Also, if the employer pays the sick leave benefit bills and tariff of possible disability pension, it can be assumed being motivated for fast rehabilitation. For example, in Finland and in the Netherlands, employers have the above-mentioned responsibilities during sick leave which encourage the cooperation aiming for faster RTW.
Motivation to find sharable solutions in stakeholders, employer, and employee, may vary. Faber et al. [35] has reported 7 topic areas of motivation: intrinsic motivation, extrinsic motivation, goal setting, expectancy, values, self-efficacy, and work readiness that seem to have a role in motivation for work participation among young people with disabilities. Motivational interviewing, a very feasible tool in OHS, can help facilitate behavior change and potentially reduce work disability and improve RTW outcomes among injured employers [36].
People who have strong influence on the job and can modify their job by themselves do not seem to benefit from multidisciplinary programs in LBP rehabilitation. Self-determination and self-efficacy are important in engagement of vocational rehabilitation among disabled individuals with low engagement, motivation, and ambivalence to employment [37]. Services that promote working alliance, autonomy, and self-efficacy of persons with disabilities may increase their capacity to obtain employment.
There are potential weaknesses in the authors' systematic review study. Even the included studies are considered as high-quality studies, there were just a few of them satisfying all the study selection criteria. The 3 studies concerning OH as an operator is far less than it was desired for the study. Secondly, workplace interventions were not a primary study focus in the included trials. The interventions were multidisciplinary and workplace interventions were a part of a big picture. This fact makes rest of interventions as confounding factors when answering to the study question. Also, workplace interventions did not reach 100% in all the included studies most likely due to the same fact. As the authors did not have access to original data of the trials, they could not erase the cases, which might skew the results in some way.
Work ability is a versatile aspect consisting of health, motivation, and work tasks. With the co-operation of employee, manager, and health care in OH injurious work assignments and motivation to sooner RTW can be tackled.
CONCLUSIONS
In chronic LBP, rehabilitation without active involvement of the employer and the workplace is bound to fail when it comes to increase RTW or decrease days of sick leave. Work ability meetings with all parties concerned is an efficient means to achieve the rehabilitation goals. High quality studies investigating only the effect of WAMs in OH setting is needed for the future.
ACKNOWLEDGMENTS
Diana Gagliardi, Ritta Sauni, Juha Liira
Footnotes
Funding: this study was supported by the Instituto Nazionale per L'assicurazione contro gli Infortune sul Lavoro (INAIL) and by the University of Helsinki (grant No. H3715 wbs 4721249). Open access was funded by the Helsinki University Library.
Author contributions
Research concept: Valtteri Kokkonen, Anne Lamminpää, Kari Reijula, Fabrizio Russo, Sergio Iavicoli, Vincenzo Denaro, Jaana Kuoppala
Research methodology: Valtteri Kokkonen, Anne Lamminpää, Kari Reijula, Jaana Kuoppala
Collecting material: Valtteri Kokkonen, Anne Lamminpää, Jaana Kuoppala
Statistical analysis: Valtteri Kokkonen, Anne Lamminpää, Jaana Kuoppala
Interpretation of results: Valtteri Kokkonen, Anne Lamminpää, Kari Reijula, Fabrizio Russo, Sergio Iavicoli, Vincenzo Denaro, Jaana Kuoppala
References: Valtteri Kokkonen, Anne Lamminpää, Kari Reijula, Jaana Kuoppala
REFERENCES
- 1.Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800. 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2021 Low Back Pain Collaborators. Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023;5(6):e316–29. 10.1016/S2665-9913(23)00098-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oliveira C, Maher C, Pinto R, Traeger A, Lin C, Chenot J-F, et al. Clinical practice guidelines for the management of nonspecific low back pain in primary care: an updated overview. Eur Spine J. 2018;27(11):2791–803. 10.1007/s00586-018-5673-2. [DOI] [PubMed] [Google Scholar]
- 4.Steffens D, Maher C, Pereira L, Stevens M, Oliveira V, Chapple M, et al. Prevention of Low Back Pain: A Systematic Review and Meta-analysis. Jama Intern Med. 2016;176(2): 199–208. 10.1001/jamainternmed.2015.7431. [DOI] [PubMed] [Google Scholar]
- 5.Hayden J, van Tulder M, Malmivaara A, Koes B. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev. 2005;2005(3):CD000335. 10.1002/14651858.CD000335.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heymans M, van Tulder M, Esmail R, Bombardier C, Koes B. Back schools for non-specific low-back pain. Cochrane Database Syst Rev. 2004;18(4):CD000261. 10.1002/14651858.CD000261.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Straube S, Harden M, Schröder H, Arendacka B, Fan X, Moore R, et al. Back schools for the treatment of chronic low back pain: possibility of benefit but no convincing evidence after 47 years of research – systematic review and metaanalysis. Pain. 2016;157(10):2160–72. 10.1097/j.pain.0000000000000640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization [Internet]. Rehabilitation [cited 2023 April 7]. Available from: https://www.who.int/newsroom/fact-sheets/detail/rehabilitation.
- 9.King P. Participatory Ergonomics A Group Dynamics Perspective. Work. 1994;4(3):195–200. 10.3233/WOR-1994-4307. [DOI] [PubMed] [Google Scholar]
- 10.Lindstöm I, Ohlund C, Eek C, Wallin L, Peterson L, Fordyce W, et al. The Effect of Graded Activity on Patients with Subacute Low Back Pain: A Randomized Prospective Clinical Study with an Operant-Conditioning Behavioral Approach. Phys Ther. 1992;72(4):279–90. 10.1093/ptj/72.4.279. [DOI] [PubMed] [Google Scholar]
- 11.Lambeek L, Anema J, van Royen B, Buijs P, Wuisman P, van Tulder M, et al. Multidisciplinary outpatient care program for patients with chronic low back pain: design of a randomized controlled trial and cost-effectiveness study. BMJ Public Health 2007;7:254. 10.1186/1471-2458-7-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kamper S, Apeldoorn A, Chiarotto A, Smeets R, Ostelo R, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ 2015;350:1–11. 10.1136/bmj.h444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teufer B, Ebenberger A, Affengruber L, Kien C, Klerings I, Szelag M, et al. Evidence-based occupational health and safety interventions: a comprehensive overview of reviews. BMJ Open 2019;9(12):1–9. 10.1136/bmjopen-2019-032528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loisel P, Durand P, Abenhaim L, Gosselin L, Simard R, Turcotte J, et al. Management of occupational back pain: the Sherbrooke model. Results of a pilot and feasibility study, Occup Environ Med. 1994;51(9):597–602. 10.1136/oem.51.9.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loisel P, Abenhaim L, Durand P, Esdaile J, Suissa S, Gosselin L, et al. A population-based, randomized clinical trial on back pain management, Spine. 1997;22(24):2911–8. 10.1097/00007632-199712150-00014. [DOI] [PubMed] [Google Scholar]
- 16.Durand M-J, Loisel P. Therapeutic Return to Work: Rehabilitation in the workplace. Work. 2001;17(1):57–63. [PubMed] [Google Scholar]
- 17.Loisel P, Lemaire J, Poitras S, Durand M-J, Champagne F, Stock S, et al. Cost-benefit and cost-effectiveness analysis of a disability prevention model for back pain management: a six year follow up study. Occup Environ Med. 2002; 59(12): 807-15. 10.1136/oem.59.12.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuoppala J, Lamminpää A. Rehabilitation and work ability: a systematic literature review. J Rehabil Med. 2008; 40(10):796–804. 10.2340/16501977-0270. [DOI] [PubMed] [Google Scholar]
- 19.Honkonen N, Liira J, Lamminpää A, Liira H. Work ability meetings – a survey of Finnish occupational physicians. Occup Med. 2018;68(8):551–4. 10.1093/occmed/kqy115. [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman D; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;3(3):e123–30. [PMC free article] [PubMed] [Google Scholar]
- 21.Karjalainen K, Malmivaara A, Pohjolainen T, Hurri H, Mutanen P, Rissanen P, et al. Mini-intervention for subacute low back pain: a randomized controlled trial. Spine. 2003; 28(6):533–40. 10.1097/01.BRS.0000049928.52520.69. [DOI] [PubMed] [Google Scholar]
- 22.Lambeek L, van Mechelen W, Knol D, Loisel P, Anema J. Randomised controlled trial of integrated care to reduce disability from chronic low back pain in working and private life. BMJ. 2010;340:1–7. 10.1136/bmj.c1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jensen C, Jensen O, Christiansen D, Nielsen C. One-year follow-up in employees sick-listed because of low back pain: randomized clinical trial comparing multidisciplinary and brief intervention. Spine. 2011;36(15):1180–9. 10.1097/BRS.0b013e3181eba711. [DOI] [PubMed] [Google Scholar]
- 24.Jensen C, Jensen O, Nielsen C. Sustainability of return to work in sick-listed employees with low-back pain. Two-year follow-up in a randomized clinical trial comparing multidisciplinary and brief intervention. BMC Musculoskelet Disord. 2012;13:156. 10.1186/1471-2474-13-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pedersen P, Nielsen C, Jensen O, Jensen C, Labriola M. Employment status five years after a randomised controlled trial comparing multidisciplinary and brief intervention in employees on sick leave due to low back pain. Scand J Public Health. 2018;46(3):383–8. 10.1177/1403494817722290. [DOI] [PubMed] [Google Scholar]
- 26.Langagergaard V, Jensen O, Nielsen C, Jensen C, Labriola M, Sørensen V, et al. The comparative effects of brief or multidisciplinary intervention on return to work at 1 year in employees on sick leave due to low back pain: A randomized controlled trial. Clin Rehab. 2021;35(9):1290–304. 10.1177/02692155211005387. [DOI] [PubMed] [Google Scholar]
- 27.Pedersen K, Langagergaard V, Jensen O, Nielsen C, Sørensen V, Pedersen P. Two-Year Follow-Up on Return to Work in a Randomised Controlled Trial Comparing Brief and Multidisciplinary Intervention in Employees on Sick Leave Due to Low Back Pain. J Occup Rehab. 2022;32(4): 697-704. 10.1007/s10926-022-10030-1. [DOI] [PubMed] [Google Scholar]
- 28.Steenstra I, Anema J, Bongers B, de Vet H, Knol D, van Mechelen W. The effectiveness of graded activity for low back pain in occupational healthcare. Occup Environ Med. 2006; 63(11):718–25. 10.1136/oem.2005.021675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lambeek L, van Mechelen W, Buijs B, Loisel P, Anema J. An integrated care program to prevent work disability due to chronic low back pain: a process evaluation within a randomized controlled trial. BMC Musculoskeletal Disorders. 2009;10:147. 10.1186/1471-2474-10-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization [Internet]. Good practice in occupational health services: a contribution to workplace health. 2002, Regional Office for Europe. P. 3. Available from: https://apps.who.int/iris/handle/10665/107448. [Google Scholar]
- 31.Ministry of Social Affairs and Health, Finland [Internet]. Occupational Healthcare Act [cited 2023 April 19]. Available from: https://finlex.fi/fi/laki/kaannokset/2001/en20011383.pdf.
- 32.Russo F, Papalia G, Gianluca V, Fontana L, Iavicoli S, Papalia R, et al. The Effects of Workplace Interventions on Low Back Pain in Workers: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021;18(23):12614. 10.3390/ijerph182312614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lappalainen L, Liira J, Lamminpää A, Rokkanen T. Work disability negotiations: supervisors' view of work disability and collaboration with occupational health services. Disability Rehab. 2019;41(17):2015–25. 10.1080/09638288.2018.1455112. [DOI] [PubMed] [Google Scholar]
- 34.Lappalainen L, Liira J, Lamminpää A. Work disability negotiations between supervisors and occupational health services: factors that support supervisors in work disability management. Intl Arch Occup Environ Health. 2021; 94(4):689–697. 10.1007/s00420-020-01623-5. [DOI] [PubMed] [Google Scholar]
- 35.Faber B, Wind H, Frings-Dresen M. An interview guide for clinicians to identify a young disabled person's motivation to work. Work. 2016;54(3):577–90. 10.3233/WOR-162337. [DOI] [PubMed] [Google Scholar]
- 36.Park J, Gross D, Rayani F, Norris C, Roberts M, James C, et al. Model of Human Occupation as a framework for implementation of Motivational Interviewing in occupational rehabilitation. Work. 2019;62(4):629–41. 10.3233/WOR-192895. [DOI] [PubMed] [Google Scholar]
- 37.Tansey TN, Iwanaga K, Bezyak J, Ditchman N. Testing an integrated self-determined work motivation model for people with disabilities: A path analysis. Rehab Psychol. 2017;62(4):534–544. 10.1037/rep0000141. [DOI] [PubMed] [Google Scholar]